Abstract
Ciliated hepatic foregut cyst (CHFC) is a rare benign cyst of the liver derived from an embryonic remnant of foregut epithelium. CHFC is typically asymptomatic and is found incidentally. Recent reports of malignant transformation may warrant surgical removal of CHFC. We present the case of a 54-year-old male who was discovered to have a CHFC while undergoing kidney transplant evaluation.
1. Introduction
Ciliated hepatic foregut cyst (CHFC) is a rare benign cyst of the liver derived from an embryonic remnant of foregut epithelium [1]. Patients with CHFC are almost always asymptomatic and mostly incidentally found on abdominal imaging. Although CHFC is benign and generally appears as a simple cyst on imaging, it has been reported to mimic appearance of hepatic cystic neoplasm on cross sectional imaging and rarely reported to be associated with malignancy [2]. With increasing utilization of abdominal cross images, and advancement in computerized tomography (CT) and magnetic resonance imaging (MRI), incidental hepatic cysts are increasingly detected, yet CHFC remains extremely uncommon [3]. Herein, we present a case of CHFC resembling a hepatic cystic neoplasm detected during kidney transplant evaluation.
2. Case Report
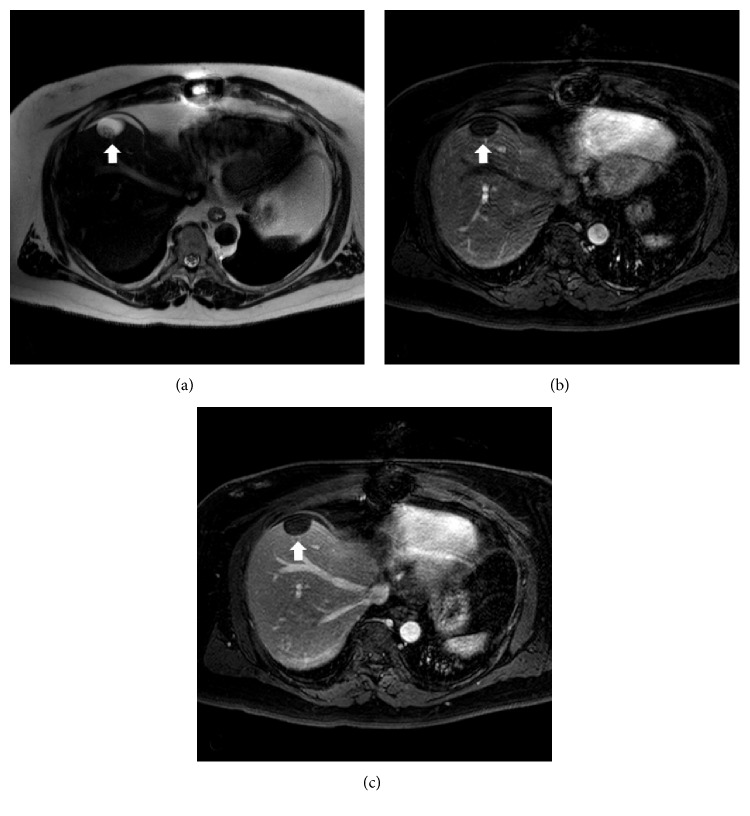
A 54-year-old male with end stage renal disease undergoing kidney transplant evaluation presented to hepatology clinic for further evaluation of a hepatic cyst. The cyst was incidentally found on abdominal CT, and the patient was completely asymptomatic. A noncontrast abdominal CT scan revealed a 2.3 cm lesion of low attenuation in segment IVa of the liver. Additional workup including, bilirubin, ALT, AST, GGT, hepatitis B, C, and HIV screening were unremarkable. A subsequent contrast enhanced abdominal magnetic resonance imaging (MRI) scan confirmed a 2.8 cm hypodense cyst with a 1.7 cm solid component in the posterior aspect of the cyst with enhancement. A follow-up contrast enhanced MRI was performed, which demonstrated persistent of solid component (Figure 1).
Figure 1.
Transverse abdominal MRI of hepatic cyst. (a) T2-weighted image. (b) Arterial phase following intravenous contrast. (c) Venous phase following intravenous contrast.
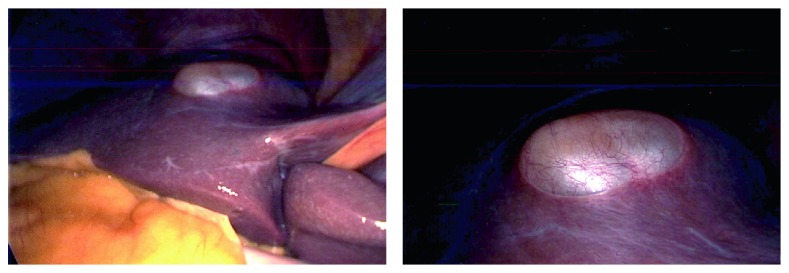
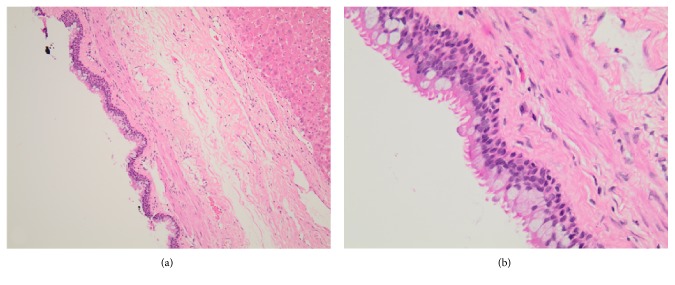
Considering the persistent 1.7 cm solid component in the cyst, concern of hepatic cystic neoplasm was entertained. Additionally, immunosuppression after kidney transplant may facilitate progression of a neoplastic process if left untreated. Therefore, the decision was made to proceed with surgical resection. A laparoscopic approach was initially performed, which revealed a superficial hepatic cyst within segment IV of the liver, consistent with prior imaging. Given the location of the cyst, it was decided to convert to an open surgical approach. A tan, thin-walled, mucin-filled cyst (2.7 × 2.0 × 1.1 cm) was removed via cyst enucleation without complication (Figure 2). The patient received hemodialysis post-operative day (POD) 1, was advanced to a general diet POD 2, and was discharged home on POD 3. Histology revealed a ciliated pseudostratified epithelium consistent with a CHFC (Figure 3).
Figure 2.
Intra-operative view of ciliated hepatic foregut cyst.
Figure 3.
Histological sample of ciliated hepatic foregut cyst with hematoxylin and eosin staining. (a) Low power magnification. (b) High-power magnification.
3. Discussion
CHFC is a rare benign hepatic cyst originally described by Wheeler and Edmonson as a cystic remnant of foregut epithelium similar to bronchogenic and esophageal cysts [1]. A literature review discovered 109 reported cases since 1964. Histologically, CHFCs classically consist of 4 layers, including a ciliated pseudostratified columnar epithelium, subepithelial connective tissue, a smooth muscle layer, and an outer fibrous capsule [1]. CHFCs are typically discovered during the fifth decade of life, but may present at any age [2–4]. Most patients are asymptomatic at time of diagnosis. When symptomatic, the majority present with right upper quadrant abdominal pain [2, 3]. However, a few cases of CHFCs causing jaundice from biliary obstruction have been reported [5, 6]. Classically, CHFCs are located in the left lobe of the liver, specifically segment IV, but can present within the right lobe as well [2, 3]. Additionally, extrahepatic locations, such as the gallbladder and extrahepatic biliary system, have been reported [2, 6–8].
Radiographic imaging is usually insufficient for diagnosis given the variability in appearance. Typically, CHFCs are small (<4 cm), subcapsular, unilocular, and fluid-filled, but may present with findings suggestive of solid debris as seen in the above patient [2, 3, 10, 11]. Ultrasound evaluation usually reveals a hypoechoic cyst and hyperdense without contrast enhancement on CT imaging [10]. Large variability is seen on MRI T1-weighted imaging, but CHFCs are nearly exclusively hyperintense on T2-weighted imaging [3, 10, 11]. The variety of imaging findings provide for a large differential which includes, simple cysts, mucinous cystic neoplasm (MCN), pyogenic abscess, amebic abscess, hydatid cyst, intrahepatic pseudocyst, biliary cystadenoma, and cystadenocarcinoma [12].
Definitive diagnosis is made through histology which reveals a pseudostratified columnar epithelium, subepithelial connective tissue layer, smooth muscle layer, and outer fibrous capsule [1]. Presence of cartilage and respiratory glands would be suggestive of a bronchogenic cyst and are absent in CHFCs. Fine needle aspiration (FNA) cytology may provide for a nonsurgical diagnosis with reports of a positive predictive value of 76% [3, 13]. The finding of pseudostratified squamous epithelium in a mucoid background is nearly diagnostic, given the absence of other liver pathology with similar cytology [13].
Although CHFCs were originally believed to be benign, more recent reports of CHFCs undergoing malignant transformation have challenged that dogma [14, 16]. Rates of malignant transformation were reported to range from 3% to 5% with squamous cell carcinoma being the most common malignancy [2, 3]. Size appears to be the largest risk factor for malignant transformation in CHFCs [2, 3]. Rates of malignant transformation are lower than those seen in MCN, which may be as high as 10% [17]. The role of carbohydrate antigen (CA) 19-9, and/or carcinoembryonic antigen (CEA) as a marker of malignant progression in CHFC does not appear helpful. There have been reports of patients with CHFC discovered to have elevated serum CEA, and elevated intra-cystic CEA and CA19-19 in the absence of malignancy [6, 16]. The current management of CHFC remains controversial. Given the potential risk of malignant transformation, most agree that surgical excision, increasingly performed through a laparoscopic approach, should be performed if the cyst is greater than 4–5 cm, symptomatic, growing, or possesses wall abnormalities on imaging [18, 19]. In the absence of radiographic features concerning for malignancy, a more conservative approach with serial imaging could be considered given the overall low risk of malignant transformation, particularly when lacking the above features.
CHFC is a rare cyst, but has been more frequently diagnosed in recent years. Given the potential for malignant transformation, it is an important diagnosis to consider in the setting of a hepatic cyst. Due to the limited number of cases, further characterization and understanding of the disease is important.
Consent
Patient consent to publish case details was verbally obtained.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Ambe C., Gonzalez-Cuyar L., Farooqui S., Hanna N., Cunningham S. C. Ciliated hepatic foregut cyst: 103 cases in the world literature. Open Journal of Pathology. 2012;2(3):45–49. doi: 10.4236/ojpathology.2012.23010. [DOI] [Google Scholar]
- 2.Sharma S., Corn A., Kohli V., Wright H. I., Sebastian A., Jabbour N. Ciliated hepatic foregut cyst: an increasingly diagnosed condition. Digestive Diseases and Sciences. 2008;7(6):581–589. doi: 10.1007/s10620-008-0203-4. [DOI] [PubMed] [Google Scholar]
- 3.Wheeler D. A., Edmondson H. A. Ciliated hepatic foregut cyst. The American Journal of Surgical Pathology. 1984;8(6):467–470. doi: 10.1097/00000478-198406000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Betalli P., Gobbi D., Talenti E., Alaggio R., Gamba P., Zanon G. F. Ciliated hepatic foregut cyst: from antenatal diagnosis to surgery. Pediatrc Radiology. 2008;38(2):230–232. doi: 10.1007/s00247-007-0648-1. [DOI] [PubMed] [Google Scholar]
- 5.Kiyochi H., Okada K., Iwakawa K., et al. Ciliated hepatic foregut cyst with obstructive jaundice. Case Reports in Gastroenterology. 2008;2(3):479–485. doi: 10.1159/000176062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bishop K. C., Perrino C. M., Ruzinova M. B., Brunt E. M. Ciliated hepatic foregut cyst: a report of 6 cases and a review of the English literature. Diagnostic Pathology. 2015;10(1) doi: 10.1186/s13000-015-0321-1.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Beteddini O. S., Amra N. K., Sherkawi E. Ciliated foregut cyst in the triangle of calot: the first report. Surgical Case Reports. 2016;2(1) doi: 10.1186/s40792-016-0147-4.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cottreau J., Costa A., Walsh M., Arnason T. Ciliated foregut cyst of the common hepatic duct: an unusual mimic of a type II choledochal cyst. International Journal of Surgical Pathology. 2016;24(7):644–647. doi: 10.1177/1066896916648449. [DOI] [PubMed] [Google Scholar]
- 9.Koletsa T., Tzioufa V., Michalopoulos A., Apostolidis S., Papadopoulos B., Hytiroglou P. Ciliated hepatic foregut cyst communicating with the gallbladder. Virchows Archiv. 2005;446(2):200–201. doi: 10.1007/s00428-004-1152-8. [DOI] [PubMed] [Google Scholar]
- 10.Boumoud M., Daghfous A., Maghrebi H., et al. Imaging features of ciliated hepatic foregut cyst. Diagnostic and Interventional Imaging. 2015;96(3):301–303. doi: 10.1016/j.diii.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Ansari-Gilani K., Modaresi Esfeh J. Ciliated hepatic foregut cyst: report of three cases and review of imaging features. Gastroenterology Report. 2017;5(1):75–78. doi: 10.1093/gastro/gov028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borhani A. A., Wiant A., Heller M. T. Cystic hepatic lesions: a review and an algorithmic approach. American Journal of Roentgenology. 2014;203(6):1192–1204. doi: 10.2214/AJR.13.12386. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan K. J., Escobar M., Alonzo M., Berlin J. W. Ciliated hepatic foregut cyst: report of a case on fine-needle aspiration. Diagnostic Cytopathology Banner. 2007;35(4):245–249. doi: 10.1002/dc.20622. [DOI] [PubMed] [Google Scholar]
- 14.Wilson J. M., Groeschl R., George B., et al. Ciliated hepatic cyst leading to squamous cell carcinoma of the liver–a case report and review of the literature. International Journal of Surgery Case Reports. 2013;4(11):972–975. doi: 10.1016/j.ijscr.2013.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang X., Wang Z., Dong Y. Squamous cell carcinoma arising in a ciliated hepatic foregut cyst: case report and literature review. Pathology–Research and Practice. 2009;205(7):498–501. doi: 10.1016/j.prp.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Ben Ari Z., Cohen-Ezra O., Weidenfeld J., et al. Ciliated hepatic foregut cyst with high intra-cystic carbohydrate antigen 19–9 level. World Journal of Gastroenterology. 2014;20(43):16355–16358. doi: 10.3748/wjg.v20.i43.16355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakayama Y., Kato Y., Okubo S., et al. A case of mucinous cystic neoplasm of the liver: a case report. Surgical Case Reports. 2015;1(1):p. 9. doi: 10.1186/s40792-014-0007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodman M. D., Mak G. Z., Reynolds J. P., Tevar A. D., Pritts T. A. Laparoscopic excision of a ciliated hepatic foregut cyst. Journal of the Society of Laparoendoscopic Surgeons. 2009;13(1):96–100. [PMC free article] [PubMed] [Google Scholar]
- 19.Saravanan J., Manoharan G., Jeswanth S., Ravichandran P. Laparoscopic excision of large ciliated hepatic foregut cyst. Journal of Minimal Access Surgery. 2014;10(3):151–153. doi: 10.4103/0972-9941.134879. [DOI] [PMC free article] [PubMed] [Google Scholar]