Introduction
Social support has long been identified as vital to sustained recovery for individuals with substance use disorders (SUD; Day et al., 2013; Havassy, Hall & Wasserman, 1991; McCrady, 2004). Research has repeatedly found that those with stronger social support networks remain in treatment longer, and have better recovery outcomes with a decreased likelihood of return to use (Dobkin, Civita, Paraherakis & Gill, 2002; Ellis, Bernichon, Yu, Roberts & Herrell, 2004; Havassy et al., 1991; Wasserman, Stewart & Delucchi, 2001). The type of social support also matters; having even one person supportive of continued drug use may have a stronger influence on recovery than having one person supportive of abstinence (Polcin & Korcha, 2017; Stout, Kelly, Magill & Pagano, 2012). These findings have led to treatment interventions that target social networks, focusing on shifting social supports from individuals supportive of continued drug use to individuals supportive of recovery (Kelly, Stout, Greene & Slaymaker, 2014; Longabaugh, Wirtz, Zweben & Stout, 1998). This study aims to identify the ways in which different social networks foster substance use change.
Types of Social Support
Mutual Aid Groups.
Mutual aid groups provide abstinence-specific support, promote recovery and foster relationships with like-minded peers seeking abstinence and community. 12-Step groups provide a sober, supportive social network, and may also build stress-coping skills (Humphreys, 1999; Litt et al., 2009; Litt et al., 2016). The service component of the 12-step model emphasizes helping other people with SUDs which also provides significant psychological and social benefits (Moos et al., 2008). While not dissimilar from ideas learned through some formal drug treatment, 12-Step group involvement may be preferable for some because meetings take place in a more naturalistic social setting, enabling generalization of skills to a variety of relationships and situations (Humphreys, 1999). 12-Step group participation is associated with short- and long-term abstinence outcomes of up to sixteen years (Hser, Huang, Teruya & Anglin, 2003; Kelly et al., 2014; Litt, Kadden, Kabela-Cormier & Petry, 2009; Litt, Kadden, Tennen & Kabela-Cormier, 2016; Longabaugh et al., 1998; Moos & Moos, 2006). Attendance has been shown to increase treatment engagement and improve overall SUD outcomes (Timko & DeBenedetti, 2007; Weiss et al., 1996). Ye and Kaskutas (2010) examined the effects of motivation for change, problem severity, social influence, help seeking behaviors and other factors on attendance through the creation of propensity scores; findings indicated that 12-Step attendance had the greatest impact on those with a lower propensity to attend meetings. Additionally, a separate group found that for individuals with cocaine use disorders, participation, not simply attendance, predicted improved SUD outcomes (Weiss et al., 2005). In sum, the research suggests active involvement may be more important than simply attending mutual aid groups and many complex factors contribute to the level of attendance and participation in these groups.
While 12-Step groups can support one’s recovery process, they are not without limitations. For example, the focus in 12-Step groups on a higher power can be off putting for some people (Harris et al, 2004). Further, some minority groups (i.e. women and people of color) have critiqued 12-Step groups reporting they have felt disempowered in these settings (Covington, 2002; Roberts, Jackson & Carlton-Laney, 2000).
Families.
Supportive family relationships, defined as relationships that encourage reduced substance use, are associated with decreased risk of recurrence of substance use following treatment (Booth, Russell, Soucek & Laughlin, 1992; Ellis et al., 2004). Further, this type of support can be categorized into structural (i.e. network of individuals available to provide support) and functional support (i.e. providing tangible aid, emotional support). Differences do arise when examining these subtypes of support such that abstinence-specific, functional familial support predicts decreases in risk for recurrence of substance use as compared to general functional support (Havassy et al., 1991) and abstinence specific structural support predicts greater abstinence from cocaine (Wasserman et al., 2001).
Family-based approaches are standard in the conceptualization and treatment of adolescent substance use disorders and are therefore seen as integral to successful intervention and recovery for adolescents with SUDs (Hogue et al., 2008; Liddle, 2004). Among adults, family-based treatment interventions are somewhat less common. The community reinforcement and family training (CRAFT) approach was created to foster treatment engagement by targeting communication and providing concerned loved ones with tools to encourage abstinence and reduce their own dependence on the person with substance use problems (Meyers, Villaneuva & Smith, 2005). As a result, family is more likely to encourage the person in active addiction to engage in treatment, and subsequently improve outcomes (Mason & Windle, 2002; Room, Greenfield, Weisner, 1991). Another program involving family in the treatment process is the Johnson Intervention. Because partners are most likely to voice concern and encourage entrance into treatment, (Room et al., 1991) interventions specific to intimate partners are more common in adult SUD treatment programs and include Behavioral Couple Therapy (Morgenstern & McKay, 2007; Powers, Vedel & Emmelkamp, 2008) and couple interventions that target combined HIV and drug-risk prevention (El-Bassel et al., 2011; Wechsberg et al., 2015). While some research indicates individuals whose partners continue using substances are significantly more likely to return to use as compared to those with abstinent partners (Ellis et al., 2004; Hser et al., 2003), other research suggests that when both partners have addiction issues and work toward recovery, they can provide each other motivation for recovery (Simmons & Singer, 2006). Although couple based interventions have proven efficacious, (El-Bassel et al., 2011; Morgenstern & McKay, 2007; Powers, Vedel & Emmelkamp, 2008), they are not widely used due to a lack of stable relationships among people with substance use problems and financial costs (Copello & Orford, 2002; Cox, Ketner & Blow, 2013).
Friends.
Close friends and peer groups influence substance use initiation in adolescence (Urberg, Değirmencioğlu, & Pilgrim, 1997), thus it is not surprising that they continue to play a role in use, recovery and recurrence of substance use. Research findings highlight the importance of one’s social network, indicating that networks supportive of abstinence yield better treatment outcomes than networks supportive of continued substance use (Havassy et al., 1991; McCrady, 2004). For individuals early in their recovery processes, maintaining close relationships with former using or drinking associates is predictive of a return to use (Zywiak, Longabaugh & Wirtz, 2002). Similarly, maintaining friendships with individuals engaged in activities including selling drugs, breaking the law, gang-involvement and violence increases the risk for return to substance use (Ellis et al., 2004). Notably, it is not the size of the network that is important, but rather the quality of the relationships and whether abstinence or continued substance use is supported (McCrady, 2004). A study examining women six-months following residential treatment found individuals with friend networks comprised of peers engaging in negative behaviors (defined as arguing and using together) were three and a half times more likely to return to use than their counterparts with friend networks engaging in positive behaviors (defined as getting along and helping each other; Ellis et al., 2004). However, research has also demonstrated that reducing one’s social network in recovery can negatively impact one’s wellbeing, which emphasizes the importance of supplanting lost social connections with other support (Best et al., 2016).
To date, few studies focus on treatment models specifically treating individuals with addiction and their peer network. One empirical study by Smith and colleagues (2016) tested the efficacy of a CRAFT-based treatment for peers of emerging adults receiving SUD treatment (Peer-CRA). The program incorporates motivational interviewing, cognitive-behaviorally based individual and joint sessions, and specific information for the peer regarding skills to reengage the individual with substance use problems in treatment (Smith et al., 2016). Findings revealed increased days of abstinence and decreased binge drinking compared to baseline reports for both the patient and the peer, suggesting the benefit of this emerging adult program (Smith et al., 2016). Another model to enhance social support in adult populations with SUDs employed a “Community Support Group” which incorporated drug-free friends and family members into an outpatient methadone program to help build sober social support (Kidorf, Brooner & King, 1997). Participation led to decreased drug use for the patients and increased community activity (Kidorf et al., 1997). The goal of this group was to encourage individuals actively using substances to engage in prosocial activities (i.e. attending 12-Step groups, religious and recreational activities) that support abstinence (Kidorf, Brooner, Peirce, Gandotra & Leoutsakos, 2018).
Lastly, therapeutic communities provide treatment aimed at building sober social support networks with attention to employment, housing, legal and psychological care. These recovery communities provide an environment where individuals with the common goal of maintaining a recovery lifestyle can cohabitate. These communities yield significant results with decreased substance use, risk for recurrent use and legal involvement for the individuals who remain in the communities (Boisvert, Martin, Grosek & Clarie, 2008; Vanderplasschen et al., 2013). Unfortunately, many individuals are reluctant to uproot their lives to participate in these types of programs for significant lengths of time and maintaining these communities is costly with little to no insurance reimbursement.
Treatment Process Variables
Less is understood about how social support impacts other treatment process variables known to affect SUD treatment outcomes, including readiness to change and substance use goals. The transtheoretical model has long been applied to addiction with five stages of change correlating with a person’s position on the continuum of active use to maintaining a life free from substances. Readiness to change has been identified as a crucial factor in an individual’s progression through the stages of change model toward recovery (DiClemente, Schlundt & Gemmell, 2004), and can be calculated by assessing scores on each of the five stages of change (DiClemente, Carbonari, Zweben, Morrel & Lee, 2001). Because increased sober social support positively impacts reductions in substance use, it could be expected that these same supports would positively correlate with greater readiness to change. Interestingly, the little research conducted on the relationship between these variables has yielded mixed results including no correlation between social support and readiness to change; and social support being a predictor of readiness to change, in particular, the Contemplation stage of change (Chakravorty et al., 2010; Cavaiola, Fulmer & Stout, 2015). Substance use goal is another variable predictive of SUD treatment outcome (Hall, Havassy, Wasserman, 1990; Maisto, Connors & Zywiak, 2000) which may also be affected by social support. Understanding the relationship between social support and readiness to change, and social support and one’s substance use goals could potentially maximize retention and outcomes through tailored treatments that emphasize techniques focusing on social support enhancement.
The present study examines how different types of perceived social support impact treatment process variables and outcomes in patients receiving continuing care after starting treatment in intensive outpatient programs (IOP). We hypothesized that greater perceived (1) familial and (2) friend support, and (3) 12-Step group involvement would be associated with (1) reduced substance use, (2) a substance use goal of abstinence, and (3) greater readiness to change. In addition, exploratory analyses to examine the potential mediating effects of 12-step involvement and substance use goal on the relation of social support to subsequent substance use were to be conducted if the pattern of results obtained in the initial analyses was suggestive of mediation effects.
Methods
This study (N = 489) combined data from two randomized controlled trials that evaluated the effect of continuing care for people with cocaine dependence (McKay et al., 2010; McKay et al., 2013). Recruitment was conducted between 2004-2007 for study one and 2007-2009 for study two. Participants were recruited and consented within their first month in an IOP. Follow-up assessments were conducted at 3, 6, 9, 12, 15, 18, 21, and 24-months post-baseline in the first study; and at 3, 6, 9, 12, 18, and 24-months post-baseline in the second study. Participants were compensated $35 for each follow-up assessment in study one and $50 in study two. Follow-up rates for the 24-month assessments were 77% in study one, and 75% in study two.
Study treatment conditions
The two trials’ main goal was to compare the effects on substance use of additional continuing care services for patients in IOP. Both trials included an IOP “treatment as usual” group counseling condition and a telephone monitoring plus counseling condition (TMC); those two groups are included in this analysis. In addition, study one had a telephone monitoring condition without counseling. Participants from this group were not included in this analysis to ensure consistency across the two studies. The present study’s pooled analysis includes only individuals assigned to the two treatment conditions described below:
Intensive outpatient program (IOP).
Treatment was provided in a group setting and covered the topics of denial, recovery management, and the value of mutual aid groups (McKay, Alterman, McLellan & Snider, 1994; McKay et al., 2010). Group treatment was provided for about nine hours per week for three-four months.
Telephone monitoring and counseling (IOP+TMC).
Participants in this group received IOP and TMC beginning after week four of IOP for participants in study one and beginning after week three of IOP for participants in study two. TMC counseling utilized a cognitive behavioral approach and was provided individually over the phone (unless the participant preferred meeting in person). The TMC sessions (weekly for the first 8 weeks and then transitioned to biweekly, monthly and bimonthly) lasted 18 months for the first study and 24 months for the second study.
In the second study, there was a second TMC condition that incentivized attendance by compensating participants $10 per TMC session attended. In this study’s analysis the TMC plus financial incentives condition is included in the IOP+TMC group because the counseling was the same in the two groups and the incentives did not impact substance use outcomes (McKay et al., 2013).
Measures
Addiction Severity Index (ASI; McLellan et al, 1992 ).
Administered at baseline, the ASI assesses several domains including: basic demographic information, medical, employment, legal, family/social, psychological, alcohol and substance use. More specifically, the present study utilized demographic variables, and information from the alcohol and substance use domains including prior treatments and patterns of substance use.
The Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 2012).
This assessment determined cocaine dependence diagnoses and mental health problems at baseline.
Perceived Social Support – Friend (PSS friend; Procidano & Heller, 1983).
This 20-item measure assessed participants’ views of general social support participants received from their friend network. Participants rated each statement on a Likert scale with a total possible score of 60, with greater scores indicating higher levels of perceived friend support. It does not specifically query abstinence specific support. The measure has excellent reliability (α = .95; Windle, 1991).
Perceived Social Support – Family (PSS family; Procidano & Heller, 1983).
This 20-item measure assessed participants’ views of general social support they received from their family, with statements (substituting the words “friends with “family”), item responses and scoring procedures identical to the PSS friend. It does not query abstinence specific support. The PSS family maintains good internal consistency and reliability (Windle, 1991).
AA/NA/CA Questionnaire.
This mutual aid group utilization measure assesses overall 12-step beliefs, attendance and participation; because we were interested specifically in involvement and not 12-Step beliefs, we selected an 8-item subscale from this questionnaire. The items in this subscale include the number of times the participant attended meetings, spoke at meetings, performed service, called their sponsor, and called a peer group member in the past 30 days. These continuous numbers were totaled with greater scores indicating higher engagement. This measure has demonstrated good internal consistency (McKay et al., 1994).
Timeline Followback (TLFB; Sobell & Sobell, 1992).
To measure alcohol and cocaine use at baseline and follow-up assessments, the TLFB, a self-report instrument, was used. Days with cocaine, alcohol or use of both substances were considered days of use. TLFB has demonstrated test-retest reliability of 0.80 and is highly correlated with urinalysis results (Ehrman & Robbins, 1994; Fals-Stewart, O’Farrell, Freitas, McFarlin & Rutigliano, 2000). The TLFB variable used for this analysis was percent days abstinent, or PDA (range 0-100%).
Thoughts about Abstinence (TAA).
This measure was used to assess one’s substance use goals and consists of a single question directing the respondent to select the abstinence goal with which they most closely align (Hall, Havassy & Wasserman, 1991). The six possible responses were transformed into a dichotomous variable for analysis (total abstinence, never use again = 0; all other less stringent abstinence goals = 1; McKay et al., 2013). We used the dichotomous variable because it was poorly distributed; this transformation is consistent with prior research (Hall et al., 1991). TAA was collected at all follow-up assessments except months 15 and 21.
University of Rhode Island Change Assessment Questionnaire (URICA).
This 32-item measure assessed respondent’s readiness to change substance using behavior by rating their agreement or disagreement with statements on a 5-point Likert scale with possible scores ranging from −4 to 14 and higher scores indicating greater readiness to change. The measure has good internal consistency (Prochaska & DiClemente, 1984).
Data Analysis
To examine the effect of family, friend and 12-Step group support (predictor variables) on substance use goals, readiness to change, and PDA (outcome variables) across the follow-up assessments, we first looked at the Pearson correlation coefficient between the predictors and outcomes (SAS PROC CORR). We then used generalized estimating equations (GEE; SAS PROC GENMOD). We used GEE because it considers the dependence of variables in repeated measure designs (Ghisletta and Spini, 2004). Our analyses looked at how the average scores of the predictor variables covaried with the average scores of the outcome variables concurrently across the follow-up assessments.
Three separate GEE analyses were conducted to look at the effect of the predictor variables on: 1) substance use goal (TAA; binary variable), 2) readiness to change (continuous variable), and 3) percent days abstinent (PDA; continuous variable). The predictor variables for all three GEE analyses included: 1) PSS friend (continuous variable), 2) PSS family (continuous variable), and 3) 12-Step involvement (continuous variable). Each of the three GEE analyses also controlled for the baseline value of the predictor variable (continuous or binary), and baseline variables that had a significant bivariate association with the respective outcome.
Prior to conducting mediation analyses, we looked at the lagged correlations (SAS PROC CORR) between the following variables across 3, 6, 9, and 12 month assessments: (1) PSS friend and family, (2) substance use goal one follow-up later (3) PDA two follow-ups later; and (1) PSS friend and family, (2) readiness to change one follow-up later, (3) PDA two follow-ups later. For lagged correlations that suggested mediation effects, formal mediation analyses were conducted (SAS PROC CAUSAL MED), controlling for baseline variables that had a significant bivariate association with PDA. Mediation analyses model whether (1) a predictor (i.e. PSS friend and family) is significantly associated with a mediator (i.e. substance use goal or readiness to change); and (2) whether the mediator and predictor are significantly associated with the outcome (i.e. PDA), yielding an indirect or mediation effect (Baron and Kenny, 1986).
Results
Participant characteristics from the two trials included in this analysis are summarized in Table 1. Most participants were men (72%), had never been married (53%) and had an annual income of under $10,000 (70%). Pearson correlation coefficients between outcome and predictor variables are displayed in Table 2. Results from the three GEE analyses are described below:
Table 1.
Sample Demographics at Baseline
| n | % | |
|---|---|---|
| Gender | ||
| Female | 135 | 27.60 |
| Male | 354 | 72.39 |
| Marital Status | ||
| Married | 45 | 9.39 |
| Divorced | 83 | 17.33 |
| Widowed | 9 | 1.88 |
| Separated | 63 | 13.15 |
| Never married | 255 | 53.24 |
| Unmarried partner | 24 | 5.01 |
| Employment | ||
| Employed | 45 | 9.39 |
| No work for less than one year | 153 | 31.94 |
| Self-employed | 20 | 4.18 |
| Homemaker | 16 | 3.34 |
| No work for more than one year | 119 | 24.84 |
| Unable to work | 126 | 26.30 |
| Annual Income | ||
| $0-9,999 | 332 | 69.60 |
| $10K-14,999 | 45 | 9.43 |
| $15K-24,999 | 25 | 5.24 |
| $20K-24,999 | 19 | 3.98 |
| $25K-34,999 | 30 | 6.29 |
| $35K-49,999 | 8 | 1.68 |
| $50K-74,999 | 10 | 2.10 |
| $75K + | 8 | 1.68 |
| Highest Grade | ||
| Grades 1-8 | 19 | 3.97 |
| Grades 9-11 | 148 | 30.90 |
| Grade 12 or GED | 200 | 41.75 |
| College 1-3 years | 95 | 19.83 |
| College 4+ years | 17 | 3.55 |
| Treatment condition | ||
| IOP | 193 | 39.39 |
| TMC | 297 | 60.61 |
| M | SD | |
| Age | 42.06 | 7.84 |
| Lifetime substance use treatment admissions | ||
| Drug | 3.93 | 5.05 |
| Alcohol | 3.04 | 4.46 |
| PSS Friend Score | 37.31 | 11.91 |
| PSS Family Score | 37.95 | 13.25 |
| Readiness to change score | 10.81 | 1.60 |
Table 2.
Pearson correlation coefficients between variables
| r p-value |
PSS friend | PSS family | 12-step involvement | Percent days abstinent | Readiness to change |
|---|---|---|---|---|---|
| PSS friend | |||||
| PSS family | .54 <.0001 |
||||
| 12-step involvement | .30 <.0001 |
.16 <.0001 |
|||
| Percent days abstinent | .21 <.0001 |
.22 <.0001 |
.26 <.0001 |
||
| Readiness to change | .23 <.0001 |
.11 <.0001 |
.17 <.0001 |
.04 .06 |
|
| TAA | −.11 <.001 |
−.12 <.0001 |
−.14 <.0001 |
−.15 <.0001 |
−.05 <.05 |
Readiness to Change as the dependent variable
GEE analysis found that greater PSS friend [X2 (1)=9.49, p<.01] and greater 12-Step involvement [X2 (1)= 15.16, p<.0001] were significantly associated with greater readiness to change controlling for the baseline readiness to change value, lifetime drug and alcohol treatment, age, and employment (Table 3). PSS family was not a significant predictor [X2 (1)=2.72, p=.10].
Table 3.
Summary of GEE analysis for variables predicting readiness to change
| Variables | B | Standard Error | Wald | df | Sig. |
|---|---|---|---|---|---|
| AA participation | .005 | .001 | 15.16 | 1 | <.0001 |
| PSS friend | .02 | .005 | 9.49 | 1 | <.01 |
| Baseline Readiness to Change | .47 | .05 | 60.24 | 1 | <.0001 |
| Lifetime Drug Treatment | .04 | .01 | 4.12 | 1 | <.05 |
| Age | −.02 | .01 | 4.52 | 1 | <.05 |
| PSS family | .007 | .004 | 2.72 | 1 | .10 |
| Lifetime Alcohol Treatment | −.03 | .01 | 1.76 | 1 | .18 |
| Employment | .48 | .20 | 10.21 | 1 | .07 |
Percent days abstinent as the dependent variable
GEE analysis found that greater PSS friend [X2 (1)=13.62, p<.001], greater PSS family [X2 (1)=10.75, p<.05], and greater 12-Step involvement [X2 (1)= 37.05, p<.0001] were significantly associated with increased PDA controlling for age, the baseline variable for PDA, lifetime drug and alcohol treatment, and treatment condition in the continuing care study (Table 4).
Table 4.
Summary of GEE analysis for variables predicting percent days abstinent
| Variables | B | Standard Error | Wald | df | Sig. |
|---|---|---|---|---|---|
| AA participation | .001 | .0006 | 37.05 | 1 | <.0001 |
| PSS family | .002 | .0006 | 10.75 | 1 | <.05 |
| PSS friend | .003 | .0007 | 13.62 | 1 | <.001 |
| Age | −.003 | .001 | 6.11 | 1 | <.01 |
| Lifetime Drug Treatment | −.003 | .002 | 2.69 | 1 | .10 |
| Lifetime Alcohol Treatment | −.001 | .002 | 0.17 | 1 | .68 |
| Treatment Condition (reference=TMC) | −.0003 | .02 | 0.00 | 1 | .98 |
| Baseline PDA | −.01 | .02 | .16 | 1 | .70 |
Substance Use Goal as the dependent variable
GEE analysis found that greater PSS family [X2 (1)=6.21, p<.01], and greater 12-Step involvement [X2 (1)= 6.02, p<.01] were significantly associated with a person’s substance use goal as measured by the TAA, controlling for the baseline TAA value (Table 5). PSS friends was not a significant predictor [X2 (1)= .29, p=.60].
Table 5.
Summary of GEE analysis for variables predicting substance use goal
| 95% Confidence Interval for Exp(B) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | B | Standard Error | Wald | df | Sig. | Exp(B) | Lower Bound | Upper Bound |
| AA participation | .003 | .001 | 6.02 | 1 | <.01 | 1.003 | 1.001 | 1.005 |
| PSS family | .001 | .005 | 6.21 | 1 | <.01 | 1.01 | 1.003 | 1.02 |
| Baseline Commitment to Abstinence (reference=0) | 1.13 | .15 | 48.93 | 1 | <.0001 | 3.11 | 2.31 | 4.18 |
| PSS friend | .003 | .01 | .29 | 1 | .60 | |||
Post-hoc Analyses: Mediation Models
The results obtained in the longitudinal models indirectly suggested that 12-Step involvement and substance use goal might in some way explain the relation between social support and substance use. In three cases, significant correlations were obtained for each leg of the mediation triangle (Figure 1), i.e., social support at Time A was correlated with the purported mediator at Time B, the mediator at Time B was correlated with PDA at Time C, and social support at Time A was correlated with PDA at Time C. Because this pattern of results suggests mediation effects, formal mediation analyses were conducted. These analyses tested whether: (1) the relation of PSS friend at 3 months to PDA at 9 months was mediated by substance use goal at 6 months; (2) the relation of PSS family at 3 months to PDA at 9 months was mediated by substance use goal at 6 months; and (3) the relation of PSS family at 6 months to PDA at 12 months was mediated by substance use goal at 9 months, controlling for age, treatment condition in the continuing care study, and lifetime alcohol and drug treatment. We did not perform further mediation analyses, as the pattern of correlations did not suggest other potential mediation effects.
Figure 1.
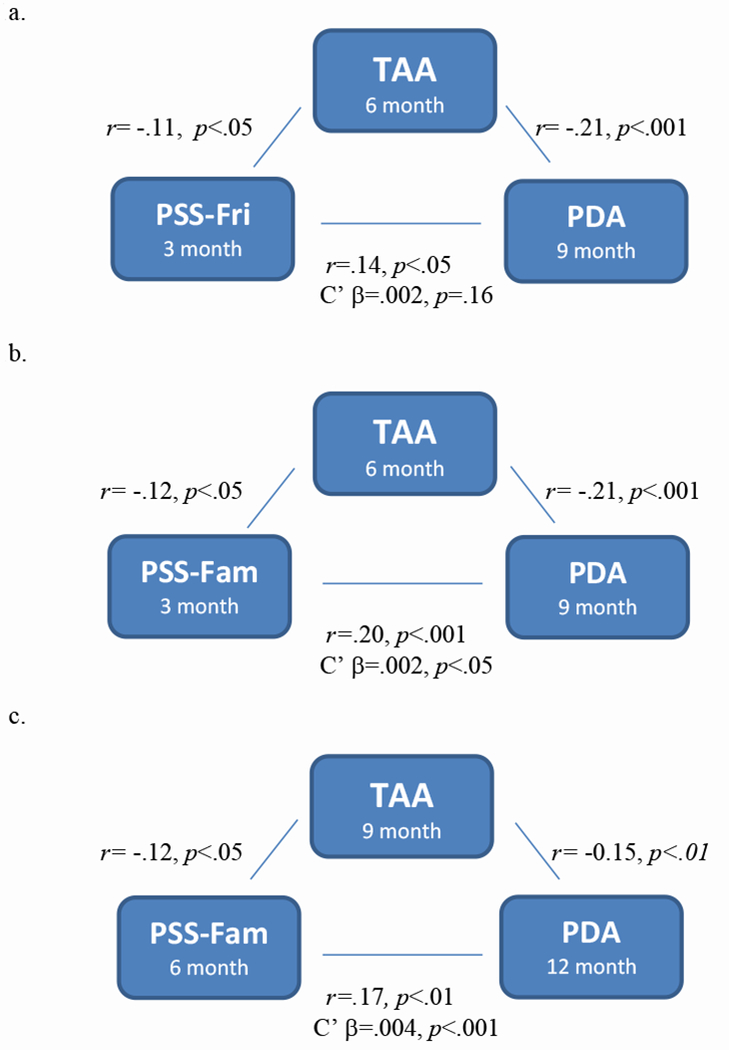
Pearson Correlation Coefficients between Perceived Social Support (PSS-Fri/Fam), Thoughts About Abstinence (TAA) and Percent Days Abstinent (PDA). C’ regression coefficients are also presented, representing the effect of PSS-Fri/Fam on PDA that is not mediated by TAA. Higher PSS-Fri/Fam scores indicate greater perceived social support. TAA was coded dichotomously where 0 = never planned to use again and 1 = all other responses. Higher PDA scores indicate more days abstinent in the reported time period. Figure 1a – 18.82% mediated, p = .13; Figure 1b – 13.77% mediated, p = .10; Figure 1c – 8.23% mediated, p = .11.
Results indicated that substance use goal at 6 months partially mediated the effect of PSS friend scores at 3 months on PDA at 9 months, trending towards significance (b=.001, SE=.0003, p=.10). Approximately 22% of the effect of PSS friend score at 3 months on PDA at 9 months was attributed to the mediation of substance use goal at 6 months. In the second mediation model, substance use goal at 6 months partially mediated the effect of PSS family scores at 3 months on PDA at 9 months, trending towards significance (b=.0005, SE=.0003, p=.10). Approximately 16% of the effect of PSS family score at 3 months on PDA at 9 months was attributed to the mediation of substance use goal at 6 months. In the third mediation model, substance use goal at 9 months partially mediated the effect of PSS family scores at 6 months on PDA at 12 months, trending towards significance (b=.0005, SE=.0003, p=.08). Approximately 11% of the effect of PSS family score at 3 months on PDA at 9 months was attributed to the mediation of substance use goal at 6 months.
Discussion
The present study found that among a sample of adults in continuing care treatment for cocaine dependence, greater general social support was associated with reduced substance use, greater readiness to change and a substance use goal of total abstinence. However, results also indicated that perceived family support, perceived friend support, and 12-Step involvement were differentially associated with these outcomes. In particular, family and friend perceived general social support were differentially associated with readiness to change and abstinence as a substance use goal. Peer support and 12-Step involvement were significantly correlated with readiness to change, whereas 12-Step involvement and familial support were significantly correlated with having the goal of maintaining abstinence. These divergent findings may be understood in the differential experiences of family and friend groups. Family members have often been present across their loved one’s addiction and may be less tolerant of the chronic nature of addiction. Therefore, family may only support complete abstinence with little room for any use, whereas friends may be more understanding of the recurrence of symptoms and substance use, or support use in moderation.
Creating an abstinence-specific social network comprised of people primarily in recovery has been associated with a stronger recovery lifestyle (Bathish et al., 2017). It may be that individuals exhibiting a greater readiness to change select friends supportive of recovery, however, the measures utilized in this study assessed general social support, so it is unclear if these friends provided abstinence specific social support. This is supported by prior findings showing people in recovery are more likely to spend time with, and remain connected to, peers in recovery (Van Melick et al. 2013). Peer sober support decreases the risk for recurrence of substance use, and is also associated with a better quality of life and sense of self-efficacy (Ellis et al., 2004; Van Melick et al., 2013). Conversely, individuals with lower social support report increased exposure to stressful life events and more mental health symptoms. These issues may be more difficult to manage due to a lack of social resources, subsequently increasing the risk for a return to use and potentially negatively impacting progress in one’s readiness to change (Dobkin et al., 2002).
Greater general family and friend perceived social support and 12-Step participation were all associated with less substance use. This aligns well with the body of literature suggesting individuals are more likely to maintain abstinence when they receive higher levels of support from family and friends (Day et al., 2013; McCrady, 2004; Dobkin et al., 2002; Wasserman et al., 2001). Recovery focused group participation and involvement (e.g. treatment and mutual aid groups) is linked to decreased alcohol consumption and the maintenance of abstinence (Beattie & Longabaugh, 1997; Kaskutas, Bond & Humphreys, 2002; Longabaugh Wirtz, Zywiak & O’Malley, 2010; Van Melick et al., 2013), and 12-Step attendance is associated with less substance use as compared to infrequent and non-12-Step attenders (Gossop, Stewart & Marsden, 2008). Moreover, 12-Step affiliation reinforces coping mechanisms, social connectedness, self-reflection and emphasizes the tenant of service, which provides a sense of accountability, responsibility, meaning, and can improve one’s overall sense of worth (Moos et al., 2008). For individuals who stay connected with support networks that encourage continued use, there is typically more ambivalence concerning abstinence, subsequently leading to an increased likelihood for return to use (Longabaugh et al., 1998; Polcin & Korcha, 2017). These findings are further supported by prior research that suggests maintaining a network of individuals from mutual aid groups who support reduced alcohol consumption predicts abstinence (Kaskutas et al., 2002).
The mediation analyses that were performed were an attempt to understand the mechanisms through which social support influences substance use outcomes. It is important to note that these analyses were exploratory and were only done in the three cases where the pattern of lagged correlations between study variables across three consecutive follow-ups in the first year of the follow-up was suggestive of possible mediation. These analyses therefore likely capitalized on chance findings and should be interpreted with caution. Moreover, they are based on lagged relations between study variables, which is crucial for mediation, rather than the concurrent relations that were examined in the longitudinal GEE analyses which took all follow-up assessments over the full 2 years into account. With these caveats in mind, the mediation analyses did find preliminary evidence that the impact of social support from friends and family at 3 months on substance use at 9 months was partially mediated by substance use goal at 6 months, and the impact of social support from family at 6 months on substance use at 12 months was partially mediated by substance use goal at 9 months. Though preliminary, these results raise the intriguing possibility that the positive effect of general social support on substance use outcomes in the first year of recovery is at least partly accounted for by increasing commitment to abstinence.
Limitations
The present study is a secondary data analysis, utilizing a combined sample from two separate studies assessing continuing care for people with cocaine addiction. The analyses are correlational in nature, so no causation can be attributed to the findings and we cannot rule out the possible impact of other variables that were not assessed. Baseline data was collected at two and three weeks into IOP treatment. As such, the variables may not represent actual baseline characteristics of individual’s readiness to change or substance use goal as they had potentially received between 18 and 27 hours of treatment and may have already undergone change in outcomes. The TAA was dichotomized based on the distribution of responses in this sample and prior research with the instrument. In doing so, meaningful analysis of this outcome may be limited with less sensitivity to minor changes or movement in one’s actual substance use goal. Additionally, the three-month periods between follow-up time points may have been too long in duration to sufficiently capture changes in these non-substance using variables. Future work should examine these variables more frequently. Further, our findings do not indicate that 12-Step groups work for everyone.
Conclusions
The results demonstrate that while general social support is associated with substance use recovery during continuing care, the source of social support (i.e. familial or friend) may have a differential relationship to other process outcomes measured concurrently. Exploratory lagged analyses also suggested that the abstinence goal may partially mediate the relation between social support and subsequent substance use outcomes in the first year of recovery. These findings support prior research indicating social support is key in sustained recovery (Ellis et al., 2004). It further highlights the importance of considering differential effects of familial and peer support on facets of the recovery process, and indicates potential future directions for interventions. Treatment programs that involve family and loved ones may aid in increased treatment enrollment and retention, enhance outcomes and repair the family system that has been affected by addiction (Copello & Orford, 2002). Programs currently offered commonly provide psychoeducation to family members and friends about the course of addiction and how to provide support that enhances recovery and does not further enable using patterns. Incorporating other skills into these programs including motivational enhancement techniques similar to what is offered through CRAFT/Peer-CRA may increase the association between support and other treatment process variables. Interventions for peer networks can also capitalize on their power to support readiness to change by providing peer motivation to the individual in active addiction. While these programs are typical in many adolescent and private residential treatment centers, they are often not available in urban and publicly-funded treatment programs. Making these programs more widely available and accessible could contribute to greater social support and changes in treatment process variables, with the goal of ultimately enhancing recovery outcomes.
Acknowledgments
Funding: This work was supported by R01 DA020623 and 2K24 DA029062 from NIDA and R01 AA14850 from NIAAA
Footnotes
Disclosures: The authors have no conflicts of interest to report.
References
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Beattie MC, & Longabaugh R (1997). Interpersonal factors and post-treatment drinking and subjective wellbeing. Addiction, 92(11), 1507–1521. [PubMed] [Google Scholar]
- Best D, Beckwith M, Haslam C, Alexander Haslam S, Jetten J, Mawson E, & Lubman DI (2016). Overcoming alcohol and other drug addiction as a process of social identity transition: the social identity model of recovery (SIMOR). Addiction Research & Theory, 24(2), 111–123. [Google Scholar]
- Bathish R, Best D, Savic M, Beckwith M, Mackenzie J, & Lubman DI (2017). “Is it me or should my friends take the credit?” The role of social networks and social identity in recovery from addiction. Journal of Applied Social Psychology, 47(1), 35–46. [Google Scholar]
- Boisvert RA, Martin LM, Grosek M, & Clarie AJ (2008). Effectiveness of a peer-support community in addiction recovery: participation as intervention. Occupational Therapy International, 15(4), 205–220. [DOI] [PubMed] [Google Scholar]
- Booth BM, Russell DW, Soucek S, & Laughlin PR (1992). Social support and outcome of alcoholism treatment: An exploratory analysis. The American journal of drug and alcohol abuse, 18(1), 87–101. [DOI] [PubMed] [Google Scholar]
- Cavaiola AA, Fulmer BA, & Stout D (2015). The impact of social support and attachment style on quality of life and readiness to change in a sample of individuals receiving medication-assisted treatment for opioid dependence. Substance abuse, 36(2), 183–191. [DOI] [PubMed] [Google Scholar]
- Copello A, & Orford J (2002). Addiction and the family: is it time for services to take notice of the evidence? Addiction, 97(11), 1361–1363. [DOI] [PubMed] [Google Scholar]
- Covington S (2002). Helping women recover: Creating gender-responsive treatment In Straussner SLA & Brown S (Eds.) The handbook of addiction treatment for women: Theory and practice, 52–72. [Google Scholar]
- Chakravorty S, Kuna ST, Zaharakis N, O’Brien CP, Kampman KM, & Oslin D (2010). Covariates of Craving in Actively Drinking Alcoholics. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions, 19(5), 450–457. 10.1111/j.1521-0391.2010.00067.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox RB Jr, Ketner JS, & Blow AJ (2013). Working with couples and substance abuse: Recommendations for clinical practice. The American Journal of Family Therapy, 41(2), 160–172. [Google Scholar]
- Day E, Copello A, Karia M, Roche J, Grewal P, George S, … & Chohan G (2013). Social network support for individuals receiving opiate substitution treatment and its association with treatment progress. European Addiction Research, 19(4), 211–221. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari J, Zweben A, Morrel T, & Lee RE (2001). Motivation hypothesis causal chain analysis. Project MATCH hypotheses: Results and causal chain analyses, 8, 206–222. [Google Scholar]
- DiClemente CC, Schlundt D, & Gemmell L (2004). Readiness and stages of change in addiction treatment. The American Journal on Addictions, 13(2), 103–119. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Civita MD, Paraherakis A, & Gill K (2002). The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction, 97(3), 347–356. [DOI] [PubMed] [Google Scholar]
- Ehrman RN, & Robbins SJ (1994). Reliability and validity of 6-month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology, 62(4), 843–50. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Witte SS, Chang M, Hill J, & Remien RH (2011). Couple-based HIV prevention for low-income drug users from New York City: A randomized controlled trial to reduce dual risks. Journal of Acquired Immune Deficiency Syndromes, 58(2), 198–206. doi: 10.1097/QAI.0b013e318229eab1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis B, Bernichon T, Yu P, Roberts T, & Herrell JM (2004). Effect of social support on substance abuse relapse in a residential treatment setting for women. Evaluation and Program Planning, 27(2), 213–221. [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, & Rutigliano P (2000). The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology, 68(1), 134–44. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2012). Structured clinical interview for DSM-IV® Axis I disorders (SCID-I), clinical version, administration booklet. Arlington, VA: American Psychiatric Publishing, Inc. [Google Scholar]
- Ghisletta P, & Spini D (2004). An introduction to generalized estimating equations and an application to assess selectivity effects in a longitudinal study on very old individuals. Journal of Educational and Behavioral Statistics, 29(4), 421–437. [Google Scholar]
- Gossop M, Stewart D, & Marsden J (2008). Attendance at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: a 5-year follow-up study. Addiction, 103(1), 119–125. [DOI] [PubMed] [Google Scholar]
- Greenfield BL, Owens MD, & Ley D (2014). Opioid use in Albuquerque, New Mexico: a needs assessment of recent changes and treatment availability. Addiction Science & Clinical Practice, 9(1), 10 10.1186/1940-0640-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, & Wasserman DA (1990). Commitment to abstinence and acute stress in relapse to alcohol, opiates, and nicotine. Journal of consulting and clinical psychology, 58(2), 175. [DOI] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, & Wasserman DA (1991). Effects of commitment to abstinence, positive moods, stress, and coping on relapse to cocaine use. Journal of consulting and clinical psychology, 59(4), 526. [DOI] [PubMed] [Google Scholar]
- Harris J, Best D, Gossop M, Marshall J, Man LH, Manning V, & Strang J (2003). Prior Alcoholics Anonymous (AA) affiliation and the acceptability of the Twelve Steps to patients entering UK statutory addiction treatment. Journal of studies on alcohol, 64(2), 257–261. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Hall SM, & Wasserman DA (1991). Social support and relapse: Commonalities among alcoholics, opiate users, and cigarette smokers. Addictive behaviors, 16(5), 235–246. [DOI] [PubMed] [Google Scholar]
- Hogue A Henderson CE Dauber S Barajas PC, Fried A, Liddle HA (2008). Treatment adherence, competence, and outcome in individual and family therapy for adolescent behavior problems. Journal of consulting and clinical psychology, 76(4), 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Huang D, Teruya C, & Anglin MD (2003). Gender comparisons of drug abuse treatment outcomes and predictors. Drug and Alcohol Dependence, 72(3), 255–264. [DOI] [PubMed] [Google Scholar]
- Humphreys K (1999). Professional interventions that facilitate 12-step self-help group involvement. Alcohol Research & Health, 23(2), 93–93. [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, & Humphreys K (2002). Social networks as mediators of the effect of Alcoholics Anonymous. Addiction, 97(7), 891–900. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Greene MC, & Slaymaker V (2014). Young adults, social networks, and addiction recovery: Post treatment changes in social ties and their role as a mediator of 12-step participation. PloS one, 9(6), e100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidorf et al. , 1997 Kidorf M, Brooner RK, and King VL: Motivating methadone patients to include drug-free significant others in treatment: A behavioral intervention. Journal of Substance Abuse Treatment 1997; 14: pp. 23–28 [DOI] [PubMed] [Google Scholar]
- Liddle HA (2004). Family-based therapies for adolescent alcohol and drug use: research contributions and future research needs. Addiction, 99(s2), 76–92. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, & Petry NM (2009). Changing network support for drinking: network support project 2-year follow-up. Journal of consulting and clinical psychology, 77(2), 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Tennen H & Kabela-Cormier E (2016). Network Support II: Randomized controlled trial of network support treatment and cognitive behavioral therapy for alcohol use disorder. Journal of consulting and clinical psychology, 77(2), 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, & Stout RL (1998). Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction, 93(9), 1313–1333. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zywiak WH, & O’Malley SS (2010). Network support as a prognostic indicator of drinking outcomes: The COMBINE study. Journal of Studies on Alcohol and Drugs, 71(6), 837–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ, & Zywiak WH (2000). Alcohol treatment changes in coping skills, self-efficacy, and levels of alcohol use and related problems 1 year following treatment initiation. Psychology of Addictive Behaviors, 14(3), 257. [DOI] [PubMed] [Google Scholar]
- Mason WA, & Windle M (2002). Family, Religious, School, and Peer Influences on Adolescent Alcohol Use. Prevention Researcher, 9(3), 6–7. [DOI] [PubMed] [Google Scholar]
- McCrady BS (2004). To have but one true friend: implications for practice of research on alcohol use disorders and social network. Psychology of Addictive Behaviors, 18(2), 113. [DOI] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, McLellan AT, & Snider EC (1994). Treatment goals, continuity of care, and outcome in a day hospital program, (151), 254–259. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn DH, Oslin DW, Lynch KG, Ivey M, Ward K, … & Coviello DM (2010). A randomized trial of extended telephone-based continuing care for alcohol dependence: Within-treatment substance use outcomes. Journal of consulting and clinical psychology, 78(6), 912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Van Horn D, Rennert L, Drapkin M, Ivey M, & Koppenhaver J (2013). Factors in sustained recovery from cocaine dependence. Journal of substance abuse treatment, 45(2), 163–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan A Thomas, Harvey Kushner, David Metzger, Roger Peters, Iris Smith, Grant Grissom, Helen Pettinati, and Milton Argeriou “The fifth edition of the Addiction Severity Index.” Journal of substance abuse treatment 9, no. 3 (1992): 199–213. [DOI] [PubMed] [Google Scholar]
- Meyers RJ Villanueva M & Smith JE (2005). The community reinforcement approach: History and new directions. Journal of Cognitive Psychotherapy, 19(3), 247. [Google Scholar]
- Moos RH, & Moos BS (2006). Participation in treatment and Alcoholics Anonymous: A 16-year follow-up of initially untreated individuals. Journal of clinical psychology, 62(6), 735–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, & McKay JR (2007). Rethinking the paradigms that inform behavioral treatment research for substance use disorders. Addiction, 102(9), 1377–1389. [DOI] [PubMed] [Google Scholar]
- Polcin DL, & Korcha R (2017). Social support influences on substance abuse outcomes among sober living house residents with low and moderate psychiatric severity. Journal of Alcohol and Drug Education, 61(1), 51–70. [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Vedel E, & Emmelkamp PM (2008). Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical psychology review, 28(6), 952–962. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, & DiClemente CC (1984). Self change processes, self efficacy and decisional balance across five stages of smoking cessation. Progress in clinical and biological research, 156, 131. [PubMed] [Google Scholar]
- Procidano ME, & Heller K (1983). Measures of perceived social support from friends and from family: Three validation studies. American journal of community psychology, 11(1), 1–24. [DOI] [PubMed] [Google Scholar]
- Roberts A, Jackson MS, & Carlton-LaNey I (2000). Revisiting the need for feminism and afrocentric theory when treating African-American female substance abusers. Journal of Drug Issues, 30(4), 901–917. [Google Scholar]
- Room R, Greenfield TK, & Weisner C (1991). People who might have liked you to drink less: changing responses to drinking by US family members and friends, 1979-1990. Contemp. Drug Probs, 18, 573. [Google Scholar]
- Simmons J, & Singer M (2006). I love you … and heroin: Care and collusion among drug-using couples. Substance Abuse Treatment, Prevention, and Policy, 1(1), 1–13. doi: 10.1186/1747-597X-1-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DC, Davis JP, Ureche DJ, & Dumas TM (2016). Six month outcomes of a peer-enhanced community reinforcement approach for emerging adults with substance misuse: A Preliminary Study. Journal of Substance Abuse Treatment, 61, 66–73. 10.1016/j.jsat.2015.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back In Measuring alcohol consumption (pp. 41–72). New Jersey: Humana Press. [Google Scholar]
- Stout RL, Kelly JF, Magill M, & Pagano ME (2012). Association between social influences and drinking outcomes across three years. Journal of Studies on Alcohol and Drugs, 73(3), 489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C, & DeBenedetti A (2007). A randomized controlled trial of intensive referral to 12-step self-help groups: One-year outcomes. Drug and alcohol dependence, 90(2-3), 270–279. [DOI] [PubMed] [Google Scholar]
- Urberg KA, Değirmencioğlu SM, & Pilgrim C (1997). Close friend and group influence on adolescent cigarette smoking and alcohol use. Developmental psychology, 33(5), 834. [DOI] [PubMed] [Google Scholar]
- Van Melick M, McCartney D, & Best D (2013). Ongoing recovery support and peer networks: A preliminary investigation of recovery peer supporters and their peers. Journal of Groups in Addiction & Recovery, 8(3), 185–199. [Google Scholar]
- Vanderplasschen W, Colpaert K, Autrique M, Rapp RC, Pearce S, Broekaert E, & Vandevelde S (2013). Therapeutic communities for addictions: a review of their effectiveness from a recovery-oriented perspective. The Scientific World Journal, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman DA, Stewart AL, & Delucchi KL (2001). Social support and abstinence from opiates and cocaine during opioid maintenance treatment. Drug and Alcohol Dependence, 65(1), 65–75. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, El-Bassel N, Carney T, Browne FA, Myers B, & Zule WA (2015). Adapting an evidence-based HIV behavioral intervention for South African couples. Substance Abuse Treatment, Prevention, and Policy, 10(6). doi: 10.1186/s13011-015-0005-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Gallop RJ, Najavits LM, Frank A, Crits-Christoph P, … & Luborsky L (2005). The effect of 12-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug and Alcohol Dependence, 77(2), 177–184. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Najavits LM, Hufford C, Kogan J, Thompson HJ, … & Siqueland L (1996). Self-help activities in cocaine dependent patients entering treatment: Results from the NIDA collaborative cocaine treatment study. Drug & Alcohol Dependence, 43(1), 79–86. [DOI] [PubMed] [Google Scholar]
- White W (2009). Long-term strategies to reduce the stigma attached to addiction, treatment, and recovery within the City of Philadelphia (with particular reference to medication-assisted treatment/recovery). Philadelphia: Department of Behavioral Health and Mental Retardation Services. [Google Scholar]
- Windle M (1991). The difficult temperament in adolescence: Associations with substance use, family support, and problem behaviors. Journal of Clinical Psychology, 47(2), 310–315. [DOI] [PubMed] [Google Scholar]
- Zywiak WH, Longabaugh R, & Wirtz PW (2002). Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. Journal of studies on alcohol, 63(1), 114–121. [PubMed] [Google Scholar]


