Abstract
Background: Parental educational attainment is shown to be protective against health problems; the Minorities’ Diminished Returns theory, however, posits that these protective effects tend to be smaller for socially marginalized groups particularly blacks than whites. Aims: To explore racial differences in the effect of parental educational attainment on body mass index (BMI) in a national sample of US adolescents. Methods: In this cross-sectional study, we used baseline data of 10,701 (8678 white and 2023 black) 12–17 years old adolescents in the Population Assessment of Tobacco and Health (PATH; 2013). Parental educational attainment was the predictor. Youth BMI (based on self-reported weight and height) was the dependent variable. Age, gender, ethnicity, and family structure were covariates. Race was the focal moderator. Results: Overall, higher parental educational attainment was associated with lower youth BMI. Race, however, moderated the effect of parental educational attainment on BMI, suggesting that the protective effect of parental educational attainment on BMI is significantly smaller for black than white youth. Conclusions: In the United States, race alters the health gains that are expected to follow parental educational attainment. While white youth who are from highly educated families are fit, black youth have high BMI at all levels of parental educational attainment. This means, while the most socially privileged group, whites, gain the most health from their parental education, blacks, the least privileged group, gain the least. Economic, social, public, and health policymakers should be aware that health disparities are not all due to lower socioeconomic status (SES) of the disadvantaged group but also diminished returns of SES resources for them. Black–white health disparities exist across all high socioeconomic status (SES) levels.
Keywords: population groups, race, whites, blacks, African-Americans, socioeconomic position, socioeconomic status, education, obesity, body mass index (BMI)
1. Background
Body Mass Index (BMI) is now universally considered a marker of health [1,2]. High BMI is a predictor of premature mortality in the general population [3,4,5] and individuals with a chronic medical condition (CMC) [6].
Compared to white youth, black youth have higher BMI in the US [7,8,9]. Epidemiological studies have shown that education [9] and race [10,11] are independent predictors of BMI [9]. High BMI may mediate some of the inequalities and disparities in health [12,13,14,15,16,17,18,19,20,21,22,23]. Finally, race, ethnicity, and economic factors have some separate, additive, or multiplicative effects [9]. Educational attainment is one of the main predictors of BMI [9].
Similarly, black youth have a higher risk of overweight and obesity compared to their white counterparts [24,25,26]. Disparities in BMI are among the main contributors to racial health disparities in other health domains including but not limited to chronic disease and mortality [27,28]. Inequality in BMI in youth is also a gateway to the very persistent disparities in the burden of obesity seen in adults [7]. Thus, there is a need to understand the socioeconomic factors that explain racial differences in BMI [29], particularly those between black and white youth [30].
Given the protective effect of high socioeconomic status (SES) against high BMI in youth [31,32,33], adults [34,35], and older adults [36,37], SES is one of the best candidates as an explanatory factor for explaining the BMI differences between blacks and whites [30]. This is particularly relevant given the literature that has linked low SES to higher BMI among black youth [32,38,39,40]. Among various SES indicators, parental educational attainment seems to be one of the main protective factors against high BMI and obesity [41,42,43].
Minorities’ Diminished Returns (MDRs) [44,45] proposes that at least some of the racial/ethnic disparities in BMI are due to less than expected protective effects of SES on BMI for the black community [32,39,46]. This suggests: (a) Racial disparities in obesity and high BMI are not all due to SES gaps across racial groups but also because of the differential health gains that follow SES resources such as parental education for black populations, and (b) the relative racial gap in obesity and BMI widens as SES increases [32,39,46], which emphasizes a need to study and address racial disparities in obesity across all SES levels, not just among low SES groups [44,45].
In a cross-sectional study that used data from the National Survey of Children’s Health (NSCH, 2003–2004), 67,610 white and 9095 black children of 2–17 years old were compared for the effect of parental income on childhood obesity. This study showed that family income reduces the odds of obesity for white but not black children [32]. In a 1-year follow up study of urban families, race by gender groups were compared to the effects of parental educational attainment at birth on future BMI at age 15. In this study, the most consistent protective effects of parental education were found for the effects of family SES against high future BMI for white girls, followed by white boys. No association was found for maternal education, family structure, and family income at birth and future youth BMI at age 15 for black boys or girls. However, this study did not use a nationally representative sample, thus the results could not be generalized to the US population [46]. Thus, despite the existing evidence that suggests MDRs may apply to racial differences in BMI of youth, there is still a need to test this hypothesis in nationally representative data sets that generate representative results.
We conducted this study to test whether race shows an interaction with parental educational attainment on youth BMI in the US. In line with the MDRs literature [32,39,46], we hypothesized that the protective effect of parental educational attainment would be significantly smaller for black than white youth. Conceptualizing race as a social rather than a biological factor, we argue that MDRs are not because of groups’ or individuals’ inherent differences in their ability to translate their resources but the differential treatment of the society that is associated with marginalization and stigmatization of blacks [44,45]. As a result of unequal life circumstances, we expect to observe MDRs for the effects of parental educational attainment on BMI in blacks than whites.
2. Methods
2.1. Design and Settings
This is a secondary analysis of wave 1 of the Population Assessment of Tobacco and Health (PATH) youth data. Funded by the NIH and FDA, PATH is a state-of-the-art study on health problems such as tobacco use, substance use, and related behavioral issues among US adolescents and adults. Overall, PATH has enrolled 53,178 individuals who were 12 years or older at baseline. From this sample, 13,650 were youth (12–17 years old). Wave 1 data were collected between 2013 and 2014. Although PATH has also recruited adults, this analysis is only focused on youth. We were interested in the association between SES and BMI rather than a change in BMI, we limited our analysis to cross-sectional data (Wave 1) of the PATH study. We used the publicly available PATH data set.
2.2. Sample and Sampling
The PATH study’s population of interest in Wave 1 was the civilian, non-institutionalized US population of 12–17 years old individuals in the US. The PATH study used a four-stage stratified area probability sample design. Stage one was the selection of a stratified sample of geographical primary sampling units (156 PSUs). These PSUs were either a county or a group of counties. Stage two formed and sampled smaller geographical segments in each PSU. Stage three sampled residential addresses, using the US Postal Service Computerized Delivery Sequence Files. The fourth stage was the selection of one person from each sampled household.
2.3. Analytical Sample
The current analysis is limited to youth who had complete data on age, gender, parental education, race, ethnicity, and BMI. Our final analytical sample was 10,701 (8678 white and 2023 black) adolescents. For the purpose of this study, the sample was specifically restricted to white and black respondents. (i.e., Asians and people of other races were excluded).
2.4. Study Variables
The study variables include age, gender, race, ethnicity, parental educational attainment, marital status of the parents (family structure), and BMI.
2.4.1. Demographic Factors
Age was a dichotomous variable as below: (1) 12 to 15 years old, and (2) 16 to 17 years old. Public PATH data set does not provide more granular data on age.
2.4.2. Race and Ethnicity
Race was self-identified and operationalized as a dichotomous variable: blacks versus whites. Ethnicity was also self-identified and operationalized as a dichotomous variable: Non-Hispanic versus Hispanic.
2.4.3. Socioeconomic Status
Parental educational attainment was a five-level variable as below: (1) less than high school, (2) high school graduate or equivalent, (3) some college including no degree or an associate degree, (4) Bachelor’s degree, and (5) advanced degree. This was a continuous measure ranging between 1 and 5.
2.4.4. Body Mass Index (BMI)
The study calculated the BMI using participants’ height and weight. First, height and weight were recorded in feet/inches and pounds, respectively. In the second step, height and weight were calculated in meters and kilograms. BMI was calculated by dividing weight (kilograms) by height squared (meters squared).
2.5. Conceptual Model
Built on the MDRs, our study is mainly focused on the interaction between race and parental educational attainment (SES). As a result, the main predictor of interest is parental educational attainment. The outcome of interest is BMI. The moderating variable is race. We expect high parental educational attainment to be associated with lower BMI in the overall sample, however, we expect this effect to be weaker in black compared to white youth. We call weaker effects of SES indicators in the non-white group as diminished returns of SES.
2.6. Data Analytical Plan
We analyzed the data using SPSS 23.0 (IBM Corporation, Armonk, NY, USA). We applied survey design weights. SPSS uses a Taylor series linearization to re-estimate standard errors (SE) of the survey data. For bivariate analysis, we tested the bivariate correlations between our study variable using the Pearson correlation test. No two variables had correlation coefficients equal or larger than 0.50 so we ruled out any collinearity between our independent variables. This strategy was taken for the full sample and also racial groups.
For multivariable analysis, we applied linear regression models. Overall, we ran four models. We ran the first two models in the pooled sample. Then we ran two additional models across racial groups. Model 1 did not have the interaction term. Model 2 included the interaction term. Model 3 was specific to white youth. Model 4 was specific to black youth. From our models, we reported regression coefficient (b), Standard Error (SE), 95% Confidence Interval (CI), and p-value. We did not impute data. Complete data cases were entered into our analysis.
We tested the assumptions and requirements for linear regression models. This includes ruling out the multicollinearity between the independent variables. We also confirmed the near to normal distribution of error terms of our linear regression models.
We did not control for income for methodological and conceptual reasons. Some evidence suggests that income may be the reason educational attainment does not generate the very same health across racial and ethnic groups [47,48]. Thus, controlling income would be adjusting for the mediator, which introduces bias due to controlling for the intermediate variable [49]. Other evidence suggests that MDRs are more relevant to educational attainment than income because less societal processes interfere with families’ abilities to use their income, compared societal barriers [47]. Thus, some evidence suggests that MDRs are most relevant to the distal (e.g., educational attainment) than proximal (e.g., income) SES indicators [47,50].
2.7. Ethics
All youth who participated in the PATH study provided assent. All their parents/guardians/caregivers provided written informed consent. The PATH study protocol was approved by the Westat institutional review board.
3. Results
3.1. Descriptive Statistics
This study included 10,701 US adolescents who were either white (n = 8,678, 81.1%) or black (n = 2023, 19.9%).
Table 1 shows descriptive statistics of the complete sample by race. White youth were more likely to be of Hispanic ethnicity (25% vs. 9.9%, p <0.01), have parents with higher educational attainment (2.89 vs. 2.62, p <0.01), and married parents (69.6% vs. 38.9%, p <0.01). We did not find significant differences in age and gender between white and black youth. On average, black youth had higher BMI than white youth (23.30 vs. 22.36, p < 0.01) (Table 1).
Table 1.
Descriptive statistics in the complete sample and by race.
| Characteristics | All | Whites | Blacks | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Ethnicity *,a | ||||||
| Non-Hispanic | 8179 | 77.8 | 6407 | 75.0 | 1772 | 90.1 |
| Hispanic | 2329 | 22.2 | 2135 | 25.0 | 194 | 9.9 |
| Age | ||||||
| 12–15 | 5474 | 51.2 | 4437 | 51.1 | 1037 | 51.3 |
| 16–18 | 5227 | 48.8 | 4241 | 48.9 | 986 | 48.7 |
| Gender | ||||||
| Women | 5143 | 48.2 | 4180 | 48.3 | 963 | 47.9 |
| Men | 5531 | 51.8 | 4483 | 51.7 | 1048 | 52.1 |
| Marital Status *,a | ||||||
| Not Married | 3870 | 36.2 | 2635 | 30.4 | 1235 | 61.1 |
| Married | 6817 | 63.8 | 6030 | 69.6 | 787 | 38.9 |
| Mean | SD | Mean | SD | Mean | SD | |
| Parental educational attainment (1–5) *,b | 2.84 | 1.22 | 2.89 | 1.23 | 2.62 | 1.16 |
| Body Mass Index (BMI) *,b | 22.53 | 5.25 | 22.36 | 5.06 | 23.30 | 5.92 |
* p < 0.01, a Chi square test for comparison of black and white youth. b Independent samples t-test for comparison of means between black and white youth.
3.2. Multivariable Models in the Pooled Sample
Table 2 presents the summary of the results of two linear regression models with parental educational attainment as the independent variable and BMI as the dependent variable. Both models were estimated in the complete sample. Model 1 was the non-interactive model that entered the main effects of educational attainment and race in addition to the covariates. Model 2 also added an interaction term between race and educational attainment. Covariates were the same in these two models.
Table 2.
Summary of linear regressions on body mass index (BMI) in the pooled sample.
| b | SE | 95% CI | p | |
|---|---|---|---|---|
| Model 1 (All, Non-interactive Model) | ||||
| Race (Blacks) | 0.84 | 0.13 | 0.58–1.10 | <0.001 |
| Parental Educational Attainment (1–5) | −0.45 | 0.04 | −0.54–−0.37 | <0.001 |
| Ethnicity (Hispanics) | 0.64 | 0.13 | 0.39–0.89 | <0.001 |
| Parents Married | −0.36 | 0.11 | −0.57–−0.15 | 0.001 |
| Gender (Boys) | 0.00 | 0.10 | −0.19–0.20 | 0.987 |
| Age (16–18 Years Old) | 1.79 | 0.10 | 1.60–1.99 | <0.001 |
| Constant | 22.88 | 0.17 | 22.54–23.23 | <0.001 |
| Model 1 (All, Interactive Model) | ||||
| Race (Blacks) | −0.65 | 0.33 | −1.29–−0.01 | 0.046 |
| Parental Educational Attainment (1–5) | −0.55 | 0.05 | −0.65–−0.46 | <0.001 |
| Race (Black) × Parental educational attainment | 0.55 | 0.11 | 0.34–0.77 | <0.001 |
| Ethnicity (Hispanics) | 0.57 | 0.13 | 0.32–0.82 | <0.001 |
| Parents Married | −0.36 | 0.11 | −0.57–−0.14 | 0.001 |
| Gender (Boys) | 0.00 | 0.10 | −0.19–0.20 | 0.979 |
| Age (16–18 Years Old) | 1.78 | 0.10 | 1.59–1.98 | <0.001 |
| Constant | 23.20 | 0.18 | 22.83–23.56 | <0.001 |
B: Regression Coefficient CI: Confidence Interval; SE: Standard Error.
Based on Model 1, high educational attainment was associated with lower BMI. In this model, being black was also associated with higher BMI. Model 2 revealed an interaction between race and parental educational attainment on BMI, suggesting that high parental educational attainment has a smaller protective effect on BMI for black than white youth. This was evident by a regression coefficient which was negative for the main effect of parental educational attainment (Model 1) and a regression coefficient which was positive for the interaction term between race and parental educational attainment (Model 2) (Table 2).
3.3. Multivariable Models by Race
Table 3 presents the results of two linear regression models with educational attainment as the independent variable and BMI as the dependent variable. These models were set up similarly, and each one was run in one racial group. Model 3 and Model 4 were estimated in whites and blacks, respectively.
Table 3.
Summary of linear regression models on body mass index (BMI) by race.
| b | SE | 95% CI | p | |
|---|---|---|---|---|
| Model 3 (Whites) | ||||
| Parental Educational Attainment (1–5) | −0.54 | 0.05 | −0.64–−0.45 | <0.001 |
| Ethnicity (Hispanics) | 0.62 | 0.13 | 0.37–0.88 | <0.001 |
| Parents Married | −0.41 | 0.12 | −0.64–−0.18 | 0.001 |
| Gender (Boys) | 0.16 | 0.11 | −0.05–0.37 | 0.139 |
| Age (16-18 Years Old) | 1.82 | 0.11 | 1.61–2.03 | <0.001 |
| Constant | 23.09 | 0.19 | 22.73–23.46 | <0.001 |
| Model 4 (Blacks) | ||||
| Parental Educational Attainment (1–5) | −0.02 | 0.11 | −0.24–0.21 | 0.869 |
| Ethnicity (Hispanics) | 0.11 | 0.45 | −0.76–0.99 | 0.804 |
| Parents Married | −0.17 | 0.27 | −0.71–0.36 | 0.529 |
| Gender (Boys) | −0.67 | 0.26 | −1.18–−0.15 | 0.012 |
| Age (16-18 Years Old) | 1.64 | 0.26 | 1.12–2.16 | <0.001 |
| Constant | 22.98 | 0.39 | 22.22–23.74 | <0.001 |
B: Regression Coefficient CI: Confidence Interval; SE: Standard Error.
Based on Model 3, high educational attainment was associated with lower BMI in whites. Model 4, however, did not show the same pattern of association for blacks. That is, high educational attainment showed a statistically significant protective effect on BMI for whites but not blacks (Table 3).
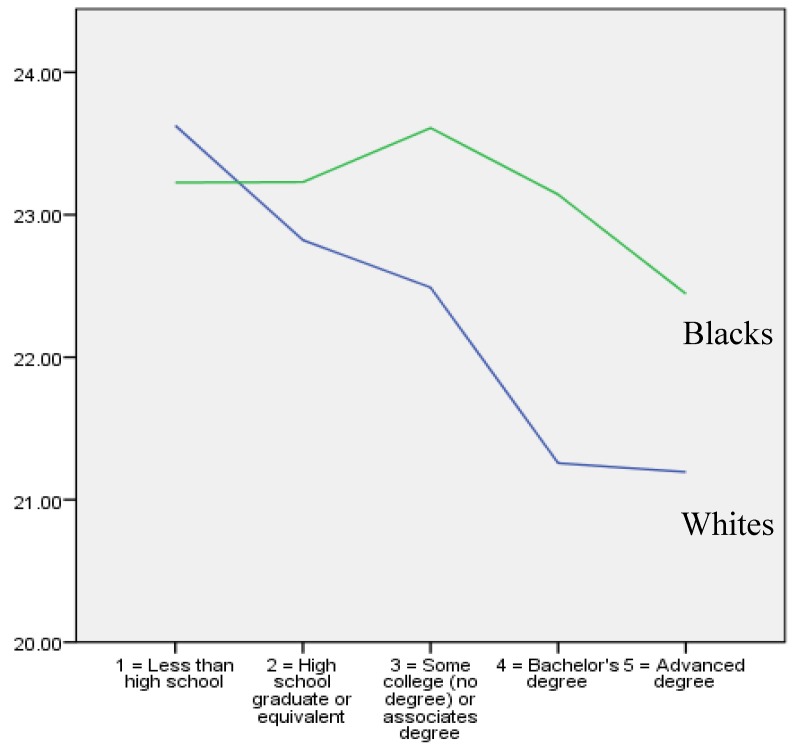
Figure 1 shows the bivariate correlation between parental educational attainment (X-axis) and BMI (Y-axis) in white and black youth. As this figure shows, there was a negative (inverse) correlation between parental educational attainment and BMI in white but not black youth.
Figure 1.
Average youth body mass index (BMI) based on parental educational attainment in whites (Blue line) and blacks (Green line).
4. Discussion
The current study showed two main findings. First, overall, higher parental educational attainment was associated with lower BMI in US youth. Second, race showed a significant interaction with parental educational attainment suggesting that high parental educational attainment has a smaller protective effect against high BMI for black than white youth. In fact, the association was only significant for whites but not blacks.
Our first finding, the inverse association between family SES and youth BMI, is in line with the extensive literature on fundamental causes [51,52,53] and social determinants of health (SDOH) [54,55,56]. A large body of research has shown that parental educational attainment is associated with better health and well-being [41,57,58,59] and lower risk of obesity [60].
Our previous work on MDRs shows black youth from high SES remain at an increased risk of high BMI compared to high SES whites [32,39,46], a pattern which is seen for a wide range of SES indicators, health outcomes, youth, adults, and older adults [61,62,63,64]. Similar patterns are reported for educational attainment [39,46], income [32,65], employment [66], and marital status [67] on obesity [39,46], depression [65], anxiety [67], self-rated health [68,69], chronic disease [70], and even mortality [66]. In several papers, smaller effects are shown for blacks than whites [32,39,46].
MDRs may be due to social stratification that operates through biological mechanisms such as those involved in responding to stress (e.g., allostatic load, weathering, metabolic syndrome) [71]. There is, however, a need for further studies to understand the role of biological and physiological pathways that may explain MDRs on BMI [72,73,74,75,76,77,78,79].
We need to better understand the role of unsafe environment [80], food deserts [81,82,83,84], density of fast food restaurants [85,86,87,88], and availability of healthy food options [89] across locations based on the intersection of race and SES. Educational attainment has smaller effects to increase blacks’ employment and enhance their living conditions, compared to whites [57,58,90,91]. For example, a larger proportion of blacks with high educational attainment remain under poverty [90]. We argue that residential segregation, racism, labor market discrimination, and limited resources in predominantly black schools all contribute to MDRs of educational attainment on BMI [46].
We see race as a political and social rather than a biological construct [92]. Social stratification by race is shaped by history, politics, and laws [93,94]. Through political power, race is a strong proxy of access to the societal resources and opportunities [92]. For example, marginalization of black men, through mass incarceration and the war on drugs, has had a strong political impact in who gets elected, and who writes the laws [92]. Political power is a major determinant of health disparities [92,93,95,96]. Social and public policies, traditionally written by policymakers and politicians, have maintained structural inequalities in the United States. Reducing racial stratification needs considerable political will. Policymakers should target the very structural context of the U.S. if we want to eliminate health inequalities [92,93,95,96]. Today’s highly polarized political environment, however, is a major barrier against reaching a bipartisan agreement on policies that are needed to solve the structural health inequalities. Unfortunately, good-faith policy intentions have failed to effectively address health disparities. This is in part because of the differential effect of resources on health without addressing structural forces [92,93,95,96].
4.1. Implications
The results may have some implications for public, economic, social, and health policies. First, we argue that policymakers should not assume that SES indicators are equally protective against health problems including high BMI for various racial groups. As new policies are being implemented, there is a need for “impact analysis” to track effects on the population overall, as well as sub-population differences in such effects. Given the limited benefit of high SES on BMI among black youths, providing incentives for health in predominantly black areas may be required. An enhancement to the quality of education and schooling in predominantly black areas are also needed. We need programs that enable black communities, with the translation of educational attainment, to obtain tangible health outcomes. Finally, the elimination of racism and segregation is needed if we want to help black families be able to turn their educational attainment to health outcomes. Societal interventions, through public policies, would probably be more effective than individual-level interventions that overemphasize individual choices and preferences and ignore social stratification [97].
National and local policies are needed to reduce the racial/ethnic and SES disparities in BMI, including those that are due to MDRs [45,46,50,62,63,64,67,68,98,99]. Additional investment is needed in reducing the societal risk factors of obesity in urban black communities. There is a need to increase the availability of healthy food, walkable spaces, green spaces and parks, and other societal resources that can help black families and youth to avoid obesity. To undo racial and ethnic disparities in obesity and related morbidity, structural changes are needed that equalize environmental opportunities for maintaining healthy BMI.
4.2. Future Research
There is also a need to conduct further studies that help us understand, based on race, why some youth with highly educated parents remain susceptible to obesity and high BMI. Research should assess how the density of healthy and unhealthy food, the walkability of living areas, availability of green spaces and parks, and other structural determinants of obesity, mediate or moderate the MDRs observed in this study. There is also a need to test the efficacy of various policies in reducing MDR-related disparities in health.
4.3. Limitations
This study had some methodological and conceptual limitations. First, given the cross-sectional design of our data, causal inferences are not plausible. The sample size was imbalanced across racial groups, which is a common pattern in national surveys. In addition, we did not have access to a wide range of other SES indicators of the household such as income, employment, and occupation type. Finally, this study used an over-simplistic measure of BMI. Several other indicators such as waist to hip ratio, sub-cutaneous adiposity, and other indicators need to be studied. The results should be interpreted with knowing that we did not compare non-Hispanic white and non-Hispanic blacks but all groups of whites and blacks. However, our robustness analysis did not show any difference in the interaction term when we limited the sample to non-Hispanic whites and blacks. Finally, we did not include area-level SES indicators. Despite these limitations, we believe that this study extends the existing literature on race, SES, and BMI. We had previously shown similar findings in the Fragile Families and Child Well-being Study (FFCWS) data. However, FFCWS was a non-representative study composed of economically at-risk families who were only selected from large cities. The results of the current study, however, are generalizable to the US youth sample, given the nationally representative nature of the sample.
5. Conclusions
In the United States, racial minority status limits the health gains that follow parental educational attainment. While high parental educational attainment helps people stay healthy and avoid high risk behaviors such as smoking, the most privileged group gains the most and the least privileged groups gain the least from such potential. As a result, we should expect an additional risk of high BMI and obesity in middle-class blacks. Researchers should not take a minimalistic and over-simplistic approach by focusing on health disparities among blacks of low SES. They should consider that health inequalities and disparities can be observed across all SES levels, and the SES gap is only a part of the story. Given that health disparities are also faced by middle-class blacks, health disparity solutions should focus on other sections of black communities, that may not be low SES but still have increased risk of poor health outcomes. Policymakers should also go beyond equalizing SES and address the barriers that are more common in the lives of blacks and hinder their ability to turn their available resources into tangible health outcomes.
Acknowledgments
The publicly available PATH data were used for this study.
Author Contributions
S.A. conceptualized the study, analyzed the data, and prepared the first draft of the paper. All other authors contributed to the conceptualization and revision of the paper. All authors approved the final draft.
Funding
Assari is supported by the following NIH grants: U54MD008149, U54MD007598, U54 TR001627, R25 MD007610, and U54CA229974. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Patel A.V., Hildebrand J.S., Gapstur S.M. Body mass index and all-cause mortality in a large prospective cohort of white and black U.S. Adults. PLoS ONE. 2014;9:e109153. doi: 10.1371/journal.pone.0109153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanchez A.M., Reed D.R., Price R.A. Reduced mortality associated with body mass index (BMI) in African Americans relative to Caucasians. Ethn. Dis. 2000;10:24–30. [PubMed] [Google Scholar]
- 3.Berrington de Gonzalez A., Hartge P., Cerhan J.R., Flint A.J., Hannan L., MacInnis R.J., Moore S.C., Tobias G.S., Anton-Culver H., Freeman L.B., et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 2010;363:2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tobias D.K., Pan A., Jackson C.L., O’Reilly E.J., Ding E.L., Willett W.C., Manson J.E., Hu F.B. Body-mass index and mortality among adults with incident type 2 diabetes. N. Engl. J. Med. 2014;370:233–244. doi: 10.1056/NEJMoa1304501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calle E.E., Thun M.J., Petrelli J.M., Rodriguez C., Heath C.W., Jr. Body-mass index and mortality in a prospective cohort of U.S. adults. N. Engl. J. Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 6.Kwon Y., Kim H.J., Park S., Park Y.G., Cho K.H. Body Mass Index-Related Mortality in Patients with Type 2 Diabetes and Heterogeneity in Obesity Paradox Studies: A Dose-Response Meta-Analysis. PLoS ONE. 2017;12:e0168247. doi: 10.1371/journal.pone.0168247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albrecht S.S., Gordon-Larsen P. Ethnic differences in body mass index trajectories from adolescence to adulthood: A focus on Hispanic and Asian subgroups in the United States. PLoS ONE. 2013;8:e72983. doi: 10.1371/journal.pone.0072983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Messiah S.E., Arheart K.L., Lopez-Mitnik G., Lipshultz S.E., Miller T.L. Ethnic group differences in cardiometabolic disease risk factors independent of body mass index among American youth. Obesity (Silver Spring) 2013;21:424–428. doi: 10.1002/oby.20343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanchez-Vaznaugh E.V., Kawachi I., Subramanian S.V., Sanchez B.N., Acevedo-Garcia D. Differential effect of birthplace and length of residence on body mass index (BMI) by education, gender and race/ethnicity. Soc. Sci. Med. 2008;67:1300–1310. doi: 10.1016/j.socscimed.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 10.Guerrero A.D., Mao C., Fuller B., Bridges M., Franke T., Kuo A.A. Racial and Ethnic Disparities in Early Childhood Obesity: Growth Trajectories in Body Mass Index. J. Racial Ethn. Health Disparities. 2016;3:129–137. doi: 10.1007/s40615-015-0122-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zilanawala A., Davis-Kean P., Nazroo J., Sacker A., Simonton S., Kelly Y. Race/ethnic disparities in early childhood BMI, obesity and overweight in the United Kingdom and United States. Int. J. Obes. (Lond.) 2015;39:520–529. doi: 10.1038/ijo.2014.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dai Z., Jafarzadeh S.R., Niu J., Felson D.T., Jacques P.F., Li S., Zhang Y. Body Mass Index Mediates the Association between Dietary Fiber and Symptomatic Knee Osteoarthritis in the Osteoarthritis Initiative and the Framingham Osteoarthritis Study. J. Nutr. 2018;148:1961–1967. doi: 10.1093/jn/nxy231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fayanju O.M., Hall C.S., Bauldry J.B., Karhade M., Valad L.M., Kuerer H.M., DeSnyder S.M., Barcenas C.H., Lucci A. Body mass index mediates the prognostic significance of circulating tumor cells in inflammatory breast cancer. Am. J. Surg. 2017;214:666–671. doi: 10.1016/j.amjsurg.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duchesne A., Liu A., Jones S.L., Laplante D.P., King S. Childhood body mass index at 5.5 years mediates the effect of prenatal maternal stress on daughters’ age at menarche: Project Ice Storm—ERRATUM. J. Dev. Orig. Health Dis. 2017;8:382. doi: 10.1017/S2040174417000022. [DOI] [PubMed] [Google Scholar]
- 15.Llewellyn A., Simmonds M., Owen C.G., Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016;17:56–67. doi: 10.1111/obr.12316. [DOI] [PubMed] [Google Scholar]
- 16.Assari S., Lankarani M.M. Mediating Effect of Perceived Overweight on the Association between Actual Obesity and Intention for Weight Control; Role of Race, Ethnicity, and Gender. Int. J. Prev. Med. 2015;6:102. doi: 10.4103/2008-7802.167616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tandon P., Thompson S., Moran L., Lengua L. Body Mass Index Mediates the Effects of Low Income on Preschool Children’s Executive Control, with Implications for Behavior and Academics. Child. Obes. 2015;11:569–576. doi: 10.1089/chi.2014.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mackenbach J.D., Lakerveld J., van Oostveen Y., Compernolle S., De Bourdeaudhuij I., Bardos H., Rutter H., Glonti K., Oppert J.M., Charreire H., et al. The mediating role of social capital in the association between neighbourhood income inequality and body mass index. Eur. J. Public Health. 2017;27:218–223. doi: 10.1093/eurpub/ckw157. [DOI] [PubMed] [Google Scholar]
- 19.Leung C.Y., Miller A.L., Kaciroti N.A., Chen Y.P., Rosenblum K., Lumeng J.C. Low-income pre-schoolers with higher temperamental surgency enjoy and respond more to food, mediating the path to higher body mass index. Pediatr. Obes. 2016;11:181–186. doi: 10.1111/ijpo.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luo X., Wang Y., Wang Z., Cai F., Xie B., Qu S., Liu M. The mediating effect of body mass index on the relationship between cigarette smoking and atopic sensitization in Chinese adults. Int. J. Environ. Res. Public Health. 2015;12:3381–3394. doi: 10.3390/ijerph120303381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boo S. Body mass index and weight loss in overweight and obese korean women: The mediating role of body weight perception. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2013;7:191–197. doi: 10.1016/j.anr.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Caperchione C.M., Duncan M.J., Mummery K., Steele R., Schofield G. Mediating relationship between body mass index and the direct measures of the Theory of Planned Behaviour on physical activity intention. Psychol. Health Med. 2008;13:168–179. doi: 10.1080/13548500701426737. [DOI] [PubMed] [Google Scholar]
- 23.Hanson M.D., Chen E. Socioeconomic status, race, and body mass index: The mediating role of physical activity and sedentary behaviors during adolescence. J. Pediatr. Psychol. 2007;32:250–259. doi: 10.1093/jpepsy/jsl024. [DOI] [PubMed] [Google Scholar]
- 24.An R. Racial/ethnic disparity in obesity among US youth, 1999–2013. Int. J. Adolesc. Med. Health. 2015 doi: 10.1515/ijamh-2015-0068. [DOI] [PubMed] [Google Scholar]
- 25.Claire Wang Y., Gortmaker S.L., Taveras E.M. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976–2006. Int. J. Pediatr. Obes. 2011;6:12–20. doi: 10.3109/17477161003587774. [DOI] [PubMed] [Google Scholar]
- 26.Harding S., Teyhan A., Maynard M.J., Cruickshank J.K. Ethnic differences in overweight and obesity in early adolescence in the MRC DASH study: The role of adolescent and parental lifestyle. Int. J. Epidemiol. 2008;37:162–172. doi: 10.1093/ije/dym252. [DOI] [PubMed] [Google Scholar]
- 27.Kumanyika S. Obesity, health disparities, and prevention paradigms: Hard questions and hard choices. Prev. Chronic Dis. 2005;2:A02. [PMC free article] [PubMed] [Google Scholar]
- 28.Jensen M.D., Ryan D.H., Apovian C.M., Ard J.D., Comuzzie A.G., Donato K.A., Hu F.B., Hubbard V.S., Jakicic J.M., Kushner R.F., et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 29.Robert S.A., Reither E.N. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc. Sci. Med. 2004;59:2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 30.Sanchez-Vaznaugh E.V., Kawachi I., Subramanian S.V., Sanchez B.N., Acevedo-Garcia D. Do socioeconomic gradients in body mass index vary by race/ethnicity, gender, and birthplace? Am. J. Epidemiol. 2009;169:1102–1112. doi: 10.1093/aje/kwp027. [DOI] [PubMed] [Google Scholar]
- 31.Ni Y.L., Chang J.H., Chen L.H. Investigating the relationship between district-level socioeconomic status and individual obesity in Taiwanese adolescents: A large-scale cross-sectional analysis. Sci. Rep. 2019;9:2928. doi: 10.1038/s41598-019-39167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Assari S. Family Income Reduces Risk of Obesity for White but Not Black Children. Children (Basel) 2018;5:73. doi: 10.3390/children5060073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rey-Lopez J.P., Hashem R., Hamer M., Mc M.A., Whincup P.H., Owen C.G., Stamatakis E. Prevalence of overweight and obesity among Kuwaiti adolescents and associations with socioeconomic indicators: The study of health and activity among adolescents in Kuwait. Minerva Pediatr. 2019;71:326–332. doi: 10.23736/S0026-4946.18.04911-3. [DOI] [PubMed] [Google Scholar]
- 34.Hwang J., Lee E.Y., Lee C.G. Measuring Socioeconomic Inequalities in Obesity among Korean Adults, 1998–2015. Int. J. Environ. Res. Public Health. 2019;16:1617. doi: 10.3390/ijerph16091617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wagner K.J.P., Bastos J.L.D., Navarro A., Gonzalez-Chica D.A., Boing A.F. Socioeconomic status in childhood and obesity in adults: A population-based study. Rev. Saude Publica. 2018;52:15. doi: 10.11606/S1518-8787.2018052000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conklin A.I., Forouhi N.G., Suhrcke M., Surtees P., Wareham N.J., Monsivais P. Socioeconomic status, financial hardship and measured obesity in older adults: A cross-sectional study of the EPIC-Norfolk cohort. BMC Public Health. 2013;13:1039. doi: 10.1186/1471-2458-13-1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ruiz-Arregui L., Castillo-Martinez L., Orea-Tejeda A., Mejia-Arango S., Miguel-Jaimes A. Prevalence of self-reported overweight-obesity and its association with socioeconomic and health factors among older Mexican adults. Salud Publica Mex. 2007;49(Suppl. 4):S482–S487. doi: 10.1590/S0036-36342007001000007. [DOI] [PubMed] [Google Scholar]
- 38.Mezuk B., Rafferty J.A., Kershaw K.N., Hudson D., Abdou C.M., Lee H., Eaton W.W., Jackson J.S. Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race, and depression. Am. J. Epidemiol. 2010;172:1238–1249. doi: 10.1093/aje/kwq283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Assari S. Education Attainment and ObesityDifferential Returns Based on Sexual Orientation. Behav. Sci. (Basel) 2019;9:16. doi: 10.3390/bs9020016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fradkin C., Wallander J.L., Elliott M.N., Tortolero S., Cuccaro P., Schuster M.A. Associations between socioeconomic status and obesity in diverse, young adolescents: Variation across race/ethnicity and gender. Health Psychol. 2015;34:1–9. doi: 10.1037/hea0000099. [DOI] [PubMed] [Google Scholar]
- 41.Cook W.K., Tseng W. Associations of Asian Ethnicity and Parental Education with Overweight in Asian American Children and Adolescents: An Analysis of 2011–2016 National Health and Nutrition Examination Surveys. Matern. Child Health J. 2019;23:504–511. doi: 10.1007/s10995-018-2662-3. [DOI] [PubMed] [Google Scholar]
- 42.Matthiessen J., Stockmarr A., Biltoft-Jensen A., Fagt S., Zhang H., Groth M.V. Trends in overweight and obesity in Danish children and adolescents: 2000–2008—Exploring changes according to parental education. Scand. J. Public Health. 2014;42:385–392. doi: 10.1177/1403494813520356. [DOI] [PubMed] [Google Scholar]
- 43.Elinder L.S., Heinemans N., Zeebari Z., Patterson E. Longitudinal changes in health behaviours and body weight among Swedish school children—Associations with age, gender and parental education—The SCIP school cohort. BMC Public Health. 2014;14:640. doi: 10.1186/1471-2458-14-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Assari S. Health Disparities due to Diminished Return among Black Americans: Public Policy Solutions. Soc. Issues Policy Rev. 2018;12:112–145. doi: 10.1111/sipr.12042. [DOI] [Google Scholar]
- 45.Assari S. Unequal Gain of Equal Resources across Racial Groups. Int. J. Health Policy Manag. 2017;7:1–9. doi: 10.15171/ijhpm.2017.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Assari S., Thomas A., Caldwell C.H., Mincy R.B. Blacks’ Diminished Health Return of Family Structure and Socioeconomic Status; 15 Years of Follow-up of a National Urban Sample of Youth. J. Urban Health. 2018;95:21–35. doi: 10.1007/s11524-017-0217-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Assari S., Lankarani M.M. Race and Urbanity Alter the Protective Effect of Education but not Income on Mortality. Front. Public Health. 2016;4:100. doi: 10.3389/fpubh.2016.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Assari S., Preiser B., Kelly M. Education and Income Predict Future Emotional Well-Being of Whites but Not Blacks: A Ten-Year Cohort. Brain Sci. 2018;8:122. doi: 10.3390/brainsci8070122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Assari S. Over-adjustment bias by controlling for overall health. Int. J. Prev. Med. 2013;4:491–492. [PMC free article] [PubMed] [Google Scholar]
- 50.Assari S. Blacks’ Diminished Return of Education Attainment on Subjective Health; Mediating Effect of Income. Brain Sci. 2018;8:176. doi: 10.3390/brainsci8090176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Link B.G., Phelan J. The social shaping of health and smoking. Drug Alcohol Depend. 2009;104(Suppl. 1):S6–S10. doi: 10.1016/j.drugalcdep.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 52.Phelan J.C., Link B.G., Diez-Roux A., Kawachi I., Levin B. “Fundamental causes” of social inequalities in mortality: A test of the theory. J. Health Soc. Behav. 2004;45:265–285. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- 53.Link B.G., Phelan J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995 doi: 10.2307/2626958. [DOI] [PubMed] [Google Scholar]
- 54.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)74234-3. [DOI] [PubMed] [Google Scholar]
- 55.Marmot M. The Status Syndrome: How Social Standing Affects Our Health and Longevity. Bloomsbury Press; London, UK: 2004. [Google Scholar]
- 56.Marmot M. Economic and social determinants of disease. Bull. World Health Organ. 2001;79:988–989. [PMC free article] [PubMed] [Google Scholar]
- 57.Assari S. Parental Education Attainment and Educational Upward Mobility; Role of Race and Gender. Behav. Sci. (Basel) 2018;8:107. doi: 10.3390/bs8110107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Assari S. Parental Educational Attainment and Mental Well-Being of College Students; Diminished Returns of Blacks. Brain Sci. 2018;8:193. doi: 10.3390/brainsci8110193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ali F.R.M., Elsayed M.A.A. The effect of parental education on child health: Quasi-experimental evidence from a reduction in the length of primary schooling in Egypt. Health Econ. 2018;27:649–662. doi: 10.1002/hec.3622. [DOI] [PubMed] [Google Scholar]
- 60.Ruiz M., Goldblatt P., Morrison J., Porta D., Forastiere F., Hryhorczuk D., Antipkin Y., Saurel-Cubizolles M.J., Lioret S., Vrijheid M., et al. Impact of Low Maternal Education on Early Childhood Overweight and Obesity in Europe. Paediatr. Perinat. Epidemiol. 2016;30:274–284. doi: 10.1111/ppe.12285. [DOI] [PubMed] [Google Scholar]
- 61.Assari S., Lankarani M.M. Education and Alcohol Consumption among Older Americans; Black-White Differences. Front. Public Health. 2016;4:67. doi: 10.3389/fpubh.2016.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Assari S., Mistry R. Educational Attainment and Smoking Status in a National Sample of American Adults; Evidence for the Blacks’ Diminished Return. Int. J. Environ. Res. Public Health. 2018;15:2084. doi: 10.3390/ijerph15102084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Assari S., Mistry R., Bazargan M. Race, Educational Attainment, and E-Cigarette Use. J. Med Res. Innov. 2020;4:e000185. doi: 10.32892/jmri.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Assari S., Farokhnia M., Mistry R. Education Attainment and Alcohol Binge Drinking: Diminished Returns of Hispanics in Los Angeles. Behav. Sci. (Basel) 2019;9:9. doi: 10.3390/bs9010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Assari S. High Income Protects Whites but Not African Americans against Risk of Depression. Healthcare (Basel) 2018;6:37. doi: 10.3390/healthcare6020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Assari S. Life Expectancy Gain Due to Employment Status Depends on Race, Gender, Education, and Their Intersections. J. Racial Ethn. Health Disparities. 2018;5:375–386. doi: 10.1007/s40615-017-0381-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Assari S., Caldwell C.H., Zimmerman M.A. Family Structure and Subsequent Anxiety Symptoms; Minorities’ Diminished Return. Brain Sci. 2018;8:97. doi: 10.3390/brainsci8060097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Assari S. Socioeconomic Status and Self-Rated Oral Health; Diminished Return among Hispanic Whites. Dent. J. (Basel) 2018;6:11. doi: 10.3390/dj6020011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Assari S., Lapeyrouse L.M., Neighbors H.W. Income and Self-Rated Mental Health: Diminished Returns for High Income Black Americans. Behav. Sci. (Basel) 2018;8:50. doi: 10.3390/bs8050050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Assari S., Caldwell C.H. Family Income at Birth and Risk of Attention Deficit Hyperactivity Disorder at Age 15: Racial Differences. Children (Basel) 2019;6:10. doi: 10.3390/children6010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Geronimus A.T., Bound J., Waidmann T.A., Rodriguez J.M., Timpe B. Weathering, Drugs, and Whack-a-Mole: Fundamental and Proximate Causes of Widening Educational Inequity in U.S. Life Expectancy by Sex and Race, 1990-2015. J. Health Soc. Behav. 2019;60:222–239. doi: 10.1177/0022146519849932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hewagalamulage S.D., Lee T.K., Clarke I.J., Henry B.A. Stress, cortisol, and obesity: A role for cortisol responsiveness in identifying individuals prone to obesity. Domest. Anim. Endocrinol. 2016;56:S112–S120. doi: 10.1016/j.domaniend.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 73.Hopkins L.B., Medina J.L., Baird S.O., Rosenfield D., Powers M.B., Smits J.A. Heated hatha yoga to target cortisol reactivity to stress and affective eating in women at risk for obesity-related illnesses: A randomized controlled trial. J. Consult. Clin. Psychol. 2016;84:558–564. doi: 10.1037/ccp0000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen X., Gelaye B., Velez J.C., Barbosa C., Pepper M., Andrade A., Gao W., Kirschbaum C., Williams M.A. Caregivers’ hair cortisol: A possible biomarker of chronic stress is associated with obesity measures among children with disabilities. BMC Pediatr. 2015;15:9. doi: 10.1186/s12887-015-0322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee T.K., Lee C., Bischof R., Lambert G.W., Clarke I.J., Henry B.A. Stress-induced behavioral and metabolic adaptations lead to an obesity-prone phenotype in ewes with elevated cortisol responses. Psychoneuroendocrinology. 2014;47:166–177. doi: 10.1016/j.psyneuen.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 76.Vicennati V., Pasqui F., Cavazza C., Pagotto U., Pasquali R. Stress-related development of obesity and cortisol in women. Obesity (Silver Spring) 2009;17:1678–1683. doi: 10.1038/oby.2009.76. [DOI] [PubMed] [Google Scholar]
- 77.Gluck M.E., Geliebter A., Lorence M. Cortisol stress response is positively correlated with central obesity in obese women with binge eating disorder (BED) before and after cognitive-behavioral treatment. Ann. N. Y. Acad. Sci. 2004;1032:202–207. doi: 10.1196/annals.1314.021. [DOI] [PubMed] [Google Scholar]
- 78.Bjorntorp P., Rossner S., Udden J. “Consolatory eating” is not a myth. Stress-induced increased cortisol levels result in leptin-resistant obesity. Lakartidningen. 2001;98:5458–5461. [PubMed] [Google Scholar]
- 79.Rosmond R., Dallman M.F., Bjorntorp P. Stress-related cortisol secretion in men: Relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J. Clin. Endocrinol. Metab. 1998;83:1853–1859. doi: 10.1210/jc.83.6.1853. [DOI] [PubMed] [Google Scholar]
- 80.Assari S., Moghani Lankarani M., Caldwell C.H., Zimmerman M.A. Fear of Neighborhood Violence During Adolescence Predicts Development of Obesity a Decade Later: Gender Differences Among African Americans. Arch. Trauma Res. 2016;5:e31475. doi: 10.5812/atr.31475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jiao J., Moudon A.V., Ulmer J., Hurvitz P.M., Drewnowski A. How to identify food deserts: Measuring physical and economic access to supermarkets in King County, Washington. Am. J. Public Health. 2012;102:e32–e39. doi: 10.2105/AJPH.2012.300675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fielding J.E., Simon P.A. Food deserts or food swamps? comment on “Fast food restaurants and food stores”. Arch. Intern. Med. 2011;171:1171–1172. doi: 10.1001/archinternmed.2011.279. [DOI] [PubMed] [Google Scholar]
- 83.Walker R.E., Keane C.R., Burke J.G. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place. 2010;16:876–884. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 84.Smith C., Morton L.W. Rural food deserts: Low-income perspectives on food access in Minnesota and Iowa. J. Nutr. Educ. Behav. 2009;41:176–187. doi: 10.1016/j.jneb.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 85.Patel O., Shahulhameed S., Shivashankar R., Tayyab M., Rahman A., Prabhakaran D., Tandon N., Jaacks L.M. Association between full service and fast food restaurant density, dietary intake and overweight/obesity among adults in Delhi, India. BMC Public Health. 2017;18:36. doi: 10.1186/s12889-017-4598-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wellard L., Havill M., Hughes C., Watson W.L., Chapman K. Energy-dense fast food products cost less: An observational study of the energy density and energy cost of Australian fast foods. Aust. N. Z. J. Public Health. 2015;39:544–545. doi: 10.1111/1753-6405.12430. [DOI] [PubMed] [Google Scholar]
- 87.Hollands S., Campbell M.K., Gilliland J., Sarma S. Association between neighbourhood fast-food and full-service restaurant density and body mass index: A cross-sectional study of Canadian adults. Can. J. Public Health. 2014;105:e172–e178. doi: 10.17269/cjph.105.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Reitzel L.R., Regan S.D., Nguyen N., Cromley E.K., Strong L.L., Wetter D.W., McNeill L.H. Density and proximity of fast food restaurants and body mass index among African Americans. Am. J. Public Health. 2014;104:110–116. doi: 10.2105/AJPH.2012.301140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kwate N.O. Fried chicken and fresh apples: Racial segregation as a fundamental cause of fast food density in black neighborhoods. Health Place. 2008;14:32–44. doi: 10.1016/j.healthplace.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 90.Assari S. Parental Education Better Helps White than Black Families Escape Poverty: National Survey of Children’s Health. Economies. 2018;6:30. doi: 10.3390/economies6020030. [DOI] [Google Scholar]
- 91.Assari S. Race, Intergenerational Social Mobility and Stressful Life Events. Behav. Sci. (Basel) 2018;8:86. doi: 10.3390/bs8100086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rodriguez J.M., Geronimus A.T., Bound J., Dorling D. Black lives matter: Differential mortality and the racial composition of the U.S. electorate, 1970–2004. Soc. Sci. Med. 2015;136–137:193–199. doi: 10.1016/j.socscimed.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rodriguez J.M., Karlamangla A.S., Gruenewald T.L., Miller-Martinez D., Merkin S.S., Seeman T.E. Social stratification and allostatic load: Shapes of health differences in the MIDUS study in the United States. J. Biosoc. Sci. 2019;51:627–644. doi: 10.1017/S0021932018000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Muhammad M., De Loney E.H., Brooks C.L., Assari S., Robinson D., Caldwell C.H. “I think that’s all a lie...I think It’s genocide”: Applying a Critical Race Praxis to Youth Perceptions of Flint Water Contamination. Ethn. Dis. 2018;28:241–246. doi: 10.18865/ed.28.S1.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Moreno-Franco B., Perez-Tasigchana R.F., Lopez-Garcia E., Laclaustra M., Gutierrez-Fisac J.L., Rodriguez-Artalejo F., Guallar-Castillon P. Socioeconomic determinants of sarcopenic obesity and frail obesity in community-dwelling older adults: The Seniors-ENRICA Study. Sci. Rep. 2018;8:10760. doi: 10.1038/s41598-018-28982-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rodriguez J.M. Health disparities, politics, and the maintenance of the status quo: A new theory of inequality. Soc. Sci. Med. 2018;200:36–43. doi: 10.1016/j.socscimed.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 97.Feliu A., Filippidis F.T., Joossens L., Fong G.T., Vardavas C.I., Baena A., Castellano Y., Martinez C., Fernandez E. Impact of tobacco control policies on smoking prevalence and quit ratios in 27 European Union countries from 2006 to 2014. Tob. Control. 2019;28:101–109. doi: 10.1136/tobaccocontrol-2017-054119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Assari S., Hani N. Household Income and Children’s Unmet Dental Care Need; Blacks’ Diminished Return. Dent. J. (Basel) 2018;6:17. doi: 10.3390/dj6020017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Assari S., Caldwell C.H., Mincy R. Family Socioeconomic Status at Birth and Youth Impulsivity at Age 15; Blacks’ Diminished Return. Children (Basel) 2018;5:58. doi: 10.3390/children5050058. [DOI] [PMC free article] [PubMed] [Google Scholar]