Abstract
Purpose
Operationalized treatments for school-age children with speech sound disorders may result in more replicable and evidence-based interventions. This tutorial describes Speech Motor Chaining (SMC) procedures, which are designed to build complex speech around core movements by incorporating several principles of motor learning. The procedures systematically manipulate factors such as feedback type and frequency, practice variability, and stimulus complexity based on the child's performance.
Method
The rationale and procedures for SMC are described. Examples are presented of how to design stimuli, deliver feedback, and adapt the approach. Free resources are provided to guide clinicians through implementation of the procedure. Data on fidelity of implementation and dose per session are presented. Clinical and research evidence is provided to illustrate likely outcomes with the procedure.
Results
SMC is a method that can result in successful acquisition of target speech patterns and generalization to untrained words. Most clinicians can implement the procedure with over 90% fidelity, and most children can achieve over 200 trials per session.
Conclusion
Clinicians and researchers can use or adapt the operationally defined SMC procedures to incorporate several principles of motor learning into treatment for school-age children with speech sound disorders.
Supplemental Material
Speech sound disorder (SSD) involves impaired production of speech sounds in relation to a person's age and language experience. In school-age children with persisting SSD, motor-based treatments requiring repeated practice of speech targets are common (Hitchcock & McAllister Byun, 2015; Murray, McCabe, & Ballard, 2012; Shriberg & Kwiatkowski, 1982). Such drill-based approaches may be appropriate to address speech errors in school-age children with SSD, including those with articulation disorders and childhood apraxia of speech. A common basis in these subtypes of SSD is impairment at some level of speech motor function (i.e., articulatory specifications for a specific phoneme, or planning and programming of speech movement sequences). Importantly, the application of motor learning theories to the treatment of motor-based SSDs suggests that attention to particular principles may be warranted (e.g., Hitchcock & McAllister Byun, 2015; Maas et al., 2008). However, it can be a complex task to structure treatment in a manner that purposefully manipulates numerous aspects of practice and feedback according to principles of motor learning. The purpose of this tutorial is to provide a description of Speech Motor Chaining (SMC), one type of structured motor-based speech sound treatment utilized in both research and clinical practice with school-age children with SSD. The tutorial presents an overview of the evidence base, the theoretical rationale, and a description of the procedures for SMC so that clinicians and clinical researchers may use and adapt the framework to fit a variety of treatment needs. Data on treatment fidelity and dose are also summarized, and a freely available data sheet with stimuli is provided to guide clinicians to implement the procedure.
Research Evidence for SMC
SMC procedures have been applied in a number of case studies and single-subject experimental designs (Preston & Leaman, 2014; Preston, Leece, & Maas, 2016, 2017; Preston, Leece, McNamara, & Maas, 2017; Preston, Maas, Whittle, Leece, & McCabe, 2016; Preston et al., 2014; Sjolie, Leece, & Preston, 2016). SMC has been used as part of treatment with children, adolescents, and adults with residual speech sound errors; children with apraxia of speech; and adults with acquired apraxia of speech. These procedures can be used both with and without biofeedback (e.g., Mental et al., 2016; Preston, Leece, & Maas, 2017; Preston et al., 2014; Vick, Mental, Carey, & Lee, 2017). Although the procedures were initially developed to provide a standardized practice structure as part of a series of studies that included biofeedback during sound production training, the SMC procedures are used in each session during periods of practice without biofeedback as well.
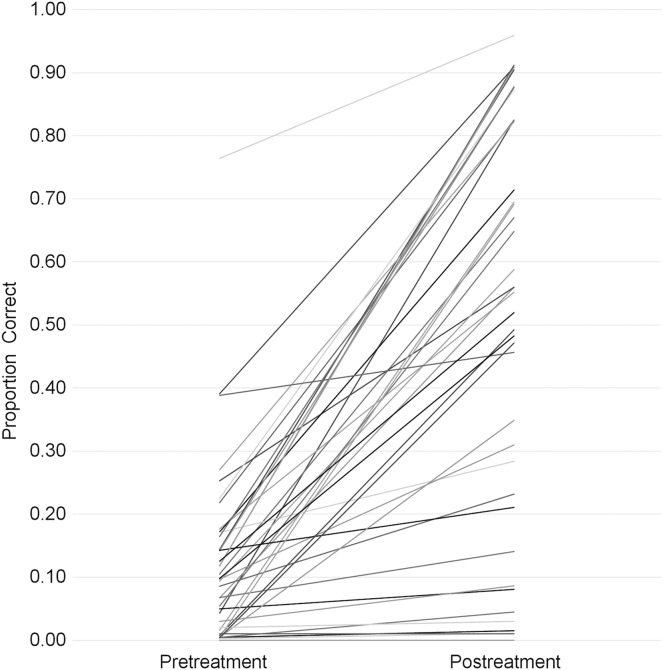
Figure 1 presents individual data from six different case series and single-subject experimental designs that have included 39 children of ages 8–21 years who were treated for residual speech errors, primarily on /ɹ/ (Preston, Leece, et al., 2016; Preston, Leece, & Maas, 2017; Preston, Leece, McNamara, et al., 2017; Preston, Maas, et al., 2016; Preston et al., 2014; Sjolie et al., 2016). Most of these children had received prior intervention that had not successfully remediated all of their sound errors. The mean pretreatment accuracy for sounds selected for treatment was 12.4% (SD = 14.5), and the mean posttreatment accuracy was 50.2% (SD = 32.1). However, these studies vary somewhat in the exact characteristics of the participants (some had childhood apraxia of speech with numerous sound errors, some had residual /ɹ/ distortions only) and in the features of the treatment (i.e., the number of hours of treatment ranged from 14 to 16, the distribution of sessions ranged from 1 to 7 weeks, and the amount of biofeedback varied from approximately 20% to 45% of the session).
Figure 1.
Target sound accuracy on untreated words for 39 children whose treatment included Speech Motor Chaining. Each line represents a separate participant.
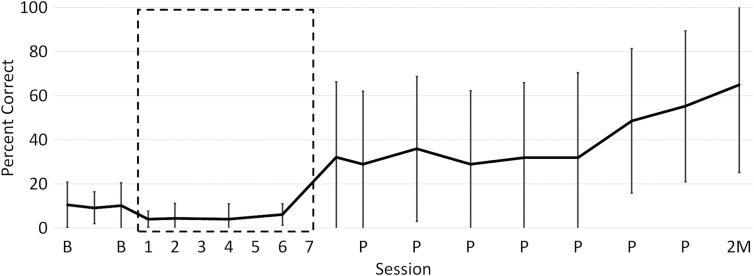
To offer an example of more homogeneous sample, Figure 2 provides data on accuracy of /ɹ/ in untrained words for children whose treatment included only SMC with no biofeedback. Accuracy is averaged across six children of ages 10–16 years with residual speech errors affecting /ɹ/ who participated in seven 1-hr treatment sessions scheduled twice per week. The average data are from a single-subject design described by Preston, Leece, and Maas (2017). Although there was individual variation in response to the treatment, the data suggest that the average improvement on untreated items was approximately 33% from pretreatment to immediately after the 7 hr of therapy. Moreover, continued monitoring for 5 weeks after withdrawal of SMC treatment suggested ongoing improvement, which is evidence of motor learning. Although more than 7 hr of therapy may be required, this provides evidence that residual speech errors can improve with this motor-based approach.
Figure 2.
Mean accuracy on word-level generalization probe for six children with /ɹ/ distortion. B = baseline (pretreatment); P = posttreatment; 2M = 2 months follow-up. Error bars represent standard deviation. Treatment occurred for seven sessions (dashed box).
Background and Theoretical Motivation for SMC
Although the primary aim of this tutorial is to describe the SMC procedures, we begin with a brief rationale. Persisting SSD can often be characterized as involving incorrect articulatory movements—that is, articulator positions and transitions between positions, which result in erred productions of speech sounds. Persisting SSD in school-age children can be the consequence of a history of speech delay, a history of normal speech sound development but failure to achieve accurate production of one or two particular speech sounds, or a history of motor speech impairment (e.g., Shriberg et al., 2010, 2017). Under the assumption that the goals of accurate speech sound production involve an acoustic target and general movement goals (e.g., Tourville & Guenther, 2011), the SMC procedures involve training speech movement patterns with feedback about both the acoustic quality of speech sounds and the articulatory actions. The procedures are intended to address isolated speech sound errors and errors associated with symptoms of impaired transitions between sounds and syllables. Therefore, the procedures have been implemented both with children with residual speech sound errors and children with persisting errors associated with childhood apraxia of speech.
Several principles derived from nonspeech motor learning literature may be relevant to speech motor learning. Critically, these principles, primarily derived from a schema-based motor learning theory, define a difference between instructional parameters that best enhance skill acquisition versus skill learning (Maas et al., 2008; Schmidt & Lee, 2011). Skill acquisition refers to increased performance during practice. In the context of speech therapy, acquisition may reflect temporary improvement in speech sound accuracy while practicing within a session. Conversely, skill learning refers to relatively permanent changes, including retention and generalization of the skill to untrained tasks. Thus, some clients show acquisition of correct articulatory patterns (improved accuracy during sessions) but fail to demonstrate learning (i.e., poor generalization or retention). In the context of therapy for SSD, early stages of treatment may require initial emphasis on skill acquisition to establish the core movements; however, a plan for systematic transition to skill learning is essential.
Maas et al. (2008) outlined several key aspects of practice and feedback, which are believed to influence skill acquisition and learning. For example, with respect to the complexity of targets, practice with simple targets (e.g., syllables) is expected to yield high performance during acquisition, whereas practice on complex targets (e.g., sentences) is more likely to facilitate skill learning. In addition, constant practice (e.g., minimal variation in consonants, vowels, and prosodic content) should enable skill acquisition, but variable practice (e.g., increasing stimulus set size and varying prosody) should enhance learning. The practice schedule may also play a role, such that blocked practice (e.g., many consecutive repetitions of the same target) leads to skill acquisition whereas random practice (e.g., mixing up stimuli) facilitates motor learning. Moreover, with respect to the feedback that is provided to the learner, knowledge of performance (KP) feedback (e.g., detailed feedback about movements, such as “the sides of your tongue were down too low for /s/”) may lead to skill acquisition, but less specific feedback or knowledge of results (KR; e.g., information about correctness, such as “good /s/ sound”) should facilitate motor learning. Skill acquisition is expected to increase when frequent feedback is provided to the learner, but learning may be facilitated by less frequent external feedback. Finally, immediate feedback is hypothesized to enhance skill acquisition, but a brief delay before feedback is provided may facilitate motor learning. Several of these principles are embedded within SMC treatment.
Individuals with SSD may require scaffolded support to achieve the goal of consistent production of articulatory movements that result in acoustically acceptable productions of phonemes. The support provided by clinicians should change over time in order to optimize learning. The SMC treatment described here involves an initial emphasis on acquisition to elicit and establish speech sounds, followed by structured steps toward speech motor learning. Therefore, SMC feedback and practice procedures are designed to initially facilitate acquisition of simple speech targets through conditions such as frequent and specific feedback and constant practice. Based on the learner's success, the treatment is dynamically adapted through five levels to address increasingly complex stimuli with strategies that include less frequent and less specific feedback and more variable practice.
Another guiding principle is the need to practice at the optimal level of difficulty while offering the appropriate level of support (Guadagnoli & Lee, 2004; Hitchcock & McAllister Byun, 2015). The assumption is that, to maximize motor learning, learners must be appropriately challenged based on the task demands and the available information (e.g., cues, feedback). Therefore, many traditional hierarchies of articulation therapy require learners to achieve a predetermined accuracy within a session (e.g., 85% accuracy on /ɹ/ at the syllable level) prior to advancing to a more complex task (e.g., /ɹ/ at the word level). However, the SMC procedures are designed to adapt more quickly as the learner is successful, with changes in the task occurring after every six trials. Thus, for children who are successful, it is possible to practice syllables, words, phrases, and sentences all within the course of approximately 2 min. For children who are unsuccessful in their productions, practice can remain at the syllable level for an entire session. This frequent decision making enables more flexibility than some traditional approaches in which modifications to linguistic level (e.g., syllables vs. words) or clinician support (e.g., amount of feedback) occur only between sessions.
Finally, the SMC procedures described herein involve stimuli that are chained. The general purpose of chaining is to quickly build to complex speech movements (i.e., words and phrases) around previously trained smaller units (i.e., sound sequences embedded in syllables). Chaining has been described for many years in the speech disorder literature as a way to teach appropriate coarticulation between sounds, to produce appropriate allophonic variation, and to maintain syllabic integrity through the smooth transitioning among syllables (Chappell, 1973; Johnson & Hood, 1988; Young, 1987). The SMC procedures described here are an attempt to operationalize a form of chaining for the purposes of clinical practice and clinical research (though other formalisms could be developed). The procedures involve the selection of a target sound in syllable position (e.g., /k/ in onset or /s/ in coda). Sound sequences (CV, VC, or CC) are chosen, which represent the target sound in syllable position. The selection of a sound sequence as the unit of training is motivated by the literature attesting to notion that the units of speech planning extend beyond individual phonemes (e.g., Bohland, Bullock, & Guenther, 2010; Redford, 2015; Tilsen, 2013). During practice, additional movements are gradually added before the target sequence (backward chaining) or after the target sequence (forward chaining). For example, when training the target /k/ in onset, one representative sound sequence is /kl/. Chaining for each sequence begins in a syllable (e.g., /kle/), followed by a monosyllabic word (e.g., claim), a multisyllabic word (e.g., proclaim or claiming), a short phrase (e.g., proclaim the news, or He wasn't claiming), and eventually a self-generated sentence (e.g., using the word proclaim or claiming in a sentence). Practice at the higher levels of linguistic complexity only occurs when there is success at the previous level. Within each level, however, the feedback provided to the learner addresses the target movement sequence (/kl/). Thus, there is an intentional plan for building complexity around each stimulus that is chosen, as the larger units (e.g., multisyllabic words) are designed to encompass the smaller units (e.g., monosyllabic words and syllables) to facilitate success.
Assessment Considerations and Treatment Planning
Treatment can be planned appropriately following a thorough assessment. In addition to a standardized assessment of speech sound production to verify the presence of a SSD, deep testing is particularly helpful when using SMC. Deep testing involves assessing a speech sound across a variety of words sampling various phonetic contexts, including different word positions, stress patterns, and adjacent phonemes (Kent, 1982). Finding prosodic environments and coarticulatory contexts in which the child is most successful can assist in selecting initial stimuli for SMC sessions. For example, for a child whose /ɹ/ in coda position is correct only 10% of the time, noting that the correct production occurs following a back vowel /ɑ/ may encourage the selection of /ɑɹ/ as one target syllable to practice in treatment, which may facilitate acquisition of /ɹ/ in other contexts.
Appropriate targets for SMC are typically sounds that are below 50% accuracy in a particular syllable position when tested at the word level. Typically, two broad targets are treated per child for each session (e.g., onset /ɹ/ and coda /k/). Following the selection of sounds in word position targets, four variants (i.e., sound sequences) are initially chosen. Variants of the target are two-phoneme (e.g. CC, CV, VC) or occasionally three-phoneme (e.g., CCC) sequences. For example, the target of onset /ɹ/ could be addressed with four variants: two /ɹ/ singleton variants such as /ɹi/ and /ɹɑ/ and two /ɹ/ cluster variants such as /dɹ-/ and /kɹ-/. Coda /k/ could be addressed with four variants such as singletons /ek/ and /ʊk/ and clusters /-kt/ and /-sk/. In each session, two different chains are chosen per variant, resulting in 16 chains per session (2 sounds × 4 variants × 2 chains). This choice of sound sequences as treatment targets (rather than isolated sounds) demands intentional focus on a movement pattern (such as a consonant transitioning into or out of various vowels), rather than simply production of a phoneme. In selecting these sequences, a relative range of difficulty could be considered based on the client's observed success during an assessment; for example, some variants may include sequences that are likely to be facilitative, and some variants may include sequences that are likely to be more challenging. Chains are then built around the chosen variants.
Phonetic context should be considered when selecting phoneme sequences that represent the target sound in word position. If a client is minimally stimulable in one phonetic context, it is important to try to practice that facilitative context in at least one chain to allow the client to experience some success in a session. If the client is not stimulable in any context, syllables can be chosen, which theoretically may be phonetically facilitative (e.g., /ɑɹ/ may be potentially facilitative for /ɹ/ because /ɑ/ promotes pharyngeal constriction; /ts/ may be facilitative for /s/ due to the presence of a preceding alveolar stop; /ʊk/ may be facilitative for /k/ due to the presence of the mid–high back vowel). When possible, the chosen sound sequences should sample a variety of phonetic environments to encourage accurate production of movement gestures across various coarticulatory contexts. Thus, when selecting vowel contexts to be paired with a consonant, nonadjacent vowels along the vowel quadrilateral should be considered. For example, variants to address /ɹ/ in onset may include /ɹi/ and /ɹɑ/, because of the high-front and low-back vowels (vis-à-vis /ɹi/ and /ɹɪ/, which are closer on the vowel quadrilateral). Similarly, choosing consonant clusters that vary in place of articulation allows for practice across various coarticulatory environments (e.g., /dɹ-/ and /ʃɹ-/ may be preferred variants because they differ in place of articulation, manner, and voicing of the first phoneme, vis-à-vis /dɹ/ and /tɹ/, which differ only in voicing). Practicing such variation may facilitate acquisition of contextually driven allophones (cf. Mielke, Baker, & Archangeli, 2016). Table 1 provides examples of target sequence selection that encourages varied phonetic contexts. Supplemental Material S1 provides further examples of how chains are built around the selected variants.
Table 1.
Examples of target sound/position and four possible variants (sound sequences) for practice across a range of phonetic contexts.
| Target sound/position | Variant 1 | Variant 2 | Variant 3 | Variant 4 |
|---|---|---|---|---|
| /ɹ/ onset | /ɹɑ/ | /ɹi/ | /dɹ/ | /kɹ/ |
| /s/ onset | /si/ | /so/ | /sk/ | /sn/ |
| /k/ rhyme | /ɪk/ | /æk/ | /sk/ | /kt/ |
| /ʧ/ rhyme | /iʧ/ | /æʧ/ | /ʌʧ/ | /nʧ/ |
Prepractice
Typically, SMC sessions are initially divided into two phases: prepractice (elicitation) and structured practice using SMC. Later, a third phase, randomized practice, may be added. Within the prepractice phase, the clinician helps the learner to identify a minimum reference for correctness such that the child becomes familiar with the distinction between correct and incorrect productions of the variants. Stimulability for the chosen variants is achieved with modeling, shaping, and verbal and visual cues for articulator placement and movement (e.g., Secord, Boyce, Donohue, Fox, & Shine, 2007). For example, to address /ɹ/, shaping strategies may involve /l/→/ɹ/ or /ɑ/→/ɹ/. However, trials within prepractice are not considered successful until the entire sound sequence is produced correctly (e.g., correct production of the syllables /ɹi/ or /ɹɑ/ with smooth transitions between segments, not just isolated /ɹ/). Phonetic placement for /ɹ/, for example, may consist of cues to elevate the anterior tongue, keep the dorsum low, elevate the sides of the tongue, retract the tongue root, or keep the lips steady. Visual cues to aid the prepractice stage may include images of vocal tract shape (e.g., http://www.seeingspeech.ac.uk/ipachart/) or tongue–palate contact with electropalatography examples (e.g., McLeod & Singh, 2009). Within the prepractice phase, the clinician provides frequent cueing and immediate detailed feedback to elicit correct productions from the client. In our approach, prepractice is continued until the client achieves several correct productions of each variant (at least three correct productions of each variant). During the prepractice phase, the clinician can determine the phonetic cues that are most valuable in helping the child achieve correct productions, and such cues may be continued during the feedback that is provided during structured practice with SMC.
SMC
After a sufficient number of correct productions of each variant are achieved during prepractice, practice with SMC begins. The SMC data sheet is designed to guide clinicians through the implementation of the following principles. Target syllables, words, and phrases are elicited in blocks of six consecutive attempts, and practice starts at the syllable level. Some example chains are shown in Table 2. Chains consist of five practice levels, which are defined by complexity around the target variants:
Table 2.
Examples of chains.
| Sound/position | Syllable | Monosyllabic word | Multisyllabic word | Phrase | Self-generated sentence |
|---|---|---|---|---|---|
| /ɹ/ onset | /ɹɑ/ | rot | rotten | rotten food | ? |
| /ɹ/ rhyme | /ɔɹ/ | for | before | just before | ? |
| /k/ onset | /ki/ | keep | keeping | keeping my money | ? |
| /k/ rhyme | /ʊk/ | book | bookshelf | on the bookshelf | ? |
| /s/ onset | /sɪ/ | sit | sitting | sitting down | ? |
| /s/ rhyme | /æst/ | cast | broadcast | national broadcast | ? |
| /ʧ/ onset | /ʧæ/ | champ | champion | world champion | ? |
| /ʧ/ rhyme | /ɪʧ/ | witch | sandwich | eat a sandwich | ? |
Note. Observe that the target sequence (in bold) remains consistent throughout the chain.
syllables, which contain at least one consonant and one vowel: CV, CC(V), VC, or (V)CC—these are the basic sound sequences (variants) representing the target;
monosyllabic words, which begin or end with the syllable and which contain both an onset and a coda;
multisyllabic words, which include two or more syllables and which contain the monosyllabic word;
phrases, which include two to five words and which contain the monosyllabic word or the multisyllabic word; and
self-generated sentences, in which the child uses either the monosyllabic word or multisyllabic word in a novel sentence.
Advancing from one level of a chain to the next level requires at least five of six correct productions in a block. For example, five correct productions of the syllable /ɹɑ/ are needed to progress to the monosyllabic word rock. Failure to achieve at least five correct productions at any level results in moving to a new chain with a different variant of the target, returning to Level 1 (e.g., switching from a /ɹɑ/ chain to a /ɹi/ chain). In the current operationalized structure, a chain is mastered when a child successfully progresses through all five levels of the chain on two separate occasions (i.e., at least five correct productions of a self-generated sentence). Once the chain is mastered, a replacement chain with the same variant is used in the next session (e.g., replace rock-rocket-my rocket ship with a chain such as rot-rotten-rotten food).
The SMC structure enables the client to quickly practice up to a level that is sufficiently challenging, similar to the “challenge point” framework (Guadagnoli & Lee, 2004; Hitchcock & McAllister Byun, 2015; Rvachew & Brosseau-Lapré, 2012). That is, clients work at a level of difficulty in which some but not all attempted utterances are likely to be correct. If the task proves too hard, practice returns to the syllable level again in conditions that are more acquisition focused (limited linguistic level/less complex, frequent and specific feedback) before building up to targets that are more learning focused (higher linguistic levels, more variability, reduced feedback).
Feedback
Verbal feedback by the clinician on any trial during SMC consists of KR, KP, or no feedback. Table 3 provides examples of clinician responses for these types of feedback.
Table 3.
Examples of knowledge of results and knowledge of performance feedback.
| Feedback type | Segments | Positive feedback | Negative feedback |
|---|---|---|---|
| Knowledge of results | Any | Correct. | Not that time. |
| You got it. | No. | ||
| Great. | Didn't get that one. | ||
| Excellent. | Not that one. | ||
| Way to go. | Not quite. | ||
| Knowledge of performance | /ɹ/ | Good, your tongue tip was raised. | Not quite. Lift the front of your tongue up a little. |
| Got it! Your sides were up. | Not quite. Try to lift the sides up to touch the back molars. | ||
| Yes, you got tongue root back into the throat. | Not that time, try to pull the tongue root back into the throat. | ||
| Good, you kept the back of your tongue down. | No, I think you raised the tongue dorsum too high. | ||
| Good, you kept the lips steady. | Not quite. Your lips were sticking out too much. | ||
| Knowledge of performance | /k/ | Awesome! You kept your tongue tip down. | No. Both the tongue tip and the tongue dorsum were up on that one. |
| Good, you raised the back of your tongue. | Not quite. You raised the tip up, not the dorsum. | ||
| Great job lifting the dorsum up. | Didn't get the dorsum up to the roof of your mouth. | ||
| Knowledge of performance | /s/ | Got it. The sides of the tongue were touching your teeth. | Not quite. The middle and sides were even. |
| I like that you made a nice deep groove. | Not that time. The groove wasn't there. | ||
| Great job keeping the air moving the whole time. | No. The air stopped and didn't move through the whole /s/ sound. |
KR refers to information only about the correctness of the speech sounds (phonetically correct or incorrect). That is, the acoustic accuracy is judged as either being a good (accurate) or poor (inaccurate) form of the target sounds. KR feedback is typically associated with motor learning because the clinician offers no specific information about why a production was correct or incorrect or what movements the client should change (Maas et al., 2008).
KP refers to feedback about the nature of the movement that was just performed. If a sound is produced in error, the KP feedback provided by the clinician should make reference to aspects of the phonetic placement, vocal tract configuration, or movement sequencing that need to change to achieve a correct production. If a target sound is produced correctly, the KP feedback should highlight aspects of the movement that resulted in correct production. The KP feedback is therefore specific to the type of error produced or the movement that was achieved. The KP feedback typically aids acquisition and is provided frequently in the early stages of treatment because the clinician offers specific information to the client about the essential aspects needed to achieve the intended speech movements. In SMC, the KP feedback is provided on four of six trials at the syllable level and on one of six trials at the sentence level. Generally, when the KP feedback is provided, it is implicitly or explicitly accompanied by the KR feedback as well. For example, “Good job [KR]! You lifted the back of your tongue up [KP] when you started /ki/.” In several previous studies, periods of treatment sessions have included verbal KP supplemented with visual KP in the form of visual biofeedback (e.g., Preston & Leece, 2017; Preston, Leece, et al., 2016; Preston et al., 2014).
The amount and type of feedback at each level is intended to change as client's progress in SMC, with successive reductions in the amount of feedback (i.e., fewer trials with feedback) and changes in the type of feedback from primarily KP to primarily KR. The type of feedback assigned to a trial is specified on the SMC data sheet.
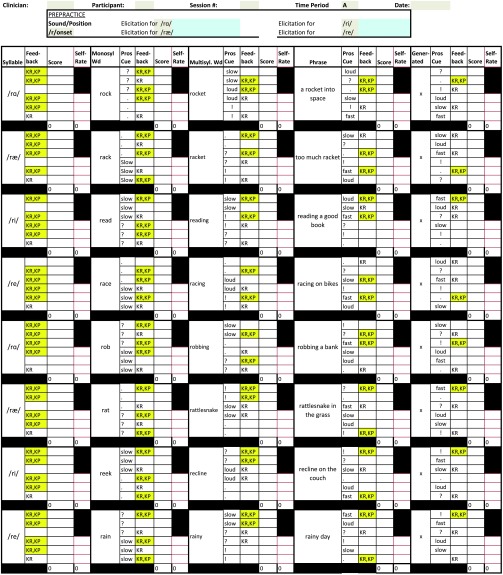
SMC Data Sheet
A data sheet is available to guide users to implement the SMC procedures. A sample data sheet is available in the Appendix. A fillable electronic copy in Microsoft Excel is freely available at https://osf.io/5jmf9/, which can be used with a computer or a tablet (see Supplemental Material S1). A number of prepopulated chains are included in the file (accessible as drop-down selection choices), although new chains can be added by users.
At the top of the data sheet, the target sound/word position is entered along with four variants. Also, along the top is a section to track the number of correct productions during prepractice.
The remainder of the data sheet displays the list of chains chosen for practice during the session. The client's performance is assessed by the clinician after every six trials to determine whether practice should build to a more complex stimulus (moving to the right on the data sheet) or whether practice should switch to a chain for a different variant (moving down on the data sheet). The criterion of five correct in a block of six is required to move to more complex targets in a chain. Thus, each trial should be scored, and a sum should be computed after each block of six trials.
The data sheet also provides information to guide the nature and type of feedback that should be provided by the clinician. Within each block, feedback in the form of KR, KP + KR, and no feedback trials are randomly allocated to the six trials while maintaining the expected proportion (e.g., at the syllable level, one trial with no feedback, one trial with KR feedback, and four trials with KP + KR feedback, but at the sentence level, there are three trials with no feedback, one trial with KR + KP feedback, and two trials with KR feedback).
Prosodic Variation
Practice variability can be included in the form of prosodic variation. This is intended to encourage practice of the target sound sequences in utterances that vary in rate, intonation, or loudness. When prosodic variation is included, clients are cued to practice utterances slow, fast, loud, as a question, as a command, or as a statement. Although this variation was found to have a minimal impact on speech sound learning in children with residual speech sound errors (Preston et al., 2014), recent research with children with childhood apraxia of speech has suggested that this prosodic variation may aid generalization and retention in that population (Preston, Leece, McNamara, et al., 2017). Thus, prosodic variation may help children learn to integrate articulatory movements with other parameters of speech that are planned.
Self-Monitoring
Another feature of SMC includes explicit requirements for clients to self-rate the accuracy of their productions. In our current version of SMC, each block of six trials requires self-rating on three trials. Before any feedback is given by the clinician, the child is asked to provide a self-evaluation of accuracy. Such procedures have been shown to facilitate generalization in speech sound learning (Koegel, Koegel, & Ingham, 1986; Ruscello & Shelton, 1979). After the child self-evaluates, the clinician may provide feedback by stating whether they agree or disagree with the child's judgment.
A sample chain including prosodic cues and self-monitoring is provided in the Appendix. In addition, a video example of portion of a session using SMC is provided in Supplemental Material S2.
Increasing Difficulty of Chains
Intentional modifications to the chains selected for treatment may influence task difficulty. Initially, chains are chosen which place the target sound sequence in a facilitative context in word-initial or word-final position, and chains include the target sound in a stressed syllable in multisyllabic words. However, over the course of treatment, chains that are mastered (i.e., produced correctly through the sentence level on multiple occasions) need not be repeated but instead can be replaced by chains that may be more challenging to the speech system. Three strategies for increasing the difficulty of chains are discussed below. The properties of the chains differ starting at the monosyllabic or multisyllabic word level. Examples of these modifications are shown in Table 4.
Table 4.
Strategies to increase the difficulty of chains.
| Variant | Monosyllabic word | Multisyllabic word options |
|||
|---|---|---|---|---|---|
| “Basic” speech motor chain | Medial position | Lexical stress | Competing sounds or multiple targets | ||
| /ɑɹ/ | tar | guitar | tarnish | starvation | rock-star |
| /ɑk/ | lock | unlock | clockwise | hemlock | gridlock |
| /se/ | sale | sailor | assailant | wholesale | sailboats |
Note. Observe that the target sequence (in bold) remains consistent throughout the chain.
Word-Medial Position
When targeting a sound sequence in word-initial or word-final position, there is only one coarticulatory transition that must be practiced (i.e., transitioning into or out of the target movement sequence, but not both, as in /kle/ at beginning of claiming). Positioning the target sound sequence in medial position of multisyllabic words creates a potentially more challenging coarticulatory environment, requiring smooth transitions into and out of the target movement pattern (e.g., /kle/ in proclaim). This change may increase the demands on motor planning as the sequences are embedded in a larger stream of movements. Often, word-medial chains are introduced with the addition of a bound morpheme (prefix or suffix), although compound word contexts (e.g., two-syllable spondees) can be used as well.
Lexical Stress
To increase the difficulty of planning multisyllabic words, the target sequences can also be practiced in syllables that do not carry primary stress. Often, targets in syllables with primary stress (e.g., /ɹi/ in reading) are more accurate because they are typically longer in duration than syllables that do not carry primary stress (e.g., /ɹi/ in realistic); thus, stressed syllables may reduce the demands on motor programming. In unstressed syllables, however, the target sequences may be more challenging to the client because there is less time to plan and execute movements and less transition time between articulatory gestures.
Competing Sounds
To increase the difficulty of chains, competing sounds may be included. Competing sounds are those that share some articulatory gestures with the target (typically manner or place of articulation of consonants). Competing sounds may also include the child's typical error for a sound and may be present in the same word or in another word in a phrase. Competing sounds challenge the speech planning system by intentionally including articulatory gestures, which may interfere with the intended sound sequences (cf. Rogers & Storkel, 1998; Tilsen, 2013). For example, competing sounds for /ɹ/ in a target sound sequence may include /l/ (which is also a liquid) or /w/ (which is also a semivowel and is a common substitute for /ɹ/). Thus, words such as Larry and rewind would be target words with competing sounds for the target sequence /ɹi/. Competing sounds for /k/ in a target sound sequence may include /ɡ/ or /ŋ/ (which are also velars) or /t/ (which is a common substitute for /k/). Thus, words such as took and book bag include competing sounds for the target sound sequence /ʊk/. The competing sounds strategy can be implemented at the monosyllabic word level; however, it is recommended that competing sounds be introduced when the client can readily produce the target sound sequence in words that do not have a competing sound. Competing sounds could also include repetition of the target sound sequence in different syllables or words, as in took the book.
Randomized Practice
SMC procedures may set the foundation to transition into more complex tasks. For example, the blocked practice in SMC may improve acquisition, but randomization may aid learning. Therefore, in our recent iteration of SMC (e.g., Preston & Leece, 2017; Sjolie et al., 2016), a period of randomized practice has been included at the end of sessions once a child is capable of progressing through prepractice quickly (i.e., with zero or one error on syllables). In the current version of practice sessions, randomized practice is included in the last 5–8 min of a session using the highest items on each chain that were produced correctly during SMC (i.e., items with at least five of six trials correct). Based on the client's performance during SMC earlier in the session, randomized practice items may range from syllables through sentences. The varied stimulus items from the chains practiced during the session can then be shuffled such that the child is unaware of which item is coming next (cf. Skelton & Hagopian, 2014). To further incorporate motor learning principles, prosodic variation is also cued during randomized practice (e.g., say the word read loudly; say the sentence I found a book as a question), and delayed KR feedback is provided on only 50% of trials during randomized practice.
Caveats
SMC procedures are designed to facilitate a transition from acquisition to motor learning. However, SMC may be supplemented with other clinical procedures. For example, auditory perception and phonological awareness are relevant skills that may be related to SSD in school-age children (e.g., Preston & Edwards, 2007; Shuster, 1998). Therefore, auditory perceptual training and phonological awareness may also be targeted in a session to address multiple levels of representation of speech (Preston & Leece, 2017; Preston, Leece, et al., 2016; Preston, Leece, McNamara, et al., 2017). Thus, a comprehensive treatment session may include SMC supplemented with additional clinical procedures.
In addition, the SMC procedures described here have been developed over time and should not be viewed as unchanging. For example, the randomized practice, self-monitoring, and prosodic variations that are included in the current iteration of SMC were not all part of the procedure when it was initially developed. Because a number of parameters have been operationalized, they can continue to be empirically tested. For example, variations in the number of items per block, frequency of feedback, and amount of self-monitoring could all be varied and tested to maximize efficiency.
Finally, it should be noted that, like all current treatments, SMC may not be appropriate for all children. For example, we expect that many 3- to 4-year-olds, or older children with significant intellectual disabilities, may not respond well to a highly structured drill-based treatment (though this speculation remains to be empirically tested). Furthermore, as was evident in Figure 1, many but not all children show signs of generalization with this treatment. To date, we have observed acquisition (correct productions of target sound patterns within treatment sessions) for nearly every child, but those gains in treatment sessions do not ubiquitously result in increased performance on generalization measures. This may be a function of an insufficient number of hours of treatment or a need for a different type of treatment. Therefore, continued refinement of the procedure remains warranted.
Implementation of SMC Procedures
In addition to the research implementation described earlier, SMC has been used by a number of certified speech-language pathologists and student clinicians in the Gebbie Speech-Language Clinic at Syracuse University. The procedures have been used with children ages 6 years through adults with various SSD profiles, including residual speech errors and childhood apraxia of speech. Although the primary implementation has been during individual therapy sessions, the procedures have also been adapted for group therapy (cf. Skelton & Richard, 2016). For example, children in the group may practice a chain one at a time (from syllable level through the highest level to which he or she can progress). To encourage generalization and attention to others' speech, children in the group can be taught to attend to others' productions and to provide KR feedback to other members of the group (cf. Johnston & Johnston, 1972). Reinforcers such as a turn-taking game can be completed with one child while another child begins a new chain.
Typically, in a clinic setting, sessions are scheduled one to two times per week for an hour, although other service delivery options are feasible. For example, a more frequent treatment schedule (e.g., daily sessions) can be considered, particularly in the early stages of acquisition (cf. Preston & Leece, 2017). SMC may also be a viable approach for implementing short individualized drill-based sessions in school settings (cf. Sacks, Flipsen, & Neils-Strunjas, 2013).
Fidelity
Procedures that are most likely to be adopted clinically are those in which high levels of fidelity can be achieved. Data from studies that have included five certified speech-language pathologists and two graduate students are listed in Table 5. The clinicians for whom fidelity data are reported engaged in a one-on-one training with the first author, with total training lasting approximately 3 hr. This training session consisted of review of the SMC data sheet, a manual, cueing and feedback strategies, and audio files of sessions. The fidelity data in Table 5 represent the proportion of trials in which the treating clinician provided feedback as specified by the procedures. The mean proportion of trials in which adequate feedback was provided exceeds 80% for all clinicians, and it exceeds 90% for all but one clinician. This suggests fidelity on the feedback structure can be achieved even for student clinicians.
Table 5.
Fidelity on feedback structure.
| Clinician | No. of sessions | Percent of trials in which prescribed feedback was provided |
|
|---|---|---|---|
| M (SD) | Range | ||
| SLP 1 | 23 | 98.5 (2.2) | 84–100 |
| SLP 2 | 15 | 97.0 (1.8) | 93–99.4 |
| SLP 3 | 12 | 81.9 (19.2) | 41.8–94.5 |
| SLP 4 | 8 | 98.0 (1.4) | 95.6–100 |
| SLP 5 | 4 | 99.1 (0.5) | 98.2–99.5 |
| SLP Student 1 | 8 | 96.3 (2.7) | 91.7–98.7 |
| SLP Student 2 | 4 | 95.1 (6.6) | 86.9–95.24 |
Note. SLP = speech-language pathologist.
Dose
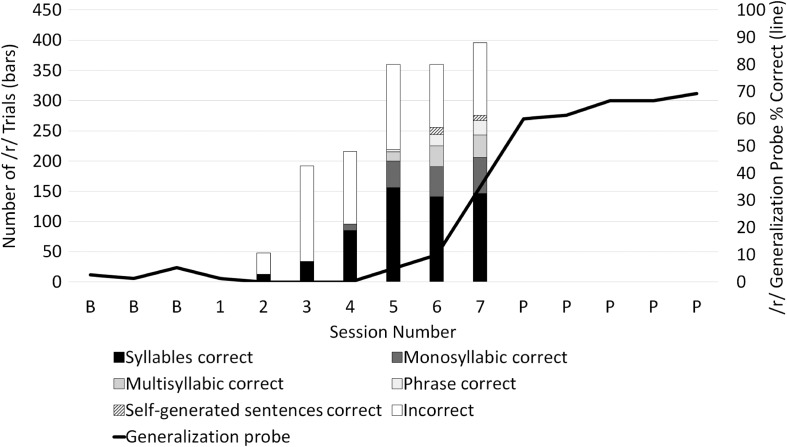
Studies have shown that a relatively high rate of practice trials in speech therapy can be beneficial for learning (e.g., Edeal & Gildersleeve-Neumann, 2011). Figure 3 shows the distribution of the average number of SMC practice trials per participant across 36 participants of ages 7–24 years reported in six studies (Preston & Leece, 2017; Preston, Leece, et al., 2016; Preston, Leece, & Maas, 2017; Preston, Leece, McNamara, et al., 2017; Preston, Maas, et al., 2016; Sjolie et al., 2016). Each participant's mean number of trials per session is based on 14–20 treatment sessions that included 40–52 min of time devoted to speech practice. One quarter of the participants (nine of the 36) practiced an average of less than 100 trials per session, primarily because they required several sessions to achieve stimulability and therefore had numerous sessions with zero trials in SMC practice. That is, a lower dose is generally due to the time spent achieving several successful productions in prepractice before moving to SMC (rather than a function of inefficient SMC). Typically, participants attempt fewer trials in early sessions (when more time is spent in prepractice and less time is spent in SMC) and increasingly more trials in later sessions (when less time is spent in prepractice and more time is spent in SMC). Overall, these participants averaged 218 trials per session (SD = 131), and the data suggest SMC may be viewed as yielding a high dose for most participants.
Figure 3.
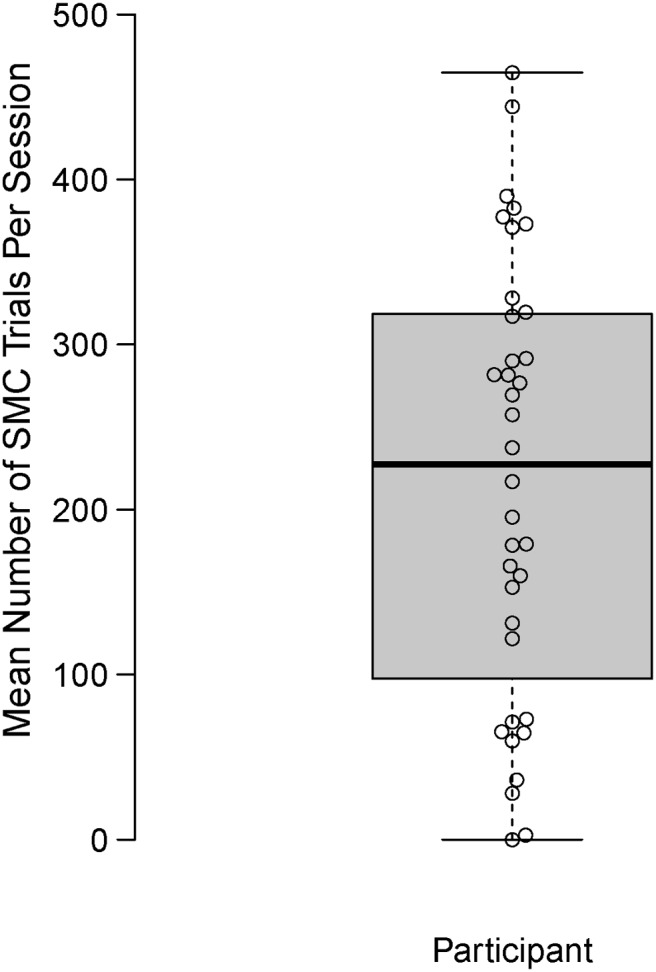
Boxplot representing mean number of Speech Motor Chaining (SMC) trials per session for 36 participants with speech sound disorders. Each data point represents mean number of trials per session across 14–20 sessions.
Performance During Acquisition Versus Generalization
The data collected during SMC are reflective of the acquisition process, but not the generalization process. Therefore, generalization data on untreated items, rather than success during SMC practice trials, should serve as a primary outcome when monitoring progress. Our practice to monitor generalization takes approximately 3 min to administer and includes probing accuracy of the target sound in word position on a list of 25 untreated monosyllabic and multisyllabic words. Items are administered by having children read a list of words (or name pictures if reading skills significantly interfere with the process). Essentially, any word that is not on the generalization list would be eligible to select for training in SMC. In several previous studies, generalization probes have been administered after approximately every two sessions. However, the requirements of frequent monitoring in an experimental design may not be the same as those required clinically; therefore, as generalization is a gradual process, probes may be useful for monitoring progress after approximately every three to four sessions. We recommend administering probes at the beginning of a treatment session rather than at the end, as accuracy at the beginning of the session will reflect not only generalization but also retention from previous sessions. As performance reaches approximately 80% or higher on untreated words, probing accuracy in 10–15 untrained sentences may replace word-level probes. Accuracy above 80% on sentence-level stimuli may be sufficient to discontinue SMC and to then shift focus to treatments that focus on conversational monitoring.
Case Example
Ryan (pseudonym) was a 10-year-old with normal language and hearing. He participated in seven 1-hr treatment sessions to address production of /ɹ/ in onsets. Prior to treatment, he was not stimulable for /ɹ/ in any contexts. His treated variants included /ɹæ/ and /ɹi/, with chains such as rap, rapid, rapid decision and read, redeem, redeeming quality. In addition to his within-session performance, progress was tracked every other session on word-level generalization probes containing untrained words. Monitoring on these probes continued weekly for 5 weeks after withdrawal of SMC treatment.
The bars in Figure 4 show within-session performance for Ryan during the seven treatment sessions. In the first session, he did not reach the criterion to advance to SMC, and he, therefore, remained in prepractice (i.e., sessions consisted of strategies such as shaping and phonetic placement cues to elicit /ɹ/ in syllables). However, in Sessions 2 and 3, he progressed from prepractice to SMC where he was successful in achieving correct productions only at the syllable level. At Session 4, he began to achieve successful productions in monosyllabic words; in Session 5, he produced chains through multisyllabic words and phrases, and in Sessions 6 and 7, he progressed to chains with sentences. It can be seen in Figure 4 that the total number of trials increased greatly as he spent less time in prepractice, became increasingly accurate, and required less feedback and instruction. Furthermore, SMC resulted in a high rate of practice with over 350 productions per hour during Sessions 5–7.
Figure 4.
Acquisition data (bars) and generalization data (line) for a 10-year-old with /ɹ/ distortion. Generalization probe data were collected before, during, and after seven sessions of treatment with Speech Motor Chaining (SMC).
Figure 4 also shows his performance on the generalization probe (solid line) before, during, and after treatment (as rated by three listeners who were blind to when the recordings were collected). He was perceived to be below 10% accurate before treatment, and the week after his SMC sessions ended, he was 66% accurate on /ɹ/ onsets. A final follow-up session 2 months later revealed word-level performance over 90%.
The acquisition data during SMC treatment and the generalization data in Figure 4 provide complementary perspectives on his performance. That is, it was only after seven sessions of treatment that he began to show signs of generalization to untreated words. It may be that a particular threshold of accuracy or a cumulative effect of many correct trials within a session is required before generalization is observed.
Conclusion
SMC is an operationalized form of speech practice, which is designed to dynamically transition from an emphasis on principles of acquisition to an emphasis on principles of motor learning. Speech movement patterns are gradually expanded, such that larger speech units (e.g., multisyllabic words) incorporate the same general movement patterns that were produced successfully in smaller speech units (e.g., monosyllabic words, which were also practiced in syllables). Moreover, as motoric and linguistic complexity expands, variability of practice is added and feedback type and frequency are manipulated. The procedures involve a rapid rate of practice with the potential for frequent changes to practice conditions. However, the procedures can be delivered with high fidelity using a freely available data sheet, allowing for replicable implementation. Furthermore, the theoretically motivated framework allows for systematic study of the key elements (an ongoing process), and modifications of the approach for clinical and research endeavors are quite feasible. SMC is therefore one approach that may be considered for treatment of SSD in school-age children.
Supplementary Material
Acknowledgments
The authors thank Patricia McCabe for feedback on early stages of the development of this approach. Research reported in this publication was supported by the National Institute on Deafness and Other Communication Disorders under Awards R15DC016426 and R03DC012152 (J. Preston, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix
Speech Motor Chaining Data Sheet
Funding Statement
The authors thank Patricia McCabe for feedback on early stages of the development of this approach. Research reported in this publication was supported by the National Institute on Deafness and Other Communication Disorders under Awards R15DC016426 and R03DC012152 (J. Preston, PI).
References
- Bohland J. W., Bullock D., & Guenther F. H. (2010). Neural representations and mechanisms for the performance of simple speech sequences. Journal of Cognitive Neuroscience, 22(7), 1504–1529. https://doi.org/10.1162/jocn.2009.21306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappell G. E. (1973). Childhood verbal apraxia and its treatment. The Journal of Speech and Hearing Disorders, 38(3), 362–368. https://doi.org/10.1044/jshd.3803.362 [DOI] [PubMed] [Google Scholar]
- Edeal D. M., & Gildersleeve-Neumann C. E. (2011). The importance of production frequency in therapy for childhood apraxia of speech. American Journal of Speech-Language Pathology, 20(2), 95–110. https://doi.org/10.1044/1058-0360(2011/09-0005) [DOI] [PubMed] [Google Scholar]
- Guadagnoli M. A., & Lee T. D. (2004). Challenge point: A framework for conceptualizing the effects of various practice conditions in motor learning. Journal of Motor Behavior, 36(2), 212–224. https://doi.org/10.3200/JMBR.36.2.212-224 [DOI] [PubMed] [Google Scholar]
- Hitchcock E. R., & McAllister Byun T. (2015). Enhancing generalisation in biofeedback intervention using the challenge point framework: A case study. Clinical Linguistics & Phonetics, 29(1), 59–75. https://doi.org/10.3109/02699206.2014.956232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H. P., & Hood S. B. (1988). Teaching chaining to unintelligible children: How to deal with open syllables. Language, Speech, and Hearing Services in the Schools, 19(2), 211–220. [Google Scholar]
- Johnston J. M., & Johnston G. T. (1972). Modification of consonant speech-sound articulation in young children. Journal of Applied Behavior Analysis, 5(3), 233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent R. D. (1982). Contextual facilitation of correct sound production. Language, Speech, and Hearing Services in Schools, 13(2), 66–76. https://doi.org/10.1044/0161-1461.1302.66 [Google Scholar]
- Koegel L. K., Koegel R. L., & Ingham J. C. (1986). Programming rapid generalization of correct articulation through self-monitoring procedures. Journal of Speech and Hearing Disorders, 51(1), 24–32. [DOI] [PubMed] [Google Scholar]
- Maas E., Robin D. A., Austermann Hula S. N., Freedman S. E., Wulf G., Ballard K. J., & Schmidt R. A. (2008). Principles of motor learning in treatment of motor speech disorders. American Journal of Speech-Language Pathology, 17(3), 277–298. https://doi.org/10.1044/1058-0360(2008/025) [DOI] [PubMed] [Google Scholar]
- McLeod S., & Singh S. (2009). Seeing speech. San Diego, CA: Plural. [Google Scholar]
- Mental R., Foye M., Lee G., Schreiber N., Barnes A., & Vick J. (2016). Opti-Speech: A newly developed biofeedback software for persistent speech sound disorders. Technical Clinical session presented at the Annual Convention of the American Speech-Language-Hearing Association, Philadelphia, PA. [Google Scholar]
- Mielke J., Baker A., & Archangeli D. (2016). Individual-level contact limits phonological complexity: Evidence from bunched and retroflex /ɹ/. Language, 92(1), 101–140. [Google Scholar]
- Murray E., McCabe P., & Ballard K. J. (2012). A comparison of two treatments for childhood apraxia of speech: Methods and treatment protocol for a parallel group randomised control trial. BMC Pediatrics, 12(112). https://doi.org/10.1186/1471-2431-12-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston J. L., & Edwards M. L. (2007). Phonological processing skills of adolescents with residual speech sound errors. Language, Speech, and Hearing Services in Schools, 38(4), 297–308. https://doi.org/10.1044/0161-1461(2007/032) [DOI] [PubMed] [Google Scholar]
- Preston J. L., & Leaman M. (2014). Ultrasound visual feedback for acquired apraxia of speech: A case report. Aphasiology, 28(3), 278–295. https://doi.org/10.1080/02687038.2013.852901 [Google Scholar]
- Preston J. L., & Leece M. C. (2017). Intensive treatment for persisting rhotic distortions: A case series. American Journal of Speech-Language Pathology, 26(4), 1066–1079. https://doi.org/10.1044/2017_AJSLP-16-0232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston J. L., Leece M. C., & Maas E. (2016). Intensive treatment with ultrasound visual feedback for speech sound errors in childhood apraxia. Frontiers in Human Neuroscience, 10(440). https://doi.org/10.3389/fnhum.2016.00440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston J. L., Leece M. C., & Maas E. (2017). Motor-based treatment with and without ultrasound feedback for residual speech-sound errors. International Journal of Language & Communication Disorders, 52(1), 80–94. https://doi.org/10.1111/1460-6984.12259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston J. L., Leece M. C., McNamara K., & Maas E. (2017). Variable practice to enhance speech learning in ultrasound biofeedback treatment for childhood apraxia of speech: A single case experimental study. American Journal of Speech-Language Pathology, 1–13. https://doi.org/10.1044/2017_AJSLP-16-0155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston J. L., Maas E., Whittle J., Leece M. C., & McCabe P. (2016). Limited acquisition and generalisation of rhotics with ultrasound visual feedback in childhood apraxia. Clinical Linguistics & Phonetics, 30(3–5), 363–381. https://doi.org/10.3109/02699206.2015.1052563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston J. L., McCabe P., Rivera-Campos A., Whittle J. L., Landry E., & Maas E. (2014). Ultrasound visual feedback treatment and practice variability for residual speech sound errors. Journal of Speech, Language, and Hearing Research, 57(6), 2102–2115. https://doi.org/10.1044/2014_JSLHR-S-14-0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redford M. A. (2015). Unifying speech and language in a developmentally sensitive model of production. Journal of Phonetics, 52, 141–152. https://doi.org/10.1016/j.wocn.2015.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers M. A., & Storkel H. L. (1998). Reprogramming phonologically similar utterances: The role of phonetic features in pre-motor encoding. Journal of Speech, Language, and Hearing Research, 41(2), 258–274. https://doi.org/10.1044/jslhr.4102.258 [DOI] [PubMed] [Google Scholar]
- Ruscello D. M., & Shelton R. L. (1979). Planning and self-assessment in articulatory training. Journal of Speech and Hearing Disorders, 44(4), 504–512. https://doi.org/10.1044/jshd.4404.504 [DOI] [PubMed] [Google Scholar]
- Rvachew S., & Brosseau-Lapré F. (2012). Developmental phonological disorders: Foundations of clinical practice. San Diego, CA: Plural. [Google Scholar]
- Sacks S., Flipsen P., & Neils-Strunjas J. (2013). Effectiveness of systematic articulation training program accessing computers (SATPAC) approach to remediate dentalized and interdental /s,z/: A preliminary study. Perceptual and Motor Skills, 117(2), 559–577. https://doi.org/10.2466/24.10.PMS.117x21z2 [DOI] [PubMed] [Google Scholar]
- Schmidt R. A., & Lee T. D. (2011). Motor control and learning: A behavioral emphasis (5th ed.). Champaign, IL: Human Kinetics. [Google Scholar]
- Secord W. A., Boyce S. E., Donohue J. S., Fox R. A., & Shine R. E. (2007). Eliciting sounds: Techniques and strategies for clinicians (2nd ed.). Clifton Park, NY: Thomson Delmar Learning. [Google Scholar]
- Shriberg L. D., Fourakis M., Hall S. D., Karlsson H. B., Lohmeier H. L., McSweeny J. L., … Wilson D. L. (2010). Extensions to the Speech Disorders Classification System (SDCS). Clinical Linguistics & Phonetics, 24(10), 795–824. https://doi.org/10.3109/02699206.2010.503006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg L. D., & Kwiatkowski J. (1982). Phonological disorders. 2. A conceptual framework for management. Journal of Speech and Hearing Disorders, 47(3), 242–256. [DOI] [PubMed] [Google Scholar]
- Shriberg L. D., Strand E. A., Fourakis M., Jakielski K. J., Hall S. D., Karlsson H. B., … Wilson D. L. (2017). A diagnostic marker to discriminate childhood apraxia of speech from speech delay: I. Development and description of the pause marker. Journal of Speech, Language, and Hearing Research. https://doi.org/10.1044/2016_JSLHR-S-15-0296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuster L. I. (1998). The perception of correctly and incorrectly produced /r/. Journal of Speech, Language, and Hearing Research, 41, 941–950. [DOI] [PubMed] [Google Scholar]
- Sjolie G. M., Leece M. C., & Preston J. L. (2016). Acquisition, retention, and generalization of rhotics with and without ultrasound visual feedback. Journal of Communication Disorders, 64, 62–77. https://doi.org/10.1016/j.jcomdis.2016.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skelton S. L., & Hagopian A. L. (2014). Using randomized variable practice in the treatment of childhood apraxia of speech. American Journal of Speech-Language Pathology, 23(4), 599–611. https://doi.org/10.1044/2014_AJSLP-12-0169 [DOI] [PubMed] [Google Scholar]
- Skelton S. L., & Richard J. T. (2016). Application of a motor learning treatment for speech sound disorders in small groups. Perceptual and Motor Skills, 122(3), 840–854. https://doi.org/10.1177/0031512516647693 [DOI] [PubMed] [Google Scholar]
- Tilsen S. (2013). A dynamical model of hierarchical selection and coordination in speech planning. PLOS ONE, 8(4), e62800 https://doi.org/10.1371/journal.pone.0062800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourville J. A., & Guenther F. H. (2011). The DIVA model: A neural theory of speech acquisition and production. Language and Cognitive Processes, 26, 37–41. https://doi.org/10.1080/01690960903498424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vick J., Mental R., Carey H., & Lee G. (2017). Seeing is treating: 3D electromagnetic midsagittal articulography (EMA) visual biofeedback for the remediation of residual speech errors. The Journal of the Acoustical Society of America, 141(5, Pt. 2), 3451–4086. [Google Scholar]
- Young E. C. (1987). The effects of treatment on consonant cluster and weak syllable reduction processes in misarticulating children. Language, Speech, and Hearing Services in Schools, 18(1), 23–33. https://doi.org/10.1044/0161-1461.1801.23 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.