Abstract
Sarecycline is a novel, narrow-spectrum, once-daily tetracycline-derived oral antibiotic that is FDA-approved in the US to be taken with or without food for moderate-to-severe acne vulgaris for ages 9 years of age and older. Sarecycline possesses anti-inflammatory properties and potent activity against Gram-positive bacteria, including activity against multiple strains of Cutibacterium acnes, while exhibiting minimal activity against enteric aerobic Gram-negative bacteria. Unlike many acne studies, sarecycline was investigated for chest and back acne. Significant reduction in inflammatory lesions was seen at week 12 at 1.5 mg/kg/day of sarecycline, with statistically significant improvement seen as early as week 3. No reports of phototoxicity, dizziness, pseudotumor cerebri or lupus but 1.2% nausea and 1.2% vaginal candidiasis was reported in the pivotal Phase III studies.
Keywords: : acne, antibiotics, microbiota, narrow spectrum, sarecycline, tetracycline
Acne vulgaris affects 80% of teenagers. By 40 years of age, 54% of adult women and 40% of adult men will still suffer from acne vulgaris [1–3]. In the evolving view of acne pathogenesis, inflammation has emerged as a key driving factor for the entire acne pathway, from microcomedones to comedones, papules, cysts and to acne scars. Acne vulgaris involves multiple inflammatory pathways, including upregulation of toll-like receptor 2 and 4, downstream upregulation of matrix metalloproteinases, breakdown of collagen, increased pro-collagen and increased T-helper cells [4]. Cutibacterium acnes itself has been shown to activate innate immune and inflammatory events in epidermal keratinocytes through TOLR, and to induce IL-1 β secretion via the NLRP3 inflammasome in human monocytes [5,6].
Oral antibiotics have been widely used in dermatology, especially in patients experiencing inflammatory lesions in moderate-to-severe acne vulgaris [4]. Antibiotic treatment has been shown to inhibit the host's inflammatory response to C. acnes while also reducing the number of bacteria within the pilosebaceous unit [7]. Oral antibiotics used for treatment of moderate-to-severe acne vulgaris include doxycycline, minocycline, tetracycline, erythromycin, azithromycin, amoxicillin, cephalexin and, trimethoprim-sulfamethoxazole [8]. Such antibiotics from the tetracycline family as doxycycline and minocycline are often used for acne treatment, but have been associated with side effects and gradually increased bacterial resistance [9,10]. In fact, the disruption of gastrointestinal tract microbiota with use of doxycycline and minocycline may contribute to the increased incidence of gastrointestinal side effects, diarrhea, intestinal and vaginal fungal overgrowth, and vaginal candidiasis, particularly in patients receiving prolonged oral antibiotic therapy [11–14]. It is also noted that multidrug-resistant Gram-negative infections are increasingly prevalent and a source of major morbidity and mortality [15].
Chemistry & clinical pharmacology
Sarecycline is in the tetracycline family, all of which are named for their four (‘tetra-’) hydrocarbon rings (‘-cycl-’) derivation (‘-ine’), to which a variety of functional groups are attached [16]. These functional chloride, methyl and hydroxyl groups may contribute to its antibacterial activity and pharmacological properties. Doxycycline was FDA approved in the US in 1967 as a broad-spectrum antibiotic, while minocycline was FDA approved in 1971 with a variety of indications. Sarecycline is an oral aminomethylcycline with a stable modification at C7-0 [16] that was FDA approved in 2018 specifically for acne.
Tetracyclines bind the 30s subunit of bacterial ribosome, thus inhibiting protein synthesis of bacteria but do not affect human cells. Due to their improved bioavailability and lipophilicity, doxycycline and minocycline have been more widely used than tetracycline for acne treatment. Tetracyclines also have anti-inflammatory effects [10]. Even at subantimicrobial doses, tetracyclines reduce inflammation via anti-collagenolytic, antimatrix-degrading metalloproteinase, and cytokine down-regulating properties [5,17–19]
With the surge of tetracycline-resistant organisms [8], concerns about overuse of antibiotics in the tetracycline family, especially with negative impact on the gut microbiota, have surfaced. Zhanel et al. describes the microbiological profile of sarecycline against clinical isolates of C. acnes compared with doxycycline, tetracycline and minocycline [20]. Sarecycline demonstrated comparable efficacy against C. acnes as well as macrolide resistant organisms, methicillin-susceptible and resistant isolates as well as Staphylococcus epidermidis. However, sarecycline was found to have four- to eight-fold less activity against bacteria that are part of the normal human microbiota. These Gram-positive anerobic bacteria included isolates of Bifidobacterium bifidum, Brevibacillus brevi, Bifidobacterium infantis, Bifidobacterium longum, Clostridium perfringens, Clostridium difficile, Lactobacillus acidophilus, Lactobacillus casei, Lactobacillus plantarum, Peptostreptococcus anaerobius, Peptostreptococcus micros, C. acnes, Streptococcus constellatus and Streptococcus intermedius. Against Gram-negative anaerobes that are part of the normal human microbiota, sarecycline was again the least active of agents against Enterobacteriaceae, Enterococcus faceium and Klebsiella pneumonia, with minimum inhibitory concentration of 32, 32 and >64 μg, respectively. The study supports narrow spectrum antibacterial activity of sarecycline [20].
Because they bind with food and also easily with magnesium, aluminum, iron and calcium, which reduces their ability to be completely absorbed by the body, short-acting tetracyclines need to be taken with a full glass of water, either 2 h after eating or 2 h before eating and not temporally when taking dairy products, antacids and preparations containing iron. Because of Phase I study results, sarecycline is FDA-approved to be taken once daily with or without food at 1.5 mg/kg/day and comes in three dosages – 60, 100 and 150 mg.
Tetracycline, doxycycline and minocycline cross the blood–brain barrier, which may explain the potential side effects of pseudotumor cerebri, headaches and dizziness. Sarecycline is less likely to cross the blood–brain barrier [21,22].
Clinical studies
14 Phase I pharmacokinetics and safety studies were performed on 378 patients with moderate-to-severe acne vulgaris exposed to sarecycline, with and without food (tablets and capsules). Because no difference in bioavailability was observed when taken with food, sarecycline has FDA approval to be taken with or without food, without any warnings to avoid food, iron, antacids or calcium supplements, unlike other antibiotics in the tetracycline family. Similarly, no phototoxicity was observed with sarecycline in Phase I studies [23].
In a Phase II multicenter, double-blind, placebo-controlled, dose-response study (PR-10411) over 12 weeks, Leyden et al. enrolled 285 subjects ranging from ages 12 to 45 years with moderate-to-severe acne vulgaris [24]. Patients were then randomized to once daily sarecycline at 0.75, 1.5, 3.0 mg/kg or placebo (1:1:1:1 ratio) treatment for 12 weeks. Inflammatory and noninflammatory lesion counts were performed at baseline, and again at weeks 1, 2, 4, 8 and 12. Safety monitoring included serum laboratory monitoring, vital signs, electrocardiograms and physical examinations. After 12 weeks of treatment, it was noted that sarecycline at doses of 1.5 and 3.0 mg/kg demonstrated significantly reduced inflammatory lesions from baseline (52.7 and 51.8%, respectively) versus the placebo group (38.3%; p = 0.02 and p = 0.03, respectively), revealing antimicrobial as well as anti-inflammatory effects of sarecycline (data on file, Allergan plc, Dublin, Ireland). However, sarecycline 3.0 mg/kg did not result in increased efficacy compared with the 1.5 mg/kg dosage. Overall, sarecycline was well tolerated across all treatment groups. Gastrointestinal adverse effects rate in the sarecycline groups were similar to placebo with nausea being the most common treatment-related adverse effects. Vertigo, dizziness and photosensitivity was noted, but only occurred in less than 1% of patients in the sarecycline treatment groups. Incidence of adverse events, which includes nausea (4.1% in placebo group and 3.3% in pooled sarecycline group), was similar across all sarecycline groups and the placebo group. Of note, patients reported no adverse events of tinnitus, urticaria, pseudotumor cerebri or vulvovaginal candidiasis [23].
Moore et al. [25] evaluated the efficacy and safety profiles of sarecycline in two identically designed, multicenter, double-blind, Phase III studies, with SC1401 conducted at 56 centers and SC1402 conducted at 54 centers. In these pivotal Phase III studies, 2002 patients between the ages of 9 and 45 years of age with moderate-to-severe-acne vulgaris were enrolled to evaluate the safety and efficacy of once daily sarecycline at 1.5 mg/kg for 12 weeks. Patients were randomized 1:1 to receive sarecycline at 1.5 mg/kg or placebo and assessed at baseline, 3, 6, 9 and 12 weeks. Co-primary endpoints of efficacy included both lesion counts (mean absolute and percentage reduction in facial inflammatory lesions) and Investigator's Global Assessment (IGA) analysis at week 12. IGA success was defined as ≥2-point improvement from the subject's baseline IGA score AND score of 0 (clear) or 1 (almost clear) at week 12. Secondary endpoints of efficacy included mean absolute and percentage reduction of facial inflammatory lesions at week 3, 6, and 9 as well as non-facial IGA (chest, neck and back). Although truncal acne is not typically evaluated as part of an acne pivotal study, chest and back acne were evaluated at baseline, 3, 6, 9 and 12 weeks as part of the pivotal trials 1401 and 1402. Any patient with an IGA of 2 or above for chest or back were included in the assessment. Lesion count reductions were not examined in truncal acne in these trials (study report CSRs for SC1401 and SC1402) [25].
For the washout period, subjects who agreed to participate in the study but who were currently receiving acne therapy with a prohibited medication then entered an appropriate washout period before beginning the screening procedures. Washout periods varied depending on the excluded medications: Any systemic retinoid(s) and/or systemic corticosteroid(s) were prohibited within 12 weeks prior to randomization; any topical retinoid(s), topical anti-inflammatory(ies) or topical corticosteroid(s), systemic antibiotic(s), and/or systemic acne treatment(s) were prohibited within 4 weeks prior to randomization; and any other topical acne treatments and/or medical facial cleanser were prohibited within 1 week prior to randomization.
Key exclusion criteria included:
Pregnancy or lactation or planning pregnancy during the study period;
Initiation of hormonal contraceptive use within 12 weeks prior to randomization or any plan to initiate or switch hormonal contraceptive products during the study period;
Any disorder causing hyperandrogenism including polycystic ovary syndrome, adrenal or ovarian tumors, Cushing's disease, or congenital adrenal hyperplasia;
Any dermatological condition of the face that could interfere with the clinical evaluations;
Any history of any of the following: allergy to tetracycline-class antibiotics or to any ingredient in the study treatment, pseudomembranous colitis or antibiotic-associated colitis;
Any treatment for any type of cancer within the 6 months prior to participation in the study;
Any known resistance to other tetracyclines;
Any significant intercurrent illness (including clinically significant abnormality in clinical laboratory tests, psychiatric disposition or other factors) that, in the opinion of the investigator or medical monitor, precluded participation in the study.
The two pivotal studies showed consistency in age, with mean age of 19.8, 19.7, 19.7 and 20.3, respectively (Table 1). With approximately half adults and half pediatric subjects in SC 1401 and in SC 1402, pediatric subjects were between the ages of 9 and 11 in 1.2, 0.8, 0.8 and 1.4% in the four groups, respectively (Table 1). Both SC1401 and SC1402 had a representative number of skin of color patients, with 78.1% Caucasian, 16.6% African–American, 2.3% Asian, 2.3% ‘mixed race’, and 0.9% ‘other’ enrolled in SC1401. Demographics in SC1402 included 78.4% Caucasian, 12.7% African–American, 4.4% Asian, 2.3% ‘mixed race’, and 1.7% ‘other’ (Table 1). Ethnicity was also consistent, with 29.8 and 25.2% Hispanic in SC1401 and SC1402, respectively (Table 1). Slightly more females than males participated in both SC1401 and SC1402 (Table 1).
Table 1. . Demographics in Phase III studies SC1401 and SC1402.
| Demographics | SC1401 | SC1402 | ||
|---|---|---|---|---|
| Placebo (n = 485) | Sarecycline (n = 483) | Placebo (n = 515) | Sarecycline (n = 519) | |
| Mean age (years): | 19.8 | 19.7 | 19.7 | 20.3 |
| – 9–11 years, n (%) | 6 (1.2) | 4 (0.8) | 4 (0.8) | 7 (1.4) |
| – 12–17 years, n (%) | 235 (48.5) | 241 (49.9) | 256 (49.7) | 227 (43.7) |
| – 18+ years, n (%) | 244 (50.3) | 238 (49.3) | 255 (49.5) | 285 (54.9) |
| Race, n (%): | ||||
| – White | 377 (77.7) | 377 (78.1) | 391 (75.9) | 407 (78.4) |
| – Black or African–American | 79 (16.3) | 80 (16.6) | 76 (14.8) | 66 (12.7) |
| – Asian | 9 (1.9) | 11 (2.3) | 21 (4.1) | 23 (4.4) |
| – Mixed race | 14 (2.9) | 11 (2.3) | 15 (2.9) | 13 (2.3) |
| – Other | 6 (1.2) | 4 (0.9) | 12 (2.3) | 9 (1.7) |
| Ethnicity: Hispanic or Latino, n (%) | 143 (29.5) | 144 (29.8) | 122 (23.7) | 131 (25.2) |
| Gender, female/male (%) | 55.9/44.1 | 55.5/44.5 | 56.7/43.3 | 60.7/39.3 |
Most of the patients (85%) in SC1401 and SC1402 had moderate facial acne, and a good number of severe facial acne subjects (15%) were included (Table 2). The mean number of facial inflammatory lesions was 30 in SC1401 as well as SC1402 (Table 2). Severity of chest IGA >2 and back IGA >2 was measured at baseline, week 6, 9 and 12. Mean IGA for the chest was 1.2 and 1.4 while mean IGA for the back was 1.6 and 1.8 in SC1401 and SC1402, respectively (Table 2). Baseline IGA >2 on the chest was 39%, while baseline IGA >2 on the back was 56% and 63% in SC1401 and SC1402, respectively (Table 2). Safety monitoring included serum laboratory monitoring, vital signs, electrocardiograms and physical examinations, and was performed at each visit. Subjects were permitted to use topical sunscreen daily but this was not provided for the subjects.
Table 2. . Baseline disease characteristics in Phase III Studies SC1401 and SC1402.
| Baseline disease characteristics | Placebo (n = 485) | Sareycycline (n = 483) | Placebo (n = 515) | Sareycycline (n = 519) |
|---|---|---|---|---|
| Mean facial inflammatory lesions (n) | 30.2 | 29.7 | 30.2 | 30.3 |
| Facial IGA, n (%): | ||||
| – 3 (moderate) | 410 (84.5) | 413 (85.5) | 439 (85.2) | 440 (84.8) |
| – 4 (severe) | 75 (15.5) | 70 (14.5) | 76 (14.8) | 79 (15.2) |
| Mean IGA for chest | 1.2 | 1.2 | 1.4 | 1.4 |
| Mean IGA for back | 1.6 | 1.6 | 1.8 | 1.8 |
| Baseline IGA ≥2 chest, n (%) | 188 (39) | 190 (39) | 246 (48) | 247 (48) |
| Baseline IGA ≥2 back, n (%) | 261 (54) | 271 (56) | 317 (62) | 325 (63) |
IGA: Investigator's global assessment.
Efficacy & safety profiles
To be considered an IGA success per FDA guidelines, subjects needed to have improved to a rating score of clear (IGA = 0) or almost clear (IGA = 1) and have achieved a 2-point improvement in IGA. In Phase III studies, IGA success rate was significantly greater in the sarecycline group in comparison with placebo group at week 6 in study SC1402 and week 9 in study SC1402. At week 12 in the SC1401 study, 21.9% of the sarecycline group versus 10.5% of the placebo group achieved IGA success (p < 0.0001; Figure 1). Study SC1402 showed 22.6% of the sarecycline group versus 15.3% of placebo group (p = 0.0038) achieved IGA success (Figure 1).
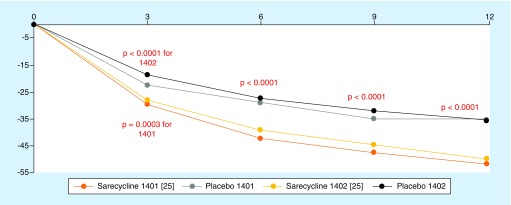
Figure 1. . Reduction of inflammatory lesions with early onset of action in Phase III trials.
The mean percent reduction in facial inflammatory lesion count from baseline was statistically significant between sarecycline and placebo, respectively, at all time points, at week 3 (-29.6 vs -22.4%; p = 0.0003), week 6 (-42.2 vs -28.9%; p < 0.0001), week 9 (-47.4 vs -34.9%; p < 0.0001) and week 12 (-51.8 vs -35.1%; p < 0.0001) for SC1401 (Figure 1). Similarly, the mean percent reduction in facial inflammatory lesion count from baseline was statistically significant between sarecycline and placebo, respectively, at all time points, at week 3 (-28 vs -18.6%; p < 0.0001), week 6 (-39.1 vs -27.3%; p < 0.0001), week 9 (-44.5 vs -31.9%; p < 0.0001) and week 12 (-49.9 vs -35.4%; p < 0.0001) for SC1402 (Figure 1). In a post-hoc analysis, the onset of efficacy for absolute reduction of noninflammatory lesion count occurred at week 6 in SC1401 (p ≤ 0.0371) and week 9 in SC1402 (p ≤ 0.0095) [23,25, Almirall Llc E, 2016, unpublished data].
The same IGA scale was used for the chest and back assessments as for facial acne. For the chest and back acne, statistically significant improvements in IGA score deemed to be clear (0) or almost clear (1) on a IGA assessment week 12, with >2-point improvement from baseline score, was seen at week 12 in the chest in SC1401 (-29.5 vs -19.6%; p < 0.05) and SC1402 (-36.6 vs -21.6%; p < 0.001) and in the back in SC1401 (-32.9 vs -17.1%; p < 0.001) and SC1402 (-33.2 vs -25.7%; p < 0.05).
The most common adverse events noted were nausea (4.6% sarecycline vs 2.5% placebo), nasopharyngitis (3.1 and 1.7%), headache (2.7% in both sarecycline and placebo groups) and vomiting (2.1 and 1.4%) in SC1401 and SC1402 (Table 3).
Table 3. . Pooled treatment-emergent adverse events in Phase III sarecycline studies.
| TEAE safety population (≥2% in either group) | SC1401 and SC1402 pooled, n (%) | |
|---|---|---|
| Sarecycline (n = 994) | Placebo (n = 996) | |
| Nasopharyngitis | 28 (2.8) | 23 (2.3) |
| Upper respiratory infection | 16 (1.6) | 16 (1.6) |
| Headache | 28 (2.8) | 38 (3.8) |
| Nausea | 32 (3.2) | 17 (1.7) |
| Vomiting | 13 (1.3) | 9 (0.9) |
| Urinary tract infection | 3 (0.3) | 11 (1.1) |
TEAE: Treatment-emergent adverse events.
Data taken from [25].
Because of the known adverse events associated with antibiotics in the tetracycline family of antibiotics, selected TEAEs were of special interest. These included sunburn, urticarial, vulvovaginal mycotic infections or candidiasis, nausea, vomiting, diarrhea, esophagitis, dizziness, tinnitus, vertigo and pseudotumor cerebri (Table 4). A slight increase was noted in vulvovaginal candidiasis and vulvovaginal mycotic infections in the sarecycline group versus placebo subjects (1.1% and 0.7% in SC1401 and 0.3% and 1.0% in group SC1402; Table 4). Similarly, an increase was noted in nausea in subjects in the sarecycline versus placebo groups, respectively, in SC1401 (4.6% vs 2.5%) and SC1402 (1.9% vs 1.0%; Table 4). A few cases of sunburn were noted in the sarecycline subjects versus placebo subjects (0.6% and 0.4% in SC1401 and 0.2% and 0.2% in SC1402; Table 4) and 1 case of photosensitivity was noted in the sarecycline group in SC1402. No increase in TEAEs were noted with sarecycline in vomiting, diarrhea, esophagitis, dizziness, tinnitus, vertigo and pseudotumor cerebri.
Table 4. . Treatment-emergent adverse events of special interest for tetracyclines in Phase III sarecycline studies.
| Selected TEAE (safety population) | SC1401, n (%) | SC1402, n (%) | ||
|---|---|---|---|---|
| Placebo (n = 483) | Sarecycline (n = 481) | Placebo (n = 513) | Sarecycline (n = 513) | |
| Sunburn | 2 (0.4) | 3 (0.6) | 1(0.2) | 1 (0.2) |
| Urticaria | 1 (0.2) | 0 | 2 (0.4) | 1 (0.2) |
| Vulvovaginal mycotic infection | 0 | 2 (0.7) | 0 | 3 (1.0) |
| Vulvovaginal candidiasis | 0 | 3 (1.1) | 0 | 1 (0.3) |
| Nausea | 12 (2.5) | 22 (4.6) | 5 (1.0) | 10 (1.9) |
| Dizziness | 7 (1.4) | 3 (0.6) | 4 (0.8) | 2 (0.4) |
| Vomiting | 7 (1.4) | 10 (2.1) | 2 (0.4) | 3 (0.6) |
| Diarrhea | 8 (1.7) | 5 (1.0) | 6 (1.2) | 6 (1.2) |
| Esophagitis | 0 | 0 | 0 | 0 |
| Tinnitus | 0 | 0 | 0 | 0 |
| Vertigo | 0 | 0 | 0 | 0 |
| Pseudotumor cerebri | 0 | 0 | 0 | 0 |
Future perspective
As American Academy of Dermatology desires for physicians to be mindful of choosing antibiotics for patients, physicians need to be aware of the negative implications for bacterial resistance as well as effects of medication side effects including effects on human microbiota [20]. Doxycycline and minocycline exhibit a broader antibacterial activity spectrum, which may result in overgrowth of tetracycline-resistant organisms such as Candida albicans [26–28]. The broad antibacterial spectrum can also negatively impact the human intestinal microbiota with potential impact on health [29–31]. Therefore, strategies to minimize negative effects of antibiotic usage are necessary. Sarecycline's narrow antibacterial spectrum may possibly result in reduced dysbiosis of gut and vaginal flora, which can reduce adverse effects such as diarrhea or vulvovaginal candidiasis. Moreover, sarecycline has shown low potential for inducing bacterial resistance [20].
Side-effect profiles need to be carefully considered when choosing an antibiotic for patients. Older tetracycline-class antibiotics were linked to staining of permanent teeth in children under the age of 8 years, which was first described in 1959 [32]. Previous studies showed variability in teeth staining from 23 to 92% in children who received a tetracycline during odontogenesis [32–37]. Therefore, FDA contraindicated use of tetracyclines in children due to concern for dental staining [37]. However, newer class tetracyclines, such as doxycycline, have lower calcium-binding capacity in comparison with older tetracyclines [37]. Multiple studies have been published showing that use of doxycycline before 8 years of age show no sign of permanent teeth staining [37–39]. The period of odontogenosis ends at 8 years of age, and no evidence of teeth staining was found in the clinical trials with sarecycline in subjects as young as 9 years of age; therefore, sarecycline has received approval for acne in patients 9 years of age and older [23,39]. Sarecycline is a viable treatment modality for younger children, especially since acne is presenting at earlier years of age, even in prepubertal children [1,40,41].
Sarecycline has significant effects on inflammatory lesions, but it was also noted to show statistically significant effect on noninflammatory acneiform lesions at certain time points [25]. Further investigation needs to be done on the exact effect of sarecycline on noninflammatory lesions. However, a possible theory is that during early stages of comedone development, sarecycline possibly has an anti-inflammatory effects on early inflammatory pathways [6,42].
Sarecycline has potent Gram-positive activity while exhibiting minimal activity against enteric aerobic Gram-negative bacteria, also demonstrating efficacy in tissue-based models of infection and effective anti-inflammatory activity, which supports its use as a novel treatment for acne that is FDA approved for acne at 1.5 mg/kg/day orally in patients aged 9 and older as a once daily antibiotic with statistically significant improvement seen as early as week 3.
Executive summary.
Sarecycline is a novel, narrow-spectrum, once-daily tetracycline-derived oral antibiotic that is FDA-approved in the US in 2018 for moderate-to-severe acne vulgaris for ages 9 years of age and older.
It can be taken with or without food.
Increased patient compliance with once daily weight-based dosing.
Decrease in inflammatory lesion count as early as week 3.
Decrease in chest and back acne by week 12.
Possesses anti-inflammatory properties and potent activity against Gram-positive bacteria.
Well tolerated with a favorable safety profile. No reports of phototoxicity, dizziness, pseudotumor cerebri or lupus but 1.2% nausea and 1.2% vaginal candidiasis in pivotal Phase III studies.
Acknowledgments
Authors thank Dr Ayman Grada and Dr Emilio Fumero for their feedback and to Almirall for providing access to the microbiological profile data on sarecycline as well as Clinical Study Reports from the clinical trials on sarecycline.
Footnotes
Financial & competing interests disclosure
AY Moore has received funds as advisory board member (A), consultant (C), clinical study investigator (I), coordinating investigator (CI) and speaker (SP) for AbbVie (I, SP), Aclaris (I, SP), Allergan (C, I, CI, SP), Almirall (SP), Astellas (I), Biofrontera (C,I), Boehringer Ingelheim (I), Bristol-Myers Squibb (C,I), Cutanea (I), Dermavant (I), Dermira (I), Eli Lilly (I), Foamix (I), Galderma (I), Incyte (I), Janssen (A,I), Leo (A, SP), Mayne Pharma (C, I), Naked Biome (I), Novartis (I), Parexel (I), Pfizer (I,SP), Verrica (I). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Open access
This work is licensed under the Attribution-NonCommercial-NoDerivatives 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
References
Papers of special note have been highlighted as: •• of considerable interest
- 1.Bhate K, Williams HC. Epidemiology of acne vulgaris. Br. J. Dermatol. 168(3), 474–485 (2013). [DOI] [PubMed] [Google Scholar]
- 2.Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J. Am. Acad. Dermatol. 41(4), 577–580 (1999). [PubMed] [Google Scholar]
- 3.Ramos-E-Silva M, Carneiro SC. Acne vulgaris: review and guidelines. Dermatol. Nurs. 21(2), 63–68 (2009). [PubMed] [Google Scholar]
- 4.Holland DB, Jeremy AH, Roberts SG, Seukeran DC, Layton AM, Cunliffe WJ. Inflammation in acne scarring: a comparison of the responses in lesions from patients prone and not prone to scar. Br. J. Dermatol. 150(1), 72–81 (2004). [DOI] [PubMed] [Google Scholar]
- 5.Jeremy AH, Holland DB, Roberts SG, Thomson KF, Cunliffe WJ. Inflammatory events are involved in acne lesion initiation. J. Invest. Dermatol. 121(1), 20–27 (2003). [DOI] [PubMed] [Google Scholar]
- 6.Brown SK, Shalita AR. Acne vulgaris. Lancet 351(9119), 1871–1876 (1998). [DOI] [PubMed] [Google Scholar]
- 7.Patel M, Bowe WP, Heughebaert C, Shalita AR. The development of antimicrobial resistance due to the antibiotic treatment of acne vulgaris: a review. J. Drugs Dermatol. 9(6), 655–664 (2010). [PubMed] [Google Scholar]
- 8.Tan H-H. Antibacterial therapy for acne. Am. J. Clin. Dermatol. 4(5), 307–314 (2003). [DOI] [PubMed] [Google Scholar]
- 9.Kircik LH. Doxycycline and minocycline for the management of acne: a review of efficacy and safety with emphasis on clinical implications. J. Drugs Dermatol. 9(11), 1407–1411 (2010). [PubMed] [Google Scholar]
- 10.Farrah G, Tan E. The use of oral antibiotics in treating acne vulgaris: a new approach. Dermatol. Ther. 29(5), 377–384 (2016). [DOI] [PubMed] [Google Scholar]
- 11.Del Rosso JQ, Webster GF, Rosen T. et al. Status Report from the Scientific Panel on Antibiotic Use in Dermatology of the American Acne and Rosacea Society: part 1: antibiotic prescribing patterns, sources of antibiotic exposure, antibiotic consumption and emergence of antibiotic resistance, impact of alterations in antibiotic prescribing, and clinical sequelae of antibiotic use. J. Clin. Aestheti. Dermatol. 9(4), 18 (2016). [PMC free article] [PubMed] [Google Scholar]
- 12.Simonart T, Dramaix M, De Maertelaer V. Efficacy of tetracyclines in the treatment of acne vulgaris: a review. Br. J. Dermatol. 158(2), 208–216 (2008). [DOI] [PubMed] [Google Scholar]
- 13.Bartlett JG, Bustetter LA, Gorbach SL, Onderdonk AB. Comparative effect of tetracycline and doxycycline on the occurrence of resistant Escherichia coli in the fecal flora. Antimicrob. Agents Chemother. 7(1), 55–57 (1975). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hinton NA. The effect of oral tetracycline HCl and doxycycline on the intestinal flora. Curr. Ther. Res. Clin. Exp. 12(6), 341–352 (1970). [PubMed] [Google Scholar]
- 15.Kaye KS, Pogue JM. Infections caused by resistant Gram-negative bacteria: epidemiology and management. Pharmacotherapy 35(10), 949–962 (2015). [DOI] [PubMed] [Google Scholar]
- 16.Chopra I, Roberts M. Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol. Mol. Biol. Rev. 65(2), 232–260 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinberg JM. The anti-inflammatory effects of tetracyclines. Cutis 75(Suppl. 4), 6–11 (2005). [PubMed] [Google Scholar]
- 18.Tilakaratne A, Soory M. Anti-inflammatory actions of adjunctive tetracyclines and other agents in periodontitis and associated comorbidities. Open Dent. J. 8, 109 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webster G, Del Rosso JQ. Anti-inflammatory activity of tetracyclines. Dermatol. Clin. 25(2), 133–135 (2007). [DOI] [PubMed] [Google Scholar]
- 20.Zhanel G, Critchley I, Lin L-Y, Alvandi N. Microbiological profile of sarecycline, a novel targeted spectrum tetracycline for the treatment of acne vulgaris. Antimicrob. Agents Chemother. 63(1), e01297–e01218 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barza M, Brown RB, Shanks C, Gamble C, Weinstein L. Relation between lipophilicity and pharmacological behavior of minocycline, doxycycline, tetracycline, and oxytetracycline in dogs. Antimicrob. Agents Chemother. 8(6), 713–720 (1975). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• These are the Phase I results.
- 22.US Securities and Exchange Commission. Paratek prospectus supplement (2015). www.sec.gov/Archives/edgar/data/1178711/000156459016014314/prtk-10k_20151231.htm
- 23.US FDA, Center for Drug Evaluation and Research. Multi Discipline Review (2018). www.accessdata.fda.gov/drugsatfda_docs/nda/2018/209521Orig1s000TOC.cfm
- 24.Leyden JJ, Sniukiene V, Berk DR, Kaoukhov A. Efficacy and safety of sarecycline, a novel, once-daily, narrow spectrum antibiotic for the treatment of moderate to severe facial acne vulgaris: results of a Phase II, dose-ranging study. J. Drugs Dermatol. 17(3), 333–338 (2018). [PubMed] [Google Scholar]; •• Shows the Phase II results.
- 25.Moore A, Green LJ, Bruce S. et al. Once-daily oral sarecycline 1.5 mg/kg/day is effective for moderate to severe acne vulgaris: results from two identically designed, Phase III, randomized, double-blind clinical trials. J. Drugs Dermatol. 17(9), 987–996 (2018). [PubMed] [Google Scholar]; •• Shows the Phase III results.
- 26.Lewis JD, Chen EZ, Baldassano RN. et al. Inflammation, antibiotics, and diet as environmental stressors of the gut microbiome in pediatric Crohn's disease. Cell Host Microbe 18(4), 489–500 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Payne S, Gibson G, Wynne A, Hudspith B, Brostoff J, Tuohy K. In vitro studies on colonization resistance of the human gut microbiota to Candida albicans and the effects of tetracycline and Lactobacillus plantarum LPK. Curr. Issues Intest. Microbiol. 4(1), 1–8 (2003). [PubMed] [Google Scholar]
- 28.McCool L, Mai H, Essmann M, Larsen B. Tetracycline effects on Candida albicans virulence factors. Infect.Dis. Obstet. Gynecol. 2008, 493508 (2008 ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Francino MP. Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front. Microbiol. 6, 1543 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jernberg C, Löfmark S, Edlund C, Jansson JK. Long-term ecological impacts of antibiotic administration on the human intestinal microbiota. ISME J. 1(1), 56 (2007). [DOI] [PubMed] [Google Scholar]
- 31.Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 8(1), 39 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shwachman H, Fekete E, Kulczycki L, Foley G. The effect of long-term antibiotic therapy in patients with cystic fibrosis of the pancreas. Antibiot. Annu. 6, 692–699 (1958). [PubMed] [Google Scholar]
- 33.Swallow J, De Haller J, Young WF. Side-effects to antibiotics in cystic fibrosis: dental changes in relation to antibiotic administration. Arch. Dis. Child. 42(223), 311 (1967). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conchie J, Munroe J, Anderson D. The incidence of staining of permanent teeth by the tetracyclines. Can. Med. Assoc. J. 103(4), 351 (1970). [PMC free article] [PubMed] [Google Scholar]
- 35.Rebich T, Kumar J, Brustman B. The St. Regis environmental health issue: assessment of dental defects. J. Am. Dent. Assoc. 106(5), 630–633 (1983). [DOI] [PubMed] [Google Scholar]
- 36.Volovitz B, Shkap R, Amir J, Calderon S, Varsano I, Nussinovitch M. Absence of tooth staining with doxycycline treatment in young children. Clin. Pediatr. 46(2), 121–126 (2007). [DOI] [PubMed] [Google Scholar]
- 37.(Fda) FaDA. Prescription drug products; doxycycline and penicillin G procaine administration for inhalational anthrax (post-exposure). Fed. Reg. 66(55679), 82 (2001). [Google Scholar]
- 38.Gaillard T, Briolant S, Madamet M, Pradines B. The end of a dogma: the safety of doxycycline use in young children for malaria treatment. Malaria J. 16(1), 148 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pöyhönen H, Nurmi M, Peltola V, Alaluusua S, Ruuskanen O, Lähdesmäki T. Dental staining after doxycycline use in children. J. Antimicrob. Chemother. 72(10), 2887–2890 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lucky AW, Biro FM, Huster GA, Morrison JA, Elder N. Acne vulgaris in early adolescent boys: correlations with pubertal maturation and age. Arch. Dermatol. 127(2), 210–216 (1991). [PubMed] [Google Scholar]
- 41.Lucky AW, Biro FM, Simbartl LA, Morrison JA, Sorg NW. Predictors of severity of acne vulgaris in young adolescent girls: results of a five-year longitudinal study. J. Pediatr. 130(1), 30–39 (1997). [DOI] [PubMed] [Google Scholar]
- 42.Norris J, Cunliffe W. A histological and immunocytochemical study of early acne lesions. Br. J. Dermatol. 118(5), 651–659 (1988). [DOI] [PubMed] [Google Scholar]