Abstract
Background:
Loneliness has been linked to greater substance use, especially among women. Yet little is known about how loneliness is associated with treatment outcomes for patients with opioid use disorder (OUD).
Objectives:
We evaluated how patient reports of using illicit opioids (i.e., heroin or non-prescription pain medications) are linked to perceptions of loneliness in a sample of adults receiving methadone maintenance treatment (MMT), and whether this link varies by gender.
Methods:
Participants for this cross-sectional observational study included 371 MMT patients aged 18 and older drawn from four opioid treatment programs in Southern New England and the Pacific Northwest. Patients completed a self-administered survey assessing sociodemographic and health information, loneliness, illicit opioid use, and MMT characteristics. Logistic regressions were estimated to examine the link between patient odds of illicit opioid use in the past month and perceived loneliness.
Results:
Patient gender moderated the association between illicit opioid use and loneliness such that severe loneliness was associated with higher odds of using illicit opioids among women (OR = 3.00, 95% CI [1.19, 7.57], p = .020) but lower odds of using illicit opioids among men (OR = 0.35, 95% CI [0.14, 0.87], p = .024), accounting for age, marital status, work status, depressive symptoms, and MMT characteristics (treatment episode, treatment duration, and methadone dose).
Conclusions/Importance:
This study underscores the importance of considering loneliness in the management of OUD. Routine clinical care and treatment may benefit from strategies to build and sustain social connections that support long-term recovery among MMT patients.
Keywords: opioid use disorder, methadone maintenance, loneliness, gender differences
Introduction
Loneliness is understood as the perceived discrepancy between one’s actual and desired social relationships (Peplau, Russell, & Heim, 1979). Heightened perceptions of loneliness are common among individuals with substance use disorders and linked to increased likelihood of relapse (e.g., Laudet, Magura, Vogel, & Knight, 2004; Levy, 2008). Nevertheless, research has primarily focused on problematic alcohol use, limiting knowledge of how loneliness may impact recovery for people who misuse other substances. With the present health crisis surrounding the misuse of opioids, it is critical to consider the implications of loneliness for people with opioid use disorder (OUD). The use of illicit opioids (i.e., heroin or non-prescription pain medications) among patients treated for OUD is a particularly important outcome because it is a key indicator of treatment response. In this study, we evaluated the link between the use of illicit opioids and loneliness among adult patients enrolled in methadone maintenance treatment (MMT), a widely applied medication assisted approach for OUD (Alderks, 2017). Loneliness may be a stronger risk factor for substance misuse among women than men (e.g., Mannes et al., 2016; Page & Cole, 1991), and so we also determined whether the association between illicit opioid use and loneliness varied by gender.
Loneliness and Substance Use
Loneliness in adult samples is associated with using alcohol and tobacco (Cacioppo et al., 2002; Greene et al., 2018; Shankur, McMunn, Banks, & Steptoe, 2011; Stanton, Moadel, Kim, Weinberger, & Shuter, 2015), greater use of sedatives and other psychotropic drugs (Boehlen et al., 2015; Taipale et al., 2011), and problematic drinking patterns (Bonin et al., 2000; Nordmyr, Forsman, & Österman, 2016; Stickley et al., 2013). Feeling lonely also appears to place people with many types of psychopathology at risk for substance misuse. Among non-depressed adults with schizophrenia or schizoaffective disorder, for example, loneliness predicts a diagnosis of drug misuse or dependence and a higher number of drugs used (Trémeau, Antonius, Malaspina, Goff, & Javitt, 2016). Furthermore, persons in recovery from co-occurring serious mental illness and substance use disorders report that loneliness is a major trigger for relapse (Laudet et al., 2004). This research suggests that loneliness may be an understudied risk factor for illicit opioid use among MMT patients.
People who are lonely may use substances for several reasons. First, loneliness might precede substance use to diminish negative emotions (Schonfeld, Rohrer, Dupree, & Thomas, 1989). Young gay men, for instance, report “self-treating” their loneliness with drug use (Hubach, DiStefano, & Wood, 2012). Likewise, older adults at risk for alcohol problems drink to relieve loneliness (Immonen Valvanne, & Pitkälä, 2011), and people who increase their alcohol use in later life attribute such increases to feeling lonely (Khan, Wilkinson, & Keeling, 2006). Second, individuals who are lonely have limited psychosocial resources to cope with stress using drug-free strategies. These individuals often report poor self-regulation, depressive symptoms, and social isolation, all of which disrupt the use of adaptive coping behaviors (Hawkley & Cacioppo, 2010; Ong, Uchino, & Wethington, 2016). Third, loneliness likely generates stress that contributes to substance use. In a sample of heavy drinking gay men, for example, loneliness mediated the link between stress and problematic alcohol consumption (Kuerbis et al., 2017). Among young adults, loneliness predicted increased stress which was associated with greater alcohol and prescription drug use (Segrin, McNelis, & Pavlich, 2018). Relatedly, people with alcohol use disorder who are lonely suffer psychosocial stress that aggravates problem drinking such as lower marital and job satisfaction (Medora & Woodward, 1991). As a whole, this work suggests that loneliness may be a key source of psychosocial stress that impacts MMT outcomes.
Loneliness in the context of MMT.
Little is known about the implications of loneliness for MMT patients. Research indicates, however, that patients receiving MMT view loneliness as a persistent challenge that encompasses multiple components including felt social inadequacy, interpersonal isolation, and self-alienation (Bahna & Gordon, 1978; Orzeck & Rokach, 2004; Wermuth et al., 1987). Patients with few supportive social connections tend to have particularly negative attitudes toward methadone such as perceiving it as an addiction, highly stigmatizing, and disempowering (Gourlay, Ricciardelli, & Ridge, 2005; Tomori et al., 2014). In addition, MMT patients are often addicted to heroin, which is generally viewed by society as criminal behavior. This criminalization may intensify social exclusion and marginalization (Ahern, Stuber, & Galea, 2007). Perhaps partly as a result of these circumstances, MMT patients have been found to attribute their perceived isolation and lack of connectedness to drug use, difficulty with treatment adherence, and ineffective illness management (Batchelder et al., 2013; Simmonds, Finley, Vale, Pugh, & Turner, 2015). Patients also report using opioids to self-medicate social pain and combat feelings of alienation, potentially exacerbating risk factors for overdose such as bingeing and mixing drugs (Bennett, Elliott, Golub, Wolfson-Stofko, & Guarino, 2017). Taken together, previous research highlights the need for a better understanding of the association between illicit opioid use and loneliness among MMT patients.
Potential gender differences.
To deliver targeted clinical care and interventions for people with OUD, knowledge of possible gender differences in the link between illicit opioid use and loneliness is needed. Compared with men, women encounter greater emotional strain from interpersonal problems (Birditt & Fingerman, 2003; Mohr et al., 2003) and are more likely to seek social support to cope with stress (Bonin et al., 2000), both of which might amplify the detrimental consequences of loneliness. Whereas some studies indicate that loneliness has similar implications for problematic drinking in women and men (Bonin et al., 2000), others show that loneliness is especially consequential for women’s heavy use of alcohol and illicit drugs (Mannes et al., 2016; Page & Cole, 1991). Moreover, among patients in treatment for substance use disorders, loneliness is reported as a primary reason for relapse in women but not men (Levy, 2008). These findings raise the question of whether loneliness is more strongly linked to illicit opioid use among women than men enrolled in MMT.
The Present Study
This study extends the literature by evaluating the association between illicit opioid use and loneliness among a multi-site sample of MMT patients. We hypothesized that patients would be significantly more likely to report illicit opioid use when they had moderate or severe loneliness relative to little or no loneliness, controlling for patient and treatment characteristics (treatment episode, treatment duration, and methadone dose) that are associated with MMT outcomes (Nosyk et al., 2009; Proctor et al., 2016; Vigna-Taglianti et al., 2016; Ward, Mattick, & Hall, 1998). We further predicted that the association between illicit opioid use and loneliness would be significantly stronger for women than for men. We controlled for age, marital status, work status, and depressive symptoms as potential confounding factors that are linked to both illicit opioid use (e.g., Havard, Teesson, Darke, & Ross, 2006; Proctor et al., 2016; Vigna-Taglianti et al., 2016) and loneliness (e.g., Cacioppo, Hawkley, & Thisted, 2010; Ge, Yap, Ong, & Heng, 2017; Hawkley, Browne, & Cacioppo, 2005; Luhmann & Hawkley, 2016).
Methods
Participants and Procedures
The sample for this cross-sectional study was recruited from four opioid treatment programs in Southern New England (n = 384) and the Pacific Northwest (n = 100) in 2017.
Participants included 484 MMT patients aged 18 and older. Individuals presenting for methadone dosing or group support/counseling as part of their treatment were invited by the investigators and other clinical staff to complete an anonymous self-administered paper survey assessing their sociodemographic and health information, substance use patterns, psychosocial functioning, and MMT characteristics and outcomes. An informed consent document was included with each survey. Individuals were excluded if they were under 18 or not fluent in English. Response rates could not be determined due to logistical barriers associated with recruiting participants during methadone administration. This study was approved by the Institutional Review Boards of Dartmouth College and Spectrum Health Services.
We removed two patients who self-identified as gender nonconforming and seven patients with missing data on gender to allow for the statistical comparison of patients who identified as men and women. Of the remaining 475 patients, 3.4% had missing data on illicit opioid use and 10.0% had missing data on loneliness. With regard to covariates, 11.2% had missing data on depressive symptoms and 3.4% or less had missing data on each of the remaining variables. The final analytic sample included 371 patients (M = 40.26 years, SD = 11.20, range = 20 – 70) with complete data. Compared with the 111 patients who were removed because of missing data, the 371 patients in this study were younger (t(134.26) = −2.95, p = .004) but did not significantly differ in their gender, marital status, work status, treatment episode, treatment duration, methadone dose, depressive symptoms, loneliness, or illicit opioid use.
Measures
Illicit opioid use.
Patients were asked, “Which best describes your illegal opioid use (heroin or non-prescription pain killers) during the past four weeks,” with the following response options: every day, at least once a week, once a month, and did not use. This item is similar to those in used in the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), which measures frequency of non-medical substance use in the past three months and has good reliability and validity (Ali et al., 2002; Humeniuk et al., 2008; McNeely et al., 2014). Illicit opioid use was assessed in the past four weeks to more closely align with the current MMT episode for all patients, some of whom had been in treatment for a month or less. We created a variable to assess whether or not patients used illicit opioids (1 = reported illicit opioid use, 0 = no reported illicit opioid use).
Loneliness.
Patient loneliness was assessed using the three-item loneliness scale adapted from the Revised UCLA Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, 2004). This measure is commonly used in survey research and has demonstrated good internal consistency as well as both concurrent and discriminant validity (Hughes et al., 2004). The three-item loneliness scale has established reliability and construct validity in studies of young, middle-aged, and older adults (e.g., Ge et al., 2017; Rico-Uribe et al., 2016; Shiovitz-Ezra & Leitsch, 2010). Patients were asked how frequently they: (a) lack companionship; (b) feel left out; and (c) feel isolated from others (1 = hardly ever, 2 = some of the time, 3 = often). Summed scores were calculated (range = 3 – 9; α = .83). On the basis of prior research (Boehlen et al., 2015; Lasgaard, Friis, & Shevlin, 2016), we categorized patients as having little or no loneliness (scores of 3 – 4), moderate loneliness (scores of 5 – 6), or severe loneliness (scores of 7 – 9).
Gender.
Patient gender was coded as 1 (female) or 0 (male).
Covariates.
Covariates included patient age in years, marital status (1 = currently married, 0 = not currently married), work status (1 = currently employed full-time or part-time, 0 = currently unemployed or on disability), and depressive symptoms. Depressive symptoms were measured with the reliable and valid two-item Patient Health Questionnaire depression module (PHQ-2; Kroenke, Spitzer, & Williams, 2003). Patients were asked how often in the past two weeks they were bothered by: (a) having little interest or pleasure in doing things; and (b) feeling down, depressed, or hopeless (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day). Summed scores were created (range = 0 – 6). The Spearman-Brown coefficient, which is recommended for two-item scales (Eisinga, Grotenhuis, & Pelzer, 2013), was .86.
We also controlled for treatment episode (1 = first time in opioid treatment, 0 = had previous opioid treatment), treatment duration, and methadone dose (mg/day). Treatment duration was assessed from patient reports of how long they have been in MMT (1 = less than 30 days, 2 = 1 month to 1 year, 3 = 2–5 years, 4 = 6–10 years, 5 = 11–19 years, 6 = 20–29 years, 7 = 30 or more years). To account for differences in illicit opioid use among patients in MMT long enough to be stable on methadone (Ward et al., 1998), we examined whether patients received MMT for two or more years versus less than 2 years (1 = 2 years or more, 0 = less than 2 years).
Statistical Analysis
Logistic regressions were estimated to evaluate whether patient reports of loneliness are independently associated with odds of reporting illicit opioid use. In the first step of the model, we entered patient loneliness as the predictor (1 = little or no loneliness, 2 = moderate loneliness, 3 = severe loneliness), along with patient gender, age, marital status, work status, and depressive symptoms, and MMT characteristics (treatment episode, treatment duration, and methadone dose) as covariates. Little or no loneliness was considered as the reference group. In the second step of the model, we included an interaction term between patient loneliness and patient gender (e.g., patient loneliness X patient gender) to test whether links between patient illicit opioid use and loneliness varied for male and female patients. Continuous covariates were grand mean centered before the analysis. We explored the nature of significant gender interactions by estimating simple slopes for women and men. Models were estimated using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Background characteristics and scores on study variables for female patients (n = 172) and male patients (n = 199) are shown in Table 1. Patient gender differences on major variables were tested in preliminary analyses using independent t tests and Pearson chi-square tests. Relative to male patients, female patients were less likely to be employed (χ2(1, N = 371) = 13.68, p < .001) and had higher methadone doses (t(369) = 2.20, p = .029). There were no significant gender differences in age, marital status, depressive symptoms, treatment episode, treatment duration, loneliness, or illicit opioid use.
Table 1.
Patient Background Characteristics and Scores on Study Variables
| Female Patients (n = 172) |
Male Patients (n = 199) |
|||||
|---|---|---|---|---|---|---|
| Variable | M | SD | Range | M | SD | Range |
| Age in years | 39.51 | 11.05 | 20–69 | 40.91 | 11.31 | 25–70 |
| Methadone dose (mg/day) | 87.94* | 40.76 | 6–240 | 78.72 | 39.95 | 3–225 |
| Depressive symptomsb | 2.72 | 1.95 | 0–6 | 2.61 | 1.97 | 0–6 |
| % | ||||||
| Educational attainment | ||||||
| Less than high school | 14.0 | 18.1 | ||||
| Completed high school | 28.5 | 31.7 | ||||
| Some college | 39.5 | 36.2 | ||||
| College graduate | 16.9 | 14.1 | ||||
| Work status (employed) | 30.8*** | 49.7 | ||||
| Marital status | ||||||
| Single/never married | 57.0 | 61.8 | ||||
| Married | 11.0 | 15.6 | ||||
| Separated | 8.7 | 3.0 | ||||
| Divorced | 18.6 | 17.1 | ||||
| Widowed | 4.7 | 2.5 | ||||
| Treatment episode (first) | 39.5 | 39.7 | ||||
| Treatment duration | ||||||
| Less than 30 days | 0.0 | 1.0 | ||||
| 1 month to 1 year | 33.7 | 26.6 | ||||
| 2–5 years | 39.5 | 42.7 | ||||
| 6–10 years | 12.2 | 16.6 | ||||
| 11 or more years | 14.5 | 13.0 | ||||
| Illicit opioid use | ||||||
| Did not use | 69.2 | 66.8 | ||||
| Once a month | 12.2 | 9.5 | ||||
| At least once a week | 11.0 | 16.1 | ||||
| Every day | 7.6 | 7.5 | ||||
| Lonelinessb | ||||||
| Little or none (scores of 3 – 4) | 41.3 | 41.2 | ||||
| Moderate (scores of 5 – 6) | 30.2 | 34.7 | ||||
| Severe (scores of 7 – 9) | 28.5 | 24.1 | ||||
Note. OUD = opioid use disorder.
Sum of two items (having little interest or pleasure and feeling down, depressed, or hopeless) ranging from 0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day.
Sum of three items (lacking companionship, feeling left out, and feeling isolated) ranging from1 = hardly ever, 2 = some of the time, 3 = often
Gender difference at p < .05.
Gender difference at p < .001.
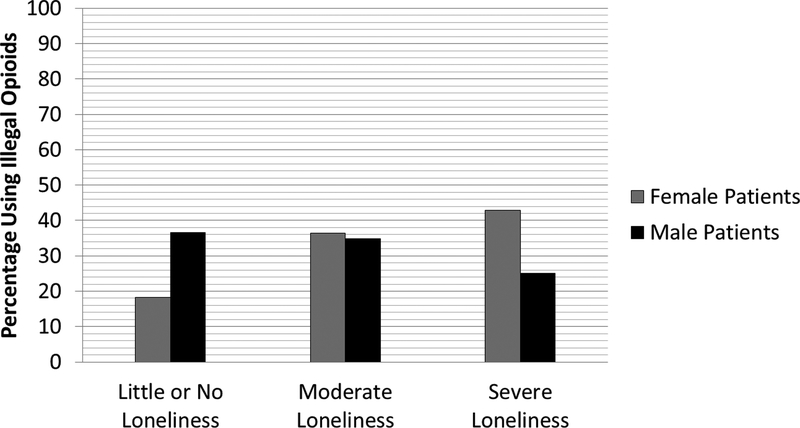
Illicit opioid use in the past month was reported by almost one-third (32.1%) of the total sample of 371 patients. Overall, roughly one in four patients (26.1%) were categorized as having severe loneliness, indicating that loneliness was prevalent in this sample. Figure 1 shows the prevalence of illicit opioid use by level of loneliness among male and female patients. Women were more likely to report illicit opioid use when they had severe loneliness (42.9%) versus little or no loneliness (18.3%) or moderate loneliness (36.5%), whereas men were more likely to report illicit opioid use when they had little or no loneliness (36.6%) versus moderate loneliness (34.8%) or severe loneliness (25.0%).
Figure 1.
The percentage of female and male patients reporting illicit opioid use by levels of reported loneliness: little or no loneliness (scores of 3 – 4), moderate loneliness (scores of 5 – 6), and severe loneliness (scores of 7 – 9).
Association Between Patient Illicit Opioid Use and Loneliness
Table 2 displays findings from the logistic regressions estimating the link between patient reports of illicit opioid use and loneliness. There was no significant direct association between patient reports of illicit opioid use and loneliness. Patient gender, however, moderated the link between illicit opioid use and both moderate loneliness (p = .042) and severe loneliness (p = .0006). Female patients reporting severe loneliness had 3.00 times higher odds of using illicit opioids relative to those reporting little or no loneliness (OR = 3.00, 95% CI [1.19, 7.57], p = .020). By contrast, male patients reporting severe loneliness had 0.35 times lower odds of using illicit opioids compared with those who reported little or no loneliness (OR = 0.35, 95% CI [0.14, 0.87], p = .024). Put differently, male patients with little or no loneliness were 2.86 times more likely to report illicit opioid use than male patients with severe loneliness (OR = 2.86, 95% CI [1.15, 7.14]). Neither female patients (OR = 2.03, 95% CI [0.85, 4.85], p = .113) nor male patients (OR = 0.63, 95% CI [0.30, 1.31], p = .215) with moderate loneliness significantly differed in their illicit opioid use from their counterparts who reported little or no loneliness.
Table 2.
Logistic Regression Estimating the Association Between Patient Illicit Opioid Use and Loneliness
|
Illicit Opioid Use |
||||
|---|---|---|---|---|
| Parameter | B | SE | OR | 95% CI |
| Step 1 | ||||
| Moderate lonelinessa | 0.05 | 0.29 | 1.05 | 0.60, 1.84 |
| Severe lonelinessa | −0.01 | 0.33 | 0.99 | 0.51, 1.90 |
| Gender (female) | −0.08 | 0.24 | 0.92 | 0.57, 1.48 |
| Age in years | −0.01 | 0.01 | 1.00 | 0.97, 1.02 |
| Marital status (married) | −0.77 | 0.40 | 0.46 | 0.21, 1.01 |
| Work status (employed) | 0.53* | 0.26 | 1.69 | 1.01, 2.83 |
| Depressive symptoms | 0.21** | 0.07 | 1.23 | 1.07, 1.42 |
| Treatment episode (first) | −0.46 | 0.25 | 0.63 | 0.39, 1.03 |
| Treatment duration (2 years or more) | −0.87*** | 0.25 | 0.42 | 0.26, 0.69 |
| Methadone dose (mg/day) | −0.004 | 0.003 | 1.00 | 0.99, 1.00 |
| AIC | 455.98 | |||
| Step 2 | ||||
| Moderate lonelinessa | −0.47 | 0.38 | ||
| Severe lonelinessa | −1.05* | 0.47 | ||
| Gender (female) | −1.12** | 0.42 | ||
| Moderate loneliness X Gender | 1.17* | 0.58 | ||
| Severe loneliness X Gender | 2.15*** | 0.63 | ||
| Age in years | −0.01 | 0.01 | 0.99 | 0.97, 1.01 |
| Marital status (married) | −0.91* | 0.41 | 0.40 | 0.18, 0.90 |
| Work status (employed) | 0.41 | 0.27 | 1.50 | 0.88, 2.55 |
| Depressive symptoms | 0.21** | 0.07 | 1.24 | 1.07, 1.43 |
| Treatment episode (first) | −0.49 | 0.25 | 0.61 | 0.37, 1.01 |
| Treatment duration (2 years or more) | −0.91*** | 0.26 | 0.41 | 0.24, 0.67 |
| Methadone dose (mg/day) | −0.01 | 0.003 | 1.00 | 0.99, 1.00 |
| AIC | 447.36 | |||
Note. AIC = Akaike information criterion.
Little or no loneliness is the reference group. N = 371 patients.
p < .05.
p < .01.
p < .001.
Discussion
The present study suggests that loneliness may be consequential in evaluating treatment response among MMT patients. In line with our hypothesis, female patients were significantly more likely to use illicit opioids when they reported severe loneliness. Contrary to prediction, however, male patients who reported severe loneliness had significantly lower odds of using illicit opioids. These findings were observed over and above treatment characteristics and a host of possible confounding factors including age, marital status, work status, depressive symptoms. Nearly one-third of patients in this study reported the use of illicit opioids in the past month and about one in four patients reported severe loneliness. This indicates that these concerns may be common among MMT patients, which underscores the potential value of considering the link between illicit opioid use and loneliness in this population.
There are a number of plausible explanations for why loneliness is linked to higher odds of using illicit opioids among women but not men. Compared with their male counterparts, female MMT patients have fewer resources and more risk factors for substance misuse (e.g., a drug-using romantic partner, physical and/or psychiatric comorbidities) that may make social relationships particularly central to their recovery (Bawor et al., 2015; Grella, Joshi, & Anglin, 2003; Puigdollers et al., 2004; Vigna-Taglianti et al., 2016). Moreover, loneliness is associated with increased risk of coronary heart disease among women but not men, beyond the effects of sociodemographic characteristics, medical comorbidities, and health behaviors (Thurston & Kubzansky, 2009). Thus, female patients may be more physiologically reactive to feeling lonely than male patients, perhaps rendering them more likely to use opioids as a coping strategy. Supporting this possibility, women (but not men) show increased alcohol consumption while alone and at home when they report higher levels of loneliness on the previous day (Arpin, Mohr, & Brannan, 2014). Disentangling the pathways through which loneliness is linked to illicit opioid use among women receiving MMT will inform targeted treatment to facilitate sustainable recovery.
The finding that men receiving MMT were significantly less likely to use opioids when they reported severe loneliness versus little or no loneliness was unexpected and suggests that loneliness may function differently for male and female patients. Whereas women typically focus on the degree of emotional closeness and intimacy in their relationships to evaluate their own loneliness, men have been found to use more structural criteria such as social network density (i.e., the extent to which network members have relationships with one another, for instance, friends of friends) (Stokes & Levin, 1986). Male patients with severe loneliness may be less likely to use illicit opioids in part because they have smaller and less connected social networks with fewer opportunities to obtain these drugs than those with little or no loneliness. Contact within a network that includes one or more drug-using members can affect drug availability, the number and frequency of drug cues, and social pressure to use drugs (Day et al., 2013; Havassy, Wasserman, & Hall, 1995). Male MMT patients with severe loneliness may, therefore, have minimal social influences to maintain their illicit opioid use. Alternatively, male patients who abstain from opioids may become severely lonely as a result of distancing themselves from drug-using network members who do not support their recovery. Men with severe loneliness might be less vulnerable to relapse during MMT; still, it is important to note that loneliness may have indirect adverse effects that warrant clinical attention. Loneliness predicts increased depressive symptoms over time among both younger and older adults (Cacioppo, Hawkley, & Thisted, 2010; Vanhalst, Luyckx, Teppers, & Goossens, 2012), and depression has been linked to heavier use of illicit drugs, more risk-taking behaviors, worse physical health, and greater psychopathology among OUD patients in MMT or buprenorphine treatment (Havard et al., 2006). Future studies should explore how loneliness is associated with other outcomes among male patients that impact their well-being and treatment response.
The present cross-sectional findings suggest that clinical guidance in drug-free strategies to manage loneliness during MMT may be beneficial. Interpersonal relationships can either promote or hinder recovery, and so it might be clinically valuable to consider characteristics of the patient’s social network. People with OUD, for example, often have drug-using family members and friends who play a powerful role in maintaining illicit opioid use (Day et al., 2013; Gogineni, Stein, & Friedmann, 2001; Havassy et al., 1995; Moshier et al., 2012). Encouraging patients to build new connections within a recovery community may offer an alternative social network that supports abstinence and minimizes loneliness. Indeed, developing relationships with abstinent peers has been found to help women with a history of trauma and substance misuse feel less alone (Harris, Fallot, & Berley, 2005).
It is worth noting that the loneliness scale in this study is a rather brief and indirect assessment that has mostly been used with older adults and may overlap with related constructs such as social isolation, social support, and social network size. Studies have shown that perceptions of loneliness are distinct from these elements of social relationships (e.g., Cacioppo et al., 2010; Ge et al., 2017; Rico-Uribe et al., 2016), yet subsequent work is needed to better understand the link between illicit opioid use and loneliness. Indirect measures of loneliness (e.g., asking people about feeling isolated or left out) may also underestimate its occurrence relative to direct measures which ask about feeling lonely (Shiovitz-Ezra & Ayalon, 2012). Future research should incorporate both direct and indirect assessments of loneliness as well as other components of social relationships among MMT patients.
Strengths of this study include a relatively large multi-site sample of MMT patients; patients ranging in age from young adulthood to older adulthood; data on numerous patient and treatment characteristics; and the statistical comparison of gender differences. Multivariate analyses controlled for an array of possible confounding variables, demonstrating that patient reports of loneliness have robust links to illicit opioid use. Consequently, the present findings generate a novel contribution to research on MMT and add to a burgeoning literature on the importance of psychosocial factors in substance use, misuse, and treatment.
We acknowledge several limitations. First and foremost, we cannot determine causal associations in a cross-sectional study. It may be, for instance, that women who use illicit opioids during MMT have a tendency to isolate from their loved ones, leading to higher levels of loneliness. Subsequent research is needed to investigate the dynamic association between illicit opioid use and loneliness over time. Second, the self-selected sample and self-reported measure of illicit opioid use could introduce bias. Future studies should include objective assessments of opioid use (e.g., urinalysis drug screens). Third, we controlled for patients’ marital status but lacked additional data on their living condition (e.g., whether patients lived alone or with others) and social network characteristics (e.g., number and quality of social relationships, number of drug-using relatives and friends), which might be associated with loneliness and/or illicit opioid use. We also lacked data on other OUD-related factors that are linked to illicit opioid use such as craving for opioids and withdrawal symptoms. Fourth, patients in this study were selected as a convenience sample, and so they may not be broadly representative of people receiving MMT. Fifth, given that the rates of missing data in the larger sample were 10.0% and 11.2% loneliness and depressive symptoms, respectively, patients with greater loneliness and/or greater depressive symptoms may have been less likely to provide a response to these measures. This represents a potential bias, and so the findings from this study may not generalize to MMT patients who are highly distressed. Last, the findings are specific to MMT and might not generalize to patients enrolled in alternative treatments for OUD (e.g., buprenorphine). Nonetheless, this study lays groundwork for future research to ascertain how and under what conditions loneliness may influence treatment outcomes among people with OUD.
Conclusions
In summary, this study indicates that perceived loneliness may be a key psychosocial factor which contributes to treatment response among individuals receiving MMT. Although additional research is needed, the current findings suggest that loneliness should be considered in the comprehensive clinical care of MMT patients. Routine clinical care and treatment may be enhanced with strategies to mitigate feelings of loneliness and leverage social connections that support the lasting recovery of individuals managing OUD.
Funding:
This work was supported by the National Institute of Mental Health under Grant number T32 MH073553–11. Courtney A. Polenick is supported by grant K01AG059829 from the National Institute on Aging. The funding organizations had no role in any of the following: design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Disclosure of interest: The authors report no conflict of interest.
References
- Ahern J, Stuber J, & Galea S (2007). Stigma, discrimination and the health of illicit drug users. Drug and Alcohol Dependence, 88(2–3), 188–196. 10.1016/j.drugalcdep.2006.10.014 [DOI] [PubMed] [Google Scholar]
- Alderks CE (2017). Trends in the use of methadone, buprenorphine, and extended-release naltrexone at substance abuse treatment facilities: 2003–2015 (Update) The CBHSQ Report. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from: https://www.samhsa.gov/data/sites/default/files/report_3192/ShortReport-3192.pdf. [PubMed] [Google Scholar]
- Ali R, Awwad E, Babor T, Bradley F, Butau T, Farrell M, … Vendetti J (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction, 9(9), 1183–1194. 10.1046/j.1360-0443.2002.00185.x [DOI] [PubMed] [Google Scholar]
- Arpin SN, Mohr CD, & Brannan D (2015). Having friends and feeling lonely: A daily process examination of transient loneliness, socialization, and drinking behavior. Personality and Social Psychology Bulletin, 41(5), 615–628. 10.1177/0146167215569722 [DOI] [PubMed] [Google Scholar]
- Bahna G, & Gordon NB (1978). Rehabilitation experiences of women ex-addicts in methadone treatment. International Journal of the Addictions, 13(4), 639–655. 10.3109/10826087809039291 [DOI] [PubMed] [Google Scholar]
- Batchelder AW, Brisbane M, Litwin AH, Nahvi S, Berg KM, & Arnsten JH (2013). “Damaging what wasn’t damaged already”: Psychological tension and antiretroviral adherence among HIV-infected methadone-maintained drug users. AIDS Care, 25(11), 1370–1374. 10.1080/09540121.2013.766303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bawor M, Dennis BB, Varenbut M, Daiter J, Marsh DC, Plater C, … Samaan Z (2015). Sex differences in substance use, health, and social functioning among opioid users receiving methadone treatment: A multicenter cohort study. Biology of Sex Differences, 6:21 10.1186/s13293-015-0038-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett AS, Elliott L, Golub A, Wolfson-Stofko B, & Guarino H (2017). Opioid-involved overdose among male Afghanistan/Iraq-era US Military Veterans: A multidimensional perspective. Substance Use and Misuse, 52(13), 1701–1711. 10.1080/10826084.2017.1306563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, & Fingerman KL (2003). Age and gender differences in adults’ descriptions of emotional reactions to interpersonal problems. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58(4), P237–P245. 10.1093/geronb/58.4.P237 [DOI] [PubMed] [Google Scholar]
- Boehlen F, Herzog W, Quinzler R, Haefeli WE, Maatouk I, Niehoff D, … Wild B (2015). Loneliness in the elderly is associated with the use of psychotropic drugs. International Journal of Geriatric Psychiatry, 30(9), 957–964. 10.1002/gps.4246 [DOI] [PubMed] [Google Scholar]
- Bonin MF, McCreary DR, & Sadava SW (2000). Problem drinking behavior in two community-based samples of adults: Influence of gender, coping, loneliness, and depression. Psychology of Addictive Behaviors, 14(2), 151–161. 10.1037/0893-164X.14.2.151 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, … Bernston GG (2002). Loneliness and health: Potential mechanisms. Psychometric Medicine, 64(3), 407–417. 10.1097/00006842-200205000-00005 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day E, Copello A, Karia M, Roche J, Grewal P, George S, … Chohan G (2013). Social network support for individuals receiving opiate substitution treatment and its association with treatment progress. European Addiction Research, 19(4), 211–221. 10.1159/000343827 [DOI] [PubMed] [Google Scholar]
- Eisinga R, Grotenhuis M, & Pelzer B (2013). The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health, 5(4), 637–642. 10.1007/s00038-012-0416-3 [DOI] [PubMed] [Google Scholar]
- Ge L, Yap CW, Ong R, & Heng BH (2017). Social isolation, loneliness and their relationships with depressive symptoms: A population-based study. PLoS ONE 12(8): e0182145 10.1371/journal.pone.0182145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogineni A, Stein MD, & Friedmann PD (2001). Social relationships and intravenous drug use among methadone maintenance patients. Drug and Alcohol Dependence, 64(1), 47–53. 10.1016/S0376-8716(00)00230-1 [DOI] [PubMed] [Google Scholar]
- Gourlay J, Ricciardelli L, & Ridge D (2005). Users’ experiences of heroin and methadone treatment. Substance Use and Misuse, 40(12), 1875–1882. 10.1080/10826080500259497 [DOI] [PubMed] [Google Scholar]
- Greene M, Hessol NA, Perissinotto C, Zepf R, Parrott AH, Foreman C, … John M (2018). Loneliness in older adults living with HIV. AIDS and Behavior, 22(5), 1475–1484. 10.1007/s10461-017-1985-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Joshi V, & Anglin MD (2003). Gender differences and treatment outcomes among methadone patients in the Drug Abuse Treatment Outcome Study. Journal of Maintenance Addiction, 2(1/2), 103–128. 10.1300/J126v02n01_07 [DOI] [Google Scholar]
- Harris M, Fallot RD, & Berley RW (2005). Qualitative interviews on substance abuse relapse and prevention among female trauma survivors. Psychiatric Services, 56(10), 1292–1296. 10.1176/appi.ps.56.10.1292 [DOI] [PubMed] [Google Scholar]
- Havard A, Teesson M, Darke S, & Ross J (2006). Depression among heroin users: 12-month outcomes from the Australian Treatment Outcome Study (ATOS). Journal Substance Abuse Treatment, 30(4), 355–362. 10.1016/j.jsat.2006.03.012 [DOI] [PubMed] [Google Scholar]
- Havassy BE, Wasserman DA, & Hall SM (1995). Social relationships and abstinence from cocaine in an American treatment sample. Addiction, 90(5), 699–710. 10.1111/j.1360-0443.1995.tb02208.x [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Browne MW, Cacioppo JT (2005). How can I connect with thee? Let me count the ways. Psychological Science, 16(10), 798–804. 10.1111/j.1467-9280.2005.01617.x [DOI] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Hubach RD, DiStefano AS, & Wood MM (2012). Understanding the influence of loneliness on HIV risk behavior in young men who have sex with men. Journal of Gay and Lesbian Social Services, 24(4), 371–395. 10.1080/10538720.2012.721676 [DOI] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk RE, Ali RA, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, … Simon S (2008). Validation of the Alcohol Smoking and Substance Involvement Screening Test (ASSIST). Addiction 103(6), 1039–1047. 10.1111/j.1360-0443.2007.02114.x [DOI] [PubMed] [Google Scholar]
- Immonen S, Valvanne J, & Pitkälä KH (2011). Older adults’ own reasoning for their alcohol consumption. International Journal of Geriatric Psychiatry, 26(11), 1169–1176. 10.1002/gps.2657 [DOI] [PubMed] [Google Scholar]
- Khan N, Wilkinson TJ, & Keeling S (2006). Reasons for changing alcohol use among older people in New Zealand. Australasian Journal on Ageing, 25(2), 97–100. 10.1111/j.1741-6612.2006.00159.x [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Kuerbis A, Mereish EH, Hayes M, Davis CM, Shao S, & Morgenstern J (2017). Testing cross-sectional and prospective mediators of internalized heterosexism on heavy drinking, alcohol problems, and psychological distress among heavy drinking men who have sex with men. Journal of Studies on Alcohol and Drugs, 78(1), 113–123. 10.15288/jsad.2017.78.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasgaard M, Friis K, & Shevlin M (2016). “Where are all the lonely people?” A population-based study of high-risk groups across the life span. Social Psychiatry and Psychiatric Epidemiology, 51(10), 1373–1384. 10.1007/s00127-016-1279-3 [DOI] [PubMed] [Google Scholar]
- Laudet AB, Magura S, Vogel HS, & Knight EL (2004). Perceived reasons for substance misuse among persons with a psychiatric disorder. American Journal of Orthopsychiatry, 74(3), 365–375. 10.1037/0002-9432.74.3.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy MS (2008). Listening to our clients: The prevention of relapse. Journal of Psychoactive Drugs, 40(2), 167–172. 10.1080/02791072.2008.10400627 [DOI] [PubMed] [Google Scholar]
- Luhmann M, & Hawkley LC (2016). Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology, 52(6), 943–959. 10.1037/dev0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannes ZL, Burrell LE, Bryant VE, Dunne EM, Hearn LE, & Whitehead NE (2016). Loneliness and substance use: The influence of gender among HIV+ Black/African American adults 50+. AIDS Care, 28(5), 598–602. 10.1080/09540121.2015.1120269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Strauss SM, Wright S, Rotrosen J, Khan R, Lee JD, Gourevitch MN (2014). Test-retest reliability of a self-administered Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in primary care patients. Journal of Substance Abuse Treatment, 47(1), 93–101. 10.1016/j.jsat.2014.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medora NP, & Woodward JC (1991). Factors associated with loneliness among alcoholics in rehabilitation centers. The Journal of Social Psychology, 131(6), 769–779. 10.1080/00224545.1991.9924664 [DOI] [PubMed] [Google Scholar]
- Mohr CD, Armeli S, Ohannessian CM, Tennen H, Carney A, & Affleck G (2003). Daily interpersonal experiences and distress: Are women more vulnerable? Journal of Social and Clinical Psychology, 22(4), 393–423. 10.1521/jscp.22.4.393.22895 [DOI] [Google Scholar]
- Moshier SJ, McHugh RK, Calkins AW, Hearon BA, Rosellini AJ, Weitzman ML, & Otto MW (2012). The role of perceived belongingness to a drug subculture among opioid-dependent patients. Psychology of Addictive Behaviors, 26(4), 812 10.1037/a0029107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordmyr J, Forsman AK, & Österman K (2016). Problematic alcohol use and problem gambling: Associations to structural and functional aspects of social ties in a Finnish population sample. Nordic Studies on Alcohol and Drugs, 33(4), 381–398. 10.1515/nsad-2016-0032 [DOI] [Google Scholar]
- Nosyk B, MacNab YC, Sun H, Fischer B, Marsh DC, Schechter MT, & Anis AH (2009). Proportional hazards frailty models for recurrent methadone maintenance. American Journal of Epidemiology, 170(6), 783–792. 10.1093/aje/kwp186 [DOI] [PubMed] [Google Scholar]
- Ong AD, Uchino BN, & Wethington E (2016). Loneliness and health in older adults: A mini-review and synthesis. Gerontology, 62(4), 443–449. 10.1159/000441651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orzeck T, & Rokach A (2004). Men who abuse drugs and their experience of loneliness. European Psychologist, 9(3), 163–169. 10.1027/1016-9040.9.3.163 [DOI] [Google Scholar]
- Page RM, & Cole GE (1991). Loneliness and alcoholism risk in late adolescence: A comparative study of adults and adolescents. Adolescence, 26(104), 925–930. [PubMed] [Google Scholar]
- Peplau LA, Russell D, & Heim M (1979). The experience of loneliness In Frieze IH, Bar-Tal D, & Caroll JS (Eds.), New approaches to social problems (pp. 53–78). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Proctor SL, Copeland AL, Kopak AM, Hoffmann NG, Herschman PL, & Polukhina N (2016). Outcome predictors for patients receiving methadone maintenance treatment: Findings from a retrospective multi-site study. Journal of Substance Use, 21(6), 601–613. 10.3109/14659891.2015.1118564 [DOI] [Google Scholar]
- Puigdollers E, Domingo-Salvany A, Brugal MT, Torrens M, Alvarós J, Castillo, … Vázquez JM (2004). Characteristics of heroin addicts entering methadone maintenance treatment: Quality of life and gender. Substance Use and Misuse, 39(9), 1353–1368. 10.1081/JA-120039392 [DOI] [PubMed] [Google Scholar]
- Rico-Uribe LA, Caballero FF, Olaya B, Tobiasz-Adamczyk B, Koskinen S, Leonardi M, … Miret M (2016) Loneliness, social networks, and health: A cross-sectional study in three countries. PLoS ONE, 11(1): e0145264 10.1371/journal.pone.0145264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonfeld L, Rohrer GE, Dupree LW, & Thomas M (1989). Antecedents of relapse and recent substance use. Community Mental Health Journal, 25(3), 245–249. 10.1007/BF00754441 [DOI] [PubMed] [Google Scholar]
- Segrin C, McNelis M, & Pavlich CA (2018). Indirect effects of loneliness on substance use through stress. Health Communication, 33(5), 513–518. 10.1080/10410236.2016.1278507 [DOI] [PubMed] [Google Scholar]
- Shankur A, McMunn A, Banks J, & Steptoe A (2011). Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology, 30(4), 377–385. 10.1037/a0022826 [DOI] [PubMed] [Google Scholar]
- Shiovitz-Ezra S & Ayalon L (2012). Use of direct versus indirect approaches to measure loneliness in later life. Research on Aging, 34(5), 572–591. 10.1177/0164027511423258 [DOI] [Google Scholar]
- Shiovitz-Ezra S, & Leitsch S (2010). The role of social relationships in predicting loneliness: The National Social Life, Health and Aging Project (NSHAP). Social Work Research, 34(3), 157–167. 10.1093/swr/34.3.157 [DOI] [Google Scholar]
- Simmonds MJ, Finley EP, Vale S, Pugh MJ, & Turner BJ (2015). A qualitative study of veterans on long-term opioid analgesics: Barriers and facilitators to multimodality pain management. Pain Medicine, 16(4), 726–732. 10.1111/pme.12626 [DOI] [PubMed] [Google Scholar]
- Stanton CA, Moadel AB, Kim RS, Weinberger AH, & Shuter J (2015). Loneliness in HIV-infected smokers. AIDS Care, 27(2), 268–272. 10.1080/09540121.2014.963017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stickley A, Koyanagi A, Roberts B, Richardson E, Abbott P, Tumanov S, & McKee M (2013). Loneliness: Its correlates and association with health behaviours and outcomes in nine countries of the former Soviet Union. PloS One, 8(7), e67978 10.1371/journal.pone.0067978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes J, & Levin I (1986). Gender differences in predicting loneliness from social network characteristics. Journal of Personality and Social Psychology, 51(5), 1069–1074. 10.1037/0022-3514.51.5.1069 [DOI] [PubMed] [Google Scholar]
- Taipale HT, Bell JS, Uusi-Kokko M, Lönnroos E, Sulkava R, & Hartikainen S (2011). Sedative load among community-dwelling people aged 75 years and older: A population-based study. Drugs and Aging, 28(11), 913–925. 10.2165/11597800-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Thurston RC, & Kubzansky LD (2009). Women, loneliness, and incident coronary heart disease. Psychosomatic Medicine, 71(8), 836–842. 10.1097/PSY.0b013e3181b40efc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomori C, Go VF, Huong NM, Binh NT, Zelaya CE, Celentano DD, & Quan VM (2014). “In their perception we are addicts”: Social vulnerabilities and sources of support for men released from drug treatment centers in Vietnam. International Journal of Drug Policy, 25(5), 897–904. 10.1016/j.drugpo.2014.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trémeau F, Antonius D, Malaspina D, Goff DC & Javitt DC (2016). Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Research, 246, 211–217. 10.1016/j.psychres.2016.09.043 [DOI] [PubMed] [Google Scholar]
- Vanhalst J, Luyckx K, Teppers E, & Goossens L (2012). Disentangling the longitudinal relation between loneliness and depressive symptoms: Prospective effects and the intervening role of coping. Journal of Social and Clinical Psychology, 31(8), 810–832. 10.1521/jscp.2012.31.8.810 [DOI] [Google Scholar]
- Vigna-Taglianti FD, Burroni P, Mathis F, Versino E, Beccaria F, Rotelli M, … VEdeTTE Study Group. (2016). Gender differences in heroin addiction and treatment: Results from the VEdeTTE cohort. Substance Use and Misuse, 51(3), 295–309. 10.3109/10826084.2015.1108339 [DOI] [PubMed] [Google Scholar]
- Ward J, Mattick RP, Hall W (1998). How long is long enough? Answers to questions about the duration of methadone maintenance treatment In: Ward J, Mattick RP, & Hall W, Eds., Methadone maintenance treatment and other opiate replacement therapies (pp. 305–336). Amsterdam: Harwood Academic Publishers. [Google Scholar]
- Wermuth L, Brummett S, & Sorensen JL (1987). Bridges and barriers to recovery: Clinical observations from an opiate recovery project. Journal of Substance Abuse Treatment, 4(3–4), 189–196. 10.1016/S0740-5472(87)80013-2 [DOI] [PubMed] [Google Scholar]