Summary
Akkermansia muciniphila (A. muciniphila), an intestinal symbiont colonizing in the mucosal layer, is considered to be a promising candidate as probiotics. A. muciniphila is known to have an important value in improving the host metabolic functions and immune responses. Moreover, A. muciniphila may have a value in modifying cancer treatment. However, most of the current researches focus on the correlation between A. muciniphila and diseases, and little is known about the causal relationship between them. Few intervention studies on A. muciniphila are limited to animal experiments, and limited studies have explored its safety and efficacy in humans. Therefore, a critical analysis of the current knowledge in A. muciniphila will play an important foundation for it to be defined as a new beneficial microbe. This article will review the bacteriological characteristics and safety of A. muciniphila, as well as its causal relationship with metabolic disorders, immune diseases and cancer therapy.
Introduction
Several microbial species are getting increasing attention for their role in modulating the gut microbiota. At present, many diseases and conditions have been reported to be closely related to gut microbiota (de Vos and de Vos, 2012), so it is of great interest to improve the host health by modulating the intestinal bacteria. Akkermansia muciniphila (A. muciniphila) is a strict anaerobe recently isolated from human faeces and uses the mucin as the sole sources of carbon and nitrogen elements (Derrien et al., 2004). This mucin degrader is affected by the nutrients in the mucus layer located at a close distance to the intestinal epithelial (Belkaid and Hand, 2014). Due to this unique function and its high universality and richness in almost all life stages, A. muciniphila has opened new avenues for the application in next‐generation therapeutic probiotics (Collado et al., 2007; Derrien et al., 2008; Belzer and de Vos, 2012; Cani and de Vos, 2017). A series of studies have revealed that A. muciniphila regulated metabolic and immune functions, thus protecting mice from high‐fat diets (Derrien et al., 2011; Everard et al., 2013). Further analysis confirmed A. muciniphila can degrade mucin and exert competitive inhibition on other pathogenic bacteria that degrade the mucin (Belzer and de Vos, 2012). These findings provide a rationale for A. muciniphila to become a promising probiotic. However, products containing A. muciniphila are currently not available worldwide. The exact mechanism underlying A. muciniphila interacts with host remains unknown. Based on previous human and animal studies, extensive assessment for A. muciniphila is still needed. Here, we will summarize and provide the updated information on the bacteriological characteristics, safety, pathogenicity, antibiotic resistance of A. muciniphila and its effects on host health and diseases.
Characteristics of A. muciniphila
Akkermansia muciniphila is a bacterium of oval shape, strictly anaerobic, non‐motile and gram‐negative and forms no endospores (Fig. 1). It was historically discovered in 2004 at Wageningen University of the Netherlands when searching for a new mucin‐degrading microbe in human faeces (Derrien et al., 2004). Akkermansia muciniphila is the first member and the only representative of the phylum Verrucomicrobia in the human gut (Miller and Hoskins, 1981; Derrien et al., 2010), which is relatively easy to detect (Rajilic‐Stojanovic and de Vos, 2014). The genome of A. muciniphila strain MucT (=ATCC BAA‐835T=CIP 107961T) involves one circular chromosome of 2.66 Mbp, which shared a limited number of genes (29%) with its closest relatives in the Verrucomicrobia phylum (van Passel et al., 2011). Recently, Guo et al. (2017) reported a high genetic diversity of A. muciniphila by whole‐genome sequencing, with 5644 unique proteins assembling a flexible open pangenome. They further classified A. muciniphila into three species‐level phylogroups, which demonstrated different function features.
Figure 1.
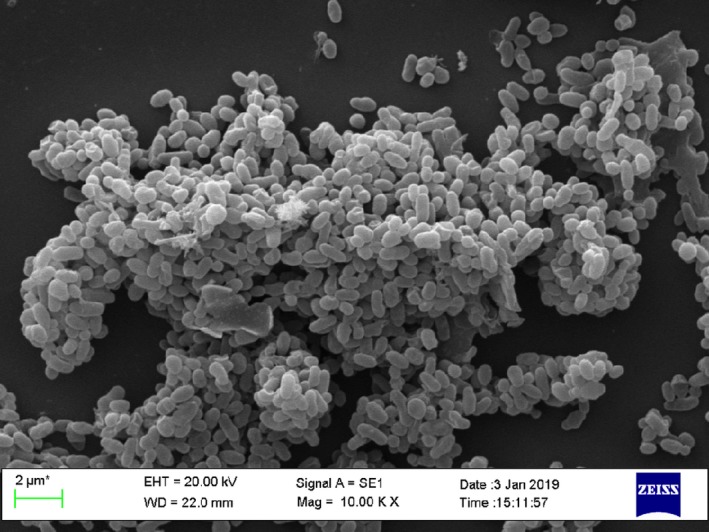
Scanning electronic micrograph of Akkermansia muciniphila. The A. muciniphila strain was isolated from a healthy Chinese donor for FMT at China fmtBank. Bar represents 2 μm.
It is widely distributed in the intestines of human and animals (Belzer and de Vos, 2012; Lagier et al., 2015). Akkermansia muciniphila was originally classified as a strictly anaerobic bacterium, but a recent study found that it can tolerate low levels of oxygen, with an oxygen reduction capacity to be 2.26 ± 0.99 mU mg−1 total protein (Ouwerkerk, et al., (2017b). This property is similar to some intestinal anaerobic colonizers such as Bacteroides fragilis and Bifidobacterium adolescentis, which could still survive after exposure to ambient air for 48 h. Akkermansia muciniphila is abundant in the host intestinal mucosal layer, with a largest number in the caecum. It is found to be ubiquitous in the guts of healthy adults and infants, and accounts for 1–4% of the total gut microbiota starting from early life (Derrien et al., 2008).
Akkermansia muciniphila is one of the normal gut symbionts throughout our life (Collado et al., 2007). This bacterium can stably colonize the human gut within 1 year after birth, and its abundance in the gut eventually reaches the same level as that in healthy adults (Collado et al., 2007; Derrien et al., 2008), but gradually decreases in the elderly (Collado et al., 2007). Previous phylogenetic and metagenomic studies based on hundreds of subjects have found that A. muciniphila is one of the top 20 most abundant species detectable in the human gut (Collado et al., 2007, 2012; Qin et al., 2010; Arumugam et al., 2011; Thomas et al., 2014; Drell et al., 2015). In addition, A. muciniphila is reported to be present in human milk (Collado et al., 2008). Human milk can act as a carrier for the transfer of A. muciniphila from mothers to infants, thereby explaining its presence in the gastrointestinal tract of newborn infants (Collado et al., 2007). At this life stage, A. muciniphila can successfully colonize the gastrointestinal tract with the active acid resistance system and the ability to degrade human milk oligosaccharides in newborn infants’ stomach (Bosscher et al., 2001).
Culturing A. muciniphila
Akkermansia muciniphila is divided into three species‐level phylogenetic groups with distinct metabolic features, but current studies still focused on the strain MucT (=ATCC BAA‐835T=CIP 107961T) (Guo et al., 2017). Akkermansia muciniphila is sensitive to oxygen, and its growth medium is animal‐derived compounds. Therefore, the clinical application of A. muciniphila is very limited due to these limitations in culture conditions. Ottman et al. (2017a,b) established a genome‐scale metabolic model to evaluate the substrate utilization abilities of A. muciniphila. It showed that A. muciniphila can utilize the mucin‐derived monosaccharides fucose, galactose and N‐acetylglucosamine. These additional mucin‐derived components might be needed for its optimal growth. Plovier et al. (2017) reported that A. muciniphila can be grown on a synthetic media, in which the mucin is replaced by a combination of glucose, N‐acetylglucosamine, peptone and threonine. This synthetic medium is capable of culturing A. muciniphila at the same efficiency as the mucin medium, while avoiding all compounds that are incompatible with humans. At the same time, A. muciniphila grown on synthetic media was confirmed to be safe for human administration (Plovier et al., 2017). A recent study reported that the genome‐scale metabolic model can be used to accurately predict growth of A. muciniphila on synthetic media (van der Ark et al., 2018). They found that glucosamine‐6‐phosphate (GlcN6P), which exists in the mucin and prompts the adaptation to the mucosal niche, is a necessity for A. muciniphila.
Moreover, Ouwerkerk et al. (2017a,b) proposed an efficient scalable workflow for the preparation and preservation of viable cells of A. muciniphila under strict anaerobic conditions for therapeutic interventions. An anaerobic plating system was used in this process to quantify the recovery and survival of viable cells of A. muciniphila. The preserved A. muciniphila cells showed very high stability with survival rate of 97.9 ± 4.5% for over 1 year at −80°C in glycerol‐amended medium. These results might pave a way for future clinical studies using A. muciniphila as a therapeutic product.
Safety and pathogenicity of A. muciniphila
Currently, a large number of researches on A. muciniphila mainly focused on explaining its relationship with diseases, but have not addressed the causality of the bacterium on the diseases (Tables 1 and 2). Several studies focusing on the direct interventions with A. muciniphila mostly used animal models (Everard et al., 2013; Hanninen et al., 2017; Chelakkot et al., 2018) (Table 3). Currently, there are no published open clinical trials of A. muciniphila for humans and therefore resulting in a lack of strong evidence on the safety of A. muciniphila in humans. This could explain why A. muciniphila has not been involved in food production or drug use. However, some preliminary studies have indicated this bacterium should be safe for interventions in human. Dubourg et al. (2013) reported that even when the abundance of A. muciniphila reached a high level of 60% in human following broad‐spectrum antibiotic treatment, no adverse events occurred. Moreover, in an ongoing clinical study, Plovier et al. (2017) have first evaluated the safety and tolerability of A. muciniphila in overweight subjects. Both live and pasteurized A. muciniphila were observed to be tolerated and safe in individuals with excess body weight after 2‐week oral administration of A. muciniphila.
Table 1.
Correlation between Akkermansia muciniphila and disease in humans
| Subject | Study type | Study group | Sample type and collection time | Sample detection | Relevance conclusion | |
|---|---|---|---|---|---|---|
| Chelakkot et al. (2018) | Type 2 diabetes | Observational | – | Faeces, at a selected time point | Metagenome | Compared to patients with type 2 diabetes, healthy human contained more A. muciniphila extracellular vesicles (AmEVs) in faeces |
| Grander et al. (2018) | Alcoholic steatohepatitis (ASH) | Observational |
|
Faeces, at a selected time point | 16S rRNA sequencing | Patients with ASH exhibited a decreased abundance of faecal A. muciniphila when compared with healthy controls that indirectly correlated with hepatic disease severity. Oral supplementation of A. muciniphila promotes intestinal barrier integrity and ameliorates experimental ALD in mice |
| Dao et al. (2016) | Overweight and obese adults | Interventional, limited energy intake for 6 weeks and followed up for 6 weeks |
|
Faeces, T0 = at baseline, T1 = 6 weeks after limiting energy intake, T2 = 12 weeks after stable body weight | Metagenomics, qPCR |
Baseline abundance of A. muciniphila was negatively correlated with fasting blood glucose, waist‐to‐hip ratio, and subcutaneous fat cell diameter Subjects with high abundance of A. muciniphila at baseline had improved insulin sensitivity and other obesity‐related clinical indicators after limiting energy intake |
| Drell et al. (2015) | Children with atopic diseases | Observational |
|
Faeces, at the age of 5 and 12 | Pyrosequencing | A decrease in the abundance of A. muciniphila in patients indicated that it plays an important role in IgE‐related atopic diseases compared to healthy people |
| Brahe et al. (2015) | Obese females | Observational | Obese females: n = 53 | Faeces, at a selected time point | Whole‐genome shotgun sequencing | Abundance of A. muciniphila was not associated with insulin resistance and dyslipidaemia |
| Remely et al. (2015a,b) | Overweight adults | Interventional, fasting for 1 week, followed by probiotic intake for 6 weeks | Overweight adults: n = 13 | Faeces, T1 = before fasting, T2 = during fasting, T3 = 6 weeks after probiotic intervention | qPCR | Compared with that during fasting (T2), the A. muciniphila abundance was detected higher before fasting (T1) and after intervention by probiotics (T3) |
| Remely et al. (2015a,b) | Obese individuals | Interventional, 16‐week weight loss diet | Obese individuals: n = 33 | Faeces, before, during and after the intervention | qPCR | After 16‐week weight loss diet, the abundance of A. muciniphila in obese individuals was higher than that before intervention |
| Kim et al. (2014) | Obese females | Interventional, ingestion of Ephedra for 8 weeks, 4 g per day | Obese females:n = 7 | Faeces, before and after ingestion of Casuarina | 16S rRNA sequencing | The increase in A. muciniphila abundance was positively correlated with the amount of weight loss in the subjects |
| Clarke et al. (2014) | Outstanding athletes | Observational |
|
Faeces, at a selected time point | 16S rRNA sequencing | Compared with that in high BMI group, the level of A. muciniphila was higher in the group of athletes and healthy men with low BMI values |
| Escobar et al. (2014) | Overweight and obese adults | Observational |
|
Faeces, at a selected time point | 16S rRNA sequencing | The level of A. muciniphila had no correlation with BMI value |
| Zhang et al. (2013) | Pre‐diabetes and newly diagnosed type 2 diabetes | Observational |
|
Faeces, at a selected time point | 16S rRNA sequencing | A. muciniphila abundance was reduced in subjects with pre‐diabetes and type 2 diabetes compared to subjects with normal glucose tolerance |
| Teixeira et al. (2013) | Obese females | Observational |
|
Faeces, at a selected time point | qPCR | The level of A. muciniphila was higher in individuals of normal weight compared to that in obese individuals |
| Weir et al. (2013) | Colorectal cancer | Observational |
|
Faeces, at a selected time point | 16S rRNA sequencing | The level of A. muciniphila was elevated in patients with colorectal cancer compared with that in healthy individuals |
| Candela et al. (2012) | Children with atopic diseases | Observational |
|
Faeces, collected within 3 days | qPCR | The abundance of A. muciniphila in children with atopic diseases was missing compared with that in healthy children |
| Karlsson et al. (2012) | Overweight and obese children (4–5 years old) | Observational |
|
Faeces, at a selected time point | qPCR, T‐RFLP | A. muciniphila was less abundant in overweight and obese children than that in normal weight children |
| Qin et al. (2012) | Type 2 diabetes | Observational |
|
Faeces, at a selected time point | Whole‐genome shotgun sequencing | A. muciniphila abundance was higher in faeces of patients with type 2 diabetic compared with that in healthy controls |
| Collado et al. (2012) | Overweight lactating women | Observational |
|
Breast milk, at 1 month and 6 months after childbirth | qPCR | Compared with that in normal weight women, the abundance of A. muciniphila was increased in breast milk of overweight women at 1 month after childbirth |
| Vigsnaes et al. (2012) | UC | Observational |
|
Faeces, subjects collected at home | qPCR | Compared with that in healthy controls, the abundance of A. muciniphila in faeces of patients with UC was reduced |
| Wang et al. (2011) | Autistic children | Observational | Autistic children: n = 23 | Faeces, at a selected time point | qPCR | The abundance of A. muciniphila was reduced in faeces of autistic children |
| Swidsinski et al. (2011) | Appendicitis, IBD and other diseases | Observational |
|
Faeces, at a selected time point | Fluorescence in situ hybridization,FISH | The abundance of A. muciniphila was inversely proportional to the severity of appendicitis |
| Collado et al. (2010) | Infants (overweight or normal weight pregnant women) | Observational |
|
Faeces, at 1 month and 6 months | qPCR,FISH‐FCM | Compared with normal weight pregnant women, A. muciniphila was more abundant in infants born to overweight pregnant women |
| Santacruz et al. (2010) | Normal weight and overweight pregnant women | Observational |
|
Faeces, at a selected time point | qPCR | In normal weight and overweight pregnant women, A. muciniphila had no difference in abundance, but its abundance was reduced in obese pregnant women |
| Png et al. (2010) | IBD | Observational |
|
Tissue specimen (distal colon, proximal colon, terminal ileum), at a selected time point | qPCR | A. muciniphila abundance was reduced in IBD patients’ intestinal mucosa compared with in healthy people |
| Zhang et al. (2009) | Morbid obese individuals | Interventional, gastric bypass |
|
Faeces, at a selected time point | 16S rRNA sequencing | A. muciniphila abundance was reduced in obese individuals compared to normal weight individuals; however, obese individuals received an increased abundance of A. muciniphila after gastric bypass |
| Collado et al. (2007) | Healthy human | Observational |
|
Faeces, at a selected time point | qPCR | A. muciniphila was colonized in the intestine when a baby was born, and its abundance reached the adult level at the age of 1. With people getting old, the abundance of A. muciniphila in the intestine was decreased than before |
AmEVs, A. muciniphila extracellular vesicles; BMI, body mass index; CD, Crohn's disease; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Table 2.
Correlation between A. muciniphila and disease in animals
| Subject | Study type | Study group | Sample collection | Sample detection | Relevance conclusion | |
|---|---|---|---|---|---|---|
| Catry et al. (2018) | Nine‐week‐old male C57Bl/6J (WT) and Apoe−/− (KO) mice | Interventional, fed an n‐3 polyunsaturated fatty acid (PUFA)‐depleted (DEF) diet for 12 weeks with or without inulin‐type fructans (ITFs) supplementation for the last 15 days |
|
Caecal content | Illumina Sequencing of the 16S rRNA gene | After prebiotic treatment of inulin‐type fructans, the endothelial dysfunction was improved in mice, and the abundance of A. muciniphila was increased |
| Zhu et al. (2017) | Six‐week‐old male C57BL/6J mice | Interventional, treated with fructo‐oligosaccharides and inulin for 6 weeks |
|
Faeces | 16S rRNA sequencing | A. muciniphila became a dominant species in Verrucomicrobia phylum after treatment with fructo‐oligosaccharides and inulin. It played an important role on maintaining balance between mucin and short‐chain fatty acids |
| Singh et al. (2017) | Male Swiss albino mice | Interventional, HFD (58% fat kcal) for 12 weeks |
|
Caecal content | 16S rRNA metagenomic sequencing | A combination of green tea extract with isomalto‐oligosaccharide exerted beneficial effects on HFD‐induced alterations in mice and improved A. muciniphila abundances |
| Song et al. (2016) | Male C57BL/6J mice | Interventional, HFD plus HPBN of 200 mg/kg for 14 weeks |
|
Faeces | 16S rRNA sequencing | Red pitaya betacyanins protect from diet‐induced obesity and its related metabolic disorders, and increase the relative abundance of A. muciniphila |
| Schneeberger et al. (2015) | Six‐week male C57BL/6 mice | Interventional, HFD |
|
Caecal contents, collected at the time mice were sacrificed | qPCR | A. muciniphila abundance was reduced in obese mice induced by a high‐fat diet |
| Gomez‐Gallego et al. (2014) | Two‐week BALB/c mice | Interventional |
|
Oral, stomach, large and small intestine contents | qPCR | Compared with the infant formula group, A. muciniphila abundance was increased in the breastfeeding group |
| Baxter et al. (2014) | 6–10 weeks male C57BL/6 mice | Interventional, transplanted the faecal bacteria from three colorectal cancer patients and three healthy people to sterile mice (gavage) |
|
Transplanted human and mouse faeces, at day 0 and day 73 | 16S rRNA sequencing, Illumina sequencing | The abundance of A. muciniphila in mice transplanted with faecal bacteria of colorectal cancer patients was higher than that of healthy adults |
| Hakansson et al. (2015) | Wild female C57BL/6 mice | Interventional, 4% DSS feeding for seven consecutive days |
|
Colon and caecum contents, at day 7 | 16S rRNA sequencing, qPCR | The A. muciniphila abundance in mice treated with 4% DSS was elevated compared to the untreated group |
| Zackular et al. (2013) | 8–12 weeks male C57BL/6 mice | Interventional, tumour‐inducing injection |
|
Faeces, collected daily during tumour‐injection | 16S rRNA sequencing, qPCR | A. muciniphila abundance was elevated in the faeces of tumour mice compared to that in healthy mice |
| Hansen et al. (2012) | NOD mice (non‐obese diabetic mice) | Interventional, 15–21 mice per group, vancomycin (83 mg kg−1 day−1) |
|
Faeces, collected at the time diagnosed as diabetes or blood glucose > 12 mM | 16S rRNA sequencing, pyrosequencing | A. muciniphila abundance was decreased in faeces of type 1 diabetic mice, and it was a protective strain of autoimmune diabetes |
| Berry et al. (2012) | 6–8 weeks Wt mice and STAT1 −/− mice | Interventional, the experimental group was given 2% DSS for 7 consecutive days, followed by drinking water for the next 3 days |
|
Colon and caecum contents, at day 10 | 16S rRNA sequencing, pyrosequencing | The abundance of A. muciniphila in mice treated with 2% DSS was elevated compared to the control group |
| Sonoyama et al. (2010) | Five‐week female BALB/c mice | Interventional, ingesting 4 varieties of rice, then inducing allergic diarrhoea by immunization |
|
Faeces, before immunization | 16S rRNA sequencing, qPCR | Compared with other groups, the abundance of A. muciniphila in the Yukihikari group was decreased, and the mice in this group were less likely to be induced to develop allergic diarrhoea |
| Sonoyama et al. (2009) | 12‐week Syrian hamster | Interventional, dietary intervention for 96 h |
|
Caecal contents, at the end of the intervention | qPCR | A. muciniphila abundance was elevated in the fasted non‐hibernation mice compared to other groups |
DSS, dextran sulfate sodium; FOS, fructo‐oligosaccharides; HFD, high‐fat diet; HPBN, hylocereus polyrhizus fruit betacyanins.
Table 3.
Causal relationship between A. muciniphila and disease
| Subject | Study type | Study group | Bacterial intervention | Bacterial status | Sample type | Sample detection | Treatment outcome | |
|---|---|---|---|---|---|---|---|---|
| Routy et al. (2018) | SPF mice | Interventional |
|
Mice exhibiting non‐response FMT‐induced dysbiosis were compensated with A. muciniphila alone or combined with E. hirae or control bacteria during PD‐1 mAb‐based therapy | Viable | Faeces | Metagenomic analysis | FMT from cancer patients who did not respond to ICIs into germ‐free or antibiotic‐treated mice failed to ameliorate the antitumour effects of PD‐1 blockade. Oral supplementation with A. muciniphila after FMT with non‐responder faeces restored the efficacy of PD‐1 blockade |
| Chelakkot et al. (2018) | Male 6–8 week C57BL/6 mice | Interventional |
|
Orally administered with 10 μg AmEVs once every two days for two weeks | Viable | Faeces, colon tissue, rat tail vein blood | 16S rRNA sequencing, immunohistochemistry, immunoblotting | A. muciniphila extracellular vesicles may improve metabolic function by altering intestinal permeability and barrier integrity in high‐fat diet mice |
| Plovier et al. (2017) | 10‐ to 11‐week‐old male C57BL/6J mice; Human subjects with excess body weight | Interventional |
Mice:
Human:
|
Human subjects were assigned to receive either a daily dose of placebo (an equivalent volume of sterile PBS containing glycerol), 1010 CFU live A. muciniphila (Akk S – 1010), 109 CFU live A. muciniphila (Akk S – 109), or 1010 CFU pasteurized A. muciniphila (Akk P – 1010) for 3 months | Live and pasteurized | Intestinal tissue, blood | Real‐time qPCR | A. muciniphila retains its efficacy when grown on a synthetic medium. Pasteurization of A. muciniphila enhanced its capacity to reduce fat mass development, insulin resistance and dyslipidaemia in mice. Administration of live or pasteurized A. muciniphila grown on the synthetic medium is safe in humans |
| Hanninen et al. (2017) | Non‐obese diabetic mice | Interventional |
|
(i) 330 μl bacterial suspension from mice with low diabetes incidence rate, twice daily for three consecutive days (ii) Orally administered 2 × 108 cfu A. muciniphila, three times a week for 7 weeks (iii) Orally administered 2 × 106 cfu A. muciniphila, three times a week for 7 weeks |
Viable | Faeces, caecal and colon contents | 16S rRNA sequencing | Transplanting the gut microbiota of mice with low diabetes incidence to mice with high diabetes incidence did not reduce the morbidity of diabetes; but transplanting the single strain A. muciniphila to mice with high incidence of diabetes can reduce the morbidity of diabetes |
| Li et al. (2016) | Eight‐week‐old male Apoe−/− mice | Interventional |
|
The Western diet‐fed mice were further separated into three groups: a group receiving daily oral gavage with live A muciniphila (WD+Akk), a group receiving daily oral gavage with heat‐killed A muciniphila (WD+hk‐Akk), and a third gavaged with PBS as vehicle control (WD+PBS) | Live | Aorta and ileum | Real‐time qPCR | Oral gavage with A muciniphila protected against western diet‐induced atherosclerotic lesion formation in Apoe−/− Mice |
| Shin et al. (2014) | C57BL/6 mice | Interventional |
|
The bacteria were harvested at the late exponential growth phase, suspended in thioglycolate–phosphate‐buffered saline (PBS) (4.0 × 108 cfu) and orally administered to HFD‐fed mice (HFD‐Akk; n = 6) | Viable | Faeces | 16S rRNA gene sequences with 454 pyrosequencing | Oral administration of Akkermansia muciniphila to HFD‐fed mice without metformin significantly enhanced glucose tolerance and attenuated adipose tissue inflammation by inducing Foxp3 regulatory T cells (Tregs) in the visceral adipose tissue |
| Kang et al. (2013) | Specific pathogen free C57BL/6 mice | Interventional |
|
2% DSS was administered to female C57BL/6 mice for 5 days, and then, mice were treated with 2% DSS and A. muciniphila (5 × 108 CFU per mouse), and treated with 2% DSS and A. muciniphila‐derived EV (AmEV, 100 mg/mouse). | Viable | Small intestinal fluids and stools | Metagenome sequencing | A. muciniphila‐derived extracellular vesicles have protective effects in the development of DSS‐induced colitis |
| Everard et al. (2013) | 10‐week C57BL/6 mice | Interventional |
|
Intragastric administration of A. muciniphila (live bacteria, heat‐killed bacteria, 2 × 108 cfu 0.2 ml−1) | Live and heat‐killed | Caecal contents, collected every day | 16S rRNA sequencing, qPCR | A. muciniphila abundance was decreased in mice with diabetes and obesity caused by high‐fat diet, and the metabolic function of mice could be improved by intragastric administration of live A. muciniphila |
AmEVs, A. muciniphila extracellular vesicles; DSS, dextran sulphate sodium; FMT, faecal microbiota transplantation; HFD, high‐fat diet; ICIs, immune checkpoint inhibitors; NCD, normal chow diet; ND, normal diet; PBS, phosphate‐buffered saline; SPF, specific pathogen‐free; WD, Western diet.
As for the pathogenicity of A. muciniphila, it has not yet been clearly associated with any disease or sign of illness (Derrien et al., 2010). The potential pathogenicity of A. muciniphila was mainly due to its process from adhesion to degradation of the intestinal mucus layer, which may involve some initial pathogenic behaviours (Donohue and Salminen, 1996; Tuomola et al., 2001; Derrien et al., 2010). Unlike pathogens, A. muciniphila as a mucin‐degrading agent mainly stays in the outer mucosal layer and does not reach the inner mucosal layer, but bacteria reaching the inner layer have been shown to be required for pathogenicity (Gomez‐Gallego et al., 2016). Although degrading mucin itself is a pathogen‐like behaviour (Donohue and Salminen, 1996), it is considered a normal process in the intestinal self‐renewal balance (Gomez‐Gallego et al., 2016). Moreover, it is reported that A. muciniphila may maintain host intestinal microbial balance by converting mucin into beneficial by‐products (Derrien et al., 2008). To date, there is no evidence that A. muciniphila alone causes pathogenicity; nevertheless, it is not known whether it may cause diseases in synergy with other bacteria.
Akkermansia muciniphila, as a gram‐negative bacterium, contains lipopolysaccharide, but it is not associated with endotoxemia. This bacterium even reduced the endotoxin level associated with high‐fat diets in mice (Everard et al., 2013). Mucin degradants are known to regulate host immune system through signals such as tumour necrosis factor alpha (TNF‐α), interferon gamma (INF‐γ), interleukin‐10 (IL‐10) and IL‐4 (Derrien et al., 2011; Collado et al., 2012; Andersson et al., 2013). There was evidence that a decreased level of the anti‐inflammatory cytokines IL‐10 and IL‐4 and an elevated level of pro‐inflammatory cytokines TNF‐α and IFN‐γ were associated with an increased level of A. muciniphila (Collado et al., 2012). From a genetic point of view, colonization of A. muciniphila in sterile mice did not cause side‐effects or the upregulated expression of pro‐inflammatory cytokines (Derrien et al., 2011). Intestinal anti‐inflammatory and protective effects were thought to be closely related to A. muciniphila (Png et al., 2010; Candela et al., 2012). Hence, we suggest that treatment with A. muciniphila should be safe with a rationale.
Colonization of A. muciniphila and its interaction with the host
The ability of A. muciniphila to adhere to the mucus layer was considered to be a beneficial probiotic characteristic (Derrien et al., 2010; Everard et al., 2013; Chelakkot et al., 2018; Hanninen et al., 2018). The intestinal mucosal layer mainly protects epithelial cells from microbial attacks and provides growth energy for microorganisms that use it as a nutrient. A low level of A. muciniphila in the intestine may result in the thinning of the mucosa, thus leading to a weakening of the intestinal barrier function, and making it easier for the toxins to invade the host. The relationship between A. muciniphila and the host is not only reflected in the intake, utilization and consumption of energy associated with glucose, protein and lipid metabolism, but also in the integrity of mucosal layer and related mucosal immune response. Akkermansia muciniphila not only participates in the host immune regulation, but also enhances the integrity of the intestinal epithelial cells and the thickness of the mucus layer, thereby promoting intestinal health (Everard et al., 2013; Reunanen et al., 2015).
Microorganisms on the surface of the intestinal mucosa are known to contribute more to host immunity, and A. muciniphila is a typical representative (Nieuwdorp et al., 2014). The host's nutrient environment could affect the growth of A. muciniphila in the intestine. For example, the property of A. muciniphila degrading mucin can be defined as a competitive advantage when the host is in nutritional deficiencies such as during fasting and in malnutrition. This was confirmed by the experiment on hamsters that the abundance of A. muciniphila was significantly increased after fasting (Sonoyama et al., 2009). The level of mucin in the intestine of rats fed with arabinose or inulin was significantly increased, and this change also contributed to the abundance of A. muciniphila.
In turn, the host will also benefit from the colonization of A. muciniphila. A. muciniphila was colonized in the sparse mucus layer, and it therefore was closer to the intestinal epithelial cells than other microorganisms colonized in the intestinal lumen. Its metabolites, such as propionic acid, were also present in the mucus layer close to the intestinal epithelial cells and were easily accessible to the host. Propionic acid can act on the host through Gpr43 (G protein‐coupled receptor 43), while other short‐chain fatty acids through Gpr41, thus causing a series of downstream pathway changes to achieve immunomodulatory effects (Le Poul et al., 2003; Maslowski et al., 2009).
In vivo, A. muciniphila was colonized in sterile mice and the effective colonization was highest in the caecum (Derrien et al., 2011). This may be explained by the reason that most of the mucin was produced in the caecum. The whole transcriptome analysis of intestinal tissue samples indicated that A. muciniphila regulated the expression of approximately 750 genes, with the changes mainly focused on genes associated with immune responses. In vitro, propionic acid and butyric acid are the main metabolites of A. muciniphila. A. muciniphila regulated the expression of 1005 genes in intestinal tissue, of which 503 genes were upregulated and 502 genes were down‐regulated. While Faecalibacterium prausnitzii only affected the expression of 190 genes, of which 86 were upregulated, and 104 genes were downregulated (Lukovac et al., 2014). Consequently, A. muciniphila can regulate the host's metabolism and immune function. However, the causal relationship between the microbes and host genomes is very complicated and needs to be further evaluated (Wang et al., 2018a,b).
Akkermansia muciniphila regulated the balance between health and disease
Akkermansia muciniphila has recently been considered as a significant factor in human physiology, including homeostatic and pathological conditions. A large number of human and animal studies have addressed the associations between the abundance of A. muciniphila and various disorders and diseases (Tables 1 and 2). The decreased level of A. muciniphila is considered to be related to the development of some diseases. Amongst which, the majority were metabolic disorders and inflammatory diseases, including obesity, type 2 diabetes, inflammatory bowel disease (IBD), autism and atopy. However, Weir et al. (2013) found that the level of A. muciniphila was obviously elevated in patients with colorectal cancer compared with that in healthy individuals. This negative correlation might be associated with some confounders such as diet and medication. For example, food intake was greatly reduced in patients with colorectal cancer, while fasting is reported to be involved in increasing the level of A. muciniphila (Remely et al., 2015a,b). A small sample size of patients might be another influencing factor. Moreover, some studies showed that no relation with A. muciniphila‐like bacteria was observed by metagenomic analysis (Zeller et al., 2014; Yu et al., 2017).
Recently, the research models of microbiome are facing a shift from focusing on association with a causality in recent years. For example, the beneficial therapeutic effects can be observed when the bacteria were administered in a viable form (Table 3). Consequently, A. muciniphila may become a biomarker of host health status, indicating the state of disease progression (Png et al., 2010; Swidsinski et al., 2011; Berry and Reinisch, 2013).
Unexpectedly, a recent study showed that pasteurized A. muciniphila can also prevent obesity and related complications, with the effectiveness be even better than live bacteria (Plovier et al., 2017). Even more exciting, the research team purified the outer membrane protein of A. muciniphila, Amuc_1100, which may exert this beneficial effect. Amuc_1100 was stable during pasteurization and interacted with Toll‐like receptor 2 to improve intestinal barrier function and to perform part of the probiotic function alone. Consistent with this finding, Ottman et al. (2017a,b) also found that Amuc_1100 could activate TLR2 and TLR4 to increase IL‐10 production and thus regulating immune response and intestinal barrier function This finding is significant and provides an important theoretical basis for the application of A. muciniphila in clinical treatments. However, the proved activity of A. muciniphila in pasteurized form has caused another controversial problem. The use of the term probiotic, which was specifically defined as live microorganisms by the Expert Panel from the Food and Agriculture Organization of the United Nations in 2001, may be misleading. A recent review stated that probiotic applications can be either live or dead forms (Hai, 2015). Regarding this modified definition, the Expert Panel previously declared that a dead probiotic is not approved. They demonstrated that if dead organisms have beneficial properties, they should be defined as a different term instead of probiotic. The perfect definition of probiotics needs further improvement in future.
Metabolic disorders and A. muciniphila
Akkermansia muciniphila is abundant in the gut microbiota of healthy individuals and exerts the effect of preventing and treating obesity, type 2 diabetes and other metabolic dysfunctions (Png et al., 2010, Santacruz et al., 2010; Karlsson et al., 2012; Everard et al., 2013; Zhang et al., 2013). Previous studies found that its abundance was inversely proportional to the body weight of mice and humans (Derrien et al., 2010; Santacruz et al., 2010; Karlsson et al., 2012; Everard et al., 2013; Teixeira et al., 2013). Akkermansia muciniphila can significantly increase glucose tolerance and attenuate adipose inflammation in obese mice by inducing Foxp3 regulatory T cells (Shin et al., 2014). With the application of probiotics to overweight subjects after fasting, an obviously increased level of A. muciniphila was observed (Remely et al., 2015a,b). Moreover, an interventional study with Akkermansia showed that the level of blood lipopolysaccharide, which functioned as an indicator of gut permeability, was significantly decreased in obese mice after the administration of Akkermansia (Everard et al., 2013). Similarly, another study established that Akkermansia‐derived extracellular vesicles could regulate the intestinal permeability and barrier integrity and thus affect the metabolic functions in mice with a high‐fat diet (Chelakkot et al., 2018). Dao et al. (2016) reported that the baseline level of A. muciniphila in obese patients was negatively related to the fasting blood glucose, waist‐to‐hip ratio and subcutaneous fat cell diameter. And after limiting energy intake for 6 weeks, patients with a high abundance of A. muciniphila at baseline had significantly improved insulin sensitivity and other obesity‐related clinical indicators. Akkermansia muciniphila can be therefore used as a metabolic marker to indicate the reduction in the risk of obesity (Brahe et al., 2015), and it might be directly used to improve the glucose and lipid metabolism to treat obesity.
Recently, Chelakkot et al. (2018) reported that compared to patients with type 2 diabetes, healthy human contained more A. muciniphila extracellular vesicles (AmEVs) in faeces. Another study found that the abundance of A. muciniphila was reduced in subjects with pre‐diabetes and type 2 diabetes compared to subjects with normal glucose tolerance (Zhang et al., 2013). The relationship between A. muciniphila and type 2 diabetes was also reflected in cases using metformin (Lee and Ko, 2014). High levels of A. muciniphila in patients seemed to contribute to enhancing the efficacy of metformin (Shin et al., 2014). This was confirmed by the correlation between an increased A. muciniphila level and the effectiveness of metformin in a recent study (Forslund et al., 2015). Although the mechanisms involved are not fully understood (van Passel et al., 2011; Swidsinski et al., 2011; Everard et al., 2013; Cani and Everard, 2014; Shin et al., 2014), these animal experiments and related human studies have provided strong support for A. muciniphila in regulating energy homeostasis and glucose metabolism.
Several animal experiments and one human study have used A. muciniphila for direct intervention to evaluate its effectiveness in treating metabolic diseases. Initially in 2013 (Everard et al., 2013), Everard et al. reported that the abundance of A. muciniphila was decreased in mice with diabetes and obesity caused by high‐fat diet, and the metabolic function of mice could be improved by intragastric administration of viable A. muciniphila. In 2017, Hanninen et al. (2017) established that transplanting the gut microbiota of mice with low incidence of diabetes, into the mice with high incidence of diabetes, did not reduce the morbidity of diabetes, but transplanting the single strain A. muciniphila into the mice with high incidence of diabetes can reduce the morbidity of diabetes. Chelakkot et al. (2018) reported that the intervention of oral administration with AmEVs may improve metabolic function by altering intestinal permeability and barrier integrity in high‐fat diet mice. Thus, based on these direct interventional studies, A. muciniphila could be a very promising beneficial microbe for treating metabolic disorders. Most importantly, Plovier et al. (2017) have implemented a clinical study to evaluate the efficacy of A. muciniphila on metabolic syndrome. Currently, complete results have not been published, but the preliminary human data at least suggested that oral administration of this bacterium is safe. Altogether, these results demonstrate that A. muciniphila promises to be a potential therapy to treat metabolic diseases.
Immune diseases and A. muciniphila
A decreased abundance of A. muciniphila in children with atopic diseases indicated that it plays an important role in IgE‐related atopic diseases (Drell et al., 2015). The correlation between a low level of A. muciniphila and immune response in atopic children suggested that A. muciniphila could interact with intestinal epithelial cells to produce IL‐8 for immunomodulatory effects (Drell et al., 2015; Reunanen et al., 2015). In addition, the reduction in the number of A. muciniphila was closely related to the occurrence of IBD (Png et al., 2010; Rajilic‐Stojanovic et al., 2013). The abundance of A. muciniphila was significantly decreased in the intestinal mucosa of IBD patients compared to that in healthy people (Png et al., 2010). Kang et al. (2013) recently found that AmEVs could regulate intestinal immunity and homeostasis and exert protective effects in the development of dextran sulfate sodium‐induced colitis in mice. However, there is still a lack of human experiments that directly interfere with A. muciniphila to illustrate the causal relationship between this microbe and host immune diseases.
Cancer therapy and A. muciniphila
Recently, three consecutive articles published in 2018 have shown the importance of gut microbiota combined with anti‐PD‐1 antibody in cancer therapy (Gopalakrishnan et al., 2018; Matson et al., 2018; Routy et al., 2018). Routy et al. (2018) analysed the relationship between the therapeutic efficacy of immune checkpoint inhibitors and the gut microbiota in patients with different cancers. They found that the intestinal level of A. muciniphila was significantly increased in patients with a positive response to the immune checkpoint inhibitor PD‐1 antibody. Furthermore, when the faecal microbiota from patients who responded positively to the immunotherapy were transplanted to sterile mouse, the corresponding positive response to the anti‐PD‐1 antibody was achieved. But when the faecal bacteria from patients who did not respond to the immunotherapy were transplanted to sterile mice, the native response was observed. Excitingly, the mice could recover their response to the anti‐PD‐1 antibody after oral administration of A. muciniphila. In addition, Matson et al. (2018) reported A. muciniphila abundance was observed in four metastatic melanoma patients with clinical response to anti‐PD‐1‐based immunotherapy. After gavaged with faecal material from responding patient donors, improved tumour control and better efficacy of immunotherapy was observed in a mouse melanoma model. Gopalakrishnan et al. (2018) also found a higher level of good intestinal bacteria in the melanoma patients who responded to the treatment of PD‐1 blockade. Combining three studies, Gharaibeh et al. (Gharaibeh and Jobin, 2018) concluded that there was a signal for more A. muciniphila in responders. The above results indicate that cancer immunotherapy combined with A. muciniphila as one of important probiotics in selective microbiota transplantation (Wu et al., 2019) is expected to achieve better clinical results for patients in the near future.
Consistently, Wang et al. (2018a,b) reported one patient with high‐grade metastatic urothelial carcinoma showed immune checkpoint inhibitors (ICI)‐associated colitis after a trial of combined CTLA‐4 and PD‐1 blockade. After ICI‐associated colitis in the patient was successfully treated with FMT, donor‐derived bacteria were observed to be effectively colonized in the patient's intestinal tract, with an obviously higher level of A. muciniphila. Consequently, A. muciniphila has shown its potential role in the treatment of cancer, and this role needs to be further confirmed by researchers.
Conclusions
Akkermansia muciniphila, as a potential probiotic that can make good use of gastrointestinal mucin, is inextricably linked to host metabolism and immune response. It promises to be a therapeutic target in the microbiota‐related diseases, such as colitis, metabolic syndrome, immune diseases and cancer. Preliminary human data suggest oral administration of A. muciniphila is safe, but its effect needs to be further verified in more human clinical trials in the near future.
Conflict of interest
None declared.
Acknowledgements
We appreciate the kindly help from Jie Zhang for providing data from China Microbiota Transplantation System (www.fmtbank.org).
Microbial Biotechnology (2019) 12(6), 1109–1125
Funding Information
This work was supported by National Natural Science Foundation of China (NO. 81873548). The funding source had no role in the design of the study, collection, analysis and interpretation of data and in writing the manuscript.
References
- Andersson, K.E. , Axling, U. , Xu, J. , Sward, K. , Ahrne, S. , Molin, G. , et al (2013) Diverse effects of oats on cholesterol metabolism in C57BL/6 mice correlate with expression of hepatic bile acid‐producing enzymes. Eur J Nutr 52: 1755–1769. [DOI] [PubMed] [Google Scholar]
- van der Ark, K.C.H. , Aalvink, S. , Suarez‐Diez, M. , Schaap, P.J. , de Vos, W.M. , and Belzer, C. (2018) Model‐driven design of a minimal medium for Akkermansia muciniphila confirms mucus adaptation. Microb Biotechnol 11: 476–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arumugam, M. , Raes, J. , Pelletier, E. , Le Paslier, D. , Yamada, T. , Mende, D.R. , et al (2011) Enterotypes of the human gut microbiome. Nature 473: 174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter, N.T. , Zackular, J.P. , Chen, G.Y. , and Schloss, P.D. (2014) Structure of the gut microbiome following colonization with human feces determines colonic tumor burden. Microbiome 2: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belkaid, Y. , and Hand, T.W. (2014) Role of the microbiota in immunity and inflammation. Cell 157: 121–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belzer, C. , and de Vos, W.M. (2012) Microbes inside–from diversity to function: the case of Akkermansia. ISME J 6: 1449–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry, D. , and Reinisch, W. (2013) Intestinal microbiota: a source of novel biomarkers in inflammatory bowel diseases?. Best Pract Res Clin Gastroenterol 27: 47–58. [DOI] [PubMed] [Google Scholar]
- Berry, D. , Schwab, C. , Milinovich, G. , Reichert, J. , Ben Mahfoudh, K. , Decker, T. , et al (2012) Phylotype‐level 16S rRNA analysis reveals new bacterial indicators of health state in acute murine colitis. ISME J 6: 2091–2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosscher, D. , Lu, Z. , Janssens, G. , Van Caillie‐Bertrand, M. , Robberecht, H. , De Rycke, H. , et al (2001) In vitro availability of zinc from infant foods with increasing phytic acid contents. Br J Nutr 86: 241–247. [DOI] [PubMed] [Google Scholar]
- Brahe, L.K. , Le Chatelier, E. , Prifti, E. , Pons, N. , Kennedy, S. , Hansen, T. , et al (2015) Specific gut microbiota features and metabolic markers in postmenopausal women with obesity. Nutr Diabetes 5: e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candela, M. , Rampelli, S. , Turroni, S. , Severgnini, M. , Consolandi, C. , De Bellis, G. , et al (2012) Unbalance of intestinal microbiota in atopic children. BMC Microbiol 12: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cani, P.D. , and de Vos, W.M. (2017) Next‐generation beneficial microbes: the case of Akkermansia muciniphila . Front Microbiol 8: 1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cani, P.D. , and Everard, A. (2014) Akkermansia muciniphila: a novel target controlling obesity, type 2 diabetes and inflammation? Med Sci 30: 125–127. [DOI] [PubMed] [Google Scholar]
- Catry, E. , Bindels, L.B. , Tailleux, A. , Lestavel, S. , Neyrinck, A.M. , Goossens, J.F. , et al (2018) Targeting the gut microbiota with inulin‐type fructans: preclinical demonstration of a novel approach in the management of endothelial dysfunction. Gut 67: 271–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelakkot, C. , Choi, Y. , Kim, D.K. , Park, H.T. , Ghim, J. , Kwon, Y. , et al (2018) Akkermansia muciniphila‐derived extracellular vesicles influence gut permeability through the regulation of tight junctions. Exp Mol Med 50: e450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, S.F. , Murphy, E.F. , O'Sullivan, O. , Lucey, A.J. , Humphreys, M. , Hogan, A. , et al (2014) Exercise and associated dietary extremes impact on gut microbial diversity. Gut 63: 1913–1920. [DOI] [PubMed] [Google Scholar]
- Collado, M.C. , Derrien, M. , Isolauri, E. , de Vos, W.M. , and Salminen, S. (2007) Intestinal integrity and Akkermansia muciniphila, a mucin‐degrading member of the intestinal microbiota present in infants, adults, and the elderly. Appl Environ Microbiol 73: 7767–7770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado, M.C. , Isolauri, E. , Laitinen, K. , and Salminen, S. (2008) Distinct composition of gut microbiota during pregnancy in overweight and normal‐weight women. Am J Clin Nutr 88: 894–899. [DOI] [PubMed] [Google Scholar]
- Collado, M.C. , Isolauri, E. , Laitinen, K. , and Salminen, S. (2010) Effect of mother's weight on infant's microbiota acquisition, composition, and activity during early infancy: a prospective follow‐up study initiated in early pregnancy. Am J Clin Nutr 92: 1023–1030. [DOI] [PubMed] [Google Scholar]
- Collado, M.C. , Laitinen, K. , Salminen, S. , and Isolauri, E. (2012) Maternal weight and excessive weight gain during pregnancy modify the immunomodulatory potential of breast milk. Pediatr Res 72: 77–85. [DOI] [PubMed] [Google Scholar]
- Dao, M.C. , Everard, A. , Aron‐Wisnewsky, J. , Sokolovska, N. , Prifti, E. , Verger, E.O. , et al (2016) Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut 65: 426–436. [DOI] [PubMed] [Google Scholar]
- Derrien, M. , Vaughan, E.E. , Plugge, C.M. , and de Vos, W.M. (2004) Akkermansia muciniphila gen. nov., sp. nov., a human intestinal mucin‐degrading bacterium. Int J Syst Evol Microbiol 54: 1469–1476. [DOI] [PubMed] [Google Scholar]
- Derrien, M. , Collado, M.C. , Ben‐Amor, K. , Salminen, S. , and de Vos, W.M. (2008) The Mucin degrader Akkermansia muciniphila is an abundant resident of the human intestinal tract. Appl Environ Microbiol 74: 1646–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrien, M. , van Passel, M.W. , van de Bovenkamp, J.H. , Schipper, R.G. , de Vos, W.M. , and Dekker, J. (2010) Mucin‐bacterial interactions in the human oral cavity and digestive tract. Gut Microbes 1: 254–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrien, M. , Van Baarlen, P. , Hooiveld, G. , Norin, E. , Muller, M. , and de Vos, W.M. (2011) Modulation of mucosal immune response, tolerance, and proliferation in mice colonized by the mucin‐degrader Akkermansia muciniphila . Front Microbiol 2: 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue, D.C. , and Salminen, S. (1996) Safety of probiotic bacteria. Asia Pacific J Clin Nutri 5: 25–28. [PubMed] [Google Scholar]
- Drell, T. , Larionova, A. , Voor, T. , Simm, J. , Julge, K. , Heilman, K. , et al (2015) Differences in gut microbiota between atopic and healthy children. Curr Microbiol 71: 177–183. [DOI] [PubMed] [Google Scholar]
- Dubourg, G. , Lagier, J.C. , Armougom, F. , Robert, C. , Audoly, G. , Papazian, L. , and Raoult, D. (2013) High‐level colonisation of the human gut by Verrucomicrobia following broad‐spectrum antibiotic treatment. Int J Antimicrob Agents 41: 149–155. [DOI] [PubMed] [Google Scholar]
- Escobar, J.S. , Klotz, B. , Valdes, B.E. , and Agudelo, G.M. (2014) The gut microbiota of Colombians differs from that of Americans, Europeans and Asians. BMC Microbiol 14: 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everard, A. , Belzer, C. , Geurts, L. , Ouwerkerk, J.P. , Druart, C. , Bindels, L.B. , et al (2013) Cross‐talk between Akkermansia muciniphila and intestinal epithelium controls diet‐induced obesity. Proc Natl Acad Sci USA 110: 9066–9071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forslund, K. , Hildebrand, F. , Nielsen, T. , Falony, G. , Le Chatelier, E. , Sunagawa, S. , et al (2015) Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528: 262–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gharaibeh, R.Z. and Jobin, C. (2018) Microbiota and cancer immunotherapy: in search of microbial signals. Gut. 10.1136/gutjnl-2018-317220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez‐Gallego, C. , Collado, M.C. , Perez, G. , Ilo, T. , Jaakkola, U.M. , Bernal, M.J. , et al (2014) Resembling breast milk: influence of polyamine‐supplemented formula on neonatal BALB/cOlaHsd mouse microbiota. Br J Nutr 111: 1050–1058. [DOI] [PubMed] [Google Scholar]
- Gomez‐Gallego, C. , Pohl, S. , Salminen, S. , De Vos, W.M. , and Kneifel, W. (2016) Akkermansia muciniphila: a novel functional microbe with probiotic properties. Benef Microbes 7: 571–584. [DOI] [PubMed] [Google Scholar]
- Gopalakrishnan, V. , Spencer, C.N. , Nezi, L. , Reuben, A. , Andrews, M.C. , Karpinets, T.V. , et al (2018) Gut microbiome modulates response to anti‐PD‐1 immunotherapy in melanoma patients. Science (New York, N.Y.) 359: 97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grander, C. , Adolph, T.E. , Wieser, V. , Lowe, P. , Wrzosek, L. , Gyongyosi, B. , et al (2018) Recovery of ethanol‐induced Akkermansia muciniphila depletion ameliorates alcoholic liver disease. Gut 67: 891–901. [DOI] [PubMed] [Google Scholar]
- Guo, X. , Li, S. , Zhang, J. , Wu, F. , Li, X. , Wu, D. , et al (2017) Genome sequencing of 39 Akkermansia muciniphila isolates reveals its population structure, genomic and functional diversity, and global distribution in mammalian gut microbiotas. BMC Genom 18: 800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hai, N.V. (2015) The use of probiotics in aquaculture. J Appl Microbiol 119: 917–935. [DOI] [PubMed] [Google Scholar]
- Hakansson, A. , Tormo‐Badia, N. , Baridi, A. , Xu, J. , Molin, G. , Hagslatt, M.L. , et al (2015) Immunological alteration and changes of gut microbiota after dextran sulfate sodium (DSS) administration in mice. Clin Exp Med 15: 107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanninen, A. , Toivonen, R. , Poysti, S. , Belzer, C. , Plovier, H. , Ouwerkerk, J.P. , et al (2018) Akkermansia muciniphila induces gut microbiota remodelling and controls islet autoimmunity in NOD mice. Gut 67: 1445–1453. [DOI] [PubMed] [Google Scholar]
- Hansen, C.H. , Krych, L. , Nielsen, D.S. , Vogensen, F.K. , Hansen, L.H. , Sorensen, S.J. , et al (2012) Early life treatment with vancomycin propagates Akkermansia muciniphila and reduces diabetes incidence in the NOD mouse. Diabetologia 55: 2285–2294. [DOI] [PubMed] [Google Scholar]
- Kang, C.S. , Ban, M. , Choi, E.J. , Moon, H.G. , Jeon, J.S. , Kim, D.K. , et al (2013) Extracellular vesicles derived from gut microbiota, especially Akkermansia muciniphila, protect the progression of dextran sulfate sodium‐induced colitis. PLoS One 8: e76520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson, C.L. , Onnerfalt, J. , Xu, J. , Molin, G. , Ahrne, S. and Thorngren‐Jerneck, K. (2012) The microbiota of the gut in preschool children with normal and excessive body weight. Obesity (Silver Spring, Md.) 20: 2257–2261. [DOI] [PubMed] [Google Scholar]
- Kim, B.S. , Song, M.Y. , and Kim, H. (2014) The anti‐obesity effect of Ephedra sinica through modulation of gut microbiota in obese Korean women. J Ethnopharmacol 152: 532–539. [DOI] [PubMed] [Google Scholar]
- Lagier, J.C. , Hugon, P. , Khelaifia, S. , Fournier, P.E. , La Scola, B. , and Raoult, D. (2015) The rebirth of culture in microbiology through the example of culturomics to study human gut microbiota. Clin Microbiol Rev 28: 237–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Poul, E. , Loison, C. , Struyf, S. , Springael, J.Y. , Lannoy, V. , Decobecq, M.E. , et al (2003) Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. J Biol Chem 278: 25481–25489. [DOI] [PubMed] [Google Scholar]
- Lee, H. , and Ko, G. (2014) Effect of metformin on metabolic improvement and gut microbiota. Appl Environ Microbiol 80: 5935–5943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, J. , Lin, S. , Vanhoutte, P.M. , Woo, C.W. , and Xu, A. (2016) Akkermansia muciniphila protects against atherosclerosis by preventing metabolic endotoxemia‐induced inflammation in apoe‐/‐ mice. Circulation 133: 2434–2446. [DOI] [PubMed] [Google Scholar]
- Lukovac, S. , Belzer, C. , Pellis, L. , Keijser, B.J. , de Vos, W.M. , Montijn, R.C. and Roeselers, G. (2014) Differential modulation by Akkermansia muciniphila and Faecalibacterium prausnitzii of host peripheral lipid metabolism and histone acetylation in mouse gut organoids. MBio 5: e01438–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowski, K.M. , Vieira, A.T. , Ng, A. , Kranich, J. , Sierro, F. , Yu, D. , et al (2009) Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461: 1282–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson, V. , Fessler, J. , Bao, R. , Chongsuwat, T. , Zha, Y. , Alegre, M.L. , et al (2018) The commensal microbiome is associated with anti‐PD‐1 efficacy in metastatic melanoma patients. Science (New York, N.Y.) 359: 104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, R.S. , and Hoskins, L.C. (1981) Mucin degradation in human colon ecosystems. Fecal population densities of mucin‐degrading bacteria estimated by a “most probable number” method. Gastroenterology 81: 759–765. [PubMed] [Google Scholar]
- Nieuwdorp, M. , Gilijamse, P.W. , Pai, N. , and Kaplan, L.M. (2014) Role of the microbiome in energy regulation and metabolism. Gastroenterology 146: 1525–1533. [DOI] [PubMed] [Google Scholar]
- Ottman, N. , Davids, M. , Suarez‐Diez, M. , Boeren, S. , Schaap, P.J. , Martins Dos Santos, V.A.P. , et al (2017a) Genome‐scale model and omics analysis of metabolic capacities of akkermansia muciniphila reveal a preferential mucin‐degrading lifestyle. Appl Environ Microbiol 83: e01014–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottman, N. , Reunanen, J. , Meijerink, M. , Pietila, T.E. , Kainulainen, V. , Klievink, J. , et al (2017b) Pili‐like proteins of Akkermansia muciniphila modulate host immune responses and gut barrier function. PLoS One 12: e0173004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouwerkerk, J.P. , Aalvink, S. , Belzer, C. , and De Vos, W.M. (2017a) Preparation and preservation of viable Akkermansia muciniphila cells for therapeutic interventions. Benef Microbes 8: 163–169. [DOI] [PubMed] [Google Scholar]
- Ouwerkerk, J.P. , van der Ark, K.C. , Davids, M. , Claassens, N.J. , Robert Finestra, T. , de Vos, W.M. and Belzer, C. (2017. b) Adaptation of Akkermansia muciniphila to the oxic‐anoxic interface of the mucus layer. Appl Environ Microbiol 82: 6983–6993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Passel, M.W. , Kant, R. , Zoetendal, E.G. , Plugge, C.M. , Derrien, M. , Malfatti, S.A. , et al (2011) The genome of Akkermansia muciniphila, a dedicated intestinal mucin degrader, and its use in exploring intestinal metagenomes. PLoS One 6: e16876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plovier, H. , Everard, A. , Druart, C. , Depommier, C. , Van Hul, M. , Geurts, L. , et al (2017) A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med 23: 107–113. [DOI] [PubMed] [Google Scholar]
- Png, C.W. , Linden, S.K. , Gilshenan, K.S. , Zoetendal, E.G. , McSweeney, C.S. , Sly, L.I. , et al (2010) Mucolytic bacteria with increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria. Am J Gastroenterol 105: 2420–2428. [DOI] [PubMed] [Google Scholar]
- Qin, J. , Li, R. , Raes, J. , Arumugam, M. , Burgdorf, K.S. , Manichanh, C. , et al (2010) A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464: 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin, J. , Li, Y. , Cai, Z. , Li, S. , Zhu, J. , Zhang, F. , et al (2012) A metagenome‐wide association study of gut microbiota in type 2 diabetes. Nature 490: 55–60. [DOI] [PubMed] [Google Scholar]
- Rajilic‐Stojanovic, M. , and de Vos, W.M. (2014) The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol Rev 38: 996–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajilic‐Stojanovic, M. , Shanahan, F. , Guarner, F. , and de Vos, W.M. (2013) Phylogenetic analysis of dysbiosis in ulcerative colitis during remission. Inflamm Bowel Dis 19: 481–488. [DOI] [PubMed] [Google Scholar]
- Remely, M. , Hippe, B. , Geretschlaeger, I. , Stegmayer, S. , Hoefinger, I. , and Haslberger, A. (2015a) Increased gut microbiota diversity and abundance of Faecalibacterium prausnitzii and Akkermansia after fasting: a pilot study. Wien Klin Wochenschr 127: 394–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remely, M. , Tesar, I. , Hippe, B. , Gnauer, S. , Rust, P. , and Haslberger, A.G. (2015b) Gut microbiota composition correlates with changes in body fat content due to weight loss. Benef Microbes 6: 431–439. [DOI] [PubMed] [Google Scholar]
- Reunanen, J. , Kainulainen, V. , Huuskonen, L. , Ottman, N. , Belzer, C. , Huhtinen, H. , et al (2015) Akkermansia muciniphila adheres to enterocytes and strengthens the integrity of the epithelial cell layer. Appl Environ Microbiol 81: 3655–3662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Routy, B. , Le Chatelier, E. , Derosa, L. , Duong, C.P.M. , Alou, M.T. , Daillere, R. , et al (2018) Gut microbiome influences efficacy of PD‐1‐based immunotherapy against epithelial tumors. Science (New York, N.Y.) 359: 91–97. [DOI] [PubMed] [Google Scholar]
- Santacruz, A. , Collado, M.C. , Garcia‐Valdes, L. , Segura, M.T. , Martin‐Lagos, J.A. , Anjos, T. , et al (2010) Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr 104: 83–92. [DOI] [PubMed] [Google Scholar]
- Schneeberger, M. , Everard, A. , Gómez‐Valadés, A.G. , Matamoros, S. , Ramírez, S. , Delzenne, N.M. , et al (2015) Akkermansia muciniphila inversely correlates with the onset of inflammation, altered adipose tissue metabolism and metabolic disorders during obesity in mice. Sci Rep 5: 16643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin, N.R. , Lee, J.C. , Lee, H.Y. , Kim, M.S. , Whon, T.W. , Lee, M.S. , and Bae, J.W. (2014) An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet‐induced obese mice. Gut 63: 727–735. [DOI] [PubMed] [Google Scholar]
- Singh, D.P. , Singh, J. , Boparai, R.K. , Zhu, J. , Mantri, S. , Khare, P. , et al (2017) Isomalto‐oligosaccharides, a prebiotic, functionally augment green tea effects against high fat diet‐induced metabolic alterations via preventing gut dysbacteriosis in mice. Pharmacol Res 123: 103–113. [DOI] [PubMed] [Google Scholar]
- Song, H. , Chu, Q. , Yan, F. , Yang, Y. , Han, W. , and Zheng, X. (2016) Red pitaya betacyanins protects from diet‐induced obesity, liver steatosis and insulin resistance in association with modulation of gut microbiota in mice. J Gastroenterol Hepatol 31: 1462–1469. [DOI] [PubMed] [Google Scholar]
- Sonoyama, K. , Fujiwara, R. , Takemura, N. , Ogasawara, T. , Watanabe, J. , Ito, H. , and Morita, T. (2009) Response of gut microbiota to fasting and hibernation in Syrian hamsters. Appl Environ Microbiol 75: 6451–6456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonoyama, K. , Ogasawara, T. , Goto, H. , Yoshida, T. , Takemura, N. , Fujiwara, R. , et al (2010) Comparison of gut microbiota and allergic reactions in BALB/c mice fed different cultivars of rice. Br J Nutr 103: 218–226. [DOI] [PubMed] [Google Scholar]
- Swidsinski, A. , Dorffel, Y. , Loening‐Baucke, V. , Theissig, F. , Ruckert, J.C. , Ismail, M. , et al (2011) Acute appendicitis is characterised by local invasion with Fusobacterium nucleatum/necrophorum. Gut 60: 34–40. [DOI] [PubMed] [Google Scholar]
- Teixeira, T.F.S. , Grzeskowiak, L.M. , Salminen, S. , Laitinen, K. , Bressan, J. and Gouveia Peluzio Mdo, C. (2013) Faecal levels of Bifidobacterium and Clostridium coccoides but not plasma lipopolysaccharide are inversely related to insulin and HOMA index in women. Clin Nutrit (Edinburgh, Scotland) 32: 1017–1022. [DOI] [PubMed] [Google Scholar]
- Thomas, L.V. , Ockhuizen, T. , and Suzuki, K. (2014) Exploring the influence of the gut microbiota and probiotics on health: a symposium report. Br J Nutr 112(Suppl. 1): S1–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuomola, E. , Crittenden, R. , Playne, M. , Isolauri, E. , and Salminen, S. (2001) Quality assurance criteria for probiotic bacteria. Am J Clin Nutr 73: 393s–398s. [DOI] [PubMed] [Google Scholar]
- Vigsnaes, L.K. , Brynskov, J. , Steenholdt, C. , Wilcks, A. , and Licht, T.R. (2012) Gram‐negative bacteria account for main differences between faecal microbiota from patients with ulcerative colitis and healthy controls. Benef Microbes 3: 287–297. [DOI] [PubMed] [Google Scholar]
- de Vos, W.M. , and de Vos, E.A. (2012) Role of the intestinal microbiome in health and disease: from correlation to causation. Nutr Rev 70(Suppl. 1): S45–S56. [DOI] [PubMed] [Google Scholar]
- Wang, L. , Christophersen, C.T. , Sorich, M.J. , Gerber, J.P. , Angley, M.T. , and Conlon, M.A. (2011) Low relative abundances of the mucolytic bacterium Akkermansia muciniphila and Bifidobacterium spp. in feces of children with autism. Appl Environ Microbiol 77: 6718–6721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Chen, L. , Zhao, N. , Xu, X. , Xu, Y. , and Zhu, B. (2018a) Of genes and microbes: solving the intricacies in host genomes. Protein Cell 9: 446–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Wiesnoski, D.H. , Helmink, B.A. , Gopalakrishnan, V. , Choi, K. , DuPont, H.L. , et al (2018b) Fecal microbiota transplantation for refractory immune checkpoint inhibitor‐associated colitis. Nat Med 24: 1804–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir, T.L. , Manter, D.K. , Sheflin, A.M. , Barnett, B.A. , Heuberger, A.L. , and Ryan, E.P. (2013) Stool microbiome and metabolome differences between colorectal cancer patients and healthy adults. PLoS One 8: e70803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, X. , Zhang, T. , Chen, X. , Ji, G. , and Zhang, F. (2019) Microbiota transplantation: targeting cancer treatment. Cancer Lett 452: 144‐151. [DOI] [PubMed] [Google Scholar]
- Yu, J. , Feng, Q. , Wong, S.H. , Zhang, D. , Liang, Q.Y. , Qin, Y. , et al (2017) Metagenomic analysis of faecal microbiome as a tool towards targeted non‐invasive biomarkers for colorectal cancer. Gut 66: 70–78. [DOI] [PubMed] [Google Scholar]
- Zackular, J.P. , Baxter, N.T. , Iverson, K.D. , Sadler, W.D. , Petrosino, J.F. , Chen, G.Y. and Schloss, P.D. (2013) The gut microbiome modulates colon tumorigenesis. mBio 4: e00692‐00613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller, G. , Tap, J. , Voigt, A.Y. , Sunagawa, S. , Kultima, J.R. , Costea, P.I. , et al (2014) Potential of fecal microbiota for early‐stage detection of colorectal cancer. Mol Syst Biol 10: 766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, H. , DiBaise, J.K. , Zuccolo, A. , Kudrna, D. , Braidotti, M. , Yu, Y. , et al (2009) Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci USA 106: 2365–2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X. , Shen, D. , Fang, Z. , Jie, Z. , Qiu, X. , Zhang, C. , et al (2013) Human gut microbiota changes reveal the progression of glucose intolerance. PLoS One 8: e71108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu, L. , Qin, S. , Zhai, S. , Gao, Y. and Li, L. (2017) Inulin with different degrees of polymerization modulates composition of intestinal microbiota in mice. FEMS Microbiol Lett 364 10.1093/femsle/fnx075. [DOI] [PubMed] [Google Scholar]


