Key Points
Question
Is the endoscopic preperiosteal midface lift an effective technique, and do the results last?
Findings
In this retrospective review, there was a significant, objective improvement (decrease) in midfacial height after the endoscopic preperiosteal midface lift that persisted for at least 5 years and up to 15 years. Validated regional and global aesthetic scales demonstrated lasting improvement in midface appearance over time.
Meaning
There is a persistent improvement in midfacial height after the endoscopic preperiosteal midface lift that is achieved without complete disruption of the midfacial ligaments.
Abstract
Importance
To our knowledge, until now, the efficacy and durability of the transtemporal endoscopic preperiosteal midface lift has not been reported in the literature.
Objective
To determine the efficacy and longevity of the endoscopic preperiosteal midface lift using objective measurements and validated aesthetic scales.
Design, Setting, and Participants
This retrospective review included patients 18 years or older who were treated for aging midface by endoscopic midface lift by the senior author (A.E.W.) between June 2000 and August 2016. Patients were categorized based on length of follow-up into 3 groups: (1) short-term (1-3 years), (2) intermediate-term (3-5 years), and (3) long-term (>5 years).
Interventions or Exposures
Endoscopic preperiosteal midface lift.
Main Outcomes and Measures
(1) Objective measurements of midfacial height (the width of the interzygomatic distance of the midface to the medial canthus [WIZDOM-MC]), (2) validated regional aesthetic scales, and (3) global aesthetic scoring systems measured preoperatively, 3 to 6 months postoperatively, and at the most recent follow-up visit.
Results
Adult patients 18 years or older (median [range] age, 59 [31-79] years) who were treated for aging midface by undergoing an endoscopic midface lift were included in this study. The medical records of 143 patients were reviewed (135 women and 8 men). The endoscopic midface lift resulted in objective improvement in midfacial height. The median WIZDOM-MC decreased by 3.4 mm after the endoscopic midface lift (interquartile range [IQR], 2.3-4.4 mm; P < .001), thus shortening the elongated lower eyelid. At 5 to 15 years after surgery, there was a sustained decrease in median WIZDOM-MC of 2.1 mm (IQR, 0.8-3.1 mm; P < .001). Improvement in the infraorbital hollow was also sustained in patients at more than 5 years’ follow-up (IQR, 0-1.0; P < .001). Improvements in upper cheek fullness and lower cheek fullness were maintained at 3 to 5 years and tended to be at baseline at more than 5 years. Global aesthetic improvement scores remained significantly improved at 5 to 15 years’ follow-up.
Conclusions and Relevance
There is a significant, objective improvement in midfacial height after the endoscopic midface lift that persists for up to 15 years. Validated midfacial scales and global aesthetic scoring systems demonstrate sustained improvement in midface appearance over time. Surgery that minimally disrupts the zygomatic and orbicularis retaining ligaments can provide long-lasting aesthetic improvements.
Level of Evidence
4.
This retrospective review examines the longevity of the endoscopic preperiosteal midface lift using aesthetic scales.
Introduction
Rejuvenation of the aging midface remains a challenge for aesthetic surgeons. Multiple procedures to address midfacial aging have been described and used with variable success. In an ongoing effort to determine the most effective way to address the aging midface, the efficacy of several of these techniques has been evaluated.1,2,3,4,5,6,7,8 In addition, the durability of various midface lift approaches have also been explored, although outcome measures have largely been subjective and the duration of follow-up is limited.9,10,11
The transtemporal preperiosteal midface lift is a single suture technique that permits elevation of the orbicularis oculi muscle and malar fat pad while allowing direct visualization and selective, partial disruption of the midfacial ligaments. The procedure is performed endoscopically and is associated with minimal morbidity.12 This technique, as originally described by Isse,13 involved extensive division of the zygomatic ligaments and the orbital retaining ligaments. We have modified this technique such that we avoid disrupting the orbicularis retaining ligament (ORL) and only minimally divide the zygomatic ligament and lateral canthal adhesion. This contradicts conventional plastic surgical dogma, which emphasizes the necessity of full ligamentous division for obtaining longevity and pleasing aesthetic results in midface lifting surgery.
To our knowledge, the efficacy and durability of a minimally disruptive approach to the midface have not been reported in the literature. In this retrospective review, we sought to determine the efficacy and longevity of the transtemporal preperiosteal midface lift using objective measurements of midfacial height, validated regional aesthetic scales, and global aesthetic assessment scores.
Methods
Study Design
Ethical approval was obtained from the Temple University institutional review board before initiating this retrospective review. All participants provided written informed consent at their preoperative visit to have their results included in a research study performed by the senior author (A.E.W.). Additionally, patient information was deidentified and stored in a password-protected file and on password-protected computer. The outpatient medical records of all patients who underwent the endoscopic midface lift procedure by the senior author (A.E.W.) between June 2000 and August 2016 were reviewed. Adult patients 18 years or older who were treated for aging midface by endoscopic midface lift were considered eligible for the study. Additional procedures performed at the time of the midface lift were documented. All procedures completed during the follow-up period were recorded. A minimum of 1 year of follow-up was required for inclusion in the study. Patients were followed up between 1 and 15 years after the endoscopic midface lift.
Surgical Technique
The senior author (A.E.W.) has consistently performed the endoscopic, transtemporal preperiosteal approach for all midface lift procedures performed for the duration of the study period. A detailed description of this surgical technique has been previously published.12 Briefly, bilateral temporal incisions are created and deepened until the superficial layer of the deep temporal fascia is encountered. An optical pocket is created above this layer using Metzenbaum scissors. A second incision is created in the paramedian position, particularly if a brow lift is performed, which enhances visualization. A 30° endoscope is used for superior visualization using a sheath that allows for the elevation of the soft tissue and irrigation as necessary (Forward-Oblique Telescope 30° and Optical Dissector 50200 ES; Hopkins). Dissection is continued inferiorly. The inferior temporal ligaments are disrupted until the sentinel veins are identified. The anterolateral expansion of the lateral canthal tendon is sharply incised at its lateral-most border, exposing the underlying orbital orbicularis at its junction with the preseptal orbicularis along the inferolateral external orbital wall. This incision allows entrance into the prezygomatic space. At this time, the space is expanded using a Trepsat dissector (ASSI), elevating the entire orbital orbicularis without disrupting the malar septum and extending the elevation laterally until resistance is met at the medial portion of the zygomatic ligament. The zygomatic ligament is divided just enough to allow for the passage of the midface lift suture. An elevator is used to free the midface.
A 25-gauge needle is then inserted externally at a point 3 cm from the lateral canthus on a line drawn from the inferior border of the tragus to the lateral canthus. A 3-0 prolene suture is placed endoscopically through the orbicularis oculi muscle at the marked point and secured to the superficial layer of the deep temporal fascia using a horizontal mattress suture with a superior vector of pull, elevating the midface. The midface moves vertically, supported by this single suture.
Photographic Documentation
All photographs used in this study were taken in a studio with consistent lighting using a Nikon D70 or D90 camera and archived on the Mirror System (Canfield). Patients were photographed in 5 different views: anteroposterior, bilateral 45° oblique, and bilateral profile views.
Patient photographs from 3 points were used for this study: (1) preoperative photographs taken at the office visit preceding the procedure, (2) postoperative photographs taken 3 to 6 months after the midface lift, and (3) photographs taken at the most recent follow-up visit. At each point, anteroposterior photographs and bilateral 45° oblique photographs were collected for analysis.
Assessment Methods
The medical records of all included patients were reviewed for relevant demographic data, including age at the time of the procedure, additional procedures performed at the time of midface lift, fat transfer at the time of midface lift, and filler administration during the follow-up period. Patients were divided into 3 groups based on length of follow-up: group 1, 1 to 3 years; group 2, 3 to 5 years; and group 3, 5 to 15 years.
Patients were assessed by the following measures: (1) the width of the interzygomatic distance of the midface–medial canthus (WIZDOM-MC), a validated, objective measurement that can be used to quantify changes in midfacial height14; (2) validated midfacial assessment scales that provide region-specific information about infraorbital hollow, upper cheek fullness, and lower cheek fullness15; and (3) the global aesthetic improvement scale, which describes perceived changes in global appearance over time.16
Data were displayed as the median (range) for continuous variables and the count (percentage) for categorical variables. Absolute changes of outcome variables from baseline to 2 follow-up points were analyzed and reported. These changes were further compared between 3 groups at each of the follow-up points using the Kruskal-Wallis test (between groups) and the sign test (within group) when appropriate. Furthermore, mixed-effects models were fitted to the outcome data measured overtime (eg, WIZDOM-MC) while adjusting for the covariates or confounders for comparisons between the groups or points. Adjusted P values were derived. A P value of <.05 was considered significant. All statistical analyses were performed using SAS, version 9.4 (SAS Institute).
Results
The medical records of 143 patients were reviewed. Of these patients, 135 (94.4%) were women. The median (range) patient age at the time of the procedure was 59 (31-79) years. At the time of the midface lift, 130 patients (90.9%) underwent endoscopic brow lift. All patients underwent lower blepharoplasty by a transconjunctival approach, and 112 patients (78.3%) underwent upper blepharoplasty at the time of the midface lift. Fat transfer was performed for 133 patients (93.0%) as part of the initial procedure. During the follow-up period, 32 patients (22.4%) underwent filler injection into the midface and 18 patients (12.6%) underwent filler injection into the tear trough region.
Complications were recorded. There were no cases of facial paralysis, facial numbness, or ectropion. Minor complications, such as chemosis, were thought to be due to other procedures performed at the time of the midface lift rather than the midface lift itself. One patient had uneven distribution of fat in the tear trough after fat transfer, which improved at 3 months.
Objective Measurements
To objectively evaluate midfacial height and compare changes in midfacial height over time, the WIZDOM-MC was measured using Adobe Photoshop 2014 (Adobe Systems) in each patient at 3 points as previously described. After the endoscopic midface lift, the median WIZDOM-MC decreased by 3.4 mm (interquartile range [IQR], 2.3-4.4 mm; P < .001), thus shortening the elongated lower eyelid. When examining each follow-up group individually, the improvement in midfacial position remained significant (Table 1). In group 1, the median WIZDOM-MC decreased by 3.7 mm after the endoscopic midface lift (IQR, 2.3-5.3 mm). The median decrease in WIZDOM-MC was 3.6 mm and 3.2 mm in groups 2 and 3, respectively (IQR, 3.0-4.8 mm and 2.2-4.3 mm, respectively; all P < .001). This decrease in midfacial height was statistically similar in all 3 groups (P = .36).
Table 1. Changes in Midfacial Height Over Time.
| Group | Δ WIZDOM-MC Preoperatively to Postoperatively | Δ WIZDOM-MC Preoperatively to Longest Follow-up | ||
|---|---|---|---|---|
| Preoperatively to Postoperatively (3-6 mo), Median (Range) | P Valuea | Preoperatively to Longest Follow-up, Median (Range) | P Valuea | |
| 1 (1-3 y) (n = 39) | 3.7 (0.0 to 8.4) | <.001 | 2.8 (−1.1 to 7.2) | <.001 |
| 2 (3-5 y) (n = 25) | 3.6 (1.3 to 6.2) | <.001 | 2.3 (−0.3 to 6.3) | <.001 |
| 3 (5-15 y) (n = 78) | 3.2 (−0.1 to 7.6) | <.001 | 2.1 (−2.7 to 7.0) | <.001 |
Abbreviation: WIZDOM-MC, width of the interzygomatic distance of the midface-medial canthus.
Sign test.
The durability of the endoscopic midface lift was investigated by comparing the differences between WIZDOM-MC measurements of preoperative photographs and photographs taken at the patient’s most recent follow-up visit (Table 1). Patients in group 1 demonstrated a sustained decrease in midfacial height of 2.8 mm (IQR, 1.2-3.8 mm; P < .001). Patients in group 2 showed a sustained improvement in median WIZDOM-MC of 2.3 mm (IQR, 1.5-2.8 mm; P < .001), representing a persistent decrease in lower eyelid length. The improvement in midfacial height after midface lift in patients in group 3 remained statistically significant at 5 to 15 years after surgery (median [IQR] 2.1 [0.8-3.1] mm; P < .001). The decreases in WIZDOM-MC seen at the longest follow-up visit were statistically similar between groups (P = .20).
Regional Aesthetic Scales
Patient photographs were evaluated by 3 facial plastic surgeons using validated midfacial assessment scales.15 The regional aesthetic rating scale is composed of 3 5-point subscales to describe infraorbital hollow (IH), upper cheek fullness (UCF), and lower cheek fullness (LCF). Scores were assigned to each patient at 3 points.
There were significant improvements postoperatively in IH, UCF, and LCF, with a median score improvement of 1 after the endoscopic midface lift in each of the 3 follow-up groups. These findings are summarized in Table 2.
Table 2. Changes in Midfacial Regional Aesthetic Scoring Systems Preoperatively to Postoperatively (3 to 6 Months) and Postoperatively (3 to 6 Months) to Longest Follow-up.
| Group | Δ Infraorbital Hollow Preoperatively to Postoperatively | Δ Infraorbital Hollow Preoperatively to Longest Follow-up | Δ Upper Cheek Fullness Preoperatively to Postoperatively | Δ Upper Cheek Fullness Preoperatively to Longest Follow-up | Δ Lower Cheek Fullness Preoperatively to Postoperatively | Δ Lower Cheek Fullness Preoperatively to Longest Follow-up |
|---|---|---|---|---|---|---|
| 1(1-3 y) (n = 39) | ||||||
| Median (range) | 1.0 (−1.0 to 4.0) | 1.0 (0.0 to 3.0) | 1.0 (0.0 to 2.0) | 1.0 (−1.0 to 2.0) | 1.0 (0.0 to 3.0) | 1.0 (−1.0 to 3.0) |
| P Valuea | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| 2 (3-5 y) (n = 25) | ||||||
| Median (range) | 1.0 (0.0 to 3.0) | 1.0 (−1.0 to 4.0) | 1.0 (0.0 to 3.0) | 1.0 (−1.0 to 2.0) | 1.0 (0.0 to 2.0) | 1.0 (−1.0 to 2.0) |
| P Valuea | <.001 | <.001 | <.001 | .01 | <.001 | .03 |
| 3 (5-15 y) (n = 78) | ||||||
| Median (range) | 1.0 (−1.0 to 3.0) | 1.0 (−1.0 to 3.0) | 1.0 (−1.0 to 4.0) | 0.0 (−2.0 to 4.0) | 1.0 (−1.0 to 3.0) | 0.0 (−2.0 to 3.0) |
| P Valuea | <.001 | <.001 | <.001 | .01 | <.001 | .001 |
Sign test.
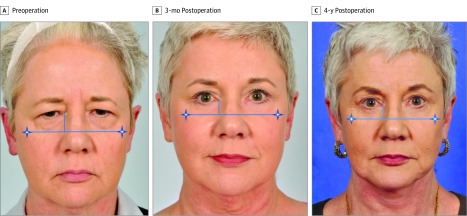
In group 1, improvements in IH, UCF, and LCF with a median change in score of 1 were sustained at 1 to 3 years after surgery (Table 2). Improvements in all 3 subscales persisted at 3 to 5 years follow-up in group 2 with a median score change of 1 (Table 2). In Figure 1, a patient is shown before surgery, 3 months after surgery, and 4 years after surgery. In group 3, IH scores remained significantly improved for 5 to 15 years after the midface lift (IQR, 0-1.0 mm; P < .001). Patients tended to appear at or better than baseline UCF and LCF at 5 to 15 years follow-up (median [IQR], 0 [0-1.0] mm; P = .01 and median [IQR], 0 [0-1.0] mm; P = .001, respectively; Table 2). Figure 2 shows a patient before surgery, 3 months after surgery, and 13 years after surgery. The change in IH, UCF, and LCF seen at longest follow-up was significantly different between groups (group 1: median [IQR], −1.0 [−2.0 to 1.0] mm; median [IQR], −1.0 [−2.0 to 0] mm; and median [IQR], −1.0 [−1.0 to 0] mm; P = .02; group 2: median [IQR], 1.0 [−1.0 to 0] mm; median [IQR], −1.0 [−1.0 to 0] mm; median [IQR], 0 [−1.0 to 0]; P = .01; and group 3: median [IQR], −1.0 [−2.0 to 1.0] mm; median [IQR], −1.0 [−1.0 to 0] mm; median [IQR], 0 [−1.0 to 0]; P = .002, for IH, UCF, and LCF, respectively).
Figure 1. Intermediate-Term Clinical Follow-up After the Endoscopic Midface Lift.
The blue lines indicate the width of the interzygomatic distance of the midface to the medial canthus.
Figure 2. Long-term Clinical Follow-up After the Endoscopic Midface Lift.
Global Aesthetic Improvement Scale
The Global Aesthetic Improvement Scale (GAIS) is a validated assessment tool that can be used to describe relative changes in midfacial appearance. Patient photographs were compared and assigned a score ranging from −3 to 3.16
Patients in group 1 demonstrated a median score of 2.0, indicating a “much improved” appearance, at 1 to 3 years follow-up (median [IQR], 2.0 [1.0-2.0] mm; P < .001). In group 2, patients had a median score of 1.0, indicating an “improved” appearance, 3 to 5 years after surgery (median [IQR], 1.0 [0-2.0] mm; P = .003). Patients in group 3 had a median score of 1.0, representing an “improved” appearance, at 5 years to 15 years after the endoscopic midface lift (median [IQR], 1.0 [−1.0 to 1.0] mm; P = .03) (Table 3). The GAIS at last follow-up was significantly different between groups (P < .001).
Table 3. Changes in Global Aesthetic Scoring Systems Preoperatively to Postoperatively and to Longest Follow-up.
| Group | GAIS Postoperative (3-6 mo) | GAIS Longest Follow-up |
|---|---|---|
| 1 (1-3 y) (n = 39) | ||
| Median (range) | 1.0 (0.0 to 3.0) | 2.0 (0.0 to 3.0) |
| P Valuea | <.0001 | <.0001 |
| 2 (3-5 y) (n = 25) | ||
| Median (range) | 1.5 (0.0 to 2.5) | 1.0 (−1.0 to 2.0) |
| P Valuea | <.0001 | .003 |
| 3 (5-15 y) (n = 78) | ||
| Median (range) | 1.5 (−1.5 to 2.5) | 1.0 (−2.0 to 3.0) |
| P Valuea | <.0001 | .03 |
Abbreviation: GAIS, Global Aesthetic Improvement Scale.
Sign test.
Discussion
To our knowledge, this is the first study to demonstrate the efficacy and durability of the endoscopic preperiosteal midface lift using objective, validated measurements. The endoscopic midface lift produces a median improvement in midfacial height or a shortening of the length of the lower eyelid of 3.4 mm (IQR, 2.3-4.4 mm; P < .001). This objective improvement is not only statistically significant, but also clinically meaningful, as demonstrated by significant improvements in the regional and global aesthetic scores assigned by 3 facial plastic surgeons. Improvements in IH, UCF, LCF, and global aesthetic appearance were seen after the endoscopic midface lift.
The benefit derived from this technique was shown to persist for more than 5 years after surgery. In patients examined 5 years to 15 years after surgery, there was a median decrease in midfacial height of 2.1 mm compared with their preoperative midfacial height (IQR, 0.8-3.1 mm; P < .001), indicating that the effects of the midface lift are maintained for years after the procedure. This sustained decrease in midfacial height and resultant elevated midfacial position is appreciated by observers, as reflected by significant improvements in regional aesthetic scores, including IH, UCF, and LCF scores. Infraorbital hollow scores remained improved by a median score change of 1 at 5 to 15 years’ follow-up. Increases in UCF and LCF scores were sustained at 3 to 5 years’ follow-up and patients tended to appear at or slightly better than their baseline at 5 to 15 years follow-up. Progressive midfacial fat compartmental volume loss in this period may account for the changes seen in these locations at longer follow-up.
Many of the patients included in this study underwent additional procedures either at the same time as the endoscopic midface lift or during the postoperative period. The effect of these additional procedures was examined to determine the true effect of the endoscopic midface lift. A multivariable regression analysis using a mixed-effects model demonstrated that having had filler administration during the follow-up period was not significantly associated with WIZDOM-MC (effect size, 0.15; P = .67); nor did it have an association with IH, UCF, LCF, or GAIS scores (effect size, 0.19; P = .13; effect size, −0.14; P = .24; effect size, −0.02; P = .88, and effect size, −0.07; P = .67, respectively). This finding is supported by a recent study by Mowlds and Lambros17 in which filler injection into the midface did not produce a change in the nasolabial fold or result in elevation of the midface. Interestingly, upper blepharoplasty appeared to have some association with WIZDOM-MC (effect size, 0.77; P = .03) and GAIS (effect size, 0.46; P = .003). Other procedures, including fat grafting, had no significant association with WIZDOM-MC (effect size, 0.25; P = .67) or GAIS (effect size, 0.15; P = .15).
The efficacy of other midface lift techniques has been studied in the literature. Marotta and Quatela5 assessed the effect of the endoscopic forehead midface lift in 15 patients and determined that the average reduction in the vertical height of the lower eyelid was 5.1 mm immediately after the procedure. In that study, the vertical height of the lower eyelid was defined as the distance from the ciliary margin to the lid-cheek junction measured from the midpupillary line. Although the metric used to determine lower eyelid length was different from that used in our study, their finding of reduced lower eyelid length after midface lift is similar to the reduction seen in our series. Interestingly, they compared the endoscopic forehead midface lift with blepharoplasty alone and showed that blepharoplasty alone had no significant association with the vertical length of the lower eyelid. This association was not measured in our study, as all patients in our series underwent lower blepharoplasty at the time of the midface lift; however, it does support the midface lift as the procedure responsible for the change in midfacial height.
The durability of other surgical approaches to the midface has been explored in the literature. In a recent study conducted by Pascali et al,11 the short- and long-term results of 2 midface lift techniques were evaluated using patient satisfaction questionnaires administered at 1 and 5 years postoperatively. The authors report that most patients remained satisfied with their appearance when surveyed at 1 and 5 years postoperatively and conclude that the effects of the midface lift persist over time. Saltz and Ohana7 reported on their 13-year experience performing the endoscopic midface lift. In this study, the average length of follow-up was 7 years; however, they report only descriptive data on postoperative appearance and postoperative complications. Ransom et al10 investigated the longevity of the endoscopic subperiosteal midface lift in 50 patients using objective, quantitative measures. They determined that a statistically significant decrease in lower eyelid height occurs after the endoscopic midface lift at 12 months postoperatively.
This study elucidates a precept that runs counter to the emphasis on complete ligamentous division being a prerequisite to successful facial rejuvenation. The efficacy of lower eyelid blepharoplasty without ligament release was the subject of a previous study.18 In this study, lower blepharoplasty was performed with and without ORL release. No significant difference in the improvement of the tear trough deformity or overall aesthetic result between patients who had ORL release and those who did not was found, with a significantly longer duration of swelling in those patients who underwent blepharoplasty with ORL release. This study supports the notion that complete ligamentous release is not a necessity and applies this concept to the midface. Our results suggest that a complete release of the midfacial ligaments is not necessary to achieve the desired aesthetic outcome in the midface. Rather, a reinforcement of the ligamentous support structures of the midface without a complete disruption of the midfacial ligaments appears to provide long-lasting aesthetic results.
This study shows that the endoscopic transtemporal preperiosteal midface lift is effective and long-lasting using objective measurements and validated aesthetic scales. This technique produces a significant decrease in midfacial height, which can be appreciated as a shortening of the lower eyelid and elevation of the midface to a more youthful position. Patients have sustained improvements in IH, UCF, and LCF that are identifiable to observers. Most patients continue to appear “better” than they did prior to surgery even 5 to 15 years after the procedure. This information is particularly useful in counseling patients and setting expectations before surgery.
Limitations
There are several limitations to this study, including its retrospective design and the complexity of objectively evaluating the midface. The WIZDOM-MC is a previously validated objective measurement of midfacial height specifically, but it does not quantify the midface in a 3-dimensional way. In an attempt to address this issue, validated midface specific scales were used. Additionally, all patients in this study underwent multiple procedures, including lower blepharoplasty. The association of lower blepharoplasty with the results is therefore unclear. A future study comparing the 2 groups to determine the true association of the lower blepharoplasty with midface lift outcomes is needed.
Conclusions
There is a significant, objective improvement in midfacial height after endoscopic midface lift that persists for at least 5 years and up to 15 years in the patients we were able to follow up. Validated midfacial scales demonstrate persistent improvements in midface appearance over time. Global aesthetic scales demonstrate that patients continue to appear better than before surgery after more than 5 years. This change is achieved without a complete disruption of the ligamentous support system of the midface.
References
- 1.Linkov G, Mally P, Czyz CN, Wulc AE. Quantification of the aesthetically desirable female midface position. Aesthet Surg J. 2018;38(3):231-240. doi: 10.1093/asj/sjx122 [DOI] [PubMed] [Google Scholar]
- 2.Sullivan SA, Dailey RA. Endoscopic subperiosteal midface lift: surgical technique with indications and outcomes. Ophthalmic Plast Reconstr Surg. 2002;18(5):319-330. doi: 10.1097/00002341-200209000-00002 [DOI] [PubMed] [Google Scholar]
- 3.Williams EF III, Vargas H, Dahiya R, Hove CR, Rodgers BJ, Lam SM. Midfacial rejuvenation via a minimal-incision brow-lift approach: critical evaluation of a 5-year experience. Arch Facial Plast Surg. 2003;5(6):470-478. doi: 10.1001/archfaci.5.6.470 [DOI] [PubMed] [Google Scholar]
- 4.Pascali M, Botti C, Cervelli V, Botti G. Midface rejuvenation: a critical evaluation of a 7-year experience. Plast Reconstr Surg. 2015;135(5):1305-1316. doi: 10.1097/PRS.0000000000001189 [DOI] [PubMed] [Google Scholar]
- 5.Marotta JC, Quatela VC. Lower eyelid aesthetics after endoscopic forehead midface-lift. Arch Facial Plast Surg. 2008;10(4):267-272. doi: 10.1001/archfaci.10.4.267 [DOI] [PubMed] [Google Scholar]
- 6.Seitz IA, Llorente O, Few JW. The transconjunctival deep-plane midface lift: a 9-year experience working under the muscle. Aesthet Surg J. 2012;32(6):692-699. doi: 10.1177/1090820X12452292 [DOI] [PubMed] [Google Scholar]
- 7.Saltz R, Ohana B. Thirteen years of experience with the endoscopic midface lift. Aesthet Surg J. 2012;32(8):927-936. doi: 10.1177/1090820X12462714 [DOI] [PubMed] [Google Scholar]
- 8.Le Louarn C. Concentric malar lift in the management of lower eyelid rejuvenation or retraction: a clinical retrospective study on 342 cases, 13 years after the first publication. Aesthetic Plast Surg. 2018;42(3):725-742. doi: 10.1007/s00266-018-1079-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abraham RF, DeFatta RJ, Williams EF III. Thread-lift for facial rejuvenation: assessment of long-term results. Arch Facial Plast Surg. 2009;11(3):178-183. doi: 10.1001/archfacial.2009.10 [DOI] [PubMed] [Google Scholar]
- 10.Ransom ER, Stong BC, Jacono AA. Persistent improvement in lower eyelid-cheek contour after a transtemporal midface lift. Aesthetic Plast Surg. 2012;36(6):1277-1282. doi: 10.1007/s00266-012-9963-5 [DOI] [PubMed] [Google Scholar]
- 11.Pascali M, Quarato D, Bocchini I, Cervelli V. Midface-lift patient satisfaction: a 5-year follow-up study. Indian J Plast Surg. 2016;49(3):329-335. doi: 10.4103/0970-0358.197223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wulc AE, Sharma P. Preperiosteal midface lift/transtemporal approach In: Hartstein ME, Wulc AE, Holck DEE, eds. Midfacial Rejuvenation. New York, NY: Springer; 2016:65-81. [Google Scholar]
- 13.Isse NG. Endoscopic facial rejuvenation. Clin Plast Surg. 1997;24(2):213-231. [PubMed] [Google Scholar]
- 14.Pu LL, Coleman SR, Cui X, Ferguson RE Jr, Vasconez HC. Autologous fat grafts harvested and refined by the Coleman technique: a comparative study. Plast Reconstr Surg. 2008;122(3):932-937. doi: 10.1097/PRS.0b013e3181811ff0 [DOI] [PubMed] [Google Scholar]
- 15.Carruthers J, Rzany B, Sattler G, Carruthers A. Anatomic guidelines for augmentation of the cheek and infraorbital hollow. Dermatol Surg. 2012;38(7 Pt 2):1223-1233. doi: 10.1111/j.1524-4725.2012.02478.x [DOI] [PubMed] [Google Scholar]
- 16.Narins RS, Brandt F, Leyden J, Lorenc ZP, Rubin M, Smith S. A randomized, double-blind, multicenter comparison of the efficacy and tolerability of restylane versus zyplast for the correction of nasolabial folds. Dermatol Surg. 2003;29(6):588-595. [DOI] [PubMed] [Google Scholar]
- 17.Mowlds DS, Lambros V. Cheek volumization and the nasolabial fold. Plast Reconstr Surg. 2018;141(5):1124-1129. doi: 10.1097/PRS.0000000000004341 [DOI] [PubMed] [Google Scholar]
- 18.Chan NJ, Nazemzadeh M, Hartstein ME, Holds JB, Massry GG, Wulc AE. Orbicularis retaining ligament release in lower blepharoplasty: assessing efficacy and complications. Ophthalmic Plast Reconstr Surg. 2018;34(2):155-161. doi: 10.1097/IOP.0000000000000902 [DOI] [PubMed] [Google Scholar]