This cohort study investigates whether parathyroidectomy improves hypertension in patients with primary hyperparathyroidism.
Key Points
Question
Do patients with hypertension and parathyroidectomy for primary hyperparathyroidism have a significant reduction in their mean arterial pressure or antihypertensive medication use compared with those without surgery?
Findings
In this cohort study of 2380 patients, 501 with primary hyperparathyroidism and hypertension underwent parathyroidectomy. Patients with parathyroidectomy had significantly lower median mean arterial pressure after surgery than those without surgery, and on multivariable analysis, patients with parathyroidectomy were significantly less likely to increase antihypertensive medications at 6 months, 1 year, and 2 years after surgery.
Meaning
This study’s findings suggest that parathyroidectomy may provide cardiovascular benefits to those with primary hyperparathyroidism and hypertension.
Abstract
Importance
Hyperparathyroidism is associated with cardiovascular disease. However, evidence for a beneficial consequence of parathyroidectomy on hypertension is limited.
Objective
To investigate if parathyroidectomy improves hypertension in patients with primary hyperparathyroidism (PHPT).
Design, Setting, and Participants
In this cohort study and retrospective database review, patients with PHPT and hypertension between January 1, 2008, and December 31, 2016, were identified. The mean arterial pressure (MAP) and number of antihypertensive medications were compared between those who did and did not undergo parathyroidectomy. The setting was a large health care system. Primary hyperparathyroidism was defined using biochemical data, and hypertension was identified by International Classification of Diseases, Ninth Revision codes.
Exposure
Parathyroidectomy was identified in the database by Current Procedural Terminology codes.
Main Outcomes and Measures
The MAP and use of antihypertensive medications were compared for patients who underwent parathyroidectomy and those who did not at 6 months, 1 year, and 2 years. Multivariable logistic regression was used to assess the adjusted odds ratios for both increased and decreased use of antihypertensive medications.
Results
In this cohort study of 2380 participants (79.0% female), patients undergoing parathyroidectomy (n = 501) were younger (mean [SD] age, 65.3 [9.7] vs 71.9 [10.4] years; P < .001) and took fewer antihypertensive medications at baseline (mean [SD] number of medications, 1.2 [1.1] vs 1.5 [1.3], P < .001) than nonsurgical patients (n = 1879). Patients with parathyroidectomy showed greater improvement in their MAP at all follow-up time points (the median [SD] MAP change from baseline to 1 year was 0.1 [8.7] mm Hg without parathyroidectomy vs −1.2 [7.7] mm Hg after parathyroidectomy, P = .002). Nonsurgical patients were more likely vs those with parathyroidectomy to require more antihypertensive medications at 6 months (15.9% [n = 298] vs 9.8% [n = 49], P = .001), 1 year (18.1% [n = 340] vs 10.8% [n = 54], P < .001), and 2 years (17.6% [n = 330] vs 12.2% [n = 61], P = .004). By multivariable analysis, parathyroidectomy was independently associated with freedom from an increased number of antihypertensive medications at all periods (eg, adjusted odds ratio, 0.49; 95% CI, 0.34-0.70; P < .001 at 1 year). Among patients who were initially not taking antihypertensive medications, patients with parathyroidectomy were less likely vs no surgery to start antihypertensive medication treatment at all periods (eg, 10.2% [13 of 127] vs 30.4% [136 of 447], P < .001 at 1 year).
Conclusions and Relevance
This study’s findings suggest that, among hypertensive patients with PHPT, parathyroidectomy may be associated not only with greater decreases in their MAP but also with reduced requirements for antihypertensive medications. Parathyroidectomy decreased the number of patients who began taking antihypertensive medications. Additional study will be required to find whether there are downstream cardiovascular benefits of parathyroidectomy. Preexisting hypertension, particularly in those not already taking antihypertensive medications, should be considered when weighing surgical treatment.
Introduction
Early studies on the cardiovascular consequences of primary hyperparathyroidism (PHPT) were conflicting. Some researchers found a link between elevated parathyroid hormone (PTH) levels and coronary artery disease,1 while other studies2,3 refuted any association between PTH levels and myocardial infarction or coronary calcifications. The classic criteria for individuals with PHPT that necessitate surgery include young age, renal manifestations, skeletal consequences, and calcium levels. However, a consistently strong link between PHPT and cardiovascular outcomes has not been defined, and current guidelines do not include cardiovascular risk factors as indications for parathyroidectomy.4 Some studies5,6,7 have shown an association between PHPT and cardiovascular risk factors, including hypertension, diabetes, hyperlipidemia, coronary artery disease, heart failure, and stroke. In addition, parathyroidectomy has been associated with reduction of left ventricular hypertrophy.8
Despite the aforementioned work, there remain a limited number of studies investigating the association between parathyroidectomy and clinically significant cardiovascular risk factors. Even less work is focused on the association between PHPT and hypertension at the population level. If none exists, it follows that parathyroidectomy would be favorable for patients with PHPT, allowing for improvement of hypertension. This study aimed to address the association of parathyroidectomy with hypertension and antihypertensive medication use in a large and diverse patient population.
Methods
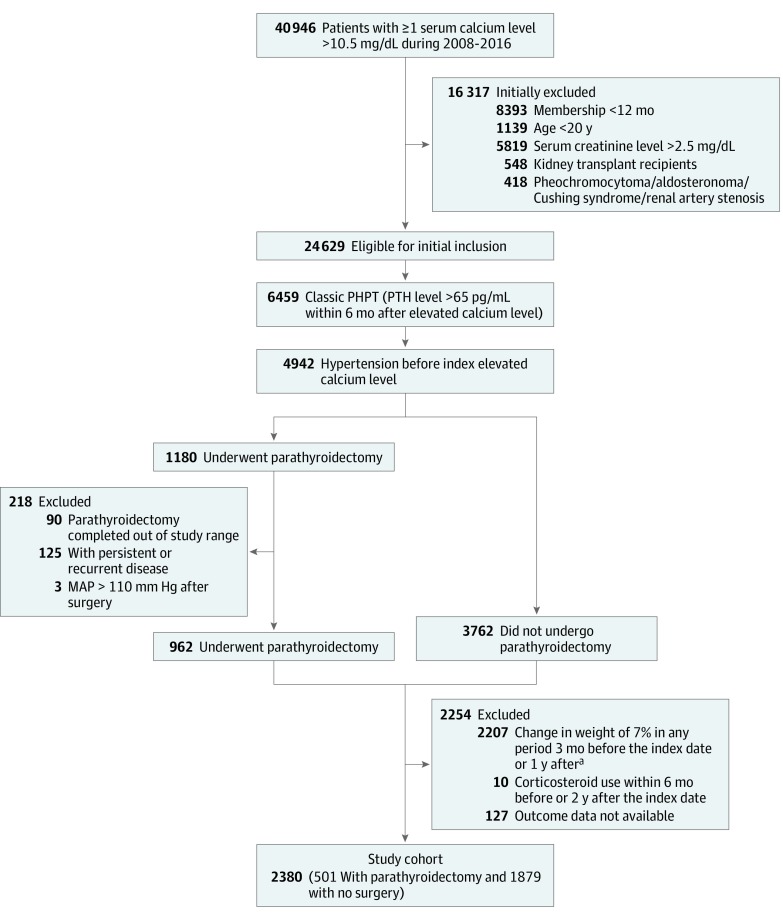
In this cohort study and retrospective database review, patients with PHPT and hypertension between January 1, 2008, and December 31, 2016, were identified from the Kaiser Permanente Southern California Region database. The initial cohort of patients with PHPT was identified using the criteria of an elevated PTH level exceeding 65 pg/mL within 6 months (to convert PTH level to nanograms per liter, multiply by 1.0) after an elevated serum calcium level exceeding 10.5 mg/dL (to convert calcium level to millimoles per liter, multiply by 0.25) (Figure 1). Patients with concurrent hypertension before the index elevated calcium level were then identified by International Classification of Diseases, Ninth Revision (ICD-9) codes for hypertension (401.1 and 401.9). Patients were excluded if they had had Kaiser Permanente membership for less than 12 months, were younger than 20 years, had a serum creatinine level exceeding 2.5 mg/dL (to convert creatinine level to micromoles per liter, multiply by 88.4), were kidney transplant recipients, or had a diagnosis of pheochromocytoma, aldosteronoma, Cushing syndrome, or renal artery stenosis.
Figure 1. Derivation of the Study Cohort.
MAP indicates mean arterial pressure; PHPT, primary hyperparathyroidism; and PTH, parathyroid hormone. To convert calcium level to millimoles per liter, multiply by 0.25; creatinine level to micromoles per liter, multiply by 88.4; and PTH level to nanograms per liter, multiply by 1.0.
aThe index date is the surgery date for those with parathyroidectomy and is the index elevated calcium level date for those who did not undergo surgery.
Before analysis, patients with persistent or recurrent PHPT after parathyroidectomy were excluded. Patients taking corticosteroids between 6 months before and 2 years after time zero were also excluded. To account for the confounding consequences of weight change on hypertension, patients with a weight change exceeding 7% between 3 months before and 1 year after time zero were excluded (n = 2117). Patients who underwent parathyroidectomy were identified by Current Procedural Terminology (CPT) codes 60500 and 60505 (Figure 1). Kaiser Permanente Southern California Institutional Review Board approval was obtained before the initiation of this research. Informed consent was waived by the institutional review board because of the retrospective nature of the study and the negligible consequences on the study cohort.
Baseline demographics and clinical characteristics were obtained for each group (no surgery and parathyroidectomy). The median mean arterial pressure (MAP) and antihypertensive medication use were analyzed for both study groups at baseline and 6 months, 1 year, and 2 years after parathyroidectomy or the date of diagnosis. Blood pressure measurements were obtained in both inpatient and outpatient settings. Antihypertensive medications were identified in the database by Generic Product Identifier and generic name. The date of surgery was considered as time zero for the parathyroidectomy group, and the date of PHPT diagnosis (the date of the index high calcium level) was considered as time zero for the nonsurgical group. When analyzing the median MAP, the following periods were used: 6 months before time zero (recorded as baseline), 2 weeks after time zero to 6 months (recorded as 6 months), 6 months after time zero to 1 year (recorded as 1 year), and between 1 and 2 years after time zero (recorded as 2 years). In addition, because of the immediate perioperative fluctuations of blood pressure, blood pressure measurements within 48 hours of surgery were excluded. For each period, available blood pressures were incorporated into the median MAP. The median numbers of blood pressure measurements included in the median MAP calculation were 5 (interquartile range [IQR], 3-10) at baseline, 5 (IQR, 3-8) at 6 months, 4 (IQR, 2-8) at 1 year, and 9 (IQR, 5-16) at 2 years. Antihypertensive medication use during the following periods was analyzed: 1 month before until time zero (recorded as baseline), 6 to 7 months after time zero (recorded as 6 months), 12 to 13 months after time zero (recorded as 1 year), and 23 to 24 months after time zero (recorded as 2 years). The mean number of antihypertensive medications in each of these periods was evaluated. The change in antihypertensive medication use was assessed by categorizing patients as (1) those taking fewer antihypertensive medications at each period compared with baseline, (2) those taking more antihypertensive medications in each period, and (3) those with no change in antihypertensive medication use.
Baseline demographic and clinical characteristics between the nonsurgical group and the parathyroidectomy group were compared using χ2 tests for categorical variables and t tests for continuous variables. The median MAP and antihypertensive medication use were plotted over time. The difference in change of the MAP and antihypertensive medications between groups was assessed using 2-tailed unpaired t tests. The proportions of patients who were prescribed more or fewer antihypertensive medications, stopped taking antihypertensive medications, or started taking antihypertensive medications relative to baseline were calculated. χ2 Tests were performed to test the balance of proportions between the nonsurgical group and the parathyroidectomy group. Multivariable logistic regression models were used to obtain adjusted odds ratios (AORs) for the strength of association between surgical intervention and both antihypertensive medication increase and antihypertensive medication decrease at 6 months, 1 year, and 2 years. All models were adjusted for baseline demographics and clinical risk factors, including age, sex, body mass index (BMI), MAP, baseline number of antihypertensive medications, PTH level and calcium level at baseline and 6 months, and Charlson Comorbidity Index (CCI) score (range, 0-33; higher index indicates a greater burden of comorbid diseases and higher risk of mortality at 1 year). A second analysis using propensity score matching was also performed comparing the parathyroidectomy group with a matched nonsurgical cohort (eMethods in the Supplement).
Statistical significance was set at 2-sided P < .05. All analyses were performed using statistical software (SAS, version 9.4; SAS Institute Inc).
Results
In total, 2380 patients (including 1880 females [79.0%]) with classic PHPT and hypertension who met inclusion and exclusion criteria for the study were identified in the database. Of those, 501 underwent parathyroidectomy. The mean (SD) length of follow-up was 1.9 (0.3) years in both study groups. There was no significant difference in the proportion of female patients (79.2% [1488 of 1879] in the nonsurgical group vs 78.2% [392 of 501] in the parathyroidectomy group, P = .64) or BMI (calculated as weight in kilograms divided by height in meters squared) (mean [SD] BMI, 29.9 [6.7] in the nonsurgical group vs 30.0 [6.5] in the parathyroidectomy group; P = .80) (Table 1). Patients who underwent parathyroidectomy were younger (mean [SD] age, 65.3 [9.7] vs 71.9 [10.4] years in the nonsurgical group; P < .001), took fewer antihypertensive medications at baseline (mean [SD], 1.2 [1.1] vs 1.5 [1.3] medications in the nonsurgical group; P < .001), and had lower CCIs (mean [SD], 1.6 [1.8] vs 2.4 [2.2] in the nonsurgical group; P < .001) (Table 1).
Table 1. Baseline Demographic and Clinical Characteristics.
| Variable | No Surgery (n = 1879) | Parathyroidectomy (n = 501) | P Value |
|---|---|---|---|
| Age, mean (SD), y | 71.9 (10.4) | 65.3 (9.7) | <.001 |
| Age, y, No. (%) | |||
| <65 | 432 (23.0) | 214 (42.7) | <.001 |
| 65-75 | 665 (35.4) | 200 (39.9) | |
| >75 | 782 (41.6) | 87 (17.4) | |
| Sex, No. (%) | |||
| Female | 1488 (79.2) | 392 (78.2) | .64 |
| Male | 391 (20.8) | 109 (21.8) | |
| Race/ethnicity, No. (%) | |||
| Non-Hispanic Asian | 132 (7.0) | 26 (5.2) | <.001 |
| Non-Hispanic black | 398 (21.2) | 96 (19.2) | |
| Hispanic | 298 (15.9) | 115 (23.0) | |
| Non-Hispanic white | 1012 (53.9) | 260 (51.9) | |
| Non-Hispanic other | 39 (2.1) | 4 (0.8) | |
| Length of follow-up, mean (SD), y | 1.9 (0.3) | 1.9 (0.3) | .89 |
| BMI, mean (SD) | 29.9 (6.7) | 30.0 (6.5) | .80 |
| BMI, No. (%) | |||
| Normal, <25 | 416 (22.1) | 108 (21.6) | .96 |
| Overweight, 25-30 | 667 (35.5) | 178 (35.5) | |
| Obese, >30 | 796 (42.4) | 215 (42.9) | |
| Median MAP (SD), mm Hg | 92.6 (9.4) | 94.3 (8.2) | <.001 |
| No. of antihypertensive medications, mean (SD) | 1.5 (1.3) | 1.2 (1.1) | <.001 |
| PTH level, mean (SD), pg/mLa | 104.7 (62.5) | 149.0 (97.6) | <.001 |
| Calcium level, mean (SD), mg/dLa | 10.9 (0.5) | 11.0 (0.7) | <.001 |
| Charlson Comorbidity Index score, mean (SD)b | 2.4 (2.2) | 1.6 (1.8) | <.001 |
| Charlson Comorbidity Index score, No. (%) | |||
| 0 | 429 (22.8) | 185 (36.9) | <.001 |
| 1-2 | 690 (36.7) | 194 (38.7) | |
| ≥3 | 760 (40.4) | 122 (24.4) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MAP, mean arterial pressure; PTH, parathyroid hormone.
SI conversion factors: To convert calcium level to millimoles per liter, multiply by 0.25; PTH level to nanograms per liter, multiply by 1.0.
Baseline PTH and calcium levels were derived as the median PTH or calcium levels within 6 months before the index date.
The Charlson Comorbidity Index score ranges from 0 to 33; a higher index indicates a higher risk of mortality at 1 year.
The median (SD) MAP was higher at baseline in the parathyroidectomy group (94.3 [8.2] vs 92.6 [9.4] mm Hg in the nonsurgical group, P < .001) (Table 1). Both study groups had improvement in their blood pressure profiles over time. The changes in the median (SD) MAP among the parathyroidectomy group were 94.3 (8.2) mm Hg at baseline, 93.3 (8.7) mm Hg at 6 months after parathyroidectomy, 93.1 (9.1) mm Hg at 1 year, and 93.5 (9.1) mm Hg at 2 years (Table 1 and Table 2). The nonsurgical group had the following median (SD) values for the same periods: 92.6 (9.4) mm Hg at baseline, 92.4 (8.9) mm Hg at 6 months, 92.7 (8.8) mm Hg at 1 year, and 92.5 (8.6) mm Hg at 2 years. The change in the median MAP at each time point was compared with the baseline. The parathyroidectomy group had a statistically significant improvement in their median MAP that was greater than the improvement in the nonsurgical group (median [SD] values were −1.0 [7.6] vs −0.2 [8.5] mm Hg, P = .046 at 6 months; −1.2 [7.7] vs 0.1 [8.7] mm Hg, P = .002 at 1 year; and −0.8 [7.9] vs −0.1 [8.7] mm Hg, P = .04 at 2 years) (Table 2).
Table 2. Change in Outcomes Over Timea.
| Variable | 6 mo | 1 y | 2 y | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Surgery (n = 1879) | Parathyroidectomy (n = 501) | Difference in Change (95% CI) | P Value | No Surgery (n = 1879) | Parathyroidectomy (n = 501) | Difference in Change (95% CI) | P Value | No Surgery (n = 1879) | Parathyroidectomy (n = 501) | Difference in Change (95% CI) | P Value | |
| Median MAP (SD), mm Hg | 92.4 (8.9) | 93.3 (8.7) | NA | NA | 92.7 (8.8) | 93.1 (9.1) | NA | NA | 92.5 (8.6) | 93.5 (9.1) | NA | NA |
| No. of antihypertensive medications, mean (SD) | 1.5 (1.2) | 1.2 (1.1) | NA | NA | 1.5 (1.3) | 1.1 (1.1) | NA | NA | 1.3 (1.3) | 1.0 (1.1) | NA | NA |
| Change in Outcome Compared With Baseline | ||||||||||||
| Median MAP (SD), mm Hg | −0.2 (8.5) | −1.0 (7.6) | 0.8 (0.0 to 1.6) |
.046 | 0.1 (8.7) | −1.2 (7.7) | 1.3 (0.5 to 2.2) |
.002 | −0.1 (8.7) | −0.8 (7.9) | 0.7 (0.0 to 1.8) |
.04 |
| No. of antihypertensive medications, mean (SD) | 0.0 (0.7) | −0.1 (0.6) | 0.1 (0.0 to 0.1) |
.01 | −0.0 (0.8) | −0.1 (0.7) | 0.1 (0.0 to 0.2) |
.007 | −0.3 (1.1) | −0.3 (0.9) | 0.1 (−0.1 to 0.1) |
.09 |
| No./Total No. (%) of Patients Compared With Baseline | ||||||||||||
| Prescribed more antihypertensive medications | 298 (15.9) | 49 (9.8) | NA | .001 | 340 (18.1) | 54 (10.8) | NA | <.001 | 330 (17.6) | 61 (12.2) | NA | .004 |
| No change in No. of antihypertensive medications | 1313 (69.9) | 377 (75.2) | NA | .02 | 1208 (64.3) | 342 (68.3) | NA | .10 | 986 (52.5) | 279 (55.7) | NA | .20 |
| Prescribed fewer antihypertensive medicationsb | 268/1432 (18.7) | 75/374 (20.1) | NA | .56 | 331/1432 (23.1) | 105/374 (28.1) | NA | .05 | 563/1432 (39.3) | 161/374 (43.0) | NA | .19 |
| Stopped taking antihypertensive medicationsb | 102/1432 (7.1) | 34/374 (9.1) | NA | .20 | 166/1432 (11.6) | 58/374 (15.5) | NA | .04 | 397/1432 (27.7) | 117/374 (31.3) | NA | .17 |
| Started taking antihypertensive medicationsc | 120/447 (26.8) | 12/127 (9.4) | NA | <.001 | 136/447 (30.4) | 13/127 (10.2) | NA | <.001 | 124/447 (27.7) | 18/127 (14.2) | NA | .002 |
Abbreviations: MAP, mean arterial pressure; NA, not applicable.
Difference in change is between the parathyroidectomy group and the nonsurgical group compared with baseline.
Variable includes only patients taking antihypertensive medications at baseline (1432 in the nonsurgical group and 374 in the parathyroidectomy group).
Variable includes only patients taking no antihypertensive medications at baseline (447 in the nonsurgical group and 127 in the parathyroidectomy group).
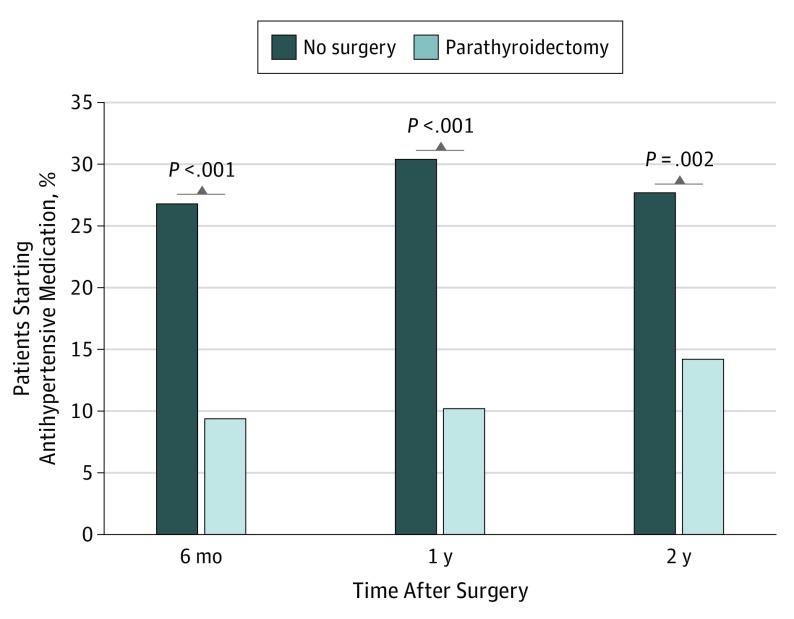
The mean (SD) number of antihypertensive medications prescribed at baseline was lower in the parathyroidectomy group (1.2 [1.1] vs 1.5 [1.3] in the nonsurgical group, P < .001) (Table 1). For the parathyroidectomy group, there was no significant difference in the mean number of antihypertensive medications at the time of diagnosis and at the time of surgery (eTable 1 in the Supplement). At all periods, the parathyroidectomy group had a more favorable pattern of antihypertensive medication use than the nonsurgical group. Most patients had no change in the number of antihypertensive medications. The proportion of patients taking fewer antihypertensive medications was higher in the parathyroidectomy group compared with the nonsurgical group. However, the difference was not statistically significant between the parathyroidectomy group vs the nonsurgical group (20.1% [75 of 374] vs 18.7% [268 of 1432], P = .56 at 6 months; 28.1% [105 of 374] vs 23.1% [331 of 1432], P = .05 at 1 year; and 43.0% [161 of 374] vs 39.3% [563 of 1432], P = .19 at 2 years). The parathyroidectomy group was less likely vs the nonsurgical group to increase the number of antihypertensive medications during the study period (9.8% [49 of 501] vs 15.9% [298 of 1879], P = .001 at 6 months; 10.8% [54 of 501] vs 18.1% [340 of 1879], P < .001 at 1 year; and 12.2% [61 of 501] vs 17.6% [330 of 1879], P = .004 at 2 years) (Table 2). Patients taking no antihypertensive medications at baseline who then started antihypertensive medication regimens during the study period were analyzed. There was a considerable difference between the 2 study groups. The parathyroidectomy group was less likely vs the nonsurgical group to begin taking antihypertensive medications (9.4% [12 of 127] vs 26.8% [120 of 447], P < .001 at 6 months; 10.2% [13 of 127] vs 30.4% [136 of 447], P < .001 at 1 year; and 14.2% [18 of 127] vs 27.7% [124 of 447], P = .002 at 2 years) (Figure 2).
Figure 2. Patients Starting Antihypertensive Medication Therapy.
Shown is the percentage of patients who were not taking antihypertensive medications at baseline but began taking antihypertensive medications during the study period.
Multivariable regression analysis revealed that the parathyroidectomy group was less likely to increase their antihypertensive medication use (AOR, 0.59; 95% CI, 0.40-0.86; P = .006 at 6 months; AOR, 0.49; 95% CI, 0.34-0.70; P < .001 at 1 year; and AOR, 0.55; 95% CI, 0.39-0.79; P = .001 at 2 years) (Table 3). Those taking more baseline antihypertensive medications were less likely to increase the number of antihypertensive medications (AOR, 0.66; 95% CI, 0.59-0.74; P < .001 at 6 months; AOR, 0.65; 95% CI, 0.59-0.73; P < .001 at 1 year; and AOR, 0.66; 95% CI, 0.59-0.73; P < .001 at 2 years). Older age was an independent risk factor associated with increasing antihypertensive medication use (AOR, 1.50; 95% CI, 1.09-2.06; P = .01 for ages 65-75 vs age <65 years at 6 months; AOR, 1.57; 95% CI, 1.15-2.13; P = .004 at 1 year; and AOR, 1.67; 95% CI, 1.23-2.26; P < .001 at 2 years). Obesity was also associated with more antihypertensive medication use at all periods (AOR, 1.44; 95% CI, 1.03-2.01; P = .03 for BMI >30 vs <25 at 6 months; AOR, 1.52; 95% CI, 1.11-2.08; P = .01 at 1 year; and AOR, 1.82; 95% CI, 1.31-2.52; P < .001 at 2 years). Higher CCIs were associated with antihypertensive medication use. Preoperative PTH, baseline calcium level, and calcium level at 6 months were not consistently associated with increasing antihypertensive medication use (Table 3).
Table 3. Multivariable Logistic Regressions for Change in Antihypertensive Medication Use.
| Variable | 6 mo | 1 y | 2 y | |||
|---|---|---|---|---|---|---|
| AOR (95% CI) | P Value | AOR (95% CI) | P Value | AOR (95% CI) | P Value | |
| Prescribed More Antihypertensive Medications (N = 2380) | ||||||
| Surgery | ||||||
| No surgery | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Parathyroidectomy | 0.59 (0.40-0.86) | .006 | 0.49 (0.34-0.70) | <.001 | 0.55 (0.39-0.79) | .001 |
| Age, y | ||||||
| <65 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 65-75 | 1.50 (1.09-2.06) | .01 | 1.57 (1.15-2.13) | .004 | 1.67 (1.23-2.26) | <.001 |
| >75 | 1.61 (1.15-2.26) | .006 | 1.73 (1.25-2.39) | <.001 | 1.55 (1.12-2.15) | .008 |
| Sex | ||||||
| Female | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Male | 0.93 (0.69-1.24) | .61 | 1.23 (0.94-1.61) | .13 | 1.07 (0.82-1.41) | .61 |
| No. of antihypertensive medicationsa | 0.66 (0.59-0.74) | <.001 | 0.65 (0.59-0.73) | <.001 | 0.66 (0.59-0.73) | <.001 |
| MAPa | 1.03 (1.01-1.04) | <.001 | 1.02 (1.01-1.03) | <.001 | 1.01 (1.00-1.02) | .10 |
| BMIa | ||||||
| Normal, <25 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Overweight, 25-30 | 1.39 (1.00-1.93) | .05 | 1.18 (0.86-1.61) | .31 | 1.56 (1.13-2.16) | .007 |
| Obese, >30 | 1.44 (1.03-2.01) | .03 | 1.52 (1.11-2.08) | .01 | 1.82 (1.31-2.52) | <.001 |
| PTH levela | 1.00 (1.00-1.00) | .57 | 1.00 (1.00-1.00) | .39 | 1.00 (1.00-1.00) | .08 |
| Calcium levela | 1.16 (0.88-1.52) | .29 | 1.40 (1.09-1.81) | .009 | 1.23 (0.95-1.58) | .11 |
| Calcium level at 6 mo | 0.95 (0.78-1.17) | .65 | 0.88 (0.73-1.07) | .21 | 0.86 (0.71-1.04) | .11 |
| Charlson Comorbidity Index scoreb | ||||||
| 0 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 1-2 | 1.55 (1.13-2.14) | .007 | 1.53 (1.13-2.08) | .006 | 1.57 (1.15-2.13) | .004 |
| ≥3 | 2.04 (1.46-2.85) | <.001 | 2.06 (1.50-2.84) | <.001 | 2.07 (1.50-2.86) | <.001 |
| Prescribed Fewer Antihypertensive Medications (n = 1806)c | ||||||
| Surgery | ||||||
| No surgery | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Parathyroidectomy | 1.33 (0.94-1.90) | .11 | 1.45 (1.05-2.00) | .02 | 1.30 (0.98-1.72) | .07 |
| Age, y | ||||||
| <65 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 65-75 | 0.62 (0.45-0.86) | .004 | 0.56 (0.41-0.75) | <.001 | 0.78 (0.61-1.02) | .07 |
| >75 | 0.83 (0.60-1.17) | .29 | 0.80 (0.59-1.08) | .15 | 0.86 (0.66-1.13) | .28 |
| Sex | ||||||
| Female | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Male | 1.30 (0.98-1.72) | .07 | 1.11 (0.85-1.45) | .43 | 1.01 (0.80-1.28) | .92 |
| No. of antihypertensive medicationsa | 1.51 (1.35-1.69) | <.001 | 1.43 (1.28-1.59) | <.001 | 1.25 (1.13-1.37) | <.001 |
| MAPa | 1.01 (0.99-1.02) | .36 | 1.01 (0.99-1.02) | .32 | 1.01 (1.00-1.03) | .02 |
| BMIa | ||||||
| Normal, <25 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Overweight, 25-30 | 0.93 (0.66-1.31) | .87 | 1.01 (0.74-1.37) | .97 | 0.96 (0.74-1.26) | .79 |
| Obese, >30 | 0.97 (0.69-1.36) | .67 | 0.86 (0.63-1.17) | .33 | 0.87 (0.66-1.13) | .30 |
| PTH levela | 1.00 (1.00-1.00) | .29 | 1.00 (1.00-1.00) | .83 | 1.00 (1.00-1.00) | .14 |
| Calcium levela | 0.91 (0.70-1.19) | .51 | 1.07 (0.84-1.36) | .59 | 1.15 (0.93-1.29) | .19 |
| Calcium level at 6 mo | 1.08 (0.88-1.33) | .46 | 1.10 (0.91-1.33) | .33 | 1.09 (0.93-1.18) | .31 |
| Charlson Comorbidity Index scoreb | ||||||
| 0 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 1-2 | 1.05 (0.74-1.49) | .78 | 0.92 (0.68-1.26) | .60 | 0.91 (0.70-1.18) | .47 |
| ≥3 | 1.13 (0.79-1.62) | .52 | 1.01 (0.73-1.39) | .95 | 1.19 (0.90-1.57) | .22 |
Abbreviations: AOR, adjusted odds ratio; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MAP, mean arterial pressure; NA, not applicable; PTH, parathyroid hormone.
Variable represents values at baseline.
The Charlson Comorbidity Index score ranges from 0 to 33; a higher index indicates a higher risk of mortality at 1 year.
Variables include only patients taking antihypertensive medications at baseline.
Multivariable regression analysis to assess factors associated with decreased antihypertensive medication use revealed an increased number of antihypertensive medications at baseline to be a positive risk factor (AOR, 1.51; 95% CI, 1.35-1.69; P < .001 at 6 months; AOR, 1.43; 95% CI, 1.28-1.59; P < .001 at 1 year; and AOR, 1.25; 95% CI, 1.13-1.37; P < .001 at 2 years). The parathyroidectomy group was more likely to decrease their antihypertensive medication use relative to the nonsurgical group only at the 1-year period (AOR, 1.45; 95% CI, 1.05-2.00; P = .02). Preoperative PTH level, baseline calcium level, and calcium level at 6 months after parathyroidectomy were not associated with decreasing antihypertensive medication use (Table 3).
Propensity score matching included 438 patients in each study group. The 2 study groups were well matched; none of the variables had a standardized difference exceeding 0.10 (eTable 2 in the Supplement). Patients in the parathyroidectomy group were less likely to require more antihypertensive medications (AOR, 0.49; 95% CI, 0.31-0.80; P = .004 at 6 months; AOR, 0.44; 95% CI, 0.27-0.70; P < .001 at 1 year; and AOR, 0.61; 95% CI, 0.39-0.96; P = .03 at 2 years) (eTable 3 in the Supplement).
Discussion
This study’s findings suggest that parathyroidectomy for patients with PHPT and hypertension may be associated with a decrease in the MAP as well as with a decrease in the requirement for antihypertensive medications. Studies of the mechanisms underlying the association between PHPT and hypertension have focused on the renin-angiotensin-aldosterone system and the possible influence of PTH on vascular smooth muscle. Parathyroid hormone stimulates renin production, which in turn contributes to increased blood pressure and vessel sensitization to vasopressors.9 Investigations of the reactivity of PTH with vascular smooth muscle have been conflicting. Parathyroid hormone infusion led to an increase in blood pressure in normotensive patients but a decrease in blood pressure in hypertensive patients.10,11
In the clinical realm, other research has supported the notion that there is a link between cardiovascular outcomes and parathyroidectomy. In their prospective study of the association of parathyroidectomy with cardiovascular outcomes, Agarwal et al12 observed improvements in left ventricular mass, systolic and diastolic function, and smooth muscle–mediated vasodilation from 3 to 6 months after parathyroidectomy. McMahon et al8 found that parathyroidectomy reduced left ventricular mass in the first 6 months after surgery. However, some data contradict the idea that parathyroidectomy has beneficial cardiovascular consequences. In a prospective study of 21 patients, Dural et al13 showed that coronary artery calcification was not altered by parathyroidectomy, while arterial stiffness changes were heterogeneous after parathyroidectomy.
A limited number of clinical studies examining hypertension and parathyroidectomy have exhibited a link between the two. In their retrospective study of 147 patients with PHPT and hypertension, Heyliger et al14 observed that parathyroidectomy reduced both systolic and diastolic blood pressure, with the mean reduction exceeding 10 mm Hg. A database study of a large population by Kalla et al6 investigated the association between PHPT and cardiovascular risk factors and events. In their multivariable regression analysis, they found that PHPT was an independent predictor of hypertension. Our population-based study reinforces these findings in that antihypertensive medication use and the median MAP improved in those patients who underwent parathyroidectomy.
In this retrospective population-based study, the association between parathyroidectomy and hypertension was evaluated using the clinically significant end points of the MAP and the use of antihypertensive medications. The large database allowed for the application of rigorous exclusion criteria, including 2117 patients with a weight change exceeding 7%. In keeping with previous findings on PHPT in the Kaiser Permanente Southern California Region database,15 a creatinine level of 2.5 mg/dL or less was used herein as a cutoff to exclude patients with renal failure. Our 2 study groups were similar in their female to male ratio, length of follow-up, and BMI, but they differed in age, baseline number of antihypertensive medications, PTH level, and calcium level (Table 1). Other comorbidities that may alter cardiovascular outcomes, such as coronary artery disease, history of stroke, congestive heart failure, and diabetes, were not considered in the present study. Our study focused on the outcome of hypertension; while the aforementioned other comorbidities may relate to overall patient morbidity and mortality, they are not determinants of hypertension. There may potentially have been differences between the 2 study groups for which there was no control. However, the use of multivariable regression analysis, inclusion of the CCI, and propensity score matching mitigated the consequences of these differences on the relevant outcome of antihypertensive medication use.
There was a statistically significant improvement in the median MAP among the parathyroidectomy group compared with the nonsurgical group (Table 2). The improvement in the median MAP is consistent with the findings by Heyliger et al14 in that blood pressure improved after parathyroidectomy. The absolute difference in the median MAP herein was small but statistically significant. This measured change in the median MAP may overlook greater absolute changes for some individuals. It may also have been limited because of adaptive changes in treatment regimens instituted by the patients’ primary care physicians, reflected by the increased number of antihypertensive medications in the nonsurgical group. The limited change in the median MAP in both study groups may reflect effective clinical management, limiting differences in the degree of control of hypertension, although this was not specifically evaluated in our analysis.
To our knowledge, this study is the first detailed investigation of the possible association of parathyroidectomy with changes in antihypertensive medication use at the population level. Antihypertensive medication use is a relevant clinical factor that reflects the association of parathyroidectomy with hypertension. The pattern of antihypertensive medication use for both study groups improved over time. The mean number of antihypertensive medications was lower at all periods relative to baseline (Table 2). Both univariate and multivariable analyses showed that those who underwent parathyroidectomy were less likely to require an increase in antihypertensive medications at any time point (Tables 2 and 3). Similar results for antihypertensive medication increase and parallel findings for antihypertensive medication decrease at 1 year were seen on the propensity score–matched analysis, which further reinforce our observations. In addition, patients who were not taking any antihypertensive medications at baseline were far less likely to start an antihypertensive medication regimen if they underwent parathyroidectomy. For example, 1 year after parathyroidectomy, the nonsurgical group was 3 times more likely to have started taking antihypertensive medications (10.2% [13 of 127] in the parathyroidectomy group vs 30.4% [136 of 447] in the nonsurgical group, P < .001) (Table 2). This is clinically relevant and reinforces the potential beneficial cardiovascular implications of parathyroidectomy. In those patients with borderline hypertension, who may be on the verge of requiring antihypertensive medication for management of their hypertension, parathyroidectomy may allow them to avoid initiating treatment. Parathyroidectomy may also have implications at the population level, allowing for more cost-effective care by preventing antihypertensive medication use and reducing the use of associated health care resources.
Parathyroidectomy was also an independent predictor of decreasing antihypertensive medication use at the 1-year period. However, surgery did not predict decreasing antihypertensive medication use at the 6-month and 2-year time points (Table 3). This finding suggests that the potential beneficial outcome of parathyroidectomy for decreasing antihypertensive medication use may be transient.
In accord with the well-established findings of the associations of age and obesity with hypertension, this study showed these factors to be independent risk factors for increasing antihypertensive medication use (Table 3). Anderson et al5 found that PTH level was linked to hypertension. However, in the present study, baseline PTH level was not associated with later antihypertensive medication use. Similarly, baseline calcium levels and postoperative calcium levels were not associated with the number of antihypertensive medications patients required in our study.
Limitations
Our study has some limitations. These include its retrospective design and the lack of data regarding antihypertensive medication dosage. This study was also constrained in that ICD-9 and CPT codes were used, and coding errors could have altered the data.
Conclusions
In this large, population-based study of hypertensive patients with PHPT, parathyroidectomy was associated with greater decreases in the MAP, as well as reduced requirements for antihypertensive medications. Among patients who were never taking antihypertensive medications, parathyroidectomy reduced the proportion of patients who started taking antihypertensive medications. Additional study will be required to find whether there are downstream cardiovascular benefits of parathyroidectomy. Preexisting hypertension, particularly in those not already taking antihypertensive medications at the time of diagnosis, should be considered in weighing surgical treatment.
eMethods. Propensity Score Matching Description
eTable 1. Number of Antihypertensive Medications Prescribed for Parathyroidectomy Patients
eTable 2. Patient Characteristics After Propensity Score Matching
eTable 3. Estimated Effects of Parathyroidectomy on Change in Antihypertensive Medication Use (Matched Cohort)
References
- 1.Herrmann G, Hehrmann R, Scholz HC, et al. Parathyroid hormone in coronary artery disease: results of a prospective study. J Endocrinol Invest. 1986;9(4):265-271. doi: 10.1007/BF03346923 [DOI] [PubMed] [Google Scholar]
- 2.Joborn H, Lundin L, Hvarfner A, Johansson G, Wide L, Ljunghall S. Serum electrolytes and parathyroid hormone in patients in a coronary care unit. J Intern Med. 1989;225(1):9-14. doi: 10.1111/j.1365-2796.1989.tb00029.x [DOI] [PubMed] [Google Scholar]
- 3.Watson KE, Abrolat ML, Malone LL, et al. Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation. 1997;96(6):1755-1760. doi: 10.1161/01.CIR.96.6.1755 [DOI] [PubMed] [Google Scholar]
- 4.Bilezikian JP. Primary hyperparathyroidism. J Clin Endocrinol Metab. 2018;103(11):3993-4004. doi: 10.1210/jc.2018-01225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson JL, Vanwoerkom RC, Horne BD, et al. Parathyroid hormone, vitamin D, renal dysfunction, and cardiovascular disease: dependent or independent risk factors? Am Heart J. 2011;162(2):331-339.e2. doi: 10.1016/j.ahj.2011.05.005 [DOI] [PubMed] [Google Scholar]
- 6.Kalla A, Krishnamoorthy P, Gopalakrishnan A, Garg J, Patel NC, Figueredo VM. Primary hyperparathyroidism predicts hypertension: results from the National Inpatient Sample. Int J Cardiol. 2017;227:335-337. doi: 10.1016/j.ijcard.2016.11.080 [DOI] [PubMed] [Google Scholar]
- 7.Pepe J, Cipriani C, Sonato C, Raimo O, Biamonte F, Minisola S. Cardiovascular manifestations of primary hyperparathyroidism: a narrative review. Eur J Endocrinol. 2017;177(6):R297-R308. doi: 10.1530/EJE-17-0485 [DOI] [PubMed] [Google Scholar]
- 8.McMahon DJ, Carrelli A, Palmeri N, et al. Effect of parathyroidectomy upon left ventricular mass in primary hyperparathyroidism: a meta-analysis. J Clin Endocrinol Metab. 2015;100(12):4399-4407. doi: 10.1210/jc.2015-3202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gennari C, Nami R, Gonnelli S. Hypertension and primary hyperparathyroidism: the role of adrenergic and renin-angiotensin-aldosterone systems. Miner Electrolyte Metab. 1995;21(1-3):77-81. [PubMed] [Google Scholar]
- 10.Jespersen B, Randløv A, Abrahamsen J, Fogh-Andersen N, Kanstrup IL. Effects of PTH(1-34) on blood pressure, renal function, and hormones in essential hypertension: the altered pattern of reactivity may counteract raised blood pressure. Am J Hypertens. 1997;10(12, pt 1):1356-1367. doi: 10.1016/S0895-7061(97)00275-6 [DOI] [PubMed] [Google Scholar]
- 11.Fliser D, Franek E, Fode P, et al. Subacute infusion of physiological doses of parathyroid hormone raises blood pressure in humans. Nephrol Dial Transplant. 1997;12(5):933-938. doi: 10.1093/ndt/12.5.933 [DOI] [PubMed] [Google Scholar]
- 12.Agarwal G, Nanda G, Kapoor A, et al. Cardiovascular dysfunction in symptomatic primary hyperparathyroidism and its reversal after curative parathyroidectomy: results of a prospective case control study. Surgery. 2013;154(6):1394-1403. doi: 10.1016/j.surg.2013.06.047 [DOI] [PubMed] [Google Scholar]
- 13.Dural C, Okoh AK, Seicean A, et al. A pilot study investigating the effect of parathyroidectomy on arterial stiffness and coronary artery calcification in patients with primary hyperparathyroidism. Surgery. 2016;159(1):218-224. doi: 10.1016/j.surg.2015.07.037 [DOI] [PubMed] [Google Scholar]
- 14.Heyliger A, Tangpricha V, Weber C, Sharma J. Parathyroidectomy decreases systolic and diastolic blood pressure in hypertensive patients with primary hyperparathyroidism. Surgery. 2009;146(6):1042-1047. doi: 10.1016/j.surg.2009.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeh MW, Ituarte PH, Zhou HC, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013;98(3):1122-1129. doi: 10.1210/jc.2012-4022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Propensity Score Matching Description
eTable 1. Number of Antihypertensive Medications Prescribed for Parathyroidectomy Patients
eTable 2. Patient Characteristics After Propensity Score Matching
eTable 3. Estimated Effects of Parathyroidectomy on Change in Antihypertensive Medication Use (Matched Cohort)