Abstract
Background
In Norway, as in other European countries, the ageing population is increasing rapidly. Governments seek to enable older people stay in their homes for as long as possible, and welfare technology (WT) has been proposed as a possible solution. Human behaviour modelling (HBM) is a welfare technology that identifies an individual’s behaviour patterns and detects abnormal behaviours, including falls and early signs of dementia. However, the successful development of HBM WT requires the consideration of the older people’s attitudes on this.
Aim
The present study sought to explore attitudes and perspectives about welfare technology among older people living alone in Norway.
Methods
We used an exploratory, qualitative approach in which semi-structured, in-depth interviews were conducted with five women and four men between the ages of 79 and 91. The interviews were analysed using qualitative content analysis.
Results
Two categories and four subcategories were identified: 1) preferences and concerns of welfare technology (i) feeling confident-proactive approach of future technology, (ii) concerns and dilemmas, and 2) reflections of today and tomorrow- awareness of own health (i) feeling healthy, independent, self-sufficient and safe, (ii) facing own ageing- preparedness on unpredictable scenarios. The main theme, welfare technology - a valuable addition to tomorrow’s homes, represents how the participants held positive and proactive attitudes towards the use of WT in their homes.
Conclusion
Participants trusted the Norwegian healthcare system and did not rely on their families for care. Independence, autonomy, and feeling safe were essential for all participants, and most participants regarded welfare technology as empowering them to remain in their homes for as long as possible. Participants already confidently used various technologies in their daily lives. Surprisingly, they expressed no concerns about privacy, but some mention concerns about loss of autonomy and dignity. We conclude that a person-centred approach to integrating new WT is necessary.
Keywords: assistive technology, ambient assistive living, ethical challenges, healthcare, ageing in place, human behaviour
Introduction
In Norway, as in other European countries, the proportion of older people in the population is increasing rapidly. In the European Union, 12.7% of the population will be 80 or older by 2080, compared to just 5.5% in 2017.1 Furthermore, in Norway, 38.5% of people aged 65 and over live alone.2
Norwegian municipalities are obligated to provide healthcare services for older people, including home healthcare, practical assistance with daily tasks, and, if needed, nursing homes.3,4 Healthcare services are regulated by the Norwegian Municipal Health and Care Service Act of 2011, and anyone living in Norway has the legal right to access necessary healthcare services.5
The need for nursing and healthcare services in Norway increased by 18% from 2007 to 2017.6 The Norwegian nursing association has reported that there is a shortage of 6,000 nurses at present projected to increase to 30,000 in 20 years.7 People living in large cities often have to wait longer to receive care services than people in less populated areas.4 Given this increasing shortage and the fact that people are living longer, several studies have concluded that the Norwegian state will not be able to cope with rising demand for eldercare services, creating a need for more nursing homes.3,8–10 However, nursing home availability in Norway also decreased by 2% from 2015 to 2018.11
Furthermore, the ability for older people to stay in their own homes, also known as ageing in place, presents many advantages compared to moving to residential care facilities. Studies in Europe and New Zeland12–14 have shown that remaining in a familiar environment increases independence, is cost-effective, decreases the risk of contracting infectious disease, and helps individuals cope with the shortage of healthcare. Enabling older people to remain in their homes for as long as they are in good health and can take care of themselves has therefore been a stated goal of the Norwegian state for the last 70 years.15,16
New solutions are therefore needed that allow older people to remain at home. In addition, as life expectancy increases, so does the need for staying healthy while ageing.17 Welfare technology, defined as ‘technology used for environmental control, safety and wellbeing, in particular for elderly and disabled people’10 (and more often referred to as 'ambient assisted living' outside of Scandinavia), can contribute to facilitating sustainable healthcare for older people.18,19 Its general goal is to construct technological solutions that enable a better and safer environment for older people and people with disabilities. Moreover, previous studies have shown that welfare technology increases older people’s abilities to age in place and is regarded as good care that meets older people’s needs and is easy to use.20 Welfare technology can also help enable older people to remain healthier while ageing in place.21 It is thus consistent with the goals of health promotion, which is defined as 'the process of enabling people to increase control over and to improve their health'.22 The Norwegian government has therefore invested in welfare technology, including digital safety alarms, electronic door locking, digital supervision, nurse call systems, electronic pill dispensers, and ‘smart houses’6,23,24—that is, living environments that have been designed to assist residents with their daily activities and to promote independent lifestyles.8,25
Nevertheless, ageing in place also carries risks, including health deterioration and safety issues like falls and dizziness.13 Human behaviour modelling (HBM) is a type of welfare technology that can recognise an individual’s behaviour patterns in a smart house, thereby helping to construct a safe environment. HBM aims to detect abnormal behaviours, such as falls and early signs of dementia, in order to alert family members or a caretaker if assistance is needed. The concept is based on an assumption that individuals tend to follow recognisable patterns in their daily lives,26,27 thereby making it possible to predict their future behaviours and actions. However, welfare technology that can detect human behaviour in this manner is relatively new, and research is still sparse.28–32
Studies have shown that it is important to consider end-users’ feedback from the beginning of the research and development stage, in order to avoid their later rejection of the developed technology.8,33 This is also consistent with the person-centred research principle of keeping individuals’ values central to decision-making.34 Technology contributes to changes in relationships; in the case of older people, in particular, this affects not only their social lives but also their healthcare practices, thereby introducing new risks and ethical questions.
The person‐centred research perspective emphasises the necessity of respecting the individual35 and seeks to study 'how technology influences relationships […] and how it contributes to humanistic values or diminishes them',19 with the ultimate goal of developing a final product that is genuinely useful to end-users—in this case, older people.17,36 Older people who live alone stand to benefit the most from welfare technology, including HBM, and in order to plan for and create a sustainable and targeted healthcare solution for them, it is important to understand their attitudes to welfare technology which is underpinned by person-centred principles.34 However, there has been limited attention to this topic.
Aim And Research Question
The aim of this study is to explore older people’s attitudes to welfare technology. The research question is as follows: What characterises the attitudes of and experiences with welfare technology among older people living alone in Norway?
Design And Methodology
This study used an explorative, qualitative design37 with semi-structured interviews that followed the principles stated by Kallio.38 The data were analysed using the content analysis method described by Graneheim and Lundman.39
Recruitment Procedure And Sample
Two strategies were used to recruit participants. A first recruitment was done through criterion sampling, which consists on selecting participants that meet predetermined inclusion criteria;40 living alone; being older than 75 years old; speaking Norwegian, English, or Spanish; and not receiving any kind of public healthcare services. E-mails and letters were sent to five different interest organizations of retired people, without having positive responses. One organization did not have time for distributing information, the other four organizations did not responded. Consequently, an informational poster describing the project and criteria was posted in a senior centre in southeast Norway. Two participants were recruited by this procedure.
Due to the lack of responses and the slow recruitment, snowball sampling was implemented as an additional recruitment procedure. This approach involves asking knowledgeable people about whom could participate. As described by Patton,40 ‘by asking a number of people who else to talk with, the snowball gets bigger and bigger as you accumulate new information-rich cases’. One of the researcher contacted the leader of an interest organisation of older persons, the knowledgeable person, to inform about the study. This organisation leader then informed a fellow member, who informed others, resulting in seven participants. Thus, the two recruitment procedures resulted in a total of nine participants.
The data were collected from May 2017 to January 2018, in the south-eastern region of Norway. The final sample comprised five women and four men between the ages of 75 and 91, where all of them were retired (Table 1). No more participants were recruited because we assessed the collected data to be rich enough41 to answer the research question. Marshall42 states that 'in practice, the number of required subjects usually becomes obvious as the study progresses, as new categories, themes or explanations stop emerging from the data (data saturation)'. Additionally, qualitative research sampling has no fixed minimum nor maximum number of participants and hence the sample may involve small numbers of participants and large amount of data collected. The most important is that 'sufficient depth of information is gathered to fully describe the phenomena being studied'.43
Table 1.
Demographic Characteristics
| Participant | Gender | Age | Civil status | Type Of House | Years Living Alone | Years In Current House |
|---|---|---|---|---|---|---|
| P1 | Female | 91 | Widow | Senior apartment | No data | 22 years |
| P2 | Male | 79 | Widow | Own house | 2 years | 49 years |
| P3 | Male | 80 | Widow | Senior apartment | 6 years | 2 years |
| P4 | Male | 79 | Widow | Own house | 14 years | 14 years |
| P5 | Male | 79 | Widow | Own house | 1.5 years | No data |
| P6 | Female | 83 | Divorced | Own house | 60 years | 13 years |
| P7 | Female | 84 | Widow | Apartment | 11 years | 20 years |
| P8 | Female | 84 | Widow | Own house | 10 years | 52 years |
| P9 | Female | 89 | Widow | Senior apartment | 16 years | 7 years |
Data Collection
Since welfare technology that can detect changes in the person’s behaviour, such as HMB, is still in the research stage, before each interview the researcher explained to the participant how such technology would work. Each interview then began by exploring the participant’s prior experiences with other welfare technological devices, and these responses formed the background for the present study.
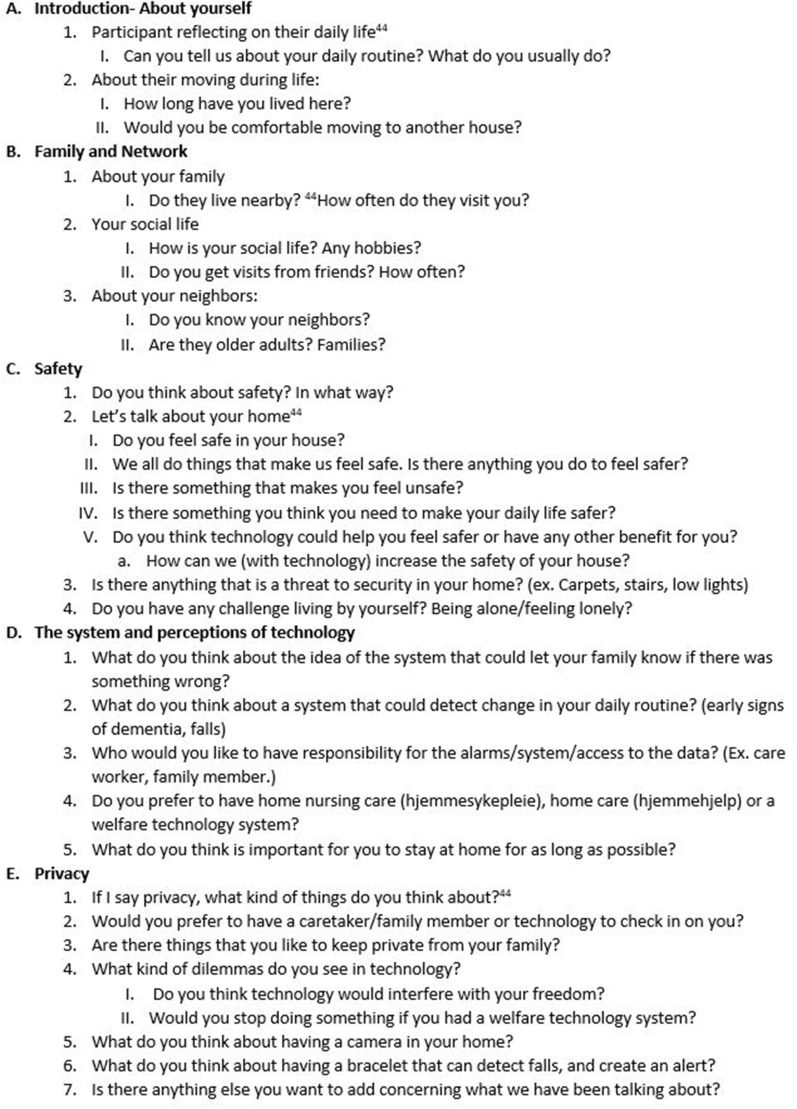
Based on a thorough examination of earlier studies44 and in line with the aim of this study, an interview guide was developed and pilot-tested with a volunteer. After the pilot test, some minor adjustments were made based on the volunteer’s responses. Figure 1 shows the semi-structured interviews guide. In addition to demographic data, including family and community information, three broad themes of inquiry were investigated: 1) reflections on safety issues, 2) experiences with and attitudes towards welfare technology, and 3) experiences with and attitudes towards privacy issues. The interview format sought to invite open dialogue and used open-ended questions, for example about participants’ prior experiences with technology and reflections on welfare technology. Questions such as 'Could you tell me about some experiences you have had with any technological devices?' and 'Could you describe [prior statement] even more thoroughly?' encouraged in-depth responses.
Figure 1.
Semi-structured interview questionnaire guide.
Interviews were conducted in each participant’s own home to help participants visualise their circumstances and reflect about the questions based on their current lived experiences at home, for example about whether their home had any stairs or carpets that could be tripping hazards. All but one of the interviews were digitally recorded and transcribed verbatim; due to one participant’s request, manual field notes were instead used to record one interview. The interviews ranged from 45–75 mins in length.
Data Analysis
One interview was randomly selected for initial analysis by all of the authors. Its content was analysed using the method described by Graneheim and Lundman39 who defined content analysis as an analysis of both the manifest content and of the interpretations of latent content. Manifest content is that which is written explicitly, while latent content refers to what the text implicitly addresses. The interpretation of latent content during analysis is thus a 'co-creation of the researchers and the text', and thus the 'data and interpretation are co-creations of the interviewee and the interviewer'.45,46
The analysis of the first interview started by every member of the research team individually identifying 'meaning units'—i.e., words, sentences, or paragraphs on the same topic. The meaning units were then condensed and codified, followed by preliminary suggestions of subcategories topic (Table 2). After all members of the research team had discussed and agreed on the preliminary analysis of the first transcript, the eight remaining interviews transcripts were analysed by VGS following the same procedure. All transcriptions were read several times by all members. A total of 52 codes were identified and thoroughly discussed by the research team. After unanimous consent, the codes were then grouped into subcategories of topics that shared similarities.47 This process continued until the final analysis could be summarised as a single theme, with two main categories reflecting the manifest content of the subcategories. Table 3 shows the four main analytical steps drawn during the data analysis with the corresponding number of meaning units, codes, sub-categories and categories for each step. Between analysis step 2 and 3, the total of 366 meaning units were reduced from the initial list. When the team worked through the list together, several of the meaning units were assessed to be either not relevant to the research questions or could be merged together. Examples of meaning units of no relevance could comprise information like 'I used to work a lot outside, like farming', 'I moved a lot before settling here'.
Table 2.
Example Of The Analysis Procedure From A Manifest To A Latent Level
| Manifest Level | Latent Level | |||
|---|---|---|---|---|
| Meaning Units | Condensed Meaning Unit | Code | Sub-Categories | Categories |
| There is a nurse that comes just to deliver pills to my neighbour four times a day, it is not nice, but it is worse to have a machine for that | Home care nurse delivering pills is better than technology | Technology care should not replace human care | Concerns and dilemmas | Preferences and concerns of welfare technology |
| I am very careful, I always have my mobile in my night table and with me, even when I go to the bathroom in the night just in case I could fall or anything happens | Carrying phone to be able to call in case of emergency or falling | Having an action plan in case of emergency | Facing own ageing- preparedness for unpredictable scenarios | Reflections of today and tomorrow- awareness of own health |
Table 3.
Number Of Meaning Units, Codes, Sub-Categories And Categories Throughout The Four Main Analysis Steps
| Meaning Units | Codes | Sub-Categories | Categories | |
|---|---|---|---|---|
| Analysis 1 | 981 | 85 | 19 | 4 |
| Analysis 2 | 981 | 76 | 13 | 4 |
| Analysis 3 | 615 | 52 | 7 | 3 |
| Analysis 4 (Final) | 615 | 52 | 4 | 2 |
The findings were thus discussed in depth by all members of the research team until consensus was achieved. Categories were then compared in reverse with the manifest text to verify their accuracy and trustworthiness, using the trustworthiness criteria established by Lincoln and Guba:48 credibility, transferability, dependability, and confirmability. In the present study, credibility was achieved through prolonged engagement and analyst triangulation; transferability was established by providing detailed descriptions that could be applied to other contexts; dependability was assessed using stepwise replication and a code-recode strategy to ensure that the findings were consistent and replicable; and confirmability was assessed using reflexivity throughout the analysis process and in consecutive discussions among the research team.
Ethical Considerations
All participants received verbal and written information from the interviewers about the project before proceeding to the interviews. Eight participants signed an informed consent form to participate in the study, while one participant gave oral informed consent. Confidentiality and anonymity were assured; no names were used in the transcriptions nor in the present study. Participation was voluntary and no economic compensation was given. The study was reported to the Norwegian Center for Research Data (NSD, project number 53841). NSD does not approves projects but they must be notified about the processing of personal data in the project, even if only anonymous data is published.49
Results
The analysis revealed a theme, two main categories and two sub-categories, presented in Table 4 below.
Table 4.
Subcategories, Categories, And Main Theme
| Sub-Categories Categories | Main Theme | |
|---|---|---|
| i. Feeling confident- proactive approach to future technology | I. Preferences and concerns of welfare technology | Welfare technology - a valuable addition to tomorrow’s homes |
| ii. Concerns and dilemmas | ||
| i. Feeling healthy, independent, self-sufficient and safe | II. Reflections of today and tomorrow- awareness of own health | |
| ii. Facing own ageing- preparedness for unpredictable scenarios | ||
Preferences And Concerns Of Welfare Technology
Feeling Confident - Proactive Approach To Future Technology
All but one of the participants expressed a positive response to the idea of HBM welfare technology that could detect changes in their behaviour, and they reported no objections to a welfare technology that could identify their daily routine. In general, the participants conveyed that if the welfare technology improved their safety, it was good for them. One participant stated:
When you feel that you have your five senses working, and you think that yes, I can live here for as long as I live, just knowing that I can live safe, be safe, knowing that I will be picked up if I fall, that is the most important. [P6]
The majority of the participants were familiar with other technologies and regularly used devices such as iPads, computers, e-mail, global positioning systems (GPS), smart watches, mobile telephones, Bluetooth, online bank transactions, and social media. Some participants also kept updated online medical journals that allowed healthcare personnel to review their medications and health concerns. One participant discussed welfare technology in the following terms:
Yes, I’m very interested in it [welfare technology] because I cannot think of moving out of my house … I also have thought about the possibility of installing electronics [devices in my house], just in case I fall, although I’m not that bad, I’m not there yet, but I can give my opinion [on welfare technology] anyways. [P5]
Most participants said that they had never fallen and that falling was not a concern for them; many said that they were not so old that falling would cause problems. For example, one woman stated:
I have strong arms, so I can easily lift myself up [from the bathtub] and get out of it [P8].
However, most participants also said that they had changed their habits or bought assistive devices when they felt it necessary for their safety. For example, a few participants were afraid of falling in the shower, and one participant had called the central aid station and asked for safety rails to be installed in her shower; another participant had a small chair in the shower; several participants had replaced their bathtubs with shower stalls to reduce the risk of falling; and several stated that they kept a hallway light on at night to help avoid falls. Several participants had also changed their furniture to avoid falling and had removed carpets after tripping on them. Other participants mentioned using poles, boots with grips, or track spikes to walk on slippery ground because they did not wish to fall and break an arm or leg. One participant even said that he would like an apartment entirely adapted to his needs:
I feel that, yes I have changed things, I have made it so it would be safer … [I would like] an apartment built so I can live there, with no door thresholds and an adapted bathroom, built so I can live there with a wheelchair or walker. [P4]
However, some participants noted that falling could happen to anybody, not only the older people, and that thus they did not worry about it much.
Regarding technological welfare adaptations, some participants had fall alarms and expressed that they had no need for additional welfare technology. However, others were glad to know about the existence of welfare technology that could assist them in the event of a fall. Furthermore, some participants were happy that welfare technology could provide peace of mind to their families and would avoid the need for their family to constantly check on them and worry if they failed to answer. For example, one woman mentioned that her relatives always feared the worst if she did not pick up the phone immediately when they called. Likewise, some participants wished for a waterproof fall alarm that could be used in the shower. Some participants were also open to the possibility of a wearable device, so long as it was small and comfortable, such as a watch or bracelet. Some participants also indicated a desire for an alarm with a GPS that could give an exact location to emergency services; most of the participants were more afraid of falling outside, for example while going for a walk, than of falling within their homes. One participant also expressed a desire for a GPS alarm in case they got lost:
GPS could be good to have in case I begin to get Alzheimer’s and I go for a walk and cannot find my way back, it [GPS] would be good. [P9]
Concerns And Dilemmas
Some participants also expressed concerns and dilemmas regarding the implementation of welfare technology. One participant also stated that she preferred to receive help from her family than from technology or healthcare workers. However, other concerns related to specific details about potential technologies.
One specific concern related to the costs of welfare technologies. All of the participants who owned fall alarms had purchased them with their own money, so that they would not feel like a burden on the municipality. Several said they would buy any device that could make their life easier and safer as long as they were affordable.
Participants also expressed concerns about a loss of autonomy and personal dignity from the use of welfare technology. They wondered who would control decisions about their technology use if they become weaker or developed a cognitive impairment, and they were concerned whether they would be forced to have a smart house; one man stated that
I say that I do not want it [welfare technology] now, but at some point there will be someone who will say that I should have it without me even having a say on it. [P2]
However, he also reflected, with resignation, that if he developed dementia, his wishes would not matter in any case.
It was noteworthy that the majority of participants had no privacy concerns. Some said that they saw no inherent conflict between technology and privacy. One participant stated that
No, privacy is not interesting for me, it is not important, there is nothing dangerous about it. [P8]
Others expressed that they were fine with sharing information with people who cared about them:
I do not mind that the information about me is available to others who care about me [P4].
When asked with whom their private data should be shared, many said their doctors, while others said both their doctors and family members. Participants considered it practical for doctors to have their health data in case they needed assistance. Nevertheless, one participant did express concern about the misuse of her data:
I am not afraid that people come and look at my health data information at the doctor, for example, I’m not afraid of that, there is nothing dangerous for me, but I think that it’s bad if there would be misuse of my identity. [P7]
Likewise, another participant stated that they did not know how to protect their data.
Throughout the interviews, some participants expressed a concern that welfare technology could make them feel monitored; however, they still felt positive about it overall. Some said that the use of cameras would be inappropriate, but others thought that cameras would be acceptable if videos were only sent to their doctor in the event of a fall. Some participants also expressed a desire for welfare technology to be automated, as they felt that pressing buttons or programming a system would be tedious.
Participants also expressed concern about welfare workers losing their jobs to technology. However, one participant noted that technology always differed from generation to generation and that new changes needed to be embraced:
… things can look quite obvious to a new generation, but then there are those barriers that must be broken for us [the older], we must accept that things don’t stay the same. [P2]
Isolation was also mentioned as a concern. One participant stated that he did not wish to stay alone at home watching TV or staring at a wall unable to move if he became sick and had to rely on help. Instead, he regarded a nursing home as a place with people around:
I saw when my wife was at the nursing home, there she had people to talk to. My neighbour has no one to talk to, I go every now and then [to visit her] for 10 or 15 minutes but, no, I will absolutely go to the nursing home, I already told my sons, if I begin to get dementia I don’t want to stay at home and stare at the wall. [P3]
Most participants also stated that they preferred human care to technological care. However, some noted that they felt no need to bother home care staff for minor needs, such as pill administration; instead, they would prefer a pill-dispenser device. However, many emphasised that welfare technology should not replace human care, such as one woman who stressed that
Nothing can replace human contact. The more helpless you are, the more you need for people to come and check on you once in a while. [P9]
Reflections Of Today And Tomorrow- Awareness Of Own Health
Feeling Healthy, Independent, Self-Sufficient And Safe
Most of the participants were autonomous and performed daily housework such as cooking, ironing, and grocery shopping. However, many said that they also hired cleaning aids, although mainly for convenience rather than out of necessity. In general, they took good care of their health and had an active life. Many had yearly medical check-ups, exercised several times a week, went for daily walks outside, or even tested their balance by standing on one leg.
All participants said that their independence, including the freedom to enjoy different hobbies and activities, was very important to them. They mentioned numerous activities, such as going to music clubs, hunting, watching TV, gardening, meeting friends for coffee, skiing, cooking, going to church and greeting people, going to dinner at social clubs, woodworking, knitting, reading, dancing, singing, etc. Some expressed that as long as they could live fully, they enjoyed their ageing. One of the oldest participants (89 years old) stated:
I would like to live long, see how it goes with everything and everyone, as long as I can have fun, take part in things, see, read, and dance and sing … I would very much like to be independent and live by myself. [P9]
An interesting finding was that many participants expressed no fear of dying, but were afraid of falling or of being mistreated, hospitalised, or in pain. One participant noted:
I have lived a long life already, and I cannot think of being crippled and unable to move or the like, lying in a bed or the like, no. [P5]
Regarding their situational safety, all participants felt safe in their neighbourhoods and stated that neighbours took care of each other; for example, neighbours called to check on them if they saw something off, and vice versa. One said:
I was in [city name] last week and stayed overnight but I didn’t turn off the lights from my house when I left, because I didn’t want my house to be so dark when I came back. So she [neighbour] called me in the evening and asked me if I was sick because she saw light in my house but no noise. [P6]
Similarly, some participants knew a neighbour’s phone number and had given a relative’s phone number to a neighbour to use in case of emergency. In addition, one participant’s neighbours had a key to her house to use in case something happened to her. Others said that they always told their neighbours if they planned to be away for a night or longer.
Facing Own Ageing- Preparedness For Unpredictable Scenarios
Although all participants felt relatively healthy, most had minor health problems, such as back pain, vertigo, high blood pressure, sciatica, heart problems, or knee pain. Most of the participants expressed that their health conditions determined their life choices and activities; sometimes they had needed to stop an activity or change their habits due to ageing, such as needing to sleep at specific times due to back pain, giving up playing golf due to increasing allergies, reading less, or playing cards instead of doing more physical activities.
Participants were also aware of the increased risks of becoming sick due to ageing. All but one were widowed and had experienced the loss of a partner, and several of the male participants expressed that it had been difficult to deal with their wives’ sicknesses. In addition, some participants had neighbours with health issues, which had caused them to reflect about their own health risks. Participants mentioned strokes, being confined to a wheelchair, falling and being unable to get up, and needing assistance with medication as being among their fears of future health problems. Most of the participants had prepared an action plan to implement in case something happened to them, such as calling an ambulance immediately. Most also said that they would prefer that any welfare technology alarm be sent directly to an ambulance first, and then alert their families afterwards.
Some participants also noted that living alone could present risks and challenges, especially in case of sickness. Some of the male participants also expressed a dislike of living alone:
I think it is very sad to sit here alone in the mornings, when it is dark and I don’t want to go out … you come home, there is no one waiting for you, no, nothing, I have done it for several years now. [P3]
However, many of the female participants enjoyed living alone. One woman said:
It is a luxury you know, it’s a luxury to live like this, alone all the time, I eat whatever I want, I can buy whatever I want, eat food whenever I want, and I enjoy myself with it, I can go to bed whenever I want (laughs), I can watch whatever I please on the TV, and I do not need to consider anybody, but of course, one misses one or two to talk to, on what I have seen on the TV, on what I have read. [P9]
These two participants gave different perspective of living alone. Most interestingly, the five female participant shared the same perspective of enjoyment living alone, while the four male participants expressed displeasure of living alone.
Reflecting on the question of staying in their homes for the rest of their lives, one woman expressed that the future is uncertain:
That is hard to answer because it is hard to say what one wishes for, one can relate to how the reality is today, there’s no problem to live here, but no one knows the future, so I cannot answer that exactly, it will be what it will be … But I don’t go around worrying about how my future will be, I don’t do that. [P7]
Welfare Technology—A Valuable Addition To Tomorrow’s Homes
Participants in this study described their attitudes towards welfare technology based on their current experiences. They reflected on the benefits and drawbacks that welfare technology could bring as they aged. Most desired to live in their homes for as long as they could maintain their independence and a dignified lifestyle, suggesting that welfare technology could be a valuable addition for them in the future. The main theme we identified regarding our participants’ attitudes towards welfare technology can therefore be summarised as ‘welfare technology—a valuable addition to tomorrow’s homes’.
Discussion
This study explored the attitudes of older people towards welfare technology. Throughout the interviews, participants reflected about their current and future lives. Overall, most of the participants felt themselves to be healthy and independent, but they were aware of their ageing and had reflected on changes that might be needed in the future to make it safer to remain in their own homes. Most participants tried to maintain a healthy lifestyle, both physically and mentally; they stated that health was the most important factor for ageing in place and that their lifestyle was dictated by their health. They were therefore aware that ageing is accompanied by frailty and vulnerability, especially when living alone, and they recognised the need to adapt as they aged and were open to making changes as needed. This likely influenced their receptiveness to welfare technology. In addition, some participants had already adapted their homes to their needs by removing furniture or carpets to reduce the risk of falling, and many were therefore glad to learn about the development of HBM welfare technology.
Notably, all participants stated that they trusted the Norwegian healthcare system. Most said that health alarms should first be sent to their doctors and only second to their families. One possible reason for such trust could be that Norway, along with other Scandinavian countries, operates a 'welfare state' that emphasises egalitarianism and individual autonomy regardless of social class.5 Scandinavians therefore believe in freedom with autonomy5 and the right to good public services. A similar context to the Scandinavian is the one of the United Kingdom, where both regions have a single-payer health care system which facilitates the government willingness to invest and engage in welfare technology promotion in public policy. These countries provide good support for the transition to welfare technology, partially thanks to the government implementation of privacy policies and regulations, contrary to the context of the United States.50 In addition, the healthcare provided by the Norwegian government is regarded as a ‘material basis for not becoming dependent on others’5 including one’s family. According to the Norwegian Municipal Health and Care Service Act of 2011, municipalities in Norway are obligated to provide healthcare to residents when needed.51 However, although all of our participants were aware of the municipalities’ legal obligations, they stated that they preferred to buy anything they could afford instead of asking for health care services to the municipality for small needs, such as pill administration. Several participants also viewed welfare technology as advantageous because they perceived it as being more cost-effective than human healthcare services, as also reported in previous studies.25
Most participants also said that they did not wish to be a burden on their families or society. This sense of 'burden' might be due to the fact that families in Norway, as in other Scandinavian countries, are seen as having a 'balance reciprocity between the social and emotional obligations with individual boundaries and autonomy'.5 As such, traditional obligations are disregarded because personal dependency is reduced. Thus, there is no obligation for children to take care of their parents when ageing, nor do ageing parents expect it. This could be seen in some participants’ references to fears of losing their autonomy and independence if they moved in with their children.
Another interesting finding was that the majority of the participants frequently used technology, contrary to a common belief that older people are reluctant to engage with technology.52 Previous studies have also found that older people’s perceptions of technology depend on their 'personal, social, and physical context'.53 In this study, the participants embraced technology that made their lives easier, such as online banking and keeping in touch with their families via social media. Thus, most participants also felt positively about welfare technology, which they regarded as enabling their safety while preserving their autonomy.
In contrast, some participants were not worried about falling and said that they currently had no ageing-related difficulties; they stated that they felt young and healthy and did not need help. However, they acknowledged that maybe 'other older people' might need it or that they might even need it themselves in the future; some noted that the future is uncertain and some things are beyond individual control. Consequently, many participants said that they had no need for welfare technology at present but acknowledged that this could change in the future, indicating an overall positive response to the development of welfare technology.
Another important finding was participants’ preferences regarding the use of technology versus human care. In general, participants preferred the idea of a combination of both. They felt that welfare technology could better preserve their independence and accommodate their preferences, and welfare technology was therefore preferable to moving to a nursing home as long as they could still take care of themselves. A possible reason for this preference among the participants could be that Scandinavian countries are recognized to be early adopters of technology for health care usage.54 However, a nursing home environment was preferable if they needed constant care or were no longer self-sufficient. This finding is consistent with previous research that human care and attention cannot be replaced with technology, because technology cannot handle human emotions or unexpected interactions.19,55 Previous research has also found that increased technology use can lead to patients being neglected;56 with technology providing care and 24 hr monitoring, 'face‐to‐face contact and hands‐on care'57 can decrease, and the consequent increase in social isolation is detrimental to older people’s social well-being.8,58 Consistent with these findings, participants in the present study emphasised that they did not wish to be isolated and that technology should never replace humans.
Although gender perspective were kept in mind during this study, only minor difference were found and should be used carefully due to the small number of participants. The sample consisted of almost half women and half men. The female participants expressed satisfaction in living along while the male participants were more social driven, and disliked to be alone.
Losses of dignity and autonomy were also central concerns among the participants. Ageing in place claims to be more cost-effective than nursing home care,25 but many participants therefore wondered if their dignity would be sacrificed to the economic interests of the municipality, such as by being forced to use welfare technology if they became cognitively impaired. A similar tension can be seen between the values of autonomy and safety.19 For example, Jacobs, et al19 argued that the use of technology in healthcare can be simultaneously both humanising and dehumanising, and they emphasised the importance of considering different aspects of person-centredness when implementing such technologies. Surprisingly, however, the participants had no concerns about privacy; instead, they felt that their safety was paramount. Hence, any concerns about being monitored or other invasions of privacy were superseded by concerns about safety. This is consistent with previous findings that older people are willing to trade privacy for autonomy8,50 and that the need for welfare technology thus outweighs privacy concerns.20
Strengths And Limitations
A strengths is that, although this study was performed in a Norwegian context, we consider the findings to be relevant in other contexts in which publicly funded healthcare for older people is regarded as a right and a form of natural autonomy.5
Another strength of this study is its focus on older women and men representing a group sparingly studied. The study thus contributes a new understanding of this group’s attitudes towards welfare technology. However, this study was exploratory in nature and our participants did not have personal experience of HBM welfare technology; further research is therefore needed about older people’s preferences and concerns after having “real” experiences with HBM welfare technology in their homes.
The participants all shared many things in common, such as self-perceived good health, an active lifestyle, and frequent use of modern technology; this represents a limitation of our sampling strategy that may have biased our results. It is conceivable that regional differences could also influence older people’s attitudes to welfare technology. For example, people from other parts of the country might have contributed to different attitudes. However, although a larger and more heterogeneous sample could lead to a more in-depth understanding, our participants nonetheless offered rich and varied descriptions of critically relevant issues.
Research on the implementation of welfare technology in older people is limited and this study contributes to the knowledge on this topic. Further research should pay attention to gender perspective differences, older people who are already users of welfare technology services, more attention to the different dimensions of participant’s health, multiple ethnicities, or a more varied grouped of socio economic status. Further research should also include younger older people (60–75 years old) than those targeted by the present research. This population might have different concerns regarding the use of such technology, including greater concerns related to privacy, as compared to the participants (> 75 years old) interviewed in this research. Their views are important as they may still be among the first group with a widespread ability to implement welfare technology.
Conclusion
The use of welfare technology is growing and promises many advantages for older people. HBM welfare technology that can detect abnormal behaviour in an individual, such as falls, is in the early stage of development, and older peoples’ attitudes towards its use therefore need to be explored. The present study suggests that older people view welfare technology as very convenient. The participants in this study were not 'afraid' of technology; rather, they perceived it as empowering, and welcomed any type of help to make their life better, easier, and safer. They wished to maintain their independence and to live at their own home for as long as they were self-sufficient, and although they raised some concerns and dilemmas about welfare technology, these were less important to them than the possible improvements to their safety and ability to age in place.
Acknowledgments
We thank all interviewees for participating in this project. We would also like to thank the SMART research group at University of South-eastern Norway for their financial support with interview transcriptions. The contribution did not have any role in the planning nor carrying out the study.
Abbreviations
HBM, Human behaviour modelling; GPS, Global positioning system.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Eurostat. Population structure and ageing. May 2018. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing_#_The_share_of_elderly_people_continues_to_increase Accessed March27, 2019.
- 2.Norway S. Population projections. June 26, 2018. Available from: https://www.ssb.no/en/folkfram Accessed March27, 2019.
- 3.Sanchez VG, Pfeiffer CF Legal aspects on smart house welfare technology for older people in Norway. Paper presented at: Intelligent Environments (Workshops); London, UK, 2016. [Google Scholar]
- 4.Norway S. Innbyggerne i store kommuner venter lengst på omsorgstjenester. 2017. Available from: https://www.ssb.no/helse/artikler-og-publikasjoner/innbyggerne-i-store-kommuner-venter-lengst-pa-omsorgstjenester Accessed April17, 2019.
- 5.Vike H. Politics and Bureaucracy in the Norwegian Welfare State: An Anthropological Approach. Springer; 2017. [Google Scholar]
- 6.Norway S. Nursing and care services 2017. 2018. Available from: https://www.ssb.no/en/helse/artikler-og-publikasjoner/nursing-and-care-services-2017 Accessed May06, 2019.
- 7.sykepleierforbund n. Stor sykepleiermangel i Norge. 2019. Available from: https://www.nsf.no/vis-artikkel/4383476/1740674/Stor-sykepleiermangel-i-Norge Accessed April17, 2019.
- 8.Sánchez VG, Taylor I, Bing-Jonsson PC. Ethics of smart house welfare technology for older adults: a systematic literature review. Int J Technol Assess Health Care. 2017;33(6):691–699. doi: 10.1017/S0266462317000964 [DOI] [PubMed] [Google Scholar]
- 9.Rashidi P, Mihailidis A. A survey on ambient-assisted living tools for older adults. IEEE J Biomed Health Inform. 2013;17(3):579–590. [DOI] [PubMed] [Google Scholar]
- 10.Brynn R. Universal design and welfare technology. Stud Health Technol Inform. 2016;229:335–344. [PubMed] [Google Scholar]
- 11.Norway S. Færre institusjonsplassar i omsorgstenesta. 2019. Available from: https://www.ssb.no/helse/artikler-og-publikasjoner/faerre-institusjonsplassar-i-omsorgstenesta Accessed April17, 2019.
- 12.Fachinger U, Henke K-D. Der private Haushalt als Gesundheitsstandort. Theoretische Und Empirische Analysen Europäische Schriften Zu Staat Und Wirtschaft. 2010;31. [Google Scholar]
- 13.Jankowski N, Schönijahn L, Wahl M. Telemonitoring in home care: creating the potential for a safer life at home In: Kollak I, editor. Safe at Home with Assistive Technology. Cham: Springer; 2017:81–93. [Google Scholar]
- 14.Wiles JL, Allen RE, Palmer AJ, Hayman KJ, Keeling S, Kerse N. Older people and their social spaces: A study of well-being and attachment to place in Aotearoa New Zealand. Soc Sci Med. 2009;68(4):664–671. doi: 10.1016/j.socscimed.2008.11.030 [DOI] [PubMed] [Google Scholar]
- 15.Otnes B. Utviklingslinjer i pleie‐og omsorgstjenestene. Bærekraftig Omsorg. 2012;57–78. [Google Scholar]
- 16.Anker-Hansen C On Making the Invisible Visible [Doctoral Thesis]. Norway: Department of Nursing and Health Sciences, University of South-Eastern Norway; 2019. [Google Scholar]
- 17.Kollak I. Prerequisites: assistive technologies between user centered assistance and ‘Technicalization’ In: Kollak I, editor. Safe at Home with Assistive Technology. Cham: Springer; 2017:1–4. [Google Scholar]
- 18.Official Norwegian Reports NOU 2011: 11 Chapter 1, 2 and 3. Innovation in the Care Services. Norway: Ministry of Health and Care Services; 2011. [Google Scholar]
- 19.Jacobs G, van der Zijpp T, van Lieshout F, van Dulmen S. Research into person-centred healthcare technology: A plea for considering humanization dimensions In: McCormack B, Dulmen S, Eide H, Skovdahl H, Eide T, editors.Person-Centred Healthcare Research. Oxford: Wiley-Blackwell; 2017:61–68. [Google Scholar]
- 20.Karlsen C, Moe CE, Haraldstad K, Thygesen E. Caring by telecare? A hermeneutic study of experiences among older adults and their family caregivers. J Clin Nurs. 2018. doi: 10.1111/jocn.14744 [DOI] [PubMed] [Google Scholar]
- 21.Mahoney DF, Purtilo RB, Webbe FM, et al. In-home monitoring of persons with dementia: ethical guidelines for technology research and development. Alzheimer’s Dementia. 2007;3(3):217–226. doi: 10.1016/j.jalz.2007.04.388 [DOI] [PubMed] [Google Scholar]
- 22.Nutbeam D. Health promotion glossary. Health Promot Int. 1998;13(4):349–364. doi: 10.1093/heapro/13.4.349 [DOI] [PubMed] [Google Scholar]
- 23.Health TNDo. Recommendations on welfare technology solutions in the municipalities. 2019. Available from: https://www.helsedirektoratet.no/tema/velferdsteknologi/anbefalinger-om-velferdsteknologiske-losninger-i-kommunene Accessed May07, 2019.
- 24.Finkena S, Mörtbergba C. The Thinking House: configurings of an infrastructure of care. Infrastruct Healthcare. 2011:43. [Google Scholar]
- 25.Chan M, Estève D, Escriba C, Campo E. A review of smart homes—present state and future challenges. Comput Methods Programs Biomed. 2008;91(1):55–81. doi: 10.1016/j.cmpb.2008.02.001 [DOI] [PubMed] [Google Scholar]
- 26.Alam M, Reaz M, Ali MM, Samad SA, Hashim FH, Hamzah M Human activity classification for smart home: a multiagent approach. Paper presented at: 2010 IEEE Symposium on Industrial Electronics and Applications (ISIEA) Penang, Malaysia; 2010. [Google Scholar]
- 27.Bourobou S, Yoo Y. User activity recognition in smart homes using pattern clustering applied to temporal ANN algorithm. Sensors. 2015;15(5):11953–11971. doi: 10.3390/s150511953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fatima I, Fahim M, Lee Y-K, Lee S. A unified framework for activity recognition-based behavior analysis and action prediction in smart homes. Sensors. 2013;13(2):2682–2699. doi: 10.3390/s130202682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brdiczka O, Langet M, Maisonnasse J, Crowley JL. Detecting human behavior models from multimodal observation in a smart home. IEEE Trans Autom Sci Eng. 2009;6(4):588–597. doi: 10.1109/TASE.2008.2004965 [DOI] [Google Scholar]
- 30.Debes C, Merentitis A, Sukhanov S, Niessen M, Frangiadakis N, Bauer A. Monitoring activities of daily living in smart homes: understanding human behavior. IEEE Signal Process Mag. 2016;33(2):81–94. doi: 10.1109/MSP.2015.2503881 [DOI] [Google Scholar]
- 31.Sánchez VG, Skeie N-O Decision trees for human activity recognition in smart house environments. Paper presented at: Proceedings of The 59th Conference on Simulation and Modelling (SIMS 59); 26–28 September; 2018; Norway, Oslo Metropolitan University. [Google Scholar]
- 32.Park K, Lin Y, Metsis V, Le Z, Makedon F Abnormal human behavioral pattern detection in assisted living environments. Paper presented at: Proceedings of the 3rd International Conference on PErvasive Technologies Related to Assistive Environments; Samos, Greece, 23–25 June 2010. [Google Scholar]
- 33.Rozo C. Consideraciones éticas de la tecnología de asistencia en personas en condición de discapacidad: posibilitar o limitar la autonomía? Revista Latinoamericana De Bioética. 2010;10(18):056–065. doi: 10.18359/rlbi.978 [DOI] [Google Scholar]
- 34.McCormack B. Researching nursing practice: does person‐centredness matter? 1. Nurs Philoso. 2003;4(3):179–188. [DOI] [PubMed] [Google Scholar]
- 35.Baraas RC, Hagen LA, Pedersen HR, Gjelle JV. 15 doing eye and vision research in a person‐centred way. Person-Centred Healthcare Res. 2017;181. [Google Scholar]
- 36.Garrett JJ. Elements of User Experience, The: User-centered Design for the Web and Beyond. Pearson Education; 2010. [Google Scholar]
- 37.Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358(9280):483–488. doi: 10.1016/S0140-6736(01)05627-6 [DOI] [PubMed] [Google Scholar]
- 38.Kallio H, Pietila AM, Johnson M, Kangasniemi M. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72(12):2954–2965. doi: 10.1111/jan.13031 [DOI] [PubMed] [Google Scholar]
- 39.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 40.Patton MQ. Qualitative Evaluation and Research Methods. SAGE Publications, inc; 1990. [Google Scholar]
- 41.Sandelowski M. Sample size in qualitative research. Res Nurs Health. 1995;18(2):179–183. doi: 10.1002/nur.4770180211 [DOI] [PubMed] [Google Scholar]
- 42.Marshall MN. Sampling for qualitative research. Fam Pract. 1996;13(6):522–526. doi: 10.1093/fampra/13.6.522 [DOI] [PubMed] [Google Scholar]
- 43.Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry. 2002;36(6):717–732. doi: 10.1046/j.1440-1614.2002.01100.x [DOI] [PubMed] [Google Scholar]
- 44.Lie ML, Lindsay S, Brittain K. Technology and trust: older people’s perspectives of a home monitoring system. Ageing Soc. 2016;36(7):1501–1525. doi: 10.1017/S0144686X15000501 [DOI] [Google Scholar]
- 45.Graneheim UH, Lindgren B-M, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ Today. 2017;56:29–34. doi: 10.1016/j.nedt.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 46.Mishler EG. Research Interviewing: Context and Narrative. Cambridge: Harvard University; 1986. [Google Scholar]
- 47.Krippendorff K. Content Analysis. New York: Oxford University Press; 1989. [Google Scholar]
- 48.Lincoln YS, Guba EG. Establishing trustworthiness. Naturalistic Inquiry. 1985;289:331. [Google Scholar]
- 49.NSD. The Norwegian Center for Research Data - Assessment of projects. Available from: https://nsd.no/personvernombud/en/help/index.html Accessed September17, 2019.
- 50.Berridge C. Breathing room in monitored space: the impact of passive monitoring technology on privacy in independent living. Gerontologist. 2016;56(5):807–816. doi: 10.1093/geront/gnv034 [DOI] [PubMed] [Google Scholar]
- 51.Fjelltun AMS, Henriksen N, Norberg A, Gilje F, Normann HK. Carers’ and nurses’ appraisals of needs of nursing home placement for frail older in Norway. J Clin Nurs. 2009;18(22):3079–3088. doi: 10.1111/j.1365-2702.2008.02663.x [DOI] [PubMed] [Google Scholar]
- 52.Mitzner TL, Boron JB, Fausset CB, et al. Older adults talk technology: technology usage and attitudes. Comput Human Behav. 2010;26(6):1710–1721. doi: 10.1016/j.chb.2010.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peek ST, Luijkx KG, Rijnaard MD, et al. Older adults’ reasons for using technology while aging in place. Gerontology. 2016;62(2):226–237. doi: 10.1159/000430949 [DOI] [PubMed] [Google Scholar]
- 54.Berridge C, Furseth PI, Cuthbertson R, Demello S. Technology-based innovation for independent living: policy and innovation in the United Kingdom, Scandinavia, and the United States. J Aging Soc Policy. 2014;26(3):213–228. doi: 10.1080/08959420.2014.899177 [DOI] [PubMed] [Google Scholar]
- 55.Sparrow R, Sparrow L. In the hands of machines? The future of aged care. Minds Mach. 2006;16(2):141–161. doi: 10.1007/s11023-006-9030-6 [DOI] [Google Scholar]
- 56.Grisot M, Moltubakk Kempton A, Hagen L, Aanestad M. Data-work for personalized care: examining nurses’ practices in remote monitoring of chronic patients. Health Informatics J. 2019;1460458219833110. [DOI] [PubMed] [Google Scholar]
- 57.McCormack B, van Dulmen S, Eide H, Skovdahl K, Eide T. Person-centred Healthcare Research. John Wiley & Sons; 2017. [Google Scholar]
- 58.Detweiler CA, Hindriks KV. A survey of values, technologies and contexts in pervasive healthcare. Pervasive Mob Comput. 2016;27:1–13. doi: 10.1016/j.pmcj.2015.09.002 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Eurostat. Population structure and ageing. May 2018. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing_#_The_share_of_elderly_people_continues_to_increase Accessed March27, 2019.