Abstract
Background: Metastasis to the thyroid gland or nonthyroid malignancy (NTM) is rarely an indication for thyroidectomy and constitute 1-3 % of all thyroid carcinomas. NTM has a poor prognosis, due to the advanced stage of the primary tumor. This study aimed to present the incidence, clinical characteristics, and treatment outcome of NTM in a single, high volume center.
Case series: We retrospectively analyzed all patients who had undergone thyroidectomy at the Center for Endocrine Surgery in Belgrade, during the period from 1995 to 2015. Out of 13,385 patients who were submitted to thyroidectomy, 3,344 (24.2 %) patients had thyroid malignancy. The diagnosis of NTM, based on the histopathological findings, was found in ten patients (0.075 % of all patients who had thyroid surgery, i.e., in 0.3 % of patients with thyroid cancer), with a mean age of 59.5 years. The most frequent primary tumor location in NTM was kidney in four patients, esophagus in two patients, and pharynx, breast and lungs (one case each). Total thyroidectomy was performed in four patients and lobectomy in two patients. Mean survival time following thyroid surgery was 43.2 months.
Conclusion: NTM are uncommon, and their prognosis is generally poor and depends on the characteristics of the primary tumor. Nevertheless, in selected cases, surgical treatment of NTM should be considered. HIPPOKRATIA 2018, 22(3): 137-140.
Keywords: Thyroid gland, thyroid malignancy, metastasis, nonthyroid malignancy, survival
Introduction
Although metastasis to the thyroid gland or nonthyroid malignancy (NTM) rarely represents the main indication for thyroid surgery, the true incidence of metastasis to the thyroid gland is not so uncommon. NTMs constitute 1-3 % of all thyroid carcinomas1,2. On the other hand, autopsy studies conducted during the mid-twentieth century have shown that the incidence of NTM varies in a range from 1.9 to 24 % in patients with some other types of malignances3,4. This discrepancy may be explained by the fact that in the vast majority of cases NTMs found are, in fact, micrometastases. In contrast to primary thyroid carcinomas, which are characterized by good prognosis in most cases, NTM has a poor prognosis, since it represents an advanced stage of a distant primary tumor.
The thyroid gland can be affected by a nonthyroid malignancy by two pathways: i) direct infiltration (local spreading) from the surrounding organs (usually the esophagus, pharynx, and larynx) and ii) metastasizing from distant sites (mainly kidney, lungs, breast, and gastrointestinal tract)5.
Patients are usually subjected to thyroid surgery for metastatic disease with NTM previously diagnosed by fine needle aspiration biopsy (FNAB). However, in some cases, the diagnosis of NTM is established after thyroidectomy, by definitive histopathology analysis. Due to the relatively low incidence of NTM, there is no adequate consensus regarding the treatment of these patients. The majority of expert opinions expressed, agree that NTM should be surgically treated if that is the only detectable metastasis, and the tumor can be safely resected5.
This study aimed to present the incidence, clinical characteristics, and treatment outcome of NTM in a single, high volume center, and to analyze literature data dealing with this topic.
Case series
In this study, we retrospectively analyzed all patients who had undergone thyroid surgery at the Center for Endocrine Surgery in Belgrade, during the period from 1995 to 2015. Patients with a confirmed diagnosis of thyroid malignancy were identified based on the results of the histopathology analyses. According to the definitive histopathology results, patients with the diagnosis of NTM were particularly reviewed and included in the study. General characteristics (information regarding age and gender), characteristics of the tumor (location of the primary tumor, clinical presentation of the disease and the metastatic profile - the timing, number, and location of metastases), as well as survival time, interval from diagnosis of primary tumor to thyroid surgery, follow-up and treatment outcome were obtained from the database and by interview. When NTM was diagnosed, patients were referred to the oncologists specialized to the care of the primary tumor, in order to decide regarding further or adjuvant treatment (postoperative radiotherapy and/or chemotherapy).
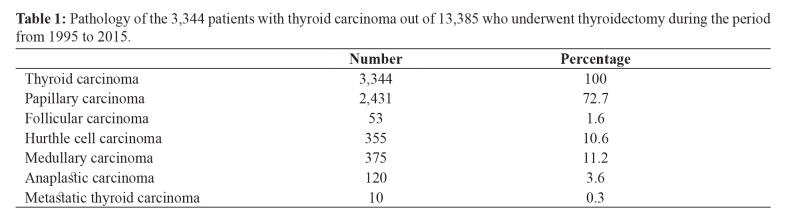
During the study period, a total of 13,385 patients were submitted to surgery for thyroid pathology at our Institution. Out of them, 3,344 patients (24.2 %) had thyroid cancer, confirmed by definitive histopathological analyses (not including patients with micropapillary thyroid carcinoma). NTMs were found in ten patients; 0.075 % of all patients who underwent thyroid surgery and 0.3 % of patients with thyroid cancer (Table 1).
Table 1. Pathology of the 3,344 patients with thyroid carcinoma out of 13,385 who underwent thyroidectomy during the period from 1995 to 2015.
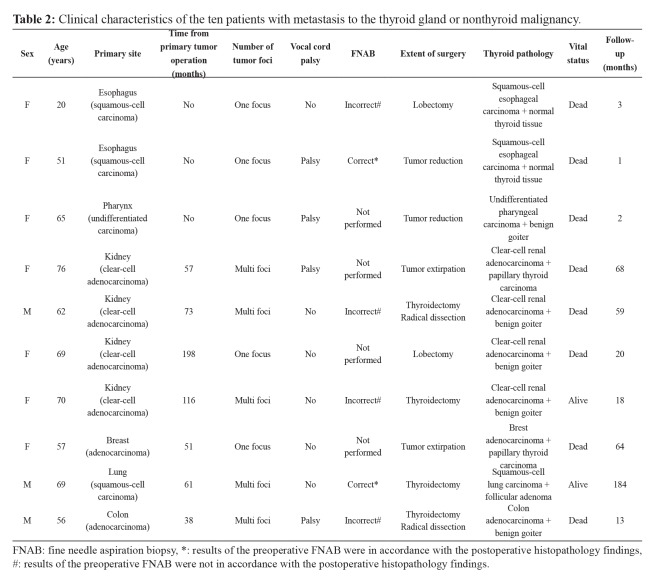
NTM patients had a mean age of 59.5 (range 20-76) years, at the time of thyroid surgery, and the majority were females (7 of 10). In three patients, the thyroid gland was directly infiltrated by tumor spreading from nearby organs (two from the esophagus and one from pharynx), while in seven patients metastases from distant primary sites were present. The most frequent primary tumor location for these patients with distant metastases was the kidney (57 %). In three patients who were initially considered as primary thyroid tumor, the thyroidectomy was the first surgical procedure, and intraoperatively a direct tumor infiltration was found from a locally advanced esophageal or pharyngeal carcinoma; overall survival in these patients was very short, ranging from one to three months. In all seven patients who had distant metastases to the thyroid, resection of the primary tumor had been performed before the thyroid surgery. The mean time elapsed from the first operation to the thyroid surgery was 84.8 (range 38-198) months. The mean survival time following thyroid surgery was 43.2 (range 1-204) months. Two patients were still alive at the time of completion of the study (Table 2). Four patients (40 %) had unilateral vocal cord palsy preoperatively, as a result of recurrent laryngeal nerve infiltration by the tumor.
Table 2. Clinical characteristics of the ten patients with metastasis to the thyroid gland or nonthyroid malignancy.
FNAB: fine needle aspiration biopsy, *: results of the preoperative FNAB were in accordance with the postoperative histopathology findings, #: results of the preoperative FNAB were not in accordance with the postoperative histopathology findings.
Total thyroidectomy was performed in four patients and lobectomy in two patients. In two patients, thyroidectomy had been previously performed due to papillary thyroid cancer and metastases developed in local recidivism. In two patients, a radical operation could not be safely achieved, so reduction of the tumor was done. Neck dissection was not performed in any case. External beam radiotherapy was postoperatively administered in a patient with metastasis from lung carcinoma.
Half of the patients had metastatic cancer with a sole focus in the thyroid gland. An FNAB was performed preoperatively in 60 % and in two out of these six patients (33 %), the cytological diagnosis was correct, and the existence of a tumor originating from a distant site outside the thyroid gland, was suspected. Intraoperative frozen sections were not utilized, as we do not routinely use such analyses in thyroid surgery at our Institution.
Benign euthyroid goiter was present in one-half of all cases with NTM. Thyroid gland was normal in two cases, in those patients who had direct infiltration by tumor originating from nearby organs. Two patients had previously been operated due to papillary thyroid carcinoma and NTM developed in the remains of thyroid tissue.
Discussion
The incidence of NTM in our study was 0.3 % among the patients operated due to thyroid cancer. The true incidence, i.e., the overall number of patients who present metastases to the thyroid is probably far more substantial, but the precise number can only be evaluated with autopsy studies. The percentage of patients with NTM among patients operated due to thyroid cancer was found slightly higher in previous studies, at 1.4-3 %1,2,6,7.
In our study, most NTM (80 %) developed on the field of an already altered thyroid gland. Only two cases with normal thyroid gland had direct infiltration by tumor originating from nearby organs. Thus it confirms the hypothesis that metastases are more likely to develop in already pathologically altered thyroid1,2.
More than half of patients with distant metastases operated in our study, were patients with metastases from kidneys (four patients), and this is in accordance with existing literature data; the most common sources of metastases to the thyroid are kidneys, followed by lungs, and breast. Somewhat less frequently NTM can originate from the gastrointestinal tract, melanomas, and genitourinary tract. Russell et al analyzed in 2016 the literature during the preceding 20 years and found 818 patients with NTM. The most commonly reported primary site of NTM was kidney (35.8 %) then lungs, and gastrointestinal tract8. A multicenter study from Italy, conducted in 2008, also found that NTM most commonly originates from kidney, in 60 % of cases7.
In order to adequately estimate a preoperative diagnosis, FNAB should be utilized. More than half of the patients in the present study had a preoperative FNAB performed, and the findings were accurate in 33 %. According to the literature, the percentage of correct cytology diagnoses is very heterogeneous and depends vastly on the primary tumor site. The lowest percentage of correct diagnoses was encountered to NTM arising from the esophagus, about 50 % while the highest percentage of correct diagnoses was in NTM from the breast. Also, a very high percentage of correct diagnosis can be detected in cases with metastases originating from the lungs and colon; about 90 %1,9,10.
The mean survival time after thyroid surgery in patients with NTM from kidneys was found in our study to be 55.5 months. In a large multicenter study from Germany and Austria, the mean survival time of 45 patients with NTM from kidneys was 71 months, with a 5-year and 10-year survival rate of 51 % and 20 %, respectively11. In other studies, the mean survival time was in a range from 27 to 56.4 months12,13.
Among our patients, there was one case with metastasis of lung squamous cell carcinoma to the thyroid gland. The particular importance of this case is highlighted by the fact that this patient is still alive and without any sign of disease, 17 years after the thyroidectomy, and 22 years after lung lobectomy. According to the literature, 8.3 % of NTM originate from lung cancers1. The most common type of lung carcinoma that can give NTM is squamous cell carcinoma, while the other types rarely metastasize to the thyroid14,15. Survival rates of patients with NTM that originate from the lungs are significantly shorter compared to survival rates of patients with NTM arising from kidneys and breast. This is attributed to the more aggressive nature of the primary disease.
Colorectal cancer represents one of the most common cancers in human pathology, with 30-40 % of patients having distant metastases at the time of initial diagnosis. However, metastases to the thyroid are relatively rare; only 10.4 % of all NTM originate from the colon1,16. In our series, one patient had NTM that originated from the colon, with relatively short survival time; 13 months following thyroid surgery8.
It is questionable whether surgery for NTM is justified. Furthermore, the extent of surgery is a matter of debate. Russell et al in a large meta-analysis compared survival time of NTM patients with and without thyroid surgery8. They have shown that survival time is longer in patients who had undergone thyroid surgery. The most significant difference regarding survival length was evident in patients with renal cancer (6 vs 27 months) than in patients with lung, and gastrointestinal cancers8. On the other hand, according to that study, as well as according to the study by Bautner et al, no differences were observed between patients who underwent total thyroidectomy and operations less than total thyroidectomy8,13. This supports the argument that operation less than total thyroidectomy (i.e., lobectomy) can be performed if the contralateral thyroid lobe has no evident pathology or if the resection margins are negative8.
According to the previously mentioned meta-analysis by Russell et al, longer survival time is associated with a more extended period between surgery of the primary tumor and thyroid surgery for the NTM, and this is probably explained by the fact that tumors with indolent character have better survival1,8.
Conclusions
Since metastases to the thyroid gland are uncommon, even highly specialized endocrine surgeons rarely encounter these tumors. Surgical treatment of NTM should be considered, especially in selected cases, i.e., when thyroid metastases are the only known metastases.
Conflict of interest
None declared by Authors.
References
- 1.Chung AY, Tran TB, Brumund KT, Weisman RA, Bouvet M. Metastases to the thyroid: a review of the literature from the last decade. Thyroid. 2012;22:258–268. doi: 10.1089/thy.2010.0154. [DOI] [PubMed] [Google Scholar]
- 2.Papi G, Fadda G, Corsello SM, Corrado S, Rossi ED, Radighieri E, et al. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf) 2007;66:565–571. doi: 10.1111/j.1365-2265.2007.02773.x. [DOI] [PubMed] [Google Scholar]
- 3.Nixon IJ, Coca-Pelaz A, Kaleva AI, Triantafyllou A, Angelos P, Owen RP, et al. Metastasis to the Thyroid Gland: A Critical Review. Ann Surg Oncol. 2017;24:1533–1539. doi: 10.1245/s10434-016-5683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cordes M, Kuwert T. Metastases of non-thyroidal tumors to the thyroid gland: a regional survey in middle franconia. Exp Clin Endocrinol Diabetes. 2014;122:273–276. doi: 10.1055/s-0034-1372623. [DOI] [PubMed] [Google Scholar]
- 5.Montero PH, Ibrahimpasic T, Nixon IJ, Shaha AR. Thyroid metastasectomy. J Surg Oncol. 2014;109:36–41. doi: 10.1002/jso.23452. [DOI] [PubMed] [Google Scholar]
- 6.Nakhjavani MK, Gharib H, Goellner JR, van Heerden JA. Metastasis to the thyroid gland. A report of 43 cases. Cancer. 1997;79:574–578. doi: 10.1002/(sici)1097-0142(19970201)79:3<574::aid-cncr21>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 7.Calzolari F, Sartori PV, Talarico C, Parmeggiani D, Beretta E, Pezzullo L, et al. Surgical treatment of intrathyroid metastases: preliminary results of a multicentric study. Anticancer Res. 2008;28:2885–2888. [PubMed] [Google Scholar]
- 8.Russell JO, Yan K, Burkey B, Scharpf J. Nonthyroid Metastasis to the Thyroid Gland: Case Series and Review with Observations by Primary Pathology. Otolaryngol Head Neck Surg. 2016;155:961–968. doi: 10.1177/0194599816655783. [DOI] [PubMed] [Google Scholar]
- 9.Cichoń S, Anielski R, Konturek A, Barczyński M, Cichoń W. Metastases to the thyroid gland: seventeen cases operated on in a single clinical center. Langenbecks Arch Surg. 2006;391:581–587. doi: 10.1007/s00423-006-0081-1. [DOI] [PubMed] [Google Scholar]
- 10.Rahman M, Okada AR, Guan K, Tauchi-Nishi P. Metastatic neoplasms to the thyroid diagnosed by fine-needle aspiration/core needle biopsy: Clinicopathologic and cytomorphologic correlation. Cytojournal. 2017;14:16. doi: 10.4103/cytojournal.cytojournal_50_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iesalnieks I, Winter H, Bareck E, Sotiropoulos GC, Goretzki PE, Klinkhammer-Schalke M, et al. Thyroid metastases of renal cell carcinoma: clinical course in 45 patients undergoing surgery. Assessment of factors affecting patients’ survival. Thyroid. 2008;18:615–624. doi: 10.1089/thy.2007.0343. [DOI] [PubMed] [Google Scholar]
- 12.Cesaretti M, Trotta M, Varaldo E, Ansaldo G, Leale I, Borgonovo G. Metastases to the thyroid gland from renal cancer. Tumori. 2013;99:e107–e110. doi: 10.1177/030089161309900327. [DOI] [PubMed] [Google Scholar]
- 13.Beutner U, Leowardi C, Bork U, Lüthi C, Tarantino I, Pahernik S, et al. Survival after renal cell carcinoma metastasis to the thyroid: single center experience and systematic review of the literature. Thyroid. 2015;25:314–324. doi: 10.1089/thy.2014.0498. [DOI] [PubMed] [Google Scholar]
- 14.Osawa M, Takigawa N, Kiura K, Ichimura K, Matsuoka J, Hotta K, et al. Isolated metastasis of lung cancer to the thyroid gland. Lung Cancer. 2007;58:156–158. doi: 10.1016/j.lungcan.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 15.Can AS, Köksal G. Thyroid metastasis from small cell lung carcinoma: a case report and review of the literature. J Med Case Rep. 2015;9:231. doi: 10.1186/s13256-015-0707-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kolligs FT. Diagnostics and Epidemiology of Colorectal Cancer. Visc Med. 2016;32:158–164. doi: 10.1159/000446488. [DOI] [PMC free article] [PubMed] [Google Scholar]