Abstract
Background
African Americans have disproportionately high rates of cardiovascular disease (CVD). Left ventricular hypertrophy (LVH) is an independent risk factor for CVD and may contribute to this disparity. Psychological stress contributes to LVH in African Americans and other populations.
Objective
This study evaluated the effects of stress reduction with the Transcendental Meditation (TM) technique on preventing LVH in African American adults with hypertension.
Setting
Martin Luther King Hospital - Charles R. Drew University of Medicine and Science, Los Angeles, CA.
Method
In this trial, 85 African American adults (average 52.8 years) were randomly assigned to either TM program or health education (HE) control group and completed posttesting. Participants were tested at baseline and after six months for left ventricular mass index (LVMI) by M-mode echocardiography, blood pressure, psychosocial stress and behavioral factors. Change in outcomes was analyzed between groups by ANCOVA and within groups by paired t-test.
Results
The TM group had significantly lower LVMI compared with the HE group
(-7.55gm/m2, 95% CI -14.78 to -.34 gm/m2, P=.040). Both interventions showed significant within group reductions in BP, (SBP/DBP changes for TM: -5/ -3 mm Hg, and for HE: -7/-6 mm Hg, P=.028 to <.001) although between group changes were not significant. In addition, both groups showed significant reductions in anger (P=.002 to .001). There were no other changes in lifestyle factors.
Conclusions
These findings indicate that stress reduction with TM was effective in preventing LVMI progression and thus may prevent LVH and associated CVD in high-risk African American patients.
Keywords: Left Ventricular Hypertrophy, Left Ventricular Mass Index, Stress Reduction, Transcendental Meditation, Health Disparity, Cardiovascular Disease
Introduction
African Americans have disproportionately high rates of cardiovascular disease (CVD).1 LVH is an independent risk factor for CVD.2 It increases the risk of acute myocardial infarction, congestive heart failure, atrial fibrillation, sudden cardiac death and all-cause mortality by 2-3-fold.2 African Americans have a higher prevalence of LVH (41% compared with 19% in Whites),3 CVD morbidity and mortality compared with the majority population.1
Chronic psychosocial stress and cardiovascular reactivity to stress have been found to contribute to LVH prevalence and development.4,5 The disproportionately high rates of LVH and CVD in African Americans may be associated with the burden of psychosocial stress imposed by socioeconomic disparities and perceived racism.1,6
Effective stress reduction therapies can reduce high BP and associated CVD.7 A recent American Heart Association (AHA) Scientific Statement on Meditation and Cardiovascular Risk Reduction suggested that stress reduction with meditation may be useful in the prevention of cardiovascular disease.8 The Transcendental Meditation technique has been found to be distinctly effective in primary and secondary prevention of CVD morbidity and mortality in African Americans and Whites.9,10
A recent scientific statement from the American Heart Association emphasized “the potential for interventions that promote positive psychological health and reduce stress levels (for) improving health behaviors and ultimately health outcomes of African Americans.”1 This was echoed concurrently by the Stress and Health Disparities report of the American Psychological Association.11 In light of the current emphasis on the potential of stress-reducing strategies for reducing CVD disparities in African Americans, we reviewed and re-analyzed data from an earlier clinical trial on meditation and CVD in African Americans for effects on left ventricular hypertrophy as an independent risk factor for cardiovascular morbidity and mortality.12
Studies on the effect of stress reduction on LVH are few. To our knowledge, there are only two published studies that reported the effect of stress reduction on LVH. One was a pilot trial conducted in 34 hypertensive African American adults.13 The second study was a randomized control trial in African American adolescents with high normal blood pressure (BP).14 However, the earlier studies had relatively small sample sizes.
Therefore, in the current trial, the overall objective was to assess the effects of stress reduction with Transcendental Meditation on LVMI, BP and related behavioral factors in adult hypertensive African Americans.
Methods
This randomized, controlled, single-blinded, clinical trial was conducted to compare the effect of Transcendental Meditation (TM) and health education (HE) on left ventricular mass index (LVMI) in hypertensive African American adults. Results from a substudy were previously reported.12 The trial was conducted between 1994 – 1999 at the Martin Luther King Jr. Medical Center, Charles R. Drew University of Medicine and Science clinical site in Los Angeles, CA in collaboration with the data and administrative coordinating center at Maharishi University of Management in Fairfield, Iowa. The trial was approved by institutional ethics review boards of Charles R. Drew University. All procedures followed were in accordance with the ethical standards of the IRB and the Helsinki Declaration of 1975, as revised in 2000. All subjects provided signed written informed consent.
Inclusion Criteria
The study included self-identified African American men and women aged 20-75 years with systolic blood pressure (SBP) of 120-179 mm Hg and/or diastolic blood pressure (DBP) of 80-109 mm Hg, with or without antihypertensive medications.
Exclusion Criteria
Patients with a history of stroke, transient ischemic attack, heart failure, myocardial infarction, angina pectoris or with significant ECG abnormalities, major psychiatric or behavioral disorders such as alcoholism (>28 drinks per week) were excluded. Patients were not assessed for hypertrophic obstructive cardiomyopathy or aortic stenosis.
Study Protocol
Patients were pre-tested for primary and secondary outcomes at the baseline and posttested after a six-month intervention period. A baseline period of three visits included three BP assessments, echocardiography for left ventricular mass (LVM) for calculating LVMI, psychometric testing, and behavioral factors assessment to determine the eligibility of the individual for participation. At the end of the baseline period, averaged BP recordings from the last two visits were used along with other factors to determine the eligibility.
A computer-generated list of random sequence numbers was used to randomize patients to either TM or HE (allocation ratio 1:1) group. Randomization was stratified by age, sex, mean arterial pressure, left ventricular mass index (LVMI), and antihypertensive medication.
Investigators, data collectors, and data management staff were blinded to group assignment. The biostatistician conveyed the group allocation to the project manager who then informed each participant and instructed them not to reveal it to the research and data collection staff during the course of the study. Intervention groups met separately in different rooms to minimize contamination. Both the experimental and control groups were given the same information about the anticipated benefits of the treatments. Both treatment interventions were also matched on the number of treatment visits, length of each session, duration of treatment and attention from instructors.
Intervention
The Transcendental Meditation (TM) technique is a standardized, simple mental procedure, practiced twice a day for 20 minutes while sitting comfortably with eyes closed.15 Patients’ instruction in the TM program involved a seven-step course over five sessions (90-minute meetings). This included the presentation of principles, TM benefits, discussion of mechanics of the technique, and a brief personal interview (session 1), personal instruction (session 2), and three follow-up meetings in small-groups (sessions 3,4, and 5). The last four sessions were conducted over four consecutive days. TM requires 20 minutes of practice twice daily for its maximum physiological benefits.15 Patients were advised to practice the technique for 20 minutes twice daily at home, seven days/week (fourteen sessions/week) for the duration of the study. Follow-up refresher meetings were conducted 1 week later, every 2 weeks for 2 months, and once a month for 3 months. A trained and certified African American TM instructor taught the TM course. The TM group patients did not receive any specific nutritional recommendations as did the HE group.
The Health Education intervention provided behavioral instructions for CVD risk factor prevention that included nutritional hygiene recommendations from the Trials of Hypertension Prevention.16 This group received written materials, structured presentations, didactic instructions and group support for modifying the major cardiovascular risk factors including salt restriction, weight reduction, aerobic exercise, alcohol, and smoking cessation. The topic of stress was covered, but patients did not learn a specific stress reduction technique. The HE group participants attended a 90-minute meeting once a week for the first 5 weeks, followed by 2-week sessions for 2 months, and once a month for the last 3 months.
Outcome Measures
The primary outcome was change in LVMI. M-mode echocardiography was used to measure left ventricular mass. Measurements were obtained at the end-diastole. Interventricular septal thickness, posterior wall thickness, and left ventricle internal dimension were measured. Penn equation was used to calculate LVM because of its use in previous clinical trials and its high correlation to necropsy findings.17 Left ventricle cross-section area, relative wall thickness, and left ventricle diastolic dimension were also calculated. Each participant’s LVM was indexed by his/ her body surface area to yield LVMI.18
The secondary outcome variables were SBP and DBP, psychosocial stress and behavioral factors. A trained research technician measured BP in the supported right arm while the participant remained seated and resting for 5 minutes. Critikon Dinamap 1846 SX/P version 0846 with cuff size based on the participant’s arm circumference was used. Average of three successive readings taken at 30-second intervals was noted. Patients were told not to practice any stress-reduction technique immediately before or during BP recording.
Psychological functions were assessed at baseline and at posttest. Patients were administered the Anger Expression Scale,19 the Perceived Stress Scale,20 a 5-item subset of the California Self-Evaluation Scale to measure, self-esteem, and the Personal Efficacy scale. Self-report diaries were used to evaluate the level of physical activity, duration of activity, tobacco, alcohol, and other substance use.
The power and the sample size estimates were based on the LVM and BP changes. A sample size of 85 for each of the groups was calculated to provide 80% power to detect a reliable comparative reduction in LV mass with a two-sided P<.05.
Analysis
The analysis was conducted on patients who completed the pretesting and posttesting for the primary outcome. SPSS software, versions 24.0 and 25.0 (IBM SPSS) was used for analysis. The effect of attrition on the composition of the groups was analyzed for demographic variables and for cardiovascular variables at pre-test by t-test of the baseline variables with treatment and attrition versus non-attrition as grouping variables. Outlier analysis was done as per standard procedure using the interquartile range of baseline LVMI and multiplying by a factor of 2.2.21
Baseline characteristics of the two treatment groups were compared with t-tests, chi-square test and Fischer’s exact test. Outcome data were assessed for between group differences by analysis of covariance (ANCOVA). For between-groups change in LVMI, the baseline LVMI and baseline mean arterial pressure were used as covariates. Baseline mean arterial pressure value was missing for one subject, which was imputed by multiple imputations method. Between-group differences for all secondary outcome variables were assessed by ANCOVA using the baseline level of the respective variable as a covariate. Paired t-test was used to report within group Ps. >
Post-hoc Analysis
Test of interaction22 using two-way ANCOVA was conducted to investigate whether treatment effects on primary outcome vary by sex, age (participants above and below the median age of 52 years), antihypertensive medication use, or by the class of antihypertensive medication use. The results were calculated from pooled values from the multiple imputed data.
Results
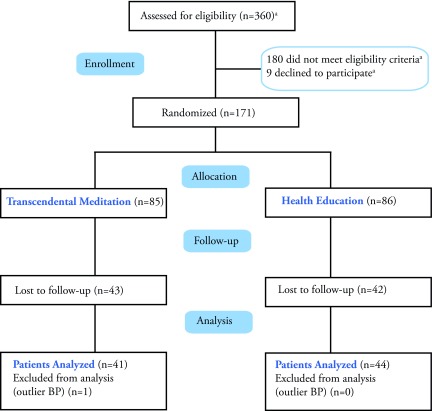
The study’s patient flow diagram can be seen in Figure 1. Of the 171 randomized participants, 86 (50.29 %) completed post-test for LVM. The analysis was conducted on 85 participants, as one participant’s LVMI was an outlier and these data were removed from the final analysis.
Figure 1. Flow of participants from randomization to analysis.
a. estimated.
Effects of Attrition
The rates of dropout were not different between the groups (Figure 1). There were no significant differences between attritors and non-attritors with regard to baseline levels of SBP and DBP, and LVMI.
Baseline Characteristics
Baseline characteristics of the 85 participants are displayed in Table 1. The study group was predominantly female (64.7%). Average age was 52.81±10.2 years. Baseline mean SBP was 147±12.47 mm Hg, DBP was 85.51±10.83 mm Hg, baseline LVMI was 94.4+28.2gm/m2 in males and 81.6+17.7 gm/m2 in females. The number of patients taking antihypertensive medication at baseline were not different between groups (P=.818) (Table 1). At baseline, the distribution of participants taking angiotensin-converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB), calcium channel blockers (CCB), diuretics, beta or alpha-blockers was not different between the groups (P=.926). Also, number of participants taking ACE/ARB compared with other classes of antihypertensive medication was not different between the groups (P=.696). At pre-test, groups did not differ significantly on any measure except mean arterial pressure. (Table 1)
Table 1. Demographic and baseline characteristics by treatment group.
| Variables | Transcendental Meditation Group, n=41 | Health Education Group, n=44 | Comparison between the group |
| Mean (SD) | Mean (SD | P | |
| Age, years | 53.3 (9.431) | 52.27 (11.069) | .619 |
| Females | 29 (70.73%) | 26(59.09%) | .791 |
| Married | 13(34.2%) | 18(43.9%) | .490 |
| Educated up to high school level | 6(15.8%) | 4(9.5%) | .505 |
| Annual income <$20,000 | 12(31.6%) | 12(28.6%) | .811 |
| Weight, kg | 88.12(14.98) | 93.62(19.39) | .149 |
| BMI, kg/m2 | 30.29(4.63) | 32.17(7.29) | .164 |
| On antihypertensive drugs | 29(70.7%) | 30(68.2%) | .818 |
| Class of antihypertensive medicationa | ACE I or ARB=6, CCB=4, Diuretic=5, β-blocker=2, α blocker=1 | ACE I or ARB =3, CCB=4, Diuretic=3, β-blocker=2, α blocker=2 | .926 |
| LVM, gm | 170.79(45.47) | 175.92(55.11) | .642 |
| LVMI, g/m2 | 85.96(21.40) | 86.350(24.434) | .938 |
| SBP, mm Hg | 144.64(12.317) | 149.40(12.436) | .082 |
| DBP, mm Hg | 83.61(8.840) | 87.24(12.316) | .128 |
| MAP, mm Hg | 104.207(7.529) | 108.204(9.697) | .039 |
| Pulse, bpm | 76.81(11.084) | 76.13(11.655) | .783 |
| Exercise, hours/week | 6.602(4.486) | 7.716(4.367) | .278 |
| Smoke, cigarettes/day | .65 (3.278) | .93 (4.212) | .734 |
| Anger-in scores | 2.502(.900) | 2.521(.929) | .923 |
| Anger-out scores | 2.2103(.51006) | 2.244(.505) | .760 |
| Perceived stress scores | .6189(.126) | .635(.147) | .581 |
| Personal efficiency scores | 2.187(.790) | 2.244(.895) | .761 |
| Self-esteem scores | 7.280(1.199) | 7.272(1.10) | .977 |
BMI, body mass index; ACE I, angiotensin converting enzyme inhibitor; ARB; angiotensin receptor blocker; CCB, calcium channel blocker; bpm, beats/-minute; DBP, diastolic blood pressure; LVM, left ventricle mass; LVMI, left ventricle mass index; MAP, mean arterial pressure; SBP, systolic blood pressure; SD, standard deviation.
a. Out of available record of n=31 patients on antihypertensive medication.
Left Ventricular Mass Index
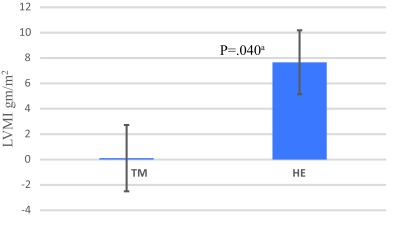
After 6.8±1.3 months of intervention, the TM group had significantly lower (-7.55 gm/m2) LVMI than the HE group (P=.040). (Figure 2)
Figure 2. Change in left ventricle mass index (±standard error of mean) between the groups after six-month intervention.
TM; Transcendental Meditation, HE; health education, LVMI; left ventricle mass index.
a. significant P.
Blood Pressure, Pulse Rate, Behavioral and Lifestyle Factors, Psychological Outcomes, Anti-Hypertension Therapy (Table 2)
Table 2. Changes in outcomes after six-month intervention.
| Outcome | Transcendental Meditation group | Health education group | Comparison between the groups | |||
| Adjusted mean change from baseline (SEM) | Within group P | Adjusted mean change from baseline (SEM) | Within group P | Adjusted mean difference (95% CI) | Between groups P | |
| LVMI | .107 (2.614) | .742 | 7.665 (2.521) | .099 | -7.55 (-14.780 to -.335) | .040a |
| LVM | -.882 (5.750) | .745 | 14.90 (5.545) | .148 | -15.78 (-31.66 to .105) | .051 |
| SBP, mm Hg | -5.978 (1.661) | .003a | -7.497(1.582) | .00a | 1.51 (-3.043 to 6.081) | .509 |
| DBP, mm Hg | -3.258(1.270) | .028a | -6.629(1.210) | .00a | 3.37 (-.118 to 6.860) | .058 |
| Pulse, bpm | -3.888(1.641) | .002a | -2.693(1.565) | .155 | -1.19 (-5.706 to 3.316) | .5996 |
| Exercise, hours/week | .051(.814) | .517 | -1.406(.785) | .071 | 1.457(-.793 to 3.707) | .202 |
| Weight, kg | -.098(.906) | .913 | -1.075(.884) | .320 | .977 (-1.54 to 3.49) | .443 |
| BMI, kg/m2 | -.037(.310) | .906 | -0.351(.302) | .335 | .3140 (-.547 to 1.175) | .433 |
| Anger-in scores | -.264(.066) | .002a | -.218(.063) | .001a | -.046 (-.227 to .135) | .615 |
| Anger-out scores | -.110(.065) | .082 | -.185(.062) | .016a | .075 (-.103 to .253) | .40 |
| Self-esteem scores | .051(.118) | .732 | .285(.112) | .732 | -.234 (-.557 to .089) | .154 |
| Personal efficiency scores | -.038(.089) | .820 | -.012(.086) | .814 | .026 (-.272 to .220) | .834 |
| Perceived stress scores | .042(.017) | .004a | .049(.017) | .028a | -.006 (-.054 to .042) | .791 |
LVMI, left ventricular mass index; LVM, left ventricular mass; BMI, body mass index; CI, confidence interval; DBP, diastolic blood pressure; HE, health education; mean, mean change adjusted for baseline value of respective variable; n, number of patients; SBP; systolic blood pressure, SEM; standard error of mean; TM; Transcendental Meditation
a. significant P. For LVMI and LVM the mean was adjusted for baseline mean arterial pressure and baseline value of respective variable. For other outcomes, mean was adjusted for baseline value of respective variable.
SBP and DBP decreased significantly within both groups but the decrease was not significantly different between groups.
The change in pulse rate did not differ significantly between the treatment groups. Within the TM group, pulse rate was significantly decreased from baseline (P=.002).
There were no significant differences between or within the groups on weight, BMI or number of hours of exercise per week.
Though the anger-in scores decreased significantly and perceived stress scores increased significantly within both the HE and TM groups, the change was not significant between the two groups. For other psychological parameters, changes were not significantly different between the TM and HE groups.
Of the patients analyzed, 69.4% patients (n=59; TM=29, HE=30) were taking antihypertensive medication at baseline, when there was no difference in the number of patients taking antihypertensive medication between the groups (Table 1). After the 6-month intervention, 4.8% (n=3; TM=2, HE=1) patients who were not taking antihypertensive medication earlier, started the antihypertensive therapy and 11.3% (n=3; TM=2, HE=5) patients who were earlier on antihypertensive medication stopped taking the medicine. The number of patients who started taking antihypertensive medication during the study or those who stopped taking medication during the study period was not different between the TM and HE groups (P=.493).
Subgroup Results
The results showed no interaction of treatment with age (above or below median age of 52 years) (P=.459), sex (P=.143), and antihypertensive medication (P=.427) on LVMI. Of the 59 patients who were on antihypertensive medication, we had records of class of medication for 31 patients (Table 1). The distribution of patients for each class of antihypertensive medication is shown in Table 1. The interaction analysis showed no difference in the effect of treatment with class of antihypertensive medication (P=.097).
Discussion
The results showed significantly lower LVMI in the TM compared with the HE group after the 6-month intervention. This suggests that an effective stress reduction modality may prevent the progression of LVMI in hypertensive adults.
The increased LVMI observed in the HE group of the current study represents the natural progression of LVMI in hypertensive patients and is similar to the increased LVMI reported in the control or placebo arm of other trials.23,24 In comparison, significantly lower LVMI observed in the TM group demonstrates the effectiveness of TM practice in preventing LVMI progression and thus LVH in hypertensive patients. This has direct implications for the prevention of CVD associated with LVH in this high-risk African American population.
Approximately 70% of the participants in TM and ~60% participants in the control group were women but the impact of treatment was not moderated by sex. Women have a lower prevalence of LVH than men for any given blood pressure but LVH is a stronger risk factor for stroke and heart failure in women compared with men.25 There was no significant interaction between sex and treatment response. The prevention of LVMI progression in this study is relevant to the prevention of stroke and heart failure as well as CHD in women.
The effect of treatment was not moderated by the age, use of antihypertensive medication or the class of antihypertensive medication, although the sample size in each class of antihypertensive medication subgroup was small.
The significant BP reduction (SBP -6 mm Hg, DBP -3 mm Hg) observed in the TM group of the present study is consistent with the range of BP decrease reported by meta-analysis of studies on BP reductions with TM practice.26 However, BP reduction was not different from HE. Despite the similar BP reductions, lower LVMI in the TM group suggests the additional effect of TM in modulating factors that promote LVM progression independent of BP. Psychological stress,4,5 increased sympathetic activity,27 catecholamines,28 and activation of renin-angiotensin-aldosterone system29 play a role in LVH pathophysiology independent of BP. All these are independent predictors of LVH and are reported to be reduced by TM practice.30 We hypothesize that TM practice could have modulated some or all of these factors to demonstrate the observed effect on LVMI.
The results of this trial provide evidence to support the recent American Heart Association scientific statement that suggested the contributory role of psychological stress in cardiovascular disease disparities in African Americans1 and proposed the relevance of stress-reducing interventions for improving health outcomes in this higher risk population.1
The outcomes of our study are generally consistent with two previous independently conducted trials on the effects of the TM program on LVM. In a pilot study13 conducted in 34 mildly hypertensive (DBP=90-104 mm Hg) adults, investigators found a one-year intervention of TM and HE led to LVMI reduction in both treatment groups but no significant differences between groups.13 By contrast, in the current study, we found lower LVMI in African American adults in the TM compared with the HE group. The smaller sample size of the pilot study13 could explain the difference in results compared with the present study. Similar to the results of the current study, a study conducted by Barnes et al reported significantly reduced LVM in TM compared with the HE group.31
By preventing LVMI progression in the present study, TM may reduce the likelihood of cardiovascular morbidity and mortality associated with LVH. Devereux et al32 reported that every 23.5 gm/m2 increase in LVMI, increases the risk of cardiovascular mortality by 38% and all-cause mortality by 28%. Based on these findings, patients randomized to TM in the current study would have an 11% reduced risk of cardiovascular mortality and 8% reduced the risk of all-cause mortality compared with the HE group.
Previously, studies have reported a decrease in cardiovascular mortality and morbidity with TM practice in prehypertensive and stage-I hypertensive adults33 and in coronary heart disease patients.10 Though LVMI was not measured in these trials, prevention of LVMI progression with TM practice could be a possible reason for the decreased cardiovascular morbidity and mortality found in those trials.
Strengths and Limitations
There are several limitations to the present study. First, only hypertensive African American patients were studied; therefore, the results may not generalize to other racial/ethnic groups. Future studies with a larger and more ethnically diverse sample would provide evidence about the generalizability of these findings.
Second, high attrition might have reduced power for some of our findings. However, the attrition was not significantly different between the TM and the HE groups, thus reducing potential subject bias in the final sample. Moreover, the attritors and completers were not significantly different in demographic or physiological characteristics at baseline that prevented the occurrence of systematically biased treatment outcomes. Post-hoc power calculations are not recommended and were not done for the current study.34 Hoenig and Heisy convincingly argue that post-hoc power analyses are fundamentally flawed. “Power calculations tell us how well we might be able to characterize nature in the future given a particular state and statistical study design, but they cannot use information in the data to tell us about the likely states of nature (in the past). With traditional frequentist statistics, this is best achieved with confidence intervals, appropriate choices of null hypotheses, and equivalence testing.”34 This view is echoed by Goodman and Berlin35 and others who critically review the issue of post hoc power calculations. In this article, we follow this statistical guidance and report appropriate confidence intervals and equivalence testing in the results. At the same time, we acknowledge the potential of attrition bias in this study. We controlled for that, at least in part by comparing the baseline characteristics of attritors and completers. From this analysis, we might infer that attrition was randomly distributed. Nevertheless, the results of the completer analysis are clinically and statistically relevant.
Third, both the treatment conditions in the present study are behavioral interventions for hypertensive heart disease; a three-arm design, with both (TM and HE) to examine synergistic effects is suggested for future research. An inactive control group was deemed not to be ethical. Fourth, significant reductions between groups were not found in the psychological variables that might be because of subjective variability in the perception of stress and in emotional reactivity to those experiences. These results are consistent with previous studies of TM indicating that this practice may produce physiological changes associated with stress in the absence of changes in self-reported psychological variables.36,37 Fifth, no record of compliance for home TM practice was collected. However, the record of meeting attendance was significantly higher in the TM (80.6%) as compared with HE (50.2%) group (P=.001). Sixth, more research is needed to identify the biologic mechanisms or trophic factors that are affected by TM practice. Lastly, no measure of 24-hour BP was collected and therefore it cannot be excluded that a more substantial effect of TM on nocturnal BP as a mechanism for its potential independent effect.
Conclusion
The findings of this study suggest that stress reduction with TM practice is an effective behavioral technique for preventing LVMI progression in African American hypertensives who, especially, are at high risk of developing LVH and associated CVD.
Acknowledgments
The authors would like to thank David W. Orme-Johnson, PhD for his contributions to an earlier version of the manuscript, Amparo Castillo, MD for literature review and collection of reports, Chinelo Haney for managing the project on site, Laura Valls for data management and Jean Symington Craig for administrative assistance.
Preliminary findings from this study were presented at the International Society for Hypertension in Blacks and published as an abstract: Schneider R, Alexander C, Orme-Johnson D, Castillo-Richmond A, Rainforth M, Nidich S and Salerno J. A controlled trial of effects of stress reduction on left ventricular mass in hypertensive African Americans. Ethn Dis. 2004;14:S2-54.
Data Sharing Statement. The authors are willing to share and make available the raw datasets and supplemental data to the publication at the written and reasonable request of the inquiring researcher(s).
This work was supported by National Heart, Lung, and Blood Institute of the National Institutes of Health, US #R01 HL5159.
References
- 1. Carnethon MR, Pu J, Howard G, et al. ; American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; and Stroke Council . Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. 2017;136(21):e393-e423. 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 2. Bauml MA, Underwood DA. Left ventricular hypertrophy: an overlooked cardiovascular risk factor. Cleve Clin J Med. 2010;77(6):381-387. 10.3949/ccjm.77a.09158 [DOI] [PubMed] [Google Scholar]
- 3. Koren MJ, Mensah GA, Blake J, Laragh JH, Devereux RB. Comparison of left ventricular mass and geometry in black and white patients with essential hypertension. Am J Hypertens. 1993;6(10):815-823. 10.1093/ajh/6.10.815 10.1093/ajh/6.10.815 [DOI] [PubMed] [Google Scholar]
- 4. Schnall PL, Pieper C, Schwartz JE, et al. The relationship between ‘job strain,’ workplace diastolic blood pressure, and left ventricular mass index. Results of a case-control study. JAMA. 1990;263(14):1929-1935. 10.1001/jama.1990.03440140055031 [DOI] [PubMed] [Google Scholar]
- 5. Taylor TR, Kamarck TW, Dianzumba S. Cardiovascular reactivity and left ventricular mass: an integrative review. Ann Behav Med. 2003;26(3):182-193. 10.1207/S15324796ABM2603_03 [DOI] [PubMed] [Google Scholar]
- 6. Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. Am J Med Sci. 2003;325(6):315-331. 10.1097/00000441-200306000-00003 10.1097/00000441-200306000-00003 [DOI] [PubMed] [Google Scholar]
- 7. Marwaha K, Schneider RH. Stress, Stress Reduction and Hypertension: an updated review. In: Giuseppe M, Guido G, Konstantinos T, Anna D, Enrico A-R, eds. Manual of Hypertension of the European Society of Hypertension. 3rd ed Boca Raton, FL: CRC Press; 2019:109-117, 10.1201/9780429199189-14 [DOI] [Google Scholar]
- 8. Levine GN, Lange RA, Bairey-Merz CN, et al. ; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Hypertension . Meditation and Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. J Am Heart Assoc. 2017;6(10):e002218. 10.1161/JAHA.117.002218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons > or = 55 years of age with systemic hypertension. Am J Cardiol. 2005;95(9):1060-1064. 10.1016/j.amjcard.2004.12.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schneider RH, Grim CE, Rainforth MV, et al. Stress reduction in the secondary prevention of cardiovascular disease: randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012;5(6):750-758. 10.1161/CIRCOUTCOMES.112.967406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Psychological Association Stress and Health Disparities: Contexts, Mechanisms, and Interventions among Racial/Ethnic Minority and Low-Socioeconomic Status Populations. 2017. Last accessed from https://www.apa.org/pi/health-disparities/resources/stress-report.pdf.
- 12. Castillo-Richmond A, Schneider RH, Alexander CN, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;31(3):568-573. 10.1161/01.STR.31.3.568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kondwani K, Schneider R, Alexander CN, et al. Left ventricular mass regression with the Transcendental Meditation technique and a health education program in hypertensive African Americans. J Soc Behav Pers. 2005;17(1):181-200. [Google Scholar]
- 14. Barnes VA, Orme-Johnson DW. Prevention and treatment of cardiovascular disease in adolescents and adults through the transcendental meditation(®) program: a research review update. Curr Hypertens Rev. 2012;8(3):227-242. 10.2174/157340212803530411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roth B. Strength in Stillness: The Power of Transcendental Meditation. New York: Simon & Schuster; 2018. [Google Scholar]
- 16. Whelton PK, Kumanyika SK, Cook NR, et al. ; Trials of Hypertension Prevention Collaborative Research Group . Efficacy of nonpharmacologic interventions in adults with high-normal blood pressure: results from phase 1 of the Trials of Hypertension Prevention. Am J Clin Nutr. 1997;65(2)(suppl):652S-660S. 10.1093/ajcn/65.2.652S [DOI] [PubMed] [Google Scholar]
- 17. Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57(6):450-458. 10.1016/0002-9149(86)90771-X 10.1016/0002-9149(86)90771-X [DOI] [PubMed] [Google Scholar]
- 18. Devereux RB, Lutas EM, Casale PN, et al. Standardization of M-mode echocardiographic left ventricular anatomic measurements. J Am Coll Cardiol. 1984;4(6):1222-1230. 10.1016/S0735-1097(84)80141-2 10.1016/S0735-1097(84)80141-2 [DOI] [PubMed] [Google Scholar]
- 19. Spielberger C, Johnson E, Russell S, Crane RJ, Jacobs GA, Worden TJ The experience and expression of anger (construction and validation of an anger expression scale). In: In M. A. Chesney & R. H. Rosenman (Eds.), ed. Anger and Hostility in Cardiovascular and Behavioral Disorders. New York: Hemisphere/ McGraw-Hill; 1985:5–30.
- 20. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 21. Hoaglin DC, Iglewicz B. Fine-tuning some resistant rules for outlier labeling. J Am Stat Assoc. 1987;82(400):1147-1149. 10.1080/01621459.1987.10478551 [DOI]
- 22. Pocock SJ, McMurray JJV, Collier TJ. Statistical controversies in reporting of clinical trials: part 2 of a 4-part series on statistics for clinical trials. J Am Coll Cardiol. 2015;66(23):2648-2662. 10.1016/j.jacc.2015.10.023 [DOI] [PubMed] [Google Scholar]
- 23. Lonn E, Shaikholeslami R, Yi Q, et al. Effects of ramipril on left ventricular mass and funcÂtion in cardiovascular patients with controlled blood pressure and with preserved left ventricÂular ejection fraction: a substudy of the Heart Outcomes Prevention Evaluation (HOPE) Trial. J Am Coll Cardiol. 2004;43(12):2200-2206. https://doi.org/ 10.1016/j. jacc.2003.10.073 PMID:15193680 [DOI] [PubMed]
- 24. Ofili EO, Cohen JD, St Vrain JA, et al. Effect of treatment of isolated systolic hypertension on left ventricular mass. JAMA. 1998;279(10):778-780. 10.1001/jama.279.10.778 [DOI] [PubMed] [Google Scholar]
- 25. Agabiti-Rosei E, Muiesan ML. Left ventricular hypertrophy and heart failure in women. J Hypertens Suppl. 2002;20(2):S34-S38. [PubMed] [Google Scholar]
- 26. Anderson JW, Liu C, Kryscio RJ. Blood pressure response to transcendental meditation: a meta-analysis. Am J Hypertens. 2008;21(3):310-316. 10.1038/ajh.2007.65 10.1038/ajh.2007.65 [DOI] [PubMed] [Google Scholar]
- 27. Grassi G. Sympathetic overdrive as an independent predictor of left ventricular hypertrophy: prospective evidence. J Hypertens. 2006;24(5):815-817. 10.1097/01.hjh.0000222748.37078.2d [DOI] [PubMed] [Google Scholar]
- 28. Matsumura K, Fujii K, Oniki H, Oka M, Iida M. Role of aldosterone in left ventricular hypertrophy in hypertension. Am J Hypertens. 2006;19(1):13-18. https://doi.org/ 10.1016/j amjhyper.2005.05.013 PMID:16461184 [DOI] [PubMed]
- 29. Malmqvist K, Öhman KP, Lind L, Nyström F, Kahan T. Relationships between left ventricular mass and the renin-angiotensin system, catecholamines, insulin and leptin. J Intern Med. 2002;252(5):430-439. 10.1046/j.1365-2796.2002.01053.x [DOI] [PubMed] [Google Scholar]
- 30. Schneider S, Diehl K, Bock C, Herr RM, Mayer M, GÃrig T. Modifying health behavior to prevent cardiovascular diseases: a nationwide survey among German primary care physicians. Int J Environ Res Public Health. 2014;11(4):4218-4232. 10.3390/ijerph110404218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barnes VA, Kapuku GK, Treiber FA. Impact of transcendental meditation on left ventricular mass in african american adolescents. Evid Based Complement Alternat Med. 2012;2012:923153. 10.1155/2012/923153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Devereux RB, Wachtell K, Gerdts E, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA. 2004;292(19):2350-2356. 10.1001/jama.292.19.2350 [DOI] [PubMed] [Google Scholar]
- 33. Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons > or = 55 years of age with systemic hypertension. Am J Cardiol. 2005;95(9):1060-1064. 10.1016/j.amjcard.2004.12.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hoenig JM, Heisey DM. The abuse of power: the pervasive fallacy of power calculations for data analysis. Am Stat. 2001;55(1):19-24. 10.1198/000313001300339897 [DOI] [Google Scholar]
- 35. Goodman SN, Berlin JA. The use of predicted confidence intervals when planning experiments and the misuse of power when interpreting results. Ann Intern Med. 1994;121(3):200-206. 10.7326/0003-4819-121-3-199408010-00008 10.7326/0003-4819-121-3-199408010-00008 [DOI] [PubMed] [Google Scholar]
- 36. Duraimani S, Schneider RH, Randall OS, et al. Effects of lifestyle modification on telomerase gene expression in hypertensive patients: a pilot trial of stress reduction and health education programs in African Americans. PLoS One. 2015;10(11):e0142689. 10.1371/journal.pone.0142689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Paul-Labrador M, Polk D, Dwyer JH, et al. Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med. 2006;166(11):1218-1224. 10.1001/archinte.166.11.1218 [DOI] [PubMed] [Google Scholar]