Through the actions of multi‐stakeholder communities, Learning Health Systems (LHSs) undertake cyclical activities that generate new knowledge and, as seamlessly as possible, apply that new knowledge in direct pursuit of health improvement.1 Therefore, knowledge links the discovery and intervention components of LHS activity and, metaphorically, as shown in Figure 1, can be seen as the “keystone” supporting the learning cycle.
Figure 1.
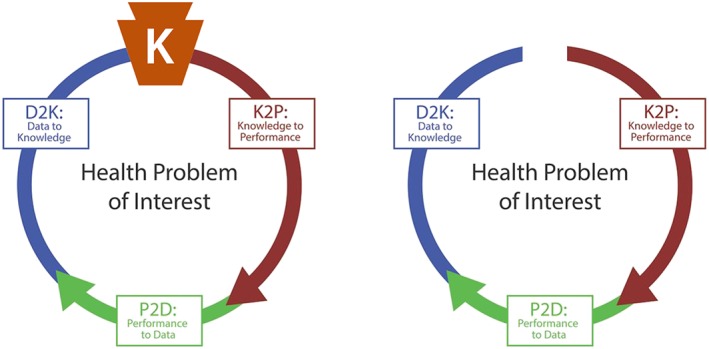
Knowledge as the “keystone” of the learning cycle (left). Absence of persistent knowledge creates a gap in the cycle (right)
In this context, health‐related knowledge is the result of an analytic and/or deliberative process that holds significance for an identified community. Additionally, health knowledge is actionable when it can motivate and shape an intervention. For example, a community seeking to reduce mortality and morbidity from preventable diseases may learn, from data about many persons, a mathematical model that determines an individual's risk of developing a specific disease in the future.2 In this case, the predictive model embodies the newly learned knowledge. In an LHS, after local qualification,3 the model would then be applied in practice to combine an instance of data from one person to compute a prediction for him/her. If that person is found to be at risk for the disease, this will trigger appropriate preventive measures by their care provider(s). While this familiar pattern of training, testing, and using models describes methods employed in machine learning, here, this process is viewed more generally to include any systematic method resulting in and applying new knowledge, including knowledge derived from purely deliberative processes. Moreover, health knowledge spans the domains of health care, public health, biomedical research across the translational spectrum, and health professions education.
New knowledge is fundamental to the LHS concept and its operation. Knowledge embodies what the system “learns.” It follows that knowledge has a central, but often underappreciated, role in successful LHS operation. In particular, many descriptions of LHSs are explicit about the key role of “big data” in these systems, while leaving implicit the role of knowledge.4, 5 Inattention to knowledge creates a learning cycle without a keystone, leaving a dysfunctional gap (see Figure 1) between discovery and intervention.6 It follows that infrastructure supporting the operation of LHSs must address the management and implementation of knowledge as much as the generation of it.
Complementing the conceptual importance of knowledge to LHSs is the more concrete importance of supplementing human‐readable knowledge with representations of that same knowledge in machine‐executable forms, what may be called “computable knowledge”.7, 8, 9 Human‐readable knowledge is expressed in words, pictures, and mathematical symbols—and persistently stored in journals and books. Any action triggered by human‐readable knowledge requires an individual to read and comprehend the article or book before deciding what action might be taken in response. This is a slow, serial process. Creating a digital representation of human‐readable knowledge, using pdf or similar file formats, changes the way this knowledge is accessed but does not alter how the knowledge is used in the world.
By contrast, computable knowledge is expressed in code, fundamentally machine‐executable instructions that are inaccessible to direct human comprehension. When fed instances of data, computable knowledge can generate useful advice.10 Applying this idea to the earlier example of disease risk prediction, a machine‐executable version of the predictive model can be encoded in any appropriate computer language. When given an instance of data about an individual, this encoded model can quickly and accurately generate a risk prediction for that individual, and with equal ease, multiple models in computable form can generate a panel of predictions for that same individual. When, sequentially but extremely rapidly, one or more computable models are given instances of data about multiple individuals, they can generate predictions for these many individuals. For all practical purposes, these predictions are generated simultaneously.
Whereas the 15th century printing press revolutionized the world by enabling mass‐access to human‐readable knowledge, 21st century information technology now enables mass‐action application of computable knowledge. (See Figure 2.) This has enormous implications for Learning Health Systems because, on the implementation side of their cyclic operation (“knowledge to performance”), LHSs benefit from economies of both scale and scope made possible through mass‐action. With economy of scale, generating and transmitting actionable advice for thousands of instances across multiple locations, requires little more time and energy than generating advice for one. With economy of scope, advice generation, transmission, and subsequent action‐taking across multiple domains can be achieved as easily as for one, without fundamentally altering the infrastructure supporting the system. Exclusive reliance on mass‐access to human readable knowledge can realize neither of these economies.
Figure 2.
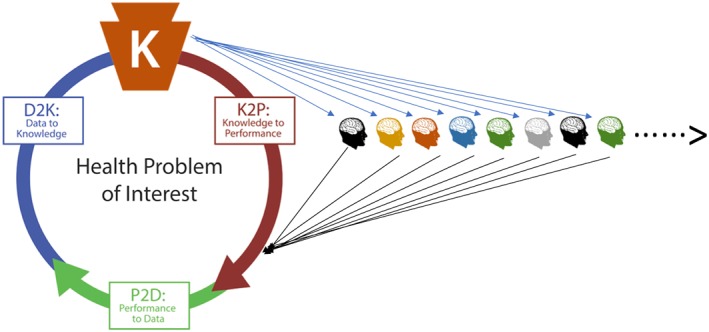
Scalable mass action in a learning cycle enabled by computable knowledge
Equally important, LHSs must accommodate learning across a range of tempos, and be able to support domains where learning will occur very rapidly 11. As noted previously, the “keystone” of the LHS is the representation of the knowledge the system has adopted for implementation at any point in time. As the system continues to learn over successive cycles of operation, there should be no lag between knowledge change and the capability for performance change aligned with the new knowledge. Particularly in domains where learning will occur very rapidly, the potential to implement performance change as rapidly as learning occurs can be achieved only through representations of knowledge that are encoded in computable forms.
Interest in this topic has given rise to a nascent movement to “Mobilize Computable Biomedical Knowledge” (MCBK).12 Two meetings jointly sponsored by the University of Michigan and the National Library of Medicine, held on the NIH campus in July of 2018 and 2019, have demonstrated the importance of machine‐executable knowledge as a key strategy to improve health.13, 14
For these reasons, it is both appropriate and necessary for Learning Health Systems to publish peer‐reviewed, machine‐executable knowledge. Accordingly, the Journal has established “Computable Knowledge” as a new publication type and welcomes submissions, initially under a pilot set of policies and procedures. Instructions for authors may be found at https://onlinelibrary.wiley.com/page/journal/23796146/homepage/forauthors.html. Complete publications will include computable versions of the knowledge that can be downloaded for general use, through an appropriate open source license. We will publish papers of two types:
Full‐length Computable Knowledge Enhanced Publications will describe a previously unpublished scientific effort resulting in one or more computable artifacts that will be an integral component of the publication.
Shorter Computable Knowledge Implementation Publications will serve as a “bridge to implementation” of a knowledge model that has been previously published. These articles will describe technical deployment and implementation details and include the computable artifacts.
We are proud that our Journal, in taking this step, will be one of the first biomedical journals to publish peer‐reviewed software in pursuit of scalable and sustainable Learning Health Systems.
Friedman CP, Flynn AJ. Computable knowledge: An imperative for Learning Health Systems. Learn Health Sys. 2019;3:e10203 10.1002/lrh2.10203
Dr Friedman is Editor in Chief, Learning Health Systems
Footnotes
IBM Watson,15 which uses automated methods to “read” human‐readable knowledge and provide advice, is not, in this view, an example of persistent computable knowledge. Watson does not convert what it has learned into computable models for consistent mass action. Instead, Watson learns an extensive but ever‐changing knowledge base and uses it to address each case as, effectively, a new problem.
REFERENCES
- 1. Friedman CP, Rubin JC, Sullivan KJ. Toward an information infrastructure for Global Health Improvement. Yearb Med Inform. 2017;26(01):16‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adriaans P. Learning as data compression In: Conference on Computability in Europe. Berlin, Heidelberg: Springer; 2007:11‐24. [Google Scholar]
- 3. Lehmann HP, Downs SM. Desiderata for sharable computable biomedical knowledge for learning health systems. Learning Health Syst. 2018;2(4):e10065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schneeweiss S. Learning from big health care data. N Engl J Med. 2014;370(23):2161‐2163. [DOI] [PubMed] [Google Scholar]
- 5. Bates DW, Saria S, Ohno‐Machado L, Shah A, Escobar G. Big data in health care: using analytics to identify and manage high‐risk and high‐cost patients. Health Aff. 2014;33(7):1123‐1131. [DOI] [PubMed] [Google Scholar]
- 6. Guise JM, Savitz LA, Friedman CP. Mind the gap: putting evidence into practice in the era of learning health systems. J Gen Intern Med. 2018;33(12):2237‐2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Adler‐Milstein J, Nong P, Friedman CP. Preparing healthcare delivery organizations for managing computable knowledge. Learning Health Syst. 2019;3(2):e10070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Library of Medicine . A platform for biomedical discovery and data‐powered health: National Library of Medicine Strategic Plan 2017–2027. US Department of Health and Human Services National Insitute of Health 2017.
- 9. Somers J. The scientific paper is obsolete. The Atlantic. 2018.
- 10. Flynn AJ. (in press) Theory of advice as an information object targeted at an unmade decision. Journal of Documentation
- 11. Goble C, De Roure D, Bechhofer S. Accelerating scientists' knowledge turns In: International Joint Conference on Knowledge Discovery, Knowledge Engineering, and Knowledge Management. Berlin, Heidelberg: Springer; 2011:3‐25. [Google Scholar]
- 12. http://mobilizecbk.org. Accessed .
- 13. https://medicine.umich.edu/dept/lhs/2018-mcbk-meeting , Accessed .
- 14. https://medicine.umich.edu/dept/lhs/2019-mcbk-meeting , Accessed .
- 15. High R. The era of cognitive systems: An inside look at IBM Watson and how it works. Armonk, New York: IBM Corporation, Redbooks; Dec. 12 2012. [Google Scholar]


