Abstract
BACKGROUND.
Lung cancer incidence rates among American Indians and Alaska Natives (AI/ANs) in the United States have not been described well, primarily because of race misclassification and, until the 1990s, incomplete coverage of their population by cancer registries. Smoking, the predominant cause of lung cancer, is particularly prevalent among this population.
METHODS.
Data from the National Program of Cancer Registries and the Surveillance, Epidemiology, and End Results Program were combined to estimate age-adjusted incidence rates of lung cancer during 1999 through 2004. Cases were linked to Indian Health Service (IHS) registration databases to identify AI/ANs whose race may have been misclassified. Age-adjusted rates were calculated for Contract Health Service Delivery Area (CHSDA) counties and for all counties by IHS region, and comparisons were made between AI/ANs and non-Hispanic whites (NHWs).
RESULTS.
Among populations living in CHSDA counties, NHWs overall had higher rates of lung cancer than AI/ANs. However, the rates (per 100,000 population) among AI/ANs varied substantially between IHS regions from 14.9 (South-west) to 87.1 (Southern Plains), 93.2 (Alaska), and 104.3 (Northern Plains). Approximately 41.6% of AI/AN lung cancer cases were diagnosed before age 65 years compared with approximately 29.8% of NHW lung cancer cases. The overall percentage stage distribution was not different between AI/ANs and NHWs. Squamous cell carcinomas were slightly more common and adenocarcinomas were less common among AI/ANs than among NHWs. Lung cancer rates were not decreasing for AI/ANs as they were for NHWs.
CONCLUSIONS.
Data from this study clarified the need for culturally appropriate tobacco prevention and control policies and resources for AI/ANs in all regions, and especially in the Plains and Alaska.
Keywords: cancer, incidence, American Indian, Alaska Native, misclassification, National Program of Cancer Registries, Surveillance, Epidemiology, and End Results, United States, health disparity
In the United States, lung cancer is the most frequently diagnosed invasive cancer. Because it is difficult to treat, it is also the leading cause of cancer deaths, accounting for approximately 158,000 deaths each year in the United States.1 Although this cancer occurs throughout the United States population, incidence rates vary considerably between racial and ethnic populations, particularly because of the variations in tobacco use across the United States. Cigarette smoking is the most important cause of lung cancer, accounting for 90% of lung cancer deaths in males and 75%–80% of lung cancer deaths in females in the United States.2–4 Exposure to other risk factors for lung cancer, such as asbestos, naturally occurring radon gas in homes, and an occupational history of uranium mining, also are contributors.1,5–12
Several studies have demonstrated that AI/AN cancer incidence historically has been underreported with the result that the burden of cancer in this population has been described inaccurately.13–16 This underreporting has 2 sources: First, AI/AN cancer incidence rates reported in the Surveillance, Epidemiology, and End Results (SEER) data were dominated by the large AI population ascertained by the New Mexico Tumor Registry (NMTR), which is one of the original SEER cancer registries, and often were cited as representative of all AI/AN populations in the United States. However, lung cancer incidence rates in the Southwestern AI population, as reflected in the NMTR data, are much lower than in other regions.17 A second source of the underreporting is that the race of AI/ANs often is misclassified in medical records, vital statistics, cancer registries, and other databases. Linking state cancer registry data with Indian Health Service (IHS) patient registration information can correct some underreporting because of the misclassification of race. In previous linkage studies, AI/AN mortality and incidence rates in some locations have doubled subsequent to such linkages.18,19
The objective of this study was to reduce the misclassification of AI/AN race through linkages with analyses restricted to the IHS Contract Health Services Delivery Area (CHSDA) counties, where a larger percent of the population is AI/AN and misclassification of AI/AN race is believed to be lower than in other counties.20 The cancer data used in this study are from population-based cancer registries across the United States and thereby provide an opportunity to present a more complete picture of lung cancer incidence in regional AI/AN populations.
MATERIALS AND METHODS
Case Identification
The cancer incidence data for this study were obtained from state and regional cancer registries throughout the United States for cases diagnosed during 1999 through 2004. All of these registries participate in either the Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries (NPCR) or the National Cancer Institute’s (NCI) SEER Program,21 or both. Data were included from those registries that agreed to participate and met the United States Cancer Statistics standards for high-quality data.21 Only 4 states were excluded from the analysis: Kansas, Maryland, South Carolina, and Vermont. Primary cancer site and histology data were coded according to the International Classification of Diseases for Oncology (ICD-O) edition in that was use at the time of diagnosis and are converted to the third edition.22 Invasive lung cancer cases were identified with the ICD-O version 3 codes C340 through C349.22 Histologies that involved hematopoietic diseases, mesothelioma, and Kaposi sarcoma were excluded (M9590–9989, 9050–9055, and 9140). For 1999 through 2000, SEER Summary Stage 1977 was used; for 2001 through 2003, SEER Summary Stage 2000 was used; and, for 2004, collaborative stage was coded, but the data were not available for analysis. For this study, stage data for 2001 through 2003 only are presented because of differences observed in comparative analyses of the 2 SEER Summary Stage systems.23,24 Cell types were classified as adenocarcinoma (M8140–8389, 8401, 8408, 8410–8411, 8413, 8441, 8450, 8460, 8470, 8480–8482, 8490, 8500, 8503–8504, 8510, 8520, 8525, 8530, 8560, 8571–8574, 8576, 9070, and 9110), squamous cell carcinoma (M8050–8071, 8074–8089, and 8094), small cell carcinoma (M8041, 8044, and 8073), and large cell carcinoma (M8012–8014, 8045, and 8072).25
To obtain the most accurate race information, states worked with the IHS to link cancer registry databases with IHS patient registration data. This linkage effectively identified those individuals who may not have been classified as AI/AN in the state cancer registries but were known to be members of federally recognized tribes and enrolled in the IHS healthcare system. If an individual was not identified as AI/AN in the cancer registry but was identified as AI/AN in the IHS database, then the individual was classified as AI/AN for this analysis. For more details about the linkage methodology, see the report by Espey et al in this supplement to Cancer.26 Hispanic origin was identified for all individuals in the registry databases using the North American Association of Central Cancer Registry Hispanic Identification Algorithm.27 Individuals who were included in the AI/AN race category were included regardless of Hispanic origin. For all analyses, AI/ANs were compared with NHWs.
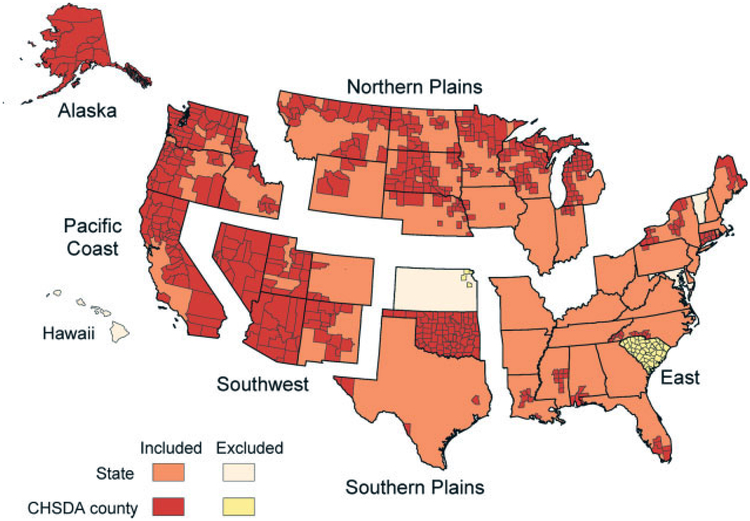
Population Estimates, Regional Definitions, and Geographic Coverage
County level annual population estimates for the years 1999 through 2004 were modified in 2 ways to be used in the denominators of the rate calculations. First, since 2000, the population estimates from the US Bureau of the Census have included data from individuals who identify themselves as belonging to more than 1 racial group. The CDC National Center for Health Statistics collaborated with the Bureau of the Census to develop methods for converting the multiple race data collected into single race categories.28 Second, the NCI provided additional refinements to race and county codes for use in the SEER*Stat software program.29,30 To assess regional variation in incidence, the states were grouped into 6 previously developed IHS regions (Fig. 1).26 The ‘all-counties’ incidence rates, for which no geographic restrictions apply, included data from registries in 46 states and the District of Columbia. For most tabulations, however, the analyses were restricted to ‘Contract Health Service Delivery Area’ (CHSDA) counties, which, in general, contain federally recognized tribal lands or are adjacent to tribal lands (Fig. 1). For incidence rates restricted to CHSDA counties, data from 33 registries were included. Restricting the analysis to CHSDA counties was another method used to minimize racial misclassification.26 Approximately 56% of the United States AI/AN population resides in CHSDA counties. This proportion varies by IHS region (Alaska, 100%; East, 13.1%; Northern Plains, 59%; Southern Plains, 64.1%; Pacific Coast, 55.6%; Southwest, 87.5%).
FIGURE 1.
States and Contract Health Service Delivery Areas (CHSDA) counties by Indian Health Service region are illustrated.
Statistical Analysis
Age-adjusted lung cancer incidence rates, expressed as the number of cases per 100,000 population and age-adjusted by 19 age groups to the 2000 United States standard population, were calculated for AI/AN and NHW populations using SEER*Stat software version 6.3.6.30 Percent distributions for stage and histology also were age-adjusted to the same standard population. For all analyses, exact counts were suppressed when the category of interest contained <6 cases.
By using the age-adjusted incidence rates, standardized rate ratios (RRs) were calculated for AI/AN populations using NHW rates for comparison. Confidence intervals (CIs) for age-adjusted rates and standardized RRs were calculated based on methods described by Tiwari et al31 using SEER*Stat 6.3.6.30 An RR >1.0 indicated that the AI/AN rate was greater than the NHW rate. Similarly, an RR <1.0 indicated an AI/AN rate less than the NHW rate. The annual percentage change (APC) was calculated for both AI/AN and NHW lung cancer incidence rates to assess trends during 1999 through 2004 (P<.05). Percentage changes were calculated using 2 years for each endpoint, and the APC was not calculated if it was based on fewer than 10 cases for at least 1 year within the time interval.
RESULTS
Lung cancer incidence rates in CHSDA counties varied nearly 7-fold for AI/ANs across IHS regions in the United States (Table 1). Among AI/ANs, rates were highest in the Northern Plains (104.3), Alaska (93.2), and the Southern Plains (87.1) and lowest in the Southwest (14.9). This same pattern was observed in the analysis of all counties combined, although the rates were lower and the variation was nearly 5-fold. Lung cancer incidence rates for NHWs did not exhibit the same magnitude of variation or the same pattern of regional variation; in the CHSDA counties, NHW rates were highest in the Southern Plains (82.2) and the East (74.2). All subsequent presentations of data refer to CHSDA county data unless noted otherwise.
TABLE 1.
Invasive Lung and Bronchus Cancer Incidence Rates by Indian Health Service Region and Sex for American Indians/Alaska Natives and Non-Hispanic Whites: United States, 1999–2004a
| CHSDA Counties | All Counties | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IHS Region | Sex | AI/AN Count | AI/AN Rateb | 95% Cl for AI/AN Rate | NHW Rateb | RR (AI/AN:NHW)c | 95% Cl for RR | AI/AN Count | AI/AN Rateb | 95% Cl for AI/AN Rate | NHW Rateb | RR (AI/AN:NHW)c | 95% Cl for RR |
| Northern Plains | Both Sexes | 719 | 104.3 | 96.4–112.7 | 65.5 | 1.59d | 1.47–1.72 | 951 | 81.9 | 76.4–87.7 | 69.6 | 1.18d | 1.10–1.26 |
| Males | 349 | 119.8 | 106.3–134.3 | 84.6 | 1.42d | 1.25–1.59 | 467 | 95.9 | 86.4–106.1 | 89.7 | 1.07 | 0.96–1.18 | |
| Females | 370 | 93.8 | 84.1–104.2 | 51.1 | 1.83d | 1.64–2.04 | 484 | 72.6 | 66.0–79.7 | 55.3 | 1.31d | 1.19–1.44 | |
| Alaskae | Both sexes | 326 | 93.2 | 82.9–104.2 | 71.6 | 1.30d | 1.14–1.48 | 326 | 93.2 | 82.9–104.2 | 71.6 | 1.30d | 1.14–1.48 |
| Males | 185 | 115.3 | 97.9–134.7 | 85.0 | 1.36d | 1.13–1.62 | 185 | 115.3 | 97.9–134.7 | 85.0 | 1.36d | 1.13–1.62 | |
| Females | 141 | 75.4 | 63.1–89.1 | 60.7 | 1.24d | 1.02–1.50 | 141 | 75.4 | 63.1–89.1 | 60.7 | 1.24d | 1.02–1.50 | |
| Southern Plains | Both sexes | 1131 | 87.1 | 82.0–92.4 | 82.2 | 1.06 | 1.00–1.13 | 1227 | 69.3 | 65.4–73.5 | 77.3 | 0.90d | 0.85–0.95 |
| Males | 620 | 111.0 | 101.9–120.5 | 108.5 | 1.02 | 0.94–1.11 | 665 | 85.8 | 79.0–93.1 | 100.7 | 0.85d | 0.78–0.92 | |
| Females | 511 | 69.9 | 63.9–76.3 | 62.6 | 1.12d | 1.02–1.22 | 562 | 57.2 | 52.5–62.2 | 60.0 | 0.95 | 0.87–1.04 | |
| Pacific Coast | Both sexes | 605 | 51.8 | 47.5–56.4 | 70.1 | 0.74d | 0.68–0.80 | 755 | 35.8 | 33.1–38.6 | 66.8 | 0.54d | 0.50–0.58 |
| Males | 293 | 57.6 | 50.6–65.3 | 82.5 | 0.70d | 0.61–0.79 | 373 | 40.2 | 35.9–44.9 | 78.3 | 0.51d | 0.46–0.57 | |
| Females | 312 | 48.0 | 42.6–53.9 | 60.9 | 0.79d | 0.70–0.88 | 382 | 32.7 | 29.4–36.3 | 58.4 | 0.56d | 0.50–0.62 | |
| East | Both sexes | 144 | 46.8 | 39.2–55.4 | 74.2 | 0.63d | 0.53–0.75 | 639 | 28.4 | 26.1–30.8 | 75.8 | 0.37d | 0.34–0.41 |
| Males | 71 | 51.0 | 39.0–65.3 | 91.5 | 0.56d | 0.43–0.71 | 379 | 37.8 | 33.8–42.2 | 96.8 | 0.39d | 0.35–0.44 | |
| Females | 73 | 43.5 | 33.9–54.7 | 61.7 | 0.71d | 0.55–0.89 | 260 | 21.0 | 18.5–23.8 | 60.4 | 0.35d | 0.31–0.39 | |
| Southwest | Both sexes | 240 | 14.9 | 13.0–17.0 | 65.6 | 0.23d | 0.20–0.26 | 268 | 15.0 | 13.2–16.9 | 59.2 | 0.25d | 0.22–0.29 |
| Males | 144 | 21.2 | 17.7–25.1 | 77.3 | 0.27d | 0.23–0.33 | 161 | 21.1 | 17.8–24.8 | 70.9 | 0.30d | 0.25–0.35 | |
| Females | 96 | 10.4 | 8.4–12.7 | 56.3 | 0.18d | 0.15–0.23 | 107 | 10.5 | 8.6–12.7 | 50.1 | 0.21d | 0.17–0.25 | |
| Total | Both sexes | 3165 | 57.4 | 55.4–59.5 | 70.3 | 0.82d | 0.79–0.85 | 4166 | 43.8 | 42.4–45.2 | 72.4 | 0.61d | 0.59–0.62 |
| Males | 1662 | 69.5 | 66.0–73.2 | 85.9 | 0.81d | 0.77–0.85 | 230 | 53.7 | 51.3–56.2 | 91.4 | 0.59d | 0.56–0.61 | |
| Females | 1503 | 48.5 | 46.0–51.1 | 58.6 | 0.83d | 0.78–0.87 | 1936 | 36.5 | 34.8–38.2 | 58.5 | 0.62d | 0.60–0.65 | |
Source: Cancer registries in the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program.
CHSDA indicates Contract Health Service Delivery Area; IHS, Indian Health Service; AI/AN, American Indians/Alaska Natives; NHW, non-Hispanic whites; CI, confidence interval.
AI/AN race is reported by NPCR and SEER registries or through linkage with the IHS patient registration database. AI/AN persons of Hispanic origin are included.
Rates are per 100,000 persons and are age-adjusted to the 2000 U.S. standard population (19 age groups; Census P25–1130; see Day 199632).
RRs were calculated in SEER*Stat prior to rounding of rates and may not equal the RRs calculated from rates presented in the table.
The RR is statistically significant (P <.05).
Rates and RRs for Alaska in the CHSDA Counties section are the same as those in the All Counties section, because all counties in Alaska are CHSDA counties.
Years of data and registries used: 1999–2004 (41 states and the District of Columbia): Alaska,* Alabama,* Arkansas, Arizona,* California,* Colorado,* Connecticut,* the District of Columbia, Delaware, Florida,* Georgia, Hawaii, Iowa,* Idaho,* Illinois, Indiana,* Kentucky, Louisiana,* Massachusetts,* Maine,* Michigan,* Minnesota,* Missouri, Montana,* North Carolina,* Nebraska,* New Hampshire, New Jersey, New Mexico,* Nevada,* New York,* Ohio, Oklahoma,* Oregon,* Pennsylvania,* Rhode Island,* Texas,* Utah,* Washington,* Wisconsin,* West Virginia, and Wyoming*; 1999 and 2002–2004: North Dakota*; 2001–2004: South Dakota*; 2003–2004: Mississippi* and Virginia; 2004: Tennessee (asterisks indicate states with at least 1 county designated as a CHSDA).
Percentage regional coverage of AI/AN in CHSDA counties compared with AI/AN in all counties: Alaska, 100%; East, 13.1%; Northern Plains, 59.0%; Southern Plains, 64.1%; Pacific Coast, 55.6%; Southwest, 87.5%.
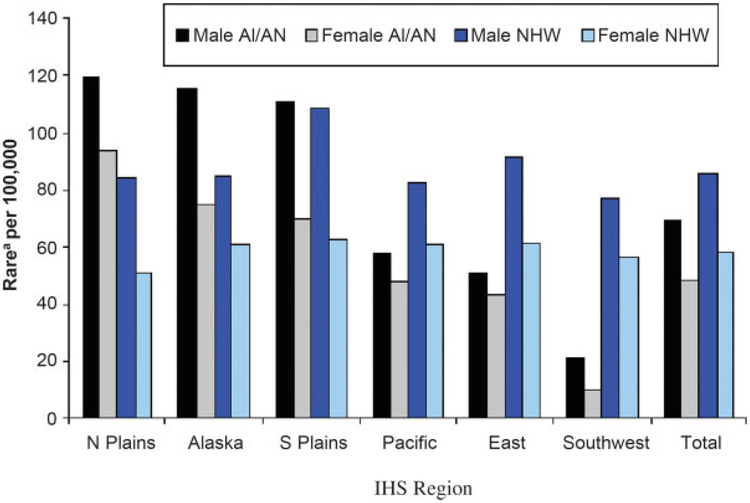
Among the populations living in CHSDA counties, AI/ANs had significantly higher rates (P <.05) of lung cancer than NHWs for both males and females in the Northern Plains and Alaska and for females in the Southern Plains (Table 1). In the Southern Plains, AI/AN males had lung cancer incidence rates that were approximately the same as those for NHWs, although that rate was significantly higher than the national NHW rate. In contrast, incidence rates for AI/ANs in the Pacific Coast, East, and Southwest regions all were significantly lower than the rates for NHWs in the same regions for both males and females (Table 1, Fig. 2).32 From 1999 through 2004, male NHW lung cancer incidence rates decreased significantly for all regions combined, whereas male AI/AN rates remained approximately level (Table 2). Over the same period, rates among AI/AN females and NHW females did not change.
FIGURE 2.
Lung and bronchus cancer incidence rates for American Indians and Alaska Natives (AI/AN) and non-Hispanic whites (NHW) by Indian Health Service (IHS) region and Sex in Contract Health Service Delivery Area (CHSDA) counties in the United States from 1999 to 2004. aRates are age-adjusted to 2000 United States standard population (19 age groups; Census P25–1130; see Day, 199632). N Plains indicates Northern Plains; S Plains, Southern Plains. Source: cancer registries in the Centers for Disease Control and Prevention’s National Program of Cancer Registries and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.
TABLE 2.
Invasive Lung and Bronchus Cancer Incidence Annual Percentage Change by Year of Diagnosis and Indian Health Service Region for American Indians/Alaska Natives and Non-Hispanic Whites in Contract Health Service Delivery Area Counties: United States, 1999–2004
| Both Sexes | Males | Females | ||||
|---|---|---|---|---|---|---|
| IHS Region | AI/AN APC | NHW APC | AI/AN APC | NHW APC | AI/AN APC | NHW APC |
| Northern Plains | −4.5 | −0.5 | −3.1 | −0.9 | −5.9 | −0.1 |
| Alaska | 5.6 | −2.6 | 2.0 | −0.7 | 10.8 | −5.2 |
| Southern Plains | 1.6 | −0.7 | 2.1 | −2.2 | 0.2 | 1.1 |
| Pacific Coast | 0.9 | −1.8a | 2.6 | −2.8a | 0.0 | −0.8a |
| East | −10.8 | −0.8a | −16.0a | −1.8a | −8.2 | 0.2 |
| Southwest | −5.1 | −1.1 | −2.8 | −2.1a | −7.5 | −0.1 |
| Total | −0.2 | −1.2a | 0.1 | −2.1a | −0.6 | −0.3 |
Source: Cancer registries in the Centers for Disease Control and Prevention’s National Program of Cancer Registries and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.
IHS indicates Indian Health Service; AI/AN, American Indians/Alaska Natives; APC, annual percentage change; NHW, non-Hispanic whites.
The APC is significantly different from zero (P<.05).
The highest rates among AI/ANs for each age group were in the Northern Plains, Alaska, and the Southern Plains (Table 3). Similar regional patterns were not observed for NHWs, and their highest rates were observed among those living in the Southern Plains and the East. Like for many other forms of cancer, rates increased with age, and the highest rates occurred in the oldest age group (aged >65 years). Among individuals aged ≥50 years, lung cancer incidence rates were significantly higher among AI/ANs than among NHWs in the Northern Plains and Alaska. Also, among individuals aged 50 years, the rates were significantly lower among AI/ANs than among NHWs in the Southwest, East, and Pacific Coast regions. AI/ANs were diagnosed with lung cancer at younger ages than NHWs. Among AI/ANs, 58.5% of cases were aged ≥65 years at diagnosis compared with 70.2% of cases among NHWs.
TABLE 3.
Invasive Lung and Bronchus Cancer Incidence Rates by Age and Indian Health Service Region for American Indians and Alaska Natives and Non-Hispanic Whites in Contract Health Service Delivery Area Counties: United States, 1999–2004
| <50 Years | 50–64 Years | ≥65 Years | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IHS Region | Count | % of Casesa | Rateb | 95% CI | Count | % of Casesa | Rateb | 95% CI | Count | % of Casesa | Rateb | 95% CI |
| AI/AN | ||||||||||||
| Northern Plains | 48 | 6.7 | 5.6 | 4.1–7.4 | 261 | 36.3 | 179.3c | 158.2–202.4 | 410 | 57.0 | 580.8c | 524.2–641.9 |
| Alaska | 19 | 5.8 | 4.6 | 2.8–7.1 | 113 | 34.7 | 163.2c | 134.4–196.2 | 194 | 59.5 | 517.0c | 445.0–597.5 |
| Southern Plains | 107 | 9.5 | 8.9 | 7.3–10.7 | 376 | 33.2 | 157.4 | 141.9–174.1 | 648 | 57.3 | 451.3 | 416.9–487.8 |
| Pacific Coast | 30 | 5.0 | 2.0d | 1.3–2.8 | 221 | 36.5 | 83.6d | 72.9–95.4 | 354 | 58.5 | 299.4d | 268.2–333.2 |
| East | 13 | 9.0 | 3.6 | 1.9–6.1 | 46 | 31.9 | 72.8d | 53.2–97.0 | 85 | 59.0 | 263.3d | 209.6–326.7 |
| Southwest | 13 | 5.4 | 0.6d | 0.3–1.1 | 68 | 28.3 | 20.9d | 16.2–26.5 | 159 | 66.3 | 89.7d | 76.1–105.0 |
| Total | 230 | 7.3 | 3.7d | 3.2–4.2 | 1085 | 34.3 | 98.0d | 92.3–104.0 | 1850 | 58.5 | 317.0d | 302.4–332.0 |
| NHW | ||||||||||||
| Northern Plains | 1686 | 5.0 | 4.9 | 4.7–5.2 | 8809 | 26.2 | 114.2 | 111.8–116.6 | 23,131 | 68.8 | 354.8 | 350.3–359.4 |
| Alaska | 111 | 8.8 | 4.6 | 3.8–5.5 | 450 | 35.9 | 108.5 | 98.6–119.1 | 694 | 55.3 | 411.9 | 381.2–444.4 |
| Southern Plains | 808 | 4.8 | 6.7 | 6.2–7.2 | 4521 | 27.1 | 148.8 | 144.5–153.3 | 11,333 | 68.0 | 435.3 | 427.3–443.4 |
| Pacific Coast | 2720 | 4.1 | 4.3 | 4.1–4.5 | 16,144 | 24.4 | 112.0 | 110.2–113.7 | 47,311 | 71.5 | 397.3 | 393.7–400.9 |
| East | 2358 | 4.7 | 5.9 | 5.6–6.1 | 12,572 | 25.0 | 130.8 | 128.5–133.1 | 35,331 | 70.3 | 398.1 | 393.9–402.3 |
| Southwest | 1095 | 3.8 | 4.3 | 4.1–4.6 | 7451 | 25.6 | 111.9 | 109.4–114.5 | 20,549 | 70.6 | 361.8 | 356.8–366.8 |
| Total | 8778 | 4.5 | 4.9 | 4.8–5.0 | 49,947 | 25.3 | 119.3 | 118.2–120.3 | 138,349 | 70.2 | 386.7 | 384.7–388.8 |
Source: Cancer registries in the Centers for Disease Control and Prevention’s National Program of Cancer Registries and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. IHS indicates Indian Health Service; CI, confidence interval; AI/AN, American Indians/Alaska Natives; NHW, non-Hispanic whites.
Percentages may not add to 100% because of rounding.
Rates are per 100,000 persons and are age-adjusted to the 2000 U.S. standard population (19 age groups; Census P25–1130; see Day 199632).
The AI/AN rate is statistically significantly higher than the NHW rate (P<.05).
The AI/AN rate is statistically significantly lower than the NHW rate (P<.05).
Table 4 displays an analysis of the lung cancer incidence by disease stage at diagnosis among AI/ANs and NHWs for CHSDA counties in the 6 IHS regions. For both populations across all regions, approximately 44% of cases were diagnosed at a distant stage. In the Southwest, AI/ANs had the highest percentage of distant-stage disease (53.3%) and the lowest percentage of local-stage disease (11.3%). Although AI/ANs in the Southern Plains had among the higher lung cancer incidence rates, AI/ANs in the same region had the lowest percentage of cases diagnosed with distant-stage disease (40.5%). For all regions combined, AI/AN females were more likely than AI/AN males to have their lung cancer diagnosed at a local stage and to have less distant-stage disease (data not shown). Among NHWs, the highest proportion of distant-stage disease was observed in the Pacific Coast and Alaska regions; the percentage stage distributions did not differ appreciably by sex (data not shown).
TABLE 4.
Invasive Lung and Bronchus Cancer Incidence, Percentage Distribution by Summary Stage and Indian Health Service Region for American Indians and Alaska Natives and Non-Hispanic Whites in Contract Health Service Delivery Area Counties: United States, 1999–2003a
| Localized | Regional | Distant | Unstaged | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IHS Region | Count | Rateb | 95% CI | %of Casesc | Count | Rateb | 95% CI | %of Casesc | Count | Rateb | 95% CI | %of Casesc | Count | Rateb | 95% CI | %of Casesc |
| AI/AN | ||||||||||||||||
| Northern Plains | 64 | 17.4 | 13.2–22.4 | 16.8 | 109 | 26.3 | 21.4–32.0 | 25.4 | 170 | 44.4 | 37.6–51.9 | 42.9 | 45 | 15.3 | 11.0–20.5 | 14.8 |
| Alaska | 24 | 13.3 | 8.3–19.9 | 14.4 | 43 | 24.0 | 17.2–32.5 | 25.9 | 79 | 41.8 | 32.7–52.4 | 45.1 | 19 | 13.6 | 8.0–21.0 | 14.7 |
| Southern Plains | 98 | 14.9 | 12.1–18.2 | 17.0 | 135 | 20.0 | 16.7–23.7 | 22.9 | 239 | 35.4 | 30.9–40.2 | 40.5 | 106 | 17.1 | 14.0–20.8 | 19.6 |
| Pacific Coast | 50 | 8.1 | 5.9–10.8 | 14.4 | 72 | 12.1 | 9.3–15.4 | 21.5 | 169 | 28.1 | 23.7–32.9 | 49.9 | 41 | 8.1 | 5.7–11.0 | 14.4 |
| East | 16 | 10.0 | 5.6–16.2 | 19.4 | 19 | 11.4 | 6.7–18.0 | 22.1 | 33 | 21.4 | 14.5–30.2 | 41.5 | 11 | 8.7 | 4.3–15.3 | 16.9 |
| Southwest | 15 | 1.7 | 0.9–2.9 | 11.3 | 21 | 2.4 | 1.4–3.6 | 16.0 | 65 | 8.0 | 6.1–10.2 | 53.3 | 25 | 3.0 | 1.9–4.4 | 20.0 |
| Total | 267 | 9.4 | 8.3–10.6 | 16.0 | 399 | 13.5 | 12.2–15.0 | 22.9 | 755 | 26.2 | 24.2–28.2 | 44.5 | 247 | 9.8 | 8.6–11.2 | 16.6 |
| NHW | ||||||||||||||||
| Northern Plains | 3156 | 12.1 | 11.7–12.6 | 18.4 | 4345 | 16.7 | 16.2–17.2 | 25.4 | 6864 | 26.4 | 25.8–27.0 | 40.2 | 2786 | 10.4 | 10.0–10.8 | 15.8 |
| Alaska | 95 | 11.2 | 8.9–13.8 | 15.6 | 141 | 15.7 | 13.0–18.7 | 21.8 | 318 | 34.1 | 30.1–38.4 | 47.4 | 83 | 11.1 | 8.7–13.8 | 15.4 |
| Southern Plains | 1535 | 15.1 | 14.3–15.8 | 18.1 | 1995 | 19.7 | 18.8–20.5 | 23.6 | 3513 | 34.7 | 33.6–35.9 | 41.6 | 1438 | 14.1 | 13.4–14.8 | 16.9 |
| Pacific Coast | 5386 | 11.4 | 11.1–11.7 | 16.4 | 7679 | 16.3 | 15.9–16.6 | 23.4 | 16,529 | 34.9 | 34.3–35.4 | 50.1 | 3414 | 7.0 | 6.8–7.3 | 10.1 |
| East | 4315 | 12.7 | 12.4–13.1 | 17.2 | 5655 | 16.9 | 16.4–17.3 | 22.8 | 10,823 | 32.1 | 31.5–32.7 | 43.4 | 4331 | 12.3 | 11.9–12.7 | 16.6 |
| Southwest | 2219 | 9.9 | 9.5–10.3 | 14.9 | 2747 | 12.3 | 11.8–12.7 | 18.6 | 5,900 | 26.5 | 25.8–27.2 | 40.0 | 3956 | 17.7 | 17.1–18.2 | 26.7 |
| Total | 16,706 | 11.9 | 11.7–12.1 | 16.9 | 22,562 | 16.1 | 15.9–16.3 | 22.9 | 43,947 | 31.2 | 31.0–31.5 | 44.3 | 16,008 | 11.1 | 11.0–11.3 | 15.8 |
Source: Cancer registries in the Centers for Disease Control and Prevention’s National Program of Cancer Registries and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program.
IHS indicates Indian Health Service; CI, confidence interval; AI/AN, American Indians/Alaska Natives; NHW, non-Hispanic whites.
SEER Summary Stage 2000 was used.
Rates are per 100,000 persons and are age-adjusted to the 2000 U.S. standard population (19 age groups; Census P25–1130; see Day 199632).
Percentages are age-adjusted to the 2000 U.S. standard population; percentages may not add to 100% because of rounding.
A comparison of the percentage distribution of histologic type among microscopically confirmed lung and bronchus cancer in cases between AI/ANs and NHWs in CHSDA counties is presented in Table 5. For all regions combined, AI/ANs had relatively less adenocarcinoma (29.2%) and slightly more squamous cell histology (24.0%) than NHWs (37.1% and 20.4%, respectively), except in the Southern Plains and Southwest, where the histology distributions for the 2 populations were similar.
TABLE 5.
Percentage Distribution of Histologic Type of Invasive Lung and Bronchus Cancer Among Microscopically Confirmed Cases for American Indians/Alaska Natives and Non-Hispanic Whites by Indian Health Service Region in Contract Health Service Delivery Counties: United States, 1999–2004
| Adenocarcinomaa | Squamous Cell Carcinomab | Small Cell Carcinomac | Large Cell Carcinomad | Other Malignant Histologiese | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AI/AN | NHW | AI/AN | NHW | AI/AN | NHW | AI/AN | NHW | AI/AN | NHW | |||||||||||
| IHS Region | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf | Count | %of Casesf |
| Northern Plains | 182 | 27.0 | 10,529 | 36.0 | 162 | 26.4 | 6537 | 22.3 | 120 | 18.8 | 4616 | 15.9 | 36 | 6.2 | 1634 | 5.6 | 134 | 21.6 | 5943 | 20.2 |
| Alaska | 77 | 25.1 | 453 | 39.8 | 76 | 29.0 | 232 | 22.4 | 48 | 16.4 | 172 | 15.0 | 11 | 3.8 | 50 | 4.2 | 72 | 25.7 | 207 | 18.5 |
| Southern Plains | 306 | 31.4 | 4339 | 31.3 | 199 | 21.4 | 3119 | 22.3 | 140 | 14.1 | 2154 | 15.6 | 85 | 9.1 | 1272 | 9.2 | 224 | 24.1 | 3021 | 21.7 |
| Pacific Coast | 148 | 28.2 | 21,933 | 38.4 | 112 | 22.8 | 11,253 | 19.7 | 93 | 17.7 | 7867 | 13.8 | 28 | 5.4 | 2735 | 4.8 | 136 | 25.9 | 13,398 | 23.3 |
| East | 36 | 28.1 | 17,240 | 39.3 | 35 | 27.8 | 8886 | 20.0 | 19 | 15.7 | 5938 | 13.6 | 9 | 8.5 | 2266 | 5.2 | 25 | 20.1 | 9722 | 22.0 |
| Southwest | 68 | 34.2 | 8778 | 35.0 | 41 | 22.5 | 4947 | 19.6 | 32 | 14.2 | 3512 | 14.0 | 9 | 5.0 | 1372 | 5.5 | 47 | 24.2 | 6527 | 26.0 |
| Total | 817 | 29.2 | 63,272 | 37.1 | 625 | 24.0 | 34,974 | 20.4 | 452 | 16.1 | 24,259 | 14.2 | 178 | 6.9 | 9329 | 5.6 | 638 | 23.8 | 38,818 | 22.7 |
Source: Cancer registries in the Centers for Disease Control and Prevention’s National Program of Cancer Registries and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program (for the states included, see Table 1).
AI/AN indicates American Indians/Alaska Natives; NHW, non-Hispanic whites; IHS, Indian Health Service.
Includes histology codes 8140–8389, 8401, 8408, 8410–8411, 8413, 8441, 8450, 8460, 8470, 8480–8482, 8490, 8500, 8503–8504, 8510, 8520, 8525, 8530, 8560, 8571–8574, 8576, 9070, and 9110.
Includes histology codes 8050–8071, 8074–8089, and 8094.
Includes histology codes 8041, 8044, and 8073.
Includes histology codes 8012–8014, 8045, and 8072.
Includes histology codes 8000–8011, 8015–8040, 8042–8043, 8046–8049, 8090–8093, 8095–8139, 8390–8400, 8402–8407, 8409, 8412, 8414–8440, 8442–8449, 8451–8459, 8461–8469, 8471–8479, 8483–8489, 8491–8499, 8501–8502, 8505–8509, 8511–8519, 8521–8524, 8526–8529, 8531–8559, 8561–8570, 8575, 8577–9069, 9071–9109, and 9111–9989.
Percentages are age-adjusted to the 2000 U.S. standard population; percentages may not add to 100.0% because of rounding.
DISCUSSION
This is the most comprehensive study of the incidence of lung cancer among the AI/AN populations in the United States to date. Combining NPCR and SEER data for broad population coverage and using linkages to improve on the misclassification of race among AI/ANs provided the opportunity to describe both regional and national estimates of lung cancer incidence for AI/ANs. Our findings confirmed the dramatic regional differences in lung cancer rates that have been reported in studies using death certificates.16 Lung cancer incidence rates in AI/ANs varied 7-fold across IHS regions (in CHSDA counties), with the highest rates observed in the Northern and Southern Plains and Alaska and the lowest rates observed in the Southwest. AI/AN males and females were diagnosed with lung cancer at a younger age than NHWs, but the distribution of disease stage did not differ between the 2 populations. Adenocarcinoma was less common and squamous cell histology was slightly more common among AI/ANs than among NHWs.
Cigarette smoking and exposure to environmental tobacco have been linked directly to lung cancer and many other diseases, including heart disease, stroke, and multiple cancers,2,3,33 that translate into multibillion dollar medical and lost productivity costs in the United States.34 AI/ANs have the highest prevalence of daily cigarette use of any population in the United States.35 The prevalence of tobacco use varies greatly among AI/ANs by region.36 Thus, regional lung cancer rates also can be expected to vary; and, similar to the current study, such variations were observed in earlier incidence and mortality studies.13–16,37
Tobacco use survey information must be interpreted with caution, because many American Indians use tobacco for traditional or ceremonial purposes and may or may not also be habitual smokers.38,39 Tobacco has been a key element in the ceremonial practices of many American Indian people from pre-Columbian times. Many Native stories emphasize the sacredness of the plant and its powers to heal if used properly and to harm if used improperly. Traditional tobacco mixes may include the Nicotiana plant, kinnick-kinnick, and other herbs. However, commercial tobacco products, by virtue of convenience, are used sometimes for ceremonial functions. Inhalation of tobacco smoke during ceremonial use typically is brief and does not occur every day; therefore, it is unlikely to lead to lung cancer.
Data from 15 years of Behavioral Risk Factor Surveillance System (BRFSS) surveys indicate that AI/AN current smoking rates have not been declining.36,38–40 According to aggregate data from the 2000 through 2006 BRFSS, AI/AN respondents were more likely to be currently smoking cigarettes (31.1%) than the NHW population (22.8%).36 Current cigarette smoking was highest in the Northern Plains (40.2%) and Alaska (40%) and was lowest in the Southwest (21.1%).36 For all racial and ethnic groups, data on current cigarette smoking from the 2006 National Health Interview Survey show the highest rate among AI/ANs (26.9%), followed by NHWs (22.6%), Native Hawaiian/Pacific Islanders (22.5%), African Americans (21.8%), Hispanics (14.5%), and Asians (10.7%).35
Although it is estimated that tobacco is a causal factor in nearly 90% of lung cancers, other occupational and environmental exposures also are known lung carcinogens. These include asbestos, radon, arsenic, and uranium mining.1 According to a 1999 Institute of Medicine report, an estimated 21,800 new diagnoses of lung cancer are related to radon (14%) each year in the United States, which makes radon the second leading cause of lung cancer deaths after cigarette smoking.41 Other studies have suggested a synergistic relation between radon exposure and cigarette smoking that may increase the risk of lung cancer to 6 to 10 times higher than among nonsmokers.11,12,42 Radon gas occurs naturally in small amounts in soils and rocks throughout the United States. Radon can become trapped in homes and other structures, creating the potential for elevated exposure.43 The Environmental Protection Agency (EPA) has established 4 pico Curies per liter (pCi/L) as the threshold above which action should be taken to alter a structure to reduce radon exposure.44 EPA maps of radon zones indicate that homes in the part of the country with a high proportion of AI/ANs contain high (4 pCi/L) or moderate (2 pCi/L) levels of radon, which may contribute to some cases of lung cancer among AI/ANs.45 Another form of exposure to radon is in the process of uranium mining. This occupational exposure has long been documented as a strong causal factor in the development of lung cancer. In the Southwest, many AI/AN males worked in uranium mines in the 1950s and 1960s; it has been demonstrated that this is an important cause of lung cancer in a population that historically has had a very low prevalence of smoking.5,6 The Southwest region has had the lowest lung cancer incidence rates, despite the extensive exposure to uranium mining that occurred in that region.
Other known risk factors for lung cancer may include tuberculosis and chronic obstructive pulmonary disease.46 Exposure to arsenic, chromium, nickel, aromatic hydrocarbons, and ethers, most commonly in an occupational setting, also may increase the risk of lung cancer.47
The IHS patient registration database contains records of individuals who are members of federally recognized tribes, and linking these data with SEER and NPCR registries corrected some of the misclassification of race for AI/ANs.26 Restricting the sample to the CHSDA counties also contributed to improved rate estimates, because AI/ANs in those counties are more likely to be registered for care with the IHS, and less misclassification has been noted in these counties.20 Because misclassification of AI/AN race is so common in both state and national databases,18,48–51 these processes contributed to improved descriptions of the lung cancer burden for AI/ANs.
Despite these improvements, there are some limitations to the data. Because most analyses were restricted to CHSDA counties, in which only 56% of AI/ANs live and which tend to be located in more rural areas and Western states (Fig. 1), the results may not be generalizable to all AI/ANs (or NHWs) in the United States. In addition, the percentage of AI/ANs residing in CHSDA counties varied greatly among the 6 IHS regions (Table 1). The percentage was particularly low in the East region (13.1%), which may help to explain the puzzling occurrence in this region of relatively low lung cancer incidence rates and high prevalence estimates of cigarette smoking.36 Another limitation is that IHS records capture only enrolled members of recognized tribes who seek healthcare from the IHS and, thus, do not include others who may self-identify in the United States Census as AI/AN, notably urban AI/ANs and those who are from tribes not recognized by the federal government. Misclassification is likely to be greatest in the Pacific Coast and East regions, where the IHS has a relatively small presence and only serves a small percentage of AI/ANs.
To our knowledge, this is the most complete accounting of lung cancer occurrence among AI/AN to date and demonstrates the substantial differences in the incidence of this deadly cancer among the various AI/AN populations. Until the 1990s, most AI/ANs were not included in areas that were covered by high-quality, population-based cancer registries. Currently, the NPCR and SEER annually produce the United States Cancer Statistics, covering 98% of United States population.21 In fact, national rates of lung cancer incidence for all races combined reportedly were higher than had been noted before United States Cancer Statistics availability.52 Although the methods used for this analysis improved the completeness of reporting cancers among AI/AN by correcting for some of the misclassification of race, the linkage protocols need to be continued. Furthermore, additional linkages with tribal rosters that were not included in the current efforts are needed to further improve the misclassification of race in AI/AN populations.
In conclusion, lung cancer is a significant problem for a large portion of AI/AN populations, notably those who live in the Northern Plains states and Alaska, where dramatic disparities in lung cancer incidence rates exist between AI/AN and NHW populations. AI/ANs in these regions have high estimates of smoking prevalence compared with NHWs36 as well as high lung cancer incidence rates. The 7-fold difference between the lowest and highest lung cancer rates (Southwest vs Northern Plains) likely reflects in large part the strong association between cigarette smoking and the development of lung cancer. Indeed, BRFSS and local survey data indicate that AI/ANs in Alaska and the Plains use tobacco at rates higher than any other racial or ethnic population in the United States.39 Our study underscores the need for aggressive tobacco control programs within AI/AN populations and communities.
Acknowledgments
This supplement was sponsored by Cooperative Agreement Number U50 DP424071–04 from the Centers for Disease Control and Prevention, Division of Cancer Prevention and Control.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This article is a US Government work and, as such, is in the public domain in the United States of America.
REFERENCES
- 1.American Cancer Society. Cancer Facts and Figures, 2007. Atlanta, Ga: American Cancer Society; 2007. [Google Scholar]
- 2.US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 3.US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 4.Hecht SS. Tobacco smoke carcinogens and lung cancer. J Natl Cancer Inst. 1999;91:1194–1210. [DOI] [PubMed] [Google Scholar]
- 5.Gilliland FD, Hunt WC, Pardilla M, Key CR. Uranium mining and lung cancer among Navajo men in New Mexico and Arizona, 1969 to 1993. J Occup Environ Med. 2000;42:278–283. [DOI] [PubMed] [Google Scholar]
- 6.Samet JM, Kutvirt DM, Waxweiler RJ, Key CR. Uranium mining and lung cancer in Navajo men. N Engl J Med. 1984;310:1481–1484. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services. Report on Carcinogens, 11th ed Atlanta, Ga: US Department of Health and Human Services, Public Health Service, National Toxicology Program; 2005. [Google Scholar]
- 8.Agency for Toxic Substances and Disease Registry (ATSDR). Toxicology Profile for Radon. Atlanta, Ga: US Department of Health and Human Services, Public Health Service; 1990. [Google Scholar]
- 9.Environmental Protection Agency (EPA). A Citizen’s Guide to Radon: The Guide to Protecting Yourself and Your Family from Radon, 3rd ed Washington, DC: US Environmental Protection Agency; 2005. [Google Scholar]
- 10.National Research Council (NCR) Committee on Health Risks of Exposure to Radon. BEIR VI. Health Effects of Exposure to Radon. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 11.Frumkin H, Samet JM. Radon. CA Cancer J Clin. 2001; 51:337–344, 322; quiz 345–348. [DOI] [PubMed] [Google Scholar]
- 12.Mendez D, Warner KE, Courant PN. Effects of radon mitigation vs smoking cessation in reducing radon-related risk of lung cancer. Am J Public Health. 1998;88:811–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bleed DM, Risser DR, Sperry S, Hellhake D, Helgerson SD. Cancer incidence and survival among American Indians registered for Indian Health Service care in Montana, 1982–1987. J Natl Cancer Inst. 1992;84:1500–1505. [DOI] [PubMed] [Google Scholar]
- 14.Nutting PA, Freeman WL, Risser DR, et al. Cancer incidence among American Indians and Alaska Natives, 1980 through 1987. Am J Public Health. 1993;83:1589–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paltoo DN, Chu KC. Patterns in cancer incidence among American Indians/Alaska Natives, United States, 1992–1999. Public Health Rep. 2004;119:443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Espey DK, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990–2001. Cancer. 2005;103:1045–1053. [DOI] [PubMed] [Google Scholar]
- 17.Kelly JJ, Lanier AP, Alberts S, Wiggins CL. Differences in cancer incidence among Indians in Alaska and New Mexico and US whites, 1993–2002. Cancer Epidemiol Biomarkers Prev. 2006;15:1515–1519. [DOI] [PubMed] [Google Scholar]
- 18.Sugarman JR, Holliday M, Ross A, Castorina J, Hui Y. Improving American Indian cancer data in the Washington State Cancer Registry using linkages with the Indian Health Service and tribal records. Cancer. 1996;78(7 suppl):1564–1568. [PubMed] [Google Scholar]
- 19.Partin MR, Rith-Najarian SJ, Slater JS, Korn JE, Cobb N, Soler JT. Improving cancer incidence estimates for American Indians in Minnesota. Am J Public Health. 1999;89: 1673–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jim MA, Espey DK, Wiggins C, Cobb N, Wingo PA. Racial Misclassification of American Indians Residing Near IHS Facilities: Poster P-47, Final Program and Abstracts. Presented at the 2006 North American Association of Central Cancer Registries Annual Conference, Regina, Saskatchewan, Canada, June 10–16, 2006. [Google Scholar]
- 21.US Cancer Statistics Working Group. United States Cancer Statistics: 2004 Incidence. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2007. [Google Scholar]
- 22.Fritz A, Percy C, Jack A. International Classification of Diseases for Oncology. Geneva, Switzerland: World Health Organization; 2000. [Google Scholar]
- 23.Howe HL, Jamison PM, Havener L, Chen VW, Ries LAG. Site-Specific Comparison of Summary Stage 1977 and Summary Stage 2000 Coding. Springfield, Ill: North American Association of Central Cancer Registries; 2005. [Google Scholar]
- 24.Phillips J, ed. Summary Stage: Data Effects of the Changes in 2000. Springfield, Ill: North American Association of Central Cancer Registries; 2003. Available at: http://www.naaccr.org/filesystem/pdf/Summary%20Stage%20Report%201-21-04b.pdf. Accessed on January 13, 2008. [Google Scholar]
- 25.Ries L, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2004 (based on the November 2006 SEER data submission, posted to the SEER website, 2007). National Cancer Institute. Bethesda, Md: National Cancer Institute; 2007. Available at: http://seer.cancer.gov/csr/1975_2004/. Accessed on January 13, 2008. [Google Scholar]
- 26.Espey DK, Wiggins CL, Jim MA, Miller BA, Johnson CJ, Becker TM. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008;113(5 suppl):1120–1130. [DOI] [PubMed] [Google Scholar]
- 27.North American Association of Central Cancer Registries (NAACCR) Latino Research Work Group. NAACCR Guideline for Enhancing Hispanic/Latino Identification: Revised NAACCR Hispanic/Latino Identification Algorithm [NHIA v2]. Springfield, Ill: North American Association of Central Cancer Registries; 2005. [Google Scholar]
- 28.Ingram DD, Parker JD, Schenker N, et al. United States Census 2000 Population With Bridged Race Categories. DHHS Publication PHS 2003–1334 Vital and Health Statistics, Series 2, No. 135. Data Evaluation and Methods Research. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2003. [PubMed] [Google Scholar]
- 29.National Cancer Institute, Surveillance Epidemiology and End Results (SEER) Program. Population estimates used in NCI’s SEER*Stat software. Available at: http://seer.cancer.gov/popdata/methods.html. Accessed on January 13, 2008.
- 30.Surveillance Research Program. SEER*Stat software. National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch; 2007. Available at: http://www.seer.cancer.gov/seerstat. Accessed on January 13, 2008.
- 31.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006; 15:547–569. [DOI] [PubMed] [Google Scholar]
- 32.Day JC. Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995 to 2050, US Bureau of the Census, Current Population Reports, P25–1130. Washington, DC: US Government Printing Office; 1996. [Google Scholar]
- 33.Zhang X, Shu XO, Yang G, Li, et al. Association of passive smoking by husbands with prevalence of stroke among Chinese females nonsmokers. Am J Epidemiol. 2005;161:213–218. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (CDC). Annual smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 1997–2001. MMRW Morbid Mortal Wkly Rep. 2005;54:625–628. [PubMed] [Google Scholar]
- 35.Pleis JR, Lethbridge-Cejku M. Summary health statistics for US adults: National Health Interview Survey, 2006. Vital Health Stat 10. 2007;(235):1–153. [PubMed] [Google Scholar]
- 36.Steele CB, Cardinez CJ, Richardson LC, Tom-Orme L, Shaw KM. Surveillance for health behaviors of American Indians and Alaska Natives—findings from the Behavioral Risk Factor Surveillance System, 2000–2006. Cancer. 2008;113(5 suppl):1131–1141. [DOI] [PubMed] [Google Scholar]
- 37.Espey DK, Wu XC, Swan J, et al. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007:110: 2119–2152. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC). Tobacco use among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2006;55:1145–1148. [PubMed] [Google Scholar]
- 39.National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]
- 40.Denny CH, Holtzman D, Cobb N. Surveillance for health behaviors of American Indians and Alaska Natives. Findings from the Behavioral Risk Factor Surveillance System, 1997–2000. MMWR Surveill Summ. 2003;52:1–13. [PubMed] [Google Scholar]
- 41.National Research Council, Committee on Health Risks of Exposure to Radon. BEIR VI. Health Effects of Exposure to Radon. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 42.Environmental Protection Agency (EPA). EPA Assessment of Risks from Radon in Homes. Washington, DC: US Environmental Protection Agency; 2003. [Google Scholar]
- 43.Agency for Toxic Substances and Disease Registry (ATSDR). Toxicology Profile for Radon. Atlanta, Ga: US Department of Health and Human Services, Public Health Service; 1990. [Google Scholar]
- 44.Environmental Protection Agency (EPA). A Citizen’s Guide to Radon: The Guide to Protecting Yourself and Your Family from Radon, 3rd ed Washington, DC: US Environmental Protection Agency; 2005. [Google Scholar]
- 45.Environmental Protection Agency (EPA). EPA Map of Radon Zones. Available at: http://epa.gov/radon/zonemap.html. Accessed April 21, 2008.
- 46.Turner MC, Chen Y, Krewski D, Calle EE, Thun MJ. Chronic obstructive pulmonary disease is associated with lung cancer mortality in a prospective study of never smokers. Am J Respir Crit Care Med. 2007;178:285–290. [DOI] [PubMed] [Google Scholar]
- 47.National Cancer Institute (NCI). Cancer Topics. Available at: www.cancer.gov/cancertopics. Accessed October 12, 2007.
- 48.Frost F, Taylor V, Fries E. Racial misclassification of Native Americans in a Surveillance, Epidemiology, and End Results cancer registry. J Natl Cancer Inst. 1992;84:957–962. [DOI] [PubMed] [Google Scholar]
- 49.Kwong S, Perkings C, Snipes K, Wright W. Improving American Indian cancer data in the California Cancer Registry by linkage with the Indian Health Service. J Registry Manage. 1998;25:17–20. [Google Scholar]
- 50.Becker TM, Bettles J, Lapidus J, et al. Improving cancer incidence estimates for American Indians and Alaska Natives in the Pacific Northwest. Am J Public Health. 2002; 92: 1469–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Harwell TS, Miller SH, Lemons DL, Helgerson SD, Gohdes D. Cancer incidence in Montana: rates for American Indians exceed those for whites. Am J Prev Med. 2006; 30:493–497. [DOI] [PubMed] [Google Scholar]
- 52.Wingo PA, Jamison PM, Hiatt RA, et al. Building the infrastructure for nationwide cancer surveillance and control—a comparison between the National Program of Cancer Registries (NPCR) and the Surveillance, Epidemiology, and End Results (SEER) Program (United States). Cancer Causes Control. 2003;14:175–193. [DOI] [PubMed] [Google Scholar]