Abstract
Introduction: Matrix metalloproteinases (MMPs) are a family of zinc-dependent proteinases involved in remodeling the extracellular matrix. Tissue inhibitors of metalloproteinases (TIMPs) are a family of four proteins that act to limit the degradative actions of MMPs. Chronic kidney disease (CKD) and acute kidney injury (AKI) are public health problems worldwide, the prevalence of which has been increasing. Recent concept considers MMPs and TIMPs as critical factors before the onset of microalbuminuria, as well as accelerating factors associated with the breakdown of the glomerular basement membrane, renal scarring, and fibrosis during the progression of kidney diseases. Here we reviewed studies of the expression of MMPs and TIMPs in humans, using as clinical samples serum, plasma, and urine, with a focus on their potential role as molecular markers in CKD and AKI, as non-invasive markers.
Material and methods: We used as data sources, studies at Medline database using combinations of the following keywords: CKD, AKI, MMP, TIMP, serum, plasma, and urine.
Results: Evidence suggests that MMPs/TIMPs could be potential targets for therapeutic intervention in kidney diseases; future studies should attempt to improve the diagnostic or prognostic power of these families.
Discussion: Considering published guides, such as biospecimen reporting for improved study quality (BRISQ), strengthening the reporting of observational studies in epidemiology (STROBE), an updated list of essential items for reporting diagnostic accuracy studies (STARD), transparent reporting of a multivariate prediction model for individual prognosis or diagnosis (TRIPOD), and on the studies reviewed here, we have adapted published recommendations and proposed other news in order to enhance the transparency and quality of MMPs/TIMPs research in CKD and AKI. This review reinforces the complexities of MMPs/TIMPs in the pathobiology of the kidney and the need for well-designed and transparent biomedical studies. HIPPOKRATIA 2018, 22(3): 99-104.
Keywords: Matrix metalloproteinases, tissue inhibitors of metalloproteinases, chronic kidney disease, acute kidney injury
Introduction
Chronic kidney disease (CKD) is defined as abnormalities in the kidney structure or function, present for three or more months, with implications for health. It is classified based on its cause, glomerular filtration rate (GFR) category, and albuminuria category1. The GFR is widely accepted as the best overall index of the kidney’s function in terms of health and disease; however, it is difficult to measure and is commonly estimated from the serum creatinine (SCr)1,2.
The development of CKD eventually progresses to end-stage renal disease and leads to irreversible loss of renal function1. Most patients with reduced renal function are not identified in the stages at which it is possible to slow down, or even prevent, the progression of CKD1. Chronicity is not synonymous of irreversibility; in some cases, CKD can be reversible1.
Acute kidney injury (AKI) is defined as an increase in SCr by ≥0.3 mg/dl within a period of 48 hours or an increase in SCr to ≥1.5 times the baseline, that is known or presumed to have occurred within the previous seven days, or a urine volume <0.5 ml/kg/h for six hours2. AKI is a predictor of immediate and long-term adverse outcomes and is a significant risk factor for CKD2. As with CKD, AKI is amenable to early detection and possible prevention1,2.
Matrix metalloproteinases (MMPs) are a family of zinc-dependent proteinases that are involved in the remodeling of the extracellular matrix (ECM). MMPs are multidomain enzymes, generally consisting of a pro-domain, a catalytic domain, a hinge region, and a hemopexin-like domain3. To date, over 20 mammalian MMPs have been described and are subdivided into collagenases, gelatinases, stromelysins, matrilysins, membrane type, and “other MMPs”4. MMPs are traditionally conceived as antifibrotic players in the conventional view of progression; however, recent concept considers MMPs as compensatory factors before the onset of microalbuminuria and as accelerating factors associated with the breakdown of the glomerular basement membrane (GBM), renal scarring, and fibrosis during the progression of kidney diseases (KD)5,6.
Tissue inhibitors of metalloproteinases (TIMPs) are a family of four proteins that their action limits the degradative actions of MMPs. TIMPs interact with MMP active sites to block reversible their proteolytic activity7. TIMPs have activities independent of MMPs, including cell growth, migration, and differentiation8. Here, we review MMPs and TIMPs expression studies in serum, plasma, and urine, with a focus on their potential role as molecular markers in CKD and AKI. We included diabetes mellitus (DM) and hypertension studies since these diseases are among the most frequent causes of CKD1.
Methods
Search strategy
The Medline database was searched on the 28 February 2018, using combinations of the following key words: CKD, AKI, MMP, TIMP, serum, plasma, and urine. A total of 284 articles were obtained. The recommendations of the PRISMA group were followed in terms of identification, screening, eligibility, and inclusion criteria9.
Eligibility, inclusion, and exclusion criteria
The abstract of each article was carefully studied to verify the following eligibility criteria: i) English or Spanish language, ii) original or primary research concerning human renal function, iii) expression of MMPs/TIMPs families, and iv) CKD, AKI, DM or hypertension. The criteria for exclusion from consideration were: i) number of subjects in the group(s) of nine or less cases, ii) DNA sequencing study only, iii) renal transplant study only, and iv) studies performed in patients with a mean or median age under 18 years. Applying these criteria, 247 studies were discarded, and 37 were reviewed to verify the following inclusion criteria: i) reference to the sex and age of the groups, ii) agreement of data in the text and tables. Exclusion criteria were featuring data that, in our judgment, were duplicated. After applying these criteria, 17 studies were included, and a further 37 studies were incorporated into the introduction and conclusions. The description and discussion of these studies include the original name of the study groups, according to their authors.
MMPs and TIMPs in CKD and AKI
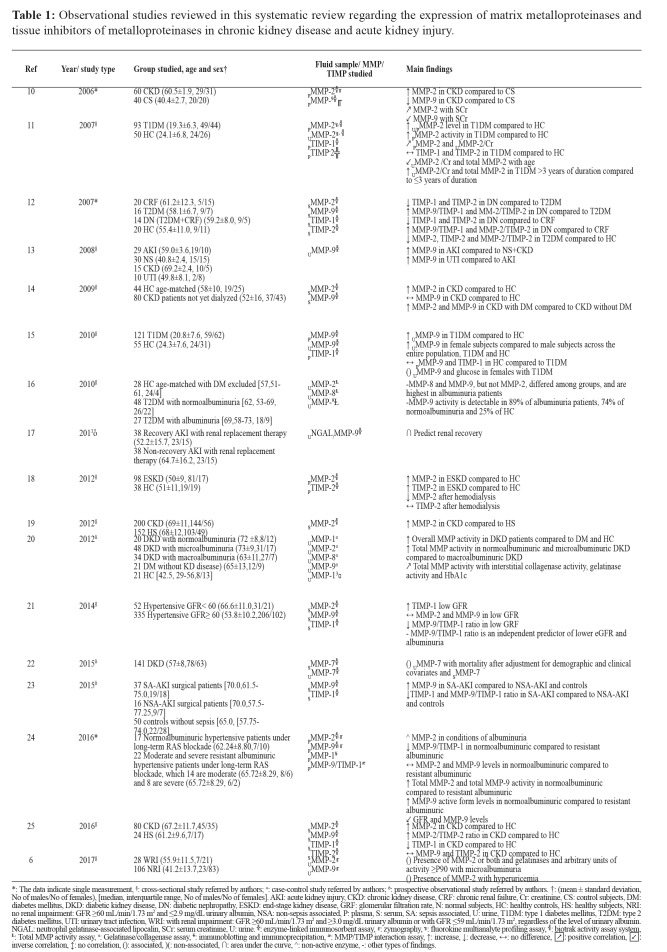
While the activity and the spatial and temporal expression of MMP/TIMP families in the human kidney have not been thoroughly characterized, the observational studies reviewed here demonstrated dysregulation of these families in a wide variety of kidney disorders in different fluids (Table 1).
Table 1. Observational studies reviewed in this systematic review regarding the expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in chronic kidney disease and acute kidney injury.
*: The data indicate single measurement, §: cross-sectional study referred by authors; «: case-control study referred by authors; ȍ: prospective observational study referred by authors. †: (mean ± standard deviation, No of males/No of females), [median, interquartile range, No of males/No of females]. AKI: acute kidney injury, CKD: chronic kidney disease, CRF: chronic renal failure, Cr: creatinine, CS: control subjects, DM: diabetes mellitus, DKD: diabetic kidney disease, DN: diabetic nephropathy, ESKD: end-stage kidney disease, GRF: glomerular filtration rate, N: normal subjects, HC: healthy controls, HS: healthy subjects, NRI: no renal impairment: GFR ≥60 mL/min/1.73 m2 and ≤2.9 mg/dL urinary albumin, NSA: non-sepsis associated, P: plasma, S: serum, SA: sepsis associated, U: urine, T1DM: type 1 diabetes mellitus, T2DM: type 2 diabetes mellitus, UTI: urinary tract infection, WRI: with renal impairment: GFR ≥60 mL/min/1.73 m2 and ≥3.0 mg/dL urinary albumin or with GFR ≤59 mL/min/1.73 m2, regardless of the level of urinary albumin. NGAL: neutrophil gelatinase-associated lipocalin, SCr: serum creatinine, U: urine. ╬: enzyme-linked immunosorbent assay, ╓: zymography, ╗: fluorokine multianalyte profiling assay, ╣: biotrak activity assay system, Ⱡ: Total MMP activity assay, ɞ: Gelatinase/collagenase assay, ¥: immunoblotting and immunoprecipitation, æ: MMP/TIMP interaction assay, ↑: increase, ↓: decrease, ↔: no difference, ↗: positive correlation, ↙: inverse correlation, ↕: no correlation, (): associated, )(: non-associated, ∩: area under the curve, ^: non-active enzyme, -: other types of findings.
Most of the studies focused on the levels of MMP-2 and MMP-9 quantified using enzyme-linked immunosorbent assay (ELISA) (Table 1); however, for KD type, fluid analyzed [in this case serum (S)] and formula used to calculate the GFR (Modification of Diet in Renal Disease), only three studies were comparable: Peiskerova et al14 analyzed SMMP-2 and SMMP-9 in non-dialyzed patients with CKD at stages 1-5; Smith et al19 investigated SMMP-2 in predominantly male and hypertensive pre-dialysis CKD patients with stages 3 and 4; and Gluba-Brzozka et al25 determined SMMP-2 and SMMP-9 in CKD patients with stages 1-5, where patients at stage 5 had mean dialysis time of 27.9 months. These studies also quantified levels of gelatinase, compared to those of healthy subjects14,19 or volunteers without CKD25, noting a consistent increase in the levels of SMMP-2 in CKD, compared to the reference group, while for SMMP-9 they report no differences. These data are of great interest since they are the product of studies conducted in different countries and patients diagnosed with CKD through diverse etiologies, at different stages of the disease, with a wide variety of comorbidities and under different schemes of treatment14,19,25.
Moreover, other studies report that plasma (P) MMP-2 (PMMP-2) is upregulated in CKD10, type 1 DM (T1DM)11 and end-stage kidney disease18, compared to control subjects10 or healthy controls (HC)11,18. Upregulation of PMMP-2 is also observed in normoalbuminuric hypertensive patients, compared to albuminuric resistant hypertensive patients24. On the other hand, urinary (U) MMP-2 (UMMP-2) is proposed as a marker for elevated risk of hyperglycemia, hyperfiltration, and microalbuminuria in patients with T1DM11. In subjects with renal impairment living at high altitude UMMP-2 is also associated with microalbuminuria6.
The fraction sMMP-9 associated with TIMP-1, among other findings, has been reported as a predictor of low GFR in hypertensive patients21, upregulated in diabetic nephropathy compared to T2DM12 and chronic renal failure12, but down-regulated in sepsis-associated AKI, compared to non-sepsis-associated AKI and controls23.
Data regarding UMMP-9 concentration analyzed in patients with AKI, as an absolute value or normalized to UCreatinine, indicated that the results do not markedly differ, although authors reported that normalizing to UCreatinine is less than ideal due to its non-steady state balance in those patients13. An elevated UMMP-9 level could function as a molecular marker of AKI13, T1DM15, and urinary tract infection (UTI)13. Differential levels according to gender have been reported for UMMP-9 in T1DM15 and HC15.
Different proportions have also been observed in detection of the activity of UMMP-916 and PMMP-924 according to the albuminuria category in T2DM and hypertensive patients, respectively. Most of the studies have likely focused on MMP-2 and MMP-9, due to their action on col-IV, the main ECM protein in the GBM, tubular basement membrane, and mesangium5,26. On the other hand, UMMP-8 in 24-hour collection is upregulated in T2DM and its levels depend on the albuminuria category16.
Finally, the only study in which the outcome was death states that UMMP-7 is associated with an increased risk of mortality in patients with T2DM and diabetic kidney disease22. This association remains robust after adjustment of demographic and clinical covariates, while SMMP-7 is not associated with mortality and does not attenuate the association of UMMP-722.
Since the evidence suggests that progressive glomerulosclerosis is characterized by a profound shift in ECM turnover27 and that MMPs/TIMPs could be potential targets for therapeutic intervention in KD28, future studies should attempt to improve the diagnostic or prognostic power of these genetic families through methods to optimize reproducibility, as well as increased sample sizes and greater numbers of MMPs/TIMPs analyzed.
Recommendations to enhance the transparency and quality of MMPs/TIMPs research in CKD and AKI
In this sense, we make some recommendations regarding procurement, storage and quality assurance of frozen biospecimens29,30 and the guides STROBE31, STARD32, TRIPOD33, adapting these, in some cases, to studies in humans with CKD or AKI:
1. Describe the study design33 and sample size calculation31,33. Some statistical methods for calculating confidence intervals for relative risk and standardized ratios are for large sample approximations and are unreliable for studies with less than 20 cases34.
2. Describe the criteria of inclusion, exclusion, and elimination of all the groups and how subjects flow through the study; a diagram may be helpful33,35. Where applicable, specify whether stratification or matching was carried out. If exist indicate criteria of exclusion about habits, illnesses, and treatments. Note that PMMP-9 is up-regulated in tobacco smokers36 and that significant change in its level is observed 12 weeks after smoking cessation37.
3. Specify the period of recruitment and the population base, e.g., primary care, secondary care, general, rural or urban population33.
4. Indicate whether there is control of the conditions that affect pre-analytical and analytical urinary albumin to creatinine ratio, such as UTI, exercise and patients with amputations, which muscle mass could which be lower1,2.
5. Indicate the formula used to calculate GFR.
6. Provide minimum anthropometric data, such as body mass index and waist size, and minimum sociodemographic information, e.g., sex, age, education level, economic level, and access to health services. Note that the term “race” is controversial in biomedical studies38,39. In human genetic research, the use of biological concepts of race has been described as “problematic at best and harmful at worst”40. Smart et al argue that “it seems currently unlikely that a genetic concept of race and ethnicity will ever be portable enough to wholly supplant a socio-political one”39.
7. Indicate whether there are differences between the age and sex proportions in the study groups. Note that renal MMP expression appears to be sex- and age-dependent15,41.
8. Refer to the duration of the illness32or, where appropriate, indicate that this is unknown. Refer similarly to symptoms and comorbidities32. In the case of patients undergoing dialysis treatment, indicate the type and duration.
9. Above all, in patients with DM, indicate the glycemic control.
10.Identify the use of certain antibiotics that alter the expression of MMPs, such as doxycycline and minocycline42,43.
11. Indicate the initial process by which the biospecimens were stabilized during collection; type of long-term preservation, the constitution of preservative time or range between biospecimens acquisition and distribution or analysis and storage duration13,30,43-45. Where applicable, the number of freeze/thaw cycles of the biospecimens6,13,46,47.
12. In studies with clinical blood samples, indicate the fluid type analyzed as well as the preservative, given that some reports indicate discrepancies between levels of certain MMPs/TIMPs in serum and plasma, explained by additional unspecific release during the collection of serum47,48 and/or by the additive type48-50.
13. In studies with clinical urine samples, indicate the type: 24-hour collection, minuted; sample isolated by spontaneous micturition in the morning or random, mid-stream programmed sample, obtained via a probe through a supra-pubic puncture. Indicate whether biospecimens with hematuria were excluded to avoid false positives6,51. Indicate whether the analyses were with cell-free urine20.
14. Indicate whether the assay used has been validated in the fluid studied11. Specify whether the assay was performed blinded. Assay methods should be reported completely and transparently with a level of detail that would enable another laboratory to reproduce the measurement technique35. It may be helpful to use supplementary material.
15. Studies utilizing ELISA should include the limit of detection, the coefficients of intra- and inter-assay variation.
16. Studies utilizing gel zymography should indicate the limit of detection, concentration, and type of chelant used in the control gels or, where applicable, indicate that they were not conducted52.
17. Indicate whether the analyses were conducted with the absolute values of the MMPs/TIMPs or whether these were normalized.
Conclusions
MMPs and TIMPs are essential components in many physiological and pathological processes due to their ability to remodel ECM components53. The ECM is not a mere scaffold for cells; it is a versatile and dynamic compartment that harbors cryptic biological functions that can be revealed on proteolysis53. ECM is involved in modulating cell proliferation, migration, differentiation, and apoptosis28,46,54. MMPs have been associated with renal hypertrophy, renal scarring, tubular cell proliferation, and fibrosis4. This sheds new light on the interplay between ECM, cells, and MMPs/TIMPs in renal pathophysiology.
Finally, it is important to highlight that studies in animal models were excluded from this review due to the complexity of MMPs/TIMPs in the kidney and because the expression of these families has been proposed as likely to be species-specific3. Moreover, experimental models do not always recapitulate the clinical findings of MMPs/TIMPs4,28. Collectively, these data highlight the complexities of MMPs/TIMPs in the pathophysiology of KD and the continued need for biomedical studies. We hope that these recommendations will help the scientific community in planning future research.
Conflict of interest
Authors declare no conflict of interest.
Acknowledgement
A support was received (POA 2017) by the Instituto de Salud Pública, Universidad Veracruzana.
References
- 1.Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kindey Diseases. Kidney Int Suppl. 2013;3:1–150. doi: 10.1038/ki.2013.243. Available at: https://kdigo.org/wp-content/uploads/2017/02/KDIGO_2012_CKD_GL.pdf, date accessed:31/05/2018. [DOI] [PubMed] [Google Scholar]
- 2.Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl. 2012;2:1–138. Available at: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-AKI-Guideline-English.pdf, date accessed: 31/05/2018. [Google Scholar]
- 3.Catania JM, Chen G, Parrish AR. Role of matrix metalloproteinases in renal pathophysiologies. Am J Physiol Renal Physiol. 2007;292:F905–F911. doi: 10.1152/ajprenal.00421.2006. [DOI] [PubMed] [Google Scholar]
- 4.Thrailkill KM, Clay Bunn R, Fowlkes JL. Matrix metalloproteinases: their potential role in the pathogenesis of diabetic nephropathy. Endocrine. 2009;35:1–10. doi: 10.1007/s12020-008-9114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dimas G, Iliadis F, Grekas D. Matrix metalloproteinases, atherosclerosis, proteinuria and kidney disease: Linkage-based approaches. Hippokratia. 2013;17:292–297. [PMC free article] [PubMed] [Google Scholar]
- 6.Hernández-Hernández ME, Morales-Romero J, Sampieri CL, Luna Lozano DJ, Valencia Lezama IDC, Muñoz Contreras MJ, et al. Association of Urinary Activity of MMP-2 with Microalbuminuria in an Isolated Sample of Subjects Living in High Altitude Rural Locations in Mexico. High Alt Med Biol. 2017;18:209–218. doi: 10.1089/ham.2016.0144. [DOI] [PubMed] [Google Scholar]
- 7.Lambert E, Dassé E, Haye B, Petitfrère E. TIMPs as multifacial proteins. Crit Rev Oncol Hematol. 2004;49:187–198. doi: 10.1016/j.critrevonc.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Brew K, Nagase H. The tissue inhibitors of metalloproteinases (TIMPs): an ancient family with structural and functional diversity. Biochim Biophys Acta. 2010;1803:55–71. doi: 10.1016/j.bbamcr.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang HR, Yang SF, Li ML, Lin CC, Hsieh YS, Lian JD. Relationships between circulating matrix metalloproteinase-2 and -9 and renal function in patients with chronic kidney disease. Clin Chim Acta. 2006;366:243–248. doi: 10.1016/j.cca.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Thrailkill KM, Bunn RC, Moreau CS, Cockrell GE, Simpson PM, Coleman HN, et al. Matrix metalloproteinase-2 dysregulation in type 1 diabetes. Diabetes Care. 2007;30:2321–2326. doi: 10.2337/dc07-0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rysz J, Banach M, Stolarek RA, Pasnik J, Cialkowska-Rysz A, Koktysz R, et al. Serum matrix metalloproteinases MMP-2 and MMP-9 and metalloproteinase tissue inhibitors TIMP-1 and TIMP-2 in diabetic nephropathy. J Nephrol. 2007;20:444–452. [PubMed] [Google Scholar]
- 13.Han WK, Waikar SS, Johnson A, Betensky RA, Dent CL, Devarajan P, et al. Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008;73:863–869. doi: 10.1038/sj.ki.5002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peiskerová M, Kalousová M, Kratochvílová M, Dusilová-Sulková S, Uhrová J, Bandúr S, et al. Fibroblast growth factor 23 and matrix-metalloproteinases in patients with chronic kidney disease: are they associated with cardiovascular disease? . Kidney Blood Press Res. 2009;32:276–283. doi: 10.1159/000243050. [DOI] [PubMed] [Google Scholar]
- 15.Thrailkill KM, Moreau CS, Cockrell GE, Jo CH, Bunn RC, Morales-Pozzo AE, et al. Disease and gender-specific dysregulation of NGAL and MMP-9 in type 1 diabetes mellitus. Endocrine. 2010;37:336–343. doi: 10.1007/s12020-010-9308-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Zijl NJ, Hanemaaijer R, Tushuizen ME, Schindhelm RK, Boerop J, Rustemeijer C, et al. Urinary matrix metalloproteinase-8 and -9 activities in type 2 diabetic subjects: A marker of incipient diabetic nephropathy? Clin Biochem. 2010;43:635–639. doi: 10.1016/j.clinbiochem.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Srisawat N, Wen X, Lee M, Kong L, Elder M, Carter M, et al. Urinary biomarkers and renal recovery in critically ill patients with renal support. Clin J Am Soc Nephrol. 2011;6:1815–1823. doi: 10.2215/CJN.11261210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marson BP, Lacchini R, Belo V, Dickel S, da Costa BP, Poli de Figueiredo CE, et al. Matrix metalloproteinase (MMP)-2 genetic variants modify the circulating MMP-2 levels in end-stage kidney disease. Am J Nephrol. 2012;35:209–215. doi: 10.1159/000336108. [DOI] [PubMed] [Google Scholar]
- 19.Smith ER, Tomlinson LA, Ford ML, McMahon LP, Rajkumar C, Holt SG. Elastin degradation is associated with progressive aortic stiffening and all-cause mortality in predialysis chronic kidney disease. Hypertension. 2012;59:973–978. doi: 10.1161/HYPERTENSIONAHA.111.187807. [DOI] [PubMed] [Google Scholar]
- 20.Altemtam N, Nahas ME, Johnson T. Urinary matrix metalloproteinase activity in diabetic kidney disease: a potential marker of disease progression. Nephron Extra. 2012;2:219–232. doi: 10.1159/000339645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu TY, Zhang Y, Li Y, Zhu DL, Gao PJ. The association of serum inflammatory biomarkers with chronic kidney disease in hypertensive patients. Ren Fail. 2014;36:666–672. doi: 10.3109/0886022X.2014.890002. [DOI] [PubMed] [Google Scholar]
- 22.Afkarian M, Zelnick LR, Ruzinski J, Kestenbaum B, Himmelfarb J, de Boer IH, et al. Urine matrix metalloproteinase-7 and risk of kidney disease progression and mortality in type 2 diabetes. J Diabetes Complications. 2015;29:1024–1031. doi: 10.1016/j.jdiacomp.2015.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bojic S, Kotur-Stevuljevic J, Kalezic N, Stevanovic P, Jelic-Ivanovic Z, Bilanovic D, et al. Diagnostic Value of Matrix Metalloproteinase-9 and Tissue Inhibitor of Matrix Metalloproteinase-1 in Sepsis-Associated Acute Kidney Injury. Tohoku J Exp Med. 2015;237:103–109. doi: 10.1620/tjem.237.103. [DOI] [PubMed] [Google Scholar]
- 24.Pulido-Olmo H, García-Prieto CF, Álvarez-Llamas G, Barderas MG, Vivanco F, Aranguez I, et al. Role of matrix metalloproteinase-9 in chronic kidney disease: a new biomarker of resistant albuminuria. Clin Sci (Lond) 2016;130:525–538. doi: 10.1042/CS20150517. [DOI] [PubMed] [Google Scholar]
- 25.Gluba-Brzózka A, Michalska-Kasiczak M, Franczyk B, Nocuń M, Toth P, Banach M, et al. Markers of increased atherosclerotic risk in patients with chronic kidney disease: a preliminary study. Lipids Health Dis. 2016;15:22. doi: 10.1186/s12944-016-0191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C, Li C, Gong W, Lou T. New urinary biomarkers for diabetic kidney disease. Biomark Res. 2013;1:9. doi: 10.1186/2050-7771-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dimas GG, Didangelos TP, Grekas DM. Matrix Gelatinases in Atherosclerosis and Diabetic Nephropathy: Progress and Challenges. Curr Vasc Pharmacol. 2017;15:557–565. doi: 10.2174/1570161115666170202162345. [DOI] [PubMed] [Google Scholar]
- 28.Tan RJ, Liu Y. Matrix metalloproteinases in kidney homeostasis and diseases. Am J Physiol Renal Physiol. 2012;302:F1351–F1361. doi: 10.1152/ajprenal.00037.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shabihkhani M, Lucey GM, Wei B, Mareninov S, Lou JJ, Vinters HV, et al. The procurement, storage, and quality assurance of frozen blood and tissue biospecimens in pathology, biorepository, and biobank settings. Clin Biochem. 2014;47:258–266. doi: 10.1016/j.clinbiochem.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moore HM, Kelly AB, Jewell SD, McShane LM, Clark DP, Greenspan R, et al. Biospecimen reporting for improved study quality (BRISQ) Cancer Cytopathol. 2011;119:92–101. doi: 10.1002/cncy.20147. [DOI] [PubMed] [Google Scholar]
- 31.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–1524. doi: 10.1016/j.ijsu.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 32.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527. doi: 10.1136/bmj.h5527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moons KG, Altman DG, Reitsma JB, Collins GS. New Guideline for the Reporting of Studies Developing, Validating, or Updating a Multivariable Clinical Prediction Model: The TRIPOD Statement. Adv Anat Pathol. 2015;22:303–305. doi: 10.1097/PAP.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 34.Morris JA, Gardner MJ. Calculating confidence intervals for relative risks (odds ratios) and standardised ratios and rates. Br Med J (Clin Res Ed) 1988;296:1313–1316. doi: 10.1136/bmj.296.6632.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting recommendations for tumor marker prognostic studies (REMARK): explanation and elaboration. BMC Med. 2012;10:51. doi: 10.1186/1741-7015-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ilumets H, Mazur W, Toljamo T, Louhelainen N, Nieminen P, Kobayashi H, et al. Ageing and smoking contribute to plasma surfactant proteins and protease imbalance with correlations to airway obstruction. BMC Pulm Med. 2011;11:19. doi: 10.1186/1471-2466-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sørensen LT, Toft BG, Rygaard J, Ladelund S, Paddon M, James T, et al. Effect of smoking, smoking cessation, and nicotine patch on wound dimension, vitamin C, and systemic markers of collagen metabolism. Surgery. 2010;148:982–990. doi: 10.1016/j.surg.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 38.Cooper RS. Race in biological and biomedical research. Cold Spring Harb Perspect Med. 2013;3:pii: a008573. doi: 10.1101/cshperspect.a008573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smart A, Tutton R, Martin P, Ellison GT, Ashcroft R. The standardization of race and ethnicity in biomedical science editorials and UK biobanks. Soc Stud Sci. 2008;38:407–423. doi: 10.1177/0306312707083759. [DOI] [PubMed] [Google Scholar]
- 40.Yudell M, Roberts D, DeSalle R, Tishkoff S. SCIENCE AND SOCIETY. Taking race out of human genetics. Science. 2016;351:564–565. doi: 10.1126/science.aac4951. [DOI] [PubMed] [Google Scholar]
- 41.Thrailkill KM, Kumar S, Rosenberg CK, Auten KJ, Fowlkes JL. Characterization of matrix metalloproteinases in human urine: alterations during adolescence. Pediatr Nephrol. 1999;13:223–229. doi: 10.1007/s004670050597. [DOI] [PubMed] [Google Scholar]
- 42.Fiotti N, Altamura N, Moretti M, Wassermann S, Zacchigna S, Farra R, et al. Short term effects of doxycycline on matrix metalloproteinases 2 and 9. Cardiovasc Drugs Ther. 2009;23:153–159. doi: 10.1007/s10557-008-6150-7. [DOI] [PubMed] [Google Scholar]
- 43.Anderson R, Tintinger G, Cockeran R, Potjo M, Feldman C. Beneficial and Harmful Interactions of Antibiotics with Microbial Pathogens and the Host Innate Immune System. Pharmaceuticals (Basel) 2010;3:1694–1710. doi: 10.3390/ph3051694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rouy D, Ernens I, Jeanty C, Wagner DR. Plasma storage at -80 degrees C does not protect matrix metalloproteinase-9 from degradation. Anal Biochem. 2005;338:294–298. doi: 10.1016/j.ab.2004.10.052. [DOI] [PubMed] [Google Scholar]
- 45.Tarr GP, Williams MJ, Phillips LV, van Rij AM, Jones GT. Seasonal variation and stability of matrix metalloproteinase-9 activity and tissue inhibitor of matrix metalloproteinase-1 with storage at -80 degrees C. Clin Biochem. 2011;44:1346–1348. doi: 10.1016/j.clinbiochem.2011.08.1139. [DOI] [PubMed] [Google Scholar]
- 46.Sun J, Wang Y, Cui W, Lou Y, Sun G, Zhang D, et al. Role of Epigenetic Histone Modifications in Diabetic Kidney Disease Involving Renal Fibrosis. J Diabetes Res. 2017;2017:7242384. doi: 10.1155/2017/7242384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jung K, Wu CY. Methodological weakness in using correlation coefficients for assessing the interchangeability of analyte data between samples collected under different sampling conditions--the example of matrix metalloproteinase 9 determined in serum and plasma samples. Clin Chem Lab Med. 2010;48:733–736. doi: 10.1515/CCLM.2010.135. [DOI] [PubMed] [Google Scholar]
- 48.Zucker S, Cao J. Measurement of matrix metalloproteinases in serum of patients with melanoma: snarled in technical pitfalls. Clin Cancer Res. 2005;11:5069–5070. doi: 10.1158/1078-0432.CCR-05-0774. [DOI] [PubMed] [Google Scholar]
- 49.Mannello F. Effects of blood collection methods on gelatin zymography of matrix metalloproteinases. Clin Chem. 2003;49:339–340. doi: 10.1373/49.2.339. [DOI] [PubMed] [Google Scholar]
- 50.Jung K, Laube C, Lein M, Lichtinghagen R, Tschesche H, Schnorr D, et al. Kind of sample as preanalytical determinant of matrix metalloproteinase 2 and 9 and tissue inhibitor of metalloproteinase 2 in blood. Clin Chem. 1998;44:1060–1062. [PubMed] [Google Scholar]
- 51.Sherief MH, Low SH, Miura M, Kudo N, Novick AC, Weimbs T. Matrix metalloproteinase activity in urine of patients with renal cell carcinoma leads to degradation of extracellular matrix proteins: possible use as a screening assay. J Urol. 2003;169:1530–1534. doi: 10.1097/01.ju.0000049201.91150.9d. [DOI] [PubMed] [Google Scholar]
- 52.Vandooren J, Geurts N, Martens E, Van den Steen PE, Opdenakker G. Zymography methods for visualizing hydrolytic enzymes. Nat Methods. 2013;10:211–220. doi: 10.1038/nmeth.2371. [DOI] [PubMed] [Google Scholar]
- 53.Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res. 2003;92:827–839. doi: 10.1161/01.RES.0000070112.80711.3D. [DOI] [PubMed] [Google Scholar]
- 54.Sato Y, Yanagita M. Resident fibroblasts in the kidney: a major driver of fibrosis and inflammation. Inflamm Regen. 2017;37:17. doi: 10.1186/s41232-017-0048-3. [DOI] [PMC free article] [PubMed] [Google Scholar]