Abstract
Background:
Adherence to medication is important for control of blood pressure (BP) and prevention of its complications. Identifying factors which improve adherence to treatment helps in improving cardiovascular outcome.
Aim:
The aim is to study the adherence of hypertensive patients to medication using modified medication adherence scale (MMAS).
Materials and Methods:
This study was done as a cross-sectional study in the Department of General medicine in Aarupadai Veedu Medical College and Hospital, Puducherry, from May 2017 to October 2017. All adult patients of both sexes diagnosed to have hypertension were included in the study after obtaining informed consent. Adherence to hypertension was assessed using MMAS and results were analyzed. SPSS 22 software (International Business Machines Corporation, Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY) was used for statistical purposes.
Results:
A total of 150 patients were included in the study. There were 83 males and 67 females in the study. Good adherence was observed in 74 (49%) out of the total 150. Forty-nine (59%) males and 25 (37%) females were found adherent to treatment. Patients with monotherapy had a good adherence compared to those with polytherapy. Patients with good adherence had a good control of BP.
Conclusion:
MMAS is a simple and useful tool for assessing medication adherence among hypertensive patients.
Keywords: Adherence, blood pressure, hypertension, modified medication adherence scale
INTRODUCTION
Mean systolic blood pressure (BP) of more than 140 mmHg or above, mean diastolic pressure of 90 mm Hg or above, defines hypertension.[1] Hypertension doubles the risk of cardiovascular diseases, including coronary heart disease, congestive heart failure, ischemic and hemorrhagic stroke, renal failure, and peripheral arterial disease. It is often associated with additional cardiovascular risk factors and the risk of cardiovascular disease increases with the total burden of risk factors.[2] Poor adherence is associated with higher residual cardiovascular risk and a high health-care burden.[3] In approximately half of the cases, uncontrolled hypertension has been attributed to patients failure to follow properly a prescribed drug regimen.[4]
MATERIALS AND METHODS
This cross-sectional single-visit study was done in Aarupadai Veedu Medical College and Hospital, Puducherry, from May 2017 to October 2017. Informed consent was obtained from all patients before the study. All adult patients above the age of 18 years attending hypertension clinic in the department of General Medicine diagnosed to have hypertension according to JNC-7[1] for at least 1 year were included in the study. Pregnant patients and those diagnosed to have secondary hypertension were excluded. Detailed information regarding age, number of drugs taken, duration of hypertension, smoking history, presence of diabetes, and presence of medication side effects was noted. Body mass index (BMI) was measured and inquiry about knowledge of BP goal (<140/90 mmHg[1] as per JNC-7) was made. BP (both systolic and diastolic) was measured using standard mercury sphygmomanometer in the right upper limb in sitting position. Adherence to hypertensive treatment was analyzed using modified medication adherence scale (MMAS)[5] consisting of seven questions, derived from two different adherence questionnaires, the Hill–Bone adherence,[6] in which three important behavioral domains of high BP treatment are assessed to BP scale and the 8-item Morisky Medication Adherence Scale,[7] most commonly used to assess adherence of patients.
Each question in the MMAS has a 4-point response format. Each response carries a score: all the time = 1, most of the time = 2, some of the time = 3, none of the time = 4. Total scores of each patient are added. Total scores can extend from 7 to 28. Higher scores indicate good adherence to medication therapy. A full score of 28 or score of 27 (due to 1 point deducted from either question 1 or 6) was defined as adherence. A score of 26 or lower was defined as nonadherence.[5]
RESULTS
Age group of patients ranged from 40 to 76 years. There were 51 (34%) in the age group 30–49 years and 72 (48%) patients in the age group 50–59 years [Table 1]. Eighty-three patients were male and 67 were female. A total of 62 patients (41.3%) had knowledge of BP goal and 64 patients (42.7%) were treated with a single drug, 77 patients (51.3%) with two drugs, and 6% with three drugs. Diabetes was present in 22 patients (14.7%). Side effects due to medication were present in 22 (14.7%) and dizziness was the most common side effect reported. Smoking history was present in 20 (13.3%) patients. Mean duration of hypertension was 5.9 years. Mean BMI was 25.5 and mean systolic and diastolic BPs were 128.9 and 80.17, respectively [Table 2]. Based on the patient's responses to the MMAS scores, a total of 74 patients which included 49 males and 25 females were found adherent to treatment [Table 3].
Table 1.
Age distribution of patients studied
| Age (years) | Number of patients (%) |
|---|---|
| 30-49 | 51 (34) |
| 50-59 | 72 (48) |
| 60-69 | 19 (12.7) |
| ≥70 | 8 (5.3) |
| Total | 150 (100) |
Table 2.
Mean and standard deviation of clinical parameters
| Clinical parameters | Mean±SD |
|---|---|
| BMI | 25.587±1.872 |
| Duration of hypertension | 5.9±2.618 |
| SBP | 128.907±4.155 |
| DBP | 80.173±2.741 |
SD=Standard deviation, BMI=Body mass index, SBP=Systolic blood pressure, DBP=Diastolic blood pressures
Table 3.
Adherence by sex of patients
| Sex | n | Mean adherence score | Adherers, frequency (%) | Nonadherers, frequency (%) |
|---|---|---|---|---|
| Male | 83 | 26.83 | 49 (59) | 34 (41) |
| Female | 67 | 25.63 | 25 (37.3) | 42 (62.7) |
| Total | 150 | 26.29 | 74 (49.3) | 76 (50.7) |
DISCUSSION
To achieve desired clinical outcomes, medication adherence is the key.[8] More than half of the patients (55.3%) were male in the present study. The age group of patients ranged from 40 to 76 years and mean age of the group was 52.84 ± 7.4. Among all patients, 68 (45.3%) had hypertension for <5 years. Only 6 (4%) patients had a duration of hypertension for more than 10 years. Most patients (68.6%) were overweight with a BMI of more than 24.9. The most important reason for uncontrolled BP is nonadherence to hypertensive medication.[9] Adherence estimates vary widely depending on the operational definition used.[10] In our study, which is the first Indian study done using MMAS for hypertension, 74 (49.3%) patients were found adherent to treatment which included 49 males and 25 females. The adherence rate of the present study is similar to study done in Malaysia and Korea[5,11] which reported an adherence rate 0f 53.4% and 49.7%, respectively. 44.1% were found adherent to treatment in a Chinese study[12] and 23.4% in another Indian study[13] done using Morisky Medication Adherence Scale. The difference in adherence in these two studies may be due to varied sociodemographic pattern of the two countries.[4] Males were found more adherent (59%) to treatment than females (37%) in the present study. This is in contrast to the previous Indian and Russian studies[4,13,14] done using Morisky Medication Adherence Scale, where good adherence was noticed in females compared to males. However, a study done in the UK[15] showed good adherence in males compared to females. Adherence rate was high among the age group 50–59 years (55.6%) as compared to those in the age group 40–49 years (52.9%) and poor adherence of 31.6% and 12.5% in the age groups 60–69 years and more than 70 years, respectively [Table 4]. Most common cause of nonadherence was forgetfulness followed by running out of medicines and improper intake during travel [Table 5]. A total of 55 (36.7%) had a full score of 28 in the adherence scale [Table 6]. Only 62 (41.3%) patients had a knowledge on BP goal and good adherence rate (82%) was observed among them compared to those without it (26%) reflecting the effect of education contributing to positive outcome [Table 7]. Majority of patients (69%) were on calcium channel blockers and only 16% were on diuretics [Figure 1]. More than half of the patients (51%) were on two drugs while only 6% were on three drugs. Good adherence rate was observed in those on a single drug (60.9%) while it was 42.9% and 22.2% in those on two and three drugs, respectively, suggesting decreasing rate of adherence with increasing number of drugs [Table 8]. These results are similar to the studies done earlier.[4,9,15] No particular drug class was associated with high adherence, as in the case of an earlier study.[15] A previous study[16] to assess the relation between drug class and adherence also showed similar results. Table 9 shows logistic regression analysis. Odds ratio suggesting by what multiplicative factor odds of adherence to medication increase per unit change of predictor variable. There was no significant association between duration of hypertension, BMI, and adherence rate. Presence of side effects due to medication also did not alter the adherence pattern [Table 10]. Adherence rate among diabetics was slightly less (45.5%) than that of nondiabetic (50%) [Table 11]. Strong beliefs of the necessity of medications and threatening views of illness substantially contribute to positive medication adherence.[17] Patients who were adherent to treatment had a lower mean values of systolic (77.8) and diastolic BP (125.6) as compared to nonadherers with values of 82.3 and 132, respectively, suggesting good control of hypertension associated with adherence [Table 12]. Good adherence improved hypertension control in our study, which was similar to a study done in Kolkata, India which showed good adherers had 1.71 times more chance of adequate control of hypertension compared to those who were nonadherent.[18] However, in the previous study,[18] patients with long duration of hypertension had a good adherence in contrary to the present study.
Table 4.
Adherence by age of patients
| Age category (years) | n | Mean adherence score | Adherers, frequency (%) | Nonadherers, frequency (%) |
|---|---|---|---|---|
| 30-49 | 51 | 26.49 | 27 (52.9) | 24 (47.1) |
| 50-59 | 72 | 26.49 | 40 (55.6) | 32 (44.4) |
| 60-69 | 19 | 25.37 | 6 (31.6) | 13 (68.4) |
| ≥70 | 8 | 25.5 | 1 (12.5) | 7 (87.5) |
| Total | 150 | 26.29 | 74 (49.3) | 76 (50.7) |
Table 5.
Adherence scores in modified medication adherence scale
| Questions | Adherence score, frequency (%) |
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| How often do you forget to take your medicine? | 0 | 0 | 52 (34.7) | 98 (65.3) |
| How often do you decide not to take your medicine? | 0 | 1 (0.7) | 13 (8.7) | 136 (90.7) |
| How often do you miss taking your medicine because you feel better? | 0 | 0 | 8 (5.3) | 142 (94.7) |
| How often do you decide to take less of your medicine? | 0 | 0 | 15 (10) | 135 (90) |
| How often do you stop taking your medicine because you feel sick due to effects of the medicine? | 0 | 0 | 4 (2.7) | 146 (97.3) |
| How often do you forget to bring along your medicine when you travel away from home? | 4 (2.7) | 13 (8.7) | 46 (30.7) | 87 (58) |
| How often do you not take you medicine because you run out of them at home? | 0 | 14 (9.3) | 50 (33.3) | 86 (57.3) |
Table 6.
Frequency distribution of adherers and nonadherers (n=150)
| Adherence score | Adherence status | Frequency, n (%) |
|---|---|---|
| Full score (28) | Adherers | 55 (36.7) |
| 27 (one point deducted from either question 1 or 6) | Adherers | 19 (12.7) |
| 27 (one point deducted due to other questions) | Nonadherers | 9 (6) |
| 23-26 | Nonadherers | 62 (41.3) |
| 19-22 | Nonadherers | 5 (3.3) |
| 7-19 | Nonadherers | 0 |
| Total | 150 (100) | |
Table 7.
Adherence by knowledge of blood pressure
| Knowledge of BP goal | n | Mean adherence score | Adherers, frequency (%) | Nonadherers, frequency (%) |
|---|---|---|---|---|
| Yes | 62 | 27.53 | 51 (82.3) | 11 (17.7) |
| No | 88 | 25.42 | 23 (26.1) | 65 (73.9) |
| Total | 150 | 26.29 | 74 (49.3) | 76 (50.7) |
BP=Blood pressure
Figure 1.
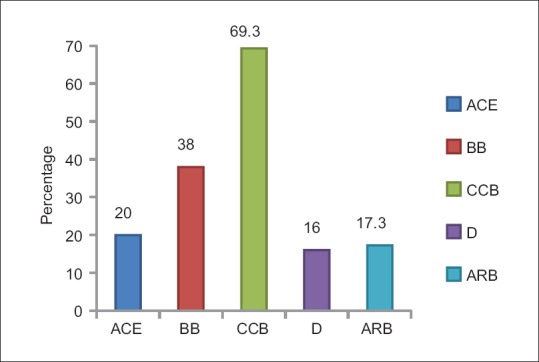
Distribution by drug group. ACEI-Angiotensin converting enzyme inhibitors, BB-Beta blockers, CCB-Calcium channel blockers, D-Diuretics, ARB-Angiotensin receptor blockers
Table 8.
Adherence by number of drug taken by patients
| Number of drug taken | n | Mean adherence score | Adherers, frequency (%) | Nonadherers, frequency (%) |
|---|---|---|---|---|
| 1 | 64 | 26.77 | 39 (60.9) | 25 (39.1) |
| 2 | 77 | 26.04 | 33 (42.9) | 44 (57.1) |
| 3 | 9 | 25.11 | 2 (22.2) | 7 (77.8) |
| Total | 150 | 26.29 | 74 (49.3) | 76 (50.7) |
Table 9.
Logistic regression for factors predicting medication adherence
| Predictor variables | OR | 95% of CI | P |
|---|---|---|---|
| Age | 1.120 | 1.028-1.219 | 0.009* |
| Sex | |||
| Male | 1.000 | 0.148-0.873 | 0.24* |
| Female | 0.359 | ||
| Number of drugs currently taken | 2.555 | 1.146–5.694 | 0.022* |
| Presence of diabetes | |||
| Yes | 1.000 | 0.122–1.632 | 0.223 |
| No | 0.447 | ||
| Presence of side effects | |||
| Yes | 1.000 | 0.225–3.86 | 0.923 |
| No | 0.933 | ||
| Knowledge of BP goal | |||
| Yes | 1.000 | 0.024–0.158 | <0.001* |
| No | 0.062 | ||
| BMI | 0.842 | 0.645–1.101 | 0.209 |
| Duration of hypertension | 0.949 | 0.78–1.156 | 0.604 |
*Significant. OR=Odds ratio, CI=Confidence interval, BMI=Body mass index, BP=Blood pressure
Table 10.
Adherence by the presence of side effects in patients
| Presence of side effects | n | Mean adherence score | Adherers, frequency (%) | Nonadherers, frequency (%) |
|---|---|---|---|---|
| Yes | 22 | 25.55 | 8 (36.4) | 14 (63.6) |
| No | 128 | 26.42 | 66 (51.6) | 62 (48.4) |
| Total | 150 | 26.29 | 74 (49.3) | 76 (50.7) |
Table 11.
Adherence by the presence of diabetes in patients
| Presence of diabetes | n | Mean adherence score | Adherers, frequency (%) | Nonadherers, frequency (%) |
|---|---|---|---|---|
| Yes | 22 | 25.95 | 10 (45.5) | 12 (54.5) |
| No | 128 | 26.35 | 64 (50) | 64 (50) |
| Total | 150 | 26.29 | 74 (49.3) | 76 (50.7) |
Table 12.
Blood pressure in adherers and nonadherers
| Adherence status | Mean DBP±SD | Mean SBP±SD |
|---|---|---|
| Adherers | 77.89±1.361 | 125.68±2.71 |
| Nonadherers | 82.39±1.1729 | 132.05±2.612 |
| Total | 80.17±2.741 | 128.91±4.155 |
SD=Standard deviation, SBP=Systolic blood pressure, DBP=Diastolic blood pressures
CONCLUSION
MMAS is a simple and useful tool for assessing medication adherence among hypertensive patients. Good adherence is the cornerstone for optimum control of BP. Overall medication adherence in the present study was 49.3%. Hypertensive patients on multiple drugs have poor adherence. Knowledge on the level of BP goal is associated with good adherence.
Ethical approval
The study was approved by the Institutional Ethics Committee.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's principles of internal medicine. 19th edition. New York: McGraw Hill Education; 2015. p. 1611. [Google Scholar]
- 3.de Jager RL, van Maarseveen EM, Bots ML, Blankestijn PJ SYMPATHY Investigators. Medication adherence in patients with apparent resistant hypertension: Findings from the SYMPATHY trial. Br J Clin Pharmacol. 2018;84:18–24. doi: 10.1111/bcp.13402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venkatachalam J, Abrahm SB, Singh Z, Stalin P, Sathya GR. Determinants of patient's adherence to hypertension medications in a rural population of Kancheepuram district in Tamil Nadu, South India. Indian J Community Med. 2015;40:33–7. doi: 10.4103/0970-0218.149267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence. 2012;6:613–22. doi: 10.2147/PPA.S34704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2000;15:90–6. doi: 10.1111/j.1751-7117.2000.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 7.de Oliveira-Filho AD, Morisky DE, Neves SJ, Costa FA, de Lyra DP., Jr The 8-item Morisky medication adherence scale: Validation of a Brazilian-Portuguese version in hypertensive adults. Res Social Adm Pharm. 2014;10:554–61. doi: 10.1016/j.sapharm.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Khayyat SM, Khayyat SM, Hyat Alhazmi RS, Mohamed MM, Abdul Hadi M. Predictors of medication adherence and blood pressure control among Saudi hypertensive patients attending primary care clinics: A Cross-sectional study. PLoS One. 2017;12:e0171255. doi: 10.1371/journal.pone.0171255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmieder RE, Ott C, Schmid A, Friedrich S, Kistner I, Ditting T, et al. Adherence to antihypertensive medication in treatment-resistant hypertension undergoing renal denervation. J Am Heart Assoc. 2016;5:pii: e002343. doi: 10.1161/JAHA.115.002343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hude KT, Rabi QD. Measuring medication adherence: Standardized definitions are needed to allow for comparisons. Int J Popul Data Sci. 2017;1:40. [Google Scholar]
- 11.Bae SG, Jeon HJ, Yang HS, Kim BK, Park KS. Medication Adherence and its Predictors in Community Elderly Patients with Hypertension. Korean J Health Promot. 2015;15:121–8. [Google Scholar]
- 12.Lo SH, Chau JP, Woo J, Thompson DR, Choi KC. Adherence to antihypertensive medication in older adults with hypertension. J Cardiovasc Nurs. 2016;31:296–303. doi: 10.1097/JCN.0000000000000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah AJ, Singh V, Patil SP, Gadkari MR, Ramchandani V, Doshi KJ. Factors Affecting Compliance to Antihypertensive Treatment among Adults in a Tertiary Care Hospital in Mumbai. Indian Journal of Community Medicine. 2018;43(1):53–55. doi: 10.4103/ijcm.IJCM_40_17. doi:10.4103/ijcm.IJCM_40_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Efanov A. Predictors of antihypertensive medical treatment adherence decline. Eur Heart J. 2017;38(Supp 1.ehx501):193. [Google Scholar]
- 15.Ghembaza M.A, Senoussaoui Y, KendouciTani M, Meguenni K. Impact of Patient Knowledge of Hypertension Complications on Adherence to Antihypertensive Therapy. Current Hypertension Reviews. 2014;10:41–48. doi: 10.2174/157340211001141111160653. [DOI] [PubMed] [Google Scholar]
- 16.Moise N, Schwartz J, Bring R, Shimbo D, Kronish IM. Antihypertensive drug class and adherence: An electronic monitoring study. Am J Hypertens. 2015;28:717–21. doi: 10.1093/ajh/hpu199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: Evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. 2014;20:58–65. doi: 10.18553/jmcp.2014.20.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhandari S, Sarma PS, Thankappan KR. Adherence to antihypertensive treatment and its determinants among urban slum dwellers in Kolkata, India. Asia Pac J Public Health. 2015;27:NP74–84. doi: 10.1177/1010539511423568. [DOI] [PubMed] [Google Scholar]


