Abstract
Background:
Recognition of total elbow arthroplasties (TEAs) on plain radiographs is difficult due to a multitude of different types and models. Especially if surgery reports and documentation are not available, lost or when the primary surgery was performed in another hospital the prosthesis type may be undeterminable. Therefore we investigated in this platform study if a flowchart aids in recognition of thirteen different total elbow arthroplasty models on plain radiographs.
Methods:
An online questionnaire on the Shoulder and Elbow Platform was developed. Plain radiographs of thirteen TEA models were shown with and without the help of an especially developed flowchart describing distinguishing features.
Results:
Ten orthopedic surgeons specialized in upper extremity surgery completed the study. Recognition rates of the thirteen total elbow arthroplasty models ranged between 20 and 100 percent without the flowchart. Using the flowchart recognition varied between 40 and 90 percent. The recognition rates with the flowchart were not significantly higher. Inter-observer reliability did not increase on a significant level.
Conclusion:
Correct recognition of total elbow arthroplasty models with plain radiographs remains imperfect with our developed flowchart. The flowchart increased correct recognition rates and inter-observer reliability.
Key Words: Arthroplasty, Decision Trees, Elbow, Observer variation, Radiography, Recognition (Psychology), Replacement
Introduction
Recognition of total elbow arthroplasties (TEAs) on plain radiographs is difficult due to a multitude of different types and models. Especially if surgery reports and documentation are not available, lost or when the primary surgery was performed in another hospital prosthesis type may be undeterminable. Since the 1970s many different models and brands of TEAs have been used (1,2). Commonly the hinge mechanism is used to classify TEAs in two basic design forms: linked and unlinked prostheses. Besides linkage type, fixation methods in the bone differ as well. The prosthesis can be fixated by screws, cement or with an osseo-integrative coating (2).
The differences in the hinge design and linkage type are important for pre-operative planning of revision surgery. Special equipment, such as model-specific screwdrivers for decoupling or broaches for removal of a cement mantle, need more preparation and scheduled time for revision surgery.
We assumed that recognition might be aided by a flowchart that uses the main distinguishing characteristics of each prosthesis. In literature we identified one study that describes model-specific characteristics of total elbow arthroplasties (3). In other studies, total elbow arthroplasties are only described by their function of replacing the elbow joint (4–7). This information only helps the surgeon by giving an overview of arthroplasty models.
This study compares accuracy and inter-observer agreement of orthopedic surgeons specialized in upper limb arthroplasty to recognize prosthesis models with and without a flowchart. Our primary hypothesis is that there is no difference in recognition of arthroplasty models with and without a flowchart. Our secondary hypothesis is that the flowchart makes no difference in inter-observer reliability.
Materials and Methods
Study Design and Setting
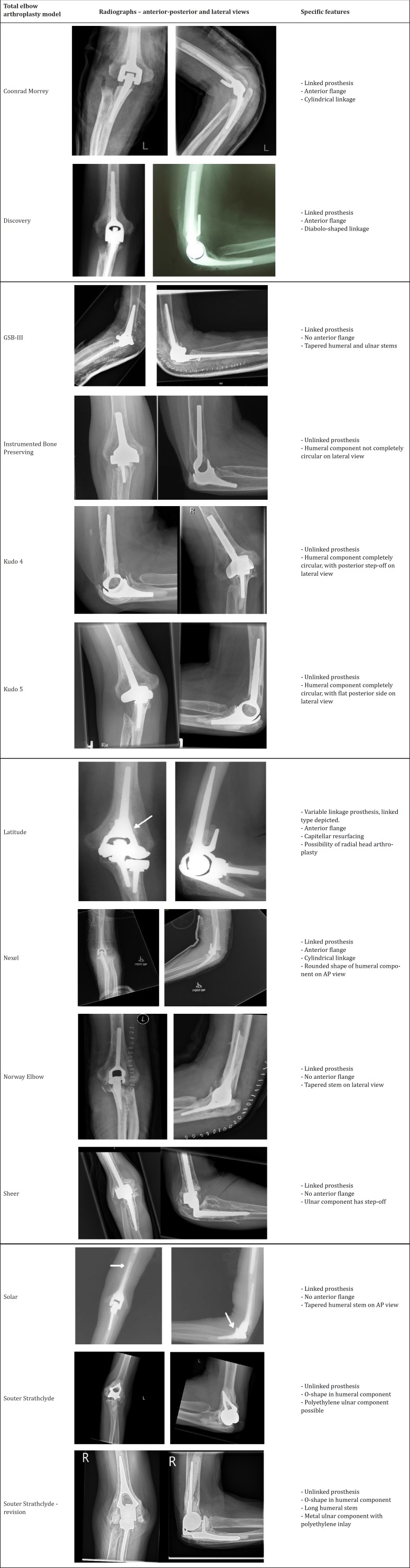
An online questionnaire on the Shoulder and Elbow Platform was developed at the Amphia Hospital, Breda, the Netherlands. Plain radiographs of thirteen TEA models were shown [Figure 1]. The questionnaire consisted of anterior-posterior and lateral radiographs of each model. The participants had to choose from a list of all included models. After choosing a model name from the list and confirmation of the choice, no feedback was provided and the next model was shown.
Figure 1.
The radiographs used in the questionnaire with their specific design features
Participants
Sixty-five independent orthopedic surgeons were invited from different countries who had participated before on the Shoulder and Elbow Platform and who are specialized in upper limb surgery. On behalf of the senior authors, the Platform website sent an e-mail providing an internet link to the questionnaire. A reminder e-mail was sent to initial non-responders.
Study description
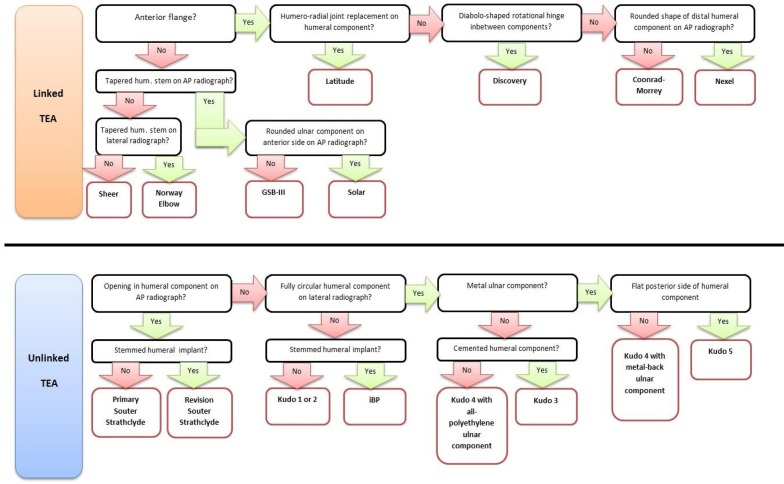
We developed a flowchart focused on distinctive features of each design [Figure 2]. The first session was performed without this flowchart. The same set of radiographs was presented in the same order. After the first session, a link to the flowchart appeared highlighted in the announcement of the second session. Then the same set of total elbow arthroplasty models was presented in a different order than before. A new link to the flowchart accompanied every new question in case of closure of the flowchart.
Figure 2.
Flowchart to aid in recognition of total elbow arthroplasties, describing distinguishing features. By answering the questions the correct model is found
Statistical analysis
Inter-observer reliability of the use of the flowchart was tested with Fleiss’ kappa test for multiple observers. Frequently used interpretations of kappa values are used (8). Percentages of correct recognition per arthroplasty model and per surgeon were calculated for both sessions by dividing the number of correct answers by all possible answers. Significance was set at a p-value of less than 0.05. Differences were analyzed with McNemar’s test for paired dichotomous data. The outcomes were scored by recognition of coupling mechanism (linked and unlinked) and by model type if applicable, as for instance the Kudo prosthesis has been produced in several versions.
Results
Ten orthopedic surgeons specialized in upper extremity surgery completed the study. Seven worked in the Netherlands, two in Belgium and one in France. Percentages of correctly recognized total elbow arthroplasty models, including p-values of statistical difference for the use of the flowchart [Table 1].
Table 1.
Recognition rates per total elbow arthroplasty model with and without the flowchart. The p-values are shown in the right column
| Total elbow arthroplasty model |
Correct – no flowchart
(%) |
Correct – with flowchart
(%) |
Difference
(%) |
Significance
( p -value ) |
|---|---|---|---|---|
| Coonrad Morrey | 100 | 80 | -20 | 0.50 |
| Discovery | 50 | 90 | +40 | 0.38 |
| GSB-III | 30 | 40 | +10 | 1.00 |
| Instrumented Bone Preserving | 60 | 80 | +20 | 0.50 |
| Kudo 4 | 20 | 40 | +20 | 0.63 |
| Kudo 5 | 40 | 40 | = | 1.00 |
| Latitude | 90 | 90 | = | 1.00 |
| Nexel | 30 | 50 | +20 | 0.63 |
| Norway Elbow | 50 | 70 | +20 | 0.63 |
| Sheer | 30 | 40 | +10 | 1.00 |
| Solar | 30 | 60 | +30 | 0.38 |
| Souter Strathclyde | 80 | 90 | +10 | 1.00 |
| Souter Strathclyde - revision | 80 | 90 | +10 | 1.00 |
Recognition of the Coonrad Morrey prosthesis scored a lower value with the use of the flowchart, compared to all other models who demonstrated an equal or higher recognition rate. However, any model had a significant change in recognition.
Seven out of ten surgeons performed better with the flowchart, two performed the same and one performed worse. Accuracy per surgeon is shown, as well as significance [Table 2]. Surgeon no. 5 performed significantly better with the flowchart than without.
Table 2.
Overall recognition rates per surgeon, for with and without the flowchart. The p-values are shown in the right column
| Orthopedic surgeon |
Correct – no flowchart
(n) |
Correct – with flowchart
(n) |
Difference (%) |
Significance
( p -value ) |
|---|---|---|---|---|
| 1 | 11 | 11 | = | 1.00 |
| 2 | 4 | 7 | +30 | 0.25 |
| 3 | 7 | 12 | +50 | 0.06 |
| 4 | 2 | 6 | +40 | 1.00 |
| 5 | 5 | 12 | +70 | 0.02 |
| 6 | 11 | 12 | +10 | 1.00 |
| 7 | 9 | 9 | = | 1.00 |
| 8 | 4 | 7 | +30 | 0.25 |
| 9 | 4 | 5 | +10 | 1.00 |
| 10 | 9 | 6 | -30 | 0.45 |
Inter-observer reliability increased in twelve of thirteen arthroplasty models. As demonstrated, five of thirteen models demonstrated substantial to almost perfect inter-observer reliability with use of the flowchart compared to two of thirteen without the flowchart [Table 3].
Table 3.
Inter-observer agreement per total elbow arthroplasty model. Shown values are Fleiss’ kappa values (κ-values). Interpretation of κ values: <0, less than chance. 0-0.20, slight. 0.21-0.40, fair. 0.41-0.60, moderate. 0.61-0.80, substantial. 0.81-0.99, almost perfect. 1, perfect
| Total elbow arthroplasty model | Inter-observer agreement – no flowchart | Inter-observer agreement – with flowchart |
|---|---|---|
| Coonrad Morrey | 0.62 | 0.67 |
| Discovery | 0.33 | 0.65 |
| GSB-III | 0.00 | 0.09 |
| Instrumented Bone Preserving | 0.31 | 0.53 |
| Kudo 4 | 0.04 | 0.30 |
| Kudo 5 | 0.18 | 0.17 |
| Latitude | 0.70 | 0.78 |
| Nexel | 0.07 | 0.23 |
| Norway Elbow | 0.14 | 0.35 |
| Sheer | 0.07 | 0.24 |
| Solar | 0.09 | 0.25 |
| Souter Strathclyde | 0.59 | 0.88 |
| Souter Strathclyde - revision | 0.40 | 0.78 |
Analysis of incorrect answers revealed six percent (8/130) of possible choices in the wrong category of linkage model without the flowchart. With flowchart, this percentage decreased to three percent (4/130). The correct possible choices of any Kudo prosthesis (Kudo 4 of Kudo 5) increased from 65 percent to 85 percent using the flowchart. Souter Strathclyde prosthesis (Souter Strathclyde primary or revision prosthesis) recognition increased from 85 percent to 95 percent.
Discussion
Using the flowchart correct model recognition improved in seven of ten orthopedic surgeons, however significant for one surgeon. We found no significant difference in correct recognition per arthroplasty model with and without the flowchart, and therefore we have to accept our primary hypothesis.
As a secondary hypothesis, we tested the inter-observer reliability. Inter-observer reliability increased for all TEA models using the flowchart. However, the increase was not significant, whereby the secondary hypothesis has to be accepted. Nevertheless, recognition of linkage type appears acceptable on plain radiographs.
Since different total elbow arthroplasties have been used, correct model recognition is important to plan revision surgery and to anticipate on model-specific pitfalls or implant linkage instruments. Correct recognition of model type is therefore paramount. This is the first study to determine reliability of recognition of total elbow arthroplasty models on plain radiographs. In literature, only one article emphasizes on distinguishing characteristics of different models of total elbow arthroplasty (3). Therefore, unfortunately, no comparisons can be made to other studies.
With the multidtude of models, recognition is more difficult and could be misinterpreted between clinicians, just as eponyms, who have a very low inter-observer agreement (9).
For clinical practice, a flowchart offers a simple tool for aid in recognition. The contemporary practice at our institution is consulting a colleague, which requires face-to-face or telephone contact, exchange of patient identification numbers and viewing the radiographs. This process might be time consuming. On the contrary, a flowchart is always available and repeatable and a colleague can still be consulted as well.
This study should be interpreted in light of its limitations. Firstly, a relative small group of observers completed the study. The number of orthopedic surgeons specialized in elbow arthroplasty is relatively low compared to, for example, hip and knee surgeons. This together with non-responders lead to a fairly small number of observers. Secondly, we did not perform intra-observer reliability since inter-observer agreement is clinically more relevant as the surgery requirements are ordered once per surgery.
On plain radiographs three-dimensional structures can be depicted inaccurately because of angulation and relative magnification of the radiation beam. Flexion contractures of the elbow can distort the two-dimensional view of the radiographs. A computerized three-dimensional shape-recognition programme might aid in distorted images. Correct recognition of orthopedic implants remains a challenge, as assessors have to be aware of the appearance of contemporary and historic implant models (5).
Correct recognition of total elbow arthroplasty models with plain radiographs remains imperfect with our developed flowchart. In general, however not significant, the flowchart increased correct recognition rates and inter-observer reliability. Therefore, we do encourage use of the flowchart to aid in determining unknown total elbow arthroplasty models.
Acknowledgements
We would like to thank the Shoulder and Elbow Platform surgeons who participated in this study: A. L. Boerboom, A. van Tongel, C.J.A. van Bergen, J. Cheung, M. van der Pluijm, P. Mansat, M.L. Wagener, I. Degreef, D. van Deurzen, C.L.E. Gerritsma.
Disclosures:
None, for all authors. See disclosure forms.
Conflict of Interest:
All authors declare that they have no conflict of interest.
References
- 1.Fajardo M, Kwon YW. The rise of the metal elbow. Bull Hosp Joint Dis. 2013;71(1):24–31. [PubMed] [Google Scholar]
- 2.Prkić A, van Bergen CJ, The B, Eygendaal D. Total elbow arthroplasty is moving forward: Review on past, present and future. World J Orthop. 2016;7(1):44–9. doi: 10.5312/wjo.v7.i1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oflazoglu K, Koenrades N, Somford MP, van den Bekerom MPJ. Recognizing the elbow prosthesis on conventional radiographs. Strategies Trauma Limb Reconstr. 2016;11(3):161–8. doi: 10.1007/s11751-016-0263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taljanovic MS, Hunter TB, Miller MD, Sheppard JE. Gallery of medical devices: part 1: orthopedic devices for the extremities and pelvis. Radiographics. 2005;25(3):859–70. doi: 10.1148/rg.253055010. [DOI] [PubMed] [Google Scholar]
- 5.Taljanovic MS, Jones MD, Hunter TB, Benjamin JB, Ruth JT, Brown AW, et al. Joint arthroplasties and prostheses. Radiographics. 2003;23(5):1295–314. doi: 10.1148/rg.235035059. [DOI] [PubMed] [Google Scholar]
- 6.White E, Lu D, Eyer B, Gottsegen C, Ahlmann E, Allison C. Gallery of uncommon orthopedic implants: a guide for emergency radiologist. Emerg Radiol. 2010;17(3):227–47. doi: 10.1007/s10140-009-0834-6. [DOI] [PubMed] [Google Scholar]
- 7.Hunter TB, Lund P. Gallery of medical devices. Curr Probl Diagn Radiol. 2005;26(3):109–52. doi: 10.1016/s0363-0188(97)90008-6. [DOI] [PubMed] [Google Scholar]
- 8.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. [PubMed] [Google Scholar]
- 9.Viveen J, Somford MP, Koenraadt KL, van den Bekerom MP, Eygendaal D, Schipper IB, et al. The use of eponyms for surgical approaches and fractures in elbow surgery: accuracy and reliability pre-and post-training. Arch Bone Jt Surg. 2019;7(2):191. [PMC free article] [PubMed] [Google Scholar]