Key Points
Question
What is the epidemiologic pattern of firearm-related ocular trauma in the pediatric population in the United States?
Findings
In this analysis of 1972 firearm-related ocular injuries recorded in the National Trauma Data Bank, almost a quarter of all such injuries between 2008 and 2014 occurred in the pediatric population, mostly among male adolescents 12 to 18 years of age. Although most firearm-related ocular injuries occurred in white patients, male black adolescents were represented disproportionately.
Meaning
The study findings suggest that pediatric firearm-related ocular injuries may be associated with substantial morbidity and mortality; identifiable risk factors in vision loss among children included race/ethnicity, sex, and age group.
This study evaluates the epidemiologic patterns of firearm-related ocular injuries among children and adolescents in the United States, using multiyear demographic, hospitalization, and clinical data reported in the National Trauma Data Bank.
Abstract
Importance
Gun violence represents a substantial public health issue, and firearm-related injuries rank second among the causes of injury-related deaths in children aged 0 to 17 years in the United States. Ocular trauma from firearm-related injuries can lead to devastating vision loss, but little is known to date about the specific demographics and characteristics of such injuries in children.
Objective
To evaluate the epidemiologic pattern of pediatric firearm-related ocular injuries.
Design, Setting, and Participants
This retrospective analysis used deidentified data from the National Trauma Data Bank, the largest national registry of hospitalized trauma cases in the United States. The firearm-related ocular injuries (n = 1972) of pediatric patients (defined as those younger than 21 years) hospitalized between January 1, 2008, and December 31, 2014, were analyzed. Statistical analyses were conducted from July 15, 2017, to June 15, 2019.
Exposure
Firearm-related ocular trauma.
Main Outcomes and Measures
Pediatric patients with firearm-related ocular injuries were identified using International Classification of Diseases, Ninth Revision, Clinical Modification codes and external causes of injury codes. Patient demographics (age, sex, and race/ethnicity), type of ocular injury, injury intent, geographic location, length of hospital admission, health insurance status, disposition at discharge, Injury Severity Score (ISS), and Glasgow Coma Scale (GCS) score were collected.
Results
A total of 8715 firearm-related ocular injuries were identified. Of these injuries, 1972 (22.6%) occurred in pediatric patients, most of whom were male (1678 [85.1%]) and adolescents (1037 [52.6%]), with a mean (SD) age of 15.2 (5) years. Common locations of injury were home (761 [38.6%]) and street (490 [24.8%]). Mean (SD) hospital length of stay was 7.6 (12) days, ISS was 16 (13.1), and GCS score was 11 (5.1). The most common types of firearm-related ocular injuries were open wound of the eyeball (820 [41.6%]) and ocular adnexa (502 [25.5%]), orbital injuries or fractures (591 [30.0%]), and contusion of the eye or adnexa (417 [21.1%]). Patients aged 0 to 3 years had greater odds of unintentional injuries (odds ratio [OR], 4.41; 95% CI, 2.51-7.75; P < .001) and injuries occurring at home (OR, 5.39; 95% CI, 2.81-10.38; P < .001), and those aged 19 to 21 years had greater odds of assault injuries (OR, 2.17; 95% CI, 1.77-2.66; P < .001) and injuries occurring on the street (OR, 1.61; 95% CI, 1.3-1.98; P < .001). Black patients had the greatest odds of having injuries with assault intention (OR, 4.53; 95% CI, 3.68-5.59; P < .001), and white patients had the greatest likelihood for self-inflicted injury (OR, 7.1; 95% CI, 5.92-9.51; P < .001). Traumatic brain injury resulted mostly from self-inflicted trauma (OR, 5.99; 95% CI, 4.16-8.63; P < .001), as did visual pathway injuries (OR, 2.86; 95% CI, 1.95-4.20; P < .001). The inpatient mortality rate was 12.2%.
Conclusions and Relevance
This study found that pediatric firearm-related ocular injuries from 2008 through 2014 were predominantly sight-threatening and associated with traumatic brain injury. If the possible risk factors, including sex, age, race/ethnicity, and injury intention, can be confirmed for 2015 through 2019, these findings may be useful in developing strategies to prevent pediatric firearm-related ocular injuries.
Introduction
The United States far outranks other countries in firearm-related mortality. Data from 2010 show that, compared with other affluent countries, this country has a 25.2 times higher gun-related homicide rate, 8.0 times higher gun-related suicide rate, and 6.2 times higher gun-related unintentional death rate.1 Ninety-one percent of all children worldwide aged 0 to 14 years who died from firearm injuries were from the United States.1 Injury from firearms represents the third leading cause of death and the second leading cause of injury-related deaths among children aged 0 to 17 years.2 From 2012 to 2014, almost 5790 children received medical attention in an emergency department (ED) for and 1300 children died of firearm-related injuries.3 Accessibility to firearms may play a role in these statistics. In 2013, Carter et al4 found that almost 25% of pediatric patients with assault injury who presented to a level 1 trauma center ED reported firearm possession within the past 6 months; only 17% of these patients had obtained the guns legally.
As illustrated by the preceding statistics, gun violence poses a serious public health problem, especially for the pediatric population. It leads to acute hospitalizations and chronic disability that consume medical resources and taxpayer dollars. About 40% of firearm-related injuries in children require hospitalization to the intensive care unit, with 50% to 69% of these patients undergoing surgical intervention.5 It has been estimated that, annually, approximately 3200 children in the United States with a firearm-related injury sustain a chronic disability.5 The US lifetime medical and work loss costs associated with firearm injuries and deaths have been estimated at more than $48 billion annually.6
In addition, violence has psychological implications for younger populations. Children exposed to violence in general are likely to have intrusive thinking, anxiety, and depression.7
The eye and visual pathways are susceptible to trauma. Injury leading to visual impairment may have an association with childhood development. Children are already vulnerable in cognitive, motor, and social development, and their risk for delayed learning, limitations in skills acquisition, and impaired social relationships increases with visual impairment.8 Children who are visually impaired have lower quality-of-life scores compared with their peers.9 Therefore, risk factors in vision loss in the young, such as trauma and gun violence, should be addressed to prevent developmental consequences.
Strategies for violence and gun prevention have been postulated, including environmental, legal, and public health modifications.10,11 However, to prevent injury and reduce the public health burden from firearm trauma, we need to gather and assess the data on this topic. Previous studies have addressed specific characteristics of paintball- and pellet gun–associated ocular injuries in the pediatric population.12,13,14 Few studies to date have dealt with powder-firearm injuries.15
The present study sought to evaluate the epidemiologic patterns of firearm-related ocular injuries in children, using available data from a national registry. We focused on visually impairing injury because visual development is most critical during childhood. Findings from this study may help improve the understanding of the risk factors associated with pediatric firearm-related ocular injuries and reduce the risk of devastating vision loss from such injuries.
Methods
This retrospective study was approved by the institutional review board at the Albert Einstein College of Medicine. Informed consent was waived because the study used deidentified data from the National Trauma Data Bank (NTDB). Only patients who were admitted, including ED admissions, were included in this study. The NTDB, established by the American College of Surgeons, is the largest national registry of hospitalized trauma cases, with submissions from more than 900 US facilities.16 It was designed to centralize data for trauma research in the United States.17 Access to the NTDB is provided on request to the American College of Surgeons.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes and external causes of injury (E) codes were used to identify pediatric patients who were hospitalized after sustaining firearm-related trauma with associated ocular injuries between January 1, 2008, and December 31, 2014. Injuries from firearms, including automatic shotguns, hunting rifles, handguns, and military firearms, were divided by injury intention according to ICD-9-CM E codes: unintentional (E922.0-E922.9), assault (E965.0-E965.4), self-inflicted (E955.0-E955.9), legal intervention (E970.0), and undetermined (E985.0-E985.4).18 Pediatric patients were defined as younger than 21 years, per the guidelines published by the US federal government and the American Academy of Pediatrics.19,20,21 Ocular injuries were grouped by ICD-9-CM code categories: open wound of the ocular adnexa (870.0-870.9), open wound of the eyeball (871.0-871.7 and 871.9), superficial injury of the eye and adnexa (918.0-918.2 and 918.9), contusion of the eye and adnexa (921.0-921.4, 921.9, 364.0-364.1, and 364.3), foreign body on external eye (930.0-930.2 and 930.8-930.9), burn to the eye and adnexa (940.0-940.5 and 940.9), injury to the optic nerve or visual pathways (950.0-950.3 and 950.9), cranial nerve injury other than optic nerve (951.0-951.4 and 951.9), and orbital injuries (802.6-802.9 and 376.32-376.33). Patients were identified as having traumatic brain injury (TBI) on the basis of Centers for Disease Control and Prevention criteria22 and ICD-9-CM codes: skull fracture (800.0-801.9 and 803.0-804.9), intracranial injury (850.0-854.1), injury to optic chiasm, optic pathway, or visual cortex (950.1-950.3), and head injury not otherwise specified (959.01). All subclassifications of injuries within each primary diagnostic code were included in the data extraction.
We documented age, sex, race/ethnicity, types of ocular injury, intent of injury, length of admission, health insurance coverage, level of hospital trauma service (levels I-IV, both American College of Surgeons–verified and state-designated centers), disposition on discharge, and geographic location and US census region (Northeast, West, Midwest, and South) of trauma. Injury Severity Score (ISS) and Glasgow Coma Scale (GCS) score by emergency medical services and on arrival to the ED also were documented. The ISS is a numerical value, from 0 to 75, determined by an injury’s anatomical location and severity, with scores above 15 designated as major trauma and highest scores indicating severe injury. The GCS assesses the level of consciousness after a head injury, with values ranging from 3 to 15 and lowest scores indicating greater levels of TBI. Inpatient mortality rate was determined by examining the disposition data, including home discharge, transfer to another hospital, transfer to a nursing home, transfer to a rehabilitation facility, leaving against medical advice, and death on discharge.
Statistical Analysis
The mean (SD) and median (interquartile range [IQR]) were calculated for all continuous variables. These variables were grouped into categories to facilitate statistical analysis. Children were divided into developmental age groups of 0 to 3, 4 to 6, 7 to 11, 12 to 18, and 19 to 21 years. The ISSs were categorized according to the NTDB subclassifications of minor (ISS = 1-8), moderate (ISS = 9-15), severe (ISS = 16-24), and very severe (ISS>24). The GCS scores were categorized into mild (GCS = 13-15), moderate (GCS = 9-12), and severe (GCS<8) TBI. The GCS scores from the ED were used in descriptive and analytical calculations.
Categorized data were analyzed for associations between variables, using the paired, 2-tailed t test and χ2 tests. Univariate logistic regression analysis was conducted to identify relative associations, which were expressed in odds ratios (ORs), 95% CIs, and 2-tailed P values. Statistical significance was set at P < .05. Descriptive and analytical calculations were performed using SPSS software, version 24 (IBM Corp). Graphs and tables were constructed using Excel and Word (Microsoft Corp). Cases with characteristics classified as unknown or undetermined were excluded from analyses. Statistical analyses were conducted from July 15, 2017, to June 15, 2019.
Results
Descriptive Characteristics
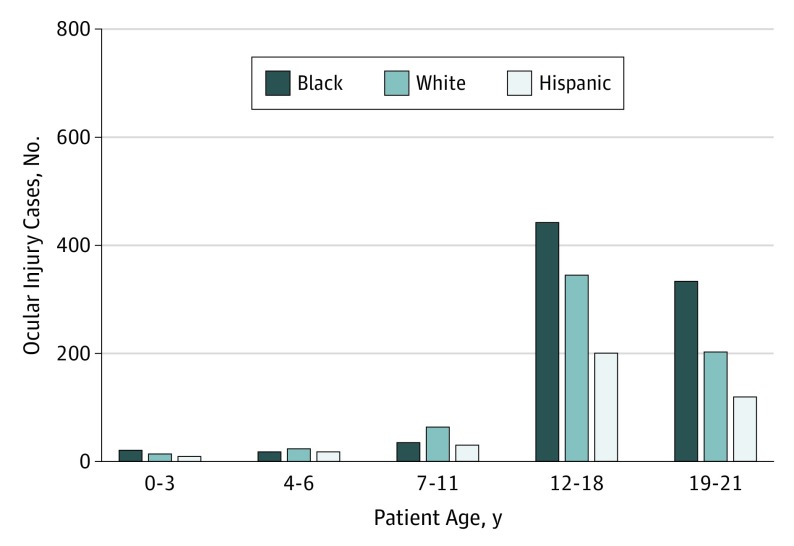
Between 2008 and 2014, a total of 8715 firearm-related ocular injuries were identified, of which 1972 (22.6%) occurred in pediatric patients. The Table provides a summary of the general characteristics of the patients and their injuries. A mean frequency of 282 injuries occurred annually, and most patients with such injuries presented to level I (829 [42.0%]) and level II (304 [15.4%]) trauma centers. Most patients (1037 [52.6%]) were adolescents (aged 12-18 years), and the mean (SD) age by sex was 15.2 (5) years in males and 16.4 (4.1) years in females. Male patients represented 85.1% (n = 1678) of those with firearm-related ocular injuries and outnumbered female patients (294 [14.9%]) in all age groups. The racial/ethnic breakdown was 851 black (43.2%), 651 white, (33%), 372 Hispanic (18.9%), and 470 other (23.8%) patients (Figure 1).
Table. Descriptive Findings and Demographic Data of Pediatric Patients With Firearm-Related Ocular Trauma, 2008-2014.
| Variable | No. (%) |
|---|---|
| Age, y | |
| Mean (SD) | 16.2 (4.3) |
| Median (IQR) | 18 (15-19) |
| 0-3 | 51 (2.6) |
| 4-6 | 58 (2.9) |
| 7-11 | 138 (7.0) |
| 12-18 | 1037 (52.6) |
| 19-21 | 688 (34.9) |
| Sex | |
| Male | 1678 (85.1) |
| Female | 294 (14.9) |
| Race/ethnicity | |
| White | 651 (33.0) |
| Black | 851 (43.2) |
| Hispanic | 372 (18.9) |
| Other | 470 (23.8) |
| Year of injury | |
| 2008 | 268 (13.6) |
| 2009 | 316 (16.0) |
| 2010 | 278 (14.1) |
| 2011 | 273 (13.8) |
| 2012 | 283 (14.4) |
| 2013 | 269 (13.6) |
| 2014 | 285 (14.5) |
| Common injury type | |
| Contusion of the eye or adnexa | 417 (21.1) |
| Orbital fracture | 591 (30.0) |
| Open wound of the ocular adnexa | 502 (25.5) |
| Superficial | 167 (8.5) |
| Open wound of the eyeball | 820 (41.6) |
| Optic nerve or visual pathway | 151 (7.7) |
| Related cranial nerves | 107 (5.4) |
| Retinal edema | 192 (9.7) |
| TBI | 1091 (55.3) |
| Intention of injury | |
| Unintentional | 346 (17.5) |
| Assault | 1241 (62.9) |
| Self-inflicted | 258 (13.1) |
| Unknown or undetermined | 127 (6.4) |
| Type of discharge | |
| Home | 1119 (56.7) |
| Transfer to another hospital | 89 (4.5) |
| Nursing home | 55 (2.8) |
| Rehabilitation facility | 141 (7.2) |
| Left against medical advice | 4 (0.2) |
| Unknown | 324 (16.4) |
| ISS | |
| Mean (SD) | 16 (13.1) |
| Median (IQR) | 14 (4-25) |
| ≤15 | 1004 (50.9) |
| 16-24 | 332 (16.8) |
| >24 | 534 (27.1) |
| Unknown | 102 (5.2) |
| GCS score | |
| Mean (SD) | 11 (5.2) |
| Median (IQR) | 15 (4-15) |
| ≤8 | 591 (30.0) |
| 9-12 | 88 (4.5) |
| 13-15 | 1144 (58.0) |
| Unknown | 149 (7.6) |
| Hospital LOS, d | |
| Mean (SD) | 7.6 (12) |
| Median (IQR) | 3 (1-9) |
| 1 | 641 (32.5) |
| 2-3 | 442 (22.4) |
| 4-6 | 289 (14.7) |
| >6 | 596 (30.2) |
| Inpatient mortality | 240 (12.2) |
| Common locations | |
| Home | 761 (38.6) |
| Street | 490 (24.8) |
| Public building | 62 (3.1) |
| Recreation facility | 53 (2.7) |
| Undetermined or unknown | 419 (21.2) |
| Other | 176 (8.9) |
| Insurance coverage | |
| Commercial or private | 506 (25.7) |
| Medicaid | 687 (34.8) |
| Medicare | 7 (0.4) |
| Self-pay | 390 (19.8) |
| Not billed | 19 (1) |
| Unknown | 176 (8.9) |
| Other | 161 (8.2) |
| Not applicable | 26 (1.3) |
Abbreviations: GCS, Glasgow Coma Scale (range: 3-15, with the lowest scores indicating greater levels of TBI); IQR, interquartile range; ISS, Injury Severity Score (range: 0-75, with the highest scores indicating severe injury); LOS, length of stay; TBI, traumatic brain injury.
Figure 1. Distribution of Pediatric Firearm-Related Ocular Trauma by Age and Race/Ethnicity, 2008-2014.
From a total of 8715 firearms-associated ocular injuries during the study period, 1972 (22.6%) occurred in pediatric patients, most of whom were male (1678 [85.1%]), adolescent (1037 [52.6%]), and black (851 [43.2%]).
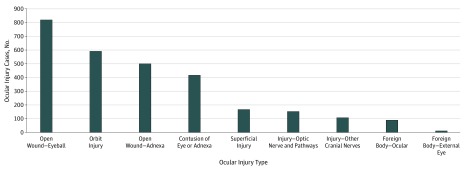
Assault intention represented 1241 (62.9%) cases; unintentional, 346 (17.5%); and self-inflicted, 258 (13.1%). The most common types of firearm-related ocular injuries were open wound of the eyeball (820 [41.6%]) and ocular adnexa (502 [25.5%]), orbital injuries or fractures (591 [30.0%]), and contusion of the eye or adnexa (417 [21.1%]) (Figure 2). The frequency of TBI was 55.3% (1091). The mean (SD) ISS was 16 (13.1), with a median (IQR) of 14 (4-25). The mean (SD) GCS score was 11 (5.1), with a median (IQR) of 15 (4-15). Common locations of injury were the home (761 [38.6%]) and street (490 [24.8%]). Reported regional distribution was as follows, in declining order: 778 (39.5%) in the South, 496 (25.2%) in the Midwest, 415 (20.9%) in the West, and 255 (12.9%) in the Northeast. The remaining 28 (14.2%) were from undetermined regions. The mean (SD) hospital stay was 7.6 (12) days. Most patients had Medicaid coverage (687 [34.8%]), followed closely by commercial or private health insurance (506 [25.7%]) and self-pay (390 [19.8%]). The inpatient mortality rate was 12.2% (240), and most patients were discharged home (1119 [56.7%]) (Table).
Figure 2. Frequency of Pediatric Firearm-Related Ocular Trauma by Type of Injury, 2008-2014.
Most injuries were open wound of the eyeball (820 [41.6%]), open wound of the ocular adnexa (502 [25.5%]), and orbital fractures (591 [30%]).
Comparative Analysis: Demographic Differences
Logistic regression analysis revealed distinct demographic differences in location, mechanism, and intention of injury. With respect to location, white patients had the greatest odds of injury in the home (OR, 2.89; 95% CI, 2.38-3.52; P < .001) compared with other locations, whereas black (OR, 2.33; 95% CI, 1.89-2.87; P < .001) and Hispanic (OR, 1.30; 95% CI, 1.01-1.68; P = .04) patients had greater odds of injury on the street (eTable 1 in the Supplement). When divided by sex, differences in common locations were observed. White female patients had the greatest odds of home location (OR, 2.70; 95% CI, 1.53-4.78; P < .001), black female patients had the greatest odds of street location (OR, 1.65; 95% CI, 1.07-2.55; P = .02), and Hispanic female patients also had the greatest odds of home location (OR, 1.94, 95% CI, 0.92-4.08; P = .08). For black and white male patients and male patients of Hispanic ethnicity, the propensity for certain locations was similar to that of their whole group. Patients aged 0 to 3 years exhibited the greatest odds of home injury (OR, 5.39; 95% CI, 2.81-10.38; P < .001). Those aged 19 to 21 years were most likely to be injured on the street (OR, 1.61; 95% CI, 1.3-1.98; P < .001), and injuries among those aged 12 to 18 years occurred most often in recreational facilities (OR, 1.78; 95% CI, 1.00-3.16; P = .05) (eTable 2 in the Supplement).
With respect to insurance coverage, white patients were most likely to have commercial or private insurance (OR, 3.21; 95% CI, 2.59-3.99; P < .001), black patients were most likely to have Medicaid (OR, 1.67; 95% CI, 1.38-2.03; P < .001), and Hispanic patients were most likely to self-pay (OR, 1.32, 95% CI, 1.00-1.73; P = .05). Self-pay patients were most likely to have injury from assault intention compared with those with other intentions (OR, 1.52; 95% CI, 1.12-1.93; P < .001).
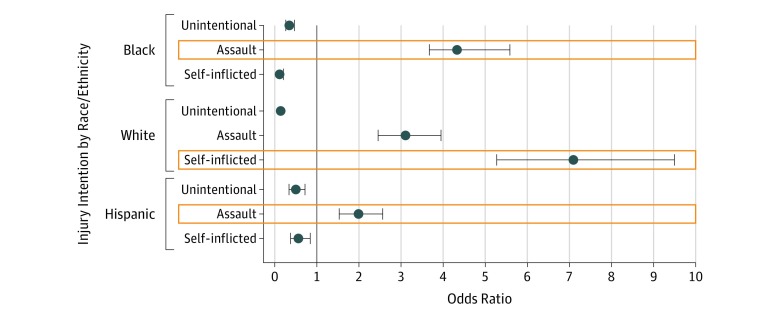
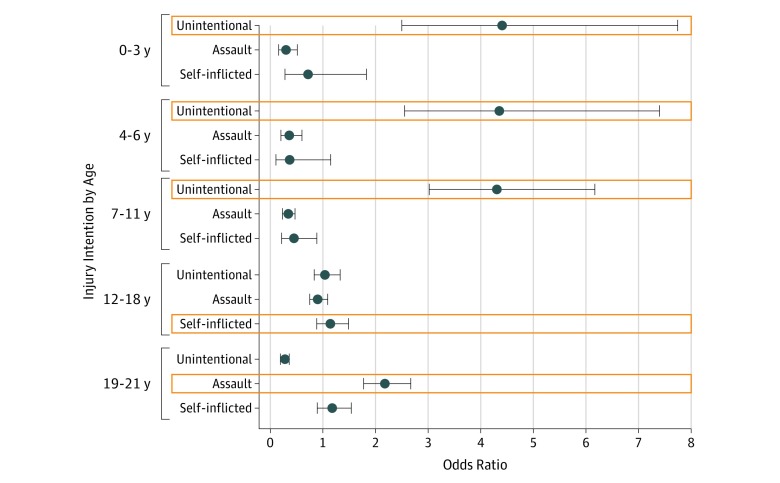
For both sexes, assault injuries were most common, with similar frequencies for men (1055 [62.9%]) and women (186 [63.3%]). However, male patients had greater odds of self-inflicted injury (OR, 1.65; 95% CI, 1.10-2.53; P = .02) compared with female patients. White patients had greater odds of self-inflicted injury (OR, 7.1; 95% CI, 5.92-9.51; P < .001) compared with black patients. Black (OR, 4.53; 95% CI, 3.68-5.59; P < .001) and Hispanic (OR, 1.99; 95% CI, 1.54-2.57; P < .001) patients had greater odds of injury with assault intention compared with other intentions. Infants (aged 0-3 years) had the greatest odds of unintentional injuries (OR, 4.41; 95% CI, 2.51-7.75; P < .001). Older adolescents (aged 19-21 years) had the greatest odds of having assault injury (OR, 2.17; 95% CI, 1.77-2.66; P < .001) compared with other intentions (Figure 3 and Figure 4).
Figure 3. Logistic Regression Analysis of Association Between Race/Ethnicity and Injury Intention in Pediatric Firearm-Related Ocular Trauma, 2008-2014.
Black and Hispanic children had the greatest odds of assault, whereas white children had the greatest odds of self-inflicted injury. Boxed plots represent the greatest odds ratio in each category.
Figure 4. Logistic Regression Analysis of Association Between Age Group and Injury Intention in Pediatric Firearm-Related Ocular Trauma, 2008-2014.
Infants had the greatest odds of unintentional injury, whereas older adolescents had the greatest odds of assault. Boxed plots represent the greatest odds ratio in each category.
Optic nerve and visual pathway injuries were associated with self-inflicted trauma (OR, 2.86; 95% CI, 1.95-4.20; P < .001), as were orbital injuries (OR, 1.87; 95% CI, 1.43-2.45; P < .001), TBI (OR, 5.99; 95% CI, 4.16-8.63; P < .001), and inpatient mortality (OR, 3.75; 95% CI, 2.74-5.13; P < .001). Open globe injuries, however, most commonly occurred in the setting of unintentional trauma (OR, 1.62; 95% CI, 1.29-2.05; P < .001).
Severity and Firearm-Related Ocular Injury
Open wound to the eye and adnexa injuries were associated with mild ISSs (OR, 2.17; 95% CI, 1.79-2.64; P < .001 and OR, 2.39; 95% CI, 1.93-2.96; P < .001) and mild GCS scores (OR, 1.57; 95% CI, 1.29-1.91; P < .001 and 1.89; 1.49-2.38; P < .001). Optic nerve and visual pathway injuries were most associated with severe ISSs (OR, 2.01; 95% CI, 1.38-2.93; P < .001) and severe GCS scores (OR, 1.83; 95% CI, 1.30-2.58; P = .001) (eTables 3 and 4 in the Supplement). These injuries also had the greatest association with hospital lengths of stay longer than 6 days (OR, 3.19; 95% CI, 2.28-4.48; P < .001). Patients classified as having TBI were most likely to have associated optic nerve and pathway injuries (OR, 4.47; 95% CI, 2.88-6.93; P < .001) and orbital injuries (OR, 3.05; 95% CI, 2.47-3.76; P < .001). The 19- to 21-year age group had 1.63 higher odds of TBI (P < .001) compared with other age groups (eTable 5 in the Supplement). No observed difference in TBI risk was observed between black and white patients. However, white patients had greater odds of death (OR, 1.64; 95% CI, 1.23-2.14; P < .001) when admitted with firearm-related ocular injuries compared with blacks and Hispanic patients. No age-related propensity for death was observed with firearm-related ocular injuries. The associations of age, race/ethnicity, and intention in inpatient mortality with pediatric firearm-related ocular injuries are detailed in eTables 6 and 7 in the Supplement. Intention was associated with injury severity and TBI degree, with unintentional injuries more likely to have mild ISSs (OR, 2.33; 95% CI, 1.84-2.96; P < .001) and GCS scores (OR, 1.39; 95% CI, 1.07-1.79; P = .01), whereas self-inflicted injuries had very severe ISSs (OR, 3.52; 95% CI, 2.69-4.63; P < .001) and severe GCS scores (OR, 5.71; 95% CI, 4.26-7.66; P < .001). Assault injuries had the greatest odds of a mild ISS and moderate GCS score (eTables 8 and 9 in the Supplement).
Discussion
Firearms are a major cause of morbidity and mortality in the United States. The need for improved gun control has become an everyday topic of conversation, particularly with the rise in the number of school shootings and the 2018 national school walkout in protest of gun violence.23 With an improved understanding of firearm-related trauma, we can start to better address this public health issue.
The NTDB has been useful to trauma researchers given its accessibility and large sample size.24 Its vast data pool, comprising more than 8 million records, has helped researchers make substantial progress in examining trauma. Previous studies that obtained data from the NTDB have evaluated pediatric vascular trauma,25 firearm fatalities,26 penetrating neck trauma,27 and self-inflicted injuries,28 to name a few. Several studies have investigated sports and recreation–associated ocular injuries from paintball, air or nonpowder, and BB or pellet guns.12,13,14,29 Lee and Fredrick15 found more than a 600% rise in hospital admission rates from air gun–related eye injuries in children and reported that 28% of air soft– or BB-gun injuries had poor visual outcomes after treatment. Currently, literature is lacking on all firearm-related ocular injuries, including nonrecreational firearm injuries, particularly in children.
To this end, we used the NTDB data set from January 1, 2008, to December 31, 2014 to investigate pediatric firearm-related ocular injuries and found that 1972 (22.6%) of firearm-related ocular injuries in the United States occurred in children, who make up roughly 23% of the national population.30 Previous studies into pediatric firearm-related ocular injuries showed that such injuries commonly occurred in black, adolescent, male children under assault intention.31,32,33,34,35,36 We affirmed these patterns in the demographics and injury intent, with 1037 (52.6%) pediatric firearm-related ocular injuries occurring in patients aged 12 to 18 years, 1678 (85.1%) in male patients, 851 (43.2%) in black patients, and 1241 (62.9%) as a result of assault. In addition, we found that white patients had a greater likelihood of being injured in the home, and black and Hispanic patients were more likely to sustain injury in the street. White males were more likely to be injured in recreational facilities compared with black and Hispanic males. With respect to intention, white patients were more likely to have self-inflicted injuries, whereas the injuries of black and Hispanic patients were more likely to come from assault. Self-inflicted injuries had the greatest association with TBI, optic nerve and visual pathway injuries, and death. Self-inflicted intention may be associated with the higher likelihood of death in white compared with black patients in this study. Crutcher et al37 found a similar trend in penetrating intracranial gunshot wounds, with higher odds of inflicted self-harm in white individuals and assault injury in black individuals.
Firearm injury is generally classified as penetrating trauma, lending itself to an increased risk for severe, visually disabling harm. Although common ocular injuries included ruptured globe, open wound of the ocular adnexa, and orbital fractures, optic nerve and visual pathway injuries had the greatest association with severe GCS score (TBI) and ISS. All types of TBI were present in most patients (with or without optic nerve or visual pathway injuries) in this study. Studies have shown that even mild TBI is associated with symptomatic visual problems that include diminished visual acuity and color vision, visual field defects, photosensitivity, spatial neglect, and convergence insufficiency. These deficits have implications for the pediatric and geriatric populations.38,39 Patients with ophthalmologic manifestations of TBI may find vision rehabilitation advantageous in addition to the usual occupational, vestibular, cognitive, and physical therapies. We found that most patients survived their injuries and were discharged home after hospitalization. We believe these findings highlight the large proportion of pediatric patients who survive with varying degrees of disability and compromised development.
We performed subgroup analyses to investigate the health care disparities among those with pediatric firearm-associated ocular injuries. Racial/ethnic disparities have been identified in health care, with differences in access to care and the quality of care provided.40 We found that white patients had greater odds of having commercial or private health insurance, whereas black patients were more likely to have Medicaid coverage. The self-pay rate in this study was 19.8%, and most self-pay patients were Hispanic and associated with assault injuries. This finding is consistent with that of the 2002 Medical Expenditure Panel Survey, which found that racial/ethnic minorities, such as black and Hispanic people, more commonly received health insurance coverage from public programs or remained uninsured.41 The 2002 Medical Expenditure Panel Survey also reported that black individuals had a shorter life expectancy and longer periods of being uninsured and in poorer health compared with their white counterparts, putting black people at substantially increased health risk.
Future investigations are needed to assess whether racial/ethnic differences are factors in injury severity and morbidity. Whether different behavioral, cultural, educational, or environmental exposures play a role in the associations between race/ethnicity and pediatric firearm-related ocular injuries is subject to speculation. The racial/ethnic disparities mentioned here are intriguing and suggest that future interventions for firearm safety may need to be tailored to the target population.
Most patients in this study survived with potentially lifelong disability and impeded physical, academic, and social development. These findings, if they can be confirmed in analyses for 2015 through 2019, suggest that the prevention of firearm-related ocular injuries may require a multifaceted and targeted approach that could use the associated factors that we have identified.
Limitations
The limitations of this study include the limitation of data to 2008 through 2014; confirmation of data from 2015 through 2019 is needed. The study is also limited by its retrospective design and access to only parts of the clinical records. Detailed specifics of the injuries and their visual function outcomes were not available. A 2006 study by Kuhn et al42 used the United States Eye Injury Registry to establish a list of factors that increased the risk of legal blindness in an injured eye. Risk factors included injury by assault and injury occurring by gunshot. More data on this topic would be helpful in risk stratification for visual and ocular prognosis in pediatric firearm-related ocular injuries.
Another limitation was the lack of data on the type of firearm implicated in the ocular injury. Recreational and nonpowder firearms have the potential to inflict serious injury, with reports of 7% of patients sustaining a functional deficit, of which 42% were ocular injuries.43 In a study by Bratton et al44 that evaluated pediatric air gun injuries, 66% of children with eye injuries sustained permanent vision loss, and 39% of these children went blind. Looking into the type of firearm used may help stratify the severity and type of injury. In addition, NTDB data primarily detail trauma in admitted patients and those who are dead on arrival. Our exclusion of patients who died in the field may underestimate the true implication of firearm-related trauma. Limitations notwithstanding, this study, to our knowledge, is among the few to examine firearm-related ocular injuries of this scope and with the pediatric population as a focus.
Conclusions
This study found that pediatric firearm-related ocular injuries in the United States disproportionately occurred in male, black, adolescent patients and were mostly from assault. Most injuries were sight-threatening; associated with severe ISS and GCS scores; and varied by age, sex, location, intention, and geographic region.
eTable 1. Common Locations by Race and Ethnicity in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 2. Common Locations by Age in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 3. Association of Common Pediatric Firearm-related Ocular Injury and Injury Severity Score; NTDB 2008-2014
eTable 4. Association of Common Pediatric Firearm-related Ocular Injury and Glasgow Coma Score; NTDB 2008-2014
eTable 5. Traumatic Brain Injury by Age, Race, and Ethnicity in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 6. Association of Age, Race and Ethnicity and Inpatient Mortality in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 7. Association of Intention and Inpatient Mortality in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 8. Association of Intention and Injury Severity in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 9. Association of Intention and Level of Traumatic Brain Injury (GCS) in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
References
- 1.Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266-273. doi: 10.1016/j.amjmed.2015.10.025 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Welcome to WISQARS. http://www.cdc.gov/injury/wisqars. Accessed January 21, 2018.
- 3.Fowler KA, Dahlberg LL, Haileyesus T, Gutierrez C, Bacon S. Childhood firearm injuries in the United States. Pediatrics. 2017;140(1):e20163486. doi: 10.1542/peds.2016-3486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carter PM, Walton MA, Newton MF, et al. Firearm possession among adolescents presenting to an urban emergency department for assault. Pediatrics. 2013;132(2):213-221. doi: 10.1542/peds.2013-0163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiScala C, Sege R. Outcomes in children and young adults who are hospitalized for firearms-related injuries. Pediatrics. 2004;113(5):1306-1312. doi: 10.1542/peds.113.5.1306 [DOI] [PubMed] [Google Scholar]
- 6.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med. 2015;79:5-14. doi: 10.1016/j.ypmed.2015.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kliewer W, Lepore SJ, Oskin D, Johnson PD. The role of social and cognitive processes in children’s adjustment to community violence. J Consult Clin Psychol. 1998;66(1):199-209. doi: 10.1037/0022-006X.66.1.199 [DOI] [PubMed] [Google Scholar]
- 8.Keil S, Fielder A, Sargent J. Management of children and young people with vision impairment: diagnosis, developmental challenges and outcomes. Arch Dis Child. 2017;102(6):566-571. doi: 10.1136/archdischild-2016-311775 [DOI] [PubMed] [Google Scholar]
- 9.Chadha RK, Subramanian A. The effect of visual impairment on quality of life of children aged 3-16 years. Br J Ophthalmol. 2011;95(5):642-645. doi: 10.1136/bjo.2010.182386 [DOI] [PubMed] [Google Scholar]
- 10.Mair JS, Mair M. Violence prevention and control through environmental modifications. Annu Rev Public Health. 2003;24:209-225. doi: 10.1146/annurev.publhealth.24.100901.140826 [DOI] [PubMed] [Google Scholar]
- 11.Hemenway D, Miller M. Public health approach to the prevention of gun violence. N Engl J Med. 2013;368(21):2033-2035. doi: 10.1056/NEJMsb1302631 [DOI] [PubMed] [Google Scholar]
- 12.Listman DA. Paintball injuries in children: more than meets the eye. Pediatrics. 2004;113(1 Pt 1):e15-e18. doi: 10.1542/peds.113.1.e15 [DOI] [PubMed] [Google Scholar]
- 13.Fleischhauer JC, Goldblum D, Frueh BE, Koerner F. Ocular injuries caused by airsoft guns. Arch Ophthalmol. 1999;117(10):1437-1439. https://jamanetwork.com/journals/jamaophthalmology/fullarticle/412457 [PubMed] [Google Scholar]
- 14.Sharif KW, McGhee CN, Tomlinson RC. Ocular trauma caused by air-gun pellets: a ten year survey. Eye (Lond). 1990;4(Pt 6):855-860. doi: 10.1038/eye.1990.136 [DOI] [PubMed] [Google Scholar]
- 15.Lee R, Fredrick D. Pediatric eye injuries due to nonpowder guns in the United States, 2002-2012. J AAPOS. 2015;19(2):163-8.e1. doi: 10.1016/j.jaapos.2015.01.010 [DOI] [PubMed] [Google Scholar]
- 16.National Trauma Data Bank. NTDB Research Data Set User Manual and Variable Description List. Admission Years 2002-2016 Chicago, IL: NTDB; 2018. https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/ntdb%20rds%20user%20manual%20all%20years.ashx. Accessed July 3, 2019.
- 17.American College of Surgeons. About NTDB. https://www.facs.org/quality-programs/trauma/tqp/center-programs/ntdb/about. Accessed September 23, 2018.
- 18.Harrison J. ICD-coding of firearm injuries. https://www.cdc.gov/nchs/injury/ice/amsterdam1998/amsterdam1998_guncodes.htm. Published August 1997. Accessed May 12, 2018.
- 19.US Department of Health and Human Services, Food and Drug Administration, Center for Devices and Radiological Health Guidance for industry and FDA staff. Pediatric expertise for advisory panels. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm082188.pdf. Published June 3, 2003. Accessed January 21, 2018.
- 20.Hagan JF Jr, Shaw JS, Duncan P, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children and Adolescents 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017. https://brightfutures.aap.org/Bright%20Futures%20Documents/BF4_Introduction.pdf. Accessed January 3, 2019.
- 21.Hardin AP, Hackell JM; Committee on Practice and Ambulatory Medicine . Age limit of pediatrics. Pediatrics. 2017;140(3):e20172151. doi: 10.1542/peds.2017-2151 [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention Traumatic brain injury in the United States: emergency department visits hospitalizations and deaths 2002-2006. https://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. Accessed January 21, 2018.
- 23.Yee V, Blinder A National school walkout: thousands protest against gun violence across the U.S. New York Times March 14, 2018. https://www.nytimes.com/2018/03/14/us/school-walkout.html. Accessed March 27, 2018.
- 24.Fantus RJ. Annual Report 2017: ICD-10. Bulletin of the American College of Surgeons. http://bulletin.facs.org/2018/01/annual-report-2017-icd-10/#.WmDUmKinHIU. Accessed January 21, 2018.
- 25.Barmparas G, Inaba K, Talving P, et al. Pediatric vs adult vascular trauma: a National Trauma Databank review. J Pediatr Surg. 2010;45(7):1404-1412. doi: 10.1016/j.jpedsurg.2009.09.017 [DOI] [PubMed] [Google Scholar]
- 26.Oyetunji TA, Haider AH, Obirieze AC, et al. Epidemiology of 577 pediatric firearm fatalities: a 2-year review of the National Trauma Data Bank. Am Surg. 2014;80(4):366-371. [PubMed] [Google Scholar]
- 27.Stone ME Jr, Farber BA, Olorunfemi O, et al. Penetrating neck trauma in children: an uncommon entity described using the National Trauma Data Bank. J Trauma Acute Care Surg. 2016;80(4):604-609. doi: 10.1097/TA.0000000000000976 [DOI] [PubMed] [Google Scholar]
- 28.Cutler GJ, Flood A, Dreyfus J, Ortega HW, Kharbanda AB. Emergency department visits for self-inflicted injuries in adolescents. Pediatrics. 2015;136(1):28-34. doi: 10.1542/peds.2014-3573 [DOI] [PubMed] [Google Scholar]
- 29.Miller KN, Collins CL, Chounthirath T, Smith GA. Pediatric sports- and recreation-related eye injuries treated in US emergency departments. Pediatrics. 2018;141(2):e20173083. doi: 10.1542/peds.2017-3083 [DOI] [PubMed] [Google Scholar]
- 30.ChildStats.gov. Population figures. In America’s Children in Brief: Key National Indicators of Well-being 2018. https://www.childstats.gov/americaschildren/pop_fig.asp. Accessed March 27, 2018.
- 31.Barmparas G, Dhillon NK, Smith EJT, et al. Assault in children admitted to trauma centers: injury patterns and outcomes from a 5-year review of the National Trauma Data Bank. Int J Surg. 2017;43:137-144. doi: 10.1016/j.ijsu.2017.05.068 [DOI] [PubMed] [Google Scholar]
- 32.Leventhal JM, Gaither JR, Sege R. Hospitalizations due to firearm injuries in children and adolescents. Pediatrics. 2014;133(2):219-225. doi: 10.1542/peds.2013-1809 [DOI] [PubMed] [Google Scholar]
- 33.McGwin G Jr, Owsley C. Incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol. 2005;123(5):662-666. doi: 10.1001/archopht.123.5.662 [DOI] [PubMed] [Google Scholar]
- 34.Bachier-Rodriguez M, Freeman J, Feliz A. Firearm injuries in a pediatric population: African-American adolescents continue to carry the heavy burden. Am J Surg. 2017;213(4):785-789. doi: 10.1016/j.amjsurg.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 35.Davis JS, Castilla DM, Schulman CI, Perez EA, Neville HL, Sola JE. Twenty years of pediatric gunshot wounds: an urban trauma center’s experience. J Surg Res. 2013;184(1):556-560. doi: 10.1016/j.jss.2012.12.047 [DOI] [PubMed] [Google Scholar]
- 36.Carter PM, Cook LJ, Macy ML, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Individual and neighborhood characteristics of children seeking emergency department care for firearm injuries within the PECARN network. Acad Emerg Med. 2017;24(7):803-813. doi: 10.1111/acem.13200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crutcher CL II, Fannin ES, Wilson JD. Racial disparities in cranial gunshot wounds: intent and survival. J Racial Ethn Health Disparities. 2016;3(4):687-691. doi: 10.1007/s40615-015-0187-7 [DOI] [PubMed] [Google Scholar]
- 38.Barnett BP, Singman EL. Vision concerns after mild traumatic brain injury. Curr Treat Options Neurol. 2015;17(2):329-343. doi: 10.1007/s11940-014-0329-y [DOI] [PubMed] [Google Scholar]
- 39.Singman EL. Automating the assessment of visual dysfunction after traumatic brain injury. Med Instrum. 2013;1:3. doi: 10.7243/2052-6962-1-3 [DOI] [Google Scholar]
- 40.Smedley BD, Stith AY, Nelson AR, eds; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Board on Health Policy. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care Washington, DC: The National Academies Press; 2002. http://www.precaution.org/lib/iom_on_health_disparities.020601.pdf. Accessed September 23, 2018. [PubMed]
- 41.Roberts M. Racial and ethnic differences in health insurance coverage and usual source of health care, 2002. In MEPS Chartbook No. 14. AHRQ Publication No. 06-0004. Rockville, MD: Agency for Healthcare Research and Quality; 2006. https://meps.ahrq.gov/data_files/publications/cb14/cb14.pdf. Accessed September 23, 2018.
- 42.Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States eye injury registry. Ophthalmic Epidemiol. 2006;13(3):209-216. doi: 10.1080/09286580600665886 [DOI] [PubMed] [Google Scholar]
- 43.Scribano PV, Nance M, Reilly P, Sing RF, Selbst SM. Pediatric nonpowder firearm injuries: outcomes in an urban pediatric setting. Pediatrics. 1997;100(4):E5. doi: 10.1542/peds.100.4.e5 [DOI] [PubMed] [Google Scholar]
- 44.Bratton SL, Dowd MD, Brogan TV, Hegenbarth MA. Serious and fatal air gun injuries: more than meets the eye. Pediatrics. 1997;100(4):609-612. doi: 10.1542/peds.100.4.609 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Common Locations by Race and Ethnicity in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 2. Common Locations by Age in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 3. Association of Common Pediatric Firearm-related Ocular Injury and Injury Severity Score; NTDB 2008-2014
eTable 4. Association of Common Pediatric Firearm-related Ocular Injury and Glasgow Coma Score; NTDB 2008-2014
eTable 5. Traumatic Brain Injury by Age, Race, and Ethnicity in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 6. Association of Age, Race and Ethnicity and Inpatient Mortality in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 7. Association of Intention and Inpatient Mortality in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 8. Association of Intention and Injury Severity in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014
eTable 9. Association of Intention and Level of Traumatic Brain Injury (GCS) in Pediatric Firearm-related Ocular Injury; NTDB 2008-2014