Abstract
Objective
To evaluate the clinical efficacy of two types of condom uterine balloon tamponade systems, namely Chhattisgarh condom balloon device “CG balloon (CGB)” having a central drainage channel as well as indigenous tying system to fasten condom to the catheter and conventional condom uterine balloon device (C-UBT) as a second-line intervention in post-partum haemorrhage (PPH).
Materials and Methods
The present non-randomised prospective case series was carried out from December 2014 to September 2016 and included 60 women having PPH which was refractory to first-line management and who were treated with either of the two condom balloon tamponade devices prepared on spot. Women with allergy to latex, retained placenta, uterine rupture, anomaly, genital infection and/or malignancy were excluded. Case report forms were filled for all participants and analysed. Primary outcome was arrest of haemorrhage, and one of the secondary outcomes was cost and consistency of the devices.
Results
CGB was used in 46 and C-UBT in 14 women. The overall success rate was 98.33%. The mean blood loss was 1417 mL. Women of C-UBT group had greater blood loss, higher inflation volume and delays due to technical issues (OR 7.6). CGB was cheaper and more consistent than C-UBT by omitting the use of suture material.
Conclusion
CGB and conventional condom balloon tamponade both are easy to use, feasible and efficacious for control of PPH, but CGB condom balloon device has the advantage of a central drainage lumen for real-time assessment of blood loss and therefore early corrective action.
Electronic supplementary material
The online version of this article (10.1007/s13224-018-1185-6) contains supplementary material, which is available to authorized users.
Keywords: Post-partum haemorrhage, Innovative condom balloon tamponade, CG Balloon, Low-resource settings, Maternal mortality
Introduction
Post-partum haemorrhage (PPH) remains the leading cause of death in resource-poor settings. The cause of PPH is atonic uterus in 80% and is primarily managed by medical means, failing which easy but effective interventions are critically needed in these facilities where surgical recourse and blood bank are often unavailable [1]. Uterine balloon tamponade (UBT) is a recommended second-line intervention as least invasive, most rapid and highly effective treatment option [2–5].
The commercially available uterine-specific devices have a prohibitively high cost. Low-resource settings rely on lower-cost adaptations like condom uterine balloon tamponade (C-UBT) [6]. It is NUS (non-uterine specific) device.
The main disadvantage of C-UBT is not having a drainage port and therefore not allowing the real-time assessment of ongoing haemorrhage as blood needs to soak through the yards of vaginal pack to reveal itself. This may lead to delay in resorting to the next step in the management and is a major pitfall [7]. Another drawback is the suture which is used to tie the condom to catheter with inherent problem of loose or tight knot, cutting through the condom and inadequate sterilisation in emergency if the thread is used.
The authors had designed a uterine-specific (US) device named “Chhattisgarh balloon” (CGB). It was designed to overcome both these disadvantages. It can be assembled on the spot [8, 9]. The present study was carried out with the aim to evaluate the clinical efficacy of CGB and C-UBT over 2 years of use.
Materials and Methods
This prospective observational case series was conducted at a Government Hospital in Chhattisgarh (CG), India, from December 2014 to September 2016. An approval for this study was obtained by institutional ethical committee.
The study included women having PPH (defined as loss of > 500 mL, > 1 L in vaginal delivery or caesarean section respectively, and/or deteriorating hemodynamic changes owing to bleeding) refractory to first-line management, namely uterine massage and uterotonics in cases of atonic uterus or failed attempt at surgical repair in lower genital tract tears.
A total of 60 women were included in the study after obtaining informed consent for the procedure. Any of the two devices was prepared on the spot and dipped in antiseptic solution for 3 min before insertion.
The conventional UBT (C-UBT) was assembled by rolling the condom over Foley’s catheter and tied with silk/polyglactin. After vaginal birth, the device was introduced in the uterine cavity with the help of sponge holding forceps under direct vision till the rim of condom disappeared inside. This was followed by gravity-driven insufflation with saline through an infusion set which continued till the balloon conformed to the shape of uterus and/or arrest of bleeding. The distal end of the device was occluded by tying with a suture/clamp/knotting on itself. Vagina was packed with roller gauze.
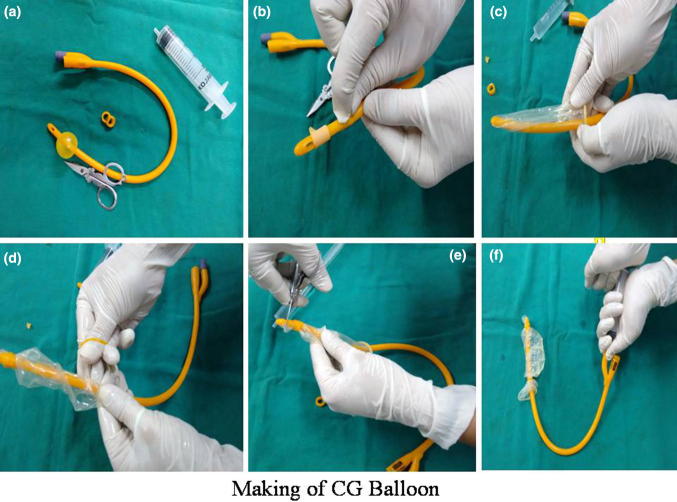
The CG balloon was prepared as per published method [8] (Fig. 1) and introduced in the uterine cavity after holding it between two fingers till the rim of the condom reached external cervical os. This was followed by vaginal packing to prevent expulsion. Inflation was done through the bulb inflation port using syringes in an alternating repetitive manner till haemostasis became evident by observing the ongoing blood loss in the drainage port connected to a collecting bag. Distal end of device did not need occlusion as the saline was self-retained.
Fig. 1.
a Bulb of the Foley’s catheter (20–24 Fr) inflated with 5 mL air excised. b Inflated bulb is excised completely or flaps are everted after cutting circumferentially. c Condom unfolded over proximal one-third of catheter. d Double secure the condom over catheter leaving 1 cm from both the ends of condom using the rings (1–2 mm width) cut from the drainage tube of catheter. e Excise the tip of the Foley’s catheter and condom together. f Balloon is inflated with saline through the bulb inflation port of the catheter by syringes
During caesarean sections, either balloon device was placed in the uterine cavity through uterine incision and catheter shaft was made to traverse through cervical canal into the vagina and was pulled out by an assistant. The balloon was inflated partially. The uterine incision was repaired taking care not to damage the bulb of the device. Further inflation to ensure haemostasis was done after closing the uterine incision but before closing the abdominal wall.
The successful tamponade was defined as arrest of bleeding with inflation of ≤ 500 mL of saline, whereas the failure of tamponade was the persistence of uterine bleeding in spite of inflation volume of 500 mL. After a successful procedure, bladder catheterisation was done and uterine margins were marked. An oxytocin infusion of 10 units in 500 ml of saline was started at the rate of 40 drops per minute for 6–8 h. Broad-spectrum antibiotic coverage was given.
The balloon was deflated 6–24 h later by reversing the distal end occlusion method in C-UBT and withdrawal of saline in CGB. In the absence of recurrence of bleeding in next 30 min, vaginal pack and device were removed.
In case of failure of tamponade, the woman was taken for surgical treatment to arrest haemorrhage.
The woman was followed and monitored in the post-partum period till discharge. Complications such as perforation, pain, pyrexia and infection (uterine tenderness/malodorous vaginal discharge) were noted.
The primary outcome was a successful tamponade.
The secondary outcome measures were average blood loss before balloon insertion, interval between onset of PPH to balloon insertion, inflation volume to create tamponade, inflation to haemostasis interval, tamponade to deflation interval and the cost and consistency of the two devices.
Exclusion criteria were as follows: known allergy to latex, having retained placenta, uterine rupture, genital infection suspected (rupture of membranes for > 18 h) or overt, genital anomaly or malignancy.
Case report forms were filled for all the 60 participants of the study and analysed.
Statistical analysis was performed and analysed using the Statistical Package for Social Sciences (SPSS) version 20 software and presented in figures and tables. Chi-square test was used for comparisons with statistical significance as p value of less than or equal to 0.05.
Result
There were 15764 deliveries in our hospital during the study period. A total of 709 women had PPH and 60 women not responding to first-line interventions were managed with UBT; out of these, CGB was used in 46 (including 13 cases already published [9]) and C-UBT in 14 cases.
Out of 60 women, 48 (80%) delivered vaginally, 44 (73%) were unbooked, 43 (71%) were from rural background, 55 (91.6%) were between the age groups of 18–34 years, five (8.3%) were > 35 years of age, seven (11.6%) were grand multipara, 47 (78%) were anaemic and 48 (80%) delivered at gestational age between 37 and 40 weeks.
The mean values of all 60 cases are given in Table 1. Majority, i.e. 35/60 (58.3%), had blood loss > 1000 mL, whereas 16 (26.6%) had severe haemorrhage (> 2000 mL), the mean being 1417 mL. The mean time between onset of major PPH and balloon insertion was 30 min; however, in eight (13.3%) cases it had to be inserted within 15 min owing to haemodynamic instability resulting out of brisk bleeding and included two cases of bleeding bed of central placenta previa, two after manual removal of placenta, two after reposition of inverted uterus with haemorrhage, one with contraindications to second-line uterotonic agents and one with disseminated intravascular coagulation (DIC).
Table 1.
Demographic and tamponade statistics
| Mean | Standard deviation | Confidence interval | |
|---|---|---|---|
| Age (years) | 24.9833 | ± 3.454 | 21.53–28.43 |
| Gravidity | 2.48 | ± 1.02 | 1.46–3.5 |
| Gestational age (weeks) | 37.4 | ± 2.08 | 35.32–39.48 |
| Pre tamponade blood loss (ml) | 1416.666 | ± 437.284 | 979.38–1853.94 |
| Volume of fluid in tamponade (ml) | 222.583 | ± 41.133 | 181.45–263.71 |
| Time interval from PPH to tamponade insertion (min) | 30.25 | ± 10.495 | 19.755–40.745 |
| Interval from tamponade to haemostasis (min) | 8.75 | ± 5.798 | 3.05–14.45 |
| Time interval from tamponade insertion to removal (h) | 22.85 | ± 5.281 | 17.57–28.13 |
| Total blood transfused (unit) | 2 | ± 0.5 | 1.5–2.5 |
| Duration of stay (days) | 4.53 | ± 1.245 | 3.29–5.77 |
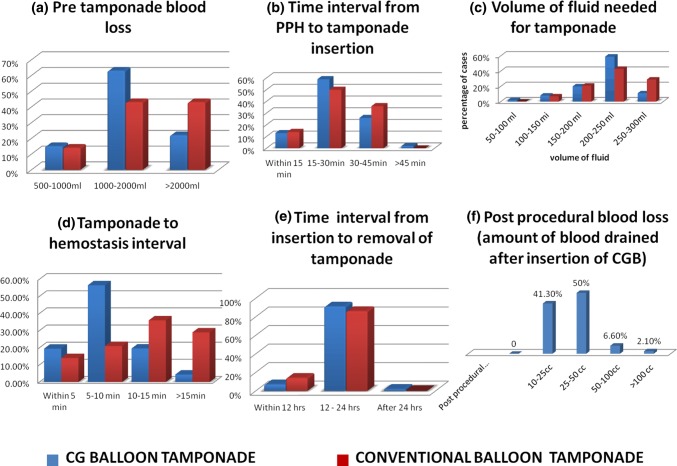
Table 2 shows that atonic PPH was the commonest indication in both the groups. Figure 2 shows the comparison between the C-UBT and CGB groups; there was no significant difference in PPH to tamponade device insertion (1-b) as well as deflation intervals (1-e), whereas more women of the former group had blood loss of > 2000 mL [6 (43%) vs 10 (22%) (p = 0.052, NS)] (1-a), and they also needed > 250 mL of saline to achieve haemostasis [4 (29%) vs 5 (11%) (p = 0.0136, S)] (1-c) and achieved haemostasis in > 15 min in comparison with the later group [4 (29%) vs 2 (4.4%) (p = 0.002, HS)] (1-d).
Table 2.
Indications of tamponade insertion
| Indications of tamponade insertion | CG balloon tamponade (CGB) (n = 46) | Conventional balloon tamponade (C-UBT) (n = 14) | p value | ||
|---|---|---|---|---|---|
| No. of cases | Percentage | No. of cases | Percentage | ||
| Uterine atony | 38 | 82.6 | 13 | 92.8 | 0.198 |
| Jaundice (HeE) | 02 | 4.3 | 00 | 00 | – |
| Placenta previa | 02 | 4.3 | 00 | 00 | – |
| Genital tear | 01 | 2.1 | 01 | 7.2 | 0.233 |
| Secondary PPH | 01 | 2.1 | 00 | 0 | – |
| Uterine inversion (recurrent) | 02 | 4.3 | 0 | 0 | – |
| Total | 46 | 100 | 14 | 100 | |
Fig. 2.
Comparative clinical evaluation of CG balloon and C-UBT
There were instances of delay arising out of failure to inflate due to technical problem in 2 (12.5%) and 1 (2.27%) cases of C-UBT and CGB, respectively (OR 7.6, 95% CI 7.23–7.99). In C-UBT, the cause was loose and tight knot in one case each causing leakage/difficulty during inflation, whereas in CGB, the tip of the catheter was excised too low leading to leakage. In all three cases, the device was withdrawn, reassembled, reinserted, reinflated and ultimately achieved haemostasis.
The overall success rate was 98.33% (59 of 60 cases). One woman of CGB died of DIC and was the only failure [9].
The average post-placement blood loss (measurable in CGB only) was 33.56 mL.
The average cost of C-UBT use was Rs. 400 (approximately $5), and that of CGB was Rs. 120 (approximately $2).
No complications were noted in the either group.
Discussion
“If you can fill that unforgiving minute with worth of 60 s, run”
No statement explains management of PPH better!
To make every second accountable, we followed the protocol of starting prompt resuscitation and measures to achieve haemostasis within one (golden) hour of beginning of major PPH. This reflects in the mean interval of 30 min for inserting the balloon (after failure of first-line management) and being inversely proportional to volume and rate of loss of blood and deteriorating hemodynamic status.
The mean blood loss of 1416 mL (with ongoing haemorrhage) as the threshold of balloon insertion is in accordance with the published guidelines by the California Maternal Quality Care Collaborative (CMQCC) in obstetric haemorrhage [10].
The CMQCC protocol includes medical and obstetric interventions along with transfusion management, according to stages of obstetric haemorrhages defined as four groups: stage 0–3. Stage 0 is every woman in labour, stage 1: blood loss > 500 ml in vaginal or > 1000 ml in caesarean birth, stage 2: continued bleeding with blood loss < 1500 ml and stage 3 total blood loss > 1500 ml. One of the recommended obstetric interventions in “stage 2” haemorrhage is placing intrauterine balloon along with second-line uterotonics after vaginal birth. During caesarean birth, either B-Lynch suture or placing intrauterine balloon may be employed. In stage 3, surgical recourse is the mainstay of treatment.
Various studies have reported mean blood loss ranging between 1200 and 4812 mL [11, 12]. Studies using condom balloon devices have reported lesser mean blood loss as a threshold for second-line intervention as major bleeding may be more detrimental to already anaemic women of developing world which is compounded by the lurking uncertainty of getting blood products in contrast to developed nations. The cost of intervention also differs significantly ($ 200–250 for uterine-specific device vs $5 for C-UBT).
Although our primary intention was to use both devices in equal numbers, soon, a preference to use CGB by the duty doctors was noticed. On analysis, the following facts emerged.
By virtue of its design, CGB was better supported throughout its length along with conical apex of the drainage tip. This facilitated smoother insertion, whereas in C-UBT, the condom tended to fold upon itself near the tip owing to its unsupported segment proximal to catheter tip. The consistent distance from tip of CGB to rim of condom allowed a definite landmark in the form of rim once it reached cervical os while deciding the extent to which the device is to be inserted in the uterus. There was lack of any clear landmark in C-UBT probably due to a varying distance of the catheter tip to rim of condom. The vagina could be packed immediately after placing the CGB in uterine cavity to prevent its expulsion during inflation as the bleeding could be measured at collecting tube. This successfully tackled the issue of expulsion which is a challenge [13]. C-UBT had no drainage port, and vagina had to be packed after haemostasis.
In addition to above observations, the odds of inconsistency owing to use of suture material were higher in C-UBT, whereas CGB assembly used the rings cut out of catheter itself which were optimally tight when wound around twice. Rings had never cut through the condom and were already sterilised. The only mentioned error with CGB assembly never recurred after taking precaution of cutting the tip at the level of drainage hole and not below it. Inconsistencies were inherent problems with C-UBT as tightness of the knot was quite subjective and varied with each assembly.
Less volume of saline was needed for tamponade effect in comparison with C-UBT of our own case series as well those of others [6, 14]. Real-time assessment of the ongoing haemorrhage and filling the balloon with syringes helped in optimising the tamponade volume as impending tamponade was accompanied with increasing resistance felt through syringe used for manual filling.
Lack of drainage channel is a major limitation of C-UBT where bleeding has to soak through yards of gauze of vaginal pack in order to become evident and possibly delaying the next corrective step. In contrast, the CGB allows real-time blood loss assessment and thereby allows stepwise management of PPH to become a reality. It also allows its use for various other indications which are reported in the literature in conjunction with uterine-specific devices only (having the central drainage lumen) [15]. In the present study too, CGB was used in cases of placenta previa, after reposition of inverted uterus and in combination with other methods. The last was in two cases of sandwich surgery, in combination with classical B-Lynch, and could successfully avert hysterectomy.
The two cases of jaundice with PPH were diagnosed as having hepatitis E and had coagulation abnormality. In both the instances, PPH was refractory to oxytocin, and in lieu of relative contraindication to other drugs, CGB was used which arrested uterine bleeding successfully. Out of two cases of lower genital tract tear, one was not accessible for surgical repair but responded to tamponade by CGB [9] and another was of vaginal tear near its apex which bled briskly following attempts of suturing owing to oedematous vagina. In this case, C-UBT was used.
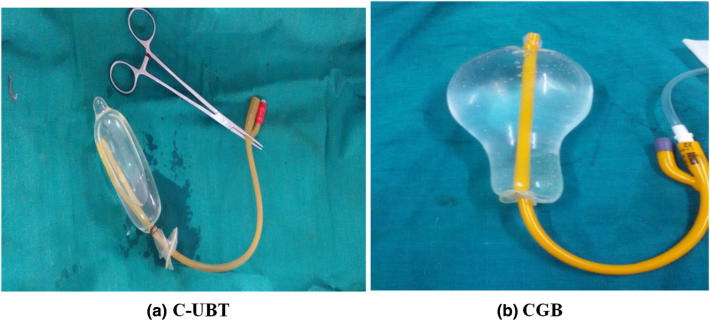
The post-placement blood loss in CGB was less than reported by others [16]. The authors could not find any plausible explanation for this. Blockage of the drainage lumen was ruled out retrospectively after deflation. Probably soft CGB remoulds itself better to post-partum uterus once inflated (Fig. 3). The resultant hydrostatic pressure effect over uterine arteries is supposed to be a mechanism of action of balloon tamponade [4].
Fig. 3.
Comparative images of conventional condom balloon tamponade showing condom tied to catheter with thread, distal end needing occlusion (accomplished with clamp) and without any drainage channel (C-UBT) and CG balloon showing condom fastened to catheter using indigenous rings cut from the catheter itself, distal end not requiring any occlusion as the fluid is self-retained and there is a central drainage channel for real-time assessment of ongoing blood loss
Our success rate of 98.33 is in accordance with the studies done over last 10 years using condom balloon tamponade with overall success rate of 96.75% (Table 3) [6, 11, 14, 17–24]. Initial report from India on condom balloon tamponade dates back to 2003, where in authors had reported 94.05% success rates [25].
Table 3.
Studies showing the use of condom balloon tamponade during last 10 years
| Author/country | Setting | Year | Method | No of cases | Success of tamponade | % of success |
|---|---|---|---|---|---|---|
|
Bagga et al. [17] India |
PGI Chandigarh |
2007 | Condom catheter | 2 | 2 of 2 | 100 |
|
Sheikh et al. [21] Pakistan |
Aga Khan University Karachi | 2008 | Undefined condom catheter | 15 | 15 of 15 | 100 |
|
Nahar et al. [18] Bangladesh |
Rajshahi Med. College Hospital | 2009 | Condom catheter | 53 | 52 of 53 (one c/o eclampsia died of DIC) | 98.11 |
|
Thapa et al. [11] Nepal |
P. Women’s Hospital, Thapathali | 2010 | Condom catheter | 14 | 14 of 14 | 100 |
|
Rather et al. [14] India |
Med. College Hospital Srinagar | 2010 | Condom catheter (red rubber) | 26 | 25 of 26 (one required Hysterectomy) | 96.2 |
|
Manaktala [19] India |
Lok Nayak Hospital | 2011 | Condom catheter | 2 | 2 of 2 | 100 |
|
Rathore [20] India |
Teaching Hospital | 2012 | Condom catheter | 18 | 17 of 18 | 94 |
|
Tort et al. [22] Benin, France |
(Feasibility study for RCT) | 2013 | Condom catheter + misoprostol | 5 | 5 of 5 (exact outcome NA) | 100 |
|
Ranatunga [6] Shri Lanka |
Castle Street Hosp, Colombo | 2013 | Condom catheter | 42 | 40 of 42 (two needed hysterectomy) | 95.2 |
|
Maya et al. [24] Africa |
College of Health S, Ghana | 2015 | Condom catheter (cervical suture/to prevent expulsion) | 3 | 3 of 3 | 100 |
|
Hasabe et al. [23] India |
NIMS Med College, Jaipur | 2016 | Condom catheter | 36 | 34 of 36 (B-Lynch in one and hysterectomy in another needed) | 94.44 |
|
Present study India |
Pt JNMMC, Raipur, CG | CGB and conventional C-UBT | 60 | 59 of 60 (one case died of DIC) | 98.33 | |
| Total | 12 | 277 | 268 | 96.75 |
In C-UBT, if the thread is used to reduce cost, optimal sterilisation remains questionable in emergency. The cost of CGB is nearly three times less than C-UBT prepared using polyglactin or silk and even lesser than pre-assembled (ESM-UBT™) device [26].
Conclusion
The present study found that both the modified and conventional condom balloon uterine tamponade devices are easy to use, feasible and efficacious for control of PPH, but the Chattisgarh condom balloon device has the advantage of a central drainage lumen for real-time assessment of blood loss and therefore early corrective action along with more consistent assembly with reproducibility, ease of insertion and tamponade with lesser inflation volume. Replacing suture material with indigenous rings prepared by cutting the same from urinary drainage port of the catheter itself ensures sterilised strings and reducing the cost of device 3–4 times in comparison with C-UBT. It is 100 times cheaper than commercially available uterine-specific devices having a drainage port. It can fill a critical gap between uterine-specific and non-specific devices in the management of PPH due to variety of causes in low-resource settings.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Inconsistencies in assembly and use of conventional condom balloon tamponade prepared by tying the condom over catheter by suture material. The knot strength varies with operator, and the video shows leaking of the saline due to loose knot when the balloon is inflated. When the knot is very tight, it precludes inflation as is shown by no flow of saline through the infusion set. The distal end has to be occluded and is shown by three methods: by tying a thread, by tying a knot in catheter itself or by a clamp. (WMV 21326 kb)
Use of CG balloon for PPH management. Video shows a PPH simulation no responding to first-line management. A CG balloon is assembled, vagina is retracted by big speculum, and anterior lip of cervix is grasped with sponge holding forceps. The CGB is kept between and along two fingers and inserted into the uterine cavity till the rim of the condom is at the level of cervical os. CGB is now inflated with saline through the bulb inflation port by alternating syringes. The inflated balloon is shown in the simulated uterine cavity. The arrest of bleeding is judged through real-time blood loss assessment through the drainage tube of catheter attached to a collecting bag. Vagina is packed; bladder is catheterised. Note: Vagina can be packed after placement of device into the uterine cavity so as to prevent expulsion during inflation. (WMV 10607 kb)
Use of CGB in combination with other method. The video shows a “Uterine sandwich surgery” combining intrauterine balloon tamponade with classical B-Lynch suture in a grand multipara anaemic woman who delivered twins by caesarean section. She had intractable bleeding due to uterine atony, not responding to any uterotonic agent or to B-Lynch suture alone which is shown to be in place already, the CGB is inserted through the uterine incision, and the catheter shaft is made to traverse through cervical canal in a retrograde manner and is pulled out by an assistant through vaginal route. The balloon is shown to be inflated partially (with 50 mL) to prevent displacement through the patulous cervical os. The B-Lynch suture is the tied and uterine incision is closed taking care not to rupture the balloon. The uterus is shown after repair of incision and with classical B-Lynch as well as CGB in situ. The bleeding is reassessed which is shown to be continuing in the drainage channel connected to the bag. Further inflation of CGB is done till arrest of bleeding (achieved at 180 mL). The abdominal wall is closed after haemostasis. (WMV 21646 kb)
Nalini Mishra
is MD, DGO, DNB (O&G), MNAMS, FICOG and is currently working as Professor, Department of Obstetrics and Gynaecology, Government Medical College, Chhattisgarh, India. She is a Master Trainer of Emergency Obstetric Care (EmOC). She has participated as invited Guest Faculty in various international and national conferences. She was a National Faculty for FOGSI PPH workshops in 2016. She has the innovation of C. G Balloon Uterine Tamponade to her credit. She has 45 publications in various journals and books of International & National repute. She was Editor-in-Chief, Souvenir North zone Yuva FOGSI 2011 and Co-Editor of two books including a handbook of obstetric emergencies and a monogram on HRT. She has keen interest in high-risk pregnancy.
Compliance with Ethical Standards
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with ethical standard of the responsible committee on human experiments (institutional and national) and with the 1975 Declaration of Helsinki, as revised in 2008(5). Informed consent was obtained from all patients for being included in the study.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Nalini Mishra is currently working as Professor, Kanchan Gulabani is working as Resident Medical Officer, Sumi Agrawal is working as Assistant Professor, and Chandrashekhar Shrivastava is working as Associate professor in the Dept of O&G, Pt JNM Med College, Raipur, Chhattisgarh, India.
Contributor Information
Nalini Mishra, Email: drmishranalini@gmail.com.
Kanchan Gulabani, Email: drkanchanjaiswani@gmail.com.
Sumi Agrawal, Email: creamy08@gmail.com.
Chandrashekhar Shrivastava, Email: chandan_1708@yahoo.co.in.
References
- 1.Tindell K, Garfinkel R, Abu-Haydar E, et al. Uterine balloon tamponade for the treatment of postpartum haemorrhage in resource-poor settings: a systematic review. BJOG. 2013;120:5–14. doi: 10.1111/j.1471-0528.2012.03454.x. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva: World Health Organization (WHO); 2012. [PubMed] [Google Scholar]
- 3.FIGO FIGO guidelines: prevention and treatment of postpartum hemorrhage in low-resource settings. Int J Gynaecol Obstet. 2012;117:108–118. doi: 10.1016/j.ijgo.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Georgiou C. A review of current practice in using Balloon Tamponade Technology in the management of postpartum haemorrhage. Hypertens Res Pregnancy. 2014;2:1–10. doi: 10.14390/jsshp.2.1. [DOI] [Google Scholar]
- 5.Doumouchtsis SK, Papageorghiou AT, Arulkumaran S. Systematic review of conservative management of postpartum hemorrhage: what to do when medical treatment fails. Obstet Gynecol Surv. 2007;62:540–547. doi: 10.1097/01.ogx.0000271137.81361.93. [DOI] [PubMed] [Google Scholar]
- 6.Ranathunga GA. Post partum haemorrhage, severe acute maternal morbidity and the condom catheter uterine tamponade [D A Ranasinghe Oration 2013] Sri Lanka J Obstet Gynaecol. 2013;35(4):100–111. doi: 10.4038/sljog.v35i4.6582. [DOI] [Google Scholar]
- 7.Lombaard H, Pattinson RC. Common errors and remedies in managing postpartum haemorrhage. Best Pract Res Clin Obstet Gynaecol. 2009;23(3):317–326. doi: 10.1016/j.bpobgyn.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Mishra N, Shrivastava C, Agrawal S. Gulabani K The CG balloon is an innovative condom balloon tamponade for the management of postpartum hemorrhage in low-resource settings. Int J Gynecol Obstet. 2016;133(3):377–378. doi: 10.1016/j.ijgo.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Mishra N, Agrawal S, Gulabani K, et al. Use of an innovative condom balloon tamponade in postpartum haemorrhage: a report. J Obstet Gynecol India. 2016;66(1):63–67. doi: 10.1007/s13224-015-0818-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.California Maternal Quality Care Collaborative. Obstetric hemorrhage: new strategies, new protocol: American congress of obstetricians and gynecologists (ACOG); 2012. Accessed 26 March 2015.
- 11.Thapa K, Malla B, Pandey S, et al. Intrauterine condom tamponade in management of post partum haemorrhage. J Nepal Health Res Counc. 2010;8:19–22. [PubMed] [Google Scholar]
- 12.Grönvall M, Tikkanen M, Tallberg E, et al. Use of Bakri balloon tamponade in the treatment of cases having PPH in the treatment of postpartum hemorrhage: a series of 50 cases from a tertiary teaching hospital. Acta Obstet Gynecol Scand. 2013;92:433–438. doi: 10.1111/j.1600-0412.2012.01531.x. [DOI] [PubMed] [Google Scholar]
- 13.Jain V. Placement of a cervical cerclage in combination with an intrauterine balloon catheter to arrest postpartum haemorrhage. Am J Obstet Gynecol. 2011;205:e15–e17. doi: 10.1016/j.ajog.2011.01.051. [DOI] [PubMed] [Google Scholar]
- 14.Rather SY, Qadir A, Parveen S, et al. Use of condom to control intractable PPH. JK Sci. 2010;12:127–129. [Google Scholar]
- 15.Nelson WL, O’Brien JM. The uterine sandwich for persistent uterine atony: combining the B-Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol. 2007;196(5):e9–e10. doi: 10.1016/j.ajog.2006.10.887. [DOI] [PubMed] [Google Scholar]
- 16.Gao Y, Wang Z, Zhang J, et al. Efficacy and safety of intrauterine Bakri balloon tamponade in the treatment of postpartum hemorrhage: a multicenter analysis of 109 cases. Zhonghua Fu Chan Ke Za Zhi. 2014;49(9):670–675. [PubMed] [Google Scholar]
- 17.Bagga R, Jain V, Sharma S, et al. Postpartum hemorrhage in two women with impaired coagulation successfully managed with condom catheter tamponade. Indian J Med Sci. 2007;61(3):157–160. doi: 10.4103/0019-5359.30752. [DOI] [PubMed] [Google Scholar]
- 18.Nahar N, Yusuf N, Ashraf F. Role of intrauterine balloon catheter in controlling massive PPH: experience in Rajshahi Medical College Hospital. Orion Med J. 2009;2:682–683. [Google Scholar]
- 19.Manaktala U, Dubey C, Takkar A, et al. Condom catheter balloon in management of massive nontraumatic postpartum haemorrhage during cesarean section. J Gynecol Surg. 2011;27:115–117. doi: 10.1089/gyn.2010.0033. [DOI] [Google Scholar]
- 20.Rathore AM, Gupta S, Manaktala U, et al. Uterine tamponade using condom catheter balloon in the management of non-traumatic postpartum hemorrhage. J Obstet Gynaecol Res. 2012;38(9):1162–1167. doi: 10.1111/j.1447-0756.2011.01843.x. [DOI] [PubMed] [Google Scholar]
- 21.Sheikh L, Najmi N, Khalid U, et al. Evaluation of compliance and outcomes of a management protocol for massive postpartum hemorrhage at a tertiary care hospital in Pakistan. BMC Pregnancy Childbirth. 2011;11(1):28. doi: 10.1186/1471-2393-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tort J, Hounkpatin B, Popowski T, et al. A randomized controlled trial to test the effectiveness of intrautetine balloon tamponade with condom catheter in severe postpartum hemorrhage management: a feasibility study in Benin. J Women’s Health Care. 2013;2:135. doi: 10.4172/2167-0420.1000135. [DOI] [Google Scholar]
- 23.Hasabe R, Gupta Rathode P. Use of condom tamponade to manage massive obstetric hemorrhage at a tertiary center in Rajasthan. J Obstet Gynecol India. 2016;66(S1):S88–S93. doi: 10.1007/s13224-015-0790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maya ET, Buntugu KA, Ako L, et al. Condom Tamponade in the Management of Primary Postpartum Haemorrhage: A Report of three cases in Ghana African Journal of Reproductive Health september. 2015;19(1):151–157. [PubMed] [Google Scholar]
- 25.Shivkar KS, Khadilkar SS, Gandhewar M. Pressure balloon therapy in uncontrolled obstetrical haemorrhage. J Obstet Gynecol India. 2003;53:338–341. [Google Scholar]
- 26.Burke TF, Ahn R, Nelson BD, et al. A postpartum haemorrhage package with condom uterine balloon tamponade: a prospective multi-centre case series in Kenya, Sierra Leone, Senegal, and Nepal. BJOG. 2016;123:1532–1540. doi: 10.1111/1471-0528.13550. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Inconsistencies in assembly and use of conventional condom balloon tamponade prepared by tying the condom over catheter by suture material. The knot strength varies with operator, and the video shows leaking of the saline due to loose knot when the balloon is inflated. When the knot is very tight, it precludes inflation as is shown by no flow of saline through the infusion set. The distal end has to be occluded and is shown by three methods: by tying a thread, by tying a knot in catheter itself or by a clamp. (WMV 21326 kb)
Use of CG balloon for PPH management. Video shows a PPH simulation no responding to first-line management. A CG balloon is assembled, vagina is retracted by big speculum, and anterior lip of cervix is grasped with sponge holding forceps. The CGB is kept between and along two fingers and inserted into the uterine cavity till the rim of the condom is at the level of cervical os. CGB is now inflated with saline through the bulb inflation port by alternating syringes. The inflated balloon is shown in the simulated uterine cavity. The arrest of bleeding is judged through real-time blood loss assessment through the drainage tube of catheter attached to a collecting bag. Vagina is packed; bladder is catheterised. Note: Vagina can be packed after placement of device into the uterine cavity so as to prevent expulsion during inflation. (WMV 10607 kb)
Use of CGB in combination with other method. The video shows a “Uterine sandwich surgery” combining intrauterine balloon tamponade with classical B-Lynch suture in a grand multipara anaemic woman who delivered twins by caesarean section. She had intractable bleeding due to uterine atony, not responding to any uterotonic agent or to B-Lynch suture alone which is shown to be in place already, the CGB is inserted through the uterine incision, and the catheter shaft is made to traverse through cervical canal in a retrograde manner and is pulled out by an assistant through vaginal route. The balloon is shown to be inflated partially (with 50 mL) to prevent displacement through the patulous cervical os. The B-Lynch suture is the tied and uterine incision is closed taking care not to rupture the balloon. The uterus is shown after repair of incision and with classical B-Lynch as well as CGB in situ. The bleeding is reassessed which is shown to be continuing in the drainage channel connected to the bag. Further inflation of CGB is done till arrest of bleeding (achieved at 180 mL). The abdominal wall is closed after haemostasis. (WMV 21646 kb)