Abstract
The aim of this cross-sectional study was to evaluate the association between the influence of occupational stress and coping style on periodontitis among Japanese workers. The study sample included 738 workers (age range: 19–65 years) at a manufacturing company in Kagawa Prefecture, Japan. To analyze occupational stress and coping style, all participants answered a self-report questionnaire composed of items on their work environment and oral health behavior. Oral examinations were performed by calibrated dentists. Among all workers, 492 (66.7%) workers were diagnosed with periodontitis, and 50 (6.8%) were diagnosed with a high stress-low coping condition. Significant differences (p < 0.05) were observed between the periodontitis and non-periodontitis groups in terms of age, gender, body mass index, smoking status, daily alcohol drinking, monthly overtime work, worker type, and stress-coping style. Logistic regression analysis showed that a high stress–low coping condition was associated with an increased risk of periodontitis (odds ratio: 2.79, 95% confidence interval: 1.05–7.43, p = 0.039). These findings suggest that a high stress-low coping condition is associated with periodontitis among the 19–65 years of age group of Japanese workers.
Keywords: occupational stress, coping, periodontitis, Japanese workers
1. Introduction
In recent years, occupational stress has become an increasingly serious problem around the world [1]. Remarkable changes in working duration, job engagement, and type of working environment have led to increased levels of occupational stress in workers [2]. The World Health Organization considers occupational stress among workers a global epidemic and is actively seeking to ascertain its severity [3]. Occupational stress is becoming a markedly serious problem among Japanese workers. According to previous studies, more than 60% of Japanese workers have reported experiencing work-related stress, and the number of workers with mental health problems has been rapidly increasing [4,5].
Occupational stress has adverse effects on employment (e.g., absenteeism, lateness, job dissatisfaction, and job turnover) [6,7,8]. Moreover, it contributes to poor physical and mental health [9]. For instance, research has shown that occupational stress is associated with certain oral health problems, including caries [10], periodontal disease [11], temporomandibular disorder, and halitosis [12]. Stress has long been regarded as an important predisposing factor for periodontal disease among workers, and an association has been reported between periodontal disease and work-related stress and dissatisfaction [13]. Coping is the response of the individual to control, minimize, or avoid the adverse and unpleasant effects of stress. According to Lazarus et al., an individual’s psychological and physical well-being depends on coping strategies more than the frequency and intensity of stress [14,15]. Concurrently, the relationship between stress and individual coping styles has been shown to be associated with periodontal disease. A 24-month prospective study involving chronic periodontitis patients found that patients with an active coping style showed a lesser degree of disease advancement than those with a passive coping style [16]. Furthermore, the effects of stress on periodontal disease can be restrained by adequate coping behaviors [17]. Another study found that coping style had a protective effect against tooth loss [18]. However, to our knowledge, no studies have explained the influence of coping style against stress, especially workplace-induced occupational stress, on periodontal disease.
Therefore, the aim of the present cross-sectional study was to investigate the influence of occupational stress and coping style on periodontitis among Japanese workers, and, thereby, test the hypothesis that the balance between occupational stress and coping style is related to periodontal disease.
2. Materials and Methods
2.1. Study Design and Participants
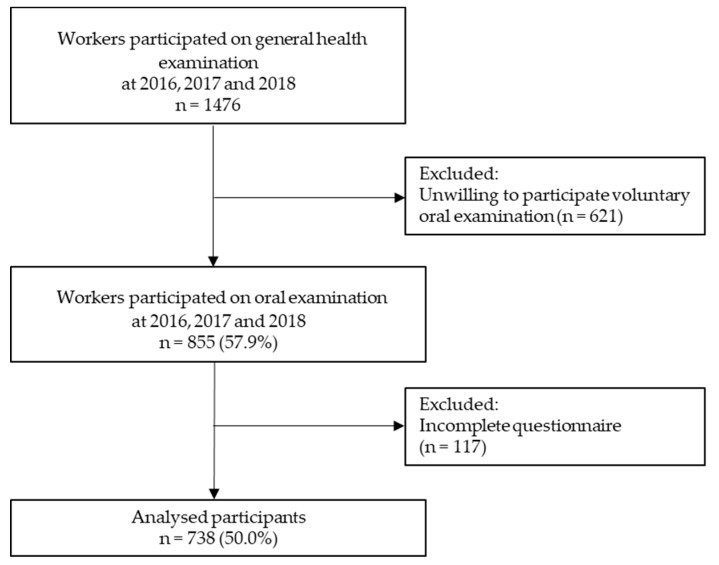
Anonymous data for this cross-sectional study were obtained from the workers of a Japanese crane manufacturing company located in Kagawa Prefecture, Japan, for the years 2016–2018 (in February each year). All workers received a routine general health checkup, including a voluntary dental checkup. We distributed the questionnaires to the participants prior to health checkups and collected them during the annual health checkups. A total of 1476 workers participated in the general health examinations, among whom, those who received a voluntary dental checkup and completed a questionnaire (n = 855) were enrolled in the study. After excluding those with incomplete questionnaires, we analyzed the data of 738 (86.3%) workers. All participants provided informed consent at the time of their interview.
2.2. Job Category
We followed the job category criteria provided by the Ministry of Health, Labor, and Welfare of Japan. According to these criteria, all participants were classified as office workers (e.g., computer operators, clerks, secretaries) or skilled workers (e.g., factory workers, construction workers).
2.3. Assessment of Stress and Coping Style
In this study, we used the “Co–Labo57 +” questionnaire [19], which is composed of six parts (parts A–F). Questions from parts A–D adopt the Brief Job Stress Questionnaire (BJSQ) to measure occupational stress. The reliability and validity of the BJSQ was confirmed for Japanese workers [12,20,21]. The BJSQ is composed of 57 items used to assess job stressors (Part A, 17 items: e.g., psychological job demands, job control), stress response (Part B, 29 items: e.g., psychological and physical stress reactions), and buffering factors (Parts C and D, 11 items: e.g., social support at work). The BJSQ program manual suggests criteria for categorizing stress levels [22]. High-stress was determined as having the highest level of a stress reaction [criterion (i)] or a moderate level of a stress reaction, along with having the highest job stressors (or lowest social support in the workplace) [criterion (ii)]. In this study, to calculate the stress reaction and job stressor scores, we summed the item scores from a four-point Likert scale (from 1 = low stress to 4 = high stress). The scores ranged from 29 to 116 for stress reactions (Part A) and from 26 to 104 for job stressors (Part B). The cutoff points were 77 for the stress reaction score for criterion (i), 63 for the stress reaction score, and 76 for the job stressor score for criterion (ii) [23]. If the score for criterion (i) or criterion (ii) was higher than the cutoff point, the participant was classified as high stress.
Coping style was assessed using the remaining two parts (E and F). The participant was considered to have a high coping style if the summed score was ≥ 20 for part E or ≥ 68 for part F.
2.4. General Health and Lifestyles Assessment
All participants underwent a mandatory general health examination. Body weight and height were measured to calculate body mass index (BMI), which was categorized as <25 or ≥25 kg/m2 [24]. In addition, the participants provided answers regarding their age, gender, and other lifestyle-related factors, including job type (office or skilled worker), smoking status (current, never, or former), daily alcohol drinking (yes or no), daily sleep duration (≥6 or <6 h) [25], and amount of overtime work (≥40 or <40 h/month) [26]. The amount of overtime work was assessed by calculating total hours worked minus the standard 8 working hours per day on weekdays, plus the number of hours worked on holidays during the entire month.
Oral health behavior was assessed by asking about the use of dental floss (yes or no) and whether the participant had a regular dental checkup in the past year (yes or no) [27].
2.5. Oral Examinations
The participants’ oral conditions (e.g., number of healthy, missing, and decayed teeth, plaque and calculus level, gingival and periodontal health, malocclusion, temporomandibular joint findings) were evaluated by calibrated dentists. Using an objective method [28], the participants were then classified into either a periodontitis or a non-periodontitis group. Briefly, no inflammation in the gingiva or redness and/or swelling of the interdental papilla without gingival recession was classified as non-periodontitis, and any redness and/or swelling in the gingiva with gingival recession and/or tooth mobility was classified as periodontitis. The intra and inter-examiner reliabilities was evaluated by kappa statistics of more than 0.8.
2.6. Ethical Considerations
The study protocol was approved by the Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences and Okayama University Hospital Ethics Committee (No. 1905-016).
2.7. Statistical Analysis
The normality of the data was investigated using a histogram, quantile–quantile plot, and the Shapiro-Wilk test [29]. The sample size was estimated using G * Power (ver. 3.1.9.2, Universität Kiel, Kiel, Germany), and the minimum sample sizes were calculated for analysis using a chi-squared test [30]. Considering an effect size of 0.3, alpha of 0.05, and power (1 − β) of 0.80, the minimum sample size required was 88 [31]. Since the company had more than an adequate number of workers to obtain reasonable results, we enrolled more than 88 workers in our study.
For the descriptive analysis, means and standard deviations were calculated for continuous variables, whereas categorical variables were presented as percentiles. p values were calculated for the continuous and categorical variables using the Mann-Whitney U test and chi-squared test, respectively. The results from the logistic regression analysis were presented as odds ratios (ORs) and 95% confidence intervals (CIs). p values < 0.05 were considered statistically significant. All analyses were performed using the SPSS statistical package (v. 25.0; SPSS Inc., Chicago, IL, USA).
3. Results
Figure 1 shows a flowchart of the enrollment procedure. Following the scoring criteria of the Co-Labo57+ questionnaire, we identified a total of 88 (11.9%) workers as high-stress and 438 (59.3%) as having a high coping style. The characteristics of the workers are shown in Table 1. Among the 738 workers, 646 were men (87.5%) and 92 were women (12.5%). The mean age was 40.7 ± 10.5 years. The prevalence of periodontitis was 66.7% (n = 492). Among the workers, 88.1% (n = 650) were classified to the “low stress,” 5.1% (n = 38) to the “high stress–high coping,” and 6.8% (n = 50) to the “high stress–low coping” group.
Figure 1.
Flowchart of the enrollment procedure.
Table 1.
Characteristics of all workers.
| Parameters (n = 738) | n (%) Mean ± SD |
|---|---|
| Age (y) | 40.7 ± 10.5 |
| Gender | |
| Male | 646 (87.5) |
| Female | 92 (12.5) |
| Daily flossing (Yes) | 95 (12.9) |
| Regular dental checkup (Yes) | 107 (14.5) |
| Periodontitis (Yes) | 492 (66.7) |
| BMI (kg/m2) | |
| <25 | 545 (73.8) |
| ≥25 | 193 (26.2) |
| Hypertension (Yes) | 47 (6.4) |
| Daily sleeping duration (≥6 h) | 631 (85.5) |
| Current smoker (Yes) | 206 (27.9) |
| Daily alcohol drinking (Yes) | 128 (17.3) |
| Monthly overtime work (≥40 h) | 187 (25.3) |
| Worker type | |
| Skilled worker | 334 (45.3) |
| Office worker | 404 (54.7) |
| Low stress | 650 (88.1) |
| High stress-High coping | 38 (5.1) |
| High stress-Low coping | 50 (6.8) |
BMI, body mass index. SD, standard deviation.
Table 2 shows a comparison between the periodontitis and non-periodontitis groups. The mean age in the periodontitis group was significantly higher than that in the non-periodontitis group (p < 0.001). Significant differences were also seen between the two groups in gender, BMI, smoking status, daily alcohol drinking, monthly overtime work, worker type, and stress-coping style (p < 0.05).
Table 2.
Comparisons of the between periodontitis and non-periodontitis groups.
| Parameters (n = 738) | Periodontitis (n = 492) | Non-Periodontitis (n = 246) | p Value |
|---|---|---|---|
| n (%) Mean ± SD |
n (%) Mean ± SD |
||
| Age (y) | 43 ± 10.1 | 34.9 ± 8.9 | <0.001 1 |
| Gender (Male) | 462 (93.9) | 184 (74.8) | <0.001 2 |
| Daily flossing (Yes) | 64 (13.0) | 31 (12.6) | 0.876 2 |
| Regular dental checkup (Yes) | 70 (14.2) | 37 (15.0) | 0.767 2 |
| BMI (kg/m2) | |||
| <25 | 336 (68.3) | 209 (85.0) | <0.001 2 |
| ≥25 | 156 (31.7) | 37 (15.0) | |
| Sleeping duration (daily) | |||
| ≥6 h | 418 (85.0) | 213 (86.6) | 0.554 2 |
| <6 h | 74 (15.0) | 33 (13.4) | |
| Current smoker (Yes) | 161 (32.7) | 45 (18.3) | <0.001 2 |
| Daily alcohol drinking (Yes) | 104 (21.1) | 26 (10.6) | <0.001 2 |
| Monthly overtime work | |||
| (≥40 h) | 145 (29.5) | 42 (17.1) | <0.001 2 |
| Worker type | |||
| Skilled worker | 245 (49.8) | 89 (36.2) | <0.001 2 |
| Office worker | 247 (50.2) | 157 (63.8) | |
| Low stress | 431 (87.6) | 219 (89.0) | <0.001 2 |
| High stress-High coping | 17 (3.5) | 21 (8.5) | |
| High stress-Low coping | 44 (8.9) | 6 (2.5) |
BMI, body mass index. SD, standard deviation. 1 Mann–Whitney U test, and 2 chi-squared test.
As shown in Table 3, the logistic regression analysis revealed that periodontitis was significantly associated with age, the male gender, BMI ≥ 25 kg/m2, and smoking status (current smoker) (p < 0.001). Moreover, periodontitis was significantly associated with the “high stress-low coping” style (p = 0.039).
Table 3.
Adjusted odds ratios (OR) and 95% confidence intervals (95% CI) for periodontitis.
| Dependent Variable | Independent Variable | OR | 95% CI | p-Value 1 | |
|---|---|---|---|---|---|
| Periodontitis | Age | 1.11 | 1.09–1.14 | <0.001 | |
| Gender | Female | Ref | |||
| Male | 5.11 | 2.81–9.30 | <0.001 | ||
| Daily flossing | Yes | Ref | |||
| No | 0.99 | 0.57–1.76 | 0.990 | ||
| Regular dental checkup | Yes | Ref | |||
| No | 1.17 | 0.69–1.99 | 0.562 | ||
| BMI (kg/m2) | <25 | Ref | |||
| ≥25 | 2.23 | 1.42–3.51 | < 0.001 | ||
| Sleeping duration (daily) | ≥6 h | Ref | |||
| <6 h | 0.98 | 0.58–1.67 | 0.938 | ||
| Current smoker | No | Ref | |||
| Yes | 2.08 | 1.35–3.22 | < 0.001 | ||
| Daily alcohol drinking | No | Ref | |||
| Yes | 1.24 | 0.73–2.11 | 0.424 | ||
| Monthly overtime work | <40 h | Ref | |||
| ≥40 h | 1.07 | 0.68–1.71 | 0.765 | ||
| Worker type | Office worker | Ref | |||
| Skilled worker | 1.31 | 0.89–1.95 | 0.175 | ||
| Low stress | Ref | ||||
| High stress-High coping | 0.30 | 0.14–0.66 | 0.003 | ||
| High stress-Low coping | 2.79 | 1.05–7.43 | 0.039 |
BMI, body mass index. CI, confidence interval. OR, odds ratio. 1 Multiple logistic regression model adjusted for age, gender, daily flossing, regular dental checkups, BMI, sleeping duration (daily), smoking status (current smoker), daily alcohol drinking, monthly overtime work, worker type, and stress-coping style.
4. Discussion
In this cross-sectional study, we focused on the influence of occupational stress and coping style on periodontitis. To the best of our knowledge, this is the first study to investigate whether the balance between occupational stress and coping style is associated with the prevalence of periodontitis among Japanese workers. Our results showed that having a low coping style against high occupational stress was significantly associated with periodontitis (adjusted ORs: 2.79, 95% CI: 1.05–7.43, p = 0.039).
The workers with the high stress–high coping style were not found to be at a higher risk for periodontitis in this study, which suggests an association between periodontitis and an effective stress-coping style. This condition can be explained by several possible mechanisms. For example, an inappropriate coping attitude (e.g., increased tobacco smoking, alcohol drinking) and the adoption of unhealthy behaviors (e.g., poor oral hygiene, insufficient nutritional intake) can lead to drastic changes in oral health [32,33,34]. Concurrently, an inadequate stress-coping style may cause mental alterations and induce immune suppression, which may aggravate chronic inflammatory diseases such as periodontitis [35].
Our results found a higher prevalence of current smokers with periodontitis than in the non-periodontitis group. Previous studies have reported smoking as a coping mechanism against stress among workers [36,37]. On the other hand, an association between smoking and the risk of periodontitis has been established [18,38,39]. Therefore, attempts should be made to prevent smoking among workers.
In the present study, no significant difference in overtime work was found between the periodontitis and non-periodontitis groups. A previous study among Korean workers reported that overtime work was associated with the prevalence of periodontitis [40]. The discrepancy in the findings from the previous study and the present study may depend on race (Korean vs. Japanese) and the percentage of overtime workers (60.3% vs. 25.3%). In addition, no significant difference in job category was found between the periodontitis and non-periodontitis groups, which is in line with previous studies finding no significant association between the job category (skilled and office workers) and periodontitis [41,42].
Additionally, in line with a previous study [43], the overweight factor was found to be a risk factor for periodontitis among workers. Other previous studies have reported finding a positive relation between coping style and BMI [44,45]. Hence, to help find balance between stress and coping, workers should be encouraged to limit their working hours and engage in a healthy lifestyle while maintaining a normal body weight.
The prevalence of periodontitis in this study was 66.7%, which differed from other studies in Japan. A five-year cohort study that defined periodontitis as having one or more sextants with a Community Periodontal Index score > 2 (pockets ≥ 4 mm deep) reported that 55.4% of Japanese workers had periodontitis [41]. Another cross-sectional study that measured periodontitis by probing pocket depth and clinical attachment loss (CAL) at mesio-buccal and mid-buccal sites for all of the teeth in two randomly selected quadrants indicated that only 13% of Japanese workers had periodontitis, which was defined as having at least one tooth with a CAL of ≥7 mm [46]. Possible causes for this discrepancy might be the type of oral examination or the study design. On the other hand, in the present study, 11.9% of workers reported having high occupational stress. This result was in line with a previous Japanese study using the same questionnaire [23].
The present study showed that the risk of periodontitis is influenced by the balance between occupational stress and coping style. Therefore, a comprehensive approach should be taken to minimize the occupational stress and improve the coping ability of the workers. Our results also suggest that, during the management of periodontitis in a clinical setting, the coping style of workers against occupational stress should be taken into consideration.
This study had some limitations. First, all workers were enrolled from a Japanese crane manufacturing company. Therefore, the influence of stress and coping style on periodontitis might differ from other types of workers. Second, no other possible confounders, such as working schedule [40], education level [3], income level [47], and family situation [48], were examined in this study. Third, periodontitis was diagnosed using an objective method due to time constraints, but no probing or X-ray findings were used. Hence, there is a possibility of presenting a large group of mild periodontitis with little clinical impact. Lastly, a causal association could not be shown because this study was cross-sectional.
5. Conclusions
The findings of the present study suggest that a high stress–low coping style is associated with an increased risk of periodontitis among the 19–65 years of age group of Japanese workers. Therefore, during the management of periodontitis, the balance between occupational stress and coping style should also be considered.
Acknowledgments
The authors are grateful to Ms. Yuriko Akazawa (Tadano Ltd., Takamatsu, Japan) and General Incorporated Association Total Health Promotion Association Kansai (Osaka, Japan) for the data entry.
Author Contributions
Conceptualization, M.M., D.E., and M.M.I. Methodology, D.E., T.Y., and A.Y. Validation, D.E. Formal analysis, M.M.I. Investigation, D.E., T.Y., and A.Y. Resources, M.M. Data curation, D.E., T.Y., and A.Y. Writing the original draft preparation, M.M.I. Writing the review and editing, all authors. Project administration, M.M.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Anderson N., Ones S., Sinangil K., Viswesvaran C. Handbook of Industrial, Work & Organizational Psychology—Volume 2: Organizational Psychology. SAGE Publications; London, UK: 2001. [Google Scholar]
- 2.Papadopoulos G., Georgiadou P., Papazoglou C., Michaliou K. Occupational and public health and safety in a changing work environment: An integrated approach for risk assessment and prevention. Saf. Sci. 2010;48:943–949. doi: 10.1016/j.ssci.2009.11.002. [DOI] [Google Scholar]
- 3.Li Y., Sun X., Ge H., Liu J., Chen L. The Status of Occupational Stress and Its Influence the Quality of Life of Copper-Nickel Miners in Xinjiang, China. Int. J. Environ. Res. Public Health. 2019;16:353. doi: 10.3390/ijerph16030353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Annual Health, Labour and Welfare Report 2009–2010 Section 7 Creating an Environment Where People Can Work with Confidence and Satisfaction. [(accessed on 12 June 2019)];Japan Ministry of Health, Labour and Welfare. Available online: https://www.mhlw.go.jp/english/wp/wp-hw/index.html.
- 5.Hara Y. Mental Disorders among Today’s Labor Force and Preventive Measures. Jpn. Lab. Rev. 2014;11:5. [Google Scholar]
- 6.Melchior M. Do psychosocial work factors and social relations exert independent effects on sickness absence? A six year prospective study of the GAZEL cohort. J. Epidemiol. Community Health. 2003;57:285–293. doi: 10.1136/jech.57.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kammeyer-Mueller J.D., Wanberg C.R. Unwrapping the organizational entry process: Disentangling multiple antecedents and their pathways to adjustment. J. Appl. Physiol. 2003;88:779–794. doi: 10.1037/0021-9010.88.5.779. [DOI] [PubMed] [Google Scholar]
- 8.Bond F.W., Bunce D. Job control mediates change in a work reorganization intervention for stress reduction. J. Occup. Health Psychol. 2001;6:290–302. doi: 10.1037/1076-8998.6.4.290. [DOI] [PubMed] [Google Scholar]
- 9.Leka S., Cox T., Griffiths A. Work Organization & Stress: Systematic Problem Approaches for Employers, Managers and Trade Union Representatives. World Health Organization; Geneva, Switzerland: 2003. [Google Scholar]
- 10.Marcenes W.S., Sheiham A. The relationship between work stress and oral health status. Soc. Sci. Med. 1992;35:1511–1520. doi: 10.1016/0277-9536(92)90054-T. [DOI] [PubMed] [Google Scholar]
- 11.Linden G.J., Mullally B.H., Freeman R. Stress and the progression of periodontal disease. J. Clin. Periodontol. 1996;23:675–680. doi: 10.1111/j.1600-051X.1996.tb00593.x. [DOI] [PubMed] [Google Scholar]
- 12.Yoshino K., Suzuki S., Ishizuka Y., Takayanagi A., Sugihara N., Kamijyo H. Relationship between job stress and subjective oral health symptoms in male financial workers in Japan. Ind. Health. 2017;55:119–126. doi: 10.2486/indhealth.2016-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atri M., Srivastava D., Kharbanda J., Bugalia A., Yousuf A., Anup N. Occupational Stress, Salivary Cortisol, and Periodontal Disease: A Clinical and Laboratory Study. J. Int. Oral Health. 2015;7:65–69. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Lazarus R.S. Stress and Emotion: A New Synthesis. Springer; New York, NY, USA: 2006. [Google Scholar]
- 15.Lazarus R.S., Folkman S. Stress, Appraisal, and Coping. Springer; New York, NY, USA: 1984. [Google Scholar]
- 16.Wimmer G., Köhldorfer G., Mischak I., Lorenzoni M., Kallus K.W. Coping with Stress: Its Influence on Periodontal Therapy. J. Periodontol. 2005;76:90–98. doi: 10.1902/jop.2005.76.1.90. [DOI] [PubMed] [Google Scholar]
- 17.Genco R., Ho A., Grossi S., Dunford R., Tedesco L. Relationship of Stress, Distress, and Inadequate Coping Behaviors to Periodontal Disease. J. Periodontol. 1999;70:711–723. doi: 10.1902/jop.1999.70.7.711. [DOI] [PubMed] [Google Scholar]
- 18.Sanders A., Slade G., Turrell G., Spencer A., Marcenes W. Does Psychological Stress Mediate Social Deprivation in Tooth Loss? J. Dent. Res. 2007;86:1166–1170. doi: 10.1177/154405910708601205. [DOI] [PubMed] [Google Scholar]
- 19.Sumiko S. Case studies and Effect of Psychological Counselling Using Co-Labo Scale (Job stress scale-Revised, EAP version) at Workplace. Job Stress Res. 2009;16:93–103. (In Japanese) [Google Scholar]
- 20.Endo M. Recurrent Sickness Absence due to Depression: A Two-year Cohort among Japanese Employees. Int. J. Epidemiol. 2015;44:i48. doi: 10.1093/ije/dyv097.186. [DOI] [PubMed] [Google Scholar]
- 21.Fukuda Y., Iwasaki S., Deguchi Y., Ogawa K., Nitta T., Inoue K. The effect of long-term sickness absence on coworkers in the same work unit. Ind. Health. 2018;56:2–9. doi: 10.2486/indhealth.2017-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health, Labour and Welfare, Japan. [(accessed on 10 June 2019)]; Available online: http://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/
- 23.Tsutsumi A., Shimazu A., Eguchi H., Inoue A., Kawakami N. A Japanese Stress Check Program screening tool predicts employee long-term sickness absence: A prospective study. J. Occup. Health. 2018;60:55–63. doi: 10.1539/joh.17-0161-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoshino K., Suzuki S., Ishizuka Y., Takayanagi A., Sugihara N., Kamijyo H. Relationship between amount of overtime work and untreated decayed teeth in male financial workers in Japan. J. Occup. Health. 2017;59:280–285. doi: 10.1539/joh.16-0247-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Utsugi M., Saijo Y., Yoshioka E., Horikawa N., Sato T., Gong Y., Kishi R. Relationships of Occupational Stress to Insomnia and Short Sleep in Japanese Workers. Sleep. 2005;28:728–735. doi: 10.1093/sleep/28.6.728. [DOI] [PubMed] [Google Scholar]
- 26.Sato Y., Miyake H., Theriault G. Overtime work and stress response in a group of Japanese workers. Occup. Med. 2009;59:14–19. doi: 10.1093/occmed/kqn141. [DOI] [PubMed] [Google Scholar]
- 27.Lang W.P., Farghaly M.M., Ronis D.L. The relation of preventive dental behaviors to periodontal health status. J. Clin. Periodontol. 1994;21:194–198. doi: 10.1111/j.1600-051X.1994.tb00303.x. [DOI] [PubMed] [Google Scholar]
- 28.Yokoi A., Ekuni D., Yoneda T., Morita M. Relationships among Metabolic Syndrome, Eating Quickly, and Oral Status in the Workplace. J. Dent. Health. 2018;68:9–14. (In Japanese) [Google Scholar]
- 29.Henderson A.R. Testing experimental data for univariate normality. Clin. Chim. Acta. 2006;366:112–129. doi: 10.1016/j.cca.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J. A power primer. Psychol. Bull. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 32.Wiebe D.J., Mccallum D.M. Health practices and hardiness as mediators in the stress-illness relationship. Health Psychol. 1986;5:425–438. doi: 10.1037/0278-6133.5.5.425. [DOI] [PubMed] [Google Scholar]
- 33.Shankardass K. Rethinking Social Epidemiology: Towards a Science of Change. Springer; Dordrecht, The Netherlands: 2012. Place-based stress and chronic disease: A systems view of environmental determinants. [Google Scholar]
- 34.Stabholz A., Soskolne W.A., Shapira L. Genetic and environmental risk factors for chronic periodontitis and aggressive periodontitis. Periodontology 2000. 2010;53:138–153. doi: 10.1111/j.1600-0757.2010.00340.x. [DOI] [PubMed] [Google Scholar]
- 35.Wimmer G., Janda M., Wieselmann-Penkner K., Jakse N., Polansky R., Pertl C. Coping with Stress: Its Influence on Periodontal Disease. J. Periodontol. 2002;73:1343–1351. doi: 10.1902/jop.2002.73.11.1343. [DOI] [PubMed] [Google Scholar]
- 36.Keller-Hamilton B., Moe A.M., Breitborde N.J.K., Lee A., Ferketich A.K. Reasons for smoking and barriers to cessation among adults with serious mental illness: A qualitative study. J. Community Psychol. 2019;47:1462–1475. doi: 10.1002/jcop.22197. [DOI] [PubMed] [Google Scholar]
- 37.Tran B.X., Vu G.T., Pham K.T.H., Vuong Q.-H., Ho M.-T., Vuong T.-T., Nguyen H.-K.T., Nguyen C.T., Latkin C.A., Ho C.S., et al. Depressive Symptoms among Industrial Workers in Vietnam and Correlated Factors: A Multi-Site Survey. Int. J. Environ. Res. Public Health. 2019;16:1642. doi: 10.3390/ijerph16091642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yamamoto Y., Nishida N., Tanaka M., Hayashi N., Matsuse R., Nakayama K., Morimoto K., Shizukuishi S. Association between passive and active smoking evaluated by salivary cotinine and periodontitis. J. Clin. Periodontol. 2005;32:1041–1046. doi: 10.1111/j.1600-051X.2005.00819.x. [DOI] [PubMed] [Google Scholar]
- 39.Ojima M., Hanioka T., Tanaka K., Inoshita E., Aoyama H. Relationship between smoking status and periodontal conditions: Findings from national databases in Japan. J. Periodontal Res. 2006;41:573–579. doi: 10.1111/j.1600-0765.2006.00915.x. [DOI] [PubMed] [Google Scholar]
- 40.Lee W., Lim S.-S., Kim B., Won J.-U., Roh J., Yoon J.-H. Relationship between long working hours and periodontitis among the Korean workers. Sci. Rep. 2017;7:7967. doi: 10.1038/s41598-017-08034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Irie K., Yamazaki T., Yoshii S., Takeyama H., Shimazaki Y. Is there an occupational status gradient in the development of periodontal disease in Japanese workers? A 5-year prospective cohort study. J. Epidemiol. 2017;27:69–74. doi: 10.1016/j.je.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morita I., Nakagaki H., Yoshii S., Tsuboi S., Hayashizaki J., Igo J., Mizuno K., Sheiham A. Gradients in periodontal status in Japanese employed males. J. Clin. Periodontol. 2007;34:952–956. doi: 10.1111/j.1600-051X.2007.01147.x. [DOI] [PubMed] [Google Scholar]
- 43.Ekuni D., Mizutani S., Kojima A., Tomofuji T., Irie K., Azuma T., Yoneda T., Furuta M., Eshima N., Iwasaki Y., et al. Relationship between increases in BMI and changes in periodontal status: A prospective cohort study. J. Clin. Periodontol. 2014;41:772–778. doi: 10.1111/jcpe.12273. [DOI] [PubMed] [Google Scholar]
- 44.Shimanoe C., Hara M., Nishida Y., Nanri H., Otsuka Y., Nakamura K., Higaki Y., Imaizumi T., Taguchi N., Sakamoto T., et al. Perceived Stress and Coping Strategies in Relation to Body Mass Index: Cross-Sectional Study of 12,045 Japanese Men and Women. PLoS ONE. 2015;10:e0118105. doi: 10.1371/journal.pone.0118105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hayward L.E., Vartanian L.R., Pinkus R.T. Coping with weight stigma: Development and validation of a Brief Coping Responses Inventory. Obes. Sci. Pract. 2017;3:373–383. doi: 10.1002/osp4.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yamamoto T., Koyama R., Tamaki N., Maruyama T., Tomofuji T., Ekuni D., Yamanaka R., Azuma T., Morita M. Validity of a Questionnaire for Periodontitis Screening of Japanese Employees. J. Occup. Health. 2009;51:137–143. doi: 10.1539/joh.L8108. [DOI] [PubMed] [Google Scholar]
- 47.Damaske S., Zawadzki M.J., Smyth J.M. Stress at work: Differential experiences of high versus low SES workers. Soc. Sci. Med. 2016;156:125–133. doi: 10.1016/j.socscimed.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao J.S., He N.P., Lovrich N., Cancino J. Marital Status and Police Occupational Stress. J. Crime Justice. 2003;26:23–46. doi: 10.1080/0735648X.2003.9721181. [DOI] [Google Scholar]