Abstract
Objective:
This study aimed to answer 2 questions: first, to what degree does hospital operative volume affect mortality for adult patients undergoing 1 of 10 common emergency general surgery (EGS) operations? Second, at what hospital operative volume threshold will nearly all patients undergoing an emergency operation realize the average mortality risk?
Background:
Nontrauma surgical emergencies are an underappreciated public health crisis in the United States; redefining where such emergencies are managed may improve outcomes. The field of trauma surgery established regionalized systems of care in part because studies demonstrated a clear relationship between hospital volume and survival for traumatic emergencies. Such a relationship has not been well-studied for nontrauma surgical emergencies.
Methods:
Retrospective cohort study of all acute care hospitals in California performing nontrauma surgical emergencies. We employed a novel use of an ecological analysis with beta regression to investigate the relationship between hospital operative volume and mortality.
Results:
A total of 425 acute care hospitals in California performed 165,123 EGS operations. Risk-adjusted mortality significantly decreased as volume increased for all 10 EGS operations (P < 0.001 for each); the relative magnitude of this inverse relationship differed substantially by procedure. Hospital operative volume thresholds were defined and varied by operation: from 75 cases over 2 years for cholecystectomy to 7 cases for umbilical hernia repair.
Conclusions:
Survival rates for nontrauma surgical emergencies were improved when operations were performed at higher-volume hospitals. The use of ecological analysis is widely applicable to the field of surgical outcomes research.
Keywords: benchmarks, emergency general surgery, high-volume hospitals, nontrauma surgical emergencies, regionalization, volume-to-outcomes
Inadequate timely availability of definitive operative interventions for patients with nontrauma surgical emergencies in the United States has been termed a “crisis” in emergency surgical care (ESC).1–3 The scope of this crisis is on par with major medical conditions considered public health problems, including diabetes mellitus, coronary artery disease, and cancer.4 The lack of access to decisive surgical treatment for readily curable surgical diagnoses has worsened over time, driven by the growing, aging US population and the increasing shortage of surgeons to cover emergency operations.5,6 Multiple surgical and medical organizations in the United States have expressed the need to find solutions to the ESC crisis, but as of now, no consensus decision or recommendation has been made.1–3,7
One potential solution is the complete restructuring of emergency surgical systems of care in the United States, which would include changing how such emergencies are triaged and redefining when and where they are managed. Such a drastic departure from our current systems of delivery for surgical care must be empirically driven, but to date there is little direct evidence to support or initiate such change. It was exactly such evidence that catalyzed the regionalization of trauma surgery 35 years ago, and trauma systems continue to mature, evolve, and be investigated today.8–15
One body of research which helped to validate the creation of regionalized trauma systems was establishing that there is a clear relationship between the volume of trauma patients a hospital treats and its outcomes for those patients.16–18 To date, however, there conflicting studies on the importance of the hospital volume-to-outcomes relationship for emergency general surgery (EGS) operations.19,20 Establishing this relationship could lead to data-driven support for the restructuring and regionalization of the entire system of ESC and potentially improve outcomes.
Volume-outcome relationships have been studied extensively in patients having elective, nonemergent operations. This research has shown that increased hospital operative volume21–27 and increased individual surgeon volume27–29 leads to better outcomes. These relationships have been generalized to exist for emergent operations. This generalization, however, may not be valid, as the EGS patient population is vastly different from its elective counterpart.30,31
This study aimed to answer 2 questions: first, to what degree does hospital operative volume impact mortality for adult patients undergoing 1 of 10 common EGS operations? Second, at what hospital operative volume threshold will nearly all patients undergoing an emergency operation realize the average mortality risk? We hypothesized that increased hospital volume would be associated with decreased mortality across a range of 10 emergency operations, and that this inverse relationship would cross a volume threshold beyond which there was a very high likelihood that an institution was performing at or above the average mortality rate.
METHODS
This study was approved by the Yale University Human Research Protection Program Institutional Review Board for biomedical research, known as the Human Investigation Committee. Because the data were from publicly available, deidentified, administrative datasets, informed consent was not required.
Datasets and Variables
This is a population-based, retrospective cohort study of all adult patients who underwent 1 of 10 EGS operations in the state of California over a 24-month period, from January 1, 2010 to December 31, 2011. Both laparoscopic and open operations were included; trauma operations were excluded. The 10 operations analyzed were appendectomy; cholecystectomy; colectomy; inguinal and femoral hernia repair (analyzed together as 1 type of operation); lysis of adhesions (note by definition no bowel resections were performed in the lysis of adhesion group); necrotizing soft tissue infection (NSTI) resection; repair of perforated peptic ulcer disease [repair of perforated gastric or duodenal ulcers (RPU)]; small bowel resection; umbilical hernia repair; and ventral hernia repair. The 2-year period was chosen as it provided a uniform comparison of operations during which surgical techniques were not greatly changing, and we were more likely to capture events in a 2- versus 1-year window.
Two types of datasets were used. The first were the State Inpatient Databases (SIDs) for California from 2010 and 2011, the most recent years available. The SIDs are part of a family of datasets developed by the Healthcare Cost and Utilization Project, and sponsored by the Agency for Healthcare Research and Quality.32 California was chosen as it is the most populous state in the United States, with a diverse population and geography, with both urban and rural areas represented. Data abstracted included patient demographics, chronic health conditions, hospital-based metrics, and in-hospital mortality. The second dataset was the American Hospital Association (AHA) Annual Survey of Hospitals Database for 2010 and 2011.33 California hospitals in the SID and the AHA were matched, and thus enabling risk adjustment at the hospital level.
For the current analyses, only patients undergoing emergent operations with specific EGS diagnoses were included. International Classification of Disease, 9th Edition (ICD-9), procedural codes (Table 1) were used to identify patients who had undergone 1 of the 10 primary core operations. ICD-9 diagnosis codes (Table 2) identified patients with a specific diagnosis of an EGS condition. Multiple EGS conditions and diagnoses were included, all requiring emergent surgical management. Given the ability to longitudinally track patients within SID, patients were not included more than once for the same operation/condition.
TABLE 1.
ICD-9 Procedure Codes and Descriptions Used to Identify Procedures
| Type of Operation | ICD-9 Procedure Code | ICD-9 Description |
|---|---|---|
| Appendectomy | ||
| 47.09 | Other appendectomy | |
| 47.01 | Laparoscopic appendectomy | |
| Cholecystectomy | ||
| 51.21 | Other partial cholecystectomy | |
| 51.22 | Cholecystectomy | |
| 51.23 | Laparoscopic cholecystectomy | |
| 51.24 | Laparoscopic partial cholecystectomy | |
| Colectomy | ||
| 17.31 | Laparoscopic multiple segmental resection of large intestine | |
| 17.32 | Laparoscopic cecectomy | |
| 17.33 | Laparoscopic right hemicolectomy | |
| 17.34 | Laparoscopic resection of transverse colon | |
| 17.35 | Laparoscopic left hemicolectomy | |
| 17.36 | Laparoscopic sigmoidectomy | |
| 17.39 | Other laparoscopic partial excision of large intestine | |
| 45.71 | Other and open multiple segmental resection of large intestine | |
| 45.72 | Other and open cecectomy | |
| 45.73 | Other and open right hemicolectomy | |
| 45.74 | Other and open resection of transverse colon | |
| 45.75 | Other and open left hemicolectomy | |
| 45.76 | Other and open sigmoidectomy | |
| 45.79 | Other and unspecified partial excision of large intestine | |
| 45.81 | Laparoscopic total intra-abdominal colectomy | |
| 45.82 | Open total intra-abdominal colectomy | |
| 45.83 | Other and unspecified total intra-abdominal colectomy | |
| Inguinal and femoral hernia repair | ||
| 17.11 | Laparoscopic repair of direct inguinal hernia with graft or prosthesis | |
| 17.12 | Laparoscopic repair of indirect inguinal hernia with graft or prosthesis | |
| 17.13 | Laparoscopic repair of inguinal hernia with graft or prosthesis, not otherwise specified | |
| 17.21 | Laparoscopic bilateral repair of direct inguinal hernia with graft or prosthesis | |
| 17.22 | Laparoscopic bilateral repair of indirect inguinal hernia with graft or prosthesis | |
| 17.23 | Laparoscopic bilateral repair of inguinal hernia, one direct and one indirect, with graft or prosthesis | |
| 17.24 | Laparoscopic bilateral repair of inguinal hernia with graft or prosthesis, not otherwise specified | |
| 53.00 | Unilateral repair of inguinal hernia, not otherwise specified | |
| 53.01 | Other and open repair of direct inguinal hernia | |
| 53.02 | Other and open repair of indirect inguinal hernia | |
| 53.03 | Other and open repair of direct inguinal hernia with graft or prosthesis | |
| 53.04 | Other and open repair of indirect inguinal hernia with graft or prosthesis | |
| 53.05 | Unilateral repair of inguinal hernia with graft or prosthesis, not otherwise specified | |
| 53.10 | Bilateral repair of inguinal hernia, not otherwise specified | |
| 53.11 | Other and open bilateral repair of direct inguinal hernia | |
| 53.12 | Other and open bilateral repair of indirect inguinal hernia | |
| 53.13 | Other and open bilateral repair of inguinal hernia, one direct and one indirect | |
| 53.14 | Other and open bilateral repair of direct inguinal hernia with graft or prosthesis | |
| 53.15 | Other and open bilateral repair of indirect inguinal hernia with graft or prosthesis | |
| 53.16 | Other and open bilateral repair of inguinal hernia, one direct and one indirect, with graft or prosthesis | |
| 53.17 | Bilateral inguinal hernia repair with graft or prosthesis, not otherwise specified | |
| 53.21 | Unilateral repair of femoral hernia with graft or prosthesis | |
| 53.29 | Other unilateral femoral hemiorrhaphy | |
| 53.31 | Bilateral repair of femoral hernia with graft or prosthesis | |
| 53.39 | Other bilateral femoral hemiorrhaphy | |
| Lysis of adhesions | ||
| 54.51 | Laparoscopic lysis of peritoneal adhesions | |
| 54.59 | Other lysis of peritoneal adhesions | |
| Necrotizing soft tissue infection debridement | ||
| 54.3 | Excision or destruction of lesion or tissue of abdominal wall or umbilicus | |
| 61.3 | Excision or destruction of lesion or tissue of scrotum | |
| 71.3 | Other local excision or destruction of vulva and perineum | |
| 83.39 | Excision of lesion of other soft tissue | |
| 83.44 | Other fasciectomy | |
| 83.45 | Other myectomy | |
| 86.22 | Excisional debridement of wound, infection, or burn | |
| Repair perforated viscus | ||
| 44.41 | Suture of gastric ulcer site | |
| 44.42 | Suture of duodenal ulcer site | |
| Small bowel resection | ||
| 45.61 | Multiple segmental resection of small intestine | |
| 45.62 | Other partial resection of small intestine | |
| Umbilical hernia repair | ||
| 53.41 | Other and open repair of umbilical hernia with graft or prosthesis | |
| 53.42 | Laparoscopic repair of umbilical hernia with graft or prosthesis | |
| 53.43 | Other laparoscopic umbilical herniorrhaphy | |
| 53.49 | Other open umbilical herniorrhaphy | |
| Ventral hernia repair | ||
| 53.51 | Incisional hernia repair | |
| 53.59 | Repair of other hernia of anterior abdominal wall | |
| 53.61 | Other open incisional hernia repair with graft or prosthesis | |
| 53.62 | Laparoscopic incisional hernia repair with graft or prosthesis | |
| 53.63 | Other laparoscopic repair of other hernia of anterior abdominal wall with graft or prosthesis | |
| 53.69 | Other and open repair of other hernia of anterior abdominal wall with graft or prosthesis |
ICD-9 indicates International Classification of Disease, 9th Edition.
TABLE 2.
ICD-9 Diagnosis Codes and Descriptions Used to Identify Procedures
| Type of Diagnosis | ICD-9 Diagnosis Code | ICD-9 Description |
|---|---|---|
| Appendicitis diagnoses | ||
| 540.0 | Acute appendicitis with generalized peritonitis | |
| 540.9 | Acute appendicitis without mention of peritonitis | |
| 541 | Appendicitis, unqualified | |
| 542 | Other appendicitis | |
| 540.1 | Acute appendicitis with peritoneal abscess | |
| Cholecystitis diagnoses | ||
| 574.00 | Calculus of gallbladder with acute cholecystitis, without mention of obstruction | |
| 574.01 | Calculus of gallbladder with acute cholecystitis and obstruction | |
| 574.10 | Calculus of gallbladder with other cholecystitis, without mention of obstruction | |
| 574.11 | Calculus of gallbladder with other cholecystitis and obstruction | |
| 574.30 | Calculus of bile duct with acute cholecystitis without mention of obstruction | |
| 574.31 | Calculus of bile duct with acute cholecystitis and obstruction | |
| 574.40 | Calculus of bile duct with other cholecystitis, without mention of obstruction | |
| 574.41 | Calculus of bile duct with other cholecystitis and obstruction | |
| 574.60 | Calculus of gallbladder and bile duct with acute cholecystitis, without mention of obstruction | |
| 574.61 | Calculus of gallbladder and bile duct with acute cholecystitis, with obstruction | |
| 574.70 | Calculus of gallbladder and bile duct with other cholecystitis, without mention of obstruction | |
| 574.71 | Calculus of gallbladder and bile duct with other cholecystitis, with obstruction | |
| 574.80 | Calculus of gallbladder and bile duct with acute and chronic cholecystitis, without mention of obstruction | |
| 574.81 | Calculus of gallbladder and bile duct with acute and chronic cholecystitis, with obstruction | |
| 575.0 | Acute cholecystitis | |
| 575.1 | Other cholecystitis | |
| 575.10 | Cholecystitis, unspecified | |
| 575.11 | Chronic cholecystitis | |
| 575.12 | Acute and chronic cholecystitis | |
| Colon diagnosis | ||
| 008.45 | Intestinal infections due to Clostridium difficile | |
| 557.0 | Acute vascular insufficiency of intestine | |
| 557.9 | Unspecified vascular insufficiency of intestine | |
| 560.0 | Intussusception | |
| 560.1 | Paralytic ileus | |
| 560.2 | Volvulus | |
| 562.11 | Diverticulitis of colon (without mention of hemorrhage) | |
| 562.12 | Diverticulosis of colon with hemorrhage | |
| 562.13 | Diverticulitis of colon with hemorrhage | |
| 564.7 | Megacolon, other than Hirschsprung’s | |
| 564.9 | Unspecified functional disorder of intestine | |
| 567.21 | Peritonitis (acute) generalized | |
| 567.22 | Peritoneal abscess | |
| 567.29 | Other suppurative peritonitis | |
| 578.1 | Blood in stool | |
| 578.9 | Unspecified, hemorrhage of gastrointestinal tract | |
| Inguinal and femoral hernia diagnoses | ||
| 550.00 | Inguinal hernia with gangrene, unilateral or unspecified (not specified as recurrent) | |
| 550.01 | Inguinal hernia with gangrene, recurrent unilateral or unspecified inguinal hernia | |
| 550.02 | Inguinal hernia with gangrene, bilateral | |
| 550.03 | Inguinal hernia with gangrene, recurrent bilateral | |
| 550.10 | Inguinal hernia with obstruction, without mention of gangrene, unilateral or unspecified | |
| (not specified as recurrent) | ||
| 550.11 | Inguinal hernia with obstruction, without mention of gangrene, recurrent unilateral or unspecified | |
| 550.12 | Inguinal hernia with obstruction, without mention gangrene, bilateral (not specified as recurrent) | |
| 550.13 | Inguinal hernia with obstruction, without mention of gangrene, recurrent bilateral | |
| 551.00 | Femoral hernia with gangrene, unilateral or unspecified (not specified as recurrent) | |
| 551.01 | Femoral hernia with gangrene, recurrent unilateral or unspecified | |
| 551.02 | Femoral hernia with gangrene, bilateral (not specified as recurrent) | |
| 551.03 | Femoral hernia with gangrene, recurrent bilateral | |
| 552.00 | Unilateral or unspecified femoral hernia with obstruction | |
| 552.01 | Recurrent unilateral or unspecified femoral hernia with obstruction | |
| 552.02 | Bilateral femoral hernia with obstruction | |
| 552.03 | Recurrent bilateral femoral hernia with obstruction | |
| Lysis of adhesions diagnoses | ||
| 560.81 | Intestinal or peritoneal adhesions with obstruction (postoperative) (postinfection) | |
| 567.21 | Peritonitis (acute) generalized | |
| 567.22 | Peritoneal abscess | |
| 567.29 | Other suppurative peritonitis | |
| 568.0 | Peritoneal adhesions (postoperative) (postinfection) | |
| 789.0 | Abdominal pain | |
| 789.00 | Abdominal pain, unspecified site | |
| 789.01 | Abdominal pain, right upper quadrant | |
| 789.02 | Abdominal pain, left upper quadrant | |
| 789.03 | Abdominal pain, right lower quadrant | |
| 789.04 | Abdominal pain, left lower quadrant | |
| 789.05 | Abdominal pain, periumbilic | |
| 789.06 | Abdominal pain, epigastric | |
| 789.07 | Abdominal pain, generalized | |
| 789.09 | Abdominal pain, other specified site | |
| 789.3 | Abdominal or pelvic swelling, mass, or lump | |
| 789.30 | Abdominal or pelvic swelling, mass or lump, unspecified site | |
| 789.31 | Abdominal or pelvic swelling, mass, or lump, right upper quadrant | |
| 789.32 | Abdominal or pelvic swelling, mass, or lump, left upper quadrant | |
| 789.33 | Abdominal or pelvic swelling, mass, or lump, right lower quadrant | |
| 789.34 | Abdominal or pelvic swelling, mass, or lump, left lower quadrant | |
| 789.35 | Abdominal or pelvic swelling, mass or lump, periumbilic | |
| 789.36 | Abdominal or pelvic swelling, mass, or lump, epigastric | |
| 789.37 | Abdominal or pelvic swelling, mass, or lump, epigastric, generalized | |
| 789.39 | Abdominal or pelvic swelling, mass, or lump, other specified site | |
| 789.4 | Abdominal rigidity | |
| 789.40 | Abdominal rigidity, unspecified site | |
| 789.41 | Abdominal rigidity, right upper quadrant | |
| 789.42 | Abdominal rigidity, left upper quadrant | |
| 789.43 | Abdominal rigidity, right lower quadrant | |
| 789.44 | Abdominal rigidity, left lower quadrant | |
| 789.45 | Abdominal rigidity, periumbilic | |
| 789.46 | Abdominal rigidity, epigastric | |
| 789.47 | Abdominal rigidity, generalized | |
| 789.49 | Abdominal rigidity, other specified site | |
| 789.60 | Abdominal tenderness, unspecified site | |
| 789.61 | Abdominal tenderness, right upper quadrant | |
| 789.62 | Abdominal tenderness, left upper quadrant | |
| 789.63 | Abdominal tenderness, right lower quadrant | |
| 789.64 | Abdominal tenderness, left lower quadrant | |
| 789.65 | Abdominal tenderness, periumbilic | |
| 789.66 | Abdominal tenderness, epigastric | |
| 789.67 | Abdominal tenderness, generalized | |
| 789.69 | Abdominal tenderness, other specified site | |
| Necrotizing soft tissue infections | ||
| 728.86 | Necrotizing fasciitis | |
| 729.4 | Unspecified fasciitis | |
| 785.4 | Gangrene | |
| Repair perforated viscus diagnoses | ||
| 531.00 | Acute gastric ulcer with hemorrhage, without mention of obstruction | |
| 531.01 | Acute gastric ulcer with hemorrhage and obstruction | |
| 531.10 | Acute gastric ulcer with perforation, without mention of obstruction | |
| 531.11 | Acute gastric ulcer with perforation and obstruction | |
| 531.20 | Acute gastric ulcer with hemorrhage and perforation, without mention of obstruction | |
| 531.21 | Acute gastric ulcer with hemorrhage, perforation, and obstruction | |
| 531.40 | Chronic or unspecified gastric ulcer with hemorrhage, without mention of obstruction | |
| 531.41 | Chronic or unspecified gastric ulcer with hemorrhage and obstruction | |
| 531.50 | Chronic or unspecified gastric ulcer with perforation, without mention of obstruction | |
| 531.51 | Chronic or unspecified gastric ulcer with perforation and obstruction | |
| 531.60 | Chronic or unspecified gastric ulcer with hemorrhage and perforation, without mention of obstruction | |
| 531.61 | Chronic or unspecified gastric ulcer with hemorrhage, perforation, and obstruction | |
| 532.00 | Acute duodenal ulcer with hemorrhage, without mention of obstruction | |
| 532.01 | Acute duodenal ulcer with hemorrhage and obstruction | |
| 532.10 | Acute duodenal ulcer with perforation, without mention of obstruction | |
| 532.11 | Acute duodenal ulcer with perforation and obstruction | |
| 532.20 | Acute duodenal ulcer with hemorrhage and perforation, without mention of obstruction | |
| 532.21 | Acute duodenal ulcer with hemorrhage, perforation, and obstruction | |
| 532.40 | Chronic or unspecified duodenal ulcer with hemorrhage, without mention of obstruction | |
| 532.41 | Chronic or unspecified duodenal ulcer with hemorrhage and obstruction | |
| 532.50 | Chronic or unspecified duodenal ulcer with perforation, without mention of obstruction | |
| 532.51 | Chronic or unspecified duodenal ulcer with perforation and obstruction | |
| 532.60 | Chronic or unspecified duodenal ulcer with hemorrhage and perforation, without mention of obstruction | |
| 532.61 | Chronic or unspecified duodenal ulcer with hemorrhage, perforation, and obstruction | |
| 533.00 | Acute peptic ulcer, unspecified site, with hemorrhage, without mention of obstruction | |
| 533.01 | Acute peptic ulcer, unspecified site, with hemorrhage and obstruction | |
| 533.10 | Acute peptic ulcer, unspecified site, with perforation, without mention of obstruction | |
| 533.11 | Acute peptic ulcer, unspecified site, with perforation and obstruction | |
| 533.20 | Acute peptic ulcer, unspecified site, with hemorrhage and perforation, without mention of obstruction | |
| 533.21 | Acute peptic ulcer, unspecified site, with hemorrhage, perforation, and obstruction | |
| 533.40 | Chronic or unspecified peptic ulcer, unspecified site, with hemorrhage, without mention of obstruction | |
| 533.41 | Chronic or unspecified peptic ulcer, unspecified site, with hemorrhage and obstruction | |
| 533.50 | Chronic or unspecified peptic ulcer, unspecified site, with perforation, without mention of obstruction | |
| 533.51 | Chronic or unspecified peptic ulcer, unspecified site, with perforation and obstruction | |
| 533.60 | Chronic or unspecified peptic ulcer, unspecified site, with hemorrhage and perforation, without mention of obstruction | |
| 533.61 | Chronic or unspecified peptic ulcer, unspecified site, with hemorrhage, perforation, and obstruction | |
| 534.00 | Acute gastrojejunal ulcer with hemorrhage, without mention of obstruction | |
| 534.01 | Acute gastrojejunal ulcer, with hemorrhage and obstruction | |
| 534.10 | Acute gastrojejunal ulcer with perforation, without mention of obstruction | |
| 534.11 | Acute gastrojejunal ulcer with perforation and obstruction | |
| 534.20 | Acute gastrojejunal ulcer with hemorrhage and perforation, without mention of obstruction | |
| 534.21 | Acute gastrojejunal ulcer with hemorrhage, perforation, and obstruction | |
| 534.40 | Chronic or unspecified gastrojejunal ulcer with hemorrhage, without mention of obstruction | |
| 534.41 | Chronic or unspecified gastrojejunal ulcer, with hemorrhage and obstruction | |
| 534.50 | Chronic or unspecified gastrojejunal ulcer with perforation, without mention of obstruction | |
| 534.51 | Chronic or unspecified gastrojejunal ulcer with perforation and obstruction | |
| 534.60 | Chronic or unspecified gastrojejunal ulcer with hemorrhage and perforation, without mention of obstruction | |
| 534.61 | Chronic or unspecified gastrojejunal ulcer with hemorrhage, perforation, and obstruction | |
| Small bowel diagnoses | ||
| 555.0 | Regional enteritis of small intestine | |
| 555.1 | Regional enteritis of large intestine | |
| 555.2 | Regional enteritis of small intestine with large intestine | |
| 555.9 | Regional enteritis of unspecified site | |
| 557.0 | Acute vascular insufficiency of intestine | |
| 557.9 | Unspecified vascular insufficiency of intestine | |
| 560.0 | Intussusception | |
| 560.1 | Paralytic ileus | |
| 560.2 | Volvulus | |
| 560.3 | Impaction of intestine | |
| 560.30 | Unspecified impaction of intestine | |
| 560.31 | Gallstone ileus | |
| 560.39 | Other impaction of intestine | |
| 560.8 | Other specified intestinal obstruction | |
| 560.81 | Intestinal or peritoneal adhesions with obstruction (postoperative) (postinfection) | |
| 560.89 | Other specified intestinal obstruction | |
| 560.9 | Unspecified intestinal obstruction | |
| 562.01 | Diverticulitis of small intestine (without mention of hemorrhage) | |
| 562.02 | Diverticulosis of small intestine with hemorrhage | |
| 562.03 | Diverticulitis of small intestine with hemorrhage | |
| 567.21 | Peritonitis (acute) generalized | |
| 567.22 | Peritoneal abscess | |
| 567.29 | Other suppurative peritonitis | |
| 568.0 | Peritoneal adhesions (postoperative) (postinfection) | |
| 578.0 | Hematemesis | |
| Umbilical hernia diagnoses | ||
| 551.1 | Umbilical hernia with gangrene | |
| 552.1 | Umbilical hernia with obstruction | |
| Ventral hernia diagnoses | ||
| 551.2 | Ventral hernia with gangrene | |
| 551.20 | Unspecified ventral hernia with gangrene | |
| 551.21 | Incisional ventral hernia, with gangrene | |
| 551.29 | Other ventral hernia with gangrene | |
| 551.3 | Diaphragmatic hernia with gangrene | |
| 551.8 | Hernia of other specified sites, with gangrene | |
| 551.9 | Hernia of unspecified site, with gangrene | |
| 552.20 | Unspecified ventral hernia with obstruction | |
| 552.21 | Incisional hernia with obstruction | |
| 552.29 | Other ventral hernia with obstruction | |
| 552.3 | Diaphragmatic hernia with obstruction | |
| 552.8 | Hernia of other specified site, with obstruction | |
| 552.9 | Hernia of unspecified site, with obstruction |
ICD-9 indicates International Classification of Disease, 9th Edition.
The patient populations were chosen as they are among most prevalent emergent surgical diagnoses requiring operative intervention in the United States, and have a nontrivial risk of postoperative morbidity and mortality.31,34,35 An emergency operation was defined within the dataset using the SID emergency operation qualifier. This is done when an operation is performed emergently/urgently.
Transfer status of the patient to and from another acute care hospital was incorporated into our inclusion/exclusion criteria. This is important, because there is evidence that in patients with time-sensitive surgical emergencies, transferred patients have poorer outcomes than those not transferred.36,37 For patients who were emergently operated on at 1 hospital and later transferred out to a second hospital, mortality was attributed to the transferring/primary hospital; this is consistent with public reporting of mortality rates.38
Hospital volume was calculated per operation and was defined as the total number of each type of operation performed at each acute care hospital over the 2-year period, in patients with the defined diagnoses of interest. Dedicated pediatric hospitals and dedicated rehabilitation hospitals were excluded from our analysis as such hospitals do not have expertise in or practice operating on adult emergency surgery patients. For each of the 10 types of emergent operations, any hospital that performed 2 or fewer of those operations over the 2 years was excluded from the analyses. We rationalized that hospitals doing an average of 1 emergent type of operation per year were not representative of the hospital types of interest. Operative mortality was defined as a death during the index inpatient hospitalization.
Statistical Analyses and Outcome Measures
Unit of Analysis
Our first research question assessed to what degree hospital operative volume affects hospital mortality rates for a specified operation. We performed ecological analysis based on the hospital, not the patient, as the unit of analysis. An ecological analysis is the proper approach for a study of the relationship between a hospital-level risk factor (volume) and a hospital-level incidence rate (mortality),39 that is, for a study of the effects of contextual risk factors on contextual outcomes (see Discussion section for more on this).
Statistical Modeling
We employed beta-logistic generalized linear regression40 to examine the relationship between hospital volume and emergency operative mortality, with adjustment for both patient case mix and other hospital characteristics. The primary outcome measure was the proportion of in-hospital mortality, defined for each operation as the number of patients who died after undergoing the operation divided by all patients undergoing the operation at that hospital over the 2 years. Mortality proportion data typically exhibit a sigmoidal, or S-shaped, curve with asymptotes at the limits of zero and one when plotted against a predictor. In general, ordinary regression does not capture this relationship, whereas a generalized linear model using the beta distribution and logit link function does capture this relationship. The beta distribution supports a range from zero to one, and the logit link ensures that the predicted mean stays within bounds (0, 1). Our model regressed the mortality proportion at each hospital on the natural logarithm of the hospital volume plus hospital-level characteristics as covariates to adjust for variation in case-mix across hospitals.
The natural logarithm transformation of volume, as opposed to actual volume alone, was used in our model for the predictor. One reason this transformation was chosen is because the logit is the canonical link function for the beta regression, and therefore both the predictor of interest (hospital volume) and the outcome of interest (proportion of mortality expressed as the odds of mortality) would both be on the natural log scale. Secondly, from a practical interpretation standpoint, the hospital volume is believed to have a multiplicative rather than an additive effect. An additive effect would represent the difference of 10 between hospitals with volumes of 5 and 15 procedures (3 times as large) as the same as having a difference of 10 between hospitals with volumes of 100 and 110 procedures (1.1 times as large).
Adjustment for Covariates
We included patient characteristics as hospital-level means or percentages to serve as covariates in the models that adjust for case-mix differences between hospitals. These included mean age, mean Elixhauser-van Walraven comorbidity index, sex, race, and payer status. The Elixhauser-van Walraven is a validated, weighted measure of a person’s chronic disease burden.41 Coexisting conditions were identified using ICD-9 diagnosis codes, which were then compiled into an Elixhauser-van Walraven comorbidity index. Both unadjusted and risk-adjusted multivariable models were tested to predict in-hospital mortality; ratios represented the effects of hospital volume on survival proportion.
Model Goodness-of-fit Statistics
For the beta regression model of each operation, we calculated a pseudo-R2 statistic42 to calibrate the generalized linear model analog to the linear regression R2 statistic (the proportion of the variance of the dependent variable explained by the model predictor of interest with covariates).
Descriptive Comparison of Patients by Survival Status
Patient-level characteristics were first compared using bivariate techniques between those who died and those who survived. Chi-squared (χ2) tests were used to compare differences in proportions of categorical variables; such data were summarized by frequencies with percentages. Group means were compared using t tests for normally distributed continuous variables; such data were summarized by mean values with standard deviations (±SD). Hospital-level characteristics (trauma center status; high technology capability; medical school affiliation) were evaluated and presented as frequencies with percentages. Trauma center status is based on American College of Surgeons Committee on Trauma verified level 1 or level 2 trauma centers.43 High-technology patient management capability was defined as hospitals which perform at least 1 of the following 3 types of major operations: adult open heart surgery and/or major heart or liver organ transplantation.33,44 The high technology variable captures a hospital’s perioperative acute care capabilities, because these 3 major operations demand intense levels of acute perioperative care, including often admission to an intensive care unit; given that it was highly correlated with other potential acute care capability variables in the AHA dataset (such as: total number of ICU beds; having any ICU beds; intensivists providing care) coupled with the fact that these other variables were missing from nearly 25% of hospitals, we only included high tech in the final model. Medical school affiliation was based on the hospital being a teaching hospital for an accredited medical school.45
Volume Thresholds
Our second research question asked at what hospital operative volume would patients undergoing an emergency operation realize average mortality risk. For each EGS operation, this volume threshold was analyzed using the results of the beta-regression models. The threshold was defined as the hospital operative volume above which 95% of the remaining hospitals were performing at or above the average mortality rate. By this construct, if a patient were to have an operation at a hospital with an EGS operative volume for that specific surgery greater than the volume threshold, there would be a 95% chance that that patient’s mortality risk (as defined by hospital mortality proportion) would be lower than the average risk-adjusted mortality for all hospitals performing that same EGS operation. Average mortality risk was defined by operation as the mean in-hospital risk-adjusted mortality for each EGS operation.
General Statistical Considerations
A P value of less than 0.05 was defined as significant. All statistical analyses were conducting using SAS 9.4 (SAS Institute Inc, Cary, NC).
RESULTS
At 425 acute care hospitals in California, a total of 165,123 patients underwent EGS operations (Table 3). Overall unadjusted mortality rate was 2%, although it varied significantly by operation, from less than 1.0% for appendectomy to 14% for RPU. Relative to the nondecedents, the decedents were more likely to be women, white, older, and on Medicare (Table 3). Further breakdown of patient level characteristics, by operation, are found in the supplementary online material, Appendix A, http://links.lww.com/SLA/B591.
TABLE 3.
Patient Characteristics*
| Variable† | Survived | Died | P‡ |
|---|---|---|---|
| Total number patients | 161935 | 3188 | - |
| Female sex | 89564 (57.8%) | 1674 (52.5%) | <0.001 |
| Race and ethnicity: | <0.001 | ||
| White | 71791 (50.5%) | 1966 (63.6%) | - |
| Black | 7189 (5.1%) | 237 (7.7%) | - |
| Non-black, Non-white | 11858 (8.3%) | 281 (9.1%) | - |
| Hispanic | 51413 (36.1%) | 609 (19.7%) | - |
| Age, y | 49.6 (19.5) | 73.2 (14.0) | <0.001 |
| Comorbidities, van Walraven score | 2.0 (5.6) | 13.5 (8.4) | <0.001 |
| Payor source | <0.001 | ||
| Medicare | 40709 (25.1%) | 2354 (73.8%) | - |
| Medicaid | 31005 (19.1%) | 385 (12.1%) | - |
| Private insurance | 63291 (39.1%) | 339 (10.6%) | - |
| Self pay or other | 26910 (16.6%) | 110 (3.5%) | - |
This table presents overall patient characteristics; for patient characteristics by operation type, see Supplementary Online Material, Appendix A; note that the number totals for “Race and ethnicity” and “Payor source” fall short of the survived and died totals for each column because of the missing individual data on those variables.
Categorical variables are presented as number (%); continuous data are presented as mean (standard deviation).
P values for overall tests of differences are from χ2 for categorical variables and t-test for continuous variables.
The 3 highest volume operations were cholecystectomy (69,052), appendectomy (52,905), and colectomy (12,574). The 3 lowest volume operations were umbilical hernia repair (1737), RPU (2231), and excision of NSTI (2616). Of the 425 acute care hospitals in California, the number meeting our inclusion criterion performing emergent operations ranged from 209 doing umbilical hernia repairs to 310 doing cholecystectomies. Further breakdown of hospital level characteristics by operation are found in the supplementary online material, Appendix B, http://links.lww.com/SLA/B591.
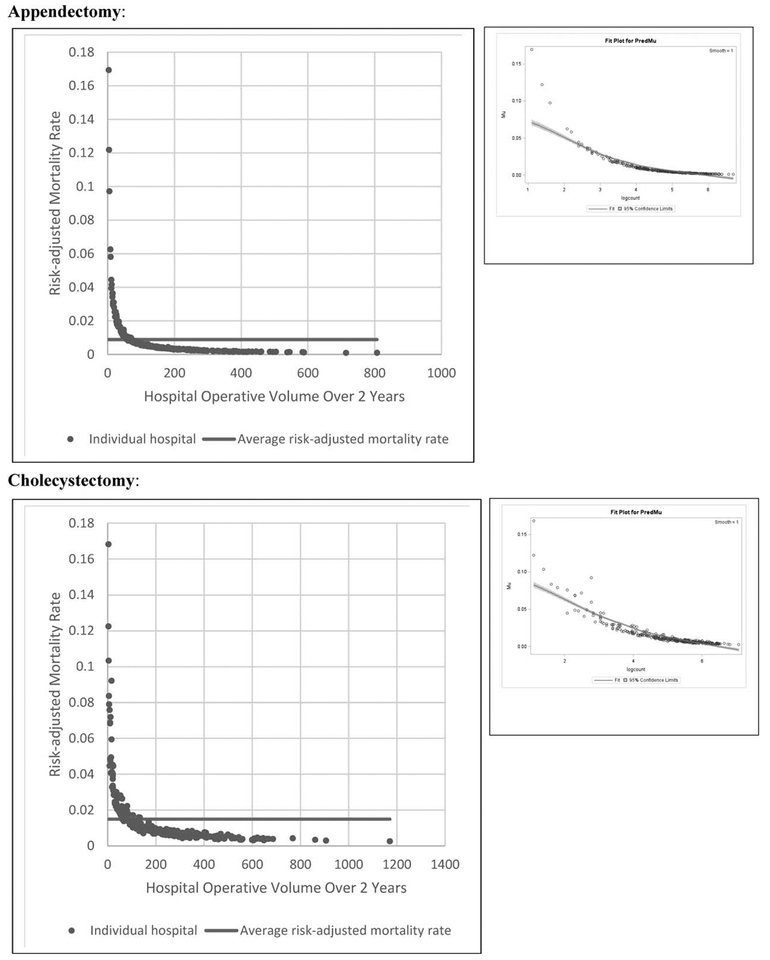
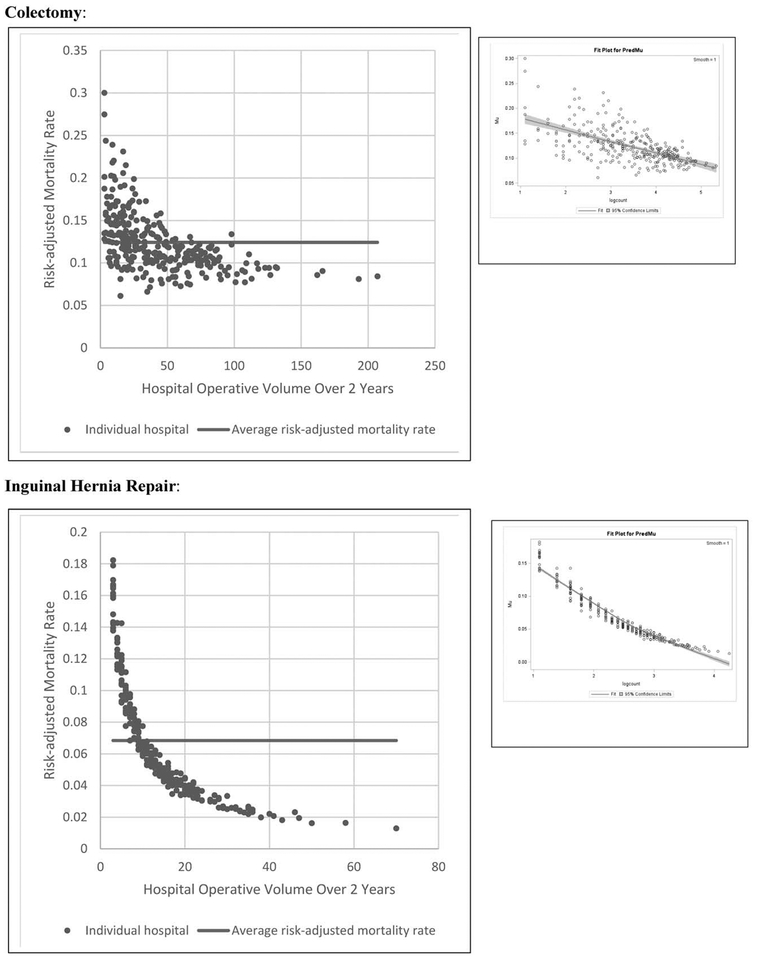
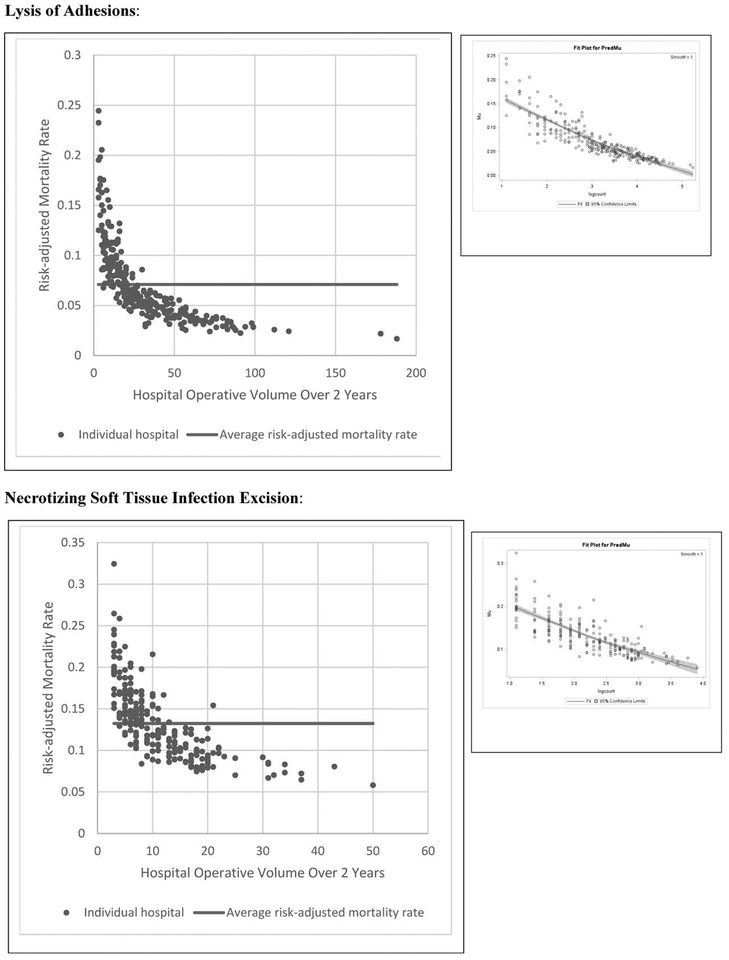
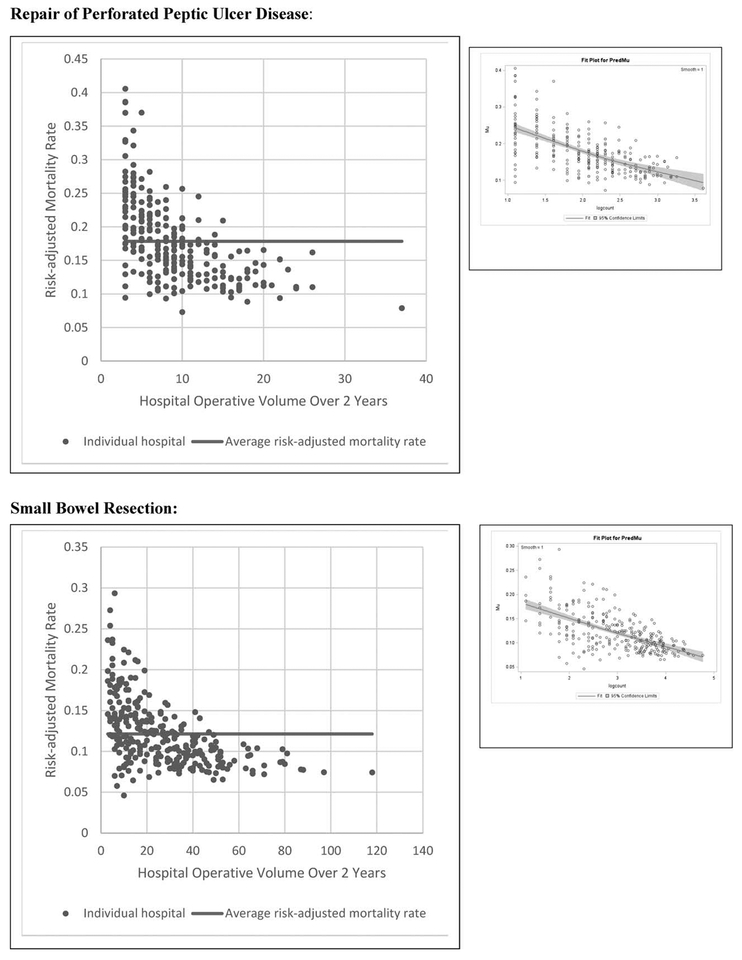
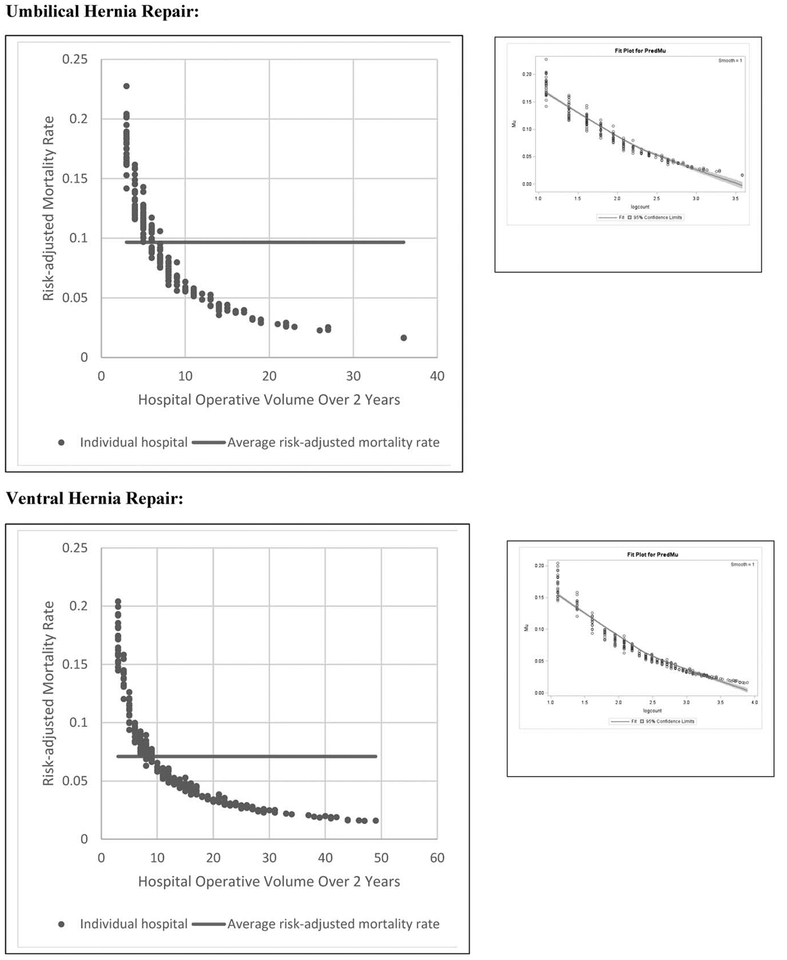
Multivariable beta regression models confirmed that risk-adjusted mortality significantly decreased as volume increased for all 10 EGS operations; the relative magnitude of this inverse relationship varied substantially by procedure (Table 4). Even with operations that have a lower risk of mortality (<2%), there remained a survival benefit to having the operation done at a higher volume hospital. The inverse volume to mortality relationship is shown graphically in the fit plots for all 10 operations (Fig. 1). In nearly every figure, the high-volume hospitals begin to cluster together, indicating less variability and higher precision, whereas at the lower volume hospitals there is wide variation of outcome. In terms of model fit, each operation’s beta regression pseudo R2 was excellent, ranging from 0.26 for NSTI to 0.93 for appendectomy. Full results of beta regression by operation, including hospital-level and patient-level covariates that were significantly associated with death, are found in the supplementary online material, Appendix C, http://links.lww.com/SLA/B591.
TABLE 4.
Beta Regression Estimates of the Decrease in Hospital Mortality Proportion When Natural Log of Hospital Volume Is Increased by 1, by Operation*
| Operation | Adjusted Model | |||
|---|---|---|---|---|
| Estimate | 95% LL | 95% UL | P† | |
| Appendectomy | 0.41 | 0.39 | 0.43 | <0.001 |
| Cholecystectomy | 0.50 | 0.47 | 0.54 | <0.001 |
| Colectomy | 0.77 | 0.70 | 0.86 | <0.001 |
| Inguinal and femoral hernia | 0.44 | 0.40 | 0.48 | <0.001 |
| Lysis of adhesions | 0.55 | 0.49 | 0.62 | <0.001 |
| Necrotizing soft tissue infection excision | 0.64 | 0.55 | 0.73 | <0.001 |
| Repair of perforated peptic ulcer disease | 0.66 | 0.57 | 0.76 | <0.001 |
| Small bowel resection | 0.76 | 0.68 | 0.86 | <0.001 |
| Umbilical hernia | 0.36 | 0.33 | 0.40 | <0.001 |
| Ventral hernia | 0.41 | 0.38 | 0.44 | <0.001 |
LL indicates lower limit; UL, upper limit.
Estimates of the decrease in hospital mortality proportion when natural log of hospital volume is increased by 1. To interpret this from an operative volume standpoint, one must transform the natural log integer into a hospital operative volume. The natural log integer can be back-converted to an actual operative volume like this: 2 = ln(x) −> x = e2 = 7.4 operations; 3 = ln(x) −> x = e3 = 20.1 operations; 4 = ln(x) −> x = e4 = 54.6 operations; and so on. In terms of operative volume, a +1 unit change in natural log from 2 to 3 (+12.7 operations) is not equivalent to the change from 3 to 4 (+34.5 operations). However, the predicted change in mortality is equivalent over the same interval. For example, a +1 unit change in natural log from 2 to 3 or from 3 to 4 for appendectomy will decrease morality by the same 61% (as defined in the table) over each interval. By comparison, a +1 unit change in natural log from 2 to 3 or from 3 to 4 for cholecystectomy will decrease morality by 49% over each interval. To summarize, the increase in operative volume from a +1 unit increase in natural log is the same for each operation; what is different between operations is the resultant decrease in mortality.
P value <0.05 is significant.
FIGURE 1.
Two beta fit plots for each of the 10 emergency general surgery operations. The left plot shows the inverse volume to mortality relationship: the x-axis is hospital operative volume over 2 years, the y-axis is risk-adjusted hospital mortality rate, the average risk-adjusted mortality is represented by the flat line, and every dot represents an individual hospital. The right plot is the relationship modeled in our beta regression analyses: the x-axis is natural log-transformed hospital operative volume, the y-axis is risk-adjusted hospital mortality rate, and every dot represents an individual hospital.
The hospital operative volume thresholds at which there was a 95% chance that that institution performed at or above the average risk-adjusted mortality rate varied by operation (Table 5), from 75 cases for cholecystectomy to 7 cases for umbilical hernia repair. The number of operations performed at these below-threshold institutions also varied, from 4% of all cases for appendectomy and cholecystectomy, to 57% of the operations for RPU. The number of hospitals failing to meet these threshold mortality standards varied by operation type, from 25% of all hospitals for appendectomy and 24% for cholecystectomy, to 78% of institutions for RPU.
TABLE 5.
Hospital Operative Volume Threshold Analysis
| Operation | Average Risk-adjusted Mortality, % | Hospital Volume Threshold With 95% Chance of Being Better Than Average Mortality* | Total Number Hospitals | Percentage of Hospitals Not Achieving Volume Threshold, % | Total Operative Volume | Number of Operations Performed at Hospitals Below Volume Threshold | Percentage of Operations at Hospitals Below Volume Threshold, % |
|---|---|---|---|---|---|---|---|
| Appendectomy | 0.9 | 61 | 305 | 25 | 52,905 | 2285 | 4 |
| Cholecystectomy | 1.5 | 75 | 310 | 24 | 69,052 | 2668 | 4 |
| Colectomy | 12.4 | 50 | 292 | 66 | 12,574 | 4423 | 35 |
| Inguinal and femoral hernia | 6.8 | 9 | 265 | 34 | 3757 | 483 | 13 |
| Lysis of adhesions | 7.1 | 19 | 292 | 38 | 9343 | 1110 | 12 |
| Necrotizing soft tissue infection excision | 13.2 | 11 | 228 | 55 | 2616 | 767 | 29 |
| Repair of perforated peptic ulcer disease | 17.8 | 13 | 245 | 78 | 2231 | 1267 | 57 |
| Small bowel resection | 12.1 | 37 | 280 | 73 | 7447 | 3450 | 46 |
| Umbilical hernia | 9.7 | 7 | 209 | 51 | 1737 | 470 | 27 |
| Ventral hernia | 7.1 | 10 | 259 | 46 | 3461 | 732 | 21 |
Hospital operative volume that optimizes probability of survival for a given operation, defined as the 2-year volume above which 95% of hospitals have better than average risk-adjusted mortality.
DISCUSSION
Mortality risk was significantly lower at higher-volume acute care hospitals in California compared to lower-volume hospitals for all 10 emergent EGS operations over the 2-year study. Increased operative volume independently translated into improved probability of survival, regardless of the baseline mortality risk of the operation. Consistent with our primary hypothesis, hospital operative volume is a statistically significant predictor of outcome for all EGS operations.
The data also indicate that at relatively low hospital operative volume thresholds, patients can realize at or better than average survival benefit. This threshold level, which was different for each operation, provides an objective mortality benchmark for these common EGS operations, at which there is 95% chance that that institution performed at or above the average risk-adjusted mortality rate. Although there are outliers at both ends of the spectrum, from exceptionally high-survival rate hospitals to low-survival rate hospitals, most, though not all, hospitals performing EGS operations have good outcomes. For appendectomy and cholecystectomy among the most common operations in adults in the US—1 out of every 4 hospitals in California (~25%) fail to meet the volume threshold to achieve the average mortality standard, although only 4% of patients underwent these operations at below benchmark institutions. At the other end of the spectrum is RPU, for which 3 out of 4 hospitals (~75%) fail to meet the average mortality standard; 57% of patients underwent RPU at below benchmark institutions.
Overall, these results confirm that hospital operative volume is an important metric of surgical quality in the field of EGS. For many surgical disciplines, the American College of Surgeons’ (ACS) Quality Programs46 use hospital volume as a fundamental criterion that institutions must meet for accreditation as a verified surgery center. For example, to become an ACS and American Society for Metabolic and Bariatric Surgery certified “Comprehensive Center” in metabolic and bariatric surgery, a hospital must perform at least 50 operations per year.47 For a hospital to secure certification as an ACS Committee on Trauma certified level I trauma center, it must admit at least 1200 trauma patients yearly, or have 240 admissions with an Injury Severity Score of more than 15.43 And for a medical center to meet criteria as an ACS level I Pediatric Surgery Center, it must perform at least 1000 surgical procedures per year on children.48
By quantifying the hospital operative volume at which mortality reaches a volume threshold (Table 5) for each of the most common EGS operations, this study has defined levels of hospital volume which could be used as a quality standard benchmark to improve survival for these cases. Although using hospital volume as a basis for surgical quality is not without its detractors,49 this may prove to be important moving forward, as the field of EGS considers implementation of a verification review process and accreditation of medical centers for surgical emergencies.
Studies within the field of trauma surgery have shown that there is a clear relationship between hospital volume and outcomes for trauma patients.16–18 This body of research has helped to validate the creation of regionalized trauma care, within set trauma systems. Based on the current study of EGS operations, hospital operative volume is also a key determinant of the variation in hospital performance for EGS operations. To lessen the negative impact of the wide variation in survival outcomes at lower volume hospitals, EGS patients may equally benefit from a formal system of emergency surgical care that consolidates operative emergencies to higher volume centers.
Although mortality outcomes at the lowest volume hospitals in our study are generally poor, for certain EGS operations (colectomy; excision of NSTIs; repair of perforated peptic ulcers; small bowel resection) a small subset of the lower volume hospitals do have acceptable, below-average mortality rates. As has been shown in the elective surgical literature,50 this may reflect system-level hospital characteristics that have a strong influence on improving survival despite the lower operative volume. Therefore, a more complete understanding of why these lower volume institutions have below-average mortality is needed before restricting where patients undergo EGS operations.
Variation in surgical mortality is a truly multidimensional construct, and hospital operative volume is just 1 determinant of postoperative mortality. While the current study was only able to assess a few system-level hospital characteristics (trauma center status; high technology capability; medical school affiliation), future in-depth qualitative investigations are needed to broadly investigate all potential factors influencing mortality variation in EGS patients. We suspect that system-level factors such as EGS-specific processes of care, process compliance, quality improvement structure, selective referral, consultation patterns, interdisciplinary teamwork, and organizational culture are key factors that contribute to high-quality EGS outcomes. These potentially lifesaving system-level characteristics can be assessed utilizing qualitative methods, and can in turn inform subsequent quantitative research that would then evaluate for the most significant determinants. Armed with these determinants, we can then develop EGS management guidelines and criteria for accreditation of medical centers for surgical emergencies. Without such information, these factors will continue to go unmeasured and underappreciated in quantitative EGS analyses using standard datasets.
Although many factors predicting poor outcomes in EGS patients cannot be altered before operative intervention—age, comorbidities, inflammatory state—the current study defines one metric that can be optimized: hospital volume. In this manner, akin to trauma patients, the trajectory of outcomes in EGS patients may be defined just as much preoperatively as intraoperatively or postoperatively. This would make sense, as EGS patients often have profound physiologic abnormalities entering the operating room, and as such are more closely comparable to trauma patients than they are to elective general surgery patients.30,31
Unlike elective general surgery, where patients can choose their surgeon ahead of an operation, this is rarely the case in unplanned nonelective surgical situations. Therefore, akin to the exceedingly safe field of anesthesia, we in general surgery should strive to make EGS operations safe regardless of individual surgeon experience or volume. In the present study, given the limitations of the SID Healthcare Cost and Utilization Project datasets, we did not have information on individual surgeons to investigate the importance of the individual surgeon. In the context of where the field of EGS stands at present, this may be viewed as a limitation to the study. However, an alternative viewpoint, and 1 we agree with, is that to investigate the individual surgeon level in a setting where a patient cannot choose their individual surgeon is incongruous with the real-world setting of emergency surgical care. With that said, there is a valid argument from the hospital’s perspective that perhaps surgeon volume should be considered and included in the analyses. This is because hospitals credential surgeons for the management of certain patient populations, and perhaps surgeon volume is a valid proxy for surgeon ability and expertise—leading to improved outcomes—in the management of complex EGS patients.
The use of an ecological analysis, with outcome as a hospital’s mortality incidence rate, rather than a patient’s probability of death, is a major strength of this study. This is because we are interested in comparing hospitals as a function of procedure volume, not comparing patient-types within or between hospitals. As an alternative, modeling risk of mortality for individual patients within hospitals via multilevel models with random hospital effects would assume conditional independence of patient outcomes within hospitals. Patient outcomes would depend only on the characteristics of that patient and the volume of the patient’s hospital, regardless of the actual mortality rate of the hospital. Thus, 2 patients with identical individual characteristics, from the same hospital or from different hospitals with the same volume, will have the same risk. This ignores contextual effects on mortality risk, such that if you are the only high-risk patient at a hospital, or among exclusively high-risk patients at a hospital with the same volume, you have the same risk of procedure failure. Another alternative would be generalized estimating equations with “sandwich” variance estimation. Such a model assumes all patients are from the same population, but adjusts variance estimates to acknowledge that there are fewer than N independent data points. With these explanations in mind, ecological analyses are optimally designed to capture the true relationship between hospital operative volume and survival.
The current study has limitations. First, our conclusions are based on results from retrospective administrative data, and are thus constrained by the limitations and biases therein. These biases could potentially be avoided with a prospective analysis with objective criteria for operative selection. Second, the definition of an emergency patient is a construct of the study. Therefore, generalizing to all emergency surgical patients may not be valid, as definitions of “emergency patient” are not standardized.7,51 Thirdly, the data are from 1 state, and California may not be representative of a national sample from which to make conclusions. Fourth, we were unable to include a rural/nonrural potential predictor into our models, given the high numbers of missing variables for this metric in the AHA dataset, and our concern therefore of introducing bias into the models. It is therefore possible that low volume is simply a marker for hospitals that are under-resourced in underserved geographic locations; this warrants further investigation. Fifth, the ability to risk-adjust the data was limited to the variables within the dataset. Specifically, physiologic parameters were not recorded; they can play a role in the outcomes of EGS patients.
In conclusion, across a variety of common emergent general surgery operations, survival rates for all adult patients were significantly improved when their operations were performed at higher volume hospitals. For each of the 10 emergency operations studied, hospital operative volume thresholds were defined to improve survival, and can potentially act as hospital volume benchmarks. These findings signify a major paradigm shift in the way we think of emergent operations: the experience of the hospital matters to the outcome as much as the patient’s illness at presentation. These results hint at the benefits to restructuring the current system of emergency surgical care and to the importance of accrediting EGS surgery centers. More data-driven research must be conducted to elucidate which of these challenging surgical patients would most benefit from higher-volume hospitals.
Supplementary Material
Acknowledgments
Disclosure: R.D.B. acknowledges that this publication was made possible by the support of the American Association for the Surgery of Trauma (AAST) Emergency General Surgery Research Scholarship Award and the Yale Center for Clinical Investigation CTSA Grant Number KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), a component of the National institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the AAST or the NIH. T.M.G. acknowledges the support of the Academic Leadership Award (K07AG043587) and Claude D. Pepper Older Americans Independence Center (P30AG021342) from the National Institute on Aging.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
The authors report no conflicts of interest.
REFERENCES
- 1.American College of Surgeons. A growing crisis in patient access to emergency surgical care. Bull Am Coll Surg. 2006;91:8–19. [PubMed] [Google Scholar]
- 2.Trunkey DD. A growing crisis in patient access to emergency care: a different interpretation and alternative solutions. Bull Am Coll Surg. 2006;91:12–22. [PubMed] [Google Scholar]
- 3.Maa J Solving the emergency care crisis in America: the power of the law and storytelling. Perm J. 2012;16:71–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gale SC, Shafi S, Dombrovskiy VY, et al. The public health burden of emergency general surgery in the United States: a 10-year analysis of the Nationwide Inpatient Sample—2001 to 2010. J Trauma Acute Care Surg. 2014;77:202–208. [DOI] [PubMed] [Google Scholar]
- 5.Acute Care Congress. Acute care congress on the future of emergency surgical care in the United States. J Trauma. 2009;67:1–7. [DOI] [PubMed] [Google Scholar]
- 6.Committee on the Future of Emergency Care in the United States Health System, Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point Consensus Report, Washington, DC: National Academies Press; Published June 13, 2006. Available at: https://www.nap.edu/read/11621/chapter/1. Accessed February 4, 2019. [Google Scholar]
- 7.Becher RD, Davis KA, Rotondo MF, et al. Ongoing evolution of emergency general surgery as a surgical subspecialty. JAm Coll Surg. 2018;226:194–200. [DOI] [PubMed] [Google Scholar]
- 8.Mackenzie EJ, Rivara FP, Jurkovich GJ, et al. The national study on costs and outcomes of trauma. J Trauma. 2007;63:S54–S67. discussion S81–S86. [DOI] [PubMed] [Google Scholar]
- 9.West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979;114:455–460. [DOI] [PubMed] [Google Scholar]
- 10.Trunkey DD. Trauma centers and trauma systems. JAMA. 2003;289:1566–1567. [DOI] [PubMed] [Google Scholar]
- 11.Trunkey D Trauma systems. A model for regionalized care. JAMA. 1995;273:421–422. [DOI] [PubMed] [Google Scholar]
- 12.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. [DOI] [PubMed] [Google Scholar]
- 13.Mann NC, Mackenzie E, Teitelbaum SD, et al. Trauma system structure and viability in the current healthcare environment: a state-by-state assessment. J Trauma. 2005;58:136–147. [DOI] [PubMed] [Google Scholar]
- 14.Cryer HG, Hiatt JR. Trauma system: the backbone of disaster preparedness. J Trauma. 2009;67:S111–S113. [DOI] [PubMed] [Google Scholar]
- 15.American College of Surgeons Committee on Trauma. Resources for Optimal Care of the Injured Patient: 2006. 5th ed, Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 16.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. [DOI] [PubMed] [Google Scholar]
- 17.Margulies DR, Cryer HG, McArthur DL, et al. Patient volume per surgeon does not predict survival in adult level I trauma centers. J Trauma. 2001;50:597–601. discussion 601–603. [DOI] [PubMed] [Google Scholar]
- 18.Richardson JD, Schmieg R, Boaz P, et al. Impact of trauma attending surgeon case volume on outcome: is more better? JTrauma. 1998;44:266–271. discussion 271–272. [DOI] [PubMed] [Google Scholar]
- 19.Ogola GO, Haider A, Shafi S. Hospitals with higher volumes of emergency general surgery patients achieve lower mortality rates: a case for establishing designated centers for emergency general surgery. J Trauma Acute Care Surg. 2017;82:497–504. [DOI] [PubMed] [Google Scholar]
- 20.Mehta A, Efron DT, Canner JK, et al. Effect of surgeon and hospital volume on emergency general surgery outcomes. JAm Coll Surg. 2017;225:666.e2–675.e2. [DOI] [PubMed] [Google Scholar]
- 21.Flood AB, Scott WR, Ewy W. Does practice make perfect? Part I: the relation between hospital volume and outcomes for selected diagnostic categories. Med Care. 1984;22:98–114. [PubMed] [Google Scholar]
- 22.Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–1751. [DOI] [PubMed] [Google Scholar]
- 23.Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. [DOI] [PubMed] [Google Scholar]
- 24.FloodAB ScottWR, EwyW. Does practice make perfect? Part II: the relation between volume and outcomes and other hospital characteristics. Med Care. 1984;22:115–125. [PubMed] [Google Scholar]
- 25.Hannan EL, O’Donnell JF, Kilburn H, et al. Investigation of the relationship between volume and mortality for surgical procedures performed in New York State hospitals. JAMA. 1989;262:503–510. [PubMed] [Google Scholar]
- 26.Dudley RA, Johansen KL, Brand R, et al. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283:1159–1166. [DOI] [PubMed] [Google Scholar]
- 27.Schrag D, Panageas KS, Riedel E, et al. Surgeon volume compared to hospital volume as a predictor of outcome following primary colon cancer resection. J Surg Oncol. 2003;83:68–78. discussion 78–79. [DOI] [PubMed] [Google Scholar]
- 28.Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg. 2007;94:145–161. [DOI] [PubMed] [Google Scholar]
- 29.Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. [DOI] [PubMed] [Google Scholar]
- 30.Becher RD, Hoth JJ, Miller PR, et al. Systemic inflammation worsens out-comes in emergency surgical patients. J Trauma Acute Care Surg. 2012; 72:1140–1149. [DOI] [PubMed] [Google Scholar]
- 31.Becher RD, Hoth JJ, Miller PR, et al. A critical assessment of outcomes in emergency versus nonemergency general surgery using the American College of Surgeons National Surgical Quality Improvement Program Database. Am Surg. 2011;77:951–959. [PubMed] [Google Scholar]
- 32.Cost Healthcare and Project Utilization. Healthcare Cost and Utilization Project (HCUP) Databases. State Inpatient Databases (SID) Overview. State Inpatient Databases (SID) Homepage. Available at: https://www.hcupus.ahrq.gov/sidoverview.jsp. Accessed January 5, 2019. [Google Scholar]
- 33.American Hospital Association (AHA). American Hospital Association (AHA) Annual Survey of Hospitals Database overview. AHA Annual Survey of Hospitals Database Homepage. Available at: https://www.ahadataviewer.com/additional-data-products/AHA-Survey/. Accessed January 5, 2019. [Google Scholar]
- 34.Shiloach M, Frencher SK, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010; 210:6–16. [DOI] [PubMed] [Google Scholar]
- 35.Schilling PL, Dimick JB, Birkmeyer JD. Prioritizing quality improvement in general surgery. J Am Coll Surg. 2008;207:698–704. [DOI] [PubMed] [Google Scholar]
- 36.Dao HE, Miller PE, Lee JH, et al. Transfer status is a risk factor for increased in-hospital mortality in patients with diverticular hemorrhage. Int J Colorectal Dis. 2013;28:273–276. [DOI] [PubMed] [Google Scholar]
- 37.Holena DN, Mills AM, Carr BG, et al. Transfer status: a risk factor for mortality in patients with necrotizing fasciitis. Surgery. 2011;150:363–370. [DOI] [PubMed] [Google Scholar]
- 38.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309:587–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levin KA. Study design VI—ecological studies. Evid Based Dent. 2006;7:108. [DOI] [PubMed] [Google Scholar]
- 40.SAS. Modeling Continuous Proportions: Normal and Beta Regression Models. Usage Note 57480: Modeling Continuous Proportions: Normal and Beta Regression Models. Available at: http://support.sas.com/kb/57/480.html. Accessed January 5, 2019. [Google Scholar]
- 41.Van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–633. [DOI] [PubMed] [Google Scholar]
- 42.Shafrin J. [January 5, 2019.];What is a Pseudo R-squared? Healthcare Economist: What is a Pseudo R-squared? Available at: http://healthcare-economist.com/2016/12/28/what-is-a-pseudo-r-squared/. Accessed.
- 43.American College of Surgeons Committee on Trauma (ACS-COT). ACS-COT Homepage. Available at: https://www.facs.org/quality-programs/trauma. Accessed January 5, 2019.
- 44.McHugh MD, Kelly LA, Smith HL, et al. Lower mortality in magnet hospitals. Med Care. 2013;51:382–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Association of American Medical Colleges (AAMC). Association of American Medical Colleges (AAMC) Organization Directory Search Result. AAMC Organization Directory Homepage. Available at: https://members.aamc.org/eweb/DynamicPage.aspx?webcode=AAMCOrgSearchResult&orgtype=Medical%20School. Accessed January 5, 2019. [Google Scholar]
- 46.American College of Surgeons. Quality Programs of the American College of Surgeons. ACS Quality Programs Homepage. Available at: https://www.facs.org/quality-programs. Accessed January 5, 2019. [Google Scholar]
- 47.Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). MBSAQIP Homepage. Available at: https://www.facs.org/quality-programs/mbsaqip. Accessed January 5, 2019. [Google Scholar]
- 48.American College of Surgeons Task Force for Children’s Surgical Care. American College of Surgeons Children’s Surgery Verification. ACS Children’s Surgery Verification Quality Improvement Program homepage. Available at: https://www.facs.org/quality-programs/childrens-surgery/childrens-surgery-verification. Accessed January 5, 2019. [Google Scholar]
- 49.LaPar DJ, Kron IL, Jones DR, et al. Hospital procedure volume should not be used as a measure of surgical quality. Ann Surg. 2012;256:606–615. [DOI] [PubMed] [Google Scholar]
- 50.Funk LM, Gawande AA, Semel ME, et al. Esophagectomy outcomes at low-volume hospitals: the association between systems characteristics and mortality. Ann Surg. 2011;253:912–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Becher RD, Meredith JW, Chang MC, et al. Creation and implementation of an emergency general surgery registry modeled after the National Trauma Data Bank. JAm Coll Surg. 2012;214:156–163. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.