Abstract
Diabetes mellitus (DM) and abnormal glucose metabolism are associated with cardiovascular (CV) disease. We investigated the prevalence and prognostic importance of dysglycaemia in patients with acute coronary syndromes (ACS) in the PLATelet inhibition and patient Outcomes (PLATO) trial. Diabetes was defined as known diabetes or HbA1c ≥ 6.5% or non-fasting glucose ≥ 11.1 mmol/L on admission, prediabetes as HbA1c ≥ 5.7% but < 6.5%, and no diabetes as HbA1c < 5.7%. The primary endpoint was the composite of CV death, spontaneous myocardial infarction type 1 (sMI) or stroke at 12 months. Multivariable Cox regression models, adjusting for baseline characteristics, and biomarkers NT-proBNP and troponin I, were used to explore the association between glycaemia and outcome. On admission, 16,007 (86.1%) patients had HbA1c and/or glucose levels available and were subdivided into DM 38.5% (6160) (1501 patients had no previous DM diagnosis), prediabetes 38.8% (6210), and no DM 22.7% (3637). Kaplan Meier event rates at 12 months for CV death, sMI or stroke per subgroups were 14.5% (832), 9.0% (522), and 8.5% (293), respectively with multivariable adjusted HRs, versus no diabetes, for diabetes: 1.71 (1.50–1.95) and for prediabetes 1.03 (0.90–1.19). Corresponding event rates for CV death were 6.9% (391), 3.4% (195) and 3.0% (102), respectively, with adjusted HRs for patients with DM of: 1.92 (1.42–2.60) and for prediabetes 1.02 (0.79–1.32). Abnormal glucose metabolism is common in ACS patients, but only patients with definite DM have an increased CV risk, indicating that prediabetes is not immediately associated with worse CV outcomes.
Keywords: Diabetes, Pre-diabetes, Hemoglobin A1C, Acute coronary syndromes, Myocardial infarction, Risk prediction
Highlights
Abnormal glucose metabolism is common in ACS patients.
Patients with definite diabetes have a doubled CV risk during the first year after an ACS event.
However, prediabetes is not immediately associated with worse CV outcomes during up to one year of follow up.
Although prediabetes is important to diagnose, the CV risk is not increased, compared with normoglycemic patients, during the first year after ACS.
Introduction
Diabetes mellitus (DM) is associated with a two- to four-fold increased risk for cardiovascular (CV) events compared with non-diabetics [1]. In patients without diagnosed DM, but with borderline increased haemoglobin A1c (HbA1c), heightened fasting glucose or abnormal glucose tolerance test, an increased risk of CV events has been observed in a general population [2, 3]. The impact of dysglycaemia on CV risk in patients with acute coronary syndrome (ACS) is less clear with partly conflicting results [2–10]. In the PLATelet inhibition and patient Outcomes (PLATO) trial, we evaluated the effect of the antiplatelet drug ticagrelor, compared to clopidogrel, in patients with ACS [11, 12]. We have previously reported ticagrelor to be both more efficacious and of similar safety compared with clopidogrel, irrespective of diabetes status [8]. In the current substudy, we stratified patients into clinically accepted subgroups of glycaemia based on admission non-fasting glucose and HbA1c to explore the impact of dysglycaemia on CV outcomes [3, 8].
Methods
Study population
The PLATO trial (NCT00391872) enrolled 18624 patients with ACS, who were randomised to either clopidogrel or ticagrelor treatment in addition to optimal medical therapy, including aspirin, and optional invasive strategy [11, 12]. All patients were evaluated for diabetes at baseline, and baseline non-fasting glucose concentration and HbA1c were collected. All participants provided written informed consent and the study complied with the declaration of Helsinki. The study was approved by all local Ethics Committees and Institutional Review Boards.
Laboratory analysis
The details of laboratory sampling and handling have previously been published [11, 12].
Plasma glucose and HbA1c concentrations were determined with sandwich immunoassays on the Cobas® Analytics e601 Immunoanalyzer (Roche Diagnostics, Mannheim, Germany) at the Uppsala Clinical Research Center laboratory, Uppsala, Sweden.
Definitions of outcome events and glycaemia subgroups
The primary endpoint of the present biomarker substudy was the composite of CV death, stroke or spontaneous myocardial infarction (sMI) within one year of follow up. sMI was defined in accordance with the universal definition of myocardial infarction (MI), hence a non-procedure-related, non-fatal, MI type 1 [13].
DM was defined as patients with known diabetes or admission HbA1c ≥ 6.5% (≥ 48 mmol/mol), or non-fasting venous glucose ≥ 11.1 mmol/L on admission. Pre-DM was defined as patients with HbA1c ≥ 5.7% but < 6.5% (≥ 39 mmol/mol but < 48 mmol/mol) [3]. Patients with HbA1c < 5.7% were considered to have neither DM nor pre-DM (referred to here as ‘non-diabetes’) [3].
Statistical analysis
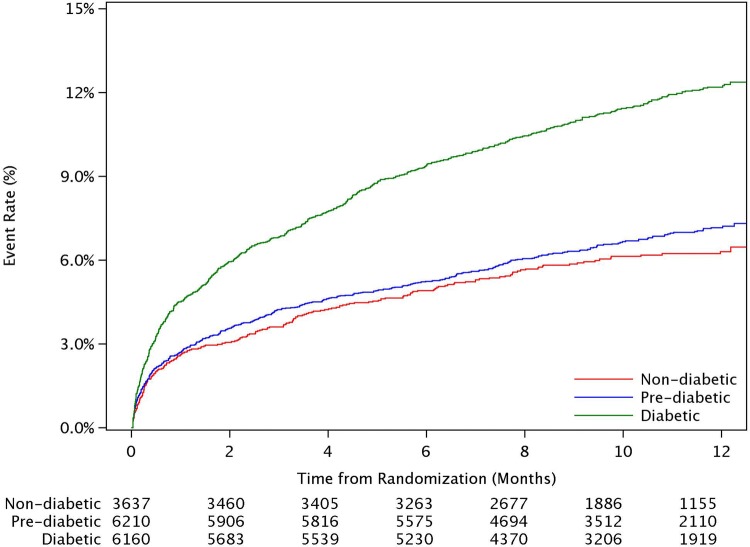
Baseline characteristics were presented by subgroups of glycaemia, and compared using chi-square or Kruskal–Wallis tests. Kaplan Meier event rates at 1-year, overall and by glycaemic subgroups, were estimated. The associations between glycaemic subgroups, with the non-diabetes group as reference, and the outcomes were assessed by Cox proportional hazard models. Unadjusted and adjusted hazard ratios were derived. Adjustment variables included baseline characteristics (age, gender, smoking status, type of ACS, and history of angina, MI, hypercholesterolemia, diabetes, hypertension, chronic kidney disease, previous; percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG); stroke or transient ischemic attack (TIA), as well as log transformed biomarkers; NT-pro-BNP and hs-troponin I. p-values less than 0.05 were considered statistically significant results. Statistical analyses were performed with SAS 9.4 (SAS Institute, Cary, NC) (Fig. 1).
Fig. 1.
Kaplan Meier plots of the composite endpoint per glycemic subgroups
Results
Information on previous DM, non-fasting glucose and/or HbA1c, were available for 16,007 patients (85.9%). On admission, 6160 patients (38.5%) had DM according to our pre-specified criteria, of which 1501 patients (9.4%) had no previous DM diagnosis, consequently new-onset DM. In the new-onset DM subgroup, 1076 patients had an HbA1c ≥ 6.5%. Another 201 individuals had non-fasting blood glucose above 11.1 mmol/L, but with normal HbA1c. A total of 224 patients had both an elevated HbA1c and non-fasting blood glucose above 11.1 mmol/L.
Patients with DM were older, and had more comorbidities compared to patients without DM (Table 1). In patients with DM, normal HbA1c (< 5.7%) was observed in 146 patients (2.4%), while HbA1c was between 5.7 and 6.4% in 811 patients (13.2%) and 4346 patients (70.5%) had an HbA1c of ≥ 6.5%. HbA1c was not available in 857 patients (13.9%) classified as diabetic by other criteria.
Table 1.
Baseline characteristics by glycemic subgroups
| Characteristic | Diabetic (N = 6160) |
Pre-diabetic (N = 6210) |
Non-diabetic (N = 3637) |
Overall (N = 16,007) |
p-value |
|---|---|---|---|---|---|
| Female gender | 2074 (33.7%) | 1703 (27.4%) | 854 (23.5%) | 4631 (28.9%) | < 0.0001 |
| Age, years (median, 25th–75th) | 64 (56–72) | 62 (54–71) | 60 (51–68) | 62 (54–71) | < 0.0001 |
| Weight, kg (median, 25th–75th) | 81.0 (70.0–92.0) | 80.0 (70.0–90.0) | 78.0 (68.0–86.0) | 80.0 (70.0–90.0) | < 0.0001 |
| Smoking status | < 0.0001 | ||||
| Non-smoker | 2794 (45.4%) | 2285 (36.8%) | 1273 (35.0%) | 6352 (39.7%) | |
| Ex-smoker | 1674 (27.2%) | 1481 (23.8%) | 875 (24.1%) | 4030 (25.2%) | |
| Habitual smoker | 1692 (27.5%) | 2444 (39.4%) | 1489 (40.9%) | 5625 (35.1%) | |
| Systolic blood pressure (mmHg) | 135 (120–150) | 130 (120–150) | 130 (120–149) | 133 (120–150) | < 0.0001 |
| Diastolic blood pressure (mmHg) | 80 (70–88) | 80 (70–90) | 80 (70–90) | 80 (70–90) | 0.0222 |
| Medical history | |||||
| Angina pectoris | 3211 (52.1%) | 2734 (44.0%) | 1361 (37.4%) | 7306 (45.6%) | < 0.0001 |
| Myocardial infarction | 1565 (25.4%) | 1180 (19.0%) | 585 (16.1%) | 3330 (20.8%) | < 0.0001 |
| Percutaneous coronary intervention | 1049 (17.0%) | 738 (11.9%) | 385 (10.6%) | 2172 (13.6%) | < 0.0001 |
| Coronary artery bypass graft | 546 (8.9%) | 293 (4.7%) | 137 (3.8%) | 976 (6.1%) | < 0.0001 |
| Non-haemorrhagic stroke | 324 (5.3%) | 206 (3.3%) | 99 (2.7%) | 629 (3.9%) | < 0.0001 |
| Hypertension | 4827 (78.4%) | 3787 (61.0%) | 1977 (54.4%) | 10,591 (66.2%) | < 0.0001 |
| Dyslipidaemia | 3389 (55.0%) | 2706 (43.6%) | 1446 (39.8%) | 7541 (47.1%) | < 0.0001 |
| Peripheral artery disease | 514 (8.3%) | 335 (5.4%) | 165 (4.5%) | 1014 (6.3%) | < 0.0001 |
| Chronic renal disease | 416 (6.8%) | 180 (2.9%) | 99 (2.7%) | 695 (4.3%) | < 0.0001 |
| Treatment approach | < 0.0001 | ||||
| Invasive | 4184 (67.9%) | 4489 (72.3%) | 2718 (74.7%) | 11,391 (71.2%) | |
| Type of ACS | < 0.0001 | ||||
| STEMI | 2183 (35.4%) | 2628 (42.3%) | 1582 (43.5%) | 6393 (39.9%) | |
| Medications at the time of randomization | |||||
| Aspirin | 5800 (94.2%) | 5834 (93.9%) | 3387 (93.1%) | 15021 (93.8%) | 0.1056 |
| Beta blockers | 4307 (69.9%) | 4382 (70.6%) | 2545 (70.0%) | 11234 (70.2%) | 0.7072 |
| ACE inhibitors | 3885 (63.1%) | 3400 (54.8%) | 186 (51.1%) | 9145 (57.1%) | < 0.0001 |
| Angiotensin II receptor blockers | 764 (12.4%) | 445 (7.2%) | 247 (6.8%) | 1456 (9.1%) | < 0.0001 |
| Statins | 4936 (80.1%) | 4978 (80.2%) | 2865 (78.8%) | 12,779 (79.8%) | 0.1904 |
| Biochemistry (median, 25th–75th) | |||||
| Creatinine clearancea (mL/min) | 76.9 (58.8–96.5) | 80.8 (64.1–98.5) | 84.3 (67.2-102.3) | 80.4 (63.0–99.0) | < 0.0001 |
| Glucose (mmol/L) | 9.3 (7.0–12.5) | 6.4 (5.6–7.5) | 6.1 (5.4–7.1) | 6.9 (5.7–8.8) | < 0.0001 |
| Haemoglobin A1c (%) | 7.2 (6.5–8.5) | 5.9 (5.8–6.1) | 5.5 (5.3–5.6) | 6.0 (5.7–6.6) | < 0.0001 |
| NT-proBNP (pmol/L) | 76 (24–244) | 53 (18–164) | 49 (17–147) | 59 (19–184) | < 0.0001 |
| High sensitivity troponin I (ng/Lµg/L) | 2.0 (0.2–11.8) | 2.0 (0.2–12.0) | 2.2 (0.2–12.2) | 2.1 (0.2–12.0) | 0.4910 |
aCockcroft Gault
In addition, 6210 (38.8%) patients had pre-DM defined as HbA1c concentrations of ≥ 5.7% but < 6.5%. Normal HbA1c concentrations (HbA1c < 5.7%) were observed in 3637 (22.7%) of the study population.
Glycaemia subgroups and outcome
The Kaplan Meier event rates at 12 months for the combined endpoint of CV death, sMI or stroke per subgroups were 12.2% (694) for patients with DM, 7.2% (409) for pre-DM and 6.3% (213) for patients with no DM (Table 2 and Fig 1). In a sensitivity analysis, all MIs (not only sMI) were evaluated in the composite endpoint (CV death, MI and stroke), with event rates at 12 months per subgroups of 14.5% (832) for patients with DM, 9.0% (522) for pre-DM and 8.5% (293) for patients with no DM.
Table 2.
Proportions, event rates and hazard ratios (HR) per glycemic subgroups
| Diabetes | Pre-diabetes | No diabetes | |
|---|---|---|---|
| Proportion and number of patients | 38.5% (6160) | 38.8% (6210) | 22.7% (3637) |
| of which were new diagnosed | 9.4% (1501) | ||
| Event rates at 12 months | |||
| CV death, sMI or stroke | 12.2% (694) | 7.2% (409) | 6.3% (213) |
| CV death | 6.9% (391) | 3.4% (195) | 3.0% (102) |
| HR (95%CI) | HR (95%CI) | ||
|---|---|---|---|
| HR versus no diabetes | |||
| CV death, sMI or stroke | 1.97 (1.69–2.29) | 1.12 (0.95–1.32) | 1 |
| CV death | 2.30 (1.85–2.86) | 1.12 (0.88–1.42) | 1 |
| Adjusted HR vs no diabetes (n = 14,033) | |||
| CV death, sMI or stroke | 1.39 (1.11–1.74) | 1.02 (0.86–1.22) | 1 |
| CV death | 1.92 (1.42–2.60) | 1.02 (0.79–1.32) | 1 |
The association between glycaemia subgroups and the combination of CV death, sMI or stroke is presented in Table 2.
The Kaplan Meier event rates for CV death alone were: 6.9% (391), 3.4% (195) and 3.0% (102), with adjusted HRs presented in Table 2.
The individual components of the composite endpoint were evaluated in secondary analysis and are presented in Table 2.
Discussion
DM is independently associated with CV events, but there are conflicting reports on the impact of pre-DM on outcomes [2–7, 9]. This may be due to differences in the identification, classification, follow-up and, in some cases, a lack of other important prognostic variables in ACS, including hs-troponin and NT-proBNP [5]. DM is a multifaceted syndrome, and the pathogenesis for CV disease may include macrovascular changes, endothelial cell dysfunction and accelerated atherosclerosis, with a subsequent increased risk for plaque rupture, thrombus formation and ultimately vessel occlusion [3].
In the current substudy, we found comorbidities to be more common in patients with DM, including disadvantageous biomarker levels such as elevated serum creatinine and NT-proBNP, indicating underlying organ dysfunction. We did not, however, observe any differences between patients with pre-DM and patients without DM.
Pre-DM, defined as blood glucose concentrations higher than normal but not meeting the definition of diabetes, is associated with an approximately 5–10% annual risk of developing type 2 DM [14]. When diagnosed with DM, the patient momentarily is considered to have heightened risk for adverse events, and the indication for cardiac revascularisation, medical treatments e.g. ACE inhibitors, and fluid therapy with angiography uses the presence of DM as a dichotomous condition [2, 3, 15]. It is, however, unknown if the observed heightened CV risk starts even at moderate levels of dysglycaemia or if abnormal glucose metabolism below a certain threshold may be non-pathogenic [3, 14].
In the current cohort, the proportion of patients with DM and at the same time a normal HbA1c was 2.5%, indicating that medical and lifestyle treatments still are not able to maintain normal HbA1c in patients with diabetes.
The increased CV risk for patients with manifest DM was, however, not observed in patients with pre-DM during the first year after ACS, and we believe this highlights that a direct effect of hyperglycaemia on clinical outcome may not be present, rather the deleterious hyperglycaemic effects may arise after a prolonged and accumulated exposure to dysglycemia.
Limitations
Manifest DM was one of several enrichment criteria employed to enter the PLATO trial if presenting with a non-STEACS [11, 12]. It is likely that the current population exhibited a larger proportion of patients with diagnosed DM than other ACS populations, and consequently proportionally smaller subgroups of patients with pre-DM and no DM. Although follow up was up to one year, the detrimental effect of DM was not observed within the first year of diagnosis in the current study, however this study was not designed to answer these important questions.
Conclusions
Abnormal glucose metabolism is common in patients with ACS and 9% of the PLATO study patients had undiagnosed diabetes. Although the overall event rate during the first year after ACS is high, we only observed patients with definite DM to have a further increased CV risk, indicating that pre-DM is not immediately associated with worse CV outcomes over the first year after ACS. Nonetheless, this finding does not diminish the need for close follow-up of patients with pre-DM in order to detect DM early, as recommended by international guidelines.
Acknowledgements
Open access funding provided by Uppsala University.
Author contributions
AÅ, DW, PGS, LW, SKJ, HAK, AS, RFS, and RCB contributed to the conception or design of the work. AÅ, DW, PGS, LW, SKJ, AB, HAK, AH, KH, AS, and RFS contributed to the acquisition, analysis, or interpretation of data for the work. AÅ and SKJ and RCB drafted the manuscript. All authors critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding
The original PLATO trial was funded by AstraZeneca. Support for the analysis and interpretation of results and preparation of the manuscript was provided through funds to the Uppsala Clinical Research Center and Duke Clinical Research Institute as part of the Clinical Study Agreement.
Compliance with ethical standards
Conflict of interest
AÅ: institutional research grants and speaker honoraria from AstraZeneca; institutional research grants from Roche Diagnostics. DW: nothing to disclose. PGS: grants and speaker/consultancy fees from Merck, Sanofi, and Servier; speaker/consultancy fees from AstraZeneca, Amarin, Amgen, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, GlaxoSmithKline, Janssen, Eli Lilly, Novartis, Pfizer, and Regeneron. LW: institutional grants from AstraZeneca, Roche Diagnostics, Merck & Co, GlaxoSmithKline, Boehringer Ingelheim, and Bristol-Myers Squibb/Pfizer; consultancy fees from Abbott; holds two patents licensed to Roche Diagnostics. SKJ: institutional research grants, honoraria, and consultancy/advisory board member fees from AstraZeneca; grants and honoraria from The Medicines Company; consultancy/advisory board member fees from Janssen and Bayer. AB: grants, honoraria, and consultancy fees from AstraZeneca, GlaxoSmithKline, Sanofi-Aventis, Bristol Myers Squibb/Pfizer, and Novartis; grants from Boehringer Ingelheim and Eisai. HAK: personal fees from AstraZeneca, Bayer Vital, and Roche Diagnostics. AH: employee at AstraZeneca. KH: grants and lecture fees from AstraZeneca; lecture fees from Bristol-Myers Squibb/Pfizer, Boehringer Ingelheim, Bayer, Daiichi Sankyo, Sanofi Aventis, and The Medicines Company. AS: institutional research grants from AstraZeneca, Roche Diagnostics, Bristol-Myers-Squibb/Pfizer, Boehringer Ingelheim, and GlaxoSmithKline; consultancy fees from Olink Proteomics. RFS: institutional research grants, honoraria, and consultancy fees from AstraZeneca and PlaqueTec; consultancy fees from Actelion, The Medicines Company, Bayer, Bristol-Myers Squibb/Pfizer, Avacta, Novartis, and Idorsia. RCB: scientific advisory board member fees from AstraZeneca and Ionis Pharmaceuticals; safety reviewing committee member fees from Portola and Akcea Therapeutics.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 2.Barr EL, Zimmet PZ, Welborn TA, Jolley D, Magliano DJ, Dunstan DW, Cameron AJ, Dwyer T, Taylor HR, Tonkin AM, Wong TY, McNeil J, Shaw JE. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab) Circulation. 2007;116:151–157. doi: 10.1161/CIRCULATIONAHA.106.685628. [DOI] [PubMed] [Google Scholar]
- 3.Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H, Marre M, Marx N, Mellbin L, Ostergren J, Patrono C, Seferovic P, Uva MS, Taskinen MR, Tendera M, Tuomilehto J, Valensi P, Zamorano JL, ESCCfP Guidelines. Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Document R, De Backer G, Sirnes PA, Ezquerra EA, Avogaro A, Badimon L, Baranova E, Baumgartner H, Betteridge J, Ceriello A, Fagard R, Funck-Brentano C, Gulba DC, Hasdai D, Hoes AW, Kjekshus JK, Knuuti J, Kolh P, Lev E, Mueller C, Neyses L, Nilsson PM, Perk J, Ponikowski P, Reiner Z, Sattar N, Schachinger V, Scheen A, Schirmer H, Stromberg A, Sudzhaeva S, Tamargo JL, Viigimaa M, Vlachopoulos C, Xuereb RG. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34:3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 4.Conaway DG, O'Keefe JH, Reid KJ, Spertus J. Frequency of undiagnosed diabetes mellitus in patients with acute coronary syndrome. Am J Cardiol. 2005;96:363–365. doi: 10.1016/j.amjcard.2005.03.076. [DOI] [PubMed] [Google Scholar]
- 5.Giraldez RR, Clare RM, Lopes RD, Dalby AJ, Prabhakaran D, Brogan GX, Jr, Giugliano RP, James SK, Tanguay JF, Pollack CV, Jr, Harrington RA, Braunwald E, Newby LK. Prevalence and clinical outcomes of undiagnosed diabetes mellitus and prediabetes among patients with high-risk non-ST-segment elevation acute coronary syndrome. Am Heart J. 2013;165:918–925 e2. doi: 10.1016/j.ahj.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Norhammar A, Tenerz A, Nilsson G, Hamsten A, Efendic S, Ryden L, Malmberg K. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet. 2002;359:2140–2144. doi: 10.1016/S0140-6736(02)09089-X. [DOI] [PubMed] [Google Scholar]
- 7.Timmer JR, Hoekstra M, Nijsten MW, van der Horst IC, Ottervanger JP, Slingerland RJ, Dambrink JH, Bilo HJ, Zijlstra F, van 't Hof AW. Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation. 2011;124:704–711. doi: 10.1161/CIRCULATIONAHA.110.985911. [DOI] [PubMed] [Google Scholar]
- 8.James S, Angiolillo DJ, Cornel JH, Erlinge D, Husted S, Kontny F, Maya J, Nicolau JC, Spinar J, Storey RF, Stevens SR, Wallentin L, Plato Study Group Ticagrelor vs. clopidogrel in patients with acute coronary syndromes and diabetes: a substudy from the PLATelet inhibition and patient Outcomes (PLATO) trial. Eur Heart J. 2010;31:3006–3016. doi: 10.1093/eurheartj/ehq325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sinnaeve PR, Steg PG, Fox KA, Van de Werf F, Montalescot G, Granger CB, Knobel E, Anderson FA, Dabbous OH, Avezum A, Grace I. Association of elevated fasting glucose with increased short-term and 6-month mortality in ST-segment elevation and non-ST-segment elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Arch Intern Med. 2009;169:402–409. doi: 10.1001/archinternmed.2008.572. [DOI] [PubMed] [Google Scholar]
- 10.Farhan S, Clare RM, Jarai R, Giugliano RP, Lokhnygina Y, Harrington RA, Kristin Newby L, Huber K. Fasting glucose, NT-proBNP, treatment with eptifibatide, and outcomes in non-ST-segment elevation acute coronary syndromes: an analysis from EARLY ACS. Int J Cardiol. 2017;232:264–270. doi: 10.1016/j.ijcard.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 11.James S, Akerblom A, Cannon CP, Emanuelsson H, Husted S, Katus H, Skene A, Steg PG, Storey RF, Harrington R, Becker R, Wallentin L. Comparison of ticagrelor, the first reversible oral P2Y(12) receptor antagonist, with clopidogrel in patients with acute coronary syndromes: rationale, design, and baseline characteristics of the PLATelet inhibition and patient Outcomes (PLATO) trial. Am Heart J. 2009;157:599–605. doi: 10.1016/j.ahj.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington RA, Plato I, Freij A, Thorsen M. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen Kristian, Alpert Joseph S., Jaffe Allan S., Simoons Maarten L., Chaitman Bernard R., White Harvey D., Thygesen Kristian, Alpert Joseph S., White Harvey D., Jaffe Allan S., Katus Hugo A., Apple Fred S., Lindahl Bertil, Morrow David A., Chaitman Bernard R., Clemmensen Peter M., Johanson Per, Hod Hanoch, Underwood Richard, Bax Jeroen J., Bonow Robert O., Pinto Fausto, Gibbons Raymond J., Fox Keith A., Atar Dan, Newby L. Kristin, Galvani Marcello, Hamm Christian W., Uretsky Barry F., Gabriel Steg Ph., Wijns William, Bassand Jean-Pierre, Menasché Phillippe, Ravkilde Jan, Ohman E. Magnus, Antman Elliott M., Wallentin Lars C., Armstrong Paul W., Simoons Maarten L., Januzzi James L., Nieminen Markku S., Gheorghiade Mihai, Filippatos Gerasimos, Luepker Russell V., Fortmann Stephen P., Rosamond Wayne D., Levy Dan, Wood David, Smith Sidney C., Hu Dayi, Lopez-Sendon José-Luis, Robertson Rose Marie, Weaver Douglas, Tendera Michal, Bove Alfred A., Parkhomenko Alexander N., Vasilieva Elena J., Mendis Shanti, Bax Jeroen J., Baumgartner Helmut, Ceconi Claudio, Dean Veronica, Deaton Christi, Fagard Robert, Funck-Brentano Christian, Hasdai David, Hoes Arno, Kirchhof Paulus, Knuuti Juhani, Kolh Philippe, McDonagh Theresa, Moulin Cyril, Popescu Bogdan A., Reiner Željko, Sechtem Udo, Sirnes Per Anton, Tendera Michal, Torbicki Adam, Vahanian Alec, Windecker Stephan, Morais Joao, Aguiar Carlos, Almahmeed Wael, Arnar David O., Barili Fabio, Bloch Kenneth D., Bolger Ann F., Bøtker Hans Erik, Bozkurt Biykem, Bugiardini Raffaele, Cannon Christopher, de Lemos James, Eberli Franz R., Escobar Edgardo, Hlatky Mark, James Stefan, Kern Karl B., Moliterno David J., Mueller Christian, Neskovic Aleksandar N., Pieske Burkert Mathias, Schulman Steven P., Storey Robert F., Taubert Kathryn A., Vranckx Pascal, Wagner Daniel R. Third universal definition of myocardial infarction. European Heart Journal. 2012;33(20):2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 14.Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S, ESC Scientific Document Group 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]