Summary
Background
Globally, per-capita, South Africa reports a disproportionately high number of cases of multidrug-resistant (MDR) tuberculosis and extensively drug-resistant (XDR) tuberculosis. We sought to estimate the prevalence of resistance to tuberculosis drugs in newly diagnosed and retreated patients with tuberculosis provincially and nationally, and compared these with the 2001–02 estimates.
Methods
A cross-sectional survey was done between June 15, 2012–June 14, 2014, using population proportionate randomised cluster sampling in the nine provinces in South Africa. 343 clusters were included, ranging between 31 and 48 per province. A patient was eligible for inclusion in the survey if he or she presented as a presumptive case during the intake period at a drug resistance survey enrolling facility. Consenting participants (≥18 years old) completed a questionnaire and had a sputum sample tested for resistance to first-line and second-line drugs. Analysis was by logistic regression with robust SEs, inverse probability weighted against routine data, and estimates were derived using a random effects model.
Findings
101 422 participants were tested in 2012–14. Nationally, the prevalence of MDR tuberculosis was 2·1% (95% CI 1·5–2·7) among new tuberculosis cases and 4·6% (3·2–6·0) among retreatment cases. The provincial point prevalence of MDR tuberculosis ranged between 1·6% (95% CI 0·9–2·9) and 5·1% (3·7–7·0). Overall, the prevalence of rifampicin-resistant tuberculosis (4·6%, 95% CI 3·5–5·7) was higher than the prevalence of MDR tuberculosis (2·8%, 2·0–3·6; p=0·01). Comparing the current survey with the previous (2001·02) survey, the overall MDR tuberculosis prevalence was 2·8% versus 2·9% and prevalance of rifampicin-resistant tuberculosis was 3·4% versus 1·8%, respectively. The prevalence of isoniazid mono-resistant tuberculosis was above 5% in all provinces. The prevalence of ethionamide and pyrazinamide resistance among MDR tuberculosis cases was 44·7% (95% CI 25·9–63·6) and 59·1% (49·0–69·1), respectively. The prevalence of XDR tuberculosis was 4·9% (95% CI 1·0–8·8). Nationally, the estimated numbers of cases of rifampicin-resistant tuberculosis, MDR tuberculosis, and isoniazid mono-resistant tuberculosis for 2014 were 13 551, 8249, and 17 970, respectively.
Interpretation
The overall prevalence of MDR tuberculosis in South Africa in 2012–14 was similar to that in 2001–02; however, prevalence of rifampicin-resistant tuberculosis almost doubled among new cases. Furthermore, the high prevalence of isoniazid mono-resistant tuberculosis, not routinely screened for, and resistance to second-line drugs has implications for empirical management.
Funding
President’s Emergency Plan for AIDS Relief through the Centers for Disease Control and Prevention under the terms of 1U19GH000571.
Introduction
Multidrug-resistant (MDR) tuberculosis was declared a public health crisis by WHO in 2013 and recognised as a global health security risk by the World Health Assembly in 2014. South Africa remains one of the highest burdened countries in all three WHO-defined tuberculosis categories, including tuberculosis, MDR tuberculosis, and tuberculosis and HIV coinfection cases. Rifampicin-resistant tuberculosis, often seen as a proxy for MDR tuberculosis and treated as such has become increasingly relevant and characterises cases of both MDR tuberculosis and rifampicin-monoresistant (RMR) tuberculosis. The difference fundamentally being the presence or absence of resistance to the second core tuberculosis drug, isoniazid. In 2014, South Africa reported the second highest absolute number of notified rifampicin-resistant cases globally (n=18734),1 following India, where 25749 cases were recorded in a population 20 times greater than South Africa.
The previous tuberculosis drug resistance survey done in South Africa during 2001–02 reported the prevalence of MDR tuberculosis as 1·6% (95% CI 1·1–2·1) in new tuberculosis cases and 6·6% (4·9–8·2) in retreatment cases.2 At that time, the prevalence of tuberculosis and HIV was rising, late presentation was common, and tuberculosis-related mortality was high, whereas laboratory testing for drug-resistant tuberculosis was limited. In 2005, at the Tugela Ferry Hospital, KwaZulu-Natal province, an outbreak of extensively resistant (XDR) tuberculosis with high mortality was identified and was followed by the emergence of totally drug-resistant tuberculosis strains identified during 2008–09 in the Eastern Cape province.3
Treatment success based on notification data has remained low at approximately 50% for MDR tuberculosis and 20% for XDR tuberculosis cases.4 However, the situation has potential for improvement with the introduction of bedaquiline, a new antimycobacterial agent, with improved outcomes compared with a background regimen.5 Furthermore, implementation of new diagnostics for early detection of drug-resistant tuberculosis, in particular the Xpert MTB/RIF assay as the primary test, and an upscaling of the antiretroviral treatment programme were important advances in South Africa since the previous drug resistance survey in 2001–02. This cross-sectional survey was initiated in mid-2012 in South Africa to evaluate the prevalence of resistance to first-line and second-line agents in new and retreatment tuberculosis cases nationally and provincially, and provide estimates as to the burden of drug-resistant tuberculosis.
Methods
Study design and participants
The survey was a population-based cross-sectional study, following WHO guidelines6 as applied to the 2001–02 survey. A population proportionate, cluster-sampling design was used to determine sample size and select study sites to provide MDR tuberculosis prevalence estimates for each province and nationally. Clusters were randomly selected using a population-proportionate cluster-sampling approach based on a list of new sputum smear-positive cases per health facilities, per province, in the year when the survey was designed, and were individual health-care facilities or a combination of facilities. A patient was eligible for inclusion in the survey if he or she presented as a presumptive case during the intake period at a drug resistance survey enrolling facility. A presumptive case was defined as a patient who had a persistent cough for more than 2 weeks or at least two of the following symptoms: fever, drenching night sweats, loss of appetite, unexplained weight loss (>1·5 kg/month), a general feeling of illness (malaise) and tiredness, and shortness of breath with chest pain. Only adults aged 18 years or older who could produce sufficient volumes of good quality sputum were included. Patients were excluded if they declined to give informed consent to participate in the survey.
The survey received ethical approval from the University of Witwatersrand Research Ethics Committee on Nov 26, 2010 (ethics clearance number M081022). Clearance was also obtained from Centers for Disease Control and Prevention, Atlanta, GA, USA. The survey was initiated after approval from the respective provinces and the South Africa National Tuberculosis Control Programme was received.
Procedures
A survey-specific sputum sample, together with a questionnaire completed through direct patient interview by a health-care worker were collected from all patients with presumptive tuberculosis who provided informed consent at selected facilities during the June 15, 2012–June 14, 2014, survey period. Auramine smear microscopy, mycobacterial culture (MGIT 960; Becton Dickinson, Sparks, MD, USA), and HIV testing (Oraquick Advance Rapid HIV—1 & 2 Antibody Test; Orasure Technologies,Bethlehem, PA, USA) on sputum were done, followed by drug susceptibility testing against first-line and second-line antituberculosis drugs on Mycobacterium tuberculosis culture-confirmed isolates.7 Data from case report forms and laboratory testing were collated and analysed.
A new case was defined as a patient with a newly registered episode of tuberculosis who, in response to direct questioning, reports never having been treated for tuberculosis or reports having taken antituberculosis drugs for less than 1 month; or where adequate documentation is available, for whom there is no evidence of having taken antituberculosis drugs for 1 month or more. A previously treated case was defined as a patient having a newly registered episode of tuberculosis who, in response to direct questioning, reports having received 1 month or more of antituberculosis drugs in the past; or where adequate documentation is available, there is evidence of having received 1 month or more of anti-tuberculosis drugs in the past. Drug resistance prevalence was determined among culture-confirmed tuberculosis cases in the survey.
Statistical analysis
Descriptive and statistical analyses accounting for the complex multistage sampling design and clustering of patients within primary sampling units, were done and compared with the 2001–02 survey. Multiple imputation was done for missing age, sex, and previous treatment history data, as well as final status for contaminated cultures and failed drug susceptibility testing. Logistic regression with robust SEs adjusting for clustering effects introduced by survey design and potential biases arising during implementation was used to determine provincial estimates of drug resistance prevalence among new and previously treated cases, and by HIV status. These estimates were pooled to generate national estimates using a random effects model. Additionally, national estimates for prevalence of second-line drug resistance including XDR tuberculosis were calculated among subgroups of RMR tuberculosis and MDR tuberculosis cases. To determine the absolute burden expected to be diagnosed for 2014 in South Africa, the 95% CIs of the prevalence estimate for rifampicin-resistant tuberculosis, isoniazid monoresistant (IMR) tuberculosis and MDR tuberculosis was applied to the reported number of microbiologically confirmed tuberculosis cases reported for the same year.8 Additional details are provided in the appendix (pp 2, 3) and estimates presented are the adjusted rates.
Role of the funding source
The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
The South African Tuberculosis Drug Resistance Survey 2012–14 tested 101 422 people from 464 randomly selected facilities (figure) for tuberculosis by culture from all nine provinces in South Africa (table 1). Of those screened and not tested, 12 043 (6%) were younger than 18 years, 13 141 (7%) did not give consent, 10 012 (5%) did not fulfil criteria for presumptive tuberculosis cases, 864 (<1%) were currently on treatment, 1434 (1%) were already included at another survey site, 61 351 (31%) supplied insufficient specimen volume, and 91 (<1%) had incomplete forms (appendix p 4). Of 10044 culture-confirmed tuberculosis cases detected, 5423 (55%) of 9793 were smear positive. Nationally, 2210 (22%) of the culture-positive cases reported having ever been previously treated for tuberculosis. The age and sex distributions are shown in the appendix (p 5). The prevalence of HIV coinfection among culture-confirmed tuberculosis cases was 63% nationally, ranging from 47% in Western Cape to 77% in Mpumalanga.
Figure: Map of randomly selected facilities included in the South African Tuberculosis Drug Resistance Survey 2012–14.
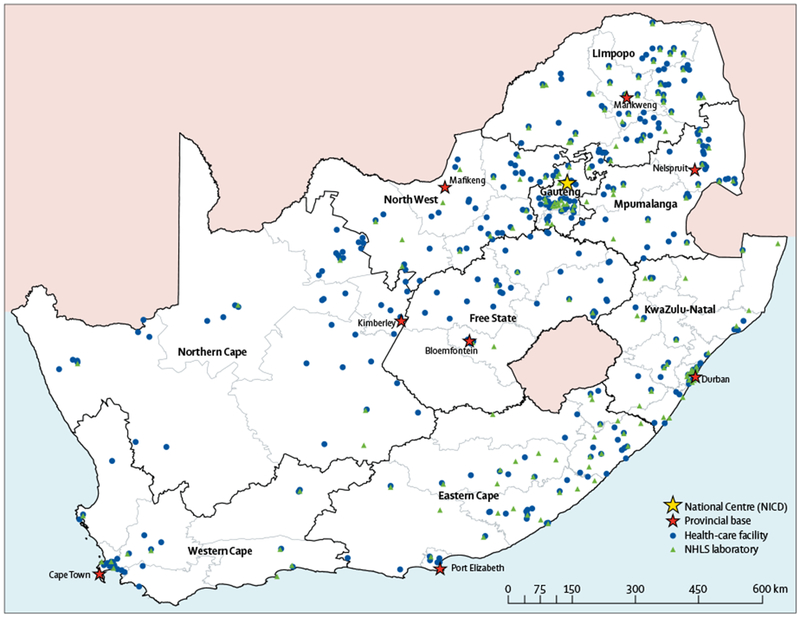
NCID=National Institute for Communicable Diseases. NHLS=National Institute for Communicable Diseases.
Table 1:
Participant enrolment cascade including previous tuberculosis (TB) treatment and HIV–TB coinfection among culture-confirmed TB cases, by province in South Africa, 2012–14
| Number of clusters | Number screened | Number tested by culture | Proportion tested of screened | Number culture positive | Proportion culture positive of tested | Number culture positive for MTB | Proportion MTB culture positive | Previous history of TB treatment (n, %)* | HIV-TB coinfection of available status (n, %) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Eastern Cape | 32 | 19 349 | 8548 | 44% | 1123 | 13% | 1033 | 92% | 279 (27%) | 543/977 (56%) |
| Free State | 39 | 26 288 | 14 079 | 54% | 1155 | 8% | 907 | 79% | 190 (21%) | 578/822(70%) |
| Gauteng | 38 | 20 101 | 11 188 | 56% | 1423 | 13% | 1123 | 79% | 202 (18%) | 823/1103(75%) |
| KwaZulu-Natal | 31 | 20 376 | 9082 | 45% | 899 | 10% | 784 | 87% | 172 (22%) | 507/733(70%) |
| Limpopo | 48 | 31 503 | 14 016 | 44% | 1442 | 10% | 1121 | 78% | 157 (14%) | 687/1081(64%) |
| Mpumalanga | 38 | 21 739 | 11 800 | 54% | 1418 | 12% | 1193 | 84% | 203 (17%) | 859/1119(77%) |
| North West | 35 | 19 589 | 10 344 | 53% | 1370 | 13% | 1024 | 75% | 205 (20%) | 691/1016(68%) |
| Northern Cape | 47 | 23 107 | 13 376 | 58% | 1688 | 13% | 1372 | 81% | 384 (28%) | 682/1319(52%) |
| Western Cape | 35 | 18 306 | 8989 | 49% | 1537 | 17% | 1487 | 97% | 520 (35%) | 617/1301(47%) |
| South Africa | 343 | 200 358 | 101 422 | 51% | 12 055 | 12% | 10 044 | 83% | 2210 (22%) | 5987/9471(63%) |
MTB=Mycobacterium tuberculosis complex.
Denominator is the number of cases culture positive for MTB in each row.
The national MDR tuberculosis prevalence estimate was 2·;1% (95% CI 1·5–2·7) in new tuberculosis cases, and higher among retreatment cases (4·6%, 3·2–6·0), with an overall estimate of 2·8% (2·0–3·6; table 2). Provincial MDR tuberculosis prevalence in six of nine provinces was below 2·0% among new cases (table 3). Mpumalanga province had the highest overall prevalence of MDR tuberculosis (5·1%, 95% CI 3·7–7·0), including both new (4·2%, 2·8–5·6) and retreatment cases (7·6%, 3·2–12·0), whereas Limpopo province had the lowest at 1·6% (0·9–2·9) overall, 1·4% (0·4–2·4) new, and 2·5% (0–5·1) retreatment cases.
Table 2:
National first-line drug resistance estimates among tuberculosis cases in South Africa, 2012–14 and 2001–02 surveys2
| New cases (%, 95% CI) |
Previously treated cases (%, 95% CI) |
Overall (%, 95% CI) |
||||
|---|---|---|---|---|---|---|
| 2001–02 | 2012–14 | 2001–02 | 2012–14 | 2001–02 | 2012–14 | |
| Multidrug resistant | 1·6% (1·1–2·1) | 2·1% (1·5–2·7) | 6·6% (4·9–8·2) | 4·6% (3·2–6·0) | 2·9% (2·4–3·5) | 2·8% (2·0–3·6) |
| Rifampicin | 1·8% (1·3–2·3) | 3·4% (2·5–4·3)* | 7·5% (5·7–9·2) | 7·1% (4·8–9·5) | 3·4% (2·8–3·9) | 4·6% (3·5–5·7) |
| Rifampicin mono-resistance (RRHS) | .. | 1·4% (0·9–1·8) | .. | 2·5% (1·2–3·7) | .. | 1·7% (1·1–2·2) |
| Rifampicin mono-resistance (RRHSZSES) | 0·2% (0·1–0·4) | 0·9% (0·5–1·3)* | 0·8% (0·4–1·2) | 1·8% (0·7–2·9) | 0·4% (0·2–0·5) | 1·1% (0·6–1·7)* |
| Rifampicin mono-resistance (RRHSZRES/RRHSZSER) | 0% | 0·4% (0·1–0·7)* | 0·1% (0–0·4) | 0·7% (0·2–1·2) | 0·0% (0·0–0·1) | 0·5% (0·2–0·8)* |
| Isoniazid | 5·7% (4·9–6·5) | 7·6% (6·4–8·7) | 11·8% (9·3–14·4) | 11·1% (9·1–13·1) | 7·4% (6·5–8·3 | 9·3% (7·9–10·7) |
| Isoniazid mono-resistance (RSHR) | .. | 5·5% (4·6–6·5) | .. | 6·5% (5·1–7·9) | .. | 6·1% (5·1–7·1) |
| Isoniazid mono-resistance (RSHRZSES) | 2·6% (2·0–3·2) | 4·5% (3·6–5·3)* | 2·9% (1·9–4·0) | 5·5% (4·3–6·8)* | 2·7% (2·2–3·2) | 4·9% (4·1–5·8)* |
| Isoniazid mono-resistance (RSHRZRES/RSHRZSER) | 1·5% (1·2–1·9) | 1·1% (0·3–1·8) | 2·3% (1·5–3·2) | 1·0% (0·4–1·6) | 1·7% (1·4–2·1) | 1·1% (0·4–1·7) |
| Ethambutol | 0·8% (0·4–1·1) | 2·0% (1·2–2·8)* | 2·4% (1·5–3·3) | 3·5% (2·2–4·8) | 1·2% (0·8–1·6) | 2·5% (1·7–3·3)* |
| Streptomycin | 4·3% (3·5–5·0) | 3·9% (2·8–5·1) | 8·1% (6·6–9·6) | 5·1% (3·8–6·5)* | 5·3% (4·7–5·9) | 4·5% (3·5–5·5) |
| Pyrazinamide | .. | 2·9% (2·2–3·6) | .. | 5·2% (3·8–6·7) | .. | 3·7% (2·9–4·5) |
| Ofloxacin | .. | 1·2% (0·7–1·7) | .. | 1·5% (0·7–2·2) | .. | 1·4% (0·9–1·8) |
R=rifampicin. H=isoniazid. Z=pyrazinamide. E=ethambutol. Subscript R=resistant. Subscript S=susceptible.
Non-overlapping 95% CIs between the two surveys.
Table 3:
Provincial prevalence of rifampicin resistance, multidrug resistance, and rifampicin mono-resistance among tuberculosis cases, South Africa, 2012–14
| New cases (%, 95% CI) |
Previously treated cases (%, 95% CI) |
Overall (%, 95% CI) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| RR | MDR | RMR | RR | MDR | RMR | RR | MDR | RMR | |
| Eastern Cape | 2·7% (1·5–3·9) | 1·7% (0·8–2·6) | 1·0% (0·3–1·7) | 4·0% (1·5–6·5) | 2·7% (0·5–5·0) | 1·2% (0–2·4) | 3·3% (2·2–4·9) | 2·1% (1·3–3·6) | 1·1% (0·6–2·0) |
| Free State | 3·5% (2·0–5·1) | 1·8% (0·8–2·8) | 1·8% (0·4–3·1) | 7·3% (2·5–12·1) | 3·9% (0·8–7·0) | 3·4% (0·5–6·3) | 4·6% (3·2–6·6) | 2·3% (1·5–3·6) | 2·2% (1·2–3·9) |
| Gauteng | 3·6% (2·1–5·2) | 2·7% (1·3–4·1) | 1·0% (0·3–1·6) | 9·3% (4·8–13·8) | 6·4% (2·6–10·3) | 2·8% (0·3–5·3) | 4·8% (3·4–6·8) | 3·4% (2·3–5·2) | 1·3% (0·8–2·2) |
| KwaZulu-Natal | 3·5% (1·6–5·5) | 1·8% (0·6–3·0) | 1·7% 0·2–3·2) | 8·8% (3·0–14·6) | 6·4% (2·3–10·4) | 2·4% (0–4·9) | 4·9% (3·2–7·5) | 2·9% (1·8–4·5) | 1·9% (1·0–3·8) |
| Limpopo | 3·4% (2·0–4·7) | 1·4% (0·4–2·4) | 2·0% (1·1–2·9) | 6·2% (2·6–9·7) | 2·5% (0–5·1) | 3·5% (0·5–6·5) | 3·9% (2·8–5·5) | 1·6% (0·9–2·9) | 2·2% (1·5–3·4) |
| Mpumalanga | 6·0% (4·4–7·7) | 4·2% (2·8–5·6) | 1·8% (0·9–2·7) | 15·5% (9·2–21·7) | 7·6% (3·2–12·0) | 7·8% (3·5–12·1) | 8·4% (6·5–11·0) | 5·1% (3·7–7·0) | 3·0% (2·0–4·5) |
| North West | 3·1% (1·5–4·6) | 1·9% (0·8–3·1) | 1·1% (0·2–2·0) | 9·7% (5·9–13·4) | 4·3% (1·4–7·1) | 5·3% (2·8–7·9) | 4·9% (3·6–6·8) | 2·6% (1·8–3·9) | 2·2% (1·4–3·5) |
| Northern Cape | 2·0% (1·1–3·0) | 1·3% (0·4–2·1) | 0·8% (0·1–1·4) | 5·0% (2·5–7·5) | 2·6% (0·8–4·3) | 2·4% (0·5–4·3) | 3·0% (2·1–4·2) | 1·7% (1·0–2·8) | 1·3% (0·7–2·3) |
| Western Cape | 2·9% (1·5–4·3) | 2·0% (0·7–3·2) | 0·9% (0·3–1·6) | 6·1% (3·6–8·6) | 4·5% (2·1–7·0) | 1·5% (0·5–2·5) | 4·2% (3·2–5·5) | 3·0% (2·1–4·2) | 1·2% (0·8–1·8) |
RR=rifampicin resistance. MDR=multidrug resistance. RMR=rifampicin mono-resistance.
Compared with the MDR tuberculosis point prevalence estimate nationally, rifampicin-resistant tuberculosis prevalence was significantly higher overall at 4·6% (95% CI 3·5–5·7, p=0·01), and in new cases at 3·4% (2·5–4·3, p=0·03), whereas in retreatment cases it was 7·1% (4·8–9·5, p=0·07; table 2). The rifampicin-resistant tuberculosis prevalence ranged between 3·0% (95% CI 2·1–4·2) and 4·9% (3·2–7·5) for eight of the provinces, whereas Mpumalanga province again had the highest prevalence at 8·4% (6·5–11·0). The higher prevalence in Mpumalanga province was observed in both new and retreatment cases. Regional variation was observed in RMR tuberculosis cases with point prevalence of MDR tuberculosis and RMR tuberculosis notably different in Gauteng province at 3·4% (95% CI 2·3–5·2) and 1·3% (0·8–2·2), and in Western Cape province it was 3·0% (2·1–4·2) and 1·2% (0·8–1·8), respectively (table 3). The MDR to RMR ratio of the point estimates was close to 1:1 for several provinces (appendix p 9). Prevalence among HIV-positive cases was higher than HIV-negative cases for both rifampicin-resistant tuberculosis (4·9%, 95% CI 3·8–6·1 vs 3·2%, 2·1–4·3) and MDR tuberculosis (3·1%, 2·2–4·0 vs 2·0%, 1·1–2·8; appendix p 8).
The prevalence of any isoniazid resistance nationally (9·3%, 95% CI 7·9–10·7) was higher than that of any rifampicin resistance (4·6%, 3·5–5·7; table 2). The point prevalence of IMR tuberculosis ranged between 5·3% and 8·1% across the nine provinces with no notable difference by previous tuberculosis treatment history (appendix p 6). The prevalence of resistance among tuberculosis cases was relatively low for pyrazinamide (3·7%, 95% CI 2·9–4·5) and the fluoroquinolone ofloxacin (1·4%, 0·9–1·8; table 2).
Second-line drug resistance prevalence was determined among MDR tuberculosis and RMR tuberculosis cases. The prevalence of resistance to drugs used empirically in the treatment of MDR tuberculosis was 44·7% (95% CI 25·9–63·6) for ethionamide and 59·1% (49·0–69·1) for pyrazinamide, contrasting with the point estimate of 5·3% (2·2–8·3) for resistance to para-aminosalicylic acid (table 4). However, among RMR tuberculosis cases, the prevalence of resistance to ethionamide (11·2%, 95% CI 0–23·8) and pyrazinamide (13·9%, 2·0–25·9) were notably lower. Resistance prevalence to the key second-line drug classes, fluoroquinolones (ofloxacin) and injectable antituberculosis drugs, were both 13·0% (95% CI 5·0–21·0; table 4; appendix). Cross-resistance between selected drugs was also assessed (appendix p 7). The XDR tuberculosis prevalence among MDR tuberculosis confirmed cases was 4·9% (95% CI 1·0–8·8) nationally (table 4).
Table 4:
National second-line drug resistance among multidrug resistance and rifampicin mono-resistance cases, South Africa, 2012–14
| MDR (%, 95% CI) | RMR (%, 95% CI) | |
|---|---|---|
| Pyrazinamide | 59·1% (49·0–69·1) | 13·9% (2·0–25·9) |
| Ethambutol | 44·1% (30·2–58·0) | 19·3% (0–45·9) |
| Streptomycin | 63·0% (52·8–73·2) | 16·7% (3·4–30·1) |
| Ethionamide | 44·7% (25·9–63·6) | 11·2% (0–23·8) |
| Para-aminosalicylic acid | 5·3% (2·2–8·3) | 16·2% (0–35·5) |
| Second-line injectable | 13·0% (5·0–20·9) | 17·8% (0–41·7) |
| Ofloxacin | 13·0% (5·0–21·0) | 10·4% (0–28·3) |
| XDR tuberculosis | 4·9% (1·0–8·8) | .. |
MDR=multidrug resistance. RMR=rifampicin mono-resistance. XDR=extensively resistant.
The midpoint estimate of the MDR tuberculosis case burden for 2014 was 8249 and was similar to the number reported as microbiologically confirmed (n=8035; table 5). For rifampicin-resistant tuberculosis, the 95% CI estimated burden ranged between 10 311 and 16 792, whereas the case burden reported (n=18 631) was higher than the estimate; this was also observed in three of the nine provinces. The number of IMR tuberculosis cases reported nationally in 2014 was 851 and was much lower than the estimate (17 970, 95% CI 15 024·20 916).
Table 5:
Estimated burden of rifampicin-resistant tuberculosis and multidrug-resistant tuberculosis compared with numbers reported for 2014 by province in South Africa
| mPTB2014 reported8 | Rifampicin-resistant tuberculosis |
Multidrug-resistant tuberculosis |
|||
|---|---|---|---|---|---|
| Number (95% CI) | Reported* | Number (95% CI) | Reported* | ||
| Eastern Cape | 60 518 | 1997 (1331–2965) | 3923 | 1271 (787–2179) | 2071 |
| Free State | 15 833 | 728 (507–1045) | 1008 | 364 (237–570) | 309 |
| Gauteng | 46 467 | 2230 (1580–3160) | 2530 | 1580 (1069–2416) | 730 |
| KwaZulu-Natal | 72 743 | 3564 (2328–5456) | 5075 | 2110 (1309–3273) | 2354 |
| Limpopo | 15 921 | 621 (446–876) | 717 | 255 (143–462) | 113 |
| Mpumalanga | 18 439 | 1549 (1199–2028) | 1680 | 940 (682–1291) | 528 |
| North West | 17 790 | 872 (640–1210) | 1036 | 463 (320–694) | 327 |
| Northern Cape | 9607 | 288 (202–403) | 508 | 163 (96–269) | 261 |
| Western Cape | 37 272 | 1565 (1193–2050) | 2154 | 1118 (783–1565) | 1342 |
| South Africa | 294 590 | 13 551 (10 311–16 792) | 18 631 | 8249 (5892–10 605) | 8035 |
mPTB=microbiologically confirmed pulmonary tuberculosis.
The WHO Global Report 20151 (reports 18 734 cases; however, it includes 103 cases with an unassigned province).
Discussion
The South African Tuberculosis Drug Resistance Survey 2012·14 provides an update of the population level first-line and second-line drug resistance estimates in a country with the highest per capita incidence of tuberculosis globally. The emergence of RMR tuberculosis among new cases and the high levels of second-line resistance are major causes of concern and have important implications for the introduction of new rapid technologies for diagnosis, as well as the use of short regimens and new therapeutic agents. Furthermore, although the number of cases of rifampicin-resistant tuberculosis and MDR tuberculosis diagnosed in the country was comparable to the burden reported through standard-of-care testing, the problem of IMR tuberculosis was largely undetected using current routine testing algorithms. To our knowledge, the present survey was the largest of its kind done globally, with over 100 000 people tested. The consistently higher prevalence across provinces of rifampicin and multidrug resistance among HIV-infected individuals, confirms the importance of HIV infection in the tuberculosis epidemic.
The national prevalence of MDR tuberculosis in 2012–14 remained relatively unchanged (2·8%) compared with that reported in 2001–02 (2·9%). Among new cases, the prevalence of MDR tuberculosis was 2·1%, and similar to the global estimate1 of 3·3%, whereas in previously treated cases it was much lower (4·6% compared with 20%, respectively). This finding might be related to a high mortality rate in the local setting, which was twice as high in 2002 compared with 20139 particularly in HIV-infected individuals not on antiretroviral therapy, and thus a second episode would not have occurred. Alternatively, introduction of new diagnostics (eg, line-probe assays in 2008 and Xpert MTB/RIF in 2011) that tested for drug resistance irrespective of treatment history, might have resulted in an effective cure and prevented a recurrence. The absolute number of cases reported for 2014 was in line with the estimate derived from the survey, which is encouraging. However, the survey estimates only included microbiologically confirmed cases; whereas 34·3% of cases notified in South Africa in 2014 were clinically diagnosed,1 the absolute number is likely an underestimate on our part.
Contributory factors for the higher provincial prevalence of MDR tuberculosis observed in Mpumalanga (5·1%) than the national estimate (2·8%), might include cross-border migration from neighbouring countries such as Swaziland, which has reported the highest MDR tuberculosis prevalence in the region.10 This finding illustrates the need for a regional approach in dealing with efforts aimed at combating drug-resistant tuberculosis. Additionally, this province also had the highest prevalence of tuberculosis-HIV coinfection (77%) in the current survey, and other socioeconomic factors might also have contributed.
The significant difference between the rifampicin-resistant tuberculosis and MDR tuberculosis estimates highlights the increasing relevance of RMR tuberculosis, which contributes to the growing drug-resistant tuberculosis crisis and counters the simplistic dogma that rifampicin-resistant tuberculosis and MDR tuberculosis are synonymous. Significant increases in rifampicin resistance among new cases compared with the previous survey (table 2) were observed, almost doubling from 1·8% to 3·4%. The same trend was evident at the provincial level, with increases in point estimates observed across all provinces among new cases. Increases in rifampicin resistance among new cases indicate primary resistance driven by transmission, which is of concern in the South African context with its high rates of HIV infection, now being coupled to an increased risk of acquiring rifampicin-resistant M tuberculosis complex infection. The introduction of Xpert MTB/RIF as a primary diagnostic tool targeting presumptive tuberculosis cases enables simultaneous detection of tuberculosis and rifampicin resistance. Widespread adoption is essential for early diagnosis of primary drug-resistant cases, which would be missed if only retreatment cases were tested. Additionally, the higher prevalence of rifampicin-resistant tuberculosis and MDR tuberculosis among HIV-infected cases, highlights the importance of using this technology universally in high burdened HIV-infected settings.
The WHO-approved mycobacteria growth indicator tube methodology was used for drug susceptibility testing in the present survey, but recent data indicate that this methodology might record false susceptible findings in strains harbouring specific rpoB mutations and could account for more than 10% of cases.11 Thus, our rifampicin-resistant tuberculosis estimates might be an underestimate in the survey, but would have been detected with the currently used molecular diagnostic methods. This possibly explains the higher case burden reported in 2014 compared with the burden estimate derived from the survey findings (table 5).
The prevalence of RMR tuberculosis in South Africa has also increased substantially since the 2001–02 survey, notably among new cases, and is the primary reason for the doubling in rifampicin-resistant tuberculosis. Clonal transmission has been shown to be an important driver of RMR tuberculosis and other drug resistance.12–14 Younger patients (aged 25–29 years), who are less likely to have had previous tuberculosis treatment exposure have also been shown to be at increased risk of RMR tuberculosis.15 Emergence of single drug resistance is unusual when standard combination therapy is used. Adequate dosage concentrations are crucial and concerns raised about the current rifampicin dosage being too low have important global implications.16 This problem is compounded when patients are on concurrent antiretroviral therapy, abuse alcohol, or take treatment irregularly, all of which have been associated with rifampicin mono-resistance related to deficient drug bioavailability.17,18 Although RMR strains might have originated through selection of rifampicin resistance during treatment, transmission will increase if left unchecked.
The WHO estimate in 2014 for MDR tuberculosis cases in South Africa was 6200, whereas 18 734 rifampicin-resistant tuberculosis and MDR tuberculosis cases were reported from the country.1 This WHO estimate for MDR tuberculosis alone was lower than the survey estimate (n=8249) and importantly did not take into account RMR tuberculosis. The latter is essentially managed as MDR tuberculosis, and as observed in the current survey, accounts for a large (39% of all rifampicin-resistant strains) and expanding burden. This major shortcoming in WHO reporting has been addressed in the 2016 report and more accurately reflects the true burden of drug-resistant tuberculosis in South Africa, which is now estimated at 20 000 cases.
Furthermore, the number of rifampicin-resistant and MDR tuberculosis cases reported by South Africa accounts for 18 734 (73%) of 25 531 cases in Africa, while among notified tuberculosis cases it was 318 193 (24%) of 1 342 400 cases. The disproportionately higher number of rifampicin-resistant and MDR tuberculosis cases from South Africa appears to be an outlier. However, the survey does confirm the high case burden of MDR tuberculosis notified from South Africa, which is likely undetected in less resourced African countries and could undermine WHO’s END-TB strategy if improvement in access to laboratory testing is not addressed.
Significant increases in overall IMR have also been noted, increasing from 2·7% in the 2001–02 survey to 4·9% in the current survey. There was no significant difference in IMR prevalence between new and previously treated cases, suggesting that previous tuberculosis combination therapy is unlikely to contribute to IMR. The IMR point estimate, irrespective of resistance to other first-line drugs, was 5% or more in all provinces (appendix p 6). IMR tuberculosis prevails across many settings in the world and in a meta-analysis by Menzies and colleagues19 it accounted for almost half of all tuberculosis drug resistance.
Globally, South Africa has one of the largest isoniazid preventative therapy programmes and both previous isoniazid preventative therapy and previous tuberculosis therapy, and younger age groups were identified as risk factors.20 An association between isoniazid preventative therapy and IMR or other drug resistance has not been shown in a WHO-initiated review of published data.21 However, a model-based study on community-administered isoniazid preventative therapy22 has suggested that this is likely to occur at a population level and could be missed when analysing studies involving small numbers of patients. The use of rifapentine in combination with isoniazid as preventative therapy does offer a promising approach to prevent the emerging risk of IMR tuberculosis and results of clinical trials are awaited.
The estimated case burden of IMR tuberculosis in 2014 was almost 20-fold higher than the reported number of diagnosed cases through the public sector laboratories in the country. Xpert MTB/RIF, which has ensured every newly diagnosed case of tuberculosis in South Africa can be concurrently tested for rifampicin resistance, does not test for isoniazid resistance. A review on IMR tuberculosis has noted poorer clinical outcomes in such cases23 and thus consideration needs to be given for all tuberculosis cases diagnosed being tested for isoniazid resistance or alternatively strengthening of the continuation regimen with a third agent. Furthermore, inadequate treatment of these cases would in effect result in rifampicin monotherapy during the continuation phase and over time lead to an increase in MDR tuberculosis, as has been previously shown.24
The present survey is the first to provide population level estimates of second-line resistance in South Africa. Although the frequency of resistance to fluoroquinolones was relatively low at 13% among MDR tuberculosis cases, high rates of resistance to companion drugs prevailed. The ethionamide resistance rate was 44·7%. MDR tuberculosis cases are by definition isoniazid-resistant and mutations in the inhA promoter region, accounting for approximately 8–43% of isoniazid-resistant strains,25 would confer cross-resistance to ethionamide. Information on inhA mutations is available through the use of line-probe assays and could be used to guide therapeutic decision making. Pyrazinamide, another drug used in drug resistance regimens, has potent sterilising activity but among MDR cases more than half showed resistance to this drug (59·1%, 95% CI 49·0–69·1). Our finding is corroborated by other studies showing similarly high prevalence of pyrazinamide resistance.24,26,27 With these high rates of resistance, further selection of resistance and consequently poor patient outcomes are likely to persist, unless new strategies and drugs are developed—this should be a global priority.
WHO has endorsed the use of the line-probe assay for second-line resistance testing to rapidly identify pre-XDR and XDR tuberculosis cases,28 constituting an important step in selecting rifampicin-resistant tuberculosis and MDR tuberculosis cases for the new seven-drug combination short-course regimen. The XDR cartridge on the GeneXpert platform, although not currently available, is an urgent need in light of the resistance levels observed and efforts to decentralise drug-resistant tuberculosis management. Although the background second-line resistance is a concern, rifampicin-resistant and RMR tuberculosis cases, which are on the increase, show lower levels of resistance and will be best suited for the short course regimen. Furthermore, isoniazid, even at a standard dosage for these RMR tuberculosis cases, would provide an effective oral agent. The inclusion of clofazimine, although not tested in the present survey, is likely to show low resistance prevalence in patients with rifampicin-resistant tuberculosis and MDR tuberculosis since the drug was historically reserved for pre-XDR tuberculosis and XDR tuberculosis cases. Thus, at least three drugs are likely to be effective despite the worrying findings from this survey.
The situation for pre-XDR tuberculosis and XDR tuberculosis cases accounting for more than one in every eight rifampicin-resistant tuberculosis cases, is however less promising unless an aggressive approach is taken to consider all the new drugs (eg, bedaquiline and delamanid) and repurposed drugs (eg, linezolid) for the development of an effective combination regimen for these cases. One drug to which very low levels of resistance have been encountered is para-aminosalicylic acid, which is re-emerging as a therapeutic option,29 although drug tolerability concerns have limited its use. Despite the excitement with the introduction of new drugs for tuberculosis, investment in drug discovery is still needed because these new drugs are arriving just in time to address a current and dire need but leave nothing for the future.
The XDR tuberculosis estimate among MDR tuberculosis cases in this survey of 4·9% was lower than that reported globally at 9·7%,1 but the difference was not significant. This finding suggests that the XDR tuberculosis problem that has seen two outbreaks during the period between the two drug resistance surveys has not become widespread across the country. A contributory factor could have been the high mortality associated with these cases. Additionally, XDR tuberculosis cases could have been concentrated in certain provinces or districts and this survey might not have been powered to assess the distribution of such cases.
The findings of this survey are important but should be seen in the context of certain limitations. This large nationwide survey was done using existing health services in a resource constrained setting. The recording of previous treatment history was by self-report and prone to recall bias; however, the retreatment rates reported here are comparable to findings observed in the 2001–02 survey. Patient screening was not consistently consecutive and a large proportion of cases were not included. Non-consecutive recruitment is unlikely to have an impact on the survey outcomes because the study population included confirmed tuberculosis cases only, and predicting tuberculosis in patients would be difficult, even for experienced clinicians. Non-inclusion did not show specific geographical localisation and was therefore likely to be random. To address these concerns, imputation and inverse probability weighting were applied, and although the estimates were similar,30 we have reported on the adjusted data. Lastly, drug susceptibility testing has inherent limitations and is less reliable for second-line drugs. However, the survey used established procedures at an International Organization for Standardization-accredited reference laboratory, which is part of the WHO supranational reference laboratory network, and showed good performance in the external quality assurance programme for both first-line and second-line drug testing. In addition, and where available, sequencing was done to cross-check resistance profiles.
Supplementary Material
Research in context.
Evidence before this study
We searched PubMed for original research that presented results for national and provincial prevalence of drug-resistant tuberculosis in South Africa published in English between Jan 1, 2000, and Dec 31, 2017. We combined search terms for tuberculosis/TB, prevalence, drug resistance, survey/DRS, and South Africa and looked for studies indicating population level prevalence estimates for first-line and second-line resistance (“rifampicin”, “isoniazid”, “MDR”, and “XDR”). Only one previous national drug resistance survey was done in South Africa in 2001–02. Although these surveys are recommended to be repeated every 5 years, this was not done. The previous survey showed low levels of multidrug-resistant (MDR) tuberculosis and showed a relatively low prevalence rate of 1·6% (95% CI 1·1–2·1) in new cases and 6·6% (4·9–8·2) in retreatment cases. Several publications have highlighted the emergence of extensively drug-resistant tuberculosis in KwaZulu-Natal and Eastern Cape provinces and more recently the emergence of rifampicin monoresistant tuberculosis in South Africa. Studies have also highlighted person-to-person transmission as an important driver of drug-resistant tuberculosis in South Africa. However, these studies have been either small or geographically restricted and not designed to provide population level estimates at a national or provincial level for the different types of drug resistance.
Added value of this study
The current survey provides updated first-line tuberculosis drug resistance prevalence estimates for South Africa that have been long overdue. An increase in rifampicin resistance nationally among new cases suggests ongoing transmission as a primary reason; rifampicin resistance is widespread requiring universal testing for drug resistance. Isoniazid resistance was close to 10% nationally and has implications for tuberculosis preventative therapy. Both ofloxacin and pyrazinamide were also tested among tuberculosis cases and provide country level information on these widely used companion drugs in new regimens being trialed. For the first time, population level second-line resistance is reported for South Africa, and is worrying. Commonly used second-line agents have shown a high prevalence of resistance with almost half being resistant to pyrazinamide and more than a quarter resistant to ethionamide. However, the national population prevalence of extensively drug-resistant tuberculosis was similar to the global average.
Implications of all the available evidence
Our findings support the universal roll-out of the Xpert MTB/RIF assay for the early detection of drug-resistant tuberculosis irrespective of previous treatment history. The endorsement of the first-line and now second-line molecular assays is a timely improvement to ensure that patients on the new short MDR tuberculosis regimen are appropriately managed and second-line resistance excluded early. South Africa uses isoniazid monotherapy for prevention and an evaluation of the impact of the intervention on emerging resistance is needed. In addition, combination therapies for prevention (eg, rifapentine and isoniazid) should be considered in light of the findings.
Acknowledgments
We thank the entire team at the TB Cluster at the National Department of Health, as well as provincial and district tuberculosis managers and their teams across all the South African provinces. We are also grateful for the support received from the National Health Laboratory Services. The survey would not have been possible without the extremely hard work and sacrifice by the survey team, comprising of field staff, laboratory staff, and data entry and management staff at the Centre for Tuberculosis at the National Institute for Communicable Diseases and support from the President’s Emergency Plan for AIDS Relief (PEPFAR) through Centers for Disease Control (CDC) South Africa. Additionally, we thank the original team for their contribution to the initial planning of the survey. We also thank Matteo Zignol, Anna Dean, and Babis Sismanidis from WHO, and Julia Ershova from the US CDC for technical support. Lastly, we thank Harry Moultrie for producing the geospatial map of the survey sites and Farzana Ismail for final proof-reading of the manuscript. This project has been supported by the PEPFAR through the CDC under the terms of 1U19GH000571. The findings and conclusions are those of the authors and do not necessarily represent the official position of funding agencies.
Footnotes
See Online for appendix
Declaration of interests
We declare no competing interests.
References
- 1.WHO. Global TB report 2015. 2015. http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf?ua=1 (accessed Jan 11, 2017).
- 2.Weyer K, Brand J, Lancaster J, Levin J, van der Walt M. Determinants of multidrug-resistant tuberculosis in South Africa: results from a national survey. S Afr Med J 2007; 97 11: 1120–28. [PubMed] [Google Scholar]
- 3.Marisa K, Robin Mark W, Cindy H, et al. Emergence and spread of extensively and totally drug-resistant tuberculosis, South Africa. Emerg Infect Dis J 2013; 19: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ndjeka N Strategic overview of MDR-TB care in South Africa. 2014. http://www.health-e.org.za/wp-content/uploads/2014/03/Strategic_overview_of_MDR_TB_RSA.pdf (accessed April 15, 2016).
- 5.Ndjeka N, Conradie F, Schnippel K, et al. Treatment of drug-resistant tuberculosis with bedaquiline in a high HIV prevalence setting: an interim cohort analysis. Int J Tuberc Lung Dis 2015; 19: 979–85. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Guidelines for surveillance of drug resistance in tuberculosis. Geneva: World Health Organization, 2015. [Google Scholar]
- 7.Salman Siddiqi SR-G, Alexander H, Drobniewski F, Feldman K. MGIT procedure manual for Bactec MGIT 960 TB system. 2006. http://www.finddiagnostics.org/export/sites/default/resource-centre/find_documentation/pdfs/mgit_manual_nov_2007.pdf (accessed Jan 3, 2017).
- 8.NICD. Microbiologically confirmed tuberculosis 2004–2015: South Africa: 2017. http://www.nicd.ac.za/index.php/centres/centre-for-tuberculosis/public-health-surveillance/surveillance-of-microbiologically-confirmed-tb/ (accessed April 5, 2017). [Google Scholar]
- 9.STATSSA. MDG goal 6: combat HIV, malaria and other diseases. 2015. http://www.statssa.gov.za/MDG/MDG_Goal6_report_2015_.pdf (accessed June 1, 2017).
- 10.Sanchez-Padilla E, Dlamini T, Ascorra A, et al. High prevalence of multidrug-resistant tuberculosis, Swaziland, 2009–2010. Emerg Infect Dis 2012; 18: 29–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rigouts L, Gumusboga M, de Rijk WB, et al. Rifampin resistance missed in automated liquid culture system for Mycobacterium tuberculosis isolates with specific rpoB mutations. J Clin Microbiol 2013; 51: 2641–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shah NS, Auld SC, Brust JC, et al. Transmission of extensively drug-resistant tuberculosis in South Africa. N Engl J Med 2017; 376: 243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dheda K, Limberis JD, Pietersen E, et al. Outcomes, infectiousness, and transmission dynamics of patients with extensively drug-resistant tuberculosis and home-discharged patients with programmatically incurable tuberculosis: a prospective cohort study. Lancet Respir Med 2017; 5: 269–81. [DOI] [PubMed] [Google Scholar]
- 14.Yoshida S, Tsuyuguchi K, Suzuki K, et al. Molecular epidemiology of rifampicin mono-resistant Mycobacterium tuberculosis [in Japanese]. Kekkaku 2012; 87: 41–45. [PubMed] [Google Scholar]
- 15.Coovadia YM, Mahomed S, Pillay M, Werner L, Mlisana K. Rifampicin mono-resistance in Mycobacterium tuberculosis in KwaZulu-Natal, South Africa: a significant phenomenon in a high prevalence TB-HIV region. PLoS One 2013; 8: e77712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Ingen J, Aarnoutse RE, Donald PR, et al. Why do we use 600 mg of rifampicin in tuberculosis treatment? Clin Infect Dis 2011; 52: e194–99. [DOI] [PubMed] [Google Scholar]
- 17.Meyssonnier V, Bui TV, Veziris N, Jarlier V, Robert J. Rifampicin mono-resistant tuberculosis in France: a 2005–2010 retrospective cohort analysis. BMC Infect Dis 2014; 14: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanders M, Van Deun A, Ntakirutimana D, et al. Rifampicin mono-resistant Mycobacterium tuberculosis in Bujumbura, Burundi: results of a drug resistance survey. Int J Tuberc Lung Dis 2006; 10:178–83. [PubMed] [Google Scholar]
- 19.Menzies D, Benedetti A, Paydar A, et al. Standardized treatment of active tuberculosis in patients with previous treatment and/or with mono-resistance to isoniazid: a systematic review and meta-analysis. PLoS Med 2009; 6: e1000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cattamanchi A, Dantes RB, Metcalfe JZ, et al. Clinical characteristics and treatment outcomes of isoniazid mono-resistant tuberculosis. Clin Infect Dis 2009; 48: 179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO. Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resourceconstrained settings. 2011. http://apps.who.int/iris/bitstream/10665/44472/1/9789241500708_eng.pdf (accessed Jan 18, 2017).
- 22.Mills HL, Cohen T, Colijn C. Community-wide isoniazid preventive therapy drives drug-resistant tuberculosis: a model-based analysis. Sci Transl Med 2013; 5: 180ra49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobson KR, Theron D, Victor TC, Streicher EM, Warren RM, Murray MB. Treatment outcomes of isoniazid-resistant tuberculosis patients, Western Cape Province, South Africa. Clin Infect Dis 2011; 53: 369–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alame-Emane AK, Xu P, Pierre-Audigier C, et al. Pyrazinamide resistance in Mycobacterium tuberculosis arises after rifampicin and fluoroquinolone resistance. Int J Tuberc Lung Dis 2015; 19: 679–84. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Yew WW. Mechanisms of drug resistance in Mycobacterium tuberculosis: update 2015. Int J Tuberc Lung Dis 2015; 19: 1276–89. [DOI] [PubMed] [Google Scholar]
- 26.Mphahlele M, Syre H, Valvatne H, et al. Pyrazinamide resistance among South African multidrug-resistant Mycobacterium tuberculosis isolates. J Clin Microbiol 2008; 46: 3459–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Louw G, Warren R, Donald P, et al. Frequency and implications of pyrazinamide resistance in managing previously treated tuberculosis patients. Int J Tuberc Lung Dis 2006; 10: 802–07 [PubMed] [Google Scholar]
- 28.WHO. The use of molecular line probe assays for the detection of resistance to second-line anti-tuberculosis drugs. 2016. http://apps.who.int/iris/bitstream/10665/246131/1/9789241510561-eng.pdf?ua=1 (accessed Feb 7, 2017).
- 29.Donald PR, Diacon AH. Para-aminosalicylic acid: the return of an old friend. Lancet Infect Dis 2015; 15: 1091–99. [DOI] [PubMed] [Google Scholar]
- 30.NICD. South African Tuberculosis Drug Resistance Survey 2012–14. 2016. http://www.nicd.ac.za/?page=south_african_tuberculosis_drug_resistance_survey&id=232 (accessed Feb 3, 2017).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


