Abstract
Objective:
To determine all-cause mortality risk in patients with and without adrenal incidentaloma.
Methods:
Retrospective cohort study of patients with CT abdomen performed within 24 hours of emergency room presentation at an academic medical center from January 1, 2005 to December 31, 2009, without history of adrenal disease, adrenal lab testing, or cancer. Incidentaloma cohort identified by database query of imaging reports followed by manual review and matched to no-nodule controls at 3:1 on age ±1 year and exam date ±3 months. Mortality ascertained by in-hospital deaths and National Death Index query. Survival analysis performed with Kaplan-Meier curves and Cox proportional hazards models.
Results:
Among 42575 adults with abdominal CT exams, 969 adrenal incidentaloma patients and 2907 no-nodule controls were identified. All 3876 individuals entered survival analysis with 31182 person-years at risk (median follow-up 8.9 years [IQR, 6.9–10.7]). All-cause mortality was significantly higher among those with adrenal incidentalomas (353/969, 36.4%) compared to those without (919/2907, 31.6%; mortality difference 7.6 per 1000 person-years; multivariable-adjusted hazard ratio [aHR] 1.14; 95% CI, 1.003–1.29). Exploratory analyses, limited by missing covariates, found that adrenal incidentalomas were associated with significantly increased incidence of malignancy (aHR 1.61; 95% CI, 1.22–2.12), diabetes (aHR 1.43; 95% CI, 1.18–1.71), heart failure (aHR 1.32; 95% CI, 1.07–1.63), peripheral vascular disease (aHR 1.28; 95% CI, 1.95–1.56), renal disease (aHR 1.21; 95% CI, 1.01–1.44), and chronic pulmonary disease (aHR 1.22; 95% CI, 1.01–1.46) compared to controls.
Conclusions:
Adrenal incidentalomas are associated with increased mortality and may represent a clinically valuable biomarker.
Keywords: adrenal gland neoplasms; incidental findings; cohort study; survival analysis; tomography, x-ray computed
Introduction
Adrenal incidentaloma are defined as adrenal masses ≥10 mm “discovered inadvertently during diagnostic testing or treatment for other clinical conditions that are not related to suspicion of adrenal disease,” and exclude patients undergoing staging and work-up for cancer [1; 2]. Also called adrenal nodule or tumor, the radiologic prevalence of adrenal incidentalomas on CT has been reported at 4.2% and 5% [3; 4].
The American College of Radiology (ACR) Incidental Findings Committee published updated management recommendations for the incidentally discovered adrenal mass in August 2017 with one notable change from 2010 [5; 6]: consideration of routine biochemical evaluation for most incidentally discovered adrenal masses, bringing the recommendations more in line with the European Society of Endocrinology, American Association of Clinical Endocrinologists (AACE) and the American Association of Endocrine Surgeons (AAES) [7; 8], who recommend biochemical workup for all masses to exclude treatable adrenal disease. Degree of radiologic and endocrinologic follow-up for benign adrenal masses remains an area of controversy on the basis of conflicting literature on potential harms [9–11]. Evidence favoring routine diagnostic workup comes from endocrinologic studies reporting an increased risk of cardiovascular events and death comparing cortisol-secreting functional adrenal tumors to nonfunctional adrenal tumors [12–15]. Lopez and colleagues observed increased risk of composite diabetes amongst individuals with even nonfunctional adrenal tumors compared to matched controls without an adrenal tumor [16].
However, the results of these highly selected endocrinologic studies are difficult to generalize as most patients with incidentally discovered adrenal nodules are not biochemically characterized with few referred to specialists. A review of routine practice by primary care physicians found that only 18.4% of patients with an incidentally discovered adrenal nodule underwent a complete initial hormonal evaluation in line with AACE/AAES guidelines [17]. There is at present no longitudinal cohort study investigating the association between adrenal nodules and overall mortality in a population of patients identified at the moment of initial radiologic reporting prior to specialist referral and irrespective of hormonal phenotype. The goal of this study was to determine the risk of all-cause mortality in a cohort of patients with incidental adrenal nodules compared to a no-nodule cohort.
Materials and Methods
This retrospective cohort study at a multicenter academic medical center included patients with newly detected adrenal incidentaloma on CT abdomen report and a group without adrenal nodules. The primary prespecified outcome was all-cause mortality with exploratory outcomes of malignancy and other chronic illnesses. Institutional review board granted approval for and waived the informed consent requirement. The study was compliant with Health Insurance Portability and Accountability Act regulations. Study protocol not previously reported.
Study Population and Cohort Identification
The enterprise data warehouse was queried using Looking Glass™ Clinical Analytics (Streamline Health) [18–20] to identify patients ≥18 with abdominal CT examinations performed within 24 hours of presentation to the emergency room from January 1, 2005 to December 31, 2009. To ensure that any forthcoming adrenal incidentaloma finding would be a “surprise” to the referring physician, patients with a history of adrenal disease (International Classification of Diseases, Ninth Revision [ICD-9] codes 194.0, 198.7, 227.0, 237.2, and 255.xx), adrenal lab testing (cortisol, catecholamines, aldosterone, renin, adrenocorticotropic hormone), or cancer (non-superficial skin cancer according to cancer registry) were excluded.
A cohort of potential adrenal incidentalomas was identified by imaging reports containing in the same sentence “adrenal” and “nodule,” “adenoma,” or “mass” and excluding those with “no” and “adrenal” in the same sentence. The imaging reports of all potential adrenal nodule patients were manually reviewed by the primary author (M.T.) for confirmation of nodule presence and further exclusions, including no description of incidentaloma, incidentaloma size uncharacterized or <1 cm, history of cancer described or unequivocal evidence of metastatic disease, or reference made to prior abdominal cross-sectional imaging. This last exclusion was made so that only incident cases of adrenal incidentaloma were under investigation, limiting survivorship bias. Subcentimeter nodules are excluded from ACR guidelines as they may overrepresent adrenal thickening [6]. The number, location, and largest dimension of adrenal incidentaloma were recorded for every individual.
A cohort of potential no adrenal incidentaloma imaging reports were randomly sampled from the remaining risk set with frequency matching on age ±1 year and exam date ±3 months to the manually-confirmed adrenal incidentaloma cohort at a three to one ratio. Imaging reports of the potential no-nodule cohort were similarly manually reviewed by the primary author for confirmation and exclusion of any described adrenal abnormality, followed by serial re-sampling and review until complete 3:1 matching was achieved.
Covariates
Looking Glass™ was used to extract the following baseline data from the electronic medical record: demographics, CT study type, insurance type, emergency room disposition, and 14 prevalent comorbidities adapted from the Charlson index: diabetes mellitus, chronic pulmonary disease, congestive heart failure, cerebrovascular disease, myocardial infarction, peripheral vascular disease, renal disease, liver disease, peptic ulcer disease, malignancy/metastasis, dementia, rheumatic disease, hemiplegia or paraplegia, and acquired immunodeficiency syndrome/human immunodeficiency virus [21]. Comorbidities were defined by documented diagnoses according to ICD-9 or 10 codes [22].
Outcomes Ascertainment
All-cause mortality, the prespecified primary outcome, was ascertained primarily by deaths recorded within the hospital system. Deaths unknown to the hospital were ascertained by vital status query to the National Death Index (NDI), a national database maintained by the Centers for Disease Control with complete death records through December 31, 2016. Individuals submitted for NDI vital status query without matching death certificates were presumed alive and censored at December 31, 2016 as vital status could not be verified thereafter. Individuals known to be alive were censored at the date of most recent clinical encounter until February 1, 2018, the study end date. Incident malignancy was ascertained by the cancer registry, from which date of cancer diagnosis, tumor location, and initial staging were recorded. All other incident secondary outcomes, adapted from the Charlson index and listed above, were ascertained by documented diagnoses [22]. Exploratory secondary outcomes assessment was restricted to patients with ≥2 years of clinical follow-up to allow for adequate documentation, with exclusion of prevalent disease and incident outcomes diagnosed within 6 months follow-up.
For the adrenal nodule cohort, additional outcomes within 12 months follow-up were extracted: adrenal incidentaloma documented diagnoses (ICD-9 codes 227.0, 237.2, 255.8, 255.9) and laboratory tests (serum cortisol following 1 mg dexamethasone administration, serum or urine catecholamines or metanephrines, plasma aldosterone and renin).
Statistical Analysis
Descriptive statistics were performed using Student’s t or Wilcoxon rank-sum test for continuous and Chi-square or Fisher’s exact test for categorical variables. Kaplan-Meier survival probabilities were compared using the log-rank test. Primary analyses evaluating the association between adrenal incidentaloma presence and development of incident outcomes was done using Cox proportional hazards regression with adjustment for all baseline covariates described above. Both full and parsimonious multivariable models were built. The proportional hazards assumption was assessed by testing time-dependent covariates and an extended Cox model was used where violations occurred. Statistical analysis was performed by the primary author using statistical software (Stata version 14.2; StataCorp). All statistical tests were two-tailed with an alpha of 0.05. Detailed methods for data and statistical analysis are presented in the Supplement.
Results
Study Population
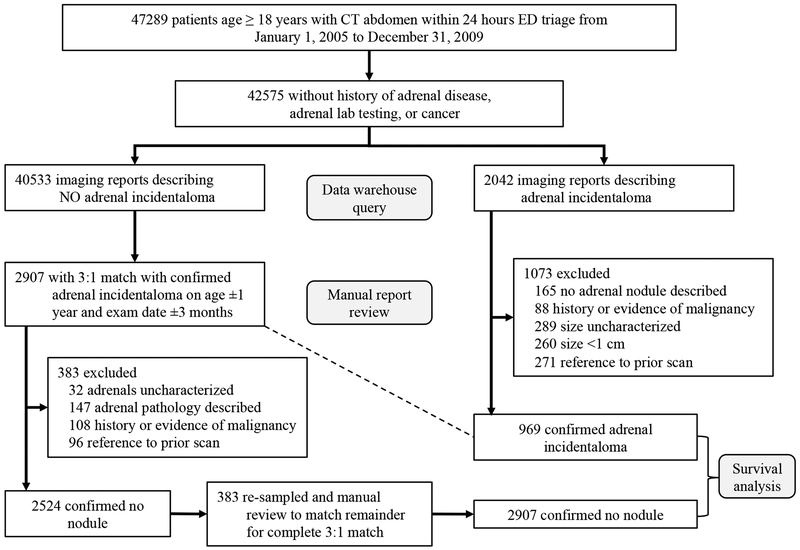
The initial query yielded 42575 patients with CT abdomen exams without a history of adrenal disease, adrenal lab testing, or cancer (Fig. 1). The population mean ± SD age was 50.2 ± 19.0 years with 63% women (n=26899). 969/42575 (2.3%) confirmed adrenal incidentaloma patients were identified and 3:1 matched to 2907 confirmed no-nodule patients on age and exam date. Table 1 shows baseline characteristics of the entire population, adrenal incidentaloma cohort, and no-nodule cohort. Adrenal incidentaloma patients were more often diabetic and white and black non-Hispanic compared to no-nodule patients.
Figure 1:
Study population, cohort identification and exclusion points.
Table 1:
Baseline characteristics of total population, adrenal incidentaloma, and no-nodule cohorts.
| Characteristics | Total Population (n = 42575) |
Adrenal Nodule Cohort (n = 969) |
No Nodule Cohorta (n = 2907) |
p valueb |
|---|---|---|---|---|
| Age (years) | 50.2 ± 19.0 | 61.6 ± 15.9 | 61.6 ± 15.9 | 0.96 |
| Female | 26899 (63) | 648 (67) | 1845 (64) | 0.06 |
| Race/Ethnicityc | < 0.001 | |||
| White non-Hispanic | 7283 (17) | 252 (26) | 563 (19) | |
| Black non-Hispanic | 12599 (30) | 315 (33) | 804 (28) | |
| Hispanic | 9988 (23) | 190 (20) | 788 (27) | |
| Other | 12705 (30) | 212 (22) | 752 (26) | |
| Comorbidities | ||||
| Diabetes | 6166 (14) | 215 (22) | 557 (19) | 0.04 |
| Chronic Pulmonary Disease | 8527 (20) | 189 (20) | 578 (20) | 0.80 |
| Congestive Heart Failure | 3212 (8) | 106 (11) | 262 (9) | 0.08 |
| Cerebrovascular Disease | 2264 (5) | 84 (9) | 210 (7) | 0.14 |
| Myocardial Infarction | 2209 (5) | 76 (8) | 210 (7) | 0.52 |
| Peripheral Vascular Disease | 1708 (4) | 58 (6) | 136 (5) | 0.11 |
| Renal Disease | 2067 (5) | 52 (5) | 155 (5) | 0.97 |
| Liver Disease | 1911 (4) | 30 (3) | 114 (4) | 0.24 |
| Peptic Ulcer Disease | 1041 (2) | 30 (3) | 87 (3) | 0.87 |
| Malignancy/Metastasisd | 1013 (2) | 26 (3) | 75 (3) | 0.86 |
| Dementia | 611 (1) | 19 (2) | 61 (2) | 0.79 |
| Rheumatic Disease | 684 (2) | 12 (1) | 46 (2) | 0.45 |
| Hemi/Paraplegia | 491 (1) | 12 (1) | 47 (2) | 0.41 |
| AIDS/HIV | 776 (2) | 11 (1) | 31 (1) | 0.86 |
| Emergency Room Disposition | 0.12 | |||
| Inpatient Admission | 18008 (42) | 500 (52) | 1416 (49) | |
| Dischargede | 24567 (58) | 469 (48) | 1491 (51) | |
| Insurance Type | 0.28 | |||
| Commercial | 17883 (42) | 310 (32) | 935 (32) | |
| Medicare | 14952 (35) | 266 (27) | 866 (30) | |
| Medicaid | 9740 (23) | 393 (41) | 1106 (38) | |
| CT Study Type | 0.63 | |||
| With IV contrast | 21878 (51) | 480 (50) | 1489 (51) | |
| Without contrast | 19696 (46) | 456 (47) | 1328 (46) | |
| With and without IV contrast | 1001 (2) | 33 (3) | 90 (3) |
AIDS acquired immunodeficiency syndrome, HIV human immunodeficiency virus. Data are mean ± SD or n (%).
3:1 match on age ±1 year and CT date ±3 months.
Calculated with t-test, Wilcoxon rank sum test, or chi-square test comparing adrenal nodule cohort to no nodule cohort.
Hispanic ethnicity may be any race. Other race includes declined and missing categories.
Cancer history as recorded in the cancer registry was an initial exclusion criteria for study entry. Persistent 3% cancer prevalence here is due to the use of ICD-9 codes for detection, which were not utilized prior. Prevalent cancer was rigorously excluded by manual review of all imaging reports mentioning cancer in the clinical history (Fig. 1). Therefore, residual documentation of cancer reflected here is unlikely to have influenced the radiologist at the time of image interpretation. Follow-up analyses on incident cancer excluded these residual prevalent cancer cases.
Discharged includes signed out against medical advice, eloped, expired, and to nursing home.
Survival
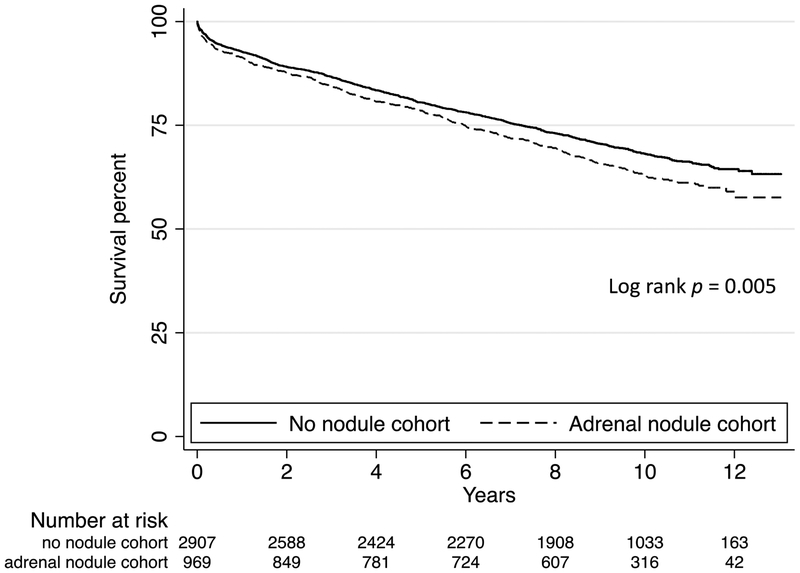
All 3876 patients from both cohorts entered survival analysis with 31182 total person-years at risk, median follow-up of 8.9 years (IQR, 6.9–10.7). Death was confirmed in 919/2907 (31.6%) no-nodule individuals and 353/969 (36.4%) adrenal incidentaloma individuals, with worse survival in the incidentaloma group (p = 0.005; Fig. 2). Adrenal incidentalomas were associated with an excess mortality risk of 7.6 deaths per 1000 person-years (95% CI, 2.1–13.0). In the unadjusted Cox proportional hazards model, adrenal incidentaloma presence was associated with significantly increased risk of death (hazard ratio [HR] 1.19; 95% CI, 1.05–1.36). In the parsimonious multivariable model (Supplemental Fig. 1), the association remained significant (adjusted HR [aHR] 1.14; 95% CI, 1.003–1.29).
Figure 2:
Kaplan-Meier survival curve for all-cause mortality by adrenal nodule presence.
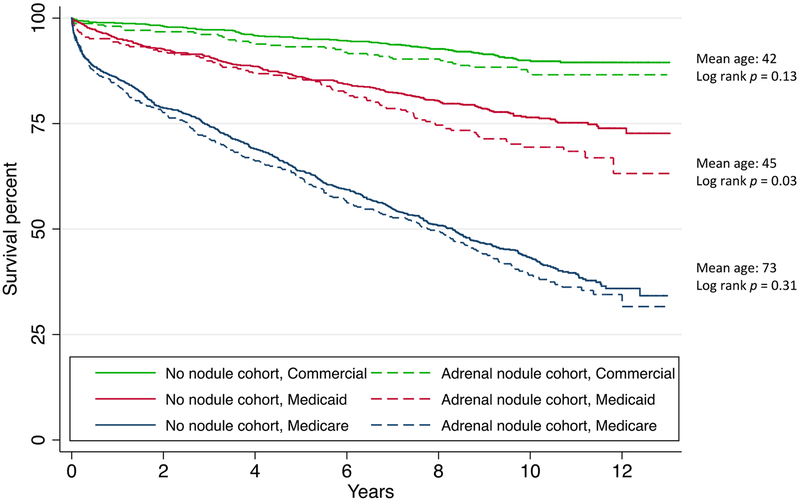
Testing for first order interactions revealed a significant effect modification of insurance type on mortality, with adrenal nodules in the Medicaid subgroup having the highest risk of death (aHR 1.57; 95% CI, 1.21–2.04) compared to non-significant risk in the Medicare (aHR 1.02; 95% CI, 0.87–1.18) and commercial (aHR 1.24; 95% CI, 0.84–1.81) insurance subgroups, respectively, shown with Kaplan-Meier curves in Figure 3.
Figure 3:
Kaplan-Meier survival curve by adrenal nodule presence and insurance type. Mean age labeled to highlight differences in insurance qualification by age that account for survival discrepancies between groups; Medicare generally includes Americans age ≥65 whereas Medicaid and Commercial insurance have no such age limitation.
310/1272 (24%) of recorded deaths were ascertained through the National Death Index and contained cause-specific mortality data (Supplemental Table 1). Deaths in the adrenal nodule cohort had a higher proportion of cardiovascular mortality (32/86 [37%] vs 76/224 [34%]), although there was no significant association between adrenal nodule presence and underlying cause of death (p = 0.97).
Nodule Size
The adrenal incidentaloma cohort had a median nodule size of 1.6 cm (IQR, 1.2–2.1), consisted of 128/969 (13%) multiple nodules, and was more often identified on the left side (Table 2). Adrenal incidentaloma patients with all-cause mortality had a significantly higher median nodule size (1.7 vs 1.6 cm, p = 0.04) and multiplicity (58/353 vs 70/616, p = 0.03) on bivariate testing, but when modeled using Cox regression with all relevant covariates, showed no significant association between all-cause mortality and nodule size categories, laterality, or number.
Table 2:
Comparison of adrenal incidentaloma cohort radiographic characteristics by survival
| Adrenal nodule characteristics | Total nodule cohort (n = 969) |
All-cause mortality (n = 353) |
Alive (n = 616) |
Bivariate p valuea | Adjusted hazard ratiob (95% CI) |
|---|---|---|---|---|---|
| Largest size (cm) | 1.6(1.2–2.1) | 1.7(1.3–2.2) | 1.5(1.2–2.0) | 0.04 | |
| Size categories (cm) | 0.33 | ||||
| 1.0 | 124 (13) | 41 (12) | 83 (13) | reference | |
| 1.1–1.9 | 519 (54) | 183 (52) | 336 (55) | 0.83 (0.58, 1.18) | |
| 2.0–3.9 | 311 (32) | 125 (35) | 186 (30) | 1.05 (0.72, 1.52) | |
| 4.0+ | 15 (2) | 4 (1) | 11 (2) | 0.97 (0.34, 2.77) | |
| Laterality | 0.10 | ||||
| Left | 589 (61) | 200 (57) | 389 (63) | reference | |
| Right | 281 (29) | 110 (31) | 171 (28) | 0.93 (0.73, 1.18) | |
| Bilateral | 99 (10) | 43 (12) | 56 (9) | 0.78 (0.42, 1.45) | |
| Multiple nodules | 128 (13) | 58 (16) | 70 (11) | 0.03 | 1.37 (0.79, 2.36) |
| Myelolipoma | 37 (4) | 8 (2) | 29 (5) | 0.06 | 0.53 (0.25, 1.10) |
CI confidence interval. Data are presented as median (IQR) or n (%).
Calculated with Wilcoxon rank sum test or chi-square test comparing those with mortality outcome to those alive.
Multivariable Cox proportional hazards regression with all-cause mortality as outcome. Model adjusted for nodule size categories, nodule laterality, presence of multiple nodules, presence of myelolipoma, age, sex, race, emergency room disposition, insurance type, CT study type, and baseline comorbidities.
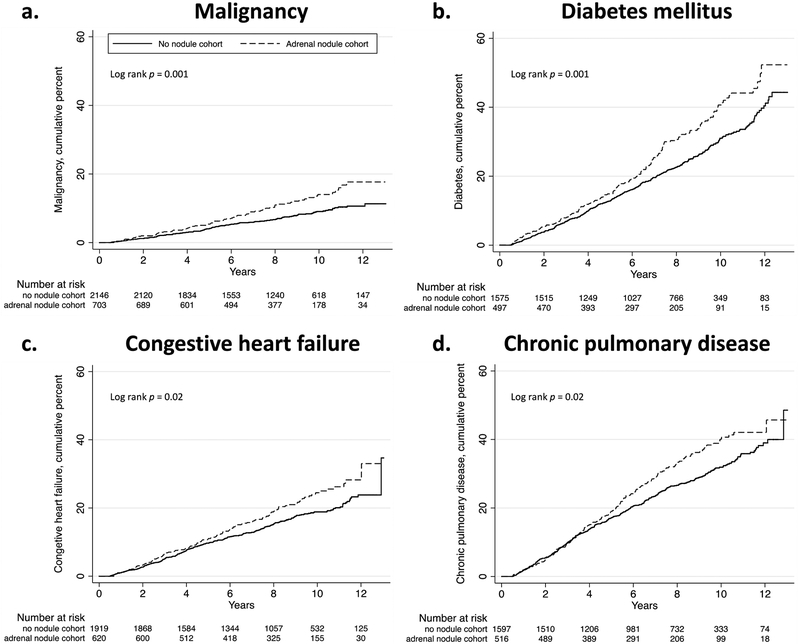
Incident Malignancy
719/969 (74%) from the adrenal incidentaloma cohort and 2182/2907 (75%) from the no-nodule cohort were eligible for exploratory analyses with ≥2 years clinical follow-up, with median follow-up of 8.6 years (IQR, 5.9–10.5). Among those with no malignancy at baseline or within 6 months of follow-up, incident malignancies of any location were detected in 78/703 (11%) of incidentaloma patients and 157/2146 (7.3%) of no-nodule patients (Fig. 4a). Adrenal incidentalomas were associated with increased risk of incident malignancy in both unadjusted (HR 1.56; 95% CI, 1.19–2.05) and fully adjusted (aHR 1.61; 95% CI, 1.22–2.12) models (Table 3).
Figure 4:
Incident outcomes diagnosed ≥6 months from initial CT exam in patients with ≥2 years clinical follow-up without outcome at baseline, by adrenal nodule presence. (a) Malignancy. (b) Diabetes mellitus. (c) Congestive heart failure. (d) Chronic pulmonary disease.
Table 3:
Incident outcomes comparing adrenal nodule cohort to no nodule cohort.
| Incident Outcome | Incident outcomes diagnosed ≥6 months from baseline in patients with ≥2 yrs clinical follow-up | Incidence rate difference per 1000 person-yrs (95% CI) | Unadjusted HR (95% CI) |
Adjusted HRa (95% CI) |
|
|---|---|---|---|---|---|
| Adrenal nodule cohort n/N (%), person-yrs at risk |
No nodule cohort n/N (%), person-yrs at risk |
||||
| Diabetes | 156/497 (31.4), 3445 | 395/1575 (25.1), 11496 | 10.9 (3.0, 18.8) | 1.35 (1.12, 1.63) | 1.42 (1.18, 1.71) |
| Pulmonary Disease | 165/516 (32.0), 3502 | 431/1597 (27.0), 11232 | 8.7 (0.7, 16.8) | 1.23 (1.03, 1.47) | 1.22 (1.01, 1.46) |
| Renal Disease | 179/667 (26.8), 4723 | 452/2023 (22.3), 14909 | 7.6 (1.4, 13.8) | 1.26 (1.06, 1.50) | 1.21 (1.01, 1.44) |
| CHF | 125/620 (20.2), 4682 | 310/1919 (16.1), 14891 | 5.9 (0.7, 11.1) | 1.29 (1.05, 1.59) | 1.32 (1.07, 1.63) |
| PVD | 142/653 (21.8), 4822 | 362/2027 (17.9), 15403 | 5.9 (0.5, 11.4) | 1.27 (1.04, 1.54) | 1.28 (1.05, 1.56) |
| Malignancy | 78/703 (11.1), 5456 | 157/2146 (7.3), 17110 | 5.1 (1.6, 8.6) | 1.56 (1.19, 2.05) | 1.61 (1.22, 2.12) |
| Liver Disease | 107/663 (16.1), 4901 | 278/2003 (13.9), 15283 | 3.6 (−1.0, 8.3) | 1.20 (0.96, 1.50) | 1.23 (0.98, 1.54) |
| Peptic Ulcer Disease | 52/676 (7.7), 5252 | 124/2063 (6.0), 16340 | 2.3 (−0.7, 5.3) | 1.31 (0.94, 1.80) | 1.41 (1.01, 1.96) |
| CVA | 94/636 (14.8), 4805 | 280/1983 (14.1), 15203 | 1.1 (−3.4, 5.6) | 1.06 (0.84, 1.34) | 1.09 (0.86, 1.38) |
| Hemi/Paraplegia | 31/713 (4.4), 5638 | 78/2138 (3.7), 17340 | 1.0 (−1.1, 3.2) | 1.23 (0.81, 1.87) | 1.36 (0.89, 2.08) |
| Myocardial Infarction | 58/656 (8.8), 5108 | 168/1996 (8.4), 15768 | 0.7 (−2.6, 4.0) | 1.06 (0.79, 1.43) | 1.08 (0.80, 1.46) |
| AIDS/HIV | 2/709 (0.3), 5682 | 20/2140 (0.9), 17382 | −0.8 (−1.5, −0.1) | 0.31 (0.07, 1.31) | 0.29 (0.07, 1.29) |
| Dementia | 58/693 (8.4), 5498 | 210/2115 (9.9), 16992 | −1,8 (−5.0, 1.4) | 0.86 (0.64, 1.15) | 1.00 (0.74, 1.35) |
| Rheumatic Disease | 15/702 (2.1), 5599 | 78/2118 (3.7), 17009 | −1.9 (−3.6, −0.2) | 0.59 (0.34, 1.02) | 0.59 (0.33, 1.02) |
HR hazard ratio, CI confidence interval, CHF congestive heart failure, PVD peripheral vascular disease, CVA cerebrovascular accident, AIDS acquired immunodeficiency syndrome, HIV human immunodeficiency virus.
Model adjusted for age, sex, race, insurance type, CT study type (with contrast, without contrast, w/wo contrast), emergency room disposition, and baseline comorbidities.
Of the total 235 incident malignancies, there were no significant association between adrenal nodule and tumor primary site or initial stage (Supplemental Tables 2 and 3). Incident primary adrenal malignancy (paraganglioma) was detected in 1/703 (0.14%) of incidentaloma patients and 0/2146 of no-nodule patients.
Within the adrenal nodule cohort, there was no significant association between nodule size categories, laterality, or number and incident malignancy (Supplemental Table 4).
Other Secondary Outcomes
Among those with no diabetes at baseline or within 6 months of follow-up, incident diabetes was detected in 156/497 (31.4%) of incidentaloma patients and 395/1575 (25.1%) of no-nodule patients (Fig. 4b). Adrenal incidentalomas were associated with increased risk of diabetes (aHR 1.43; 95% CI, 1.18–1.71; Table 3). Significant associations were also observed between incidentaloma presence and incidence of heart failure (aHR 1.32; 95% CI, 1.07–1.63), peripheral vascular disease (aHR 1.28; 95% CI, 1.95–1.56), renal disease (aHR 1.21; 95% CI, 1.01–1.44), and chronic pulmonary disease (aHR 1.22; 95% CI, 1.01–1.46; Table 3). Adrenal incidentaloma presence had no significant difference in incidence of rheumatic disease (aHR 0.59; 95% CI, 0.33–1.02). No significant associations were observed with incident myocardial infarction or cerebrovascular disease.
Adrenal incidentaloma cohort follow-up
Within 12 months of initial detection, a minority of the incidentaloma cohort, 52/969 (5.4%), had a documented diagnosis of adrenal incidentaloma and 27/969 (2.8%) underwent at least one biochemical test of adrenal function. 4/969 (0.4%) underwent evaluation with all three tests: 1 mg Dexamethasone suppression test, plasma aldosterone concentration to plasma renin activity ratio, and plasma or urine metanephrines. Patients with documented diagnoses of adrenal incidentaloma or who underwent any biochemical evaluation of adrenal function had significantly larger nodule size and multiple or bilateral nodules compared to those without a documented diagnosis or biochemical evaluation (Supplemental Tables 5 and 6). Documented diagnosis of adrenal disease was significantly associated with inpatient admission compared to those without a documented diagnosis (36/52 [69%] vs 464/917 [51%]; p = 0.009).
Discussion
Our large cohort study is the first to report significant all-cause mortality risk in patients with adrenal incidentaloma compared to no adrenal incidentaloma controls. Whereas prior mortality investigations relied on biochemical data to demonstrate worse survival comparing secreting adrenal masses to non- secreting masses [12; 14], our population includes adrenal masses at initial radiologic identification irrespective of tumor phenotype. The present framework for understanding adrenal incidentaloma morbidity lies on a continuum of cardiometabolic risk stratified by degree of cortisol secretion, from common non-functional adrenal tumors to rare Cushing’s syndromes, thereby supporting recommendations for routine biochemical workup of all adrenal masses regardless of symptomatic presentation. However, because only a minority of adrenal incidentaloma patients undergo complete biochemical evaluation following radiologic discovery [17], within which a minority represent functional masses [8; 23], many incidentalomas are excluded in such aforementioned endocrinologic studies, creating major selection bias that threatens the generalizability of these recommendations. Our population-based cohort study avoids this by including heretofore underrepresented cases of adrenal incidentaloma.
Our primary analysis demonstrated a 14% increased risk of overall mortality. This supports a growing body of evidence associating incidental adrenal nodules with adverse outcomes [12–14; 16; 24; 25]. Our secondary analyses observed significant associations with incident diabetes and heart failure, consistent with past reports on adverse cardiometabolic outcomes [12; 16; 24], to which we also add peripheral vascular disease and renal disease, two heretofore unreported cardiometabolic associations. The strong association between adrenal incidentaloma with diabetes is noteworthy, as it was the only comorbidity amongst 14 with a significant association at baseline, with the greatest incidence rate difference on follow-up. While elucidating the causal pathways between adrenal incidentaloma, diabetes, and mortality remain beyond the scope of this study, laboratory studies have linked “nonfunctional” adrenal incidentalomas with subclinical hypercortisolism and insulin resistance, where compensatory hyperinsulinema has been hypothesized to mediate adrenal mass growth via insulin-like growth factor 1 receptor expression in the adrenal cortex [26–29]. A recently published longitudinal cohort study on the topic concluded in favor of increased surveillance for glucose intolerance on the basis of a similarly observed association between nonfunctional adrenal tumors and diabetes [16].
While it is known that adrenal incidentaloma themselves confer no significant risk of primary adrenal malignancy [30], we are the first to report an association between adrenal incidentaloma and increased incidence of any malignancy. Molecular studies suggest neoplasms in endocrine glands are akin to neoplasms in other organs, both generally being mediated by abnormal expression of growth-related genes [31], thus allowing for a factor common to the promotion of both adrenal and extra-adrenal tumors. Although our study controlled for one such factor, age, our adrenal incidentaloma cohort was likely at increased baseline risk of tumorigenesis compared to controls.
Our reported effect modification of insurance type on the association between adrenal incidentalomas and mortality, with the Medicaid subgroup having the highest risk, is noteworthy. If insurance type represents varying levels of healthcare access and utilization, then adrenal incidentaloma and their associated modifiable cardiometabolic risk factors may be insufficiently managed in the Medicaid population, leading to worse survival. Taken altogether, our findings suggest routine hormonal evaluation may not mitigate risk for the population of adrenal incidentaloma patients at large. While our observed relationship with cardiometabolic outcomes are consistent with a cortisol-mediated hypothesis, this is difficult to reconcile with malignancy and chronic pulmonary disease, two pathologic states having no known direct relationship with cortisol. Unadjusted confounders such as smoking status or a yet undiscovered factor may link incidentaloma with these myriad outcomes.
Adrenal incidentaloma may be better understood as a biomarker for a variety of physical and psychosocial stresses that are associated with adverse outcomes, rather than a causal factor or disease state. That we report insurance type, a social determinant, as a significant effect modifier for incidentaloma on survival, supports this wider view.
The present study had several limitations. First is the observational design, allowing for unknown covariates that may confound the association between adrenal masses and studied outcomes. Because clinical data was limited to covariates with complete observations through database query, relevant variables known to be associated with incidentaloma and our outcomes such as obesity, hypertension, and smoking status were unaccounted for.
Our adrenal nodule radiologic prevalence of 2.3% is lower than other radiologic series reporting 4–5% [3; 4]. Our lower figure is due to report rather than image review and the exclusion of known stable and sub-centimeter adrenal nodules. The indication for CT exam was not recorded because of difficulty classifying free text inputted by the ordering provider, allowing for the possibility of confounding by indication. However, because all patients with known adrenal incidentaloma and disease were excluded from the study, creating a situation where incidentaloma presence would be a surprise finding at the time of CT study, an association between indication and incidentaloma presence is highly unlikely. In an emergency room setting where abdominal CT scans are most commonly ordered for acute abdominal pain, the decision by the clinician to request a CT examination is not expected to differ with respect to adrenal incidentaloma presence. Accordingly, because radiologic and biochemical follow-up was not the primary focus of this study, our data precludes more complex risk stratification by imaging phenotype. Nevertheless, our only quantitative radiographic variable, size, was not significantly predictive of mortality or malignancy. Limiting our population to nodules fully characterized with quantitative assessments such as by dedicated adrenal protocol would have limited the scope of our study. In the same way that the vast majority of nodules remain biochemically uncharacterized, 97.2% in our population, most remain radiographically indeterminate upon discovery, reflecting contemporary clinical practice. The majority of these indeterminate lesions are presumed to be non-functional adrenocortical adenomas, the most likely diagnosis for our incidentaloma cohort [8].
In conclusion, we have demonstrated an association between adrenal incidentaloma and increased mortality.
Malignancy and various chronic diseases were also associated with adrenal incidentaloma on secondary analysis. These results suggest that adrenal incidentalomas may be a biomarker for increased mortality and other adverse outcomes. Further mechanistic research is needed to elucidate these associations.
Supplementary Material
Key Points.
Adrenal incidentalomas are associated with increased mortality.
Adrenal incidentaloma size is not predictive of mortality.
On exploratory analyses, adrenal incidentalomas are associated with chronic illnesses.
Acknowledgements
The preliminary findings were presented as an oral presentation at the Radiological Society of North America Annual Meeting, November 26, 2018, Chicago, IL.
Funding
This study has received funding by the Einstein Montefiore Department of Radiology and a National Institutes of Health Clinical and Translational Science Awards Grant Number 1UL-1TR001073 from the National Center for Advancing Translational Sciences.
Abbreviations
- AACE
American Association of Clinical Endocrinologists
- AAES
American Association of Endocrine Surgeons
- ACR
American College of Radiology
- aHR
adjusted hazard ratio
- CI
confidence interval
- ICD-9
International Classification of Diseases Ninth Revision
- IQR
interquartile range
- NDI
National Death Index
- SD
standard deviation
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest:
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Informed Consent:
Written informed consent was waived by the Institutional Review Board.
Ethical Approval:
Institutional Review Board approval was obtained.
Methodology
- Retrospective
- Observational
- performed at one institution
References
- 1.Grumbach MM, Biller BM, Braunstein GD et al. (2003) Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med 138:424–429 [DOI] [PubMed] [Google Scholar]
- 2.Young WF Jr (2007) Clinical practice. The incidentally discovered adrenal mass. N Engl J Med 356:601–610 [DOI] [PubMed] [Google Scholar]
- 3.Song JH, Chaudhry FS, Mayo-Smith WW (2008) The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol 190:1163–1168 [DOI] [PubMed] [Google Scholar]
- 4.Hu M, Yip R, Yankelevitz DY, Henschke CI (2016) CT screening for lung cancer: Frequency of enlarged adrenal glands identified in baseline and annual repeat rounds. Eur Radiol 26:4475–4481 [DOI] [PubMed] [Google Scholar]
- 5.Mayo-Smith WW, Song JH, Boland GL et al. (2017) Management of Incidental Adrenal Masses: A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol 14:1038–1044 [DOI] [PubMed] [Google Scholar]
- 6.Berland LL, Silverman SG, Gore RM et al. (2010) Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 7:754–773 [DOI] [PubMed] [Google Scholar]
- 7.Zeiger MA, Thompson GB, Duh QY et al. (2009) American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: executive summary of recommendations. Endocr Pract 15:450–453 [DOI] [PubMed] [Google Scholar]
- 8.Fassnacht M, Arlt W, Bancos I et al. (2016) Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 175:G1–G34 [DOI] [PubMed] [Google Scholar]
- 9.Kastelan D, Kraljevic I, Dusek T et al. (2015) The clinical course of patients with adrenal incidentaloma: is it time to reconsider the current recommendations? Eur J Endocrinol 173:275–282 [DOI] [PubMed] [Google Scholar]
- 10.Cawood TJ, Hunt PJ, O’Shea D, Cole D, Soule S (2009) Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink? Eur J Endocrinol 161:513–527 [DOI] [PubMed] [Google Scholar]
- 11.Kaltsas G, Chrisoulidou A, Piaditis G, Kassi E, Chrousos G (2012) Current status and controversies in adrenal incidentalomas. Trends Endocrinol Metab 23:602–609 [DOI] [PubMed] [Google Scholar]
- 12.Di Dalmazi G, Vicennati V, Garelli S et al. (2014) Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. The Lancet Diabetes & Endocrinology 2:396–405 [DOI] [PubMed] [Google Scholar]
- 13.Morelli V, Reimondo G, Giordano R et al. (2014) Long-term follow-up in adrenal incidentalomas: an Italian multicenter study. J Clin Endocrinol Metab 99:827–834 [DOI] [PubMed] [Google Scholar]
- 14.Debono M, Bradburn M, Bull M, Harrison B, Ross RJ, Newell-Price J (2014) Cortisol as a marker for increased mortality in patients with incidental adrenocortical adenomas. J Clin Endocrinol Metab 99:4462–4470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patrova J, Kjellman M, Wahrenberg H, Falhammar H (2017) Increased mortality in patients with adrenal incidentalomas and autonomous cortisol secretion: a 13-year retrospective study from one center. Endocrine 58:267–275 [DOI] [PubMed] [Google Scholar]
- 16.Lopez D, Luque-Fernandez MA, Steele A, Adler GK, Turchin A, Vaidya A (2016) “Nonfunctional” Adrenal Tumors and the Risk for Incident Diabetes and Cardiovascular Outcomes: A Cohort Study. Ann Intern Med 165:533–542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Becker J, Woloszyn J, Bold R, Campbell MJ (2017) The Adrenal Incidentaloma: An Opportunity to Improve Patient Care. J Gen Intern Med. 10.1007/s11606-017-4240-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellin E, Fletcher DD, Geberer N, Islam S, Srivastava N (2010) Democratizing information creation from health care data for quality improvement, research, and education-the Montefiore Medical Center Experience. Acad Med 85:1362–1368 [DOI] [PubMed] [Google Scholar]
- 19.Bellin E (2017) How to Ask and Answer Questions Using Electronic Medical Record Data. CreateSpace, North Charleston, South Carolina [Google Scholar]
- 20.Bellin E (2015) Riddles in Accountable Healthcare: A primer to develop analytic intuition for medical homes and population health. CreateSpace, North Charleston, South Carolina [Google Scholar]
- 21.Quan H, Li B, Couris CM et al. (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173:676–682 [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Sundararajan V, Halfon P et al. (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139 [DOI] [PubMed] [Google Scholar]
- 23.Hong AR, Kim JH, Park KS et al. (2017) Optimal follow-up strategies for adrenal incidentalomas: reappraisal of the 2016 ESE-ENSAT guidelines in real clinical practice. Eur J Endocrinol 177:475–483 [DOI] [PubMed] [Google Scholar]
- 24.Androulakis II, Kaltsas GA, Kollias GE et al. (2014) Patients with apparently nonfunctioning adrenal incidentalomas may be at increased cardiovascular risk due to excessive cortisol secretion. J Clin Endocrinol Metab 99:2754–2762 [DOI] [PubMed] [Google Scholar]
- 25.Akkan T, Altay M, Unsal Y, Dagdeviren M, Beyan E (2017) Nonfunctioning adrenal incidentaloma affecting central blood pressure and arterial stiffness parameters. Endocrine 58:513–520 [DOI] [PubMed] [Google Scholar]
- 26.Muscogiuri G, Colao A, Orio F (2015) Insulin-Mediated Diseases: Adrenal Mass and Polycystic Ovary Syndrome. Trends Endocrinol Metab 26:512–514 [DOI] [PubMed] [Google Scholar]
- 27.Peppa M, Boutati E, Koliaki C et al. (2010) Insulin resistance and metabolic syndrome in patients with nonfunctioning adrenal incidentalomas: a cause-effect relationship? Metabolism 59:1435–1441 [DOI] [PubMed] [Google Scholar]
- 28.Kamio T, Shigematsu K, Kawai K, Tsuchiyama H (1991) Immunoreactivity and receptor expression of insulinlike growth factor I and insulin in human adrenal tumors. An immunohistochemical study of 94 cases. Am J Pathol 138:83–91 [PMC free article] [PubMed] [Google Scholar]
- 29.Ilvesmaki V, Kahri AI, Miettinen PJ, Voutilainen R (1993) Insulin-like growth factors (IGFs) and their receptors in adrenal tumors: high IGF-II expression in functional adrenocortical carcinomas. J Clin Endocrinol Metab 77:852–858 [DOI] [PubMed] [Google Scholar]
- 30.Corwin MT, Chalfant JS, Loehfelm TW, Fananapazir G, Lamba R, Mayo-Smith WW (2018) Incidentally Detected Bilateral Adrenal Nodules in Patients Without Cancer: Is Further Workup Necessary? AJR Am J Roentgenol. 10.2214/AJR.17.18543:1-5 [DOI] [PubMed] [Google Scholar]
- 31.Derwahl M, Studer H (2002) Hyperplasia versus adenoma in endocrine tissues: are they different? Trends Endocrinol Metab 13:23–28 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.