Abstract
Background
Most extremely low gestational age neonates (ELGANS, postmenstrual age at birth (PMA) < 28 completed weeks) require supplemental oxygen and experience frequent intermittent hypoxemic and hyperoxemic episodes. Hypoxemic episodes and exposure to inadequately high concentrations of oxygen are associated with an increased risk of retinopathy of prematurity (ROP), chronic lung disease of prematurity (BPD), necrotizing enterocolitis (NEC), neurodevelopmental impairment (NDI), and death beyond 36 weeks PMA.
Closed-loop automated control of the inspiratory fraction of oxygen (FiO2-C) reduces time outside the hemoglobin oxygen saturation (SpO2) target range, number and duration of hypo- and hyperoxemic episodes and caregivers’ workload. Effects on clinically important outcomes in ELGANs such as ROP, BPD, NEC, NDI and mortality have not yet been studied.
Methods
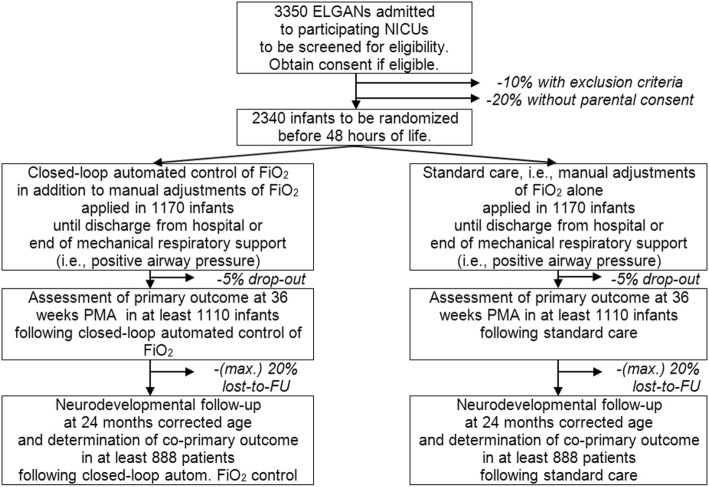
An outcome-assessor-blinded, randomized controlled, parallel-group trial was designed and powered to study the effect of FiO2-C (in addition to routine manual control (RMC) of FiO2), compared to RMC only, on death and severe complications related to hypoxemia and/or hyperoxemia. 2340 ELGANS with a GA of 23 + 0/7 to 27 + 6/7 weeks will be recruited in approximately 75 European tertiary care neonatal centers. Study participants are randomly assigned to RMC (control-group) or FiO2-C in addition to RMC (intervention-group). Central randomization is stratified for center, gender and PMA at birth (< 26 weeks and ≥ 26 weeks).
FiO2-C is provided by commercially available and CE-marked ventilators with an FiO2-C algorithm intended for use in newborn infants. The primary outcome variable (composite of death, severe ROP, BPD or NEC) is assessed at 36 weeks PMA (or, in case of ROP, until complete vascularization of the retina, respectively). The co-primary outcome variable (composite outcome of death, language/cognitive delay, motor impairment, severe visual impairment or hearing impairment) is assessed at 24 months corrected age.
Discussion
Short-term studies on FiO2-C showed improved time ELGANs spent within their assigned SpO2 target range, but effects of FiO2-C on clinical outcomes are yet unknown and will be addressed in the FiO2-C trial. This will ensure an appropriate assessment of safety and efficacy before FiO2-C may be implemented as standard therapy.
Trial registration
The study is registered at www.ClinicalTrials.gov: NCT03168516, May 30, 2017.
Keywords: Oxygen; Closed-loop automated control of the inspiratory fraction of oxygen (FiO2-C); Infant, premature; Intermittent hypoxemia and hyperoxemia
Background
Approximately 0.5% of all neonates (i.e., about 25,000 infants per year in Europe) are extremely low gestational age neonates (ELGANs), i.e. have a gestational age at birth (GA) < 28 completed weeks. The vast majority of ELGANs requires supplemental oxygen in addition to positive pressure respiratory support and frequently experience intermittent hypoxemic and hyperoxemic episodes. Intermittent hypoxemic episodes are predominantly caused by recurrent apnea due to immature development of the respiratory neuronal network (recently reviewed [1, 2]) but also secondary to active exhalation during mechanical ventilation [3]. Hyperoxemic episodes are usually a consequence of inappropriate adjustments of FiO2 (during routine manual control of FiO2 (RMC) but potentially also during closed-loop automated control of FiO2 (FiO2-C)).
Complications of prematurity associated with recurrent hypoxemic episodes
Retinopathy of prematurity (ROP)
Observational data indicated that both, severe and prolonged hypoxemic episodes [4–6], and wide fluctuations in oxygen levels [7], increase the risk of ROP. Whereas a better control of SpO2-levels was associated with a decreased risk of ROP [8].
Death and neurodevelopmental impairment (NDI)
Observational studies (recently reviewed in [9]) as well as SpO2 data recorded during the Canadian Oxygen Trial (COT [10],) suggest that late deaths (i.e. deaths beyond 36 weeks postmenstrual age (PMA)) and NDI (both cognitive and particularly motor impairment) are linked to hypoxemic episodes, particularly those of more than 60s duration [6].
Necrotizing enterocolitis (NEC)
The NeOProM (Neonatal Oxygen Prospective Meta-analysis) collaboration reported a lower rate of severe NEC (defined as NEC leading to abdominal surgery or death) in infants assigned to the higher SpO2 target range (91–95% compared to 85–89%) [11], which was linked to a lower proportion of time spent with SpO2 < 80%.
Complications of prematurity associated with hyperoxemic episodes
Considering that breathing room air (i.e., FiO2 = 0.21) leads to a relative hyperoxia compared to intrauterine oxygen partial pressures (PO2) and oxidative stress in preterm infants, hyperoxia, caused by inadequately high FiO2, is likely associated with long-term adverse effects [12].
ROP
The causal relationship between prolonged inappropriate exposure to high oxygen concentrations and ROP has long been established [13, 14]. More recently, the NeOProM studies showed increased rates of ROP with the higher SpO2-target range (91–95%) [11]. Finally, implementation of the higher SpO2-target range based on the results of the NeOProM studies, was associated with an increase in ROP rates in a recent observational study [15].
Death and NDI
Data from experimental studies in rodents indicate that higher levels of oxygen (e.g., FiO2 0.80 for 2 to 24 h [16–18]) trigger apoptotic neurodegeneration or white matter damage in the brain. These effects have been reviewed by Back et al. [19].
Chronic lung disease of prematurity (BPD)
Hyperoxia enhancing generation of reactive oxygen species triggers inflammatory processes, tissue damage and cell death in the preterm infant’s lung, eventually resulting in an increased risk of BPD development (recently reviewed in [20]).
Controlling of FiO2
To protect ELGANs from the detrimental effects of hypoxemic and hyperoxemic episodes, it can be assumed that PO2 (and in appropriate simplification SpO2) must be kept within a narrow target range. To achieve this goal despite the infants’ irregular breathing patterns and variations in lung aeration and function, frequent cautious adjustments of FiO2 are required, which are challenging, time consuming and often impossible due to limited personnel resources.
It has repeatedly been shown that FiO2-C increases the time infants spent within the SpO2-target range and reduces the burden of hyper−/hypoxemia while being safe and accurate in short-term studies (reviewed in [21, 22]). The effects of FiO2-C on clinically relevant outcomes measures (such as the hypoxia and hyperoxia-associated complications of prematurity described above) and the safety of its long-term continuous application, however, have yet to be elucidated.
Methods/design
Trial objectives
The proposed trial was designed and is powered to compare the effect of FiO2-C in addition to manual adjustments, in comparison with RMC of FiO2 only, on death, NDI and severe complications of prematurity thought to be related to hypoxia/hyperoxia in ELGANs.
Trial design
This is an outcome-assessor-blinded, randomized-controlled, multicenter parallel group comparison of phase III for superiority (evaluating FiO2-C in addition to RMC of FiO2 in comparison to RMC of FiO2 only) in ELGANs.
In Germany, this study is also considered as a phase IV pharmaceutical trial on safety of the investigational medication ‘oxygen’ using different modes of administration (decision of the German authority BfArM according to §4 para. 23,1 of the German Pharmaceutical Act). This may not apply to other countries.
Setting
Patients will be recruited in approximately 75 European tertiary care neonatal centers. Recruitment has started in Germany and is intended to expand to additional sites in other European countries, after appropriate approvals will have been obtained.
Patients
Inclusion criteria
GA at birth 23 + 0/7 to 27 + 6/7 weeks
Exclusion criteria
Decision not to provide full life support / decision for palliative care only before study entry
Severe congenital abnormalities (particularly those affecting respiratory, cardiovascular or gastrointestinal function or long-term neuro-cognitive development, whereas patent ductus arteriosus, patent foramen ovale (PFO), and atrial septal defects type II (ASDII) are not considered a congenital anomaly in preterm infants)
Postnatal age > 48 h
Lack of parental consent
Lack of device enabling closed-loop automatic control of FiO2 before randomization
Randomization and allocation concealment
Study participants are randomly assigned in a 1:1 ratio to FiO2-C in addition to RMC of FiO2 (test intervention) or RMC of FiO2 only (control intervention).
A web-based randomization tool provided by the Interdisciplinary Center of Clinical Studies at the University Medical Center of the Johannes Gutenberg University Mainz is being used in this study. This program enables bound (into the same treatment group) or free (into different treatment groups) randomization of multiples based on parental choice and the number of available devices enabling FiO2-C.
A minimization algorithm is applied to preferentially aim for an even distribution of treatment assignment in both GA strata (i.e. < 26 weeks and ≥ 26 weeks; 1st priority) and both gender strata (2nd priority) within each center.
Blinding
This study is outcome-assessor-blinded, meaning that the personnel performing the ophthalmological examinations throughout the initial hospitalization as well as the personnel performing the neurocognitive evaluation at 24 months corrected age will be blinded to the infants’ treatment group assignment. Blinding of doctors, nurses, and parents is not possible with this type of study interventions.
Study intervention
FiO2-C is provided by commercially available and CE marked infant ventilators with a FiO2-C algorithm intended for use in preterm infants. The FiO2-C algorithm must have been tested in human infants and shown to increase the %-time spent in the assigned SpO2 target range or to reduce the time in hypoxemia or hyperoxemia or to reduce the incidence/duration of hypoxemic or hyperoxemic episodes.
Each FiO2-C algorithm should be applied in its “optimal mode” (with respect to potentially variable settings provided by the manufacturer such as: averaging time of SpO2-input, response/wait-time, etc.) based on either evidence in the literature or consensus of the users.
Manual adjustments are encouraged whenever automatic FiO2 settings seem sub-optimal. In case of FiO2/SpO2-oscillations brought about by FiO2-C, settings need to be adapted or FiO2-C has to be temporarily interrupted.
Whenever possible, every study center will use only one type of FiO2-C algorithm.
Infants in the control group are treated (whenever possible) with the same type of infant ventilator for respiratory support (FiO2-C turned off) and RMC of FiO2 is applied by bedside nurse and medical staff throughout the initial hospitalization.
Care is taken in both groups that all staff are informed about the relevance of intermittent hypoxemia and hyperoxemia and trained to execute prudent and careful RMC of FiO2. This training may include a standard operating procedure for RMC, where the speed of increase/decrease in FiO2 depends on the magnitude of deviation from the SpO2 target range as previously described [23, 24].
The intervention should start as soon as possible after randomization and within 48 h after birth. The scheduled end of the study intervention is any of the following (whichever comes first):
death
discharge home from hospital
transfer to another hospital where FiO2-C is not available (whereas such transfer is discouraged)
a PMA of 36 + 0/7 weeks
-
final discontinuation of positive pressure respiratory support, which does not include limited periods without positive pressure support for weaning.
If the infant requires positive pressure respiratory support again for any reason, the infant should again be supported by FiO 2 -C (provided a device supporting FiO 2 -C is available) until (other) criteria for scheduled end of study intervention are met.
a PMA of > 32 + 0/7 weeks provided the following two additional criteria of respiratory stability are both met:
◦ A) FiO2 = 0.21 for ≥48 h (for this criterion limited time periods with higher FiO2 for rescue or for recovery of intermittent hypoxemia will not be considered)
and
◦ B) less than 5 intermittent hypoxemic episodes with an SpO2 < 80% per 8 h shift.
If criteria A) or B) are no longer met, the infant should again be supported by the FiO 2 -C device until (other) criteria for scheduled end of study intervention are met.
a PMA of > 32 + 0/7 weeks if the infant has to be transferred to an intermediate care unit where FiO2-C is not available
If the infant is re-admitted to intensive care, the infant should again be supported by FiO 2 -C (provided a device supporting FiO 2 -C is available) until (other) criteria for scheduled end of study intervention are met.
After the end of the study intervention, all study participants will be treated according to the state of the art care and local standards without further requirements or restrictions.
Concomitant interventions and medication
Any concomitant medication that is clinically considered necessary for the patient will be allowed within the study, except for the control group, where closed-loop automatic control of FiO2 or any other automatic control of airway pressure/respiratory support etc. based on SpO2 or other vital signals are not allowed.
SpO2 measurements to guide FiO2-C
All FiO2-Controllers should be based on SpO2-data generated by the same pulse oximeter technology (Masimo). In general, pre-ductal SpO2-sensor placement is preferred to guide FiO2-C as long as echocardiography demonstrates a patent ductus arteriosus.
SpO2-targets and alarm settings
The SpO2-target range selected by a center for clinical routine has to fulfill the following criteria:
Study centers need to have a written guideline on SpO2-target range to ensure that the same SpO2-target range is applied in both study groups
The SpO2-target has to be within the range of 87–95% (may include 87% and/or 95%),
Care has to be taken that the same SpO2-target ranges are applied in clinical routine and in both study groups
Documentation of the study intervention
In both study groups, the type of respiratory support, the type of ventilator and the application of FiO2-C have to be documented daily during the intervention period on a treatment log.
Primary outcome
The primary outcome measure is a composite of death, BPD or NEC assessed at 36 weeks PMA and severe ROP assessed when full vascularization of the retina is documented.
Definitions of components of the primary outcome
Severe ROP
Defined as any ROP stage 3 or higher, or acute posterior ROP, or any ROP in Zone 1, or any treatment for ROP. ROP will be diagnosed at routine ophthalmological examinations, beginning at a PMA of 32 weeks according to international recommendations and local standards until complete vascularization of the retina [25]. The severity of ROP will be graded according to the international classification [26].
BPD
Defined as requiring positive pressure support or supplemental oxygen at 36 weeks ±2 days PMA, including an oxygen reduction test for infants requiring less than 0.3 FiO2, representing ‘moderate’ or ‘severe’ BPD according to the National Institute of Child Health and Development consensus definition [27].
NEC
Defined as modified Bell stage ≥IIa [28] until 36 weeks PMA.
Co-primary outcome
The co-primary outcome (tested in a hierarchical design) is the composite outcome of death, language or cognitive delay, motor impairment, severe visual impairment or hearing impairment, all assessed at 24 ± 1 months corrected age.
Definitions of components of the co-primary outcome
Language or Cognitive delay: Defined as a language or cognitive composite score at the Bayley Scales of Infant Development 3rd edition [29] of < 85.
Motor impairment: Defined as a Gross Motor Function Classification System (GMFCS) score of 2–5 [25].
Severe visual impairment: Defined as best corrected vision in the better eye yields a visual acuity less than 6/60 m (20/200 ft) according to the relevant doctor’s reports / discharge summary.
Severe hearing impairment: need for a hearing aid or cochlear implant.
Any clinical suspicion of previously undiagnosed visual or hearing problems during the FiO2-C follow-up visit requires a referral to an eye specialist or an pedaudiologist.
If the parents refuse the assessment at the study center or if Bayley test cannot be performed:
Other assessments of neurocognitive and motor development will betaken into account, if parents refuse to attend the follow-up.
Cognitive- and language-composite-scores will then be imputed as follows:
A score “> 85” will be imputed if
a different cognitive test has been performed elsewhere and scored higher than 1SD below the mean
the family pediatrician/doctor/health professional caring for the child or the parents rate the infant as “normal”
A score “< 85” will be imputed if
a different cognitive test has been performed elsewhere and scored lower than 1SD below the mean
the family pediatrician/doctor/health professional caring for the child or the parents rate the infant as “delayed” or “impaired”.
Any such imputation will be described in the final report and the scientific publication.
Secondary outcomes
Key secondary outcome variables are the individual components of the primary (death, severe ROP, BPD, NEC) and co-primary outcome variables (death, cognitive delay or language delay, motor impairment (GMFCS score of 2–5 [30]), as well as severe visual or hearing impairment,, the composite scores of the Bayley Scales (3rd edition), the rate of cerebral palsy (CP) according to the criteria defined by the European network ‘Surveillance of CP in Europe’, and the GMFCS score.
In addition to ‘severe ROP’ as component of the primary outcome, the ‘ROP Severity Score’ (also entitled ‘ROP activity and structure score’) [31] is assessed as secondary outcome, enabling better differentiation and likely being more relevant for functional outcome.
Ethical considerations
The Helsinki Declaration shall be applied to the clinical trial, as well as Good Clinical Practice (GCP). The protocol was submitted and approved by the Ethics Committee of the University Hospital Tübingen as the lead ethics committee. Furthermore, the relevant ethics committees responsible for any of the participating study sites will have to approve participation of the site.
Community engagement
A freely accessible web page for FiO2-C has been set up (www.fioc-study.eu), providing an overview of aims, partners, study outline, progress and milestones, meetings, findings and news.
Form of consent
Written informed consent from parents or legal guardians is required for participation in the study.
Insurance
Where required by national law, insurance will be obtained for all study patients.
Sample size, power and study duration
The required sample size was calculated for the primary research hypothesis that the implementation of FiO2-C reduces the cumulative incidence of the composite primary outcome (death, severe ROP, BPD, or NEC).
The co-primary research hypothesis is that FiO2-C also reduces death or severe NDI (see outcome measures for details). These hypotheses are assessed as a-priori ordered hypotheses, where the co-primary hypothesis will only be tested in a confirmatory manner if the primary hypothesis has been confirmed. Consequently, no correction for multiple testing will be performed.
We assume that,
the cumulative incidence of the primary composite outcome of this study is 50% in the control group
FiO2-C reduces the burden of severe hypoxemia/hyperoxemia by 25–50% and (based on the assumption that (again) 25–50% of the outcome is associated with recurrent hypo−/hyperoxemia) effects a relative risk reduction in this outcome by at least 12.5%.
In summary, we assume a reduction in the primary outcome from 50% (in the control group) to 44% in the intervention group (FiO2-C).
Sample size calculations were based on a Χ2-test, assuming a power of 80% and a significance level of 5%. Based on these assumptions, 1110 infants are required in each treatment group (total 2220 infants). Because all components of this primary outcome will be determined during the initial hospitalization (i.e. until first discharge from neonatal care), the rate of drop-out before ascertainment of the primary outcome will be low as < 5%. Hence, a total of 2340 infants need to be enrolled and randomized (see Fig. 1).
Fig. 1.
Anticipated Trial Flow
Assuming an incidence of 50% for the co-primary outcome in the control group and a relative risk reduction (RRR) of 25% for the co-primary outcome in the FiO2-C group, the proposed sample size will have a power > 80% to prove this difference even if up to 20% of randomized infants will be lost to follow-up until 24 months corrected age.
It is estimated that about 90% of all ELGANs will qualify for inclusion into this study without any exclusion criteria. Estimating a participation rate of 80%, approximately 3350 infants have to be screened.
We estimate a recruitment of about 65 patients per month and therefore the recruitment phase of the study will last for approximately 36 months. The individual participation in the study will be about 27 months (between 56 and 91 days of treatment – depending on GA at birth - with an additional follow up to 24 months corrected age).
Data analysis
Analysis of the primary outcome will be based on the intention to treat analysis set, which comprises all randomized patients. Portions of infants with primary endpoint will be compared in a statistical model that accounts for the factors considered by the randomization procedure and the randomization of twins and other multiples. The treatment effect will be reported as a risk ratio and as a risk difference with 95% confidence interval. The co-primary outcome will be assessed only if superiority of FiO2-C with respect to the primary outcome is confirmed at the 2-sided level of 0.05. This hierarchical testing procedure maintains a multiple type I error of 0.05. All statistical analyses will be described in detail in a statistical analysis plan completed before closure of the database. An interim analysis for efficacy is not intended.
Monitoring safety
An independent Data Monitoring Committee (DMC) is instituted and monitors recruitment, compliance, and safety parameters after 50, 100, 200 and 300 patients have completed 44 + 0/7 weeks PMA, and after every 200 patients have reached this age thereafter.
Safety parameters
Safety parameters monitored by the DMC include:
Early deaths (for the DMC defined as < 44 weeks PMA), late deaths (for the DMC defined as ≥44 weeks PMA), all deaths, BPD, discharge on home oxygen or home positive pressure respiratory support, severe ROP, NEC, (focal) intestinal perforation requiring laparotomy, PDA requiring treatment, intraventricular hemorrhage >grade 2, cystic periventricular leukomalacia. Because the safety parameters include components of the primary outcome, the incidence rates and 95% confidence intervals, these parameters will be ‘coded’ as “safety parameter A-I”.
Furthermore, safety analyses include occurrence and rates of reported adverse events and incidents by treatment group.
Regulatory aspects
Trial sponsor
Sponsor of the FiO2-C-trial is the University Hospital Tübingen, Geissweg 3, 72,076 Tübingen, Germany. Contact is available at fioc@med.uni-tuebingen.de.
Medical ethics committees
At the time of submission, the relevant ethics committee in Germany approved the study. Applications for approvals are currently underway in additional countries (e.g., the Netherlands and Switzerland).
National Regulatory/competent authorities
At the time of submission, the National Regulatory/Competent Authority of Germany (BfArM) approved the study. Authority approval may not be necessary elsewhere – but this will be determined in collaboration with the relevant ethics committees.
Discussion
Need for a trial
Oxygen is one of the drugs most frequently used in ELGANs and yet, our knowledge on the optimal level of oxygen in arterial blood (or in appropriate simplification the optimal target range for SpO2) and even optimal technology for monitoring oxygen levels is incomplete [32–34]. Short-term studies in preterm infants demonstrated that FiO2-C improved the time within the assigned SpO2 target range. In these studies, percent time within the assigned SpO2 target range increased by approximately 10% points to around 70–90% and the improvement was independent of the SpO2 target range, the FiO2-C algorithm, and the proportion of time spent within SpO2 target range in the control-group [21, 22, 35, 36]. It is, however, unclear if more time spent within the assigned SpO2 target range will also translate into positive long-lasting effects on clinically relevant outcomes. For example, despite higher proportions of time spent within the SpO2 target range, FiO2-C might on the one hand side reduce the amplitude of SpO2 fluctuations, but, at the same time increase the frequency of SpO2 oscillations and thereby might carry additional risks. This randomized controlled trial will ensure an appropriate assessment of safety and efficacy of FiO2-C, before it is implemented into standard care.
Discussion of the study intervention period
The study intervention period was chosen because Di Fiore et al. showed that hypoxemic episodes evolve over the first 2 weeks of life and hence starting the intervention within 48 h after birth seems appropriate. This will enable a reasonable time frame to inform parents, even if birth of the infant occurs at night or on weekends, and to enable a meaningful parental decision on participation.
As described by Di Fiore et al. [5] and confirmed by Poets et al. [6], hypoxemic episodes occurring beyond the 4th week of life are more strongly associated with adverse long-term outcomes than hypoxemic episodes occurring within the first 4 weeks of life. Hence, the study intervention should not end at 32 weeks PMA. Infants with prolonged and frequent hypoxemic episodes beyond this age may benefit most from effective FiO2-C.
Discussion of chosen population
Because diseases thought to be related to inappropriate use of oxygen such as ROP and BPD essentially only occur in ELGANs, an assessment of efficacy and safety of long-term application of FiO2-C can only be performed in this patient population.
Discussion of chosen SpO2-target range
The NeOProM collaboration has shown that the higher SpO2-target range of 91 to 95% is associated with a decreased risk of early deaths at 18 to 24 months corrected age and NEC, but with an increased risk of ROP [11]. Furthermore, a post-hoc analysis of the BOOST-II data indicated that a higher proportion of time within the assigned target range could enhance this beneficial effect [37]. Consequently, in the FiO2-C trial the lower limit of the center-specific SpO2 target range has to be set to ≥87% SpO2.
Trial status
Protocol version 4: April, 26th, 2018. Recruitment has started in July 2018 and is expected to be finalized in July 2021. The last patient out (after follow-up) will be expected in October 2023.
Acknowledgements
We would like to thank the members of the Data Monitoring Committee: Josef Högel (University Hospital Ulm) and Gerhard Jorch (University Children’s Hospital Magdeburg).
The FiO2-C investigators acknowledge the contribution of Masimo Inc. (Irvine, CA), who provided Radical 7C pulse oximeters for the conduct of the study.
FiO 2 -C Study Group
Coordinating Investigator: Axel R. Franz (University Children’s Hospital Tübingen, Germany; corresponding and senior author)
Steering Committee: Axel R. Franz, Corinna Engel, and Christian F. Poets (University Children’s Hospital Tübingen, Tübingen, Germany); Helmut Hummler (Children’s Hospital University of Ulm, Ulm, Germany); Michael S. Urschitz and Jochem König (University Medical Center of the Johannes Gutenberg-University Mainz, Mainz, Germany), Hendrik J. Niemarkt (Máxima Medical Centre Veldhoven, Veldhoven, The Netherlands), Dirk Bassler (Universitätsspital Zürich, Zürich, Switzerland)
Data Management, Biometry, Monitoring and Study Coordination, all at the Center for Pediatric Clinical Studies, University Children’s Hospital Tübingen: Corinna Engel, Christian A. Maiwald, Gabriele von Oldershausen, Iris Bergmann, Monika Weiss, Caroline J. B. R. Wichera, Andreas Eichhorn, Michael Raubuch, Birgit Schuler.
Recruiting Hospitals and Local Principal Investigators
(Sorted by country, in alphabetical order):
Germany:
Klinik für Kinder- und Jugendmedizin, Universitätsklinikum Aachen, Mark Schoberer and Sonja Trepels-Kottek;
Klinik für Kinder und Jugendliche, KJF Klinik Josefinum Augsburg, Thomas M.K. Völkl and Sibylle C. Horsinka;
Diakonie Krankenhaus Bad Kreuznach kreuznacherdiakonie, Edmondo N.L. Hammond and Christoph von Buch;
Universitätskinderklinik Bochum, Perinatalzentrum, St.-Elisabeth-Hospital, Norbert Teig and Susanne Dettmers;
Klinikum Links der Weser, Bremen, Hans Thorsten Körner and Birte Tröger;
Klinik für Kinder- und Jugendmedizin Chemnitz, Annika Ander and Axel Hübler;
Universitätsklinikum Carl Gustav Carus, Dresden, Barbara Seipolt and Lars Mense;
Universitätsklinikum Düsseldorf, Klinik für Allgemeine Pädiatrie, Neonatologie und Kinderkardiologie, Thomas Hoehn and Klaus Lohmeier;
Helios Klinikum Erfurt, Hans-Jörg Bittrich and Kathrin Roefke;
Klinikum Esslingen, Christian von Schnakenburg and Klaus Niethammer;
Department of Neonatology, Medical Center- University of Freiburg, Faculty of Medicine, Freiburg, Hans Fuchs and Daniel Klotz;
Universitätsklinikum Hamburg-Eppendorf, Monika Wolf and Sarah Kabisch;
Auf der Bult, Kinder- und Jugendkrankenhaus, Hannover, Anna Koluch and Sandra Idel;
Medizinische Hochschule Hannover, Bettina Bohnhorst and Corinna Peter;
Universitätsklinikum des Saarlandes und Medizinische Fakultät der Universität des Saarlandes, Homburg, Sascha Meyer, Harald Sauer and Kathrin Lorenz;
Städtisches Klinikum Karlsruhe, Joachim Kühr and Sandra Holz;
University of Leipzig, Dept. of Women and Children’s Health, Children’s Hospital, Division of Neonatology, Ulrich H. Thome, Benjamin W. Ackermann and Corinna Gebauer;
St. Elisabethen Krankenhaus Lörrach, Catrice Celanowski, Hubert Fahnenstich and Cecil Kannan;
University Medical Center of the Johannes Gutenberg-University Mainz, Eva Mildenberger, André Kidszun and Julia Winter;
Children’s Hospital, University Hospital Marburg, Rolf F. Maier and Hana Voss;
Klinikum Memmingen, Ralf Pallacks, Kirsten M. Lang and André Gatti;
Division of Neonatology, University Children’s Hospital Dr. v. Hauner and Perinatal Center, University Hospital, LMU Munich, Andreas W. Flemmer and Susanne Herber-Jonat;
Klinik für Neonatologie, München, Klinik Schwabing, Marcus Krüger and Daniela Reber;
Department of General Pediatrics, University Children’s Hospital Muenster, Münster, Julia Sandkötter and Katja Masjosthusmann;
St. Franziskus-Hospital, Münster, Florian Urlichs and Thomas Frank;
Cnopfsche Kinderklinik, Nürnberg, Michael Schroth and Christian Grillhösl;
Division of Neonatology, University Children’s Hospital Regensburg (KUNO), University of Regensburg, Regensburg, Jochen Kittel, Holger Michel and Sven Wellmann;
Klinikum am Steinenberg/Ermstalklinik, Reutlingen, Hans-Christoph Schneider and Anja Mayer;
Krankenhaus Leopoldina der Stadt Schweinfurt, Hans-Martin Lode and Daniel Lorenz;
Diakonissen-Stiftungs-Krankenhaus, Speyer, Axel T. Bosk and Torben Lindner;
Klinikum Stuttgart, Olgahospital, Matthias Vochem and Patrick Neuberger;
Universitätsklinikum Tübingen, Abteilung für Neonatologie, Axel R. Franz and Jörg Arand;
Children’s Hospital University of Ulm, Marc R. Mendler and Jochen Essers;
Schwarzwald-Baar-Klinikum Villingen-Schwenningen, Christian Bender and Jessica Beckmann;
Rems-Murr-Kliniken, Winnenden, Ralf Rauch and Ulrich Bernbeck;
Kinderklinik und Poliklinik des Universitätsklinikums Würzburg, Kirsten Glaser and Johannes Wirbelauer
The Netherlands:
University Medical Center Rotterdam, André A. Kroon and Tom Goos;
Máxima Medical Centre Veldhoven, Hendrik J. Niemarkt and Thilo Mohns;
Isala Kliniek Zwolle, Henrica L.M. van Straaten and Estelle E.M. Mulder
Switzerland:
Department of Neonatology, UniversitätsSpital Zurich and University of Zurich, Zurich, Switzerland, Dirk Bassler und Mara Hesse
Abbreviations
- ASDII
Atrial Septal Defect II
- BfArM - Federal Institute for Drugs and Medical Devices
Bundesinstitut für Arzneimittel und Medizinprodukte
- BMBF - German Federal Ministry of Education and Research
Bundesministerium für Bildung und Forschung
- BPD
Chronic lung disease of prematurity
- CP
Cerebral palsy
- eCRF
Electronical case report form
- ELGANs
Extremely low gestational age neonates
- FiO2-Controller / FiO2-C
Closed loop automated control of FiO2
- GA
Gestational age
- GMFCS
Gross Motor Function Classification System
- NDI
Neurodevelopmental impairment
- NEC
Necrotizing enterocolitis
- paO2
Arterial oxygen partial pressures
- PFO
Patent foramen ovale
- PO2
Oxygen partial pressures
- RMC
Routine manual control
- ROP
Retinopathy of prematurity
- RRR
Relative risk reduction
Authors’ contributions
CAM drafted the first version of the manuscript. HJN, CFP, MSU, JK, HH, DB, CE, and ARF, as well as all other members of the FiO2-C study group revised the manuscript and made important contributions. All authors have read and approved the final manuscript.
Funding
This study is funded by the German Federal Ministry of Education and Research (BMBF) under grant agreement No. BMBF-Fz01KG1602. The grant was approved following peer-review of the application including key-features of this study protocol (study population, intervention, outcome measures, statistical analyses). The BMBF had no influence on the design of the study, on collection, analysis and interpretation of data and on writing this manuscript.
Publication of this manuscript was supported by Deutsche Forschungsgemeinschaft and the Open Access Publishing Fund of the University of Tübingen, Germany. They had no influence on the design of the study, on collection, analysis and interpretation of data and on writing this manuscript.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed for the current manuscript.
Ethics approval and consent to participate
The FiO2-C trial is performed in accordance with the Declaration of Helsinki and the guidelines of Good Clinical Practice (GCP). Patients can only be enrolled into the study after informed written consent was given by both parents/guardians (by the only parent/guardian in case of single-parent/guardian families). In case parents are less than 18 years of age, the relevant legal guardian(s) of the child has/have to sign the informed consent.
At the time of publication, the FiO2-C trial is currently conducted in Germany and may expand to other countries, once ethical and (if appropriate) authority approval has been obtained.
Ethics: Ethics Committee at the University Hospital Tuebingen, reference no. 170/2018AMG1, approved;
Authority: Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM), reference no. 4042695 approved conduct.
Consent for publication
Not applicable.
Competing interests
C.F. Poets received speaker honoraria from Masimo Inc. and Sentec. All other contributors declare that they do not have competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Christian A. Maiwald, Email: Christian.Maiwald@med.uni-tuebingen.de
Hendrik J. Niemarkt, Email: Hendrik.Niemarkt@mmc.nl
Christian F. Poets, Email: Christian-F.Poets@med.uni-tuebingen.de
Michael S. Urschitz, Email: urschitz@uni-mainz.de
Jochem König, Email: koenigjo@uni-mainz.de.
Helmut Hummler, Email: helmut.hummler@uni-ulm.de.
Dirk Bassler, Email: Dirk.Bassler@usz.ch.
Corinna Engel, Email: Corinna.Engel@med.uni-tuebingen.de.
Axel R. Franz, Email: Axel.Franz@med.uni-tuebingen.de
FiO2-C Study Group:
Axel R. Franz, Corinna Engel, Christian F. Poets, Helmut Hummler, Michael S. Urschitz, Jochem König, Hendrik J. Niemarkt, Dirk Bassler, Christian A. Maiwald, Gabriele von Oldershausen, Iris Bergmann, Monika Weiss, Caroline J. B. R. Wichera, Andreas Eichhorn, Michael Raubuch, Birgit Schuler, Mark Schoberer, Sonja Trepels-Kottek, Thomas M. K. Völkl, Sibylle C. Horsinka, Edmondo N. L. Hammond, Christoph von Buch, Norbert Teig, Susanne Dettmers, Hans Thorsten Körner, Birte Tröger, Annika Ander, Axel Hübler, Barbara Seipolt, Lars Mense, Thomas Hoehn, Klaus Lohmeier, Hans-Jörg Bittrich, Kathrin Roefke, Christian von Schnakenburg, Klaus Niethammer, Hans Fuchs, Daniel Klotz, Monika Wolf, Sarah Kabisch, Anna Koluch, Sandra Idel, Bettina Bohnhorst, Corinna Peter, Sascha Meyer, Harald Sauer, Kathrin Lorenz, Joachim Kühr, Sandra Holz, Ulrich H. Thome, Benjamin W. Ackermann, Corinna Gebauer, Catrice Celanowski, Hubert Fahnenstich, Cecil Kannan, Eva Mildenberger, André Kidszun, Julia Winter, Rolf F. Maier, Hana Voss, Ralf Pallacks, Kirsten M. Lang, André Gatti, Andreas W. Flemmer, Susanne Herber-Jonat, Marcus Krüger, Daniela Reber, Julia Sandkötter, Katja Masjosthusmann, Florian Urlichs, Thomas Frank, Michael Schroth, Christian Grillhösl, Jochen Kittel, Holger Michel, Sven Wellmann, Hans-Christoph Schneider, Anja Mayer, Hans-Martin Lode, Daniel Lorenz, Axel T. Bosk, Torben Lindner, Matthias Vochem, Patrick Neuberger, Jörg Arand, Marc R. Mendler, Jochen Essers, Christian Bender, Jessica Beckmann, Ralf Rauch, Ulrich Bernbeck, Kirsten Glaser, Johannes Wirbelauer, André A. Kroon, Tom Goos, Thilo Mohns, Henrica L. M. van Straaten, Estelle E. M. Mulder, and Mara Hesse
References
- 1.Di Fiore JM, Martin RJ, Gauda EB. Apnea of prematurity--perfect storm. Resp Physiol Neurobi. 2013;189(2):213–222. doi: 10.1016/j.resp.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 2.Martin RJ, Di Fiore JM, Macfarlane PM, Wilson CG. Physiologic basis for intermittent hypoxic episodes in preterm infants. Adv Exp Med Biol. 2012;758:351–358. doi: 10.1007/978-94-007-4584-1_47. [DOI] [PubMed] [Google Scholar]
- 3.Bolivar JM, Gerhardt T, Gonzalez A, Hummler H, Claure N, Everett R, et al. Mechanisms for episodes of hypoxemia in preterm infants undergoing mechanical ventilation. J Pediatr. 1995;127(5):767–773. doi: 10.1016/S0022-3476(95)70171-0. [DOI] [PubMed] [Google Scholar]
- 4.Di Fiore JM, Bloom JN, Orge F, Schutt A, Schluchter M, Cheruvu VK, et al. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J Pediatr. 2010;157(1):69–73. doi: 10.1016/j.jpeds.2010.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Fiore JM, Kaffashi F, Loparo K, Sattar A, Schluchter M, Foglyano R, et al. The relationship between patterns of intermittent hypoxia and retinopathy of prematurity in preterm infants. Pediatr Res. 2012;72(6):606–612. doi: 10.1038/pr.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poets CF, Roberts RS, Schmidt B, Whyte RK, Asztalos EV, Bader D, et al. Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. JAMA. 2015;314(6):595–603. doi: 10.1001/jama.2015.8841. [DOI] [PubMed] [Google Scholar]
- 7.Cunningham S, Fleck BW, Elton RA, McIntosh N. Transcutaneous oxygen levels in retinopathy of prematurity. Lancet. 1995;346(8988):1464–1465. doi: 10.1016/S0140-6736(95)92475-2. [DOI] [PubMed] [Google Scholar]
- 8.Chow LC, Wright KW, Sola A. Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants? Pediatrics. 2003;111(2):339–345. doi: 10.1542/peds.111.2.339. [DOI] [PubMed] [Google Scholar]
- 9.Martin RJ, Wang K, Koroglu O, Di Fiore J, Kc P. Intermittent hypoxic episodes in preterm infants: do they matter? Neonatology. 2011;100(3):303–310. doi: 10.1159/000329922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidt B, Whyte RK, Asztalos EV, Moddemann D, Poets C, Rabi Y, et al. Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. Jama. 2013;309(20):2111–20. doi: 10.1001/jama.2013.5555. [DOI] [PubMed] [Google Scholar]
- 11.Askie LM, Darlow BA, Finer N, Schmidt B, Stenson B, Tarnow-Mordi W, et al. Association between oxygen saturation targeting and death or disability in extremely preterm infants in the neonatal oxygenation prospective meta-analysis collaboration. JAMA. 2018;319(21):2190–2201. doi: 10.1001/jama.2018.5725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saugstad OD. Oxidative stress in the newborn--a 30-year perspective. Biol Neonate. 2005;88(3):228–236. doi: 10.1159/000087586. [DOI] [PubMed] [Google Scholar]
- 13.Kinsey VE. Retrolental fibroplasia; cooperative study of retrolental fibroplasia and the use of oxygen. AMA Arch Ophthalmol. 1956;56(4):481–543. doi: 10.1001/archopht.1956.00930040489001. [DOI] [PubMed] [Google Scholar]
- 14.Patz A, Hoeck LE, De La Cruz E. Studies on the effect of high oxygen administration in retrolental fibroplasia. I. Nursery observations. Am J Ophthalmol. 1952;35(9):1248–1253. doi: 10.1016/0002-9394(52)91140-9. [DOI] [PubMed] [Google Scholar]
- 15.Holmstrom G, Tornqvist K, Al-Hawasi A, Nilsson A, Wallin A, Hellstrom A. Increased frequency of retinopathy of prematurity over the last decade and significant regional differences. Acta Ophthalmol. 2018;96(2):142–148. doi: 10.1111/aos.13549. [DOI] [PubMed] [Google Scholar]
- 16.Felderhoff-Mueser U, Bittigau P, Sifringer M, Jarosz B, Korobowicz E, Mahler L, et al. Oxygen causes cell death in the developing brain. Neurobiol Dis. 2004;17(2):273–282. doi: 10.1016/j.nbd.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 17.Gerstner B, DeSilva TM, Genz K, Armstrong A, Brehmer F, Neve RL, et al. Hyperoxia causes maturation-dependent cell death in the developing white matter. J Neurosci. 2008;28(5):1236–1245. doi: 10.1523/JNEUROSCI.3213-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brehmer F, Bendix I, Prager S, van de Looij Y, Reinboth BS, Zimmermanns J, et al. Interaction of inflammation and hyperoxia in a rat model of neonatal white matter damage. PLoS One. 2012;7(11):e49023. doi: 10.1371/journal.pone.0049023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Back SA, Rosenberg PA. Pathophysiology of glia in perinatal white matter injury. Glia. 2014;62(11):1790–1815. doi: 10.1002/glia.22658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: a review of pathogenesis and pathophysiology. Respir Med. 2017;132:170–177. doi: 10.1016/j.rmed.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poets CF, Franz AR. Automated FiO2 control: nice to have, or an essential addition to neonatal intensive care? Arch Dis Child-Fetal. 2017;102(1):F5–F6. doi: 10.1136/archdischild-2016-311647. [DOI] [PubMed] [Google Scholar]
- 22.Mitra S, Singh B, El-Naggar W, McMillan DD. Automated versus manual control of inspired oxygen to target oxygen saturation in preterm infants: a systematic review and meta-analysis. J Perinatol. 2018;38(4):351–360. doi: 10.1038/s41372-017-0037-z. [DOI] [PubMed] [Google Scholar]
- 23.Claure N, Gerhardt T, Everett R, Musante G, Herrera C, Bancalari E. Closed-loop controlled inspired oxygen concentration for mechanically ventilated very low birth weight infants with frequent episodes of hypoxemia. Pediatrics. 2001;107(5):1120–1124. doi: 10.1542/peds.107.5.1120. [DOI] [PubMed] [Google Scholar]
- 24.van Kaam AH, Hummler HD, Wilinska M, Swietlinski J, Lal MK, te Pas AB, et al. Automated versus Manual Oxygen Control with Different Saturation Targets and Modes of Respiratory Support in Preterm Infants. J Pediatr. 2015;167(3):545–50.e1–2. doi: 10.1016/j.jpeds.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 25.Fierson WM. Screening Examination of Premature Infants for Retinopathy of Prematurity. Pediatrics. 2018;142[6]:e20183061. [DOI] [PubMed]
- 26.The International Classification of Retinopathy of Prematurity revisited. Archives of ophthalmology (Chicago, Ill : 1960). 2005;123(7):991–9. [DOI] [PubMed]
- 27.Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116(6):1353–1360. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- 28.Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187(1):1–7. doi: 10.1097/00000658-197801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bayley N. Bayley scales of infant and toddler development: PsychCorp, Pearson. 2006. [Google Scholar]
- 30.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 31.Smith LEH, Hellstrom A, Stahl A, Fielder A, Chambers W, Moseley J, et al. Development of a retinopathy of prematurity activity scale and clinical outcome measures for use in clinical trials. JAMA Ophthalmol. 2019;137(3):305–311. doi: 10.1001/jamaophthalmol.2018.5984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stenson BJ, Donoghoe M, Brocklehurst P, Davis PG, Juszczak E, Marschner IC, et al. Pulse Oximeter Saturation Targeting and Oximeter Changes in the Benefits of Oxygen Saturation Targeting (BOOST)-II Australia and BOOST-II UK Oxygen Trials. J Pediatr. 2019;204:301–4.e2. doi: 10.1016/j.jpeds.2018.08.033. [DOI] [PubMed] [Google Scholar]
- 33.Castillo A, Deulofeut R, Critz A, Sola A. Prevention of retinopathy of prematurity in preterm infants through changes in clinical practice and SpO (2) technology. Acta Paediatr. 2011;100(2):188–192. doi: 10.1111/j.1651-2227.2010.02001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Askie LM, Darlow BA, Davis PG, Finer N, Stenson B, Vento M, et al. Effects of targeting lower versus higher arterial oxygen saturations on death or disability in preterm infants. Cochrane Database Syst Rev 2017, Issue 4 Art No: CD011190. doi: 101002/14651858CD011190pub2. 2017. [DOI] [PMC free article] [PubMed]
- 35.Hallenberger A, Poets CF, Horn W, Seyfang A, Urschitz MS. Closed-loop automatic oxygen control (CLAC) in preterm infants: a randomized controlled trial. Pediatrics. 2014;133(2):e379–e385. doi: 10.1542/peds.2013-1834. [DOI] [PubMed] [Google Scholar]
- 36.Urschitz MS, Horn W, Seyfang A, Hallenberger A, Herberts T, Miksch S, et al. Automatic control of the inspired oxygen fraction in preterm infants: a randomized crossover trial. Am J Respir Crit Care Med. 2004;170(10):1095–1100. doi: 10.1164/rccm.200407-929OC. [DOI] [PubMed] [Google Scholar]
- 37.Tarnow-Mordi W, Stenson B, Kirby A, Juszczak E, Donoghoe M, Deshpande S, et al. Outcomes of two trials of oxygen-saturation targets in preterm infants. N Engl J Med. 2016;374(8):749–760. doi: 10.1056/NEJMoa1514212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed for the current manuscript.