Abstract
Background:
The quadriceps tendon is becoming a popular graft option for anterior cruciate ligament (ACL) reconstruction. Few studies have examined the biomechanics of the quadriceps tendon compared with more commonly used graft choices. Due to the risk associated with small-diameter hamstring tendon grafts, various modifications of hamstring tendon preparation techniques have been described—specifically, a tripled, 6-strand hamstring tendon construct. This is the first study to directly compare the biomechanical properties of quadriceps tendon and hamstring tendon grafts.
Purpose/Hypothesis:
The purpose of this study was to quantify the biomechanical properties of the quadriceps tendon and 6-strand hamstring tendon grafts, specifically evaluating ultimate load to failure, load at 3 mm of displacement, and stiffness. These parameters characterize the time zero, in vitro, static tensile properties of these graft options. Our hypothesis was that for grafts of similar size, there would not be a significant difference in the biomechanical properties.
Study Design:
Controlled laboratory study.
Methods:
Quadriceps and hamstring tendon grafts were harvested from 6 human cadaveric knees (mean age, 61.17 ± 10.38 years). These matched grafts were prepared and biomechanically tested using an all-electric dynamic test load system. The mean diameter, stiffness, ultimate load to failure, and load to 3 mm of displacement were evaluated and analyzed.
Results:
The mean diameters of the 6-strand hamstring and quadriceps tendons were 11.33 and 10.16 mm, respectively (P = .03). Despite these significantly different diameters, no differences were found in graft ultimate load to failure or load at 3 mm of displacement. The 6-strand hamstring tendon graft was significantly stiffer compared with the quadriceps tendon (1147.65 vs 808.65 N/mm; P = .04).
Conclusion:
The 6-strand hamstring tendon and quadriceps tendon graft had similar biomechanical properties with respect to ultimate load to failure and load at 3 mm of displacement in 6 matched cadaveric specimens. Both grafts were significantly stiffer than the native ACL, and the hamstring tendon construct was significantly stiffer than the quadriceps tendon.
Clinical Relevance:
The quadriceps tendon graft is a reliable alternative to a 6-strand hamstring tendon graft for ACL reconstruction.
Keywords: ACL, biomechanics, tendon, ligament, anatomy
Anterior cruciate ligament (ACL) reconstruction is one of the most commonly performed procedures by orthopaedic surgeons in the United States, where more than 200,000 such procedures are performed each year.14 Surgical technique including graft choice and fixation is typically influenced by surgeon preference and patient characteristics, as many different options are available that produce similar success. Historically, the bone–patellar tendon–bone (BPTB) graft has been considered the gold standard. However, the associated morbidity including frontal knee pain, numbness, loss of motion, patellar fracture, and patellar tendon rupture has led surgeons to investigate alternative graft options.2,5,18
Alternative graft options include hamstring tendon (HT), quadriceps tendon (QT), and allograft tissue. HT autograft is a popular graft choice, as demonstrated in a 2013 survey by the American Academy of Orthopaedic Surgeons1 in which 44% of surgeons indicated that they preferred HT autograft for primary ACL reconstruction in adult recreational athletes. However, graft harvest complications, such as saphenous nerve injury and prematurely transected grafts, and the potential for small diameter grafts, which increase the risk of rerupture, can be a dilemma for surgeons.6,10 In an attempt to address the issue of small-diameter HT grafts, various techniques of HT graft preparation have been suggested to increase the diameter of these grafts.9
The QT graft was introduced in 1979 by Marshall et al.11 A recent systematic review revealed that the QT graft had knee stability, functional outcomes, and rerupture rates comparable with HT and BPTB but decreased rates of numbness and anterior knee pain.7 An additional advantage of the QT graft is a more dependable graft size: As is the case with the BPTB graft, the surgeon can select the graft’s width at the time of harvest.22 The use of the QT graft has increased recently with advancing harvest techniques. In 2014, Middleton et al12 revealed that 11% of surgeons across 20 countries preferred the QT graft.
The QT has been compared with BPTB biomechanically, with favorable results.20 The biomechanical performance of the QT has been shown to be similar to that of a quadrupled (4-strand) HT, but to our knowledge, the QT has not been compared with a 6-strand HT graft.19
The purpose of this study was to quantify the biomechanical properties of the QT and 6-strand HT grafts, specifically evaluating ultimate load to failure, load at 3 mm of displacement, and stiffness. These parameters characterize the time zero, in vitro, static tensile properties of these graft options. Our hypothesis was that for grafts of similar size, there would not be a significant difference in biomechanical properties.
Methods
All specimen preparation and biomechanical testing were performed at Arthrex headquarters in Naples, Florida, USA.
Graft Harvest and Preparation
All fresh-frozen cadaveric knees used in this study were granted from Science Care. The mean ± SD age was 61.17 ± 10.38 years (range, 49-74 years). The cadavers were thawed, and after graft harvest, the grafts were immediately tested. All grafts were handled in similar fashion. The QTs and HTs were harvested from 6 cadavers, producing a total of 12 grafts. For the HT harvest, the gracilis and semitendinosus tendons were identified after reflection of the sartorial fascia. The tendons were isolated, and a tendon stripper was used to harvest each tendon. Muscle was stripped off the proximal tendon, and the tendons were shortened to a length of 24 cm. The tendons were combined and a No. 2 FiberLoop suture (Arthrex) was used to whipstitch each end for handling purposes (Figure 1). No. 2-0 FiberWire (Arthrex) was used to create a tripled, 6-strand HT construct, demonstrated in Figures 2 and 3. The graft was measured, and a corresponding diameter QT-specific cutting guide (Arthrex) was used to harvest the QT. This cutting guide was used on the central aspect of the QT, and a combination of a scalpel and Metzenbaum scissors were used to dissect and amputate the graft proximally. This all–soft tissue graft was then shortened to approximately 8 cm in length and whipstitched in similar fashion on each end, and the final diameter was recorded. All grafts were 8 cm in length for biomechanical testing purposes.
Figure 1.

Gracilis and semitendinosus tendons whipstitched together before production of the final graft construct.
Figure 2.
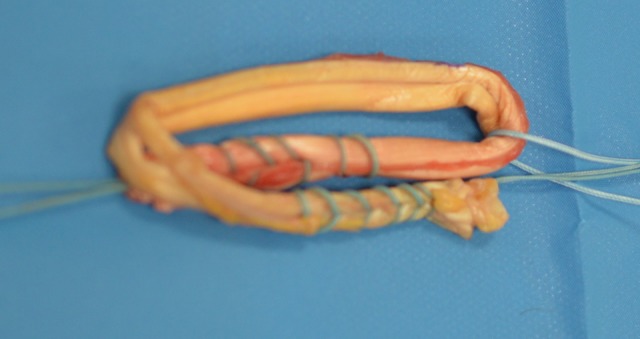
Additional suture added to loop tendons around to form a tripled 6-strand construct.
Figure 3.

Final 6-strand hamstring tendon construct before testing.
Biomechanical Testing
Cryogenic fixation techniques have been validated and commonly used for soft tissue biomechanical testing.16,17,21 The graft constructs were tested by use of an all-electric dynamic test load system (Instron E1000) using a previously published protocol (Figure 4).3 Constructs were fixed to the load system with Cryo-Grips (Arthrex) and preconditioned. A constant gauge length of 40 mm was used. The testing protocol included cyclic loading between 100 and 500 N for 100 cycles with 1-Hz frequency. After fatigue, there was a hold phase of 90 seconds for stress relaxation. After stress relaxation, the specimen was tested to failure with a 33-mm/s loading rate. We recorded ultimate load to failure (Figure 5); load at 3 mm of displacement, which represents clinical failure; and structural stiffness.
Figure 4.

Tendon construct testing with an all-electric dynamic test load system.
Figure 5.

Example of tendon rupture during ultimate load-to-failure testing.
Statistical Analysis
Standard force-elongation measurements were recorded. The mean values for ultimate load to failure, load at 3 mm of displacement, and structural stiffness for both tendon groups were compared by use of a 2-sided, paired t test. P < .05 was considered statistically significant. All data are reported as mean ± SD. A post hoc power analysis with 80% power, with the number of specimens we had, would be able to detect an 825-N difference.
Results
Results of biomechanical testing are included in Table 1.
TABLE 1.
Results of Biomechanical Testing
| Outcome | Hamstring Tendon, Mean ± SD | Quadriceps Tendon, Mean ± SD | Difference, Mean ± SE | P a |
|---|---|---|---|---|
| Diameter, mm | 11.3 ± 0.8 | 10.2 ± 0.4 | 1.2 ± 0.4 | .03 |
| Ultimate load, N | 2641 ± 662 | 2119 ± 143 | 522 ± 257 | .10 |
| Load at 3 mm of displacement, N | 1717 ± 582 | 1570 ± 326 | 147 ± 329 | .68 |
| Stiffness, N/mm | 1148 ± 339 | 809 ± 173 | 339 ± 122 | .04 |
aP values were determined by paired t test on the mean difference.
Graft Characteristics
Graft diameter was measured by use of a standard 0.5-mm incremental sizing block (Arthrex). After the HT was tripled, the mean diameter was 11.3 ± 0.8 mm (range, 10.5-12 mm). The mean diameter of the QT graft was 10.16 ± 0.41 mm (range, 9.5-10.5 mm). The difference between the grafts was found to be statistically significant (P = .03).
Ultimate Load to Failure
The ultimate load to failure was not significant between the 2 grafts. The ultimate load to failure was 2640.75 ± 662.19 and 2119.22 ± 143.26 N for the HT and QT grafts, respectively (P = .10).
Load at 3 mm of Displacement
No significant difference was found in load at 3 mm of displacement between the 2 grafts. The load at 3 mm of displacement was 1716.72 ± 582.07 and 1570.24 ± 325.50 N for the HT and QT grafts, respectively (P = .68).
Structural Stiffness
Stiffness is the deflection of the tested construct while subjected to a given load and is defined as the slope of the load-deformation curve.3 The stiffness was 1147.65 ± 339.22 and 808.65 ± 173.33 N/mm for the HT and QT grafts, respectively, which was statistically significant (P = .04).
Discussion
Our study found no significant differences in ultimate load to failure and load at 3 mm of displacement between the 6-strand HT and QT grafts, despite the larger average diameter of the HT. Load at 3 mm of displacement was used to simulate clinical failure. We did find that the stiffness of the HT graft was significantly greater than that of the QT graft. Ultimately, our hypothesis was refuted due to the difference in stiffness, but the clinical implications of this are unknown and discussed below.
Clinically, our findings likely represent similarly functioning grafts, as ultimate load to failure has often been considered the most critical biomechanical factor when choosing a graft because it represents the ability of a graft to withstand the anticipated load that initially caused the injury.4,13,19,20 Despite the older age of our cadaveric specimens (61.17 ± 10.38 years), the ultimate load to failure was similar for both of the grafts compared with the native ACL of patients aged 22 to 35 years, which was found to be 2160 ± 157 N.26,27 Also, both grafts were significantly more stiff than the native ACL, which has been documented to be 242 N/mm.26 Stiffness reflects the resistance to deformation of a structure. The clinical implications of this increased stiffness are unclear when ACL reconstructions are compared using grafts versus the native ACL.20 In comparison with previously studied graft constructs, quadrupled HT constructs have been studied before with respect to their biomechanical properties. Wilson et al25 found that the ultimate load to failure was 2422 N. This was slightly lower than the 6-strand HT construct in our study.
The 6-strand HT evolved due to the concern of small graft diameter after HT harvest.9,23 Traditionally, a longer HT graft construct has been necessary with transtibial tunnel preparation, thus requiring merely a doubling of the HT construct. Despite doubling of the graft, the potential remained for small-diameter grafts in some patients. Grafts less than 8 mm in diameter have been shown to have a higher rerupture rate.6 Multiple techniques have been described to address the issue of graft diameter, which typically requires shortening of the HT graft.9,24 However, with more anatomic tunnel preparation techniques, less HT graft length is required. Lee and Ganley9 described a 5-strand HT preparation where the semitendinosus was tripled and the gracilis tendon was doubled over this, producing a 5-strand construct. A modification of this technique was used in our study; both tendons were prepared together and then tripled, producing a 6-strand HT construct. Increasing the number of strands has been shown to produce increased stability on KT-1000 arthrometer testing and to result in improved International Knee Documentation Committee and Lysholm outcome scores.15,28 However, having enough graft length to allow for a 6-strand construct may not be possible if the patient is short or if the graft is prematurely amputated.
Graft diameter range was found to be more consistent within the QT grafts. This is due to the ability to choose the size of the graft harvesting device to set the diameter. As for the HT grafts, the patients’ anatomic features will dictate the final diameter depending on how the graft is prepared. In our practice, if a quadrupled (4-strand) HT graft is larger than 8 mm, the graft is prepared in this manner. If less than 8 mm, the graft is tripled over itself, producing the 6-strand graft evaluated in this study. The more consistent QT graft size may be desirable to surgeons who prefer a single, reproducible technique for graft harvest, tunnel preparation, and graft fixation. As for the differences in graft sizes above, we attempted to match the exact diameter of the QT, but several factors affect the final diameter. For example, if we chose an 11-mm QT harvester to match an 11-mm HT graft, we took a full-thickness, 11 mm–wide section of QT. This was then sized in a circular diameter sizer. The typical thickness of a QT is 7 to 8 mm. When QT is removed for use as a graft, it can be compressed and the diameter can be altered, so that the final graft is not necessarily 11 mm, depending on the compressibility of the graft. This ultimately can result in a different graft diameter; in our study, the QT grafts were 1 mm smaller in diameter compared with the HT grafts.
This study had some limitations. We had a relatively small sample size—6 grafts for each group. However, numerous other biomechanical studies of ACL grafts had similar sample sizes.3,8,19,20 The mean age of our specimens was 61 years; however, their biomechanical properties were similar to those of younger patients in previously published data.26,27 Another limitation was that our HT grafts were on average approximately 1 mm larger in diameter compared with the QT graft. This may affect the results; however, the smaller QT might strengthen the argument for using the QT graft, as it had similar biomechanical properties to the HT graft except for stiffness. In future studies, investigators can attempt to better match graft size, such as taking larger initial QT grafts and removing tissue as necessary to obtain grafts of similar size. Our study was performed with the help of industry funding, but this did not bias the results. We evaluated tendon biomechanical characteristics alone, rather than using any type of proprietary fixation technique. Last, our data are limited because they pertain to only the biomechanical properties of each tendon at time zero. Overall, future research is needed to expand upon this initial study with larger sample sizes and to ultimately compare clinical outcomes in patients.
Conclusion
This is the first study to directly compare the biomechanical properties of the 6-strand HT graft with a matched QT related to ACL reconstruction. The 6-strand HT graft and the QT graft had similar biomechanical properties with respect to ultimate load to failure and load to failure at 3 mm of displacement in 6 matched cadaveric specimens. Both grafts tested were significantly more stiff than the native ACL, with the HT construct being significantly stiffer than the QT. Therefore, we conclude that the QT graft is a reliable alternative to a 6-strand HT graft for ACL reconstruction.
Acknowledgment
The authors thank Matin Lendhey (Arthrex) for his help testing the grafts’ biomechanical properties. We also thank Dr Michael Gottschalk for assistance with statistical analysis.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Arthrex provided the cadaveric specimens as well as equipment and instrumentation for graft preparation and biomechanical testing. R.U. has received educational support from Smith & Nephew. S.K. has received educational support from Arthrex and consulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. American Academy of Orthopaedic Surgeons. Allografts for ACL Reconstruction Survey Report. Rosemont, IL: American Academy of Orthopaedic Surgeons, Department of Research and Scientific Affairs; 2013. [Google Scholar]
- 2. Bonamo JJ, Krinick RM, Sporn AA. Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction: a report of two cases. J Bone Joint Surg Am. 1984;66(8):1294–1297. [PubMed] [Google Scholar]
- 3. Broadhead ML, Singla AA, Bertollo N, Broe D, Walsh WR. A biomechanical comparison of 4-strand and 5-strand anterior cruciate ligament graft constructs. Orthop Rev (Pavia). 2017;9(1):6989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg Am. 1980;62(2):259–270. [PubMed] [Google Scholar]
- 5. Christen B, Jakob RP. Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg Br. 1992;74(4):617–619. [DOI] [PubMed] [Google Scholar]
- 6. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. [DOI] [PubMed] [Google Scholar]
- 7. Hurley ET, Calvo-Gurry M, Withers D, Farrington SK, Moran R, Moran CJ. Quadriceps tendon autograft in anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2018;34(5):1690–1698. [DOI] [PubMed] [Google Scholar]
- 8. Kim D, Asai S, Moon CW, et al. Biomechanical evaluation of anatomic single- and double-bundle anterior cruciate ligament reconstruction techniques using the quadriceps tendon. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):687–695. [DOI] [PubMed] [Google Scholar]
- 9. Lee RJ, Ganley TJ. The 5-strand hamstring graft in anterior cruciate ligament reconstruction. Arthrosc Tech. 2014;3(5):e627–e631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 11. Marshall JL, Warren RF, Wickiewicz TL, Reider B. The anterior cruciate ligament: a technique of repair and reconstruction. Clin Orthop Relat Res. 1979;143:97–106. [PubMed] [Google Scholar]
- 12. Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective, part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1467–1482. [DOI] [PubMed] [Google Scholar]
- 13. Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66(3):344–352. [PubMed] [Google Scholar]
- 14. Oh YK, Kreinbrink JL, Ashton-Miller JA, Wojtys EM. Effect of ACL transection on internal tibial rotation in an in vitro simulated pivot landing. J Bone Joint Surg Am. 2011;93(4):372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Prodromos CC, Joyce B. 5-strand hamstring ACL reconstruction: a new-technique with better long-term stability vs 4 strand. Arthroscopy. 2006;22:e7. [Google Scholar]
- 16. Riemersa DJ, Schamhardt HC. The cryo-jaw, a clamp designed for in vitro rheology studies of horse digital flexor tendons. J Biomech. 1982;15(8):619–620. [DOI] [PubMed] [Google Scholar]
- 17. Rincon L, Schatzmann L, Brunner P, et al. Design and evaluation of a cryogenic soft tissue fixation device—load tolerances and thermal aspects. J Biomech. 2001;34(3):393–397. [DOI] [PubMed] [Google Scholar]
- 18. Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17(6):760–765. [DOI] [PubMed] [Google Scholar]
- 19. Sasaki N, Farraro KF, Kim KE, Woo SL. Biomechanical evaluation of the quadriceps tendon autograft for anterior cruciate ligament reconstruction: a cadaveric study. Am J Sports Med. 2014;42(3):723–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shani RH, Umpierez E, Nasert M, Hiza EA, Xerogeanes J. Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(1):71–75. [DOI] [PubMed] [Google Scholar]
- 21. Sharkey NA, Smith TS, Lundmark DC. Freeze clamping musculo-tendinous junctions for in vitro simulation of joint mechanics. J Biomech. 1995;28(5):631–635. [DOI] [PubMed] [Google Scholar]
- 22. Slone HS, Romine SE, Premkumar A, Xerogeanes JW. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31(3):541–554. [DOI] [PubMed] [Google Scholar]
- 23. Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(11):1945–1949. [DOI] [PubMed] [Google Scholar]
- 24. Vinagre G, Kennedy NI, Chahla J, et al. Hamstring graft preparation techniques for anterior cruciate ligament reconstruction. Arthrosc Tech. 2017;6(6):e2079–e2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wilson TW, Zafuta MP, Zobitz M. A biomechanical analysis of matched bone patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med. 1999;27(2):202–207. [DOI] [PubMed] [Google Scholar]
- 26. Woo SL, Debski RE, Withrow JD, Janaushek MA. Biomechanics of knee ligaments. Am J Sports Med. 1999;27(4):533–543. [DOI] [PubMed] [Google Scholar]
- 27. Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex: the effects of specimen age and orientation. Am J Sports Med. 1991;19(3):217–225. [DOI] [PubMed] [Google Scholar]
- 28. Zhao J, He Y, Wang J. Double-bundle anterior cruciate ligament reconstruction: four versus eight strands of hamstring tendon graft. Arthroscopy. 2007;23(7):766–770. [DOI] [PubMed] [Google Scholar]


