Abstract
Human T cell leukemia virus type 1 (HTLV-1) is a horizontally transmitted virus infection of CD4+ lymphocytes which causes adult T cell leukemia-lymphoma (ATLL) and HTLV-associated myelopathy (HAM). The viral genome encodes two oncoproteins, transactivator protein (Tax) and helix basic zipper protein (HBZ), which are considered tumor initiator and maintenance factors, respectively. Tax is the primary inducer of clonal infected T cell expansion, and genetic instability. The immune response to Tax results in the selection of cells with little or no Tax expression, which have undergone genetic and epigenetic alterations that promote T cell activation, proliferation, and resistance to apoptosis. This selection of malignant cells occurs over several decades in 5% of infected individuals. Novel insights into the molecular details of each of these events has led to targeted therapies for ATLL.
Introduction
Human T-cell leukemia viruses (HTLV) are members of the δ-retrovirus genus, which are exogenous horizontally transmitted viruses found in several groups of mammals1. The δ-retrovirus members include HTLV and simian T-cell leukemia virus (STLV) strains 1–4, and bovine leukemia virus (BLV). HTLV-1 has infected 5–20 million individuals, based on various estimates, with the highest endemic rates of infection in southern Japan, the Caribbean islands, Central and South America, parts of Africa, northeast Iran, and Australian and Melanesian aborigines2. HTLV-2 is found in native North, Central, and South Americans, and in parts of Africa3. In the United States, the HTLV-1/2 seroprevalence rate among volunteer blood donors averages 0.016%4. HTLV-3 and 4 have been isolated in a small number of bush-meat hunters in Cameroon5.
HTLV-1 is the most clinically significant HTLV member. Approximately 5% of HTLV-1 infected individuals develop clinical disease6. These disorders include a rapidly progressive, therapy refractory, and fatal form of T-cell lymphoproliferation, characterized as leukemia or lymphoma, and designated adult T cell leukemia (ATL) or adult T-cell leukemia-lymphoma (ATLL). In addition, HTLV-1 causes a debilitating myelopathy (HAM), as well as uveitis, infectious dermatitis, and other inflammatory disorders (including pneumonitis, arthritis, myositis). HTLV-2 has been associated with milder neurological disorders and chronic pulmonary disorders, although the etiological relationship remains controversial7. HTLV-3 and 4 are not associated with a clinical disorder8.
Several excellent reviews of HTLV-1 molecular biology have been published9,10. The current review highlights recent ideas regarding the molecular basis of ATLL.
Viral Genome
The HTLV-1 genome is 8.5 kilobases (kb) in length (Fig 1)11,12. The genome is a plus, single-stranded RNA with a 5’cap and a 3’poly-A tail. Two copies of the viral genome are packaged in each virus particle. The viral RNA is reverse transcribed in infected cells into double stranded (ds) DNA, which is integrated almost randomly in the genome of the infected cell. The integrated DNA includes long-terminal repeats of approximately 600 bp, which regulate initiation and termination of viral RNA synthesis.
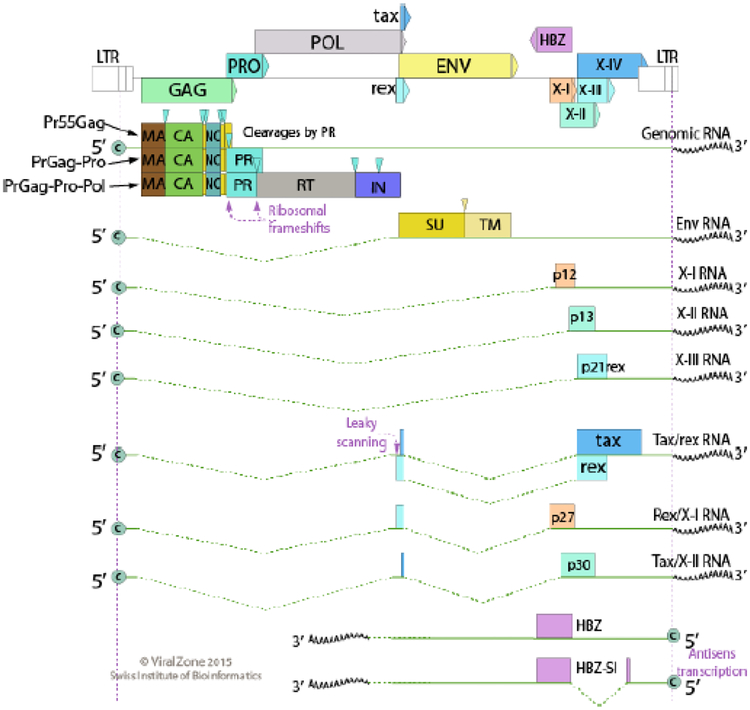
Fig 1.
HTLV-1 Genome. The integrated provirus utilizes the promoter in the 5’LTR to drive transcription. This results in an unspliced full length mRNA that serves as genomic DNA to be packaged into virions. It is also used as a template for translation of Gag, Gag-Pr (1 ribosomal frameshift), and Gag-Pr-Pol (2 ribosomal frameshifts) polyproteins. The single spliced mRNA encodes Env that is cleaved into SU and TM envelope proteins. Completely spliced mRNAs encode Tax and Rex. Four accessory protein, p27I, p12I, p13II, and p30II are produced by alternative splicing of ORFs I and II. The p8I protein is a proteolytic cleavage product from p12I. The HBZ proteins are produced from unspliced and spliced mRNAs encoded by minus strand transcripts. Reprinted with permission from Viral Zone58
The viral genome includes classical retroviral genes found in avian and other mammalian retroviruses, gag, protease (pr), pol, and env. The Gag (Group-Specific Antigen) protein is synthesized as a 55 kd precursor protein, that is processed by the viral protease into a matrix protein (MA) of 19 kd, a capsid protein (CA) of 24 kd, and a nucleocapsid (NC) protein of 15 kd. MA is situated at the inner surface of the viral lipid membrane. CA is the major structural component of the viral nucleocapsid. NC binds the viral genome and promotes reverse transcription. Pr is an aspartyl protease that processes the Gag, Gag-Pr, and Gag-Pr-Pol precursor proteins. Gag-Pr and Gag-Pr-Pol are synthesized from the same viral RNA that encodes Gag, but are the result of ribosome frameshifting events during translation. The Pol protein includes the 62 kd viral polymerase, reverse transcriptase, and the 32 kd viral integrase.
The Env glycoprotein is synthesized as a 66 kd precursor protein, which is processed by cellular furins in the endoplasmic reticulum (ER) into a 45 kd surface Env protein (SU) and a 21 kd transmembrane Env protein (TM). The Env proteins form a trimer on the surface of the virus particle. The SU protein binds to the virus receptor, and subsequent conformational changes of the SU-TM complex lead to fusion of the virus membrane with the target cell membrane.
Unlike classical mouse and avian retroviruses, δ-retrovirus genomes encode additional non-structural non-enzymatic proteins that regulate replication and pathogenesis. Tax (transcriptional activator protein from the X-gene region) is a 40 kd protein that potently promotes viral transcription via interaction with CREB-binding protein (CBP) and p300 to promote the activity of the cAMP-response protein protein (CREB) – activated T cell factor (ATF) transcription factors13. Tax promotes cellular transcription via interaction with activators of the serum-response factor (SRF) that act through Fos and other immediate early proteins. Tax also promotes cellular transcription via binding to the regulatory (γ) subunit of the IκB (nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor) kinase complex, resulting in activation of the nuclear factor kappa B (NFκB) transcriptional pathway. In addition, Tax binds several proteins resulting in repression of cell cycle inhibitors, checkpoint proteins, and DNA repair proteins. Together, the Tax-binding and Tax transcriptional target proteins have been designated the “Tax interactome”.
Rex is a 30 kd protein that regulates nuclear export of viral RNA14. This occurs through interaction with a stem-loop structure, known as the Rex-response element (RRE), present in the 3’ non-coding sequences of all viral plus strand RNAs. The HTLV-1 p12 and p8 ORF I proteins are ER and Golgi proteins which promote NFAT (nuclear factor of activated T cells)-induced T cell activation15. The p8 protein also promotes cell adhesion and virus transmission via cellular conduits16. The p30 ORF II protein is a nuclear transcription factor that represses CBP/p300 activity17. The p13 ORF II protein is a mitochondrial protein that promotes the generation of reactive oxygen species and T cell activation18. The 45 kd HBZ (helix basic zipper) protein is expressed from a gene on the viral antisense or minus strand. It binds to several different proteins involved in viral activation and cellular signaling19.
Replication and Transmission
HTLV-1 binds to a wide range of human cell types through interactions with heparin sulfate proteoglycans, glucose transporter I, and neuropilin-120. The mechanism of viral entry as well as early steps in virus uncoating remain poorly defined. HTLV-1 is capable of infecting a wide range of human cells in vitro, but in infected patients, the majority of virus infected cells are CD4+ lymphocytes. Reverse transcription occurs in the cytoplasm, and the complex of viral dsDNA is imported into the nucleus with the integrase. The linear viral dsDNA is integrated into the cellular genome at many sites with a preference for transcription start sites with a bias towards transcription factor binding sites, particularly those utilized by STAT1 (signal transducer and activator of transcription 1), TP53 (tumor protein 53), and HDAC6 (histone deacetylase 6)21. The integrated viral DNA (provirus) may be latent, with no active plus strand transcription, or it may be actively transcribed22. Unspliced, single spliced, and multiple spliced viral RNAs are exported from the nucleus for translation. The unspliced viral RNA is also utilized for viral genomic RNA packaging. Virus assembly occurs at the plasma membrane with the precursor Gag, Gag-Pr, Gag-Pr-Pol proteins, and the SU and TM Env proteins23. The resultant virus particles detach from the plasma membrane, the viral protease is auto-catalytically processed, and then it promotes cleavages of the precursor structural proteins. This results in an infectious virus particle that is transmitted to target host cells, primarily by cell-to-cell contact rather than as cell-free virus particles16. Cell-to-cell transmission involves a viral synapse, analogous to the immunological synapse that occurs in antigen presentation to T cells. However, dendritic cells can also be infected by cell-free virus
Cells have evolved a broad range of restriction factors that inhibit replication of different retroviruses. The cytidine deaminase, APOBEC 3G, has been shown to restrict HTLV-1, inducing hypermutation in the viral genome24. HTLV-1 is also restricted by the exonuclease and deoxynucleotide triphosphohydrolase SAMHD1 (SAM domain and HD domain-containing protein 1) which depletes deoxynucleoside triphosphates required for reverse transcription25. However, HTLV-1 can circumvent SAMHD1-dependent restriction, although the way this occurs is not understood. It remains to be determined whether other restriction factors or immune sensors also regulate HTLV-1 infection.
Oncogenesis
HTLV-1 is an oncogenic virus in culture and infected patients. Recent information explains why infection is often prolonged over many decades prior to the development of malignancy, and in only about 5% of infected individuals26. The current model is that infected cells expand within an infected individual primarily through cellular division of already infected cells rather than virus release and infection of new host cells10. This process has been designated clonal expansion. The two viral oncoproteins, Tax and HBZ, are thought to be critically involved in the clonal expansion process. This process is characterized by genetic instability with the accumulation of multiple genomic and epigenomic alterations. Key secondary alterations are hypothesized to be important in the development of ATLL.
Tax
Tax expression is considered to be a key early driver of both virus expression and lymphoproliferation. Tax activation of transcriptional factors NFκB, SRF, and CREB, results in transcriptional activation of cytokines and their receptors, and inhibition of apoptosis13. Tax repression of p18 and DNA polymerase β results in abnormal cell cycle regulation, and suppresses DNA repair. Tax functional inactivation of p16, p53, mitotic arrest deficient protein 1 (MAD1), and transforming growth factor β signaling promotes abnormal cell cycle regulation, genetic instability, and inhibition of apoptosis. TAX binds to numerous PDZ proteins, which result in activation of the phosphatidyl inositol 3 kinase (PI3K)-Akt pathway27.
However, Tax is also a highly immunogenic protein28. Thus, immune evasion mechanisms down-regulate Tax expression, through several different mechanisms. Promoter hypermethylation occurs in the 5’LTR, inhibiting tax expression29. Tax recruits several inhibitors of proviral transcription, including STK11 (serine threonine kinase 11), SIRT1 (nicotinamide adenine dinucleotide-dependent deacetylase sirtuin-1), TCF7 (transcription factor 7), and LEF1 (lymphoid enhancer binding factor 1)30–32. In some cases, deletions and inactivating mutations are found in the 5’LTR and tax coding region in the HTLV-1 genome in ATLL cells. Recent work has demonstrated dynamic expression of Tax in some cases of ATL, within a small proportion of ATL cells at a given time, which promote survival of the entire population of cells through an indirect mechanism that remains to be deciphered. The strong cytotoxic T cell (CTL) response directed against Tax selects for T cells with low or no Tax expression.
HBZ
The hbz gene is continuously expressed in all HTLV-1 infected subjects thoughout infection, and it is only weakly immunogenic. It has weak transforming activity, independent of Tax, and it has been proposed to be a tumor maintenance factor. The hbz RNAs include spliced and unspliced forms that promote T cell proliferation, independent of their coding capacity. The HBZ protein binds a wide range of proteins including those involved in signaling pathways, such as Smad 2,3, (Mothers against decapentaplegic homologs 2,3), NFAT, MafB (musculoaponeurotic fibrosarcoma oncogene homolog B), CREB/ATF and Jun family proteins, FoxO3a (forkhead box transcription factor 03a), IRF-1 (interferon regulatory factor 1), CBP/p300, p65 (NFκB subunit p65 or RelA), TCF1, LEF1, CENP-B (centromere protein B), T cell phenotype (FoxP3, forkhead box protein 3)), and DNA repair (GADD34, growth arrest and DNA damage protein 34). Thus, HBZ inhibits apoptosis, autophagy, inflammation, and disrupts genomic integrity. HBZ counteracts many of the functions of Tax, thus maintaining a persistent latent infection.
Genetic Alterations in ATLL
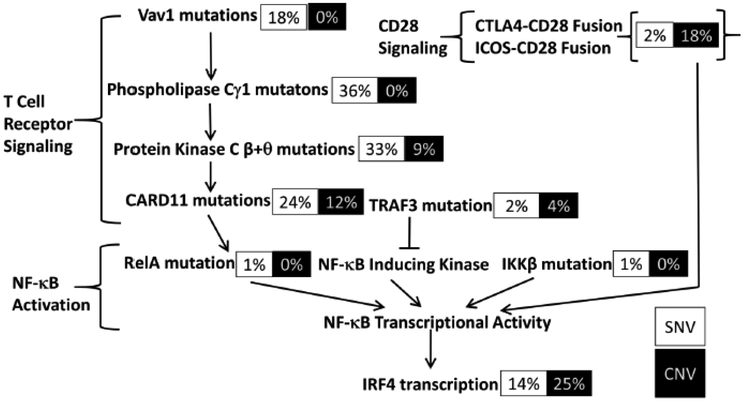
Genomic analysis of ATLL cases identified a high rate of mutations (2.9/Mb), particularly within the Tax interactome33. Mutations were particularly common in genes responsible for T cell receptor-NFκB signaling, T cell trafficking, and T cell-related pathways, as well as immunosurveillance (Fig 2). Activating mutations were identified in PLCG1 (phospholipase G1), PRKCB (protein kinase c β), CARD11 (caspase recruitment domain-containing protein 11), VAV1 (Vav guanine nucleotide exchange factor 1), IRF4, FYN (59-kDa member of the Src family of kinases),. CCR4 (chemokine receptor 4), and CCR7. Gene fusions were also notable, including CTLA4-CD28 (cytotoxic T-lymphocyte-associated protein 4 – cluster of differentiation protein 28 required for T cell activation) and ICOS-CD28 (inducible T-cell costimulator precursor – CD28). Intragenic deletions were noted in IKZF2 (zinc finger protein Helios), CARD11, and TP73, as well as mutations in GATA3 (GATA-binding protein 3), HNRNPA2B1 (heterogeneous nuclear riboprotein A2/B1), GPR183 (G-protein couple receptor 183), CSNK2A1 (casein kinase II subunit 2 alpha 1), CSNK2B, and CSNK1A1. These findings suggest that HTLV-1 infected cells develop mutations in these key oncogenic pathways survive and proliferate despite immunological selection for low levels of Tax expression.
Fig 2.
TCR Activation Pathway in ATLL. The figure depicts percentage of cases in which eachin the pathways is mutated in ATLL. SNVs are depicted in black font, CNVs in white font. Reprinted with permission from reference50. This research was originally published in Journal of Biological Chemistry. (c) the American Society for Biochemistry and Molecular Biology.
Epigenetic Alterations in ATLL
Oncoproteins of human tumor viruses regularly interact with the cellular epigenetic machinery34.. Tax activates expression of the genes for arginine and histone methyltransferases, and silences histone deacetylase 1 (HDAC1) gene expression. Epigenetic regulatory proteins, including histone deacetylase inhibitors and DNA methylation inhibitors have been shown to reactivate the latent HTLV-1 provirus22. In contrast, bromodomain and extra-terminal (BET) protein inhibition suppresses Tax-mediated tumorigenesis by inhibiting NFκB signaling35.
Key epigenetic alterations also occur in ATLL, when Tax is no longer expressed. Immortalized, but untransformed cells display very similar epigenetic changes as those in transformed ATL cells, suggesting that epigenetic changes are likely an early event in leukemogenesis. ATL is characterized by prominent CpG island DNA methylation, leading to transcriptional silencing36. These alterations occur without mutation at TET2 (Tet Methylcytosine Dioxygenase 2, IDH2 (isocitrate dehydrogenase 2), and DNMT3A (DNA methyl transferase 3A). Aberrant activation of EZH2 (protein coding enhancer of Zeste 2 polycomb repressive Complex 2 subunit), has been described in ATL, resulting in trimethylation of histone H3 lysine (K) 27, and suppression of a wide range of different genes.
A binding site (BS) for the epigenetic barrier element, CTCF, has been identified in the integrated HTLV-1 provirus37. Portions of the genome upstream of the CTCF-BS are extensively methylated at CpG sites, and bound histone 3 proteins are modified by K36 trimetylation. In contrast, portions of the genome downstream of the CTCF-BS are generally unmethylated at CpG sites, and bound histone 3 proteins are marked by K4 trimethylation. Moreover, chromatin loops between the CTCF-BS in the provirus and adjacent cellular CTCF-BS result in transcriptional activation of cellular sequences38. These findings suggest that the quarternary structure of the infected cell DNA may be a determinant of leukemogenesis.
Model for ATLL Development
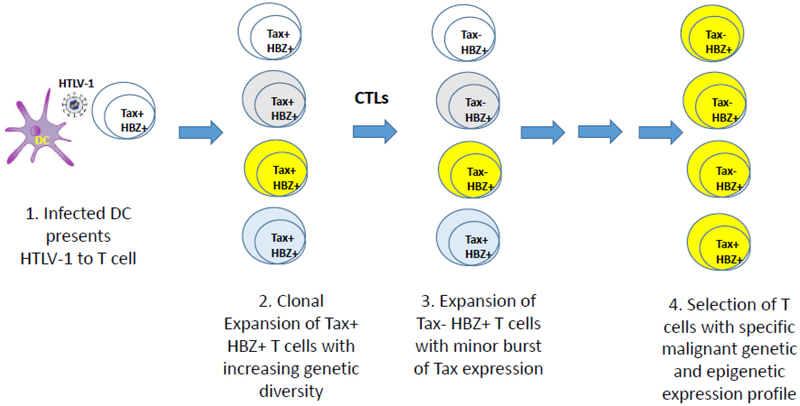
The current view of HTLV-1 transformation describes a multi-step process. Initial steps of infection may occur in dendritic cells, which then present virus to mature T cells or their precursors, via cell-to-cell transmission of the virus (Fig 3). The number of infected cells expands as a result of virus replication, and clonal amplification of infected cells. The growth promoting effects of HTLV-1 are largely attributed to the effects of the Tax protein. Tax also promotes genetic instability, leading to genetic and epigenetic alterations within infected cells. The level of Tax is regulated by HBZ, and the host immune response targets Tax, and Tax-induced viral gene products. Thus, infected cells evade these responses by down-modulating Tax expression. However, intermittent and transient expression of Tax by small numbers of cells within the infected cell population continue to drive T cell expansion and genetic damage. Thus, there is likely considerable genetic heterogeneity in the infected cell population. There is selective expansion of infected cells that have undergone cellular alterations that promote cell proliferation, resistance to apoptosis, and evasion of the immune response. Subpopulations of infected cells with key genetic and epigenetic changes evolve into leukemia or lymphoma. The prolonged period of evolution of the malignancy likely also contributes to therapy resistance, since effective anti-tumor treatments cooperate with active tumor immunity.
Fig 3.
Multiple Events of HTLV-1 Infection and Transformation. The schematic hypothesizes that the initia HTLV-1 infected cell is a dendritic cell which presents infectious virus to a T cell. Subsequent expression of Tax, HBZ, and plus strand virus genes result in infection and clonal expansion of other T cells, resulting in genetic heterogeneity, as indicated by different colored cells. Immune responses, as well as viral gene restrictions, result in little or no Tax and plus strand gene product expression from the majority of infected T cells, but a minor population of T cells with transient bursts of Tax expression. Several decades of infection result in selection of cells with specific combinations of genetic and epigenetic alterations that result in adult T-cell leukemia lymphoma.
Implications for ATLL Therapy
Therapies that block HTLV-1 replication include nucleoside reverse transcriptase inhibitors (e.g. zidovudine, abacavir) and integrase inhibitors (e.g. raltegravir). Protease inhibitors and non-nucleoside reverse transcriptase inhibitors developed for HIV-1 have little activity against analogous proteins of HTLV-1. Antivirals may impact viral load only during early stages of infection or during transient bursts of virus replication, but do not inhibit clonal expansion of previously infected cells. Thus, their role in HTLV-1 infected individuals remains unclear.
The combination of zidovudine (ZDV) and interferon alpha (FIN) has significant activity in chronic and acute forms of ATLL, but not in the lymphoma subtype of ATLL. It is doubtful that this combination is functioning by inhibiting virus replication, but more likely has direct cytotoxic effects on the cells39. Zidovudine inhibits tolemerase and reactivation of p53 during cellular senescence40. Arsenic trioxide (AsO3) synergizes with IFN to induce cell cycle arrest and apoptosis of ATLL cells. This combination induces proteasomal degradation of Tax, with shutoff of the NFκB signaling pathway41. Clinical trials of the combination of ZDV, IFN, and AsO3 for ATLL have been initiated42.
Several therapeutic efforts have focused on Tax or Tax-induced gene products. A therapeutic vaccine directed at Tax was tested in a clinical trial of ATLL, resulting in remission in two of three treated subjects43. Moreover, several Tax-induced proteins have been targeted for ATLL therapy. The α subunit of the interleukin 2 receptor (CD25) is highly expressed on ATLL cells44. Thus, antibodies and radioimmunoconjugates directed at CD25 have shown activity in ATLL treatment45. Another Tax-induced protein is chemokine receptor CCR4, which is over-expressed on ATLL cells46. A monoclonal antibody to CCR4, mogamulizumab, is an effective agent in refractory ATLL or in combination with chemotherapy or ZDV/IFN47
Activating mutations in the TCR signaling pathway may also be targets for ATLL therapy33. Protein kinase c (PKC) is activated by mutation in its gene or that for upstream mediator, phospholipase γ. Several inhibitors have been developed and tested in clinical trials. Enzastaurin is a highly specific PKC β inhibitor which was well tolerated in previous trials in subjects with B cell lymphomas48. Midostaurin is a multikinase inhibitor, approved for FLT3-mutated acute myelogenous leukemia, which has significant activity against PKC β49. Studies of these agents against ATLL cell lines are reasonable.
Another member of the TCR pathway is interferon regulatory factor 4 (IRF4). This gene is mutated in 33% of ATLL cases, and over-expressed as a result of upstream mutations in the majority of ATLL cases50. Levels of IRF4 in ATLL have been shown to correlate with prognosis51. Direct inhibitors are currently being evaluated in other diseases in which IRF4 has been shown to be pathogenic, including multiple myeloma52. Another approach to inhibit IRF4 expression is the use of an immune modulatory imide drug (IMID), such as lenalidomide53. Lenalidomide binds to the E3 ubiquitin ligase, cereblon, and increases its activity54. This promotes ubiquitination and degradation of transcription factors Ikaros and Aiolos, and overcome their ability to promote IRF4 synthesis.
A downstream transcriptional target of the TCR pathway are members of the Myc protein family, Inhibitors of the BET family have been shown to repress Myc expression, and possess activity against ATLL cells in culture55. Currently, BET inhibitors are under investigation in other clinical settings56.
Aberrant epigenetic changes in ATLL may also be therapeutically targeted. EZH2 inhibition was shown to reverse polycomb-dependent alterations in ATLL and selectively eliminate leukemia and HTLV-1 infected cells in culture57.
Conclusions
Insights into the molecular biology of HTLV-1 are leading to the development of targeted agents for ATLL. It is expected that these studies may provide an effective approach to this almost uniformly fatal malignancy, as well as approaches for prognostication and prevention of this disorder.
Acknowledgements
This work was supported by PHS grants (P01 CA100730, R01 CA063417, R21 CA234640, R21 AI26652) and Siteman Cancer Center Investmant Program awards (to L.R. and T.F.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lairmore MD, Franchini G. Human T-cell leukemia virus types 1 and 2 In: Fields B, Knipe DM, Howley PM, eds. Fields Virology. Philadelphia: Wolters Kluwer Health; 2007: 2071–106. [Google Scholar]
- 2.Goncalves DU, Prioietti FA, Ribas JGR, et al. Epidemiology, treatment, and prevention of human T-cell leukemia virus type 1-associated diseases. Clinical Microbiology Reviews 2010; 23: 577–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy EL. Infection with human T-lymphotropic virus types-1 and −2 (HTLV-1 and −2): implications for blood transfusion safety. Transfusion Clinique et Biologique 2016; 23: 13–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang YB, Kaidarova Z, Indes D, et al. Seroprevalence and demographic determinants of human T-lymphotropic virus type 1 and 2 infections among first-time blood donors-Unites States, 2000–2009. Journal of Infectious Disease 2014; 209: 523–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gessain A, Rua R, Betsem E, Turpin J, Mahieux R. HTLV-3/4 and simian foamy retroviruses in humans: discovery, epidemiology, cross-species transmission and moleuclar virology. Virology 2013; 435: 187–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lairmore MD, Anupam R, Bowden N, et al. Molecular determinants of human T-lymphotropic virus type 1 transmission and spread. Viruses 2011; 3: 1131–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwaan N, Lee TH, Chafets DM, et al. HTLV Outcomes Study (HOST) Investigators. Long-term variations in human T lymphotropic virus (HTLV)-I and HTLV-II proviral loads and association with clinical data. Journal of Infectious Diseases 2006; 194: 1557–64. [DOI] [PubMed] [Google Scholar]
- 8.Mahieux R, Gessain A. HTLV-3/STLV-3 and HTLV-4 viruses: discovery, epidemiology, seorlogy and molecular aspects. Viruses 2011; 3: 1074–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsuoka M, Jeang K-T. Human T-cell leukaemia virus type 1 (HTLV-1) infectivity and cellular transformation. Nature Reviews in Cancer 2007; 7: 270–80. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe T Adult T-cell leukemia: molecular basis for clonal expansion and transformation of HTLV-1-infected T cells. Blood 2017; 129: 1071–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferreira OC, Planelles V, Rosenblatt JD. Human T-cell leukemia viruses: epidemiology, biology, and pathogenesis. Blood Reviews 1997; 11: 91–104. [DOI] [PubMed] [Google Scholar]
- 12.Kannian P, Green PL. Human T lymphotropic virus type 1 (HTLV-1): molecular biology and oncogenesis. Viruses 2010; 2: 2037–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harhaj EW, Giam CZ. NF-kB signaling mechanisms in HTLV-1-induced adult T-cell leukemia/lymphoma. FEBS Journal 2018; 285: 3324–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakano K, Watanabe T. HTLV-1 rex tunes the cellular environment favorable for viral replication. Viruses 2016; 8: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edwards D, Fenizia C, Gold H, et al. Orf-1 and orf-II encoded proteins in HTLV-1 infection and persistence. Viruses 2011; 3: 861–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gross C, Thoma-Kress AK. Molecular mechanisms of HTLV-1 cell-to-cell transmission. Viruses 2016; 8: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anupam R, Doueiri R, Green PL. The need to accessorize: molecular roles of HTLV-1 p30 and HTLV-2 p28 accessory proteins in the viral life cycle. Frontiers in Microbiology 2013; 4: 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silic-Benussi M, Biasiotto R, Andresen V, Franchini G, D’Agostino DM, Ciminale V. HTLV-1 p13, a small protein with a busy agenda. Molecular Aspecis of Medicine 2010; 31: 350–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma G, Yasunaga J, Matsuoka M. Multifaceted functions and roles of HBZ in HTLV-1 pathogenesis. Retrovirology 2016; 13: In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones KS, Lambert S, Bouttieer M, et al. Molecular aspects of HTLV-1 entry: functional domains of the HTLV-1 surface subunit (SU) and their relationships to the entry receptors. Viruses 2011; 3: 794–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niederer HA, Bangham CR. Integration site and clonal expansion in human chronic retroviral infection and gene therapy. Viruses 2014. 6: 4140–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kulkarni A, Bangham CRM. HTLV-1: regulating the balance between proviral latency and reactivation. Frontiers in Microbiology 2018; 9: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maldonado JO, Martin JL, Mueller JD, Zhang W, Mansky LM. New insights into retroviral Gag-Gag and Gag-membrane interactions. Frontiers in Microbiology 2014; 5: 302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fan J, Ma G, Nosaka K, et al. Apobec3G generates nonsense mutations in human T cell leukemia virus type 1 proviral genomes in vivo. Journal of Virology 2010; 84: 7278–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sze A, Olagnier D, Lin R, vanGrevenynghe J, Hiscott J. SAMHD1 host restriction factor: a link with innate immune sensing of retrovirus infection. Journal of Molecular Biology 2013; 425: 4981–94. [DOI] [PubMed] [Google Scholar]
- 26.Tsukasaki K, Tobinai K. Human T-cell lymphotropic virus type I-associated adult T-cell leukemia-lymphoma: new directions in clinical research. Clinical Cancer Research 2014; 20: 5217–25. [DOI] [PubMed] [Google Scholar]
- 27.Boxus M, Twizere J-C, Legros S, Dewulf J-F, Kettmann R, Willems L. The HTLV-I Tax interactome. Retrovirology 2008; 5: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rowan AG, Suemori K, Fujiwara H, et al. Cytotoxic T lymphocyte lysis of HTLV-1 infected cells is limited by weak HBZ protein expression, but non-specifically enhanced on induction of Tax expression Retrovirology 2014; 11: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ishida T, Hamano A, Koiwa T, Watanabe T. 5’long terminal repeat (LTR)-selective methylation of latently infectd HIV-1 provirus that is demethylated by reactivation signals. Retrovirolgy 2006; 3: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ma G, Yasunaga J-i, Akari H, Matsuoka M. TCF1 and LEF1 act as T-cell intrinsic HTLV-1 antagonists by targeting Tax. Proceedings of the National Academy of Sciences 2015; 112: 2216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang HM, Gao WW, Chan CP, et al. LKB1 tumor suppressor and salt-inducible kinases negatively regulate human T-cell leukemia virus type 1 transcription. Retrovirolgy 2013; 10: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang HM, Gao WW, Chan CP, et al. SIRT1 suppresses human T-cell leukemia virus type 1 transcription. Journal of Virology 2015; 89: 8623–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kataoka K, Nagata Y, Kitanaka A, et al. Integrated molecular analysis of adult T-cell leukemia/lymphoma. Nature Genetics 2015; 47: 1304–15. [DOI] [PubMed] [Google Scholar]
- 34.Minarovits J, Demcsak A, Banati F, Niller HH. Epigenetic dysregulation in virus-associated neoplasms. Advances in Experimental Medicine and Biology 2016; 879: 71–90. [DOI] [PubMed] [Google Scholar]
- 35.Wu X, Qi J, Bradner JE, Xiao G, Chen LF. Bromodomain and extraterminal (BET) protein inhibition suppresses human T cell leukemia virus 1 (HTLV-1) Tax protein-mediated tumorigenesis by inhibiting nuclear factor κB (NF-κB) signaling. Journal of Biolgical Chemistry 2013; 288: 36094–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamagishi M, Fujikawa D, Watanabe T, Uchimaru K. HTLV-1-mediated epigenetic pathway to adult T-cell leukemia-lymphoma. Frontiers in Microbiology 2018; 9: 1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Satou Y, Miyazato P, Ishihara K, et al. The retrovirus HTLV-1 inserts an ectopic CTCF-binding site into the human genome. Proceedings of the National Academy of Sciences, USA 2016; 113: 3054–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Melamed A, Yaguchi H, Miura M, et al. The human leukemia virus HTLV-1 alters the structure and transcription of host chromatin in cis. Elife 2018; 7: e36245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nasr R, ElHajj H, Kfoury Y, deThe H, Hermine O, Bazarbachi A. Controversies in targeted therapy of adult T cell leukemia/lymnphoma: ON target or OFF target effects? Viruses 2011; 3: 750–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Datta A, Bellon M, Sinha-Datta U, et al. Persistent inhibition of telomerase reprograms adult T-cell leukemia to p53-dependent senescence. Blood 2006; 108: 1021–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nasr R, Rosenwald A, El-Sabban ME, et al. Arsenic/interferon specifically reverses 2 distinct gene networks critical for the survival of HTLV-1-infected leukemic cells. Blood 2003; 101: 4576–82. [DOI] [PubMed] [Google Scholar]
- 42.Suarez F, Marcais A, Ghez D, et al. Arsenic trioxyde in the treatment of HTLV1 associated ATLL. Retroviroloogy 2011; 8 (Suppl 1): A59. [Google Scholar]
- 43.Suehiro Y, Hasegawa A, Iino T, et al. Clinical outcomes of a novel therapeutic vaccine with Tax peptide-pulsed dendritic cells for adult T cell leukaemia/lymphoma in a pilot study. British Journal of Haematology 2015; 169: 356–66. [DOI] [PubMed] [Google Scholar]
- 44.Ballard DW, Bohnlein E, Lowenhal JW, Wano Y, Franza BR, Greene WC. HTLV Tax induces cellular proteins that activate the kappa B element in the IL-2 receptor alpha gene. Science 1988; 241: 1652–5. [DOI] [PubMed] [Google Scholar]
- 45.Waldmann TA, White JD, Carrasquillo JA, et al. Radioimmunotherapy of interleukin-2R alpha-expressing adult T-cell leukemia with Yttrium-90-labeled anti-Tac. Blood 1995; 86: 4063–75. [PubMed] [Google Scholar]
- 46.Yoshie O, Fujisawa R, Nakayama T, et al. Frequent expression of CCR4 in adult T-cell leukemia and human T-cell leukemia virus type 1-transformed T cells. Blood 2002; 99: 1505–11. [DOI] [PubMed] [Google Scholar]
- 47.Ishida T, Jo T, Takemoto S, et al. Dose-intensified chemotherapy alone or in combination with mogamulizumab in newly diagnosed aggressive adult T-cell leukaemia-lymphoma: a randomized phase II study. British Journal of Haematology 2015; 169: 672–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ysebaert L, Morschhauser F. Enzastaurin hydrochloride for lymphoma: reassessing the results of clinical trial in light of recent advances in the biology of B-cell malignancies Expert Opinion in Investigational Drugs 2011; 20: 1167–74. [DOI] [PubMed] [Google Scholar]
- 49.Goekjian PG, Jirousek MR. Protein kinase c inhibitors as novel anticancer drugs. Expert Opinion in Investigational Drugs 2001; 10: 2117–40. [DOI] [PubMed] [Google Scholar]
- 50.Cherian MA, Olson S, Sundaramoorthi H, et al. An activating mutation of IRF4 unique to adult T cell leukemia. Journal of Biolgical Chemistry 2018; 293: 6844–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ramos JC, Ruiz P, Ratner L, et al. IRF-4 and c-Rel expression in antiviral-resistant adult T-cell leukemia/lymphoma. Blood 2007; 109: 3060–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou T, Schmidt J, Fleming R, Kim Y, MacLeod AR. Therapeutic targeting of interferon regulatory factor 4 with next generation antisense oligonucleotides produces robust in vivo antitumor activity in preclinical models of multiple myeloma. American Society for Hematology; 2017. [Google Scholar]
- 53.Lu G, Middleton RE, Sun H, et al. The myeloma drug lenalidomide promotes the cereblon-dependent destruction of Ikaros proteins. 343 2014; (305–309). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lopez-Girona A, Mendy D, Ito T, et al. Cereblon is a direct protein target for immunomodulatory and antiproliferative activities of lenalidomide and pomalidomide. Leukemia 2012; 26: 2326–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nakagawa M, Shaffer AL, Ceribelli M, et al. Targeting the HTLV-1-regulated BATF3/IRF4 transcriptional network in adult T cell leukemia/lymphoma. Cancer Cell 2018; 34: 286–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hajimirza A, Emadali A, Gauthier A, Casasnovas O, Gressin R, Callanan MB. BET family protein BRD4: an emerging actor in NFkB signaling in inflammation and cancer. Biomedicine 2018; 6: E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fujikawa D, Nakagawa S, Hori M, et al. Polycomb-dependent epigenetic landscape in adult T-cell leukemia. Blood 2016; 127: 1790–802. [DOI] [PubMed] [Google Scholar]
- 58. https://viralzone.expasy.org/60?outline=all_by_species.