Abstract
Antimicrobial stewardship (AMS) and Infection prevention and control (IPC) are two key complementary strategies that combat development and spread of antimicrobial resistance. The ESGAP (ESCMID Study Group for AMS), EUCIC (European Committee on Infection Control) and TAE (Trainee Association of ESCMID) investigated how AMS and IPC activities and training are organized, if present, at national level in Europe. From February 2018 to May 2018, an internet-based cross-sectional survey was conducted through a 36-item questionnaire, involving up to three selected respondents per country, from 38 European countries in total (including Israel), belonging to the ESGAP/EUCIC/TAE networks. All 38 countries participated with at least one respondent, and a total of 81 respondents. Education and involvement in AMS programmes were mandatory during the postgraduate training of clinical microbiology and infectious diseases specialists in up to one-third of countries. IPC was acknowledged as a specialty in 32% of countries. Only 32% of countries had both guidance and national requirements regarding AMS programmes, in contrast to 61% for IPC. Formal national staffing standards for AMS and IPC hospital-based activities were present in 24% and 63% of countries, respectively. The backgrounds of professionals responsible for AMS and IPC programmes varied tremendously between countries. The organization and training of AMS and IPC in Europe are heterogeneous and national requirements for activities are frequently lacking.
Electronic supplementary material
The online version of this article (10.1007/s10096-019-03648-2) contains supplementary material, which is available to authorized users.
Keywords: Antimicrobial stewardship, Infection prevention and control, Clinical microbiology, Infectious diseases, Questionnaire
Introduction
The epidemiology of antimicrobial resistance (AMR) presents a heterogeneous pattern worldwide [1]. This is the result of a complex interaction of factors, some of them beyond the reach of healthcare professionals such as antimicrobial use in agriculture [2]. The heterogeneous implementation of antimicrobial stewardship (AMS) and infection prevention and control (IPC) programmes in different countries also contributes to this variation [3–6]. However, little is known regarding the differences in organization and training of AMS and IPC activities between countries.
The purpose of this survey was to provide an overview of how AMS and IPC are integrated in the postgraduate training of ID and CM specialists and how hospital-based AMS and IPC activities are organized at national levels in European countries.
Methods
Setting and participants
The European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Study Group for Antimicrobial StewardshiP (ESGAP), the European Committee on Infection Control (EUCIC) and the Trainee Association of ESCMID (TAE) performed a cross-sectional survey in Europe and Israel.
The 36-item online questionnaire (online_supplementary_file_1) was web-based, using SurveyMonkey® software (Palo Alto, CA, USA). Three representatives from each of the 38 countries, i.e. one respondent representing each group (ESGAP, EUCIC and TAE), were selected based on their expertise and experience in AMS and IPC activities. To have a comprehensive snapshot of activities at national level, we asked the respondents to be as representative as possible of what was occurring nationwide in their working country, even by asking other colleagues for help to answer specific questions if needed.
Participation was voluntary without any financial compensation. The purpose of the survey was clearly stated to participants before the survey started. Ethics approval was not necessary according to current regulations.
Survey design and data analysis
The questionnaire was divided in three parts. The first addressed general topics such as the way CM, ID and IPC are organized as specialties and represented at national level through official societies or even through informal organizations when it comes to trainee associations. The second and third parts were focused on AMS and IPC hospital-based activities, respectively. The respondents were encouraged to add comments and further details (e.g. weblinks or references of official documents) for each question. Although the total number of items was 36, the true number of questions to be answered could be lower, because of some filter questions.
The questionnaire was open between 18 March and 31 May 2018. The representatives from each country were contacted through e-mail by a member of ESGAP, EUCIC or TAE, providing the weblink of the survey. Periodic reminders were sent in order reach the best possible response rate.
Once the survey was closed, data completeness and consistency were checked, comparing the replies of the different respondents from the same country. Subsequently, if necessary, respondents were contacted again to solve discrepancies by majority consensus or to clarify unclear replies. If available, the investigators also double checked the official documents provided by the national representatives.
Results and discussion
Participants, national societies and trainee associations
The overall response rate was 81/114 (71%) (eTable 1). In 18 (47%) countries, the survey was filled in by three respondents (one from each group ESGAP/EUCIC/TAE), in 7 (18%) countries, there were two respondents, and one respondent replied in 13 (34%) countries.
A national professional CM and ID society was only present in 23 (61%) and 31 (82%) countries, respectively (eTables 2 and 3). In 5 (13%) countries, CM/ID were officially represented by a joint society. Official IPC and CP societies were both present in 21 (55%) countries.
A formal association of trainees was present in 10 (26%), 12 (32%), 4 (11%), and 7 (18%) countries for CM, ID, IPC and CP, respectively.
Organization and training requirements
The organization of CM, ID and IPC specialties and AMS/IPC postgraduate training was very heterogeneous (eTable 4). CM and ID were separated disciplines in 34 (89%) countries, but in two countries offered as dual training. In 26 (68%) countries, CM was a stand-alone specialty, whereas in 10 (26%), it was a sub-specialty of another discipline (mostly laboratory medicine). CM was mostly open to medical doctors only, but in some countries open to biologists and pharmacists. When ID was a subspecialty, it was generally in the framework of internal medicine. It is worrisome that in some countries, CM and ID were not recognized as specialty.
IPC was a stand-alone specialty in 7 (18%) countries and a subspecialty in 5 (13%) countries. Although in 3 countries, it was not framed as an official specialty, medical doctors could get a specific IPC qualification. In 26 (68%) countries, nurses had the possibility to obtain an IPC qualification after formal training.
Heterogenous findings and a quite variable duration of postgraduate training complicate the path to full recognition and accreditation of CM and ID professions in Europe [7]. The situation regarding IPC is even more fragmented. These results argue for an acceleration of the implementation of a standardized core curriculum for trainees in Europe [8, 9], thereby closing the current gaps among countries and harmonizing the quality of training [10, 11]. Furthermore, standardizing IPC training to become an IPC practitioner is likewise needed [7, 12, 13].
AMS and IPC activities in hospitals
In half of the countries, AMS and IPC programmes were under the same hospital department, clinical leader or team (eTable 5). Routine interactions and collaborations between AMS and IPC professionals were seen in 28 (74%) of cases. The aim should be a daily and structured cooperation for a coordinated approach to tackle AMR [14].
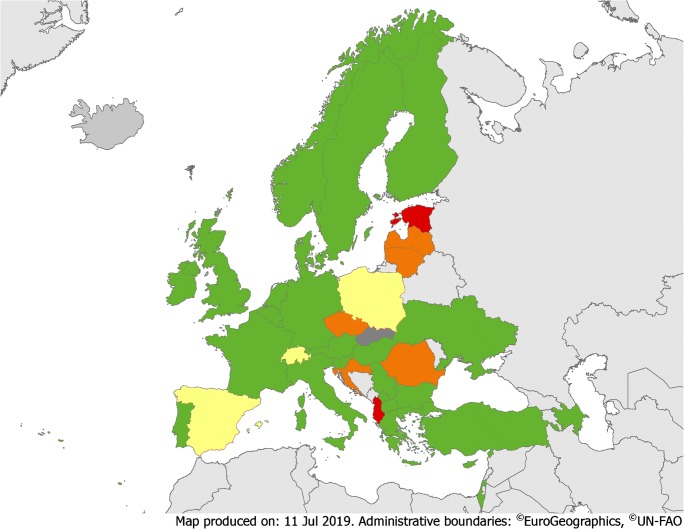
In 12 (32%) countries, there were guidance and national requirements on the implementation of AMS programmes; in 16 (42%), there was only general guidance (Fig. 1, eTable 6). These numbers are in line with a recently published survey [15], and different from IPC, where guidance and national requirements existed in nearly two-thirds of countries [16].
Fig. 1.
Overview of guidance or requirements on AMS and IPC implementation. Green = guidance or requirements on both AMS and IPC implementation. Yellow = guidance or requirements on AMS (but not on IPC implementation). Orange = guidance or requirements on IPC (but not on AMS implementation). Red = no guidance or requirements on AMS and IPC implementation. Dark grey = no data available
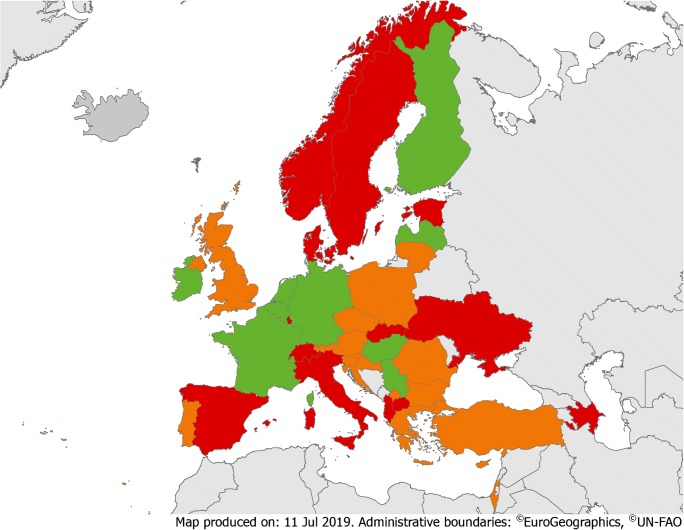
Formal national staffing standards (i.e. number of professionals per number of acute care beds) for AMS hospital-based activities existed in 9 (24%) countries (Fig. 2), which is in accordance with a previous survey [17]. Having staffing standards and proper funding to support AMS activities is crucial and has been included in global AMS core elements [14]. However, only 3 (8%) countries had official national requirements concerning formal training to become qualified as an AMS team member (eTable 7).
Fig. 2.
Overview of national staffing standards for AMS and IPC teams. Green = staffing standards for both AMS and IPC teams. Orange = staffing standards for IPC teams (but not for AMS teams). Red = no staffing standard for AMS and IPC teams
Guidance and national requirements on how to implement an IPC programme were present in 23 (61%) countries, and 24 (63%) had national staffing standards for IPC hospital-based activities (Figs. 1 and 2, eTable 8, eTable 9). A recent review recommended at least one FTE nurse per up to 250 beds and a dedicated physician [18]. Only 13 (34%) countries had national requirements regarding postgraduate training to become an IPC team member.
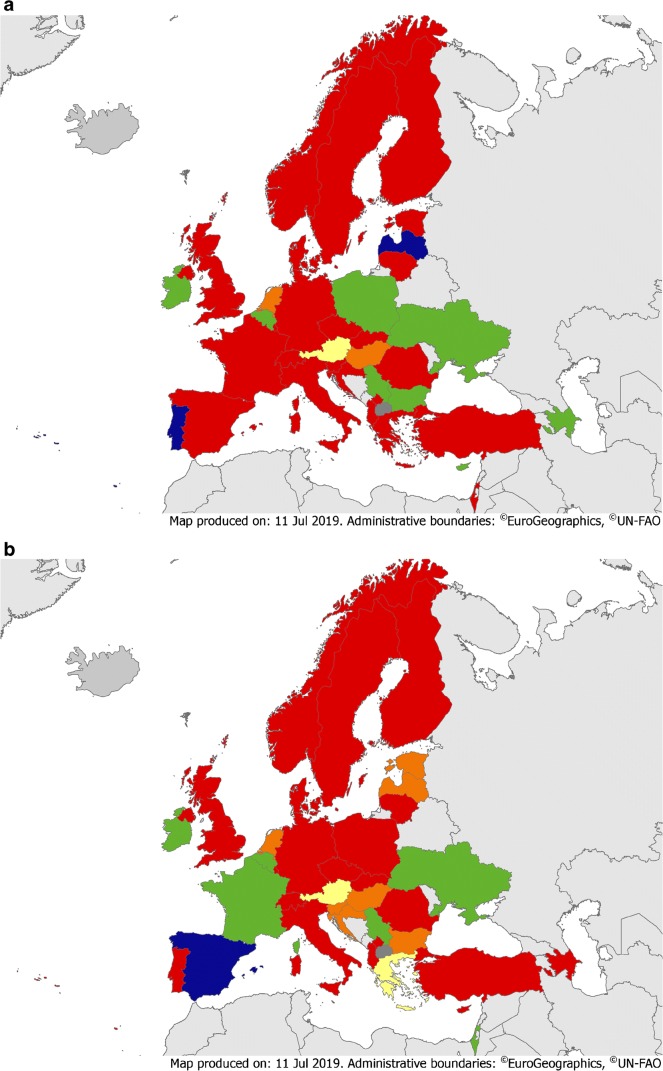
Education during postgraduate training
Mandatory formal training on how to implement an AMS programme was reported in 9/36 (25%), 8/37 (22%) and 5/15 (33%) countries for CM, ID and IPC specialties, respectively (Fig. 3a, b, eTable 10). The proportion of mandatory involvement in AMS activities during postgraduate training was 11/36 (31%), 13/37 (35%) and 6/15 (40%), respectively. Official training requirements to become an AMS team member were lacking in most countries, even though appropriate training is part of recently validated and globally relevant core elements [14]. Ideally, basic training in generic competencies for all prescribers regarding antibiotic use and stewardship should be delivered to all healthcare professionals [19].
Fig. 3.
a Educational requirements on AMS for CM trainees. Green = mandatory formal training on AMS implementation and involvement in AMS activity during training. Yellow = mandatory formal training on AMS implementation (but no involvement in AMS activity during training). Orange = mandatory involvement in AMS activity during training (but no formal training on AMS implementation). Red = no mandatory formal training on AMS implementation or involvement in AMS activity during training. Blue = not applicable. Dark grey = no data available. b Educational requirements on AMS for ID trainees. Green = mandatory formal training on AMS implementation and involvement in AMS activity during training. Yellow = mandatory formal training on AMS implementation (but no involvement in AMS activity during training). Orange = mandatory involvement in AMS activity during training (but no formal training on AMS implementation). Red = no mandatory formal training on AMS implementation or involvement in AMS activity during training. Blue = not applicable. Dark grey = no data available
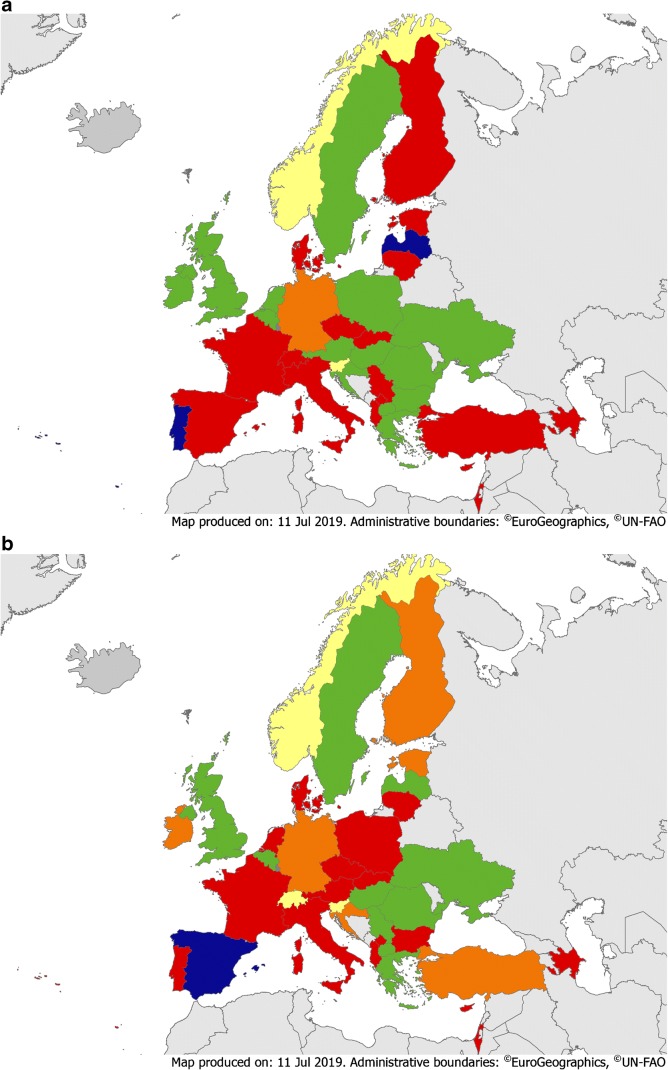
Mandatory official training on IPC implementation was reported in 16/36 (44%), 13/37 (35%) and 10/15 (67%) countries for CM, ID and IPC specialties, respectively (Fig. 4a, b, eTable 10). Furthermore, involvement in IPC activities during training for CM, ID and IPC was mandatory in 16/36 (44%), 16/37 (43%) and 13/15 (87%) countries, respectively. These low numbers are possibly linked to the lack of official acknowledgment of core competencies for IPC activities at national level [20], despite the availability of a well-defined set of requirements for European professionals [21].
Fig. 4.
a Educational requirements on IPC for CM trainees. Green = mandatory formal training on IPC implementation and involvement in IPC activity during training. Yellow = mandatory formal training on IPC implementation (but no involvement in IPC activity during training) = Yellow Orange = mandatory involvement in IPC activity during training (but no formal training on IPC implementation). Red = no mandatory formal training on IPC implementation or involvement in IPC activity during training. Blue = not applicable. Dark grey = no data available. b Educational requirements on IPC for CM trainees. Green = mandatory formal training on IPC implementation and involvement in IPC activity during training. Yellow = mandatory formal training on IPC implementation (but no involvement in IPC activity during training) = Yellow Orange = mandatory involvement in IPC activity during training (but no formal training on IPC implementation). Red = no mandatory formal training on IPC implementation or involvement in IPC activity during training. Blue = not applicable. Dark grey = no data available
Professionals responsible for conducting AMS and IPC activities
CM specialists were involved in 24/36 (67%) and 22/37 (59%) countries with regard to AMS and IPC daily hospital-based activities, respectively (eTables 11 and 12). ID specialists were involved in 30/37 (81%) and 24/37 (65%) countries for AMS and IPC, respectively. CP were involved in AMS programmes in 25/38 (66%) countries and in IPC activities in 4/38 (11%). Lastly, nurses were involved in AMS and IPC activities in 8/38 (21%) and 32/38 (84%) countries, respectively.
Limitations of the study
This study has limitations. First, only up to three representatives were consulted for each country and, in some instances, responses came from just one or two participants. Although participants were asked to provide reference documents to corroborate their answers, this information was not always available. Second, healthcare is organized at regional level in some countries, and the national situation reported here might not always reflect specific regional areas.
Conclusion
This survey demonstrates substantial heterogeneity and large room for improvement in AMS and IPC activities in European countries, both from an educational and an organizational perspective. Standardization and constant improvement of these activities is imperative in the light of the recent and alarming data regarding attributable deaths and disability related to AMR in Europe [22].
Electronic supplementary material
(PDF 273 kb)
(PDF 665 kb)
Acknowledgements
The ESGAP-EUCIC-TAE Working Group on AMS/IPC in Europe also included the following investigators/collaborators from the following countries:
Albania (Arjan Harxhi); Austria (Elisabeth Presterl, Iris Zeller, Agnes Wechsler-Fördös); Azerbaijan (Akif Gurbanov); Belgium (Stien Vandendriessche, Hilde Jansens, Tomi Kostyanev); Bulgaria (Rossitza Vatcheva-Dobrevska); Croatia (Maja Sabolić, Rok Civljak, Vera Vlahovic-Palcevski); Czech Republic (Milan Trojanek); Cyprus (Maria Yiannitsarou, Constantinos Tsioutis); Denmark (Kristina Obrink-Hansen, Bente Olesen); Estonia (Karmen Jaaniso); Finland (Mari Ala-Houhala); France (Vincent Jarlier, Alexandre Bleibtreu); Germany (Thea-Christin Zapf, Winfred V. Kern, Frauke Mattner); Greece (Kyriakos Zaragkoulias, Athanassios Tsakris); Hungary (Edit Hajdú, Gyula Prinz, Szabo Balint Gergely), Ireland (Aaron Doherty, Kirsten Schaffer, Aoife Fleming); Israel (Khetam Hussein); Italy (Elena Carrara, Leonardo Pagani, Daniele Roberto Giacobbe); Kosovo (Albina Ponosheci-Bicaku, Lul Raka, Shaip Krasniqi); Latvia (Alise Grāmatniece, Uga Dumpis); Lithuania (Rolanda Valinteliene, Tomas Kacergius); Luxembourg (Viviane Knepper); Malta (Peter Zarb); The Netherlands (Gertjan Wagenvoort, Andreas Voss); Norway (Per Espen Akselsen, Dag Berild); Poland (Joanna Kubiak, Aleksander Deptuła, Monika Wanke-Rytt); Portugal (Filipa Sofia de Sousa Fernandes, Nuno Rocha-Pereira, Carlos Palos); Republic of Northern Macedonia (Neda Milevska Kostova); Romania (Diana Gabriela Iacob, Oana Sandulescu, Roxana Filip); Serbia (Aleksandra Barac); Slovakia (Vladimír Krčméry); Slovenia (Maja Plesko, Tatjana Lejko Zupanc, Bojana Beović); Spain (José Ramón Paño Pardo, Juan Pablo Horcajada, Zaira Palacios Baena); Sweden (Thomas Tängdén, Anders Johansson, Caroline Rönnberg); Switzerland (Benedikt Huttner, Walter Zingg); Turkey (Murat Akova, Önder Ergönül); United Kingdom (Alison Holmes, Muge Cevik); Ukraine (Aidyn Salmanov).
Authors’ contribution
CP initiated the study. AEM, DSYO, CC, NTM and CP wrote the first draft of the protocol, that was reviewed by all co-authors. DSYO, NTM and CP contacted the national representatives. AEM, DSYO and CC analysed the data. AEM and DSYO wrote the first draft of the manuscript, which was first reviewed by CP, and then by all co-authors.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alberto Enrico Maraolo and David S. Y. Ong contributed equally to this work.
Contributor Information
David S. Y. Ong, Email: davidsyong@gmail.com
on behalf of the ESGAP-EUCIC-TAE Working Group on AMS/IPC mapping in Europe:
Arjan Harxhi, Elisabeth Presterl, Iris Zeller, Agnes Wechsler-Fördös, Akif Gurbanov, Stien Vandendriessche, Hilde Jansens, Tomi Kostyanev, Rossitza Vatcheva-Dobrevska, Maja Sabolić, Rok Civljak, Vera Vlahovic-Palcevski, Milan Trojanek, Maria Yiannitsarou, Constantinos Tsioutis, Kristina Obrink-Hansen, Bente Olesen, Karmen Jaaniso, Mari Ala-Houhala, Vincent Jarlier, Alexandre Bleibtreu, Thea-Christin Zapf, Winfred V. Kern, Frauke Mattner, Kyriakos Zaragkoulias, Athanassios Tsakris, Edit Hajdú, Gyula Prinz, Szabo Balint Gergely, Aaron Doherty, Kirsten Schaffer, Aoife Fleming, Khetam Hussein, Elena Carrara, Leonardo Pagani, Daniele Roberto Giacobbe, Albina Ponosheci-Bicaku, Lul Raka, Shaip Krasniqi, Alise Grāmatniece, Uga Dumpis, Rolanda Valinteliene, Tomas Kacergius, Viviane Knepper, Peter Zarb, Gertjan Wagenvoort, Andreas Voss, Per Espen Akselsen, Dag Berild, Joanna Kubiak, Aleksander Deptuła, Monika Wanke-Rytt, Filipa Sofia de Sousa Fernandes, Nuno Rocha-Pereira, Carlos Palos, Neda Milevska Kostova, Diana Gabriela Iacob, Oana Sandulescu, Roxana Filip, Aleksandra Barac, Vladimír Krčméry, Maja Plesko, Tatjana Lejko Zupanc, Bojana Beović, José Ramón Paño Pardo, Juan Pablo Horcajada, Zaira Palacios Baena, Thomas Tängdén, Anders Johansson, Caroline Rönnberg, Benedikt Huttner, Walter Zingg, Murat Akova, Önder Ergönül, Alison Holmes, Muge Cevik, and Aidyn Salmanov
References
- 1.Global antimicrobial resistance surveillance system (GLASS) report: early implementation 2016-2017 (2017). Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO
- 2.Watkins RR, Bonomo RA. Overview: global and local impact of antibiotic resistance. Infect Dis Clin N Am. 2016;30:313–322. doi: 10.1016/j.idc.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Howard P, Pulcini C, Levy Hara G, West RM, Gould IM, Harbarth S, et al. An international cross-sectional survey of antimicrobial stewardship programmes in hospitals. J Antimicrob Chemother. 2015;70:1245–1255. doi: 10.1093/jac/dku497. [DOI] [PubMed] [Google Scholar]
- 4.van Woezik AF, Braakman-Jansen LM, Kulyk O, Siemons L, van Gemert-Pijnen JE. Tackling wicked problems in infection prevention and control: a guideline for co-creation with stakeholders. Antimicrob Resist Infect Control. 2016;5:20. doi: 10.1186/s13756-016-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Read RC, Cornaglia G, Kahlmeter G. Professional challenges and opportunities in clinical microbiology and infectious diseases in Europe. Lancet Infect Dis. 2011;11:408–415. doi: 10.1016/S1473-3099(10)70294-2. [DOI] [PubMed] [Google Scholar]
- 6.Tacconelli E, Buhl M, Humphreys H, Malek V, Presterl E, Rodriguez-Baño J, et al. Analysis of the challenges in implementing guidelines to prevent the spread of multidrug-resistant gram-negatives in Europe. BMJ Open. 2019;9:e027683. doi: 10.1136/bmjopen-2018-027683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brusaferro S, Cookson B, Kalenic S, Cooper T, Fabry J, Gallagher R et al (2014) Training infection control and hospital hygiene professionals in Europe, 2010: agreed core competencies among 33 European countries. Euro Surveill 19 [DOI] [PubMed]
- 8.McKendrick MW. The European Union of Medical Specialties core training curriculum in infectious diseases: overview of national systems and distribution of specialists. Clin Microbiol Infect. 2005;11:28–32. doi: 10.1111/j.1469-0691.2005.01087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Humphreys H, Nagy E, Kahlmeter G, Ruijs GJ. The need for European professional standards and the challenges facing clinical microbiology. Eur J Clin Microbiol Infect Dis. 2010;29:617–621. doi: 10.1007/s10096-010-0906-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yusuf E, Ong DS, Martin-Quiros A, Skevaki C, Cortez J, Dedić K, et al. A large survey among European trainees in clinical microbiology and infectious disease on training systems and training adequacy: identifying the gaps and suggesting improvements. Eur J Clin Microbiol Infect Dis. 2017;36:233–242. doi: 10.1007/s10096-016-2791-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palacios-Baena ZR, Zapf TC, Ong DSY, Maraolo AE, Rönnberg C, Çimen C, et al. How are trainees in clinical microbiology and infectious diseases supervised in Europe? An international cross-sectional questionnaire survey by the Trainee Association of ESCMID. Eur J Clin Microbiol Infect Dis. 2018;37:2381–2387. doi: 10.1007/s10096-018-3386-4. [DOI] [PubMed] [Google Scholar]
- 12.Zingg W, Mutters NT, Harbarth S, Friedrich AW. Education in infection control: a need for European certification. Clin Microbiol Infect. 2015;21:1052–1056. doi: 10.1016/j.cmi.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 13.EUCIC Infection Prevention and Control Certificate. Available on: https://www.escmid.org/research_projects/eucic/training_programme/. Accessed 11 May 2019
- 14.Pulcini C, Binda F, Lamkang AS, Trett A, Charani E, Goff DA, et al. Developing core elements and checklist items for global hospital antimicrobial stewardship programmes: a consensus approach. Clin Microbiol Infect. 2019;25:20–25. doi: 10.1016/j.cmi.2018.03.033. [DOI] [PubMed] [Google Scholar]
- 15.Beović B, Pulcini C, Dumartin C, Béraud G, Nerat B, Maurel C, et al. Legal framework of antimicrobial stewardship in hospitals (LEASH): a European Society of Clinical Microbiology and Infectious Diseases (ESCMID) cross-sectional international survey. Int J Antimicrob Agents. 2018;52:616–621. doi: 10.1016/j.ijantimicag.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Mutters NT, Tacconelli E. Infection prevention and control in Europe - the picture in the mosaic. Clin Microbiol Infect. 2015;21:1045–1046. doi: 10.1016/j.cmi.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 17.Dickstein Y, Nir-Paz R, Pulcini C, Cookson B, Beović B, Tacconelli E, et al. Staffing for infectious diseases, clinical microbiology and infection control in hospitals in 2015: results of an ESCMID member survey. Clin Microbiol Infect. 2016;22:812.e9–812.e17. doi: 10.1016/j.cmi.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015;15:212–224. doi: 10.1016/S1473-3099(14)70854-0. [DOI] [PubMed] [Google Scholar]
- 19.Dyar OJ, Beović B, Pulcini C, Tacconelli E, Hulscher M, Cookson B. ESCMID generic competencies in antimicrobial prescribing and stewardship: towards a European consensus. Clin Microbiol Infect. 2019;25:13–19. doi: 10.1016/j.cmi.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Rodríguez-Baño J, del Toro MD, López-Méndez J, Mutters NT, Pascual A. Minimum requirements in infection control. Clin Microbiol Infect. 2015;21:1072–1076. doi: 10.1016/j.cmi.2015.08.025. [DOI] [PubMed] [Google Scholar]
- 21.European Centre for Disease Prevention and Control . Core competencies for infection control and hospital hygiene professionals in the European Union. Stockholm: ECDC; 2013. [Google Scholar]
- 22.Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European economic area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 273 kb)
(PDF 665 kb)