INTRODUCTION
Strategic planning for hepatitis C virus (HCV) screening and treatment requires up-to-date information on prevalence of HCV spontaneous clearance. Published estimates of HCV spontaneous clearance range from 15% to 60%.1–3 We conducted an observational study over 20 years to evaluate trends in prevalence of HCV spontaneous clearance. Our goals were to estimate the proportion of HCV antibody-positive patients who were viremic, and to identify factors associated with viremia, thus facilitating prediction of the number of patients needing treatment.
METHODS
We conducted a cross-sectional study of adult members of Kaiser Permanente Northern California (KPNC) who had a positive HCV-antibody test and subsequent HCV PCR test during 1998–2017, with continuous membership and drug coverage between tests and no evidence of HCV treatment at KPNC. We defined spontaneous clearance as a positive HCV-antibody test followed by a negative PCR test. We excluded members with a negative HCV-antibody test following their positive HCV-antibody test. Systemic lupus erythematosus and rheumatoid arthritis are associated with false-positive HCV-antibody tests; thus, members with either diagnosis were also excluded.4, 5 The institutional review board at KPNC approved this study with a waiver of written informed consent.
We computed the proportion with clearance by year of PCR test during 1998–2017. In a sensitivity analysis, we applied more conservative criteria to rule out the possibility of HCV treatment, including restricting to members with ≥5 years of health plan membership without evidence of treatment, and restricting to those with ≤14 days between HCV-antibody and PCR tests. We assessed factors potentially associated with spontaneous clearance, including age, sex, race/ethnicity, hepatitis B virus (HBV) and HIV coinfection, HCV-antibody testing in the emergency department (ED), and year of PCR test, evaluated by adjusted prevalence ratios (PRs) from Poisson regression models with robust variance.
RESULTS
Of 25,248 eligible individuals, 67.7% were born during 1945–1965, 58.4% were male, and 41.2% were of minority racial/ethnic backgrounds. Overall, 11,481 (45.5%) met the definition of spontaneous clearance of HCV; prevalence increased from 32.6% in 1998 to 68.7% in 2017 (Figure 1). Estimates of spontaneous clearance were similar in sensitivity analyses, with a prevalence of 72.3% in 2017 for those with ≥5 years of health plan membership without evidence of treatment, and 70.2% in 2017 for those with ≤14 days between HCV-antibody and PCR tests.
Figure 1. Prevalence of spontaneous clearance of HCV by year of PCR test during 1998–2017.
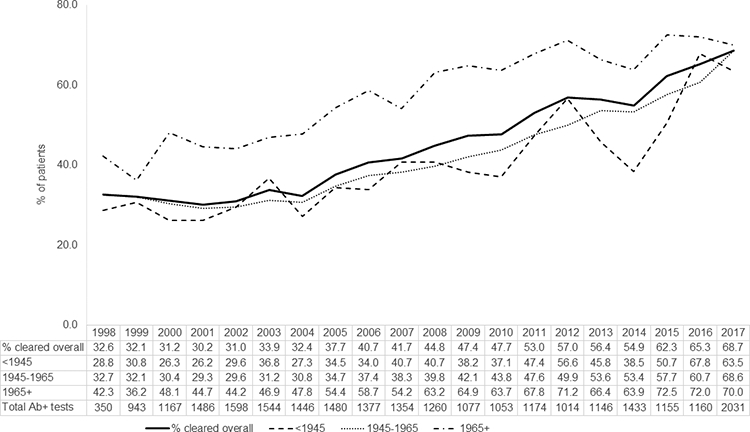
HCV, hepatitis C virus; Ab, antibody. Solid line displays percent with spontaneous clearance for all patients testing HCV-antibody positive. Dotted and dashed lines display percentage with spontaneous clearance for birth years ≥1965, 1945–1965, and <1945.
In multivariable analysis, there was a lower prevalence of spontaneous clearance in older birth cohorts, with PRs of 0.73 (95% confidence interval [CI]: 0.69–0.77) for patients born before 1945 and 0.79 (95% CI: 0.77–0.81) for patients born during 1945–1965 compared with those born after 1965. Males had a 21% lower prevalence of clearance than females (PR 0.79, 95% CI: 0.77–0.81). Black (PR 0.63, 95% CI: 0.59–0.66) and Hispanic patients (PR 0.94, 95% CI: 0.0.90–0.97) had a lower prevalence of clearance compared with White patients, while Asian patients had a higher prevalence (RR 1.21, 95% CI: 1.17–1.25). Finally, HCV-antibody testing in the ED was associated with a reduced prevalence of clearance (PR 0.82, 95% CI: 0.74–0.91).
DISCUSSION
In this large healthcare system, the prevalence of HCV spontaneous clearance doubled over the past decade and reached 68.7% in 2017, which is substantially higher than reported in prior natural history studies1–3 but approaches more recent estimates from HCV screening efforts in the 1945–1965 birth cohort.6, 7 One possible explanation for the observed trend is that patients tested earlier were more likely to be tested for diagnostic purposes or because of known risk factors rather than as true screening. Consistent with this hypothesis, we found that patients tested in the ED had a lower prevalence of clearance. We identified subgroups with a lower prevalence of clearance, highlighting populations that may benefit from targeted HCV screening. Our finding that younger patients had a higher prevalence of clearance is consistent with prior studies and may suggest a more robust response to acute HCV infection.
Our study had several limitations. First, patients treated outside of KPNC may have been misclassified as having clearance. However, most KPNC patients have comprehensive insurance coverage and do not receive treatment outside of the health plan. Our sensitivity analyses further confirmed that this potential misclassification had minimal impact. Second, our data did not allow us to identify the timing of HCV infection or clearance. Third, although HIV and HBV coinfection were not associated with clearance, we did not assess other comorbid conditions. Strengths included the size of the KPNC population, and that it mirrors the age, sex, and race/ethnicity distributions of the surrounding population, increasing generalizability.8
In conclusion, our results suggest that fewer patients than previously expected will be identified as viremic through expanded HCV screening, but that some subgroups are less likely to spontaneously clear HCV. These findings can be useful in strategic planning for HCV screening and treatment on a large scale.
Acknowledgments
Disclosures: JLM reports research grant support from Merck and has consulted on a research grant to Kaiser Permanente Northern California from Gilead. All other authors report no potential conflicts.
Grant support: This work was supported by the TPMG Delivery Science Research Program, and by the National Institute of Allergy and Infectious Diseases (K01 AI122853 to JLM).
Abbreviations:
- HCV
hepatitis C virus
- PR
prevalence ratio
- HBV
hepatitis B virus
- KPNC
Kaiser Permanente Northern California
- ED
emergency department
REFERENCES
- 1.Bulteel N, Partha Sarathy P, Forrest E, et al. Factors associated with spontaneous clearance of chronic hepatitis C virus infection. J Hepatol 2016;65:266–72. [DOI] [PubMed] [Google Scholar]
- 2.Santantonio T, Sinisi E, Guastadisegni A, et al. Natural course of acute hepatitis C: a long-term prospective study. Dig Liver Dis 2003;35:104–13. [DOI] [PubMed] [Google Scholar]
- 3.Thomas DL, Seeff LB. Natural history of hepatitis C. Clin Liver Dis 2005;9:383–98, vi. [DOI] [PubMed] [Google Scholar]
- 4.Conway R, Doran MF, O’Shea FD, et al. The impact of hepatitis screening on diagnosis and treatment in rheumatoid arthritis. Clin Rheumatol 2014;33:1823–7. [DOI] [PubMed] [Google Scholar]
- 5.Mohan P, Rajasekaran M, Ramanathan P, et al. Prevalence of hepatitis C virus antibodies in systemic lupus erythematosus. Eur J Gastroenterol Hepatol 2009;21:1437–8. [DOI] [PubMed] [Google Scholar]
- 6.Castrejon M, Chew KW, Javanbakht M, et al. Implementation of a Large System-Wide Hepatitis C Virus Screening and Linkage to Care Program for Baby Boomers. Open Forum Infect Dis 2017;4:ofx109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konerman MA, Thomson M, Gray K, et al. Impact of an electronic health record alert in primary care on increasing hepatitis c screening and curative treatment for baby boomers. Hepatology 2017;66:1805–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gordon N Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2011 California Health Interview Survey, 2015. [Google Scholar]


