By analyzing data from the HVTN 505 efficacy trial of a DNA/recombinant adenovirus 5 (rAd5) vaccine regimen, we found that host genetics, specifically Fc gamma receptor genetic variations, influenced whether receiving the DNA/rAd5 regimen was beneficial, neutral, or detrimental to an individual with respect to HIV-1 acquisition risk. Moreover, Fc gamma receptor genetic variations influenced immune responses to the DNA/rAd5 vaccine regimen. Thus, Fc gamma receptor genetic variations should be considered in the analysis of future HIV vaccine trials and the development of HIV vaccines.
KEYWORDS: Fc gamma receptor, HIV/AIDS vaccine trial, HVTN 505, genetic polymorphisms
ABSTRACT
HIV Vaccine Trials Network (HVTN) 505 was a phase 2b efficacy trial of a DNA/recombinant adenovirus 5 (rAd5) HIV vaccine regimen. Although the trial was stopped early for lack of overall efficacy, later correlates of risk and sieve analyses generated the hypothesis that the DNA/rAd5 vaccine regimen protected some vaccinees from HIV infection yet enhanced HIV infection risk for others. Here, we assessed whether and how host Fc gamma receptor (FcγR) genetic variations influenced the DNA/rAd5 vaccine regimen’s effect on HIV infection risk. We found that vaccine receipt significantly increased HIV acquisition compared with placebo receipt among participants carrying the FCGR2C-TATA haplotype (comprising minor alleles of four FCGR2C single-nucleotide polymorphism [SNP] sites) (hazard ratio [HR] = 9.79, P = 0.035) but not among participants without the haplotype (HR = 0.86, P = 0.67); the interaction of vaccine and haplotype effect was significant (P = 0.034). Similarly, vaccine receipt increased HIV acquisition compared with placebo receipt among participants carrying the FCGR3B-AGA haplotype (comprising minor alleles of the 3 FCGR3B SNPs) (HR = 2.78, P = 0.058) but not among participants without the haplotype (HR = 0.73, P = 0.44); again, the interaction of vaccine and haplotype was significant (P = 0.047). The FCGR3B-AGA haplotype also influenced whether a combined Env-specific CD8+ T-cell polyfunctionality score and IgG response correlated significantly with HIV risk; an FCGR2A SNP and two FCGR2B SNPs influenced whether anti-gp140 antibody-dependent cellular phagocytosis correlated significantly with HIV risk. These results provide further evidence that Fc gamma receptor genetic variations may modulate HIV vaccine effects and immune function after HIV vaccination.
IMPORTANCE By analyzing data from the HVTN 505 efficacy trial of a DNA/recombinant adenovirus 5 (rAd5) vaccine regimen, we found that host genetics, specifically Fc gamma receptor genetic variations, influenced whether receiving the DNA/rAd5 regimen was beneficial, neutral, or detrimental to an individual with respect to HIV-1 acquisition risk. Moreover, Fc gamma receptor genetic variations influenced immune responses to the DNA/rAd5 vaccine regimen. Thus, Fc gamma receptor genetic variations should be considered in the analysis of future HIV vaccine trials and the development of HIV vaccines.
INTRODUCTION
Fc gamma receptors (FcγRs) are expressed on the leukocyte surface and interact with the Fc domain of immunoglobulin G (IgG) antibodies. Interaction of FcγRs with IgG immune complexes initiates intracellular signaling pathways that lead to a variety of downstream events, including cellular activation and cytokine/chemokine production (1, 2). These events can have either immunostimulatory or immunosuppressive effects, making FcγRs major players that modulate a range of processes, including antibody production, antigen presentation, and activation of B cells and innate immune effector cells (3). Interestingly, FcγR genetic variation can have significant functional implications, such as modulating affinity of FcγR binding to antibodies and affecting the level of FcγR expression and effector functions in specific types of immune cells (4–7). Moreover, our sequencing and analysis of exons and the areas surrounding FcγR genes identified significant associations of single-nucleotide polymorphisms (SNPs) in FCGR2C with vaccine efficacy (VE), defined as one minus the vaccine/placebo hazard ratio of HIV-1 acquisition (HR), in the RV144 trial (8).
Considering that FcγR genetic variations have broad functional implications (4–7, 9), we hypothesized that FcγR polymorphisms also influence HIV-1 acquisition risk in vaccine recipients in other vaccine efficacy trials. The HIV Vaccine Trials Network (HVTN) 505 phase 2b trial evaluated the efficacy of a multiclade DNA prime, recombinant adenovirus serotype 5 vector boost (DNA/rAd5) vaccine regimen in circumcised, Ad5-seronegative men and transgender women who have sex with men in the United States (10). While this trial was unblinded early due to lack of overall VE, recent studies identified several correlates of HIV-1 acquisition risk in HVTN 505, including Env-specific CD8+ T-cell response magnitude and polyfunctionality score (PFS) (11), Env-specific humoral IgG responses (12) and antibody Fc effector functions (antibody-dependent cellular phagocytosis [ADCP] and FcγRIIa binding) (76). Moreover, the vaccine/placebo hazard ratio of HIV-1 acquisition significantly varied by the type of HIV-1 virus, defined by amino acid sequence distance of the HIV-1 CD4 binding site to the vaccine insert sequence, a “sieve effect” (13). Cumulatively, these findings suggest that the DNA/rAd5 vaccine regimen has had differential effects on HIV-1 acquisition depending on immunologic and virologic markers.
Together with the evidence from two previous HIV-1 vaccine efficacy trials that an rAd5 vaccine increased the risk of HIV-1 acquisition compared to placebo in a subset of individuals (14), these results raise the possibility that the DNA/rAd5 vaccine regimen has enhanced the risk of HIV-1 acquisition in some individuals while conferring a certain degree of protection in others (i.e., individuals who generated relatively strong immune responses upon vaccination and who were exposed to HIV-1 viruses sufficiently similarly to the vaccine strains), averaging out to the observed null efficacy. Our hypothesis is that genetic variations in FcγRs could explain, in part, potential variation in the vaccine’s effect on HIV-1 acquisition.
To test this hypothesis, we genotyped HVTN 505 HIV-1-infected cases and uninfected controls (including both vaccine and placebo recipients) for FcγR genes, as previously described for RV144 cases and controls (8). We assessed whether and how FcγR SNPs were modified according to (i) the vaccine/placebo HR of HIV-1 acquisition risk, (ii) the previously identified associations of immune response biomarkers or Fc effector functions with HIV-1 acquisition risk in vaccine recipients (11, 12), (iii) vaccine-induced immune responses, including Fc effector functions in vaccine recipients, and (iv) the previously identified Env-gp120 sieve effects (13). We also investigated the potential functional mechanisms of the identified FcγR SNPs by investigating their associations with FcγR expression in human B cells.
RESULTS
FCGR2C and FCGR3B genetic variants modified the effect of the DNA/rAD5 vaccine on HIV-1 acquisition risk.
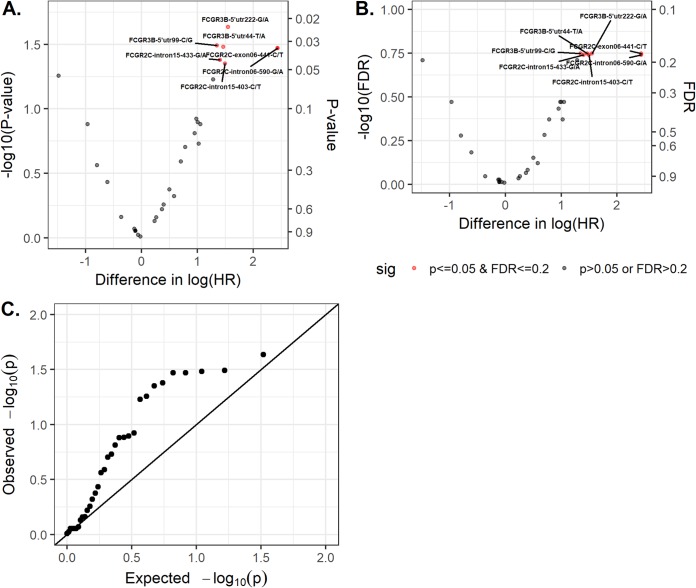
We genotyped HVTN 505 cases and controls for 162 loci over five FcγR genes (FCGR2A, FCGR2B, FCGR2C, FCGR3A, and FCGR3B). Of these loci, 33 SNPs passed selection criteria and tests (details are in Materials and Methods) and were included in further analysis. We began by assessing whether any of these 33 FcγR SNPs significantly modified the effect of the DNA/rAd5 vaccine regimen on HIV-1 acquisition risk. We found that 7 FcγR SNPs significantly modified the vaccine/placebo hazard ratio (HR) of HIV-1 acquisition after adjusting for the 33 statistical tests (P ≤ 0.05 and false discovery rate [FDR]-adjusted q value of ≤0.2) (Fig. 1; see also Table S1 in the supplemental material). These SNPs are located in two FcγR genes: four in FCGR2C (FCGR2C-exon06-441-C/T [rs138747765], FCGR2C_intron06_590-G/A, [rs78603008], FCGR2C-intron15-403-C/T [rs373013207], and FCGR2C-intron15-433-G/A [rs201984478]) and three in FCGR3B (FCGR3B-5’utr222-G/A [rs34085961], FCGR3B-5’utr44-T/A [rs34322334], and FCGR3B-5’utr99-C/G [rs61803026]). For each of these SNPs, the vaccine/placebo HR was significantly greater than one (HR = 2.6 to 9.8) in participants carrying a minor allele(s) in these FCGR2C and FCGR3B loci (Table 1), suggesting that the DNA/rAd5 vaccine have enhanced the risk of HIV-1 acquisition in these subgroups of individuals, whereas HR was less than one (HR = 0.65 to 0.88) in participants not carrying a minor allele.
FIG 1.
Assessment of whether and how each of the 33 FcγR SNPs modified the hazard ratio (vaccine/placebo) of HIV acquisition in HVTN 505. (A) Volcano plot of P value for the interaction between genotype and treatment arm (y axis, −log10 scale) versus difference in estimated log(HR) (vaccine/placebo) between genotype groups (x axis). (B) Volcano plot of false discovery rate (FDR) (y axis, −log10 scale) versus difference in estimated log(HR) between genotype groups (x axis). Red dots represent FcγR SNPs that significantly modify the HR (vaccine/placebo). (C) Quantile-quantile plot of the observed and expected P values (−log10 scale for both).
TABLE 1.
Modification of the vaccine/placebo hazard ratio of HIV-1 acquisition by FcγR SNPs and haplotypes in HVTN 505
| Gene | SNP | Genotype or haplotype | No. of cases (vaccine:placebo) | HRa | 95% CI | P valueb | Interaction P valuec | Interaction q valuec |
|---|---|---|---|---|---|---|---|---|
| FCGR3B | FCGR3B-5'utr44-T/A (rs34322334) | TT | 10:16 | 0.66 | 0.29, 1.5 | 0.317 | 0.033 | 0.178 |
| TA/AAd | 14:5 | 2.84 | 0.98, 8.18 | 0.054 | ||||
| FCGR3B-5'utr99-C/G (rs61803026) | CC | 9:14 | 0.68 | 0.29, 1.6 | 0.375 | 0.032 | 0.178 | |
| CG/GGd | 18:7 | 2.6 | 1.06, 6.37 | 0.036 | ||||
| FCGR3B-5'utr222-G/A (rs34085961) | GG | 10:16 | 0.65 | 0.29, 1.49 | 0.308 | 0.023 | 0.178 | |
| GA/AAd | 15:5 | 3.07 | 1.07, 8.75 | 0.036 | ||||
| FCGR2C | FCGR2C-exon06-441-C/T (rs138747765) | CC | 17:20 | 0.86 | 0.44, 1.7 | 0.667 | 0.034 | 0.178 |
| CT/TTd | 9:1 | 9.79 | 1.17, 81.78 | 0.035 | ||||
| FCGR2C-intron06-590-G/A (rs78603008) | GG | 17:20 | 0.86 | 0.44, 1.7 | 0.667 | 0.034 | 0.182 | |
| GA/AAd | 9:1 | 9.79 | 1.17, 81.78 | 0.035 | ||||
| FCGR2C-intron15-403-C/T (rs373013207) | CC | 15:18 | 0.88 | 0.43, 1.78 | 0.719 | 0.045 | 0.182 | |
| CT/TTd | 12:3 | 3.92 | 1.08, 14.16 | 0.037 | ||||
| FCGR2C-intron15-433-G/A (rs201984478) | GG | 13:17 | 0.82 | 0.39, 1.73 | 0.601 | 0.042 | 0.182 | |
| GA/AAd | 14:4 | 3.33 | 1.08, 10.29 | 0.036 | ||||
| CT/TTd | 11:4 | 2.14 | 0.6, 7.55 | 0.239 | ||||
| FCGR3B | FCGR3B-AGA | |||||||
| − | 11:16 | 0.73 | 0.33, 1.62 | 0.439 | 0.047 | |||
| + | 14:5 | 2.78 | 0.97, 7.94 | 0.057 | ||||
| FCGR2C | FCGR2C-TATA | |||||||
| − | 17:20 | 0.86 | 0.44, 1.7 | 0.667 | 0.034 | |||
| + | 9:1 | 9.79 | 1.17, 81.78 | 0.035 |
Vaccine/placebo hazard ratio of HIV-1 acquisition in HVTN 505 for individuals with the given genotype at the given SNP.
P value of testing for HR = 1 for individuals with the given genotype at the given SNP.
Interaction P value of testing for a difference in HR between the two indicated genotype groups. Boldface indicates P ≤ 0.05 and q ≤ 0.2.
The genotypes containing at least one minor allele.
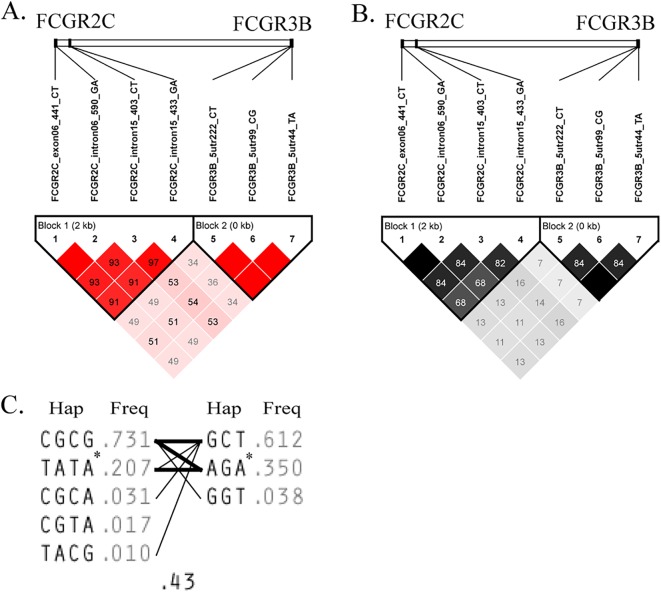
In HVTN 505 participants, the four identified FCGR2C SNPs were in high linkage disequilibrium (LD; D′ = 0.91 to 1.0, r2 = 0.68 to 1.0), likely representing one signal, and the three FCGR3B SNPs were also in high LD (D′ = 1.0, r2 = 0.84 to 1.0), likely representing a second signal. Further analysis showed that the four FCGR2C SNPs formed one haplotype block, while the three FCGR3B SNPs formed another haplotype block (Fig. 2). We found that the haplotypes FCGR2C-TATA (comprising all minor alleles in the four FCGR2C SNPs with haplotype frequency of 20.7%; Fig. 2) and FCGR3B-AGA (comprising all minor alleles of the 3 FCGR3B SNPs with haplotype frequency of 35%; Fig. 2) also significantly modified the DNA/rAd5 vaccine effect on HIV-1 acquisition (FCGR2C-TATA, HR = 9.79 and P = 0.035 for presence, HR = 0.86 and P = 0.67 for absence, with interaction P = 0.034; FCGR3B-AGA, HR = 2.78 and P = 0.057 for presence and HR = 0.73 and P = 0.44 for absence, with interaction P = 0.047) (Table 1). These results indicate that vaccine recipients carrying the FCGR2C-TATA haplotype or the FCGR3B-AGA haplotype had an increased risk of HIV-1 acquisition compared with that of placebo recipients carrying the same haplotype.
FIG 2.
SNP composition of the two haplotype blocks observed in HVTN 505 participants. One of the haplotype blocks was comprised of five FCGR2C SNPs, and the other haplotype block was comprised of three FCGR3B SNPs. (A) Linkage disequilibrium measurements (D′) between the 8 SNP genotypes. (B) Correlation (r2) between the 8 SNP genotypes. (C) Haplotypes and frequencies within FCGR2C and FCGR3B haplotype blocks. Shown in each haplotype block are the haplotypes with a frequency of ≥1%. The haplotype designated with an asterisk in each haplotype block contains all minor alleles from the composite FcγR SNPs. Lines connecting haplotypes across haplotype blocks indicate the frequency of haplotype linkage, where line width represents frequency magnitude (thin lines for a frequency of ≥1% and thick lines for a frequency of ≥10%). Plots were generated using Haploview.
The FCGR3B-AGA haplotype modified the association of Env-specific IgG and CD8+ T-cell PFS with HIV-1 acquisition risk.
To examine the potential functional impact of these FcγR SNPs, we assessed whether any of the 33 FcγR SNPs modified the immune correlates of the Env-specific CD8+ T-cell PFS and Env-specific IgG with HIV-1 acquisition risk identified previously (11, 12). We found that none of the 33 SNPs significantly modified the correlate of Env-specific CD8+ T-cell PFS with HIV-1 acquisition risk (Table S2) or the correlate of Env-specific IgG with risk (Table S3) after adjusting for the 33 statistical tests for each immune response variable. Fong et al. also found that vaccine recipients with a high CD8+ T-cell PFS generally had low risk of HIV acquisition, whereas vaccine recipients with a low CD8+ T-cell PFS and a low Env-specific IgG response had the highest risk (12). Therefore, we assessed whether any of the 33 FcγR SNPs modified the correlate with HIV-1 risk of a combination Env-specific IgG and CD8+ T-cell PFS (low in both, denoted as 0, versus medium/high in at least one variable, denoted as 1). We found that after adjusting for the 33 statistical tests, five FCGR3B SNPs (FCGR3B-5’utr425-T/G [rs76732376], FCGR3B-5’utr473-G/A [rs74127076], and the three FCGR3B SNPs reported above) passed the significance threshold (P ≤ 0.05 and q ≤ 0.2) (Table S4).
The minor alleles at these two newly identified FCGR3B SNPs were in linkage with the FCGR3B-AGA haplotype. As shown in Table 2, the FCGR3B-AGA haplotype also significantly modified the association of the combined Env-specific IgG and CD8+ T-cell PFS variable with HIV-1 risk (interaction P value of 0.044). Medium/high responders to Env-specific IgG and/or CD8+ T cells had a larger reduction in HIV-1 risk than nonresponders or low-level responders to both: 98% (odds ratio [OR] of 0.02) in recipients without the FCGR3B-AGA haplotype and 76% (OR of 0.24) in recipients with the FCGR3B-AGA haplotype (Table 2). We observed similar trends for the FCGR2C-TTATA haplotype, but the result for the test for effect modification was not statistically significant (data not shown).
TABLE 2.
Modification of identified immune correlates of risk in HVTN 505 by the FCGR3B-AGA haplotype
| Immune variable | FCGR3B-AGA haplotype | Unit | ORa | 95% CI | P value | Interaction P valuee |
|---|---|---|---|---|---|---|
| Env-specific CD8+ T-cell PFSb | − | Per 1-SD | 0.19 | 0.06, 0.6 | 0.005 | 0.377 |
| + | Per 1-SD | 0.36 | 0.15, 0.84 | 0.018 | ||
| Env-specific IgG responsec | − | Per 1-SD | 0.38 | 0.16, 0.93 | 0.034 | 0.035 |
| + | Per 1-SD | 1.41 | 0.62, 3.17 | 0.412 | ||
| Env-specific IgG and/or CD8+ T-cell PFSc,d | − | 1 vs 0b | 0.02 | 0, 0.15 | 0.0002 | 0.044 |
| + | 1 vs 0b | 0.24 | 0.06, 0.99 | 0.049 |
Odds ratio of HIV-1 infection for the given immune response and genotype group in the vaccine recipients.
From Janes et al. (11).
From Fong et al. (12).
PFS is a binary variable: 0, low on both Env-specific IgG (in 1st tertile) and Env-specific CD8 PFS (in 1st tertile); 1, all others.
Boldface indicates a P value of ≤0.05.
To better understand how the FCGR3B-AGA haplotype modified the association of the combined binary variable with HIV-1 acquisition risk, we examined the Env-specific IgG and CD8+ T-cell PFS responses separately. Interestingly, the inverse correlation of Env-specific IgG response with HIV-1 risk previously observed (12) was only observed in vaccine recipients without the FCGR3B-AGA haplotype (OR of 0.38 and P value of 0.034 for recipients without and OR of 1.41 and P value of 0.50 for vaccine recipients with the FCGR3B-AGA haplotype; interaction P value of 0.035) (Table 2). For vaccine recipients without the FCGR3B-AGA haplotype, one standard deviation (SD) increase in Env-specific IgG score was associated with an estimated 62% (OR of 0.38) decrease in the risk of HIV-1 acquisition, which was larger than the estimated 40% (OR of 0.60) decrease in the risk of HIV-1 acquisition when all vaccine recipients were considered together (12). However, for vaccine recipients with the FCGR3B-AGA haplotype, there was an estimated 1.41 times increase (albeit nonsignificant) in the risk of HIV-1 acquisition (Table 2). The inverse association of Env-specific CD8+ T-cell PFS with HIV-1 acquisition risk shown in reference 11 was observed in both haplotype groups but with a stronger correlate in the group without the FCGR3B-AGA haplotype (HR = 0.19, P = 0.005) than in the group with the FCGR3B-AGA haplotype (HR = 0.36, P = 0.018), although the difference was not significant.
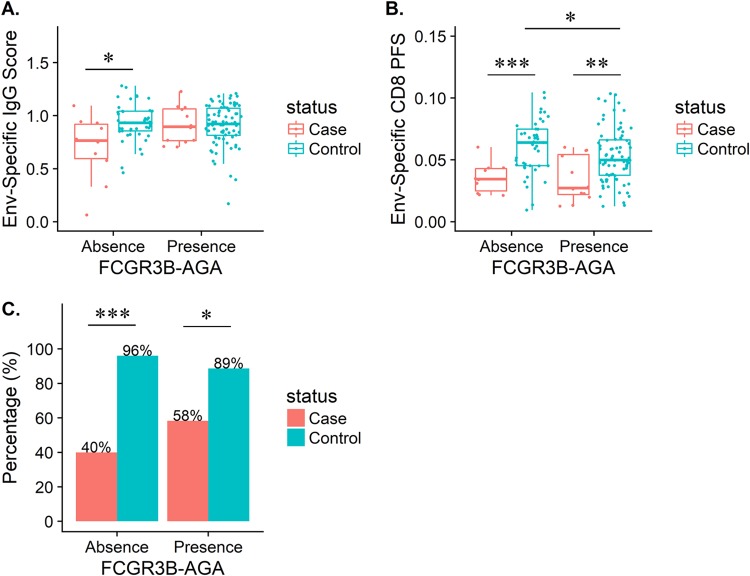
To better understand these modification effects, we plotted the distributions of these immune response biomarkers according to case/control status and FCGR3B-AGA haplotype status (present or absent) (Fig. 3). In vaccine recipients without the FCGR3B-AGA haplotype, the magnitude of the Env IgG response (Fig. 3A), the magnitude of the CD8+ T-cell PFS (Fig. 3B), and the percentage of Env IgG and/or CD8+ T-cell PFS medium/high-level responders (Fig. 3C) were all significantly lower in cases than controls. Similarly, we observed lower responses in cases than in controls for CD8+ T-cell PFS magnitude (Fig. 3B) and the percentage of Env IgG and/or CD8+ T-cell PFS responders (Fig. 3C) for vaccine recipients with the FCGR3B-AGA haplotype but not in the magnitude of the Env IgG response (Fig. 3A). Further, among controls, CD8+ T-cell PFS magnitude was lower in vaccine recipients with the FCGR3B-AGA haplotype than in those without the FCGR3B-AGA haplotype (P = 0.04) (Fig. 3B). These results suggest that DNA/rAd5 vaccination induced differential Env-specific CD8+ T-cell responses but not IgG responses between the two FCGR3B-AGA haplotype groups. Thus, for individuals with the FCGR3B-AGA haplotype (and, to a lesser extent, the FCGR2C-TTATA haplotype), vaccination was less likely to induce the potentially protective Env-specific IgG and/or CD8+ T-cell responses than for individuals without the FCGR3B-AGA haplotype.
FIG 3.
FCGR3B-AGA haplotype modified immune correlates of risk in HVTN 505. (A) Distributions of Env-specific IgG responses, as assessed by binding antibody multiplex assay, plotted according to case/control HIV infection outcome status and FCGR3B-AGA haplotype status. (B) Distributions of Env-specific CD8 polyfunctionality scores (PFS), plotted according to case/control status and FCGR3B-AGA haplotype status. (C) Percentages of HVTN 505 vaccine recipients having medium or high responses for either Env IgG or CD8 PFS in HVTN 505 cases and controls, plotted according to case/control status and FCGR3B-AGA haplotype status.
FCGR2A and FCGR2B SNPs modified the association of gp140-specific antibody-dependent cellular phagocytosis (ADCP) activity with HIV-1 acquisition risk.
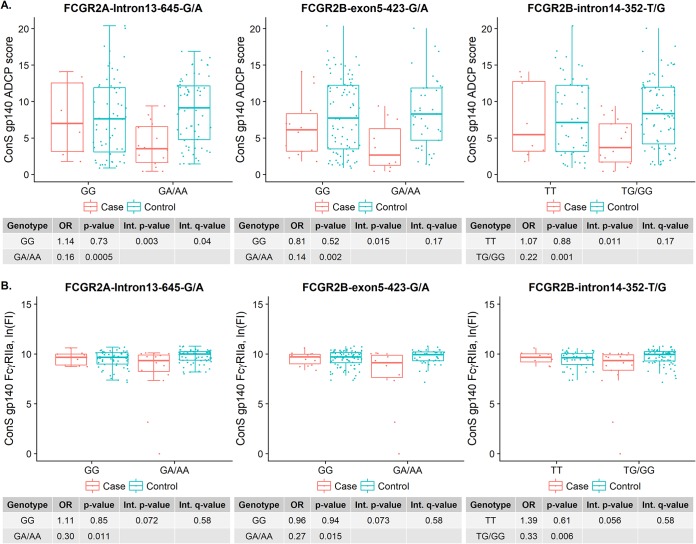
We recently found that gp140-specific antibody-dependent cellular phagocytosis (ADCP) activity and FcγRIIa binding were each inversely correlated with HIV-1 acquisition risk in HVTN 505, and that an FCGR2A SNP (FCGR2A-intron13-645-G/A [rs2165088]) significantly modified the association of ADCP with HIV-1 acquisition risk (Neidich et al., submitted). Here, we broadened the analysis of the seven FCGR2A SNPs examined in Neidich et al. (submitted) to evaluate whether any of the 33 FcγR SNPs significantly modified the associations of these two antibody Fc effector functions with HIV-1 acquisition risk. The modification of FCGR2A SNP (FCGR2A-intron13-645-G/A [rs2165088]) on the association of ADCP with HIV-1 acquisition risk remained significant after adjusting for 33*2 (33 SNPs versus 2 Fc effector functions) statistical tests (interaction P value of 0.003, interaction q value of 0.04) (Fig. 4A). In addition, two FCGR2B SNPs (FCGR2B-exon5-523-G/A [rs6665610] and FCGR2B-intron14-352-T/G [rs6666965]) significantly modified the correlation of ADCP activity with HIV-1 acquisition risk (interaction P values of 0.015 and 0.011 and interaction q values of 0.017 and 0.017) (Fig. 4A). The inverse correlation of ADCP with HIV-1 acquisition risk reported by Neidich et al. (submitted) was observed only in vaccine recipients with minor alleles at these SNP loci (OR of 0.16, 0.14, and 0.22 per one standard deviation [per 1-SD] increase in ADCP score in GA/AA of FCGR2A-intron13-645-G/A, GA/AA of FCGR2B-exon5-523-G/A, and TG/GG of FCGR2B-intron14-352-T/G, respectively) (Fig. 4A). Similarly, the inverse correlation of FcγRIIa binding with HIV-1 risk identified by Neidich et al. (submitted) was also observed only in vaccine recipients with minor alleles at the same SNP loci (OR of 0.30, 0.27, and 0.33 per 1-SD increase in FcγRIIa binding, respectively), but the interaction testing for the lack of SNP effect modification of the correlation was not significant (all P values were slightly greater than 0.05) (Fig. 4B). These results suggest that for individuals carrying the minor alleles at these identified FCGR2A and FCGR2B SNP loci, the vaccine-induced antibodies in individuals who later became HIV-1 infected were less capable of engaging effector immune cells, potentially involving less efficient antibody Fc binding for FcγRs like FcγRIIa.
FIG 4.
FcγR SNPs (FCGR2A-intron13-645-G/A [rs2165088], FCGR2B-exon5-523-G/A [rs6665610], and FCGR2B-intron14-352-T/G [rs6666965]) modified the association of Fc effector functions (ConS gp140 ADCP score and FcγRIIa binding) with HIV-1 acquisition risk. (A and B) ConS gp140 ADCP score (A) and ConS gp140 FcγRIIa binding (B). On each panel, distributions of Fc effector functions were plotted according to case/control HIV infection outcome status and genotype groups.
Similar analysis for the additional immune response variables studied in reference 12 showed that none of the 33 FcγR SNPs passed the significance threshold after multiplicity corrections (interaction q values of >0.2). Also, these 33 FcγR SNPs did not significantly modify the reported Env-gp120 sieve effects in HVTN 505 (13) after multiplicity correction (interaction q values of >0.2) or vaccine-induced immune responses or antibody Fc effector functions (q values of >0.2).
The identified FcγR SNPs could regulate FcγR gene expression.
Similar to what we found in reference 15, the identified FCGR3B variants were positively correlated with FCGR2A/C expression but negatively correlated with FCRLA expression (Fig. S1 and Table S5). However, for the three SNPs that modified the correlation of ADCP activity with the HR of HIV-1 acquisition, only one in FCGR2B (FCGR2B-exon5-523-G/A [rs6665610]) had a significant expression quantitative trait locus (eQTL), for which the minor alleles were associated with decreased expression of FCGR2A as measured by transcriptome deep sequencing (RNA-seq) analysis (Table S5). These results indicate that both sets of identified FcγR SNPs could regulate FcγR gene expression, but their collective effect is unclear.
Since we did not genotype all genetic variants in the FcγR region, we searched in the FcγR region for other SNPs that were not genotyped in this study but were in high LD (r2 > 0.8) with each of the identified FcγR SNPs using genotyping data publicly available from the 1000 Genomes Project (16). Interestingly, for all SNPs identified in this study that modify the HR of HIV-1 acquisition and/or the association of vaccine-induced immune responses or antibody Fc effector functions with HIV-1 acquisition risk, their linked SNPs were predicted to have FcγR gene regulatory potential (e.g., 5_prime_UTR_variant, upstream_gene_variant, and downstream_gene_variant) but were not predicted to alter FcγR protein sequences (Tables S6 and S7). Again, together these results imply that the identified FcγR SNPs and haplotypes have modulated the selective expression of FcγRs on immune cells.
DISCUSSION
Our previous finding that FCGR2C polymorphisms were associated with VE in RV144 raised the question of whether FcγR genetic variations are functionally relevant only for the RV144 vaccine regimen or more broadly in HIV-1 vaccine development. As reported in this study, several FcγR SNPs significantly modified the HR of HIV-1 acquisition in HVTN 505, an efficacy trial that differed from RV144 in a number of respects (canarypox prime/protein boost and general low-risk Thai population in RV144 versus DNA prime/rAd5 boost and high-risk U.S. population of men who have sex with men [MSM] in HVTN 505). Moreover, three of the FCGR2C SNPs (FCGR2C-exon06-441-C/T [rs138747765], FCGR2C-intron06-590-G/A [rs78603008], and FCGR2C-intron15-403-C/T [rs373013207]) significantly modified the vaccine’s effect on HIV-1 acquisition in both RV144 and HVTN 505. This indicates that FcγR genetic variations have broad impact, given the major differences in the vaccine regimens and populations.
This study also suggests that the functional impact of a given FcγR polymorphism on the risk of HIV-1 acquisition is context specific, dependent on the specific vaccine regimen and possibly other factors, such as demographics, virus quasispecies, and genetic background. Compared to the previous RV144 study, the effect modification of the tag FCGR2C SNP (FCGR2C-intron06-126-C/T [rs114945036]) identified in RV144 on the HR in HVTN 505 did not pass the significance threshold, even though it had a trend similar to that of the other FCGR2C SNPs (see Table S1 in the supplemental material). This result was expected, since this tag SNP was on intron 6 and in high LD with the other two FCGR2C SNPs on intron 6 described above but with reduced correlation (D′ = 1 and r2 = 0.6) in HVTN 505 compared to the correlation in RV144. Furthermore, we identified additional FcγR SNPs in HVTN 505. FCGR3B SNPs significantly modified the vaccine effect on HIV-1 acquisition risk in HVTN 505 but not in RV144. These FCGR3B SNPs also modified the association of Env-specific IgG and CD8+ T-cell PFS with HIV-1 acquisition risk in HVTN 505. In addition, FCGR2A/2B SNPs significantly modified the immune correlate of ADCP with HIV-1 acquisition risk in HVTN 505. These findings indicate that multiple FcγRs influence the vaccine’s effect on HIV-1 acquisition in HVTN 505.
It is intriguing that in HVTN 505 HIV-1 acquisition, risk was increased in vaccine recipients who carried certain FCGR2C minor alleles compared with their placebo counterparts. Similarly, in the earlier Vax004 trial, FcγR genetic polymorphisms were associated with HIV risk (17). In that study, conducted in North America among MSM, vaccination with a bivalent recombinant gp120 was associated with a 3.5-fold increased risk in HIV acquisition among low-risk participants homologous for valine (V) at amino acid position 158 of FcγRIIIa, an isoform with greater affinity for monomeric IgG1 and IgG3 and certain IgG isotype immune complexes (4), compared to that of individuals homozygous for phenylalanine (F) or the VF isoform (17). In that report, FcγRIIa genotypes did not influence HIV risk among vaccine recipients, and FcγRIIa or FcγRIIIa genotypes did not influence HIV risk among placebo recipients.
One mechanism that could explain the increased risk for infection in these two vaccine studies is that HIV vaccination potentially induces nonneutralizing or poorly neutralizing antibodies. Such antibodies could theoretically mediate antibody-dependent enhancement (ADE), a phenomenon where antibodies bind a virion but fail to neutralize it and then the resultant antibody-virus complexes attach to Fc receptor-bearing target cells (e.g., monocytes and macrophages), thereby increasing infection of such cells. Such a phenomenon has been observed in vitro for many viruses, perhaps most notably dengue virus (18, 19) and also Zika virus (20, 21), coronavirus (22), Ebola virus (23), and coxsackievirus B (24). In the case of dengue virus, an FcgRIIa polymorphism was shown to be significantly associated with dengue disease (versus subclinical infection); moreover, compelling evidence was recently published to support that ADE enhances disease severity in humans (25). Importantly, ADE has also been described for HIV in vitro (26, 27). Although it remains unknown whether ADE could increase HIV infection risk in humans (28), it has been found that patients with HIV who have antibodies capable of ADE have more rapid disease progression (29). For ADE to mediate enhanced infection risk after HIV vaccination, the vaccine regimen would need to induce nonneutralizing or poorly neutralizing antibodies; it has been shown that the HVTN 505 regimen did induce such antibodies (namely, gp41 reactive and nonneutralizing) (30). Further work would need to be done to test the hypothesis that an effect of FcγR polymorphisms of ADE of HIV infection could explain the results presented here.
Another potential mechanism is that FcγR polymorphisms may increase risk of HIV infection through modulation of innate immunity. HIV founder viruses are intrinsically resistant to type I interferons (31, 32). Plasmacytoid dendritic cells (pDC) produce high levels of interferon following HIV infection, which can restrict virus replication (33, 34). Although expression of FcγRs on pDC is low (35), opsonized viral particles can suppress type I and III interferon production by pDC, as well as other myeloid cells, through FcγR-mediated signaling (36). A decrease in the level of interferon production in pDC or other myeloid cells following signaling through FcγR engagement could lower the threshold of interferon resistance required of founder viruses to establish infection.
These hypothesized mechanisms for the increased risk of HIV infection in HVTN 505 among participants with selected FcγRIIc alleles fail to explain the protective effect observed in RV144 vaccine recipients carrying the same minor alleles. It is unclear if these same variants functioned differently in each trial or were linked to other factors that influenced risk. Various factors, such as the diversity and complexity of expression of FcγRs on immune effector cells, the consequences of their binding influenced by IgG isotypes in vaccine recipients, and antibody levels and their binding characteristics, will change during the course of vaccination. Therefore, the balance between risk and protection is not likely to be static over time. The role of FcγRs in modulating natural or vaccine-induced immunity has been evaluated in very few models of viral infections and for even fewer infections in humans. These findings, together with other published studies (17, 37, 38), strongly support the idea that host genetics should be considered in the analysis of future HIV vaccine trials to address these questions.
Another potential contributor to host genetics in this regard is the variability of the immunoglobulin constant heavy G chain (IGHG) sequences (39). While it is recognized that FcγR variation can affect binding affinity to the Fc region of IgG with functional consequence (4, 6), the level of variation in the constant regions of the individual IgG genes (IGHG3, IGHG1, IGHG2, and IGHA2, comprising the IGH locus on chromosome 14) suggests IGHG variability also affects FcγR binding (4, 40). The population-specific IGHG variation that has been observed (39) in turn is suggestive that IGHG variation in conjunction with FcγR variation plays a role in vaccine efficacy or disease susceptibility that itself is population specific. Thus, while FcγR variation may be common between populations, IGHG variation may differ and, consequently, yield distinct functional outcomes.
Because none of the FcγR SNPs that we found to modify the HR of HIV-1 acquisition or correlates of HIV-1 acquisition in HVTN 505 introduced any changes in the corresponding FcγR protein sequence, the observed effects of the FcγR polymorphisms are likely related to modulation of FcγR expression levels, perhaps through transcriptional regulation, as suggested by the associations of the FCGR3B SNPs and increased FCGR2A/C expression. However, since we did not identify any SNP associated with differential expression of its corresponding FcγR gene, it is also plausible that these SNPs are linked to some unknown functional polymorphisms in the FcγR region. Interestingly, a nonexpressed allelic form of FCGR2C (FCGR2C.nc-ORF) was previously shown to be associated with a decreased risk of alloimmunization in patients with sickle cell disease, perhaps related to lower expression of FcγRIIc on B cells in individuals with FCGR2C.nc-ORF (41). Analyses such as cell type-specific FcγR expression on autologous immune cells will be needed to facilitate the identification of causal FcγR variants (i.e., variants that impact HIV-1 acquisition risk) and their functional mechanisms after HIV-1 vaccination.
The genomic and functional complexity of the FcyRs present a major challenge for uncovering the underlying mechanisms for the effects of the FcγR variants described. While different FcγRs have distinct functions and mechanisms of regulation, they share highly similar sequences. Variations are present in both FcγR sequences and copy numbers (42, 43). While FcγR genetic variations are clearly linked to host defense against infectious diseases and other important immune functions (7, 44, 45), current approaches measure only a small portion of the existing FcγR variations. This study and our previous RV144 study (8) were by far the most comprehensive in this regard, measuring ∼10 kb of the region, including functional exons and flanking sequences from the five FcγR genes. However, the complete FcγR region extends over 200 kb, leaving considerable room for analysis of additional variations, including those that are bona fide causal variations. While there are currently over 20,000 SNPs documented in the FcγR region (Ensembl Variation database, https://www.ensembl.org/info/genome/variation/index.html; accessed 20 September 2017), the lack of phasing of these data subverts their direct utility for causal variant identification. To fully define the extent of human FcγR genetic variation, it is necessary to obtain complete haplotype-resolved FcγR genomic sequences across vaccine trials using approaches such as those outlined in references 46 and 47. Even with the complete FcγR genomic sequences, significant effort is still needed to locate causal variants of a particular phenotype, such as control of FcγR expression levels. A potential solution is to use parallel transcriptome analysis to systematically identify variants affecting FcγR gene expression, as illustrated in references 15 and 48, and to assess the collective effects of multiple FcγR variants across individual immune cell types.
Also, the identified FcγR polymorphisms might have influenced the development of HIV-1-specific IgG antibodies after vaccination. For example, the difference in Env-specific IgG responses between cases and controls in vaccine recipients without the FCGR3B-AGA haplotype did not exist in vaccine recipients with the FCGR3B-AGA haplotype. This finding suggests that FcγR polymorphisms influence the development of the binding antibody response that was associated with decreased risk of infection. Also, the differences in gp140-specific ADCP activity and FcγRIIa binding between cases and controls were only present in one genotype group of each of the identified FCGR2A and FCGR2B SNPs. This indicates that FcγR polymorphisms also contribute to the variability of the Fc domain in vaccine-induced IgG antibodies. For example, Fc glycosylation modulates the interaction between antibody and FcγR. Fc glycosylation of HIV-specific antibodies has been shown to vary naturally in HIV-1-infected individuals (49, 50) and can be regulated by HIV-1 vaccination (51). Further, the FcyR SNPs identified here were associated with changes in gene expression levels of FCGR2A/C and FCRLA in B cells. While the function of FCGR2A/C is relatively well studied, very little is known about FCRLA (52). FCRLA is located in the same region of chromosome 1 as other FcγRs but does not have a transmembrane region. Instead, FCRLA resides in the endoplasmic reticulum and can associate with multiple Ig isotypes, including IgM, IgG, and IgA (53). Considering the abundant expression of FCRLA in human germinal center B cells, FCRLA is likely involved in B cell and antibody development (52). Therefore, modulation of FCRLA expression could also be a mechanism by which FcγR genetic variation influences the development of HIV-1-specific antibodies during vaccination.
The activities of FcγRs can regulate B cell selection and IgG affinity maturation, such as the demonstrated effects of FcγRIIb expression on B cell signaling (1). Moreover, susceptibility to autoimmune diseases, such as systemic lupus erythematosus, has been linked to differential expression of functional FcγRIIb, driven by genetic variations in the FCGR2B promoters (54, 55), FcγR copy number variation (56), or amino acid changes in FcγRIIb (57). A recent study of IgG antibodies elicited by administration of the trivalent influenza virus vaccine in healthy subjects showed that the abundance of sialylated Fc glycans (sFc) predicted the quality of vaccine response (58). Further, sFc within immune complexes has been shown to trigger the upregulation of FcγRIIb on B cells (58). Increased levels of FcγRIIb on B cells can elevate the threshold for B-cell antigen receptor affinity, which is required for B cell survival and production of higher-affinity protective IgG antibodies (58). In addition, one recent study analyzed the temporal changes in Fc effector functionality of HIV-specific IgG antibodies in HIV-1-infected individuals (59). As early as 6 months postinfection, individuals who later developed broadly neutralizing antibodies (bnAbs) already had significantly higher levels of antibody-dependent complement deposition (ADCD) and cellular trogocytosis (ADCT), which correlated with antibody binding to C1q and FcγRIIa, respectively (59). Antibodies from these bnAb-developing individuals also showed more IgG subclass diversity, which was correlated with Fc polyfunctionality (59). Interestingly, germinal center activity as represented by CXCL13 levels and expression of activation-induced cytidine deaminase has been found to be associated with neutralization breadth, Fc polyfunctionality, and IgG subclass diversity (59). Together, these findings suggest that it would be informative to investigate how FcγRs are involved in regulating germinal center activities that link IgG Fab and Fc domains and to evaluate if this regulation could be exploited to aid HIV-1 vaccine development.
Our statistical analysis included a large number of hypothesis tests and was not prespecified in the HVTN 505 protocol or statistical analysis plan (SAP). Although a sequel analysis plan was specified prior to data analysis and methods of multiple testing adjustment were employed, it cannot be ruled out that some significant results are false positives. Therefore, this study should be viewed as hypothesis-generating and exploratory, providing guidance for future studies in which these hypotheses are tested and can advance knowledge of the influence of FcγR genetics on vaccine effects. Another utility of this work is the preparation of laboratory and statistical methodology for application to the ongoing HIV-1 vaccine efficacy trials. For instance, it will be particularly relevant to consider FcγR genetics when assessing correlates of vaccine efficacy in the HVTN 702 trial, which is evaluating a pox-protein vaccine regimen similar to that tested in RV144, and in the HVTN 705/VAC89220HPX2008 trial of an Ad26/gp140 mosaic vaccine regimen. Each of these regimens has been shown to induce T-cell and nonneutralizing antibody responses.
As discussed in references 9, 60, and 61 and elsewhere, the role of antibody and Fc receptor interactions in HIV prevention and therapy is becoming better appreciated. Our results further demonstrate that detailed analyses of FcγR genetics and the impact of FcγR genetic variation on HIV-1 acquisition risk and/or vaccine efficacy against HIV-1 acquisition will be important for understanding correlates of protection in ongoing and future phase 2b/3 trials of preventative HIV-1 vaccines.
MATERIALS AND METHODS
FcγR SNP genotyping.
A total of 193 peripheral blood mononuclear cell (PBMC) samples (from 145 controls [defined as HIV negative at month 24] and 48 cases (defined as diagnosis of HIV-1 infection sometime between week 28 and month 24) in HVTN 505 were genotyped for five FcγR genes (FCGR2A, FCGR2B, FCGR2C, FCGR3A, and FCGR3B) using the same platform as that used in reference 8. Of the 145 control samples, 20 were from placebo recipients and 125 were from vaccine recipients. Among the 48 case samples, 21 were from placebo recipients and 27 were from vaccine recipients. A total of 162 loci across the 5 FcγRs were sequenced. After excluding indels, double mutations, and SNPs that failed to pass the minor allele frequency (MAF) threshold (≥5%) and the Hardy-Weinberg equilibrium (HWE) test (P ≥ 0.00001) based on the control samples, 33 SNPs remained in the analyses. Haploview (62) was used to generate FcγR haplotypes and linkage disequilibrium (LD) plots.
Immune response correlates of risk in HVTN 505.
In the primary T-cell correlates analysis, Janes et al. measured HIV-specific CD4+ and CD8+ T-cell responses by intracellular cytokine staining of PBMCs isolated from vaccine recipients at 2 weeks after the last vaccination (month 6.5) from the case-control cohort, comprised of 25 primary endpoint vaccine cases and 125 randomly sampled frequency-matched vaccine controls (HIV-negative at month 24), where controls were frequency matched to cases with respect to treatment group, body mass index, and race/ethnicity (11). Janes et al. also determined the COMPASS Env-specific CD4+ and CD8+ T-cell PFS using the method described in reference 63.
In the primary humoral correlates analysis, Fong et al. measured IgG and IgA binding antibody multiplex assay (BAMA) responses (64) to HIV-1 envelope antigens using serum samples collected 1 month after the last vaccination (month 7) from the same case-control cohort (12). Low-, medium-, and high-immune-response tertiles were defined in reference 12. Fong et al. also derived and analyzed the primary tier variables (12).
In the primary Fc effector function analysis, Neidich and colleagues (submitted) measured antibody-mediated FcγRIIa tetramer binding and gp140-specific ADCP activity and found that ADCP by monocytes and Env IgG binding to FcγRIIa significantly correlated with decreased HIV-1 risk (OR of 0.47 and P = 0.001 as well as OR of 0.48 and P < 0.001, respectively).
Statistical association analysis.
The case-only method (65) was employed to assess whether and how each FcγR SNP modified the vaccine/placebo hazard ratio of HIV-1 acquisition risk (HR) between week 28 and month 24. The case-only method was also used to assess whether and how each FcγR SNP modified the hazard ratio of Env sequence-specific HIV-1 acquisition risk studied in the sieve analysis (13).
To evaluate whether and how each FcγR SNP modified the previously identified associations of CD8+ T-cell PFS, IgG, and two Fc effector functions (ConS gp140 ADCP and FcγR2a binding) with HIV-1 acquisition risk in vaccine recipients (11, 12), we applied the same model and covariate adjustment as that used in the primary humoral immune correlates of risk analysis (12). As described in reference 12, this model used logistic regression methods (66) that accounted for the case-control biomarker sampling design (implemented in the R package osDesign, available at the Comprehensive Archive R Network). Pseudo-likelihood-based inference methods were chosen and sandwich variance estimates were used to estimate confidence intervals (CI) and evaluate statistical significance. Prior to regression analysis, all immune response variables were means centered and standard deviations scaled (based on distributions among vaccine recipients), such that a unit change in the variable represents a change of one standard deviation. All regression models included the following baseline covariates to adjust for potential confounding: participant age, race (white versus black versus Hispanic/other), body mass index, and the behavioral risk score defined and applied in the primary publication of HVTN 505 (10). For the primary tier humoral correlate analysis, the CD4+ and CD8+ T-cell PFS were adjusted in the models in addition to the baseline covariates.
Given the small sample size of the study, for each SNP, participants were divided into two genotype groups: homozygous genotype of the major allele and the two genotypes containing at least one minor allele (e.g., for FCGR2C-intron6-126-C/T, the two genotype groups were CC and CT/TT).
Bar charts and boxplots were generated to display the distributions of the immune response rates and magnitudes by case/control status and by genotype group. Response rates for controls were estimated with inverse probability weighting to account for the case-control cohort sampling. Logistic regression and the Wilcoxon rank-sum test with inverse probability weighting (67) were used to compare the immune response rates and magnitudes between genotype groups among control vaccine recipients. For immune response variables (e.g., IgA) with some positive responses but many negative responses (response rate of ≤20%), the choplump test (68) was used instead of the Wilcoxon rank-sum test.
For each of the four types of null hypotheses, false discovery rates (q values) were calculated to adjust for the number of statistical tests performed (69), which are detailed in Results. False discovery rates (q values) were calculated using a resampling method that retains the correlations between the SNPs and immune response variables (70, 71). Any P value less than 0.05 with a q value less than 0.2 was considered to be significant and hypothesis generating.
Association of FcγR polymorphisms with FcγR gene expression in human B cells.
To examine the associations between FcγR SNPs and FcγR gene expression in human B cells, we queried a large-scale B-cell RNA sequencing database of 462 samples from individuals curated by the 1000 Genomes Project (48), as done in reference 15. RNA-seq read mapping, genotypes, expression quantification, and expression quantitative trait locus (eQTL) mapping results reported in reference 48 were downloaded from EBI ArrayExpress (accession number E-GEUV-1). As detailed in reference 48, mRNA expression was quantified at different levels. For exon quantification, overlapping exons of a gene were first merged into meta-exons. Transcripts and splice junctions were quantified by the Flux Capacitor approach (72). Gene expression was quantified as the sum of all transcript reads per kilobase per million (RPKMs) for each gene. Before eQTL analysis, expression quantifications were normalized by PEER correction (73) and transformed into standard normal distributions. eQTLs were mapped using a linear model in Matrix eQTL (74), and permutations were used for FDR estimation.
Other SNPs in LD with the identified FcγR SNPs.
To investigate the potential functions of identified FcγR SNPs, we also searched for other SNPs in the FcγR region that were not genotyped in this study but were in LD with the FcγR SNPs found to modify the HR of HIV-1 acquisition and/or the association of vaccine-induced immune responses or antibody Fc effector functions with HIV-1 acquisition risk. To match the B-cell RNA-seq data used in the eQTL analysis (48), we used the genotyping data for the same 373 individuals of the European population from the 1000 Genomes project (16). We calculated the pairwise LD between SNPs in the FcγR region using PLINK 1.9 (75). For each of the FcγR SNPs identified above, we defined their linked SNPs as the SNPs that were in high LD (r2 > 0.8) with them. The predicted consequences of all linked SNPs were obtained from the Ensembl Variation database (https://www.ensembl.org/info/genome/variation/index.html; accessed 21 June 2018).
Supplementary Material
ACKNOWLEDGMENTS
We are indebted to the HVTN 505 volunteers and staff for their participation in and successful completion of the HIV-1 efficacy trial.
This work was supported by National Institute of Allergy and Infectious Diseases (NIAID) U.S. Public Health Service grants UM1 AI068614 (LOC: HIV Vaccine Trials Network), UM1 AI068618 (LC: HIV Vaccine Trials Network), and UM1 AI068635 (SDMC: HIV Vaccine Trials Network); NIH/NIAID grants PO1 AI120756 (G.D.T.), R21 AI120713 (X.P.), and R21 AI125040 (X.P.); NIH/NIAID Duke Center for AIDS Research grant P30 AI064518; Penn CTU grant UM1 AI069534; and Penn CFAR grant P30 AI45008. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/JVI.02041-18.
REFERENCES
- 1.Bournazos S, Ravetch JV. 2017. Fcgamma receptor function and the design of vaccination strategies. Immunity 47:224–233. doi: 10.1016/j.immuni.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu LL, Suscovich TJ, Fortune SM, Alter G. 2018. Beyond binding: antibody effector functions in infectious diseases. Nat Rev Immunol 18:46–61. doi: 10.1038/nri.2017.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nimmerjahn F, Ravetch JV. 2008. Fcgamma receptors as regulators of immune responses. Nat Rev Immunol 8:34–47. doi: 10.1038/nri2206. [DOI] [PubMed] [Google Scholar]
- 4.Bruhns P, Iannascoli B, England P, Mancardi DA, Fernandez N, Jorieux S, Daeron M. 2009. Specificity and affinity of human Fcgamma receptors and their polymorphic variants for human IgG subclasses. Blood 113:3716–3725. doi: 10.1182/blood-2008-09-179754. [DOI] [PubMed] [Google Scholar]
- 5.Li X, Wu J, Ptacek T, Redden DT, Brown EE, Alarcon GS, Ramsey-Goldman R, Petri MA, Reveille JD, Kaslow RA, Kimberly RP, Edberg JC. 2013. Allelic-dependent expression of an activating Fc receptor on B cells enhances humoral immune responses. Sci Transl Med 5:216ra175. doi: 10.1126/scitranslmed.3007097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bournazos S, Woof JM, Hart SP, Dransfield I. 2009. Functional and clinical consequences of Fc receptor polymorphic and copy number variants. Clin Exp Immunol 157:244–254. doi: 10.1111/j.1365-2249.2009.03980.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roederer M, Quaye L, Mangino M, Beddall MH, Mahnke Y, Chattopadhyay P, Tosi I, Napolitano L, Terranova Barberio M, Menni C, Villanova F, Di Meglio P, Spector TD, Nestle FO. 2015. The genetic architecture of the human immune system: a bioresource for autoimmunity and disease pathogenesis. Cell 161:387–403. doi: 10.1016/j.cell.2015.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li SS, Gilbert PB, Tomaras GD, Kijak G, Ferrari G, Thomas R, Pyo CW, Zolla-Pazner S, Montefiori D, Liao HX, Nabel G, Pinter A, Evans DT, Gottardo R, Dai JY, Janes H, Morris D, Fong Y, Edlefsen PT, Li F, Frahm N, Alpert MD, Prentice H, Rerks-Ngarm S, Pitisuttithum P, Kaewkungwal J, Nitayaphan S, Robb ML, O’Connell RJ, Haynes BF, Michael NL, Kim JH, McElrath MJ, Geraghty DE. 2014. FCGR2C polymorphisms associate with HIV-1 vaccine protection in RV144 trial. J Clin Investig 124:3879–3890. doi: 10.1172/JCI75539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boesch AW, Brown EP, Ackerman ME. 2015. The role of Fc receptors in HIV prevention and therapy. Immunol Rev 268:296–310. doi: 10.1111/imr.12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammer SM, Sobieszczyk ME, Janes H, Karuna ST, Mulligan MJ, Grove D, Koblin BA, Buchbinder SP, Keefer MC, Tomaras GD, Frahm N, Hural J, Anude C, Graham BS, Enama ME, Adams E, DeJesus E, Novak RM, Frank I, Bentley C, Ramirez S, Fu R, Koup RA, Mascola JR, Nabel GJ, Montefiori DC, Kublin J, McElrath MJ, Corey L, Gilbert PB, HVTN 505 Study Team. 2013. Efficacy trial of a DNA/rAd5 HIV-1 preventive vaccine. N Engl J Med 369:2083–2092. doi: 10.1056/NEJMoa1310566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janes HE, Cohen KW, Frahm N, De Rosa SC, Sanchez B, Hural J, Magaret CA, Karuna S, Bentley C, Gottardo R, Finak G, Grove D, Shen M, Graham BS, Koup RA, Mulligan MJ, Koblin B, Buchbinder SP, Keefer MC, Adams E, Anude C, Corey L, Sobieszczyk M, Hammer SM, Gilbert PB, McElrath MJ. 2017. Higher T-cell responses induced by DNA/rAd5 HIV-1 preventive vaccine are associated with lower HIV-1 infection risk in an efficacy trial. J Infect Dis 215:1376–1385. doi: 10.1093/infdis/jix086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fong Y, Shen X, Ashley VC, Deal A, Seaton KE, Yu C, Grant SP, Ferrari G, deCamp AC, Bailer RT, Koup RA, Montefiori D, Haynes BF, Sarzotti-Kelsoe M, Graham BS, Carpp LN, Hammer SM, Sobieszczyk M, Karuna S, Swann E, DeJesus E, Mulligan M, Frank I, Buchbinder S, Novak RM, McElrath MJ, Kalams S, Keefer M, Frahm NA, Janes HE, Gilbert PB, Tomaras GD. 2018. Modification of the association between T-cell immune responses and human immunodeficiency virus type 1 infection risk by vaccine-induced antibody responses in the HVTN 505 trial. J Infect Dis 217:1280–1288. doi: 10.1093/infdis/jiy008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.deCamp AC, Rolland M, Edlefsen PT, Sanders-Buell E, Hall B, Magaret CA, Fiore-Gartland AJ, Juraska M, Carpp LN, Karuna ST, Bose M, LePore S, Miller S, O'Sullivan A, Poltavee K, Bai H, Dommaraju K, Zhao H, Wong K, Chen L, Ahmed H, Goodman D, Tay MZ, Gottardo R, Koup RA, Bailer R, Mascola JR, Graham BS, Roederer M, O’Connell RJ, Michael NL, Robb ML, Adams E, D’Souza P, Kublin J, Corey L, Geraghty DE, Frahm N, Tomaras GD, McElrath MJ, Frenkel L, Styrchak S, Tovanabutra S, Sobieszczyk ME, Hammer SM, Kim JH, Mullins JI, Gilbert PB. 2017. Sieve analysis of breakthrough HIV-1 sequences in HVTN 505 identifies vaccine pressure targeting the CD4 binding site of Env-gp120. PLoS One 12:e0185959. doi: 10.1371/journal.pone.0185959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang Y, Follmann D, Nason M, Zhang L, Huang Y, Mehrotra DV, Moodie Z, Metch B, Janes H, Keefer MC, Churchyard G, Robb ML, Fast PE, Duerr A, McElrath MJ, Corey L, Mascola JR, Graham BS, Sobieszczyk ME, Kublin JG, Robertson M, Hammer SM, Gray GE, Buchbinder SP, Gilbert PB. 2015. Effect of rAd5-vector HIV-1 preventive vaccines on HIV-1 acquisition: a participant-level meta-analysis of randomized trials. PLoS One 10:e0136626. doi: 10.1371/journal.pone.0136626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng X, Li SS, Gilbert PB, Geraghty DE, Katze MG. 2016. FCGR2C polymorphisms associated with HIV-1 vaccine protection are linked to altered gene expression of Fc-gamma receptors in human B cells. PLoS One 11:e0152425. doi: 10.1371/journal.pone.0152425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.1000 Genomes Project Consortium, Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini JL, McCarthy S, McVean GA, Abecasis GR. 2015. A global reference for human genetic variation. Nature 526:68–74. doi: 10.1038/nature15393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forthal DN, Gabriel EE, Wang A, Landucci G, Phan TB. 2012. Association of Fcgamma receptor IIIa genotype with the rate of HIV infection after gp120 vaccination. Blood 120:2836–2842. doi: 10.1182/blood-2012-05-431361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan KR, Zhang SL, Tan HC, Chan YK, Chow A, Lim AP, Vasudevan SG, Hanson BJ, Ooi EE. 2011. Ligation of Fc gamma receptor IIB inhibits antibody-dependent enhancement of dengue virus infection. Proc Natl Acad Sci U S A 108:12479–12484. doi: 10.1073/pnas.1106568108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boonnak K, Slike BM, Donofrio GC, Marovich MA. 2013. Human FcgammaRII cytoplasmic domains differentially influence antibody-mediated dengue virus infection. J Immunol 190:5659–5665. doi: 10.4049/jimmunol.1203052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gunawardana SA, Shaw RH. 2018. Cross-reactive dengue virus-derived monoclonal antibodies to Zika virus envelope protein: panacea or Pandora’s box? BMC Infect Dis 18:641. doi: 10.1186/s12879-018-3572-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zimmerman MG, Quicke KM, O'Neal JT, Arora N, Machiah D, Priyamvada L, Kauffman RC, Register E, Adekunle O, Swieboda D, Johnson EL, Cordes S, Haddad L, Chakraborty R, Coyne CB, Wrammert J, Suthar MS. 2018. Cross-reactive dengue virus antibodies augment Zika virus infection of human placental macrophages. Cell Host Microbe 24:731–742. doi: 10.1016/j.chom.2018.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang SF, Tseng SP, Yen CH, Yang JY, Tsao CH, Shen CW, Chen KH, Liu FT, Liu WT, Chen YM, Huang JC. 2014. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun 451:208–214. doi: 10.1016/j.bbrc.2014.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takada A, Feldmann H, Ksiazek TG, Kawaoka Y. 2003. Antibody-dependent enhancement of Ebola virus infection. J Virol 77:7539–7544. doi: 10.1128/jvi.77.13.7539-7544.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sauter P, Hober D. 2009. Mechanisms and results of the antibody-dependent enhancement of viral infections and role in the pathogenesis of coxsackievirus B-induced diseases. Microbes Infect 11:443–451. doi: 10.1016/j.micinf.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Katzelnick LC, Gresh L, Halloran ME, Mercado JC, Kuan G, Gordon A, Balmaseda A, Harris E. 2017. Antibody-dependent enhancement of severe dengue disease in humans. Science 358:929–932. doi: 10.1126/science.aan6836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takeda A, Tuazon CU, Ennis FA. 1988. Antibody-enhanced infection by HIV-1 via Fc receptor-mediated entry. Science 242:580–583. doi: 10.1126/science.2972065. [DOI] [PubMed] [Google Scholar]
- 27.Homsy J, Meyer M, Tateno M, Clarkson S, Levy JA. 1989. The Fc and not CD4 receptor mediates antibody enhancement of HIV infection in human cells. Science 244:1357–1360. doi: 10.1126/science.2786647. [DOI] [PubMed] [Google Scholar]
- 28.Gorlani A, Forthal DN. 2013. Antibody-dependent enhancement and the risk of HIV infection. Curr HIV Res 11:421–426. doi: 10.2174/1570162X113116660062. [DOI] [PubMed] [Google Scholar]
- 29.Homsy J, Meyer M, Levy JA. 1990. Serum enhancement of human immunodeficiency virus (HIV) infection correlates with disease in HIV-infected individuals. J Virol 64:1437–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams WB, Liao HX, Moody MA, Kepler TB, Alam SM, Gao F, Wiehe K, Trama AM, Jones K, Zhang R, Song H, Marshall DJ, Whitesides JF, Sawatzki K, Hua A, Liu P, Tay MZ, Seaton KE, Shen X, Foulger A, Lloyd KE, Parks R, Pollara J, Ferrari G, Yu JS, Vandergrift N, Montefiori DC, Sobieszczyk ME, Hammer S, Karuna S, Gilbert P, Grove D, Grunenberg N, McElrath MJ, Mascola JR, Koup RA, Corey L, Nabel GJ, Morgan C, Churchyard G, Maenza J, Keefer M, Graham BS, Baden LR, Tomaras GD, Haynes BF. 2015. HIV-1 vaccines. Diversion of HIV-1 vaccine-induced immunity by gp41-microbiota cross-reactive antibodies. Science 349:aab1253. doi: 10.1126/science.aab1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foster TL, Wilson H, Iyer SS, Coss K, Doores K, Smith S, Kellam P, Finzi A, Borrow P, Hahn BH, Neil S. 2016. Resistance of transmitted founder HIV-1 to IFITM-mediated restriction. Cell Host Microbe 20:429–442. doi: 10.1016/j.chom.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Iyer SS, Bibollet-Ruche F, Sherrill-Mix S, Learn GH, Plenderleith L, Smith AG, Barbian HJ, Russell RM, Gondim MV, Bahari CY, Shaw CM, Li Y, Decker T, Haynes BF, Shaw GM, Sharp PM, Borrow P, Hahn BH. 2017. Resistance to type 1 interferons is a major determinant of HIV-1 transmission fitness. Proc Natl Acad Sci U S A 114:E590–E599. doi: 10.1073/pnas.1620144114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Swiecki M, Colonna M. 2015. The multifaceted biology of plasmacytoid dendritic cells. Nat Rev Immunol 15:471–485. doi: 10.1038/nri3865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doyle T, Goujon C, Malim MH. 2015. HIV-1 and interferons: who’s interfering with whom? Nat Rev Microbiol 13:403–413. doi: 10.1038/nrmicro3449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guilliams M, Bruhns P, Saeys Y, Hammad H, Lambrecht BN. 2014. The function of Fcgamma receptors in dendritic cells and macrophages. Nat Rev Immunol 14:94–108. doi: 10.1038/nri3582. [DOI] [PubMed] [Google Scholar]
- 36.Newling M, Hoepel W, Vogelpoel LTC, Heineke MH, van Burgsteden JA, Taanman-Kueter EWM, Eggink D, Kuijpers TW, Beaumont T, van Egmond M, Kapsenberg ML, Baeten DLP, den Dunnen J, Jong EC. 2018. Fc gamma receptor IIa suppresses type I and III interferon production by human myeloid immune cells. Eur J Immunol 48:1796–1809. doi: 10.1002/eji.201847615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prentice HA, Tomaras GD, Geraghty DE, Apps R, Fong Y, Ehrenberg PK, Rolland M, Kijak GH, Krebs SJ, Nelson W, DeCamp A, Shen X, Yates NL, Zolla-Pazner S, Nitayaphan S, Rerks-Ngarm S, Kaewkungwal J, Pitisuttithum P, Ferrari G, McElrath MJ, Montefiori DC, Bailer RT, Koup RA, O’Connell RJ, Robb ML, Michael NL, Gilbert PB, Kim JH, Thomas R. 2015. HLA class II genes modulate vaccine-induced antibody responses to affect HIV-1 acquisition. Sci Transl Med 7:296ra112. doi: 10.1126/scitranslmed.aab4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gartland AJ, Li S, McNevin J, Tomaras GD, Gottardo R, Janes H, Fong Y, Morris D, Geraghty DE, Kijak GH, Edlefsen PT, Frahm N, Larsen BB, Tovanabutra S, Sanders-Buell E, deCamp AC, Magaret CA, Ahmed H, Goodridge JP, Chen L, Konopa P, Nariya S, Stoddard JN, Wong K, Zhao H, Deng W, Maust BS, Bose M, Howell S, Bates A, Lazzaro M, O'Sullivan A, Lei E, Bradfield A, Ibitamuno G, Assawadarachai V, O'Connell RJ, deSouza MS, Nitayaphan S, Rerks-Ngarm S, Robb ML, Sidney J, Sette A, Zolla-Pazner S, Montefiori D, McElrath MJ, Mullins JI, Kim JH, Gilbert PB, Hertz T. 2014. Analysis of HLA A*02 association with vaccine efficacy in the RV144 HIV-1 vaccine trial. J Virol 88:8242–8255. doi: 10.1128/JVI.01164-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lefranc MP, Lefranc G. 2012. Human Gm, Km, and Am allotypes and their molecular characterization: a remarkable demonstration of polymorphism. Methods Mol Biol 882:635–680. doi: 10.1007/978-1-61779-842-9_34. [DOI] [PubMed] [Google Scholar]
- 40.Pandey JP, Li Z. 2013. The forgotten tale of immunoglobulin allotypes in cancer risk and treatment. Exp Hematol Oncol 2:6. doi: 10.1186/2162-3619-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meinderts SM, Sins JWR, Fijnvandraat K, Nagelkerke SQ, Geissler J, Tanck MW, Bruggeman C, Biemond BJ, Rijneveld AW, Kerkhoffs JH, Pakdaman S, Habibi A, van Bruggen R, Kuijpers TW, Pirenne F, van den Berg TK. 2017. Nonclassical FCGR2C haplotype is associated with protection from red blood cell alloimmunization in sickle cell disease. Blood 130:2121–2130. doi: 10.1182/blood-2017-05-784876. [DOI] [PubMed] [Google Scholar]
- 42.Hollox EJ, Hoh BP. 2014. Human gene copy number variation and infectious disease. Hum Genet 133:1217–1233. doi: 10.1007/s00439-014-1457-x. [DOI] [PubMed] [Google Scholar]
- 43.Lassauniere R, Tiemessen CT. 2016. Variability at the FCGR locus: characterization in black South Africans and evidence for ethnic variation in and out of Africa. Genes Immun 17:93–104. doi: 10.1038/gene.2015.60. [DOI] [PubMed] [Google Scholar]
- 44.Niederer HA, Willcocks LC, Rayner TF, Yang W, Lau YL, Williams TN, Scott JA, Urban BC, Peshu N, Dunstan SJ, Hien TT, Phu NH, Padyukov L, Gunnarsson I, Svenungsson E, Savage CO, Watts RA, Lyons PA, Clayton DG, Smith KG. 2010. Copy number, linkage disequilibrium and disease association in the FCGR locus. Hum Mol Genet 19:3282–3294. doi: 10.1093/hmg/ddq216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Machado LR, Hardwick RJ, Bowdrey J, Bogle H, Knowles TJ, Sironi M, Hollox EJ. 2012. Evolutionary history of copy-number-variable locus for the low-affinity Fcgamma receptor: mutation rate, autoimmune disease, and the legacy of helminth infection. Am J Hum Genet 90:973–985. doi: 10.1016/j.ajhg.2012.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pyo CW, Guethlein LA, Vu Q, Wang R, Abi-Rached L, Norman PJ, Marsh SG, Miller JS, Parham P, Geraghty DE. 2010. Different patterns of evolution in the centromeric and telomeric regions of group A and B haplotypes of the human killer cell Ig-like receptor locus. PLoS One 5:e15115. doi: 10.1371/journal.pone.0015115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pyo CW, Wang R, Vu Q, Cereb N, Yang SY, Duh FM, Wolinsky S, Martin MP, Carrington M, Geraghty DE. 2013. Recombinant structures expand and contract inter and intragenic diversification at the KIR locus. BMC Genomics 14:89. doi: 10.1186/1471-2164-14-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lappalainen T, Sammeth M, Friedländer MR, ‘T Hoen PAC, Monlong J, Rivas MA, Gonzàlez-Porta M, Kurbatova N, Griebel T, Ferreira PG, Barann M, Wieland T, Greger L, van Iterson M, Almlöf J, Ribeca P, Pulyakhina I, Esser D, Giger T, Tikhonov A, Sultan M, Bertier G, MacArthur DG, Lek M, Lizano E, Buermans HPJ, Padioleau I, Schwarzmayr T, Karlberg O, Ongen H, Kilpinen H, Beltran S, Gut M, Kahlem K, Amstislavskiy V, Stegle O, Pirinen M, Montgomery SB, Donnelly P, McCarthy MI, Flicek P, Strom TM, Lehrach H, Schreiber S, Sudbrak R, Carracedo Á, Antonarakis SE, Häsler R, Syvänen A-C, van Ommen G-J, Brazma A, Meitinger T, Rosenstiel P, Guigó R, Gut IG, Estivill X, Dermitzakis ET. 2013. Transcriptome and genome sequencing uncovers functional variation in humans. Nature 501:506–511. doi: 10.1038/nature12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ackerman ME, Crispin M, Yu X, Baruah K, Boesch AW, Harvey DJ, Dugast AS, Heizen EL, Ercan A, Choi I, Streeck H, Nigrovic PA, Bailey-Kellogg C, Scanlan C, Alter G. 2013. Natural variation in Fc glycosylation of HIV-specific antibodies impacts antiviral activity. J Clin Investig 123:2183–2192. doi: 10.1172/JCI65708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ackerman ME, Dugast AS, McAndrew EG, Tsoukas S, Licht AF, Irvine DJ, Alter G. 2013. Enhanced phagocytic activity of HIV-specific antibodies correlates with natural production of immunoglobulins with skewed affinity for FcgammaR2a and FcgammaR2b. J Virol 87:5468–5476. doi: 10.1128/JVI.03403-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mahan AE, Jennewein MF, Suscovich T, Dionne K, Tedesco J, Chung AW, Streeck H, Pau M, Schuitemaker H, Francis D, Fast P, Laufer D, Walker BD, Baden L, Barouch DH, Alter G. 2016. Antigen-specific antibody glycosylation is regulated via vaccination. PLoS Pathog 12:e1005456. doi: 10.1371/journal.ppat.1005456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blackburn TE, Santiago T, Burrows PD. 2017. FCRLA-a resident endoplasmic reticulum protein that associates with multiple immunoglobulin isotypes in B lineage cells. Curr Top Microbiol Immunol 408:47–65. doi: 10.1007/82_2017_40. [DOI] [PubMed] [Google Scholar]
- 53.Santiago T, Kulemzin SV, Reshetnikova ES, Chikaev NA, Volkova OY, Mechetina LV, Zhao M, Davis RS, Taranin AV, Najakshin AM, Hendershot LM, Burrows PD. 2011. FCRLA is a resident endoplasmic reticulum protein that associates with intracellular Igs, IgM, IgG and IgA. Int Immunol 23:43–53. doi: 10.1093/intimm/dxq456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blank MC, Stefanescu RN, Masuda E, Marti F, King PD, Redecha PB, Wurzburger RJ, Peterson MG, Tanaka S, Pricop L. 2005. Decreased transcription of the human FCGR2B gene mediated by the -343 G/C promoter polymorphism and association with systemic lupus erythematosus. Hum Genet 117:220–227. doi: 10.1007/s00439-005-1302-3. [DOI] [PubMed] [Google Scholar]
- 55.Su K, Wu J, Edberg JC, Li X, Ferguson P, Cooper GS, Langefeld CD, Kimberly RP. 2004. A promoter haplotype of the immunoreceptor tyrosine-based inhibitory motif-bearing FcgammaRIIb alters receptor expression and associates with autoimmunity. I. Regulatory FCGR2B polymorphisms and their association with systemic lupus erythematosus. J Immunol 172:7186–7191. doi: 10.4049/jimmunol.172.11.7186. [DOI] [PubMed] [Google Scholar]
- 56.Mueller M, Barros P, Witherden AS, Roberts AL, Zhang Z, Schaschl H, Yu CY, Hurles ME, Schaffner C, Floto RA, Game L, Steinberg KM, Wilson RK, Graves TA, Eichler EE, Cook HT, Vyse TJ, Aitman TJ. 2013. Genomic pathology of SLE-associated copy-number variation at the FCGR2C/FCGR3B/FCGR2B locus. Am J Hum Genet 92:28–40. doi: 10.1016/j.ajhg.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Floto RA, Clatworthy MR, Heilbronn KR, Rosner DR, MacAry PA, Rankin A, Lehner PJ, Ouwehand WH, Allen JM, Watkins NA, Smith KG. 2005. Loss of function of a lupus-associated FcgammaRIIb polymorphism through exclusion from lipid rafts. Nat Med 11:1056–1058. doi: 10.1038/nm1288. [DOI] [PubMed] [Google Scholar]
- 58.Wang TT, Maamary J, Tan GS, Bournazos S, Davis CW, Krammer F, Schlesinger SJ, Palese P, Ahmed R, Ravetch JV. 2015. Anti-HA glycoforms drive B cell affinity selection and determine influenza vaccine efficacy. Cell 162:160–169. doi: 10.1016/j.cell.2015.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Richardson SI, Chung AW, Natarajan H, Mabvakure B, Mkhize NN, Garrett N, Abdool Karim S, Moore PL, Ackerman ME, Alter G, Morris L. 2018. HIV-specific Fc effector function early in infection predicts the development of broadly neutralizing antibodies. PLoS Pathog 14:e1006987. doi: 10.1371/journal.ppat.1006987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bournazos S, DiLillo DJ, Ravetch JV. 2015. The role of Fc-FcgammaR interactions in IgG-mediated microbial neutralization. J Exp Med 212:1361–1369. doi: 10.1084/jem.20151267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gunn BM, Alter G. 2016. Modulating antibody functionality in infectious disease and vaccination. Trends Mol Med 22:969–982. doi: 10.1016/j.molmed.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barrett JC, Fry B, Maller J, Daly MJ. 2005. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 63.Lin L, Finak G, Ushey K, Seshadri C, Hawn TR, Frahm N, Scriba TJ, Mahomed H, Hanekom W, Bart P-A, Pantaleo G, Tomaras GD, Rerks-Ngarm S, Kaewkungwal J, Nitayaphan S, Pitisuttithum P, Michael NL, Kim JH, Robb ML, O'Connell RJ, Karasavvas N, Gilbert P, C De Rosa S, McElrath MJ, Gottardo R. 2015. COMPASS identifies T-cell subsets correlated with clinical outcomes. Nat Biotechnol 33:610–616. doi: 10.1038/nbt.3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tomaras GD, Yates NL, Liu P, Qin L, Fouda GG, Chavez LL, Decamp AC, Parks RJ, Ashley VC, Lucas JT, Cohen M, Eron J, Hicks CB, Liao HX, Self SG, Landucci G, Forthal DN, Weinhold KJ, Keele BF, Hahn BH, Greenberg ML, Morris L, Karim SS, Blattner WA, Montefiori DC, Shaw GM, Perelson AS, Haynes BF. 2008. Initial B-cell responses to transmitted human immunodeficiency virus type 1: virion-binding immunoglobulin M (IgM) and IgG antibodies followed by plasma anti-gp41 antibodies with ineffective control of initial viremia. J Virol 82:12449–12463. doi: 10.1128/JVI.01708-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dai JY, Li SS, Gilbert PB. 2014. Case-only method for cause-specific hazards models with application to assessing differential vaccine efficacy by viral and host genetics. Biostatistics 15:196–203. doi: 10.1093/biostatistics/kxt018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Breslow NE, Holubkov R. 1997. Weighted likelihood, pseudo-likelihood and maximum likelihood methods for logistic regression analysis of two-stage data. Stat Med 16:103–116. doi:. [DOI] [PubMed] [Google Scholar]
- 67.Lumley T, Scott A. 2017. Fitting regression models to survey data. Statist Sci 32:265–278. doi: 10.1214/16-STS605. [DOI] [Google Scholar]
- 68.Follmann D, Fay MP, Proschan M. 2009. Chop-lump tests for vaccine trials. Biometrics 65:885–893. doi: 10.1111/j.1541-0420.2008.01131.x. [DOI] [PubMed] [Google Scholar]
- 69.Benjamini Y, Hochberg Y. 1995. Controlling the false discovery rate–a practical and powerful approach to multiple testing. J R Statist Soc Ser B Methodol 57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 70.Westfall PH, Young SS. 1993. Resampling-based multiple testing: examples and methods for P-value adjustment. John Wiley & Sons, Inc, Hoboken, NJ. [Google Scholar]
- 71.Westfall PH, Troendle JF. 2008. Multiple testing with minimal assumptions. Biom J 50:745–755. doi: 10.1002/bimj.200710456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Montgomery SB, Sammeth M, Gutierrez-Arcelus M, Lach RP, Ingle C, Nisbett J, Guigo R, Dermitzakis ET. 2010. Transcriptome genetics using second generation sequencing in a Caucasian population. Nature 464:773–777. doi: 10.1038/nature08903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stegle O, Parts L, Durbin R, Winn J. 2010. A Bayesian framework to account for complex non-genetic factors in gene expression levels greatly increases power in eQTL studies. PLoS Comput Biol 6:e1000770. doi: 10.1371/journal.pcbi.1000770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shabalin AA. 2012. Matrix eQTL: ultra fast eQTL analysis via large matrix operations. Bioinformatics 28:1353–1358. doi: 10.1093/bioinformatics/bts163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. 2015. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4:7. doi: 10.1186/s13742-015-0047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Neidich SD, Fong Y, Li SS, Geraghty DE, Williamson BD, Young WC, Goodman D, Seaton KE, Shen X, Sawant S, Zhang L, deCamp AC, Blette BS, Shao M, Yates NL, Feely F, Pyo CW, Ferrari G, the HVTN 505 Team, Frank I, Karuna ST, Swann EM, Mascola JR, Graham BS, Hammer SM, Sobieszczyk ME, Corey L, Janes HE, McElrath MJ, Gottardo R, Gilbert PB, Tomaras GD. Antibody Fc-functions and IgG3 associates with decreased HIV-1 risk. J Clin Investig, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.