Abstract
HPV infection is one of the most commonly transmitted diseases among the global population. While it can be asymptomatic, non-genital HPV infection often gives rise to cutaneous warts, which are benign growths arising from the epidermal layer of the skin. This study aimed to produce a global analysis of the ways in which cutaneous wart formation affected the CpG island methylome. The Infinium MethylationEPIC BeadChip microarray was utilized in order to quantitatively interrogate CpG island methylation in genomic DNA extracted from 24 paired wart and normal skin samples. Differential methylation analysis was carried out by means of assigning a combined rank score using RnBeads. The 1000 top-ranking CpG islands were then subject to Locus Overlap Analysis (LOLA) for enrichment of genomic ranges, while signaling pathway analysis was carried out on the top 100 differentially methylated CpG islands. Differential methylation analysis illustrated that the most differentially methylated CpG islands in warts lay within the ITGB5, DTNB, RBFOX3, SLC6A9, and C2orf27A genes. In addition, the most enriched genomic region sets in warts were Sheffield’s tissue-clustered DNase hypersensitive sites, ENCODE’s segmentation and transcription factor binding sites, codex sites, and the epigenome sites from cistrome. Lastly, signaling pathway analysis showed that the GRB2, GNB1, NTRK1, AXIN1, and SKI genes were the most common regulators of the genes associated with the top 100 most differentially methylated CpG islands in warts. Our study shows that HPV-induced cutaneous warts have a clear CpG island methylation profile that sets them apart from normal skin. Such a finding could account for the temporary nature of warts and the capacity for individuals to undergo clinical remission.
Keywords: HPV, warts, DNA methylation, CpG, epigenetics
1. Introduction
The human papillomaviruses (HPV) comprise a diverse family of DNA viruses that infect a number of avian, mammalian, and reptilian species [1]. Over 170 types of HPV have been fully characterized, and these types can either infect the cutaneous integumentary system or the mucosal linings of the human body [2]. Additionally, the aforementioned HPV types can be classified as low- or high-risk depending on their carcinogenic potential [3]. In immunocompetent individuals, cutaneous HPV infection often manifests as benign tumors known as warts, which are common among the general population and children in particular [4]. Nonetheless, reports indicate that the presence of cutaneous HPV types is implicated in the development of keratinocyte cancers such as squamous cell carcinomas [5]. In fact, HPV infection has been associated with modulated oral, oropharyngeal, and laryngeal squamous cell carcinoma risk and prognoses in various populations [6,7,8,9]. Furthermore, reports have shown that such HPV-associated cancers are associated with changes in epigenetic processes, namely DNA methylation [3,10,11].
DNA methylation (DNA-m) is an epigenetic phenomenon that most commonly involves the transfer of methyl groups to the cytosines of CpG dinucleotide sites, which is a process that can be reversed and/or inherited by subsequent generations [12]. Maintaining certain patterns of DNA-m is essential for normal cell- and tissue-specific expression, and differences in DNA-m contribute to the natural variation found between discrete human populations [13]. The vast majority (70–80%) of CpG sites in humans are methylated, rendering them transcriptionally silent [14]. However, unmethylated CpG sites are mostly found in 1000-bp-long, GC-rich clusters known as CpG islands, the latter of which are associated with the majority of annotated gene promoters in the human genome and are strongly correlated with the initiation of transcription [15]. Aberrant CpG island methylation patterns have been reported for a number of human diseases, including many types of cancer as well as HPV infection [16,17,18].
Owing to the well-established link between certain HPV types and cervical cancer, the focus of epigenetic HPV research has been on those types that infect the cervical epithelia [19]. HPV-mediated DNA methylation has been implicated in the etiology of cervical cancer as well as keratinocyte cancer [18,20,21,22]. Similarly, the methylation status of HPV DNA itself has been explored, with studies showing that methylation levels differed between HPV types and that methylation at certain CpG sites could act as a cervical precancer biomarker [23,24]. In contrast to HPV-associated cancers, warts have been the subject of considerably less attention and research on the molecular level. However, the transient nature of warts strongly suggests that there are HPV-induced epigenetic changes in the methylation patterns of CpG islands, the latter of which are mostly found in the promoter regions of genes [25]. To the best of the authors’ knowledge, no previously published study has addressed or compared CpG methylation patterns in benign HPV-induced cutaneous warts compared to healthy skin. Therefore, the aim of the present study was to investigate the levels of methylation at CpG sites in cutaneous skin with and without HPV infection.
2. Results
2.1. Sample Clustering
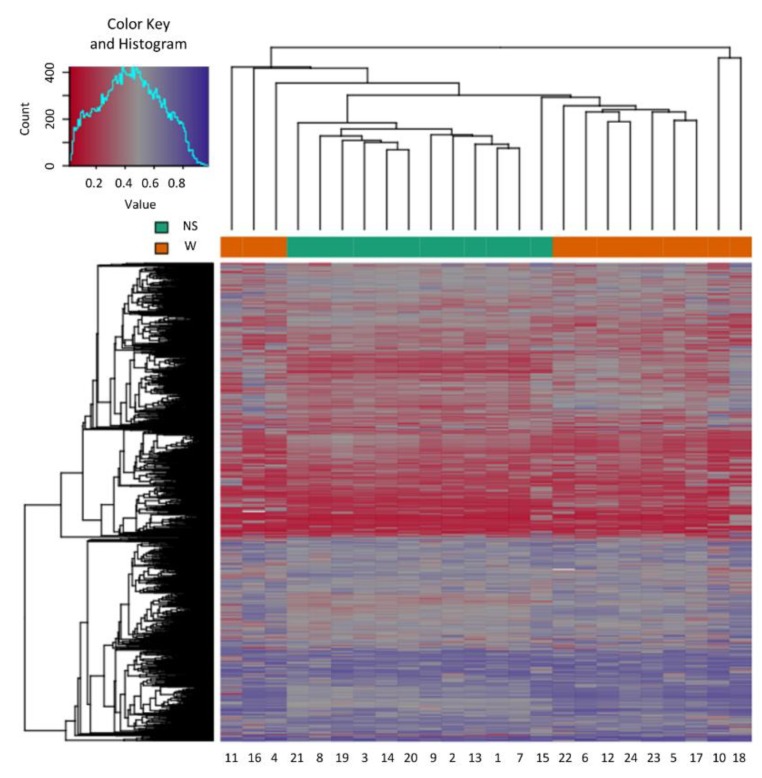
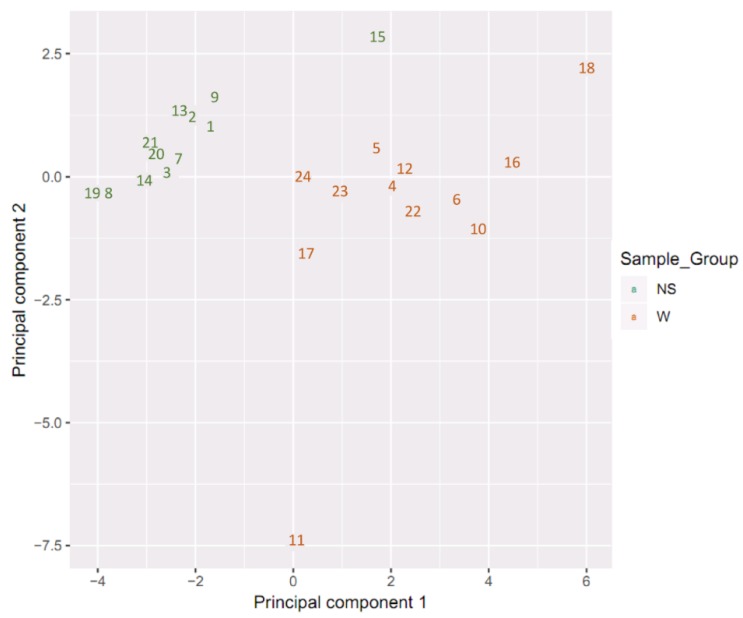
Samples showed an expected clustering based on all methylation values of the top 1000 most variable loci (Figure 1). Samples sharing similar methylation patterns or phenotypes tended to cluster together. Additionally, the dataset was subjected to principal component analysis (PCA) in order to inspect for a strong signal in the methylation values of the samples (Figure 2). PCA confirmed that the difference between warts (W) and normal skin (NS) dominates the analysis.
Figure 1.
Heatmap showing the hierarchal clustering of the 1000 most variable loci with the highest variance across the wart (W) and normal skin (NS) samples. Clustering incorporated average linkage and Manhattan distance. The numbers at the bottom horizontal axis (1 to 24) stand for the patient samples.
Figure 2.
Scatter plot showing normal skin (NS) and wart (W) samples’ coordinates on the first and second principal components. Discrimination between the NS and W samples is shown as in indicated by the color capture.
2.2. Differential Methylation of CpG Islands
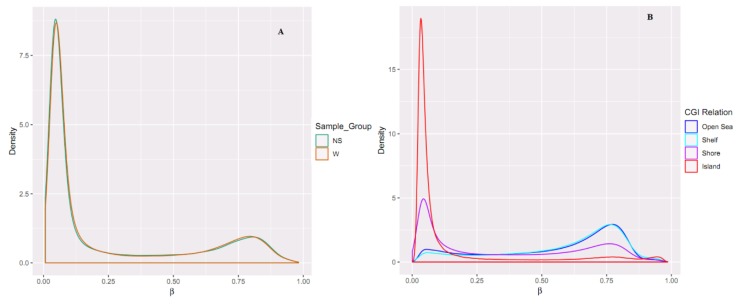
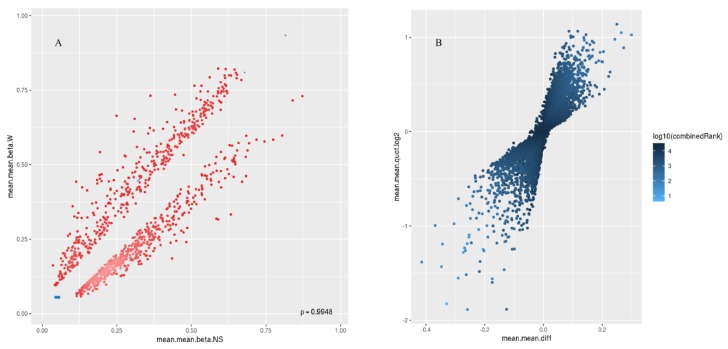
A total of 866,895 probes included in the MethylationEPIC array were processed with the RnBeads Bioconductor package. We excluded probes that overlapped with single nucleotide polymorphisms (SNPs) (n = 17,371), probes of highest impurity (n = 2310), and probes of the specified contexts (n = 2980). A total of 844,234 probes were retained, of which a total of 26,550 CpG islands passed quality control and pre-processing. The assessment of methylation value distributions of the CpG islands for W and NS showed notable differences in β values (Figure 3A). Also, more methylation was observed in the CpG islands compared to other CpG contents (open sea, shelf, and shore) (Figure 3B). The list of DM CpG islands in W was limited to the top-ranking 1000 CpG islands using the “combined rank score”. Using this scoring method, 550 CpG islands were found to be hypomethylated and 450 CpG islands were hypermethylated in W compared to NS, with a mean β difference ≥ 0.046 and ≤−0.046, and a p-value ≤ 0.006 (adjusted p-value ≤ 0.076) (Figure 4A). Of the 550 hypomethylated CpG islands, the β difference ranged from −0.046 to −0.300, and of the 450 hypermethylated CpG islands, the β difference ranged from 0.046 to 0.414. The log2 of the quotient in methylation between W and NS had a maximum value of 1.888 and minimum value of −1.138 (Figure 4B). The top 100 CpG islands with the lowest “combined rank score” are presented in Table S1 with the associated gene names.
Figure 3.
Comparing the density distributions of methylation levels (β) in (A) W and NS and in (B) the CpG content. In (B), it can be seen that the island relation has more β value density than other CpG content.
Figure 4.
Scatterplot (A) and volcano plot (B) analysis for the top 1000 most differentially methylated CpG islands. In (A), the mean of mean methylation levels (beta value) for normal skin across all sites in a region (mean.mean.beta.NS) is on the x axis, and the mean of mean methylation levels (beta value) for warts across all sites in a region (mean.mean.beta.W) is on the y axis. Methylation beta values ranged from 0 (unmethylated) to 1 (fully methylated). In (B), the figure illustrates the overall extent of hypermethylation (>0) and hypomethylation (<0) of the top 1000 most differentially methylated CpG islands. Differential methylation was quantified by log2 of the mean quotient in means across all sites in a region (mean.mean.quot.log2) and the mean difference in means across all sites in a region (mean.mean.diff) between W and NS.
2.3. Hypermethylated and Hypomethylated CpG Islands
LOLA enrichment analysis of the top 1000 hypermethylated and top 1000 hypomethylated CpG islands are shown in Figures S1 and S2 and Figures S3 and S4, respectively.
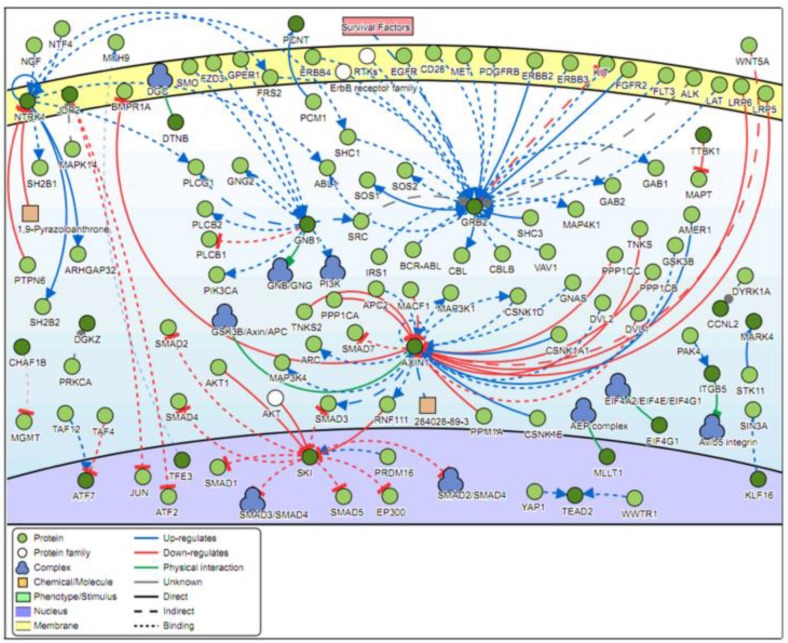
2.4. Signaling Networks
Analysis of the genes located in the top 100 DM CpG islands showed that five genes were found to be common regulators with a minimum of 12 connectivities. These genes are GRB2, GNB1, NTRK1, AXIN1, and SKI (Figure 5).
Figure 5.
Pathway signaling network generated from the genes located within the top 100 most differentially methylated CpG islands. Five genes (GRB2, GNB1, NTRK1, AXIN1, and SKI) have a minimum of 12 connectivities.
2.5. Validation of the Top Five Genes Associated with Differentially Methylated CpG Islands
Differentially methylated CpG islands were ranked using the “combined ranking score” (Table S1). Genes of interest included the five top-ranked genes (ITGB5, DTNB, RBFOX3, SLC6A9 and C2orf27A), which were selected for preliminary validation. The expression and methylation levels of these genes in warts compared to normal skin has been measured and can be seen in Table 1. The ITGB5 and DTNB genes have been found to be significantly differentially methylated in warts. Moreover, ITGB5 is up-regulated in warts compared to normal skin.
Table 1.
Methylation and expression levels of the genes associated with the five top-ranked CpG islands in warts (W) compared to normal skin (NS).
| Methylation Levels | Expression Levels | |||||
|---|---|---|---|---|---|---|
| Gene | Mean.mean β value (NS) |
Mean.mean β value (W) |
Mean.mean β value (W-NS) |
p-value | logFC | p-value |
| ITGB5 | 0.386 | 0.428 | −0.042 | 0.0002 | 0.418 | 0.0060 |
| DTNB | 0.608 | 0.604 | 0.004 | 0.0138 | −0.029 | 0.8569 |
| RBFOX3 | 0.493 | 0.473 | 0.021 | 0.0543 | n/a | n/a |
| SLC6A9 | 0.497 | 0.499 | −0.002 | 0.0602 | 0.212 | 0.3504 |
| C2orf27A | 0.600 | 0.598 | 0.002 | 0.2827 | n/a | n/a |
Mean.mean β value = mean of mean methylation levels across all sites in a region; logFC = log fold change.
3. Discussion
Since CpG islands are mostly found within promoter regions, their methylation statuses often determine whether a particular gene is transcribed or silenced [15]. Promoter-associated CpG islands are almost always unmethylated except during periods of cell development and differentiation [26]. In HPV-infected keratinocytes, apoptosis is inhibited and cell division is stimulated, leading to a number of transient cellular changes that culminates in the formation of a wart [27]. The impermanence of warts points towards the HPV-induced modulation of methylation patterns in warts compared to normal skin [3]. The present study provided a genome-wide characterization of the CpG island methylation profiles of 24 paired wart and normal skin samples from 12 Jordanian-Arab males.
The top-ranking CpG islands in cutaneous warts were found within the integrin subunit beta 5 (ITGB5), dystrobrevin beta (DTNB), RNA binding protein, fox-1 homolog 3 (RBFOX3), solute carrier family 6 member 9 (SLC6A9), and uncharacterized protein C2orf27 (C2orf27A) genes. These genes exhibited different methylation and expression patterns in warts compared to normal skin (Table 1). In a porcine model, the ITGB5 gene was reported to be a significant adhesion molecule of mucosal epithelial signaling in the response to Escherichia coli, while, in humans, ITGB5 variants were associated with airway hyperresponsiveness [28,29]. The ITGB5 gene was also found to be a key gene of the most highly enriched pathways in Het-1A cells expressing L2, the minor capsid protein of HPV [30]. Although the exact function of the DTNB gene is still unclear, its involvement in neural differentiation processes has been suggested [31]. Similarly, the RBFOX3 gene has been associated with neuronal differentiation as well as neurological disorders like Rolandic epilepsy and sleep latency [32,33]. In contrast, the SLC6A9 gene was found to be upregulated in normal human keratinocytes treated with epidermal growth factor receptor (EGFR) inhibitors [34]. Little is known about the C2orf27A gene in terms of its function, but it has been previously reported to be associated with the Ebola virus disease [35].
Among the top 1000 hypermethylated CpG islands in cutaneous warts, the most enriched genomic region set comprised the tissue-clustered DNase hypersensitive sites from Sheffield, namely primitive epithelial, skin, epithelial, and normal human epidermal keratinocyte (NHEK) sites. Similarly, the most enriched genomic region sets among the top 1000 hypomethylated CpG islands were the tissue-clustered DNase hypersensitive sites from Sheffield (normal human dermal fibroblast (NHDF), hematopoietic, and fibroblast epithelial sites), the ENCODE segmentation sites, the ENCODE transcription factor binding sites, the codex sites, and the epigenome sites from cistrome. In untransformed human fibroblasts, DNase hypersensitive regions were found to be associated with CpG sites in which methylation negatively corresponds with gene expression [36].
Signaling pathway analysis of the top 100 DM CpG islands revealed that the most common regulators were the growth factor receptor-bound protein 2 (GRB2), guanine nucleotide-binding protein G(I)/G(S)/G(T) subunit beta-1 (GNB1), neurotrophic tyrosine kinase receptor type 1(NTRK1), axin 1 (AXIN1), and ski proto-oncogene (SKI) genes. The GRB2 gene is critical in the downstream transduction of EGFR, and the aberrant expression of the latter has been implicated in several inflammatory skin diseases [37,38]. GRB2 was also found to play a major role in the life cycle of high-risk HPV types as well as associated carcinogenesis [39,40]. De novo mutations in the GNB1 gene have been associated with cutaneous mastocytosis and neurodevelopmental delays, while mutations in the NTRK1 gene were found to cause anhidrosis and palmar hyperkeratosis [41,42]. In contrast, AXIN1 expression is often dysregulated in various types of cancer cells [43,44,45,46,47]. On a similar note, the SKI oncogene has been linked to several HPV-associated cancers such as esophageal squamous cell carcinoma and cervical cancer [48,49,50].
4. Methods
4.1. Subjects
Ethical approval to conduct the present study was given by the Institutional Review Board (IRB) at Jordan University of Science and Technology (JUST), with the ethical approval number of 2/105/2017. After obtaining written informed consent, twelve Arab males with common warts were recruited from the general population. All of the warts investigated in the current study were clinically identified as Verruca vulgaris, the latter of which is associated with HPV types 1, 2, 3, 4, 5, 7, 27, 29, and 57 [51,52]. Paired tissue samples of warts and adjacent normal skin were obtained from each participant via shave biopsy, a procedure which excises only the epidermal layer of the skin. In terms of anatomical localization, 20 samples were obtained from the hands, 2 from the feet, and 2 from the forehead. The 24 samples were then stored at −20 °C until further processing.
4.2. DNA Extraction and the Infinium MethylationEPIC BeadChip
Genomic DNA was extracted by means of a QIAamp DNA Mini Kit (Qiagen, Hilden, Germany), and optional RNase A digestion was performed. The BioTek PowerWave XS2 Spectrophotometer (BioTek Instruments, Inc., Winuski, VT, USA) was employed in order to determine DNA purity, while agarose gel electrophoresis was carried out in order to examine DNA integrity. For the wart samples only, a second and heavier band was exhibited, pointing towards the presence of the circular dsDNA of HPV. Samples that met the standards for purity and integrity were then shipped on dry ice to the Melbourne node of the Australian Genome Research Facility (AGRF). At the AGRF, the quality of the samples was assessed by the QuantiFluor® dsDNA System (Promega, Madison, WI, USA) and resolution was evaluated via 0.8% agarose gel electrophoresis. The 24 samples were then normalized to approximately 500 ng of DNA in 45 μL and bisulfite converted with Zymo EZ DNA Methylation kit (Zymo Research, Owen, CA, USA). Afterwards, the Infinium MethylationEPIC BeadChip microarray (Illumina, San Diego, CA, USA) was used to carry out a genome-wide analysis of the methylation patterns of over 850,000 CpG sites.
4.3. Data Analysis and Processing
Data analysis was carried out on Illumina’s GenomeStudio v2011.1 with Methylation module 1.9.0 software, using the default Illumina settings and MethylationEPIC_v-1-0_B3 manifest file. All samples were above 850,000 detected CpG (p-value = 0.01). A computational R package (RnBeads) was adapted to process and analyze the raw intensity data from the methylation chip (IDAT files) [53]. Quality control, preprocessing, batch effects adjustment, and normalization were carried out on all probes and samples according to the RnBeads package pipeline.
4.4. Differential Methylation Analysis
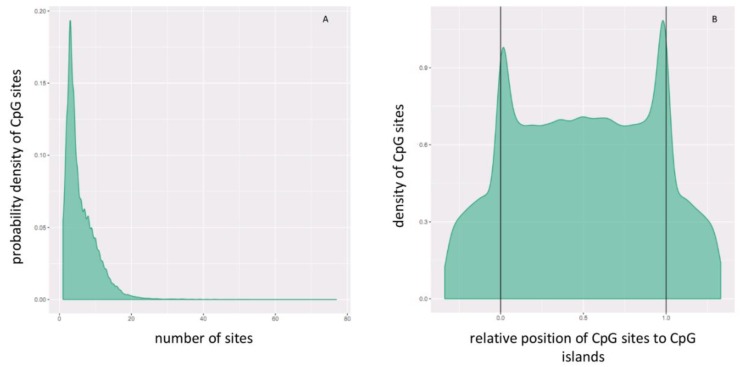
Differential methylation analysis was performed on CpG islands, at which the mean of the mean β (mean.mean β) values of all the tested CpG sites were computed. The distribution of the CpG sites per and across CpG islands can be seen in Figure 6A,B, respectively. Differential methylation (DM) for each CpG island was calculated using three measures: the mean.mean β difference between W and NS, the log2 of the mean quotient in β means across all CpG sites in a CpG island, and the adjusted combined p-value of all CpG sites in the CpG islands using a limma statistical test [54]. The Benjamini-Hochberg (B-H) procedure was used to correct for multiple testing. Moreover, these three measures were used to give each CpG island a rank, and the combined rank was computed as the maximum (=worst) rank among the three ranks. CpG islands which exhibit more DM will have a smaller combined rank [53]. CpG islands were sorted from smallest to largest using the “combined ranking score”, and the top-ranking 1000 CpG islands were selected for further analysis.
Figure 6.
CgG site distribution (A) per and (B) across CpG islands. In panel B, the relative coordinates of 0 and 1 correspond to the start and end coordinates of each CpG island. Coordinates smaller than 0 and greater than 1 denote flanking regions normalized by region length. CpG sites are more dense at the start and end of CpG islands.
4.5. Locus Overlap Analysis
Locus Overlap Analysis (LOLA) for enrichment of genomic ranges was conducted for the best 1000 CpG islands [55]. The following LOLA reference databases collections were used in the analysis: the Cistrome database from Cistrome (cistrome_cistrome), the Epigenome databases from Cistrome (cistrome_epigenome), the Codex database (CODEX), chromatin segmentation states from ENCODE (encode_segmentation), transcription factor binding sites from ENCODE (ENCODE_TFBS), tissue-clustered DNase hypersensitive sites from Sheffield et al. (2013) (Sheffield_dnase), and a collection of UCSC feature tables (UCSC_features). The LOLA tool uses Fischer’s exact test and produces a ranked list of significantly enriched region sets.
4.6. Signaling Pathway Analysis
Signaling Network Open Resource (SIGNOR) 2.0 investigates the causal relationships between biological entities, and it was used to explore the signaling network of the genes associated with the top 100 most DM CpG islands [56]. The type of relation was selected to include “all” interactions with a relaxed layout and score of “0.0”.
4.7. Validation of the Genes Associated with DM CpG Islands
Five genes which have been identified to be associated with the top-ranked DM CpG islands were subjected to further validation by examining their expression and methylation levels. These genes were validated by reviewing the results of two studies previously carried out in our lab. Using the same samples involved in the present study, one study investigated DNA methylation levels while the other measured expression levels in warts compared to normal skin [57].
5. Conclusions
In the present study, genomic DNA was extracted from paired wart and normal skin tissue samples and subjected to methylation sequencing. Differential methylation analysis revealed certain genes to be significantly hyper- and hypomethylated in warts compared to normal skin. Our findings indicate that host CpG island methylation is an integral part of the HPV infection and wart formation processes. The reversibility of DNA-m could potentially explain wart remission and clearance. To the best of the authors’ knowledge, this is the first study to compare and contrast the CpG methylation status between HPV-induced warts and adjacent normal skin. Future research is necessary to identify the functional and clinical relevance of the significantly associated CpG sites.
Acknowledgments
The authors would like to express their gratitude to King Khalid University, Saudi Arabia for providing administrative and technical support.
Abbreviations
| CpG | 5′-C-phosphate-G-3′ |
| DM | Differentially methylated |
| NS | Normal skin |
| W | Wart |
Supplementary Materials
Supplementary materials can be found at https://www.mdpi.com/1422-0067/20/19/4822/s1.
Author Contributions
L.N.A.-E. designed the method study and supervised the study. L.N.A.-E., M.A.A. and A.H.T. lead the implementation of the method, performed the data analysis and drafted the manuscript. L.N.A.-E., M.A.A., A.H.T. and F.A.A.-Q. helped with the interpretation, and description of the results. All authors read and approved the final manuscript.
Funding
This work was supported by the Deanship of Research at Jordan University of Science and Technology under grant number (Ref # 184/2017).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Van Doorslaer K. Evolution of the Papillomaviridae. Virology. 2013;445:11–20. doi: 10.1016/j.virol.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Bzhalava D., Guan P., Franceschi S., Dillner J., Clifford G. A systematic review of the prevalence of mucosal and cutaneous human papillomavirus types. Virology. 2013;445:224–231. doi: 10.1016/j.virol.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 3.Durzynska J., Lesniewicz K., Poreba E. Human papillomaviruses in epigenetic regulations. Mutat. Res. Mutat. Res. 2017;772:36–50. doi: 10.1016/j.mrrev.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Sterling J.C., Gibbs S., Haque Hussain S.S., Mohd Mustapa M.F., Handfield-Jones S.E. British Association of Dermatologists’ guidelines for the management of cutaneous warts 2014. Br. J. Dermatol. 2014;171:696–712. doi: 10.1111/bjd.13310. [DOI] [PubMed] [Google Scholar]
- 5.Accardi R., Gheit T. Cutaneous HPV and skin cancer. Presse Med. 2014;43:e435–e443. doi: 10.1016/j.lpm.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 6.De Abreu P.M., Có A.C.G., Azevedo P.L., do Valle I.B., de Oliveira K.G., Gouvea S.A., Cordeiro-Silva M.F., Louro I.D., de Podestá J.R.V., Lenzi J., et al. Frequency of HPV in oral cavity squamous cell carcinoma. BMC Cancer. 2018;18:324. doi: 10.1186/s12885-018-4247-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ducatman B.S. The Role of Human Papillomavirus in Oropharyngeal Squamous Cell Carcinoma. Arch. Pathol. Lab. Med. 2018;142:715–718. doi: 10.5858/arpa.2018-0083-RA. [DOI] [PubMed] [Google Scholar]
- 8.Smith T.J., Mendez A., Donald C., Nagel T.H. HPV-associated oropharyngeal squamous cell carcinoma. J. Am. Acad. Physician Assist. 2017;30:14–19. doi: 10.1097/01.JAA.0000510985.76167.ed. [DOI] [PubMed] [Google Scholar]
- 9.Villagómez-Ortíz V.J., Paz-Delgadillo D.E., Marino-Martínez I., Ceseñas-Falcón L.Á., Sandoval-de la Fuente A., Reyes-Escobedo A. Prevalence of human papillomavirus infection in squamous cell carcinoma of the oral cavity, oropharynx and larynx. Cirugía y Cirujanos. 2016;84:363–368. doi: 10.1016/j.circen.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Plesa A., Iancu I.V., Botezatu A., Huica I., Stoian M., Anton G. Human Papillomavirus—Research in a Global Perspective. InTech; London, UK: 2016. The Involvement of Epigenetic Mechanisms in HPV-Induced Cervical Cancer. [Google Scholar]
- 11.Di Domenico M., Giovane G., Kouidhi S., Iorio R., Romano M., De Francesco F., Feola A., Siciliano C., Califano L., Giordano A. HPV epigenetic mechanisms related to Oropharyngeal and Cervix cancers. Cancer Biol. Ther. 2018;19:850–857. doi: 10.1080/15384047.2017.1310349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jin Z., Liu Y. DNA methylation in human diseases. Genes Dis. 2018;5:1–8. doi: 10.1016/j.gendis.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heyn H., Moran S., Hernando-Herraez I., Sayols S., Gomez A., Sandoval J., Monk D., Hata K., Marques-Bonet T., Wang L., et al. DNA methylation contributes to natural human variation. Genome Res. 2013;23:1363–1372. doi: 10.1101/gr.154187.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jang H.S., Shin W.J., Lee J.E., Do J.T. CpG and Non-CpG Methylation in Epigenetic Gene Regulation and Brain Function. Genes. 2017;8:148. doi: 10.3390/genes8060148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deaton A.M., Bird A. CpG islands and the regulation of transcription. Genes Dev. 2011;25:1010–1022. doi: 10.1101/gad.2037511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paska A.V., Hudler P. Aberrant methylation patterns in cancer: A clinical view. Biochem. Medica. 2015;25:161–176. doi: 10.11613/BM.2015.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang H.-J. Aberrant DNA methylation in cervical carcinogenesis. Chin. J. Cancer. 2013;32:42–48. doi: 10.5732/cjc.012.10033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Verlaat W., Van Leeuwen R.W., Novianti P.W., Schuuring E., Meijer C.J.L.M., Van Der Zee A.G.J., Snijders P.J.F., Heideman D.A.M., Steenbergen R.D.M., Wisman G.B.A. Host-cell DNA methylation patterns during high-risk HPV-induced carcinogenesis reveal a heterogeneous nature of cervical pre-cancer. Epigenetics. 2018;13:769–778. doi: 10.1080/15592294.2018.1507197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Small W., Bacon M.A., Bajaj A., Chuang L.T., Fisher B.J., Harkenrider M.M., Jhingran A., Kitchener H.C., Mileshkin L.R., Viswanathan A.N., et al. Cervical cancer: A global health crisis. Cancer. 2017;123:2404–2412. doi: 10.1002/cncr.30667. [DOI] [PubMed] [Google Scholar]
- 20.Sen P., Ganguly P., Ganguly N. Modulation of DNA methylation by human papillomavirus E6 and E7 oncoproteins in cervical cancer (Review) Oncol. Lett. 2017;15:11–22. doi: 10.3892/ol.2017.7292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Degli Esposti D., Sklias A., Lima S.C., Beghelli-de la Forest Divonne S., Cahais V., Fernandez-Jimenez N., Cros M.-P., Ecsedi S., Cuenin C., Bouaoun L., et al. Unique DNA methylation signature in HPV-positive head and neck squamous cell carcinomas. Genome Med. 2017;9:33. doi: 10.1186/s13073-017-0419-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dankai W., Khunamornpong S., Siriaunkgul S., Soongkhaw A., Janpanao A., Utaipat U., Kitkumthorn N., Mutirangura A., Srisomboon J., Lekawanvijit S. Role of genomic DNA methylation in detection of cytologic and histologic abnormalities in high risk HPV-infected women. PLoS ONE. 2019;14:e0210289. doi: 10.1371/journal.pone.0210289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clarke M.A., Gradissimo A., Schiffman M., Lam J., Sollecito C.C., Fetterman B., Lorey T., Poitras N., Raine-Bennett T.R., Castle P.E., et al. Human Papillomavirus DNA Methylation as a Biomarker for Cervical Precancer: Consistency across 12 Genotypes and Potential Impact on Management of HPV-Positive Women. Clin. Cancer Res. 2018;24:2194–2202. doi: 10.1158/1078-0432.CCR-17-3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amaro-Filho S.M., Pereira Chaves C.B., Felix S.P., Basto D.L., de Almeida L.M., Moreira M.A.M. HPV DNA methylation at the early promoter and E1/E2 integrity: A comparison between HPV16, HPV18 and HPV45 in cervical cancer. Papillomavirus Res. 2018;5:172–179. doi: 10.1016/j.pvr.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johannsen E., Lambert P.F. Epigenetics of human papillomaviruses. Virology. 2013;445:205–212. doi: 10.1016/j.virol.2013.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jeziorska D.M., Murray R.J.S., De Gobbi M., Gaentzsch R., Garrick D., Ayyub H., Chen T., Li E., Telenius J., Lynch M., et al. DNA methylation of intragenic CpG islands depends on their transcriptional activity during differentiation and disease. Proc. Natl. Acad. Sci. USA. 2017;114:E7526–E7535. doi: 10.1073/pnas.1703087114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham S.V. Keratinocyte Differentiation-Dependent Human Papillomavirus Gene Regulation. Viruses. 2017;9:245. doi: 10.3390/v9090245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou C., Liu Z., Liu Y., Fu W., Ding X., Liu J., Yu Y., Zhang Q. Gene Silencing of Porcine MUC13 and ITGB5: Candidate Genes towards Escherichia coli F4ac Adhesion. PLoS ONE. 2013;8:e70303. doi: 10.1371/journal.pone.0070303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Himes B.E., Qiu W., Klanderman B., Ziniti J., Senter-Sylvia J., Szefler S.J., Lemanske R.F., Jr., Zeiger R.S., Strunk R.C., Martinez F.D., et al. ITGB5 and AGFG1 variants are associated with severity of airway responsiveness. BMC Med. Genet. 2013;14:86. doi: 10.1186/1471-2350-14-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eckhardt M., Zhang W., Gross A.M., Von Dollen J., Johnson J.R., Franks-Skiba K.E., Swaney D.L., Johnson T.L., Jang G.M., Shah P.S., et al. Multiple Routes to Oncogenesis Are Promoted by the Human Papillomavirus-Host Protein Network. Cancer Discov. 2018;8:1474–1489. doi: 10.1158/2159-8290.CD-17-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quaranta M.T., Spinello I., Paolillo R., Macchia G., Boe A., Ceccarini M., Labbaye C., Macioce P. Identification of β-Dystrobrevin as a Direct Target of miR-143: Involvement in Early Stages of Neural Differentiation. PLoS ONE. 2016;11:e0156325. doi: 10.1371/journal.pone.0156325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amin N., Allebrandt K. V., van der Spek A., Müller-Myhsok B., Hek K., Teder-Laving M., Hayward C., Esko T., van Mill J.G., Mbarek H., et al. Genetic variants in RBFOX3 are associated with sleep latency. Eur. J. Hum. Genet. 2016;24:1488–1495. doi: 10.1038/ejhg.2016.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lal D., Reinthaler E.M., Altmüller J., Toliat M.R., Thiele H., Nürnberg P., Lerche H., Hahn A., Møller R.S., Muhle H., et al. RBFOX1 and RBFOX3 Mutations in Rolandic Epilepsy. PLoS ONE. 2013;8:e73323. doi: 10.1371/annotation/f6aed47b-9135-45f5-bfdd-f4ceb33c8561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lulli D., Carbone M.L., Pastore S. Epidermal growth factor receptor inhibitors trigger a type I interferon response in human skin. Oncotarget. 2016;7:47777–47793. doi: 10.18632/oncotarget.10013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teng Y., Wang Y., Zhang X., Liu W., Fan H., Yao H., Lin B., Zhu P., Yuan W., Tong Y., et al. Systematic Genome-wide Screening and Prediction of microRNAs in EBOV During the 2014 Ebolavirus Outbreak. Sci. Rep. 2015;5:9912. doi: 10.1038/srep09912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wagner J.R., Busche S., Ge B., Kwan T., Pastinen T., Blanchette M. The relationship between DNA methylation, genetic and expression inter-individual variation in untransformed human fibroblasts. Genome Biol. 2014;15:R37. doi: 10.1186/gb-2014-15-2-r37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lichtenberger B.M., Gerber P.A., Holcmann M., Buhren B.A., Amberg N., Smolle V., Schrumpf H., Boelke E., Ansari P., Mackenzie C., et al. Epidermal EGFR Controls Cutaneous Host Defense and Prevents Inflammation. Sci. Transl. Med. 2013;5:199ra111. doi: 10.1126/scitranslmed.3005886. [DOI] [PubMed] [Google Scholar]
- 38.Wang H., Li S., Li H., Wang P., Huang F., Zhao Y., Yu L., Luo G., Zhang X., Wang J., et al. Grb2 interacts with SGEF and antagonizes the ability of SGEF to enhance EGF-induced ERK1/2 activation. Mol. Cell. Biochem. 2014;389:239–247. doi: 10.1007/s11010-013-1945-7. [DOI] [PubMed] [Google Scholar]
- 39.Spangle J.M., Munger K. The HPV16 E6 Oncoprotein Causes Prolonged Receptor Protein Tyrosine Kinase Signaling and Enhances Internalization of Phosphorylated Receptor Species. PLoS Pathog. 2013;9:e1003237. doi: 10.1371/journal.ppat.1003237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Santos J., Peixoto da Silva S., Costa N., Gil da Costa R., Medeiros R. The Role of MicroRNAs in the Metastatic Process of High-Risk HPV-Induced Cancers. Cancers (Basel) 2018;10:493. doi: 10.3390/cancers10120493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Szczałuba K., Biernacka A., Szymańska K., Gasperowicz P., Kosińska J., Rydzanicz M., Płoski R. Novel GNB1 de novo mutation in a patient with neurodevelopmental disorder and cutaneous mastocytosis: Clinical report and literature review. Eur. J. Med. Genet. 2018;61:157–160. doi: 10.1016/j.ejmg.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 42.Bonkowsky J.L., Johnson J., Carey J.C., Smith A.G., Swoboda K.J. An infant with primary tooth loss and palmar hyperkeratosis: A novel mutation in the NTRK1 gene causing congenital insensitivity to pain with anhidrosis. Pediatrics. 2003;112:e237–e241. doi: 10.1542/peds.112.3.e237. [DOI] [PubMed] [Google Scholar]
- 43.Salahshor S., Woodgett J.R. The links between axin and carcinogenesis. J. Clin. Pathol. 2005;58:225–236. doi: 10.1136/jcp.2003.009506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pećina-Slaus N., Martić T.N., Kokotović T., Kusec V., Tomas D., Hrasćan R. AXIN-1 protein expression and localization in glioblastoma. Coll. Antropol. 2011;35(Suppl. 1):101–106. [PubMed] [Google Scholar]
- 45.Ishiguro H., Tsunoda T., Tanaka T., Fujii Y., Nakamura Y., Furukawa Y. Identification of AXUD1, a novel human gene induced by AXIN1 and its reduced expression in human carcinomas of the lung, liver, colon and kidney. Oncogene. 2001;20:5062–5066. doi: 10.1038/sj.onc.1204603. [DOI] [PubMed] [Google Scholar]
- 46.Picco G., Petti C., Centonze A., Torchiaro E., Crisafulli G., Novara L., Acquaviva A., Bardelli A., Medico E. Loss of AXIN1 drives acquired resistance to WNT pathway blockade in colorectal cancer cells carrying RSPO3 fusions. EMBO Mol. Med. 2017;9:293–303. doi: 10.15252/emmm.201606773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koppert L.B., van der Velden A.W., van de Wetering M., Abbou M., van den Ouweland A.M.W., Tilanus H.W., Wijnhoven B.P.L., Dinjens W.N.M. Frequent loss of the AXIN1 locus but absence of AXIN1 gene mutations in adenocarcinomas of the gastro-oesophageal junction with nuclear β-catenin expression. Br. J. Cancer. 2004;90:892–899. doi: 10.1038/sj.bjc.6601589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tecalco-Cruz A.C., Ríos-López D.G., Vázquez-Victorio G., Rosales-Alvarez R.E., Macías-Silva M. Transcriptional cofactors Ski and SnoN are major regulators of the TGF-β/Smad signaling pathway in health and disease. Signal Transduct. Target. Ther. 2018;3:15. doi: 10.1038/s41392-018-0015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baldwin A., Pirisi L., Creek K.E. NFI-Ski Interactions Mediate Transforming Growth Factor β Modulation of Human Papillomavirus Type 16 Early Gene Expression. J. Virol. 2004;78:3953–3964. doi: 10.1128/JVI.78.8.3953-3964.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deheuninck J., Luo K. Ski and SnoN, potent negative regulators of TGF-beta signaling. Cell Res. 2009;19:47–57. doi: 10.1038/cr.2008.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bruggink S.C., de Koning M.N.C., Gussekloo J., Egberts P.F., ter Schegget J., Feltkamp M.C.W., Bavinck J.N.B., Quint W.G.V., Assendelft W.J.J., Eekhof J.A.H. Cutaneous wart-associated HPV types: Prevalence and relation with patient characteristics. J. Clin. Virol. 2012;55:250–255. doi: 10.1016/j.jcv.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 52.Mulhem E., Pinelis S. Treatment of nongenital cutaneous warts. Am. Fam. Physician. 2011;84:288–293. [PubMed] [Google Scholar]
- 53.Assenov Y., Müller F., Lutsik P., Walter J., Lengauer T., Bock C. Comprehensive analysis of DNA methylation data with RnBeads. Nat. Methods. 2014;11:1138–1140. doi: 10.1038/nmeth.3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ritchie M.E., Phipson B., Wu D., Hu Y., Law C.W., Shi W., Smyth G.K. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sheffield N.C., Bock C. LOLA: Enrichment analysis for genomic region sets and regulatory elements in R and Bioconductor. Bioinformatics. 2016;32:587–589. doi: 10.1093/bioinformatics/btv612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Perfetto L., Briganti L., Calderone A., Cerquone Perpetuini A., Iannuccelli M., Langone F., Licata L., Marinkovic M., Mattioni A., Pavlidou T., et al. SIGNOR: A database of causal relationships between biological entities. Nucleic Acids Res. 2016;44:D548–D554. doi: 10.1093/nar/gkv1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Al-Eitan L., Tarkhan A.H., Alghamdi M.A., Al-Qarqaz F.A., Al-Kofahi H.S. Transcriptome analysis of HPV-induced warts and healthy skin in humans. BMC Med. Genom. 2019 doi: 10.1186/s12920-020-0700-7. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.