Abstract
Purpose
Diammonium glycyrrhizinate (DG) is a replacement for glycyrrhizic acid, which is used as a hepatic protector in clinical practice for most liver diseases. The potential role of immune response during autoimmune hepatitis—induced by concanavalin A (Con A)—remains to be elucidated.
Methods
C57BL/6J mice were treated with two different doses of DG (75 and 200 mg/kg) 2 hrs before administering Con A. The mice were sacrificed after administering Con A for 0, 6, and 24 hrs. Liver damage grade and serum alanine aminotransferase (ALT), aspartate aminotransferase (AST) and total bilirubin levels were evaluated. The expression level of cleaved-caspase 3 in liver was detected by Western blotting. Inflammatory cytokines such as tumor necrosis factor α (TNF-α), interleukin-6 (IL-6), and interferon γ (IFN-γ) in liver were detected by RT-PCR. Thymus, peripheral blood, spleen, and liver tissues were collected to analyze the percentages of NKT cells, subsets of CD4+CD25−CD69+ and CD8+CD69+ T cells, and subsets of regulatory T cells (Tregs).
Results
Our results revealed that DG pre-treatment significantly decreased the serum ALT and AST levels and improved the histological damage in Con A-induced autoimmune liver injury. Pre-treatment with DG down-regulated the inflammatory cytokines upon challenge with Con A. The DG pre-treatment inhibited the apoptosis of T lymphocytes in the thymus. Further, it effectively suppressed the proliferation of CD4+CD25−CD69+ and CD8+CD69+ subsets in the peripheral blood and spleen. In addition, the DG pretreatment significantly downregulated the frequency of NKT cells, while upregulating the frequency of Tregs in the liver.
Conclusion
We believe that the potential protective effect of DG against Con A-induced hepatitis may be partially attributed to its inhibitory activities on inflammatory cytokines in the livers, lymphocyte apoptosis in the thymus, NKT cells proliferation, and activation of CD8+T cells; further, there may also be a possibility of DC promoting Tregs proliferation.
Keywords: autoimmune hepatitis, concanavalin A, diammonium glycyrrhizinate, NKT cells, regulatory T-cell
Introduction
Autoimmune hepatitis (AIH)—a chronic inflammatory liver injury—is characterized by interface hepatitis, hyper-globulinemia, appearance of autoantibodies, and immune imbalance.1 There are complex etiologies of AIH that include genes, environment, and immune disorders.2 Patients with AIH who miss timely treatment may progress to terminal liver diseases.3 Although the diagnostic guidelines for AIH have been proposed previously, there are still some problems.4,5 The main challenge is that the etiology and molecular mechanisms of AIH remain unclear; however, it is known that the imbalance between regulatory T cells (Tregs) and effector lymphocytes plays an important role in the occurrence of AIH.5 Some studies indicated that differentiation of T cells into effector T cells promoted the fatal progression of AIH in a mouse model.6 Other studies suggested that Tregs from AIH patients were more prone to acquire effect properties than those from healthy people; after treatment, Tregs from AIH patients exhibited a decreasing trend in both member and function.7 Natural killer T (NKT) cells account for about 20–35% of the total lymphocytes in the liver of mice and about 10–15% of total lymphocytes in the human liver;8 studies focused on NKT cells indicate that they play a pro-inflammatory and pro-apoptosis role in liver diseases.8–10 The NKT cells are one of the most important type of effector cells related to immune liver injury,11 and the imbalance between Tregs and NKT cells distinctly trigger the development of autoimmune responses.12 These studies suggested that once Tregs lose the capacity of inhibiting the proliferation and function of effector T cells, the disease will occur and progress rapidly.
Diammonium glycyrrhizinate (DG)—an ammonium salt preparation of 18-alpha-glycyrrhizin—exhibits anti-inflammation, immunomodulation, anti-anaphylaxis, and membranous protection effects.13–15 Currently, the family of glycyrrhizin is used in clinical practice as an effective liver protector against most hepatic diseases such as chronic viral hepatitis,16 drug-induced liver injury,17 nonalcoholic fatty liver disease,18,19 autoimmune hepatitis,20 and hepatocellular carcinoma.21 Previous studies concluded that DG exerted a protective effect by downregulating inflammation cytokines, suppressing the NF-κB pathway, and restoring superoxide dismutase.22,23 However, the potential protection mechanisms of DG in AIH are still not clear.
In this study, we established a concanavalin A (Con A)-induced autoimmune hepatitis model to identify the protective role of DG in AIH and elucidate its potential mechanisms. We investigated NKT cells and CD4+CD25+Foxp3+ Tregs from the liver, and the CD4+CD25−CD69+ and CD8+CD69+ subsets from the periphery blood, spleen, and liver because the imbalance of the immune system is considered a significant factor in AIH progression,5–7,24,25 and CD69 has gained considerable research attention owing to its complex inflammatory and immune-regulatory properties.26 The present study helped us improve our understanding of the mechanism of DG protection in an autoimmune liver injury.
Materials And Methods
Animals And Drugs
Six-to-eight-weeks-old male C57BL/6J mice were procured from the Animal Center of Health and Science Center, Peking University (Beijing, China), where mice were kept in specific pathogen-free conditions. All mice were adapted to standard laboratory conditions (regularly 12 hrs lights/dark cycle, 21±2°C) for at least one week. DG was offered by ChiaTai-Tianqing Pharmaceutical Co., Ltd. (Nanjing, China), and it was stored at room temperature. Further, it was diluted to a special concentration (10 mg/mL) with 0.9% saline and was injected intraperitoneally into the mice just single shot 2 hrs before the experiment. The animal experiments were supported by the National Institutes of Health Guide for the Care and Use of Laboratory Animals, National Institutes of Health. And the study was approved by the ethics committee of Animal Experiments and Experimental Animal Welfare Committee of Capital Medical University on December 12, 2017 [number AEEI-2017-136]. All experimental manipulations were performed in the Institute of Infectious Diseases, Beijing Ditan Hospital (Beijing, China).
Con A-Induced Hepatitis
The animals were intravenously injected with Con A (20 mg/kg) to establish immune-mediated liver-injury models. The experimental mice were pre-treated with DG intraperitoneal injections at dosages of 75 mg/kg and 200 mg/kg,13,15,17 2 hrs before the Con A injection. The control mice were injected with an equal volume of saline. The mice were then sacrificed after administering Con A for 0, 6, and 24 hrs. Meanwhile, we collected the serum of the animals for transaminases tests, and the blood, spleen, thymus, and a part of liver for subsequent flow cytometry analyses. The other part of liver specimens was used to assess the level of pathological injury. All the abovementioned experiments were performed in triplicate.
Serum Level Of Transaminases
Blood samples were collected after mice were sacrificed, and the samples were centrifuged at 3000×g for 10 mins to obtain the serum. Next, the levels of serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), and total bilirubin were measured using a biochemical kit (Sichuan Maccura Biotechnology, Sichuan, China).
Liver Histological Assessment
Livers from the mice were fixed in formalin. After paraffin embedding, sectioning, and hematoxylin-eosin staining, thin tissue sections were acquired and used to investigate the liver injury. The revised Knodell protocol was adopted to assess liver damage.27 In brief, 0 indicated no inflammation or necrosis; 1, confluent or intralobular inflammation; 2, slight piecemeal necrosis or focal necrosis; 3, medium confluent inflammation and piecemeal necrosis, or serious focal necrosis; and 4, serious confluent inflammation and piecemeal necrosis, or bridging necrosis. The damage score was evaluated in a blinded manner.
Western Blot Analysis
Liver tissues were lysed by RIPA lysis buffer (Solarbio Science & Technology Co. Ltd., Beijing, China). The proteins were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE), and transferred to polyvinylidene fluoride (PVDF) membranes. The following antibodies were used to incubate the proteins: anti-β-actin antibody (1:1000 dilution; Cell Signaling Technology, Danvers, MA, USA), anti-caspase-3 antibody (1:1000 dilution; Cell Signaling Technology, Danvers, MA, USA). Then, they were incubated with the second conjugated immunoglobulins (ZF-0316; ZSGB-BIO Co. Ltd., Beijing, China). Finally, the proteins were detected by the method of enhanced chemiluminescence (ECL).
Reverse Transcription‑polymerase Chain Reaction (RT‑qPCR) Analysis
Liver tissues were lysed by TRIzol (Invitrogen, Carlsbad, CA, USA) for total RNA extraction. Reverse transcription of total RNA into cDNA was used by a TransScript First-Strand cDNA Synthesis SuperMix (TransGen Biotech, Beijing, China). RT-PCR was performed using a PrimeScriptTM RT reagents kit (TaKaRa, Shiga, Japan) following the manufacturer’s instructions. GAPDH was determined as a reference gene and the relative levels of target genes were calculated using the 2-ΔΔCT method. The sequences of the primers used for PCR are shown as following: GAPDH Forward: TGGCCTTCCGTGTTCCTAC, GAPDH Reverse: TGGCCTTCCGTGTTCCTAC; TNF-α Forward: CTGAACTTCGGGGTGATCGG, TNF-α Reverse: GGCTTGTCACTCGAATTTTGAGA; IL-6 Forward: TAGTCCTTCCTACCCCAATTTCC, IL-6 Reverse: TTGGTCCTTAGCCACTCCTTC; IFN-γ Forward: ATGAACGCTACACACTGCATC, IFN-γ Reverse: CCATCCTTTTGCCAGTTCCTC.
Flow Cytometry
We harvested the blood, spleen, liver, and thymus when the mice were sacrificed. After lysing blood, levigating tissues, centrifuging, and filtrating, single-cell suspensions were finally obtained. For liver interstitial cells, we performed density-gradient centrifugation using Percoll. Next, these single-cell suspensions were stained with the following fluorescent monoclonal antibodies CD69-FITC, CD25-PE, CD8-PerCP, and CD4-APC for peripheral blood mononuclear cells (PBMC), splenocytes, and liver; Annexin V-FITC, CD8-PE, 7aad-PerCP, and CD4-APC for thymocytes; and NK1.1-FITC, CD3-PE, FasL-PerCP, CD4-FITC, Foxp3-PE, and CD25-PerCP for liver interstitial cells. All fluorescent monoclonal antibodies were purchased from eBioscience company (San Diego, CA, USA). The frequencies of our expected subsets were detected by flow cytometry (FACS Caliber, BD Bioscience Company, USA).
Statistical Analysis
Quantitative data were expressed as mean ± standard deviation (SD). We performed statistical analysis with SPSS 19.0. The one-way ANOVA and Kruskal–Wallis test were used to analyze most of our data. Statistical significance was determined as P < 0.05.
Results
DG Pre-Treatment Alleviated Concanavalin A-Induced Liver Damage
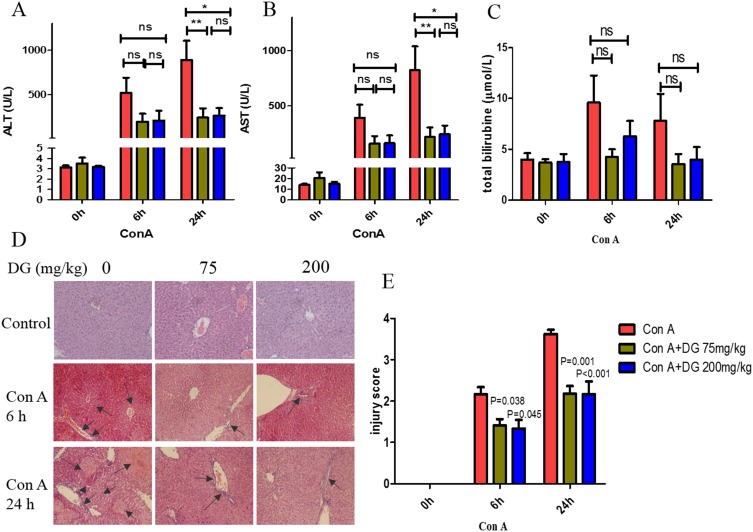
To investigate the effect of DG on Con A-induced hepatitis, we tested the serum liver enzymes and total bilirubin under Con A administration at different time-points with or without DG pre-treatment. The results showed that DG inhibited the increase of both ALT and AST levels, especially after Con A administration for 24 hrs (Figure 1A and B). Compared with only Con A administration (890.42 ± 216.32 U/L), mice that underwent DG pretreatment (75 mg/kg and 200 mg/kg) exhibited lower ALT levels after administering Con A for 24 hrs (241.71 ± 106.09 U/L, P = 0.007; 265.62 ± 82.43 U/L, P = 0.032, Figure 1A). A similar decreasing trend was observed in AST levels (823.71 ± 214.21 in Con A vs 220.06 ± 85.84 in Con A+DG 75 mg/kg, P = 0.008; and vs 244.70±79.09 in Con A+DG 200 mg/kg, P = 0.022, Figure 1B). However, the total bilirubin was not significantly different between control group and DG pre-treatment groups (Figure 1C). Next, we compared the pathological injuries caused to the livers in these different treatment groups with H&E staining (Figure 1D). The results showed that livers without DG pretreatment exhibited a more significant disorder of hepatic lobule, a larger necrosis size, and more inflammatory cells infiltration. The liver injury score was assessed using the standard mentioned above. As shown in Figure 1E, the damage score of the control group was also higher than that of the groups that received DG pretreatment.
Figure 1.
Pre-treatment with DG improves the liver injury upon challenge with Con A. Levels of serum alanine aminotransferase (ALT) (A) aspartate aminotransferase (AST) (B) and total bilirubin (C) in mice treated with different doses of DG before and after Con A administration for 6 hrs and 24 hrs. (D) H&E staining for livers (200x). The black arrows indicate the inflammatory infiltration and necrosis areas. (E) The injury score evaluation was in accordance with pathological staining. Data in the graph indicate P-values between the DG pretreatment and control groups. *, ** mean P < 0.05 and P < 0.01, respectively. N = 8 for each group. This experiment was performed in triplicate.
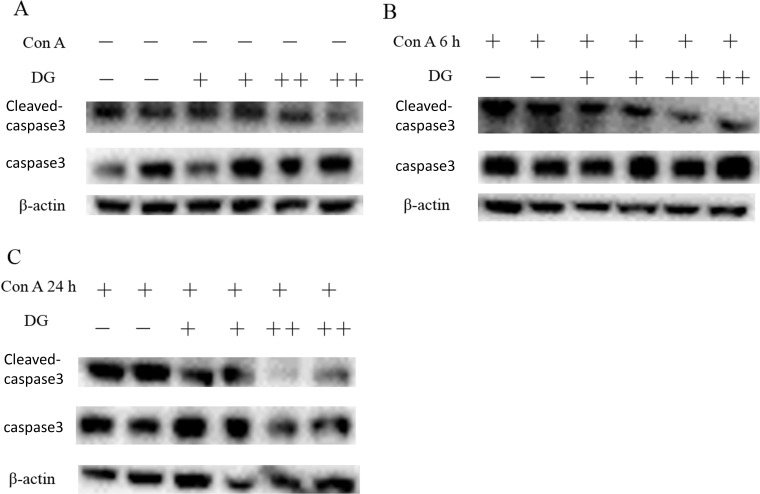
To further compare the liver injury between the control group and DG pre-treatment group in Con A-induced autoimmune injury, we detected the expression level of cleaved-caspase3 in liver tissues by Western blotting. As shown in Figure 2, there was no significant difference between the control group and DG pre-treatment group before and after Con A administrated for 6 hrs; however, after Con A administration for 24 hrs, the expression level of cleaved-caspase 3 in DG pre-treatment group (both 75 mg/kg and 200 mg/kg) exhibited a marked decreasing trend in comparison with that of control group (Figure 2C).
Figure 2.
Pre-treatment with DG inhibited the expression level of cleaved-caspase 3 in Con A-induced liver injury. (A) The expression levels of cleaved-caspase 3 with or without pre-treatment of DG at the baseline. (B), (C) The expression levels of cleaved-caspase 3 with or without pre-treatment of DG after Con A administration for 6 and 24 hrs, respectively. “+” and “++” of DG mean 75 mg/kg and 200 mg/kg, respectively. N = 2 for each group. This experiment was performed in triplicate.
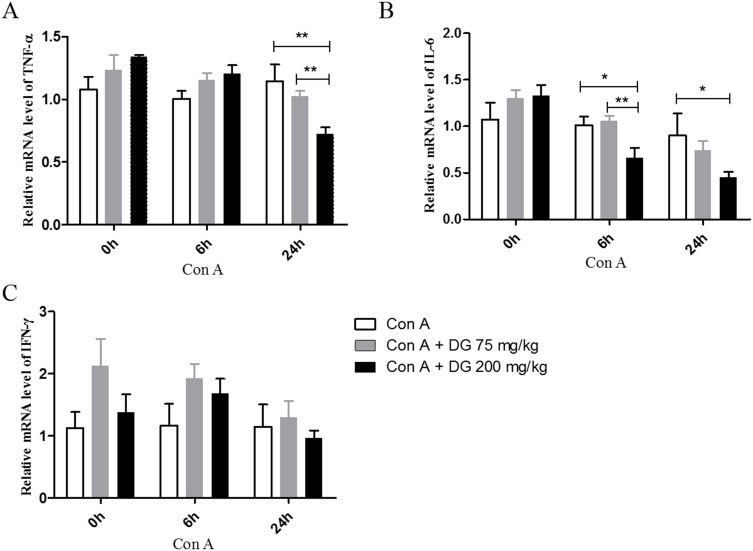
Pre-Treatment With DG Inhibited The Levels Of Inflammatory Cytokines
It is well known that inflammatory cytokines play a crucial role in autoimmune response. To investigate the effect of pre-treatment with DG on the levels of inflammatory cytokines in Con A-induced liver injury, we compared the mRNA levels of TNF-α, IL-6, and IFN-γ in liver tissues by RT-PCR. Our results showed that pre-treatment with DG significantly down-regulated the mRNA level of TNF-α after administrating with Con A for 24 hrs (Figure 3A). The mRNA level of IL-6 from the groups of DG pre-treatment exhibited a decreasing trend in comparison with that of the group of Con A administrating alone (Figure 3B). However, as for the level of IFN-γ, there was no significant difference between the control group and DG pre-treatment groups (Figure 3C).
Figure 3.
Pre-treatment with DG down-regulated the mRNA levels of inflammatory cytokines in Con A challenged mice. (A–C) The relative mRNA levels of TNF-α, IL-6, and IFN-γ, respectively. *, ** mean P < 0.05 and P < 0.01, respectively. N = 4 for each group. This experiment was performed in triplicate.
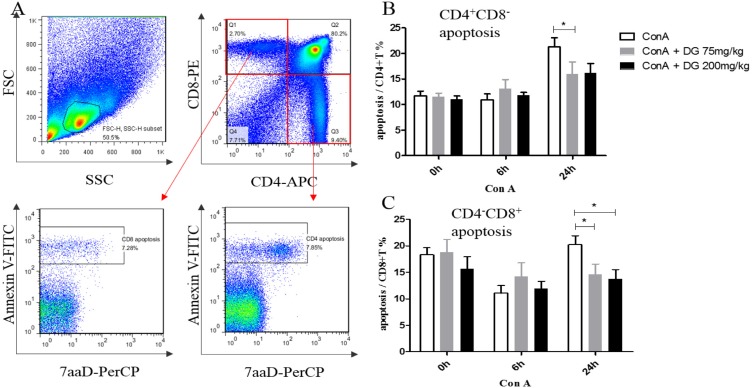
DG Pre-Treatment Suppressed CD4+ And CD8+ T Cells Apoptosis In The Thymus
The immune response of T lymphocytes is a primary defense in Con A-induced liver injury. As the thymus is the most important place for T lymphocytes development, we wondered whether lymphocytes apoptosis in the thymus could be involved in the protection mechanism of DG in Con A-induced liver injury. We analyzed the apoptosis levels of CD4+ and CD8+ single positive T cells in the thymus before and after administering Con A for 6 and 24 hrs with or without DG pretreatment (Figure 4A). Interestingly, in comparison with the only Con A treatment, CD4+ T cells from the Con A + 75 mg/kg DG group showed a lower apoptosis phenomenon after administering Con A for 24 hrs (21.30 ± 1.79 in Con A vs 14.78 ± 2.20 in Con A + DG 75 mg/kg, P = 0.025; and vs 14.54 ± 1.62 in Con A + DG 200 mg/kg, P = 0.051, Figure 4B). In addition, the same result was also obtained for CD8+ T cells. After Con A administration for 24 hrs, the apoptosis level of CD8+ T cells in the DG pretreatment group significantly decreased compared with that in the control group (20.21 ± 1.70 in Con A vs 14.63 ± 1.93 in the Con A + DG 75 mg/kg, P = 0.035; and vs 13.76 ± 1.77 in Con A + DG 200 mg/kg, P = 0.043. Figure 4C).
Figure 4.
Levels of apoptosis of CD4+CD8− and CD4−CD8+ cells in the thymus were decreased with pre-treatment of DG in Con A challenged mice. (A) Analysis of T lymphocytes apoptosis levels in the thymus. (B) The apoptosis level of CD4+CD8− cells in Con A-induced immune injury with or without DG pre-treatment. (C) The apoptosis level of CD4−CD8+ cells in Con A-induced immune injury with or without DG pre-treatment. * indicates P < 0.05. N = 8 for each group. This experiment was performed in triplicate.
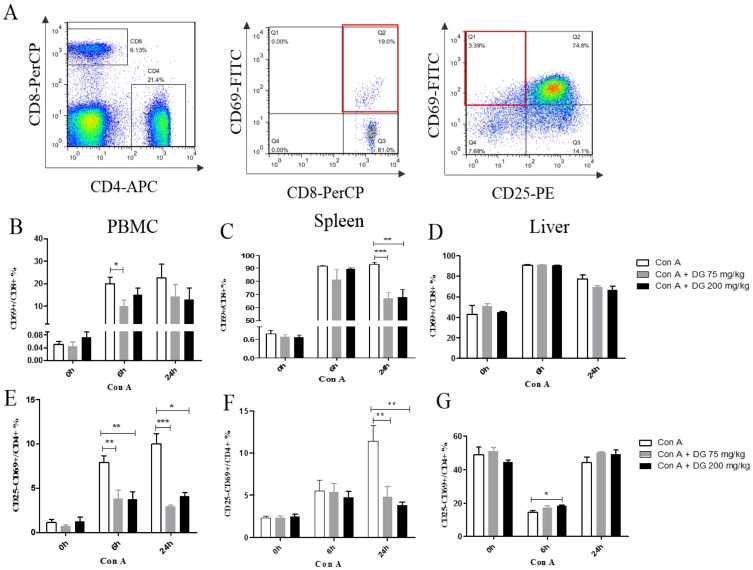
DG Inhibits The Proliferation Of CD8+CD69+ And CD4+CD25−CD69+ Subsets In Peripheral Blood And Spleen
As CD69 is considered an important immune modulatory molecule, we wondered whether CD69 accounts for the protection effect of DG in Con A-induced autoimmune hepatitis.26 We investigated the frequencies of CD8+CD69+ T cell subsets in the peripheral blood, spleen, and liver at different time-points with or without DG pretreatment (Figure 5A). After Con A was administrated, the frequency of the CD8+CD69+ subset significantly increased in the peripheral blood and spleen. Interestingly, we found that DG pretreatment inhibited the proliferation of the CD8+CD69+ subset in the splenocytes after Con A administration for 24 hrs (92.96 ± 1.24 in Con A vs 66.71 ± 4.78 in Con A + DG 75 mg/kg, P < 0.001; and vs 67.84 ± 5.79 in Con A + DG 200 mg/kg, P = 0.001, Figure 5C). A similar result also appeared in peripheral blood after Con A administration for 6 hrs (19.92±2.91 in Con A vs 9.99 ± 2.71 in Con A + DG 75 mg/kg, P = 0.022, Figure 5B). However, no statistical differences in the liver were observed between the control group and the Con A + DG group in our model (Figure 5D).
Figure 5.
Pre-treatment with DG suppressed the activation levels of CD4+ and CD8+ T cells. (A) Analysis of T lymphocytes activation levels. (B–D) The percentages of the CD8+CD69+ subset from the PBMC, spleen, and liver, respectively, in Con A-induced immune injury with or without DG pre-treatment. (E–G) The percentages of the CD4+CD25−CD69+ subset from the PBMC, spleen, and liver, respectively, in Con A-induced immune injury with or without DG pre-treatment. *, **, and *** mean P < 0.05, P < 0.01, and P < 0.001, respectively. N = 8 for each group. This experiment was performed in triplicate.
For the CD4 subset, we detected the frequencies of the CD4+CD25−CD69+ subset in blood, spleen, and liver at different time-points with or without DG pretreatment. Compared with the control group in the peripheral blood (7.90 ± 0.76), the frequency of the CD4+CD25−CD69+ subset appeared to show a decreasing trend after Con A administration for 6 hrs in the DG-pretreated group at dosages of 75 mg/kg (3.80 ± 0.97, P = 0.003) and 200 mg/kg (3.72 ± 0.89, P = 0.004, Figure 5E). Further, after Con A administration for 24 hrs, the result was found to be parallel with that of Con A administered for 6 hrs (10.01 ± 1.16 in Con A vs 2.96 ± 0.15 in Con A + DG 75 mg/kg, P < 0.001; and vs 4.06 ± 0.48 in Con A + DG 200 mg/kg, P = 0.034, Figure 5E). The frequency of the CD4+CD25−CD69+ subset in the spleen showed a similar decreasing trend at 24 hrs after Con A administration (11.47 ± 1.81 in Con A vs 4.84 ± 1.18 in Con A + DG 75 mg/kg, P = 0.002; and vs 3.80 ± 0.36 in Con A + DG 200 mg/kg, P = 0.001, Figure 5F). However, it was shown that the DG pretreatment upregulated the percentage of the CD4+CD25−CD69+ subset in the liver after Con A administration for 6 hrs (14.53 ± 1.011 in Con A vs 18.10 ± 0.694 in Con A+DG 200 mg/kg, P = 0.0236, Figure 5G).
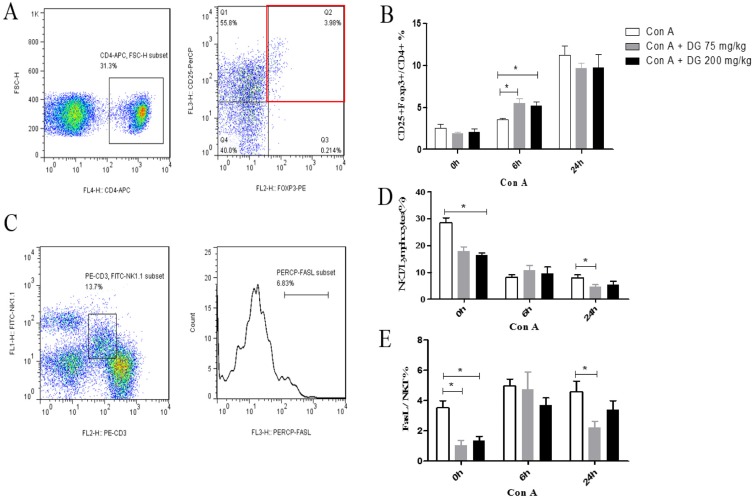
DG Promoted CD4+CD25+Foxp3+ Tregs Proliferation While Inhibiting NKT Cells Proliferation
Because NKT cells obviously account for Con A-induced autoimmune liver injury, regulatory T cells are well regulated to maintain immune homeostasis.8 We detected Tregs and NKT cells in the liver. As shown in our results, the DG pretreatment did not affect Tregs at the baseline (Figure 6B), but it markedly downregulated the percentage of NKT cells (28.47 ± 7.41 in Con A vs 17.85 ± 2.33 in Con A + DG 75 mg/kg, P = 0.068; and vs 16.5 ± 1.28 in Con A + DG 200 mg/kg, P = 0.015, Figure 6D), and the expression levels of FasL on the surface of the NKT cells (3.52 ± 1.40 in Con A vs 1.029 ± 0.482 in Con A + DG 75 mg/kg, P = 0.04; and vs 1.35 ± 0.508 in Con A + DG 200 mg/kg, P = 0.028, Figure 6E). After Con A administration, the frequency of Tregs significantly increased. Interestingly, we found that DG pretreatment significantly enhanced the increasing effect of Tregs after Con A administration for 6 hrs (3.54 ± 0.256 in Con A vs 5.56 ± 1.16 in Con A + DG 75 mg/kg, P = 0.028; and vs 5.18 ± 1.06 in Con A + DG 200 mg/kg, P = 0.023, Figure 6B). NKT cells were significantly decreased compared with the control group after Con A administration for 24 hrs (8.003 ± 2.614 in Con A vs 4.695 ± 1.611 in Con A + DG 75 mg/kg, P = 0.036, Figure 6D). Meanwhile, the expression level of FasL on the surface of NKT cells also showed a marked decreasing trend in the Con A + DG 75 mg/kg group in comparison with the control group after Con A administration for 24 hrs (4.59 ± 1.72 in Con A vs 2.24 ± 0.887 in Con A + DG 75 mg/kg, P = 0.022, Figure 6E).
Figure 6.
Pre-treatment with DG infected the frequencies of CD4+CD25+Foxp3+ Tregs and NKT cells in the livers in Con A challenged mice. (A) Analysis of Tregs in the liver. (B) The percentage of the Tregs subset from the liver in Con A-induced immune injury with or without DG pretreatment. (C) Analysis of NKT cells and expression of FasL on the surface of NKT cells in the liver. (D) The percentage of NKT cells from the liver in Con A-induced immune injury with or without DG pretreatment. (E) The percentage of FasL expressed on the surface of NKT cells from the liver in Con A-induced immune injury with or without DG pretreatment. *means P < 0.05. N = 8 for each group. This experiment was performed in triplicate.
Discussion
Diammonium glycyrrhizinate has been used as a liver protector for decades. However, its protective effect on AIH and the underlying molecular mechanism remain to be elucidated. In the present study, we found that DG pre-treatment could reduce serum ALT and AST levels and alleviate liver pathological damage in Con A-induced hepatitis. Histology staining showed mice that accepted DG pre-treatment had fewer inflammatory cells infiltration, lower hepatic cords destruction, and fewer necrosis sizes compared with that of administrating with Con A alone. Further detections indicated that pre-treatment with DG down-regulated the expression levels of cleaved-caspase 3 and the mRNA levels of inflammatory cytokines in Con A-induced liver injury. All these results indicated that DG plays a significant protective role in our experimental autoimmune hepatitis model. The potential mechanism may be related to the suppression effect of DG on the CD69+ subset proliferation of T lymphocytes, and in disrupting the balance of regulatory T cells and NKT cells.
Previous studies have shown that Con A injection induces apoptosis.28,29 We detected T cell apoptosis from the thymus in Con A-induced hepatitis with or without DG pretreatment. For our results, the apoptosis of CD4+ and CD8+ T lymphocytes in the thymus were consistent with previous studies mentioned above, which showed Con A increased apoptosis. Furthermore, DG downregulated cell apoptosis for both CD4+ and CD8+ T cells in the Con A-induced hepatitis model, which implied another protective mechanism of DG in Con A-induced liver injury. It is reported that the destruction of immune tolerance was involved in negative selection, and it induced the apoptosis of auto-reactive thymocytes.30 In this regard, we speculated that DG might mitigate the destruction of immune tolerance and reduce apoptosis in the thymus sequentially.
CD69 is a membrane receptor from the family of II C-type lectins and is known as an early leukocyte activation antigen. CD69 has a low expression in resting cells and is rapidly induced after cells activation.31 Our data showed a decreasing trend of the CD8+CD69+ subset in DG-pretreated mice compared with that of the control group. Based on this result, we speculated that CD8+CD69+ T lymphocytes play a pro-inflammation role in our model, and DG reduces liver injury probably because it downregulates the CD8+CD69+ subset. Previous studies also showed a similar result in different disease models; for example, García-Monzón et al32 detected that the CD8+CD69+ T cell subset was involved in the inflammation progression of chronic viral active hepatitis. Some researchers33 also found that enrichment of CD8+CD69+ in female adipose tissue may contribute to cardiovascular diseases. Murata et al34 established an arthritis model that can be induced by anti-type II collagen antibodies, which showed that CD69−/- mice behaved against joint inflammation. Moreover, Miki-Hosokawa et al35 found that CD69−/− mice inhibited lung inflammation by reducing the migration of Th2 cells. All these results suggested that CD69 might be a pro-inflammatory molecule in diseases' pathological progression.
Furthermore, we detected the frequency of CD4+CD25−CD69+ subsets. The percentage of the CD4+CD25−CD69+ subset showed a decreasing trend with DG pretreatment compared with only Con A administration. The CD4+CD25−CD69+ subset was first proposed in Han et al’s study,36 where CD4+CD25−CD69+ was described as a new type of Tregs and characterized by the negative expression of Foxp3 and IL-10, and it exerted a suppression effect in a cell–cell contact manner mediated by membrane-bound TGF-β1. However, the function of this subset needs to be clarified. Zhao et al37 reported that CD4+CD25−CD69+ was involved in leukemia relapse after hematopoietic stem cell transplantation. Gragegriebenow et al38 found that CD4+CD25−CD69+ might induce tumor immune escape in pancreatic ductal adenocarcinoma, which contributes to carcinoma progression. A similar result appeared in granulocyte colony-stimulating factor (G-CSF)-primed bone marrow grafts, in which the CD4+CD25−CD69+ subset showed a high frequency, which may account for severe graft-versus-host disease.39 Although further mechanism needs to be confirmed, we can speculate that the CD4+CD25−CD69+ subset may be an important trigger in tumor and immune response, and its enrichment could break or aggravate immune homeostasis. Our data presented a lower percentage of the CD4+CD25−CD69+ subset in the Con A + DG administration group compared with the group that accepted Con A administration alone. In this regard, we concluded that a lower frequency of CD4+CD25−CD69+ may contribute to the protective effect of DG in Con A-induced liver injuries.
The imbalance between the effector and regulatory cells in the immune system is known as a crucial trigger for autoimmune responses.8,12 NKT cells are abundant in liver tissues, and several studies have indicated that NKT cells contributed to liver damage as a type of effector cells.8–12,40 Alisan Kahraman et al41 indicated that NK1.1-positive NK/NKT cells accelerated the cholestatic liver injury by depending on a tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) pathway. While Tregs play an important anti-inflammation role in immune responses. Our results showed that DG pretreatment promoted CD4+CD25−CD69+ and CD4+CD25+Foxp3+ Tregs proliferation while inhibiting NKT cells proliferation, which indicated DG pretreatment protected liver injury by influencing the imbalance between effector and regulatory cells. Other studies have also reported that NKT cells and Tregs may antagonize each other in asthma.12
There were four limitations to our study. First, the protective role of DG in primary hepatocytes was not detected in vitro; second, the molecular mechanism of lymphocyte differentiation and apoptosis development still needs further clarification; third, the molecular mechanism of protective effect of DG needs further detection; fourth, the reaction between nonspecific immune-cytes and Con A-induced hepatic injury was not detected.
In conclusion, the potential protective effect of DG against Con A-induced hepatitis may be partially attributed to its inhibitory activity on inflammatory cytokines in the livers, lymphocytes apoptosis in the thymus, NKT cells proliferation, and activation of CD8+T cells. In addition, its promoting activity on Tregs proliferation may be involved.
Acknowledgments
This work was supported by the Capital Foundation for Clinical Characteristic Applied Research Projects [Number Z181100001718084]; the Digestive Medical Coordinated Development Center of Beijing Hospitals Authority [Number XXZ0404]; National Natural Science Foundation of China [Number 81271901]; and Beijing Natural Science Foundation [Number 7152073].
Abbreviations
AIH, autoimmune hepatitis; ALT, alanine aminotransferase; AST, aspartate aminotransferase; Con A, concanavalin A; DG, diammonium glycyrrhizinate; PBMC, peripheral blood mononuclear cell; Tregs, regulatory T cells.
Disclosure
The authors declare no conflicts of interests in this work.
References
- 1.Yuksel M, Wang Y, Tai N, et al. A novel “humanized mouse” model for autoimmune hepatitis and the association of gut microbiota with liver inflammation. Hepatology. 2015;62(5):1536–1550. doi: 10.1002/hep.27998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Boer YS, van Gerven NM, Zwiers A, et al. Genome-wide association study identifies variants associated with autoimmune hepatitis type 1. Gastroenterology. 2014;147(2):443–452. doi: 10.1053/j.gastro.2014.04.022 [DOI] [PubMed] [Google Scholar]
- 3.Kirstein MM, Seibel E, Manns MP, et al. Prediction of short- and long-term outcome in patients with autoimmune hepatitis. J Hepatol. 2015;62(5):1524–1535. doi: 10.1002/hep.27983 [DOI] [PubMed] [Google Scholar]
- 4.Wang QX, Yan L, Ma X. Autoimmune hepatitis in the Asia-Pacific area. J Clin Transl Hepatol. 2018;6(1):48–56. doi: 10.14218/JCTH.2017.00032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heneghan MA, Yeoman A, Verma S, Smith AD, Longhi MS. Autoimmune hepatitis. Lancet. 2013;382:1433–1444. doi: 10.1016/S0140-6736(12)62163-1 [DOI] [PubMed] [Google Scholar]
- 6.Ikeda A, Aoki N, Kido M, et al. Progression of autoimmune hepatitis is mediated by IL‐18‐producing dendritic cells and hepatic CXCL9 expression in mice. Hepatology. 2014;60:224–236. doi: 10.1002/hep.27087 [DOI] [PubMed] [Google Scholar]
- 7.Liberal R, Grant CR, Yuksel M, et al. Treg conditioning endows activated teff with suppressor function in autoimmune hepatitis/autoimmune sclerosing cholangitis. Hepatology. 2017;66(5):1570–1584. doi: 10.1002/hep.29307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang H, Yin S. Natural killer T cells in liver injury, inflammation and cancer. Expert Rev Gastroenterol Hepatol. 2015;9(8):1077–1085. doi: 10.1586/17474124.2015.1056738 [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharjee J, Kirby M, Softic S, et al. Hepatic natural killer T-cell and CD8+ T-cell signatures in mice with nonalcoholic steatohepatitis. Hepatol Commun. 2017;1(4):299–310. doi: 10.1002/hep4.1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolf M, Adili A, Piotrowitz K, et al. Metabolic activation of intrahepatic CD8+ T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell. 2014;26(4):549–564. doi: 10.1016/j.ccell.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 11.Zheng W, Du S, Tian M, et al. Lepidium meyenii walp exhibits anti-inflammatory activity against ConA-induced acute hepatitis. Mediators Inflamm. 2018;2018:8982756. doi: 10.1155/2018/8982756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu Y, Guo Y, Xu L, Li Y, Cao L. Foxp3 regulates ratio of Treg and NKT cells in a mouse model of asthma. Mol Cell Biochem. 2015;403(1–2):25–31. doi: 10.1007/s11010-015-2333-2 [DOI] [PubMed] [Google Scholar]
- 13.Shi HJ, Song HB, Wang L, Xiao S-X, Bo K-P, Ma W. The synergy of diammonium glycyrrhizinate remarkably reduces the toxicity of oxymatrine in ICR mice. Biomed Pharmacother. 2018;97:19–25. doi: 10.1016/j.biopha.2017.09.039 [DOI] [PubMed] [Google Scholar]
- 14.Zhu X, Chen C, Ye D, et al. Diammonium glycyrrhizinate upregulates PGC-1α and protects against Aβ1–42-induced neurotoxicity. PLoS One. 2012;7(4):e35823. doi: 10.1371/journal.pone.0035823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jin J, Xiong T, Hou X, et al. Role of Nrf2 activation and NF-κB inhibition in valproic acid induced hepatotoxicity and in diammonium glycyrrhizinate induced protection in mice. Food Chem Toxicol. 2014;73:95–104. doi: 10.1016/j.fct.2014.08.009 [DOI] [PubMed] [Google Scholar]
- 16.Orlent H, Hansen BE, Willems M, et al. Biochemical and histological effects of 26 weeks of glycyrrhizin treatment in chronic hepatitis C: a randomized phase II trial. J Hepatol. 2006;45(4):539–546. doi: 10.1016/j.jhep.2006.05.015 [DOI] [PubMed] [Google Scholar]
- 17.Wang H, Fang ZZ, Meng R, et al. Glycyrrhizin and glycyrrhetinic acid inhibits alpha-naphthyl isothiocyanate-induced liver injury and bile acid cycle disruption. Toxicology. 2017;386:133–142. doi: 10.1016/j.tox.2017.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Y W L, Hu YH, Zhu TT, Chu AZ, Zhu CL. Clinical efficacy of compound glycyrrhizin tablets in the treatment of children with nonalcoholic fatty liver disease. Zhongguo Dang Dai Er Ke Za Zhi. 2017;19(5):505–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun X, Duan X, Wang C, et al. Protective effects of glycyrrhizic acid against non-alcoholic fatty liver disease in mice. Eur J Pharmacol. 2017;806:75–82. doi: 10.1016/j.ejphar.2017.04.021 [DOI] [PubMed] [Google Scholar]
- 20.Yasui S, Fujiwara K, Tawada A, Fukuda Y, Nakano M, Yokosuka O. Efficacy of intravenous glycyrrhizin in the early stage of acute onset autoimmune hepatitis. Dig Dis Sci. 2011;56(12):3638–3647. doi: 10.1007/s10620-011-1789-5 [DOI] [PubMed] [Google Scholar]
- 21.Zhang X, Yang H, Yue S, et al. The mTOR inhibition in concurrence with ERK1/2 activation is involved in excessive autophagy induced by glycyrrhizin in hepatocellular carcinoma. Cancer Me. 2017;6(8):1941–1951. doi: 10.1002/cam4.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li H, Guo D, Zhang L, Feng X. Glycyrrhizin attenuates histamine-mediated MUC5AC upregulation, inflammatory cytokine production, and aquaporin 5 downregulation through suppressing the NF-κB pathway in human nasal epithelial cells. Chem Biol Interact. 2018;285:21–26. doi: 10.1016/j.cbi.2018.02.010 [DOI] [PubMed] [Google Scholar]
- 23.Zhao X, Liu J, Yang S, et al. Diammonium glycyrrhizinate alleviates hepatopulmonary syndrome, via, restoring superoxide dismutase 3 activity in rats. Eur J Pharmacol. 2017;807:144–150. doi: 10.1016/j.ejphar.2017.04.025 [DOI] [PubMed] [Google Scholar]
- 24.Lei W, Huihui D, Yibo L, et al. Chinese medicine Bu Xu Hua Yu recipe for the regulation of Treg/Th17 ratio imbalance in autoimmune hepatitis. Evid Based Complement Alternat Med. 2015;2015(3):1–14. doi: 10.1155/2015/459749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taubert R, Hardtke-Wolenski M, Noyan F, et al. Intrahepatic regulatory T cells in autoimmune hepatitis are associated with treatment response and depleted with current therapies. J Hepatol. 2014;61(5):1106–1114. doi: 10.1016/j.jhep.2014.05.034 [DOI] [PubMed] [Google Scholar]
- 26.González-Amaro R, Cortés JR, Sánchez-Madrid F, Martín P. Is CD69 an effective brake to control inflammatory diseases? Trends Mol Med. 2013;19(10):625–632. doi: 10.1016/j.molmed.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knodell RG, Ishak KG, Black WC, et al. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981;1(5):431–435. doi: 10.1002/hep.1840010511 [DOI] [PubMed] [Google Scholar]
- 28.Park J, Kim H, Lee IS. The therapeutic effects of Yongdamsagan-tang on autoimmune hepatitis models. Biomed Pharmacother. 2017;94:244–255. doi: 10.1016/j.biopha.2017.07.015 [DOI] [PubMed] [Google Scholar]
- 29.W W L, J Y Y, H L X, Bao J-K. Concanavalin A: a potential anti-neoplastic agent targeting apoptosis, autophagy and anti-angiogenesis for cancer therapeutics. Biochem Biophys Res Commun. 2011;414(2):282–286. doi: 10.1016/j.bbrc.2011.09.072 [DOI] [PubMed] [Google Scholar]
- 30.Burger ML, Leung KK, Bennett MJ, Winoto A. T cell-specific inhibition of multiple apoptotic pathways blocks negative selection and causes autoimmunity. ELife. 2014;3(3):e03468. doi: 10.7554/eLife.03468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cortés JR, Sánchez-Díaz R, Bovolenta ER, et al. Maintenance of immune tolerance by Foxp3+ regulatory T cells requires CD69 expression. J Autoimmun. 2014;55(1):51–62. doi: 10.1016/j.jaut.2014.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.García-Monzón C, Moreno-Otero R, Pajares JM, et al. Expression of a novel T cell activation antigen on intrahepatic CD8+ T lymphocytes in viral chronic active hepatitis. Gastroenterology. 1990;98(4):1029–1035. doi: 10.1016/0016-5085(90)90030-5 [DOI] [PubMed] [Google Scholar]
- 33.Hilda A, Roy-O’Reilly M, Spychala MS, et al. Sex differences in adipose tissue cd8+ t cells and regulatory t cells in middle-aged mice. Front Immunol. 2018;9:659. doi: 10.3389/fimmu.2018.00659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murata K, Inami M, Hasegawa A, et al. CD69‐null mice protected from arthritis induced with anti‐type II collagen antibodies. Int Immunol. 2003;15(8):987–992. doi: 10.1093/intimm/dxg008 [DOI] [PubMed] [Google Scholar]
- 35.Miki-Hosokawa T, Hasegawa A, Iwamura C, et al. CD69 controls the pathogenesis of allergic airway inflammation. J Immunol. 2009;183(12):8203–8215. doi: 10.4049/jimmunol.0900838 [DOI] [PubMed] [Google Scholar]
- 36.Han Y, Guo Q, Zhang M, Chen Z, Cao X. CD69+ CD4+ CD25− T cells, a new subset of regulatory T cells, suppress T cell proliferation through membrane-bound TGF-β1. J Immunol. 2009;182(1):111–120. doi: 10.4049/jimmunol.182.1.111 [DOI] [PubMed] [Google Scholar]
- 37.Zhao XS, Wang XH, Zhao XY, et al. Non-traditional CD4+ CD25− CD69+ regulatory T cells are correlated to leukemia relapse after allogeneic hematopoietic stem cell transplantation. J Transl Med. 2014;12(1):187. doi: 10.1186/1479-5876-12-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grage-Griebenow E, Jerg E, Gorys A, et al. L1CAM promotes enrichment of immunosuppressive T cells in human pancreatic cancer correlating with malignant progression. Mol Oncol. 2014;8(5):982–997. doi: 10.1016/j.molonc.2014.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao XY, Wang YT, Mo XD, et al. Higher frequency of regulatory T cells in granulocyte colony-stimulating factor (G-CSF)-primed bone marrow grafts compared with G-CSF-primed peripheral blood grafts. J Transl Med. 2015;13(1):145. doi: 10.1186/s12967-015-0541-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kumar V. NKT-cell subsets: promoters and protectors in inflammatory liver disease. J Hepatol. 2013;59(3):618–620. doi: 10.1016/j.jhep.2013.02.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kahraman A, Barreyro FJ, Bronk SF, et al. TRAIL mediates liver injury by the innate immune system in the bile duct–ligated mouse. Hepatology. 2008;47(4):1317–1330. doi: 10.1002/hep.22136 [DOI] [PMC free article] [PubMed] [Google Scholar]