Abstract
OBJECTIVES:
To investigate the effectiveness of mini-implant (MI)-facilitated micro-osteoperforations (MOPs) in accelerating mandibular anterior teeth alignment.
MATERIALS AND METHODS:
Thirty teenage patients with mandibular crowding (Little's irregularity index between 4 and 6 mm) were randomly allocated to either “experimental” group (micro-osteoperforation assisted alignment) or “control” group (conventional orthodontics). Blinding was done at the data analysis stages. Six MOPs were performed using MI on the labial aspect in the mandibular anterior region. The primary outcome was the overall treatment time needed to complete alignment of mandibular anterior teeth. The secondary outcomes were to compare the marginal bone height loss and volumetric root resorption around mandibular incisors along with subject's perception of pain, comfort and satisfaction.
RESULTS:
There was statistically significant difference in the total treatment duration for complete alignment of mandibular incisors. The completion of cases in experimental group was 43.93% times faster than the control group. There were no statistically significant differences in volumetric root resorption and marginal alveolar bone height loss around mandibular incisors as well as pain perception between the two groups.
CONCLUSIONS:
MI-facilitated MOPs accelerated tooth movement significantly upto nine weeks without any significant pain and discomfort, with no increase in root resorption and marginal alveolar bone height loss.
Keywords: Accelerated tooth movement, dental crowding, micro-osteoperforations
Introduction
The two major concerns associated with orthodontic treatment are pain and the long treatment duration of fixed orthodontic therapy. Lengthy orthodontic treatment duration is a major concern as it is associated with negative sequelae such as discomfort, pain, white spot lesions, and decreased patients' compliance.[1,2] Hence, modalities to reduce treatment duration are an actively pursued area of research these days. Of the various approaches being researched for accelerated tooth movement (ATM) i.e., biological, mechanical, physical and surgical approaches, the surgical procedures have been found to be the most consistent and promising in achieving the desired results.[3] However the invasiveness of the surgical techniques have resulted in their low acceptance by the patients and hence lesser invasive methods are explored. The surgical methods for accelerated orthodontics are based on the regional acceleratory phenomenon (RAP) which involves an intensified remodeling process in response to a noxious stimulus. The success of these lesser invasive methods lie in reducing the invasiveness along with taking the advantage of the RAP phenomenon.
One such less invasive method using flapless shallow “cortical perforations” was tested in animal studies for enhanced tooth movement.[4] Alikhani et al.[5] described it as “micro-osteoperforations” (MOPs) in a human clinical study using the Propel device designed for this purpose. These days mini-implants (MIs) are commonly utilized tool in an orthodontic office. Realizing MOPs as an effective and safe procedure to accelerate the tooth movement and the ready acceptability of mini-implant by the patients and clinicians, we tried to investigate if mini-implants can be used to place micro-osteoperforations and if these MI-facilitated MOPs can induce ATM. During the course of our study we came across two studies testing MI-facilitated MOP thus showing increasing interest in this technique, but the contradictory findings in these studies point towards the need of more high quality RCTs for more clarity.[6,7]
To the best of our knowledge, this is the first well-designed RCT to investigate the effectiveness of MI-facilitated MOPs in accelerating mandibular anterior teeth alignment along with patient's pain and satisfaction.[5,6,7,8,9] Marginal alveolar bone height loss and volumetric root resorption which has not been assessed in any of the previous studies was also assessed in our study using CBCT.
Materials and Methods
This study was a prospective, single-blinded, two arm, parallel-group, randomized controlled clinical study with a 1:1 allocation. The CONSORT statement was used as a guide for this study.[10]
Ethical approval was obtained (PGIDS/IEC/2016/92) and the trial was also preregistered (CTRI/2017/11/010610). Date of approval: 30-11-2016. Participants were recruited by the coinvestigator from patients coming to the OPD of the department seeking orthodontic treatment and fulfilling the selection criteria. The inclusion and exclusion criteria are summarized in Table 1. Consent was obtained from the patients before starting the trial.
Table 1.
Inclusion and exclusion criteria for the study
| Inclusion criteria | Exclusion criteria |
|---|---|
| Mandibular anterior irregularity index between 4-6 mm | Inability to place bracket or breakage of any of the mandibular anterior brackets that had not been replaced within a week. |
| Age range between 14-19 years | Failure to provide oral and written consent to participation. |
| Non-extraction treatment in the mandibular arch | Previous orthodontic treatment |
| Presence of full complement of dentition from first molar to first molar with no spacing in the mandibular arch | Presence of primary or missing permanent teeth in the mandibular anterior area |
| Patient with healthy periodontium and no attachment loss of >2 mm | Medical problems that affect tooth movement. |
Sample size calculation
Based on a type I error frequency of 5% and the power of the statistical test set at 90% using previous studies[4,5] as a guide to detect at least 50% difference in the rate of tooth movement, (effect size of 1.154) resulted in 11 subjects per group. Considering 20% attrition rate, 15 patients per group (total 30) were enrolled in the present study.
Randomization
Stratified randomization method was used to ensure a 1:1 allocation ratio and allocation concealment was achieved with similar looking sealed opaque envelopes. Thirty pieces of paper were taken and on fifteen pieces the word “control” and on the other fifteen pieces, the word “experimental” was written and were then put in similar looking white opaque envelopes. Seven “control” and seven “experimental” envelopes were put in a box with the marking M for male group while the remaining sixteen envelopes were put in a box marked F for female group to equally distribute the data on a gender basis. The envelopes of the appropriate box as per the gender of the patient were shuffled by the co-investigator each time a patient was asked to pick one envelope from the box. The patient was then assigned to the group designated and recorded by the main investigator who was not involved in the data recording and analysis and who carried out the treatment according to the allotted group.
Intervention
All the participants in both treatment groups were bonded by the principal investigator with 0.022-inch slot MBT prescription appliance (Ortho Organizers, San Marcos, Calif). MOPs were placed in the experimental group before placing the initial leveling archwire. Panoramic radiographs were utilized to assess the long axis of the teeth and root proximity prior to the procedure.
Surgical procedure
The patients were asked to rinse their mouth by chlorhexidine for 1 minute. MOPs were performed by the principal investigator, under local anesthesia (2% lidocaine with 1:100,000 epinephrine) with standard asepsis using a self-drilling 1.6 mm × 8 mm orthodontic mini-implant (DENTAURUM GmbH & Co. KG) with the help of MI_screw driver (Tomas, DENTAURUM GmbH & Co. KG). MOPs were placed at three sites i.e., interproximally between mandibular canine and lateral incisor on both sides and between central incisors in the midline on labial aspect of mandible [Figure 1a]. Each site received 2 MOP's, first 2 mm apical to alveolar crest and second 2 mm below the first in a vertical line making a total of six MOPs [Figure 1b]. The depth of perforation was decided by adding gingival tissue depth (measured by transgingival probing using Williams probe) plus buccal cortical bone depth (using coronal and sagittal sections of CBCT) at the level of planned perforation sites. MI depth guides were customized using syringe and self-cure acrylic to reach the respective depth of penetration [Figure 2]. After reaching marked depth, the MI was removed by rotating MI screwdriver anticlockwise. Pressure was applied using cotton pellets to achieve hemostasis after MOPs placement.
Figure 1.
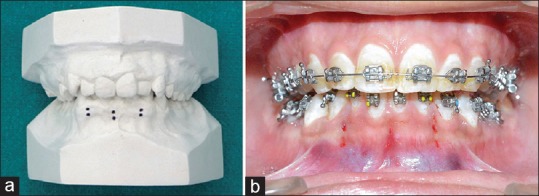
(a) MOP sites in the study shown on the study model. (b) MOP sites in the study shown clinically
Figure 2.
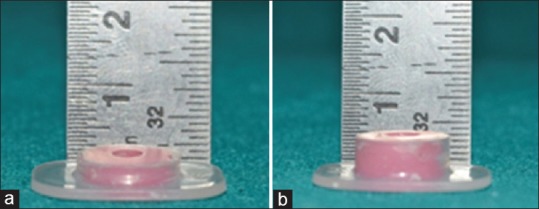
Mini implant depth guides used in the study (a) 3 mm (b) 5 mm
Orthodontic procedure
The leveling orthodontic wire (0.014” NiTi) was ligated using 0.010” steel ligature wires during the same appointment at which MOPs were placed for the experimental group and during the bonding appointment for the control group. The arch wire sequence used was 0.014-inch, 0.016-inch, 0.016 × 0.022-inch, 0.017 ×.025-inch NiTi and finally 0.019 × 0.025-inch SS and was similar in both the groups.[11] Archwires were replaced when expected improvement with tied wire was achieved and next wire could be inserted with minimal amount of deflection during full ligation.
Data collection
Mandibular study models were made just before bonding and then at all subsequent visits every 3rd week till the completion of study. Overall time needed to complete alignment of mandibular anteriors was calculated by the number of weeks between T0-T5 with T0 denoting the time at start and rest every 3 weeks i.e., T1-3rd week, T2-6th, T3-9th, T4-12th, and T5-15th week.
Little's irregularity index (LII) was used to measure the amount of crowding on the dental models at every appointment using Insize digimatic 1108-150 digital caliper (with accuracy upto 0.03 mm).[12] When the irregularity index of 0-1mm was achieved between the mandibular anterior teeth and an improvement in alignment did not exceed 0.5 mm between two consecutive appointments, the study was considered complete. The patients were advised to refrain from using analgesics like NSAIDs, unless the pain was unbearable. All subjects were asked to fill out two questionnaires[13] during the first week and one month after placement of the first wire.
The secondary outcome of pain was assessed by asking the patients to mark their level of discomfort on the day of appliance placement immediately, 4 hours, 12 hours, 24 hours, 3rd day and 7th day with visual analog scale (VAS). The marginal bone height loss and volumetric root resorption around mandibular anterior teeth aligned were assessed through CBCT. Limited Field of view (5 × 5 cm) CBCT images were obtained before starting treatment and after six months using Carestream CS-9300 imaging system with 90 micrometer voxel size; tube voltage 80-84 kVp; tube current 5-8 mA; and exposure time 20 seconds. 3D volume rendering of the DICOM data of the CBCT scans was performed with Invivo 5.2 licensed software (Anatomage, San Jose, CA, USA) with Microsoft Windows 10. Upon volume rendering, the regions of the scan outside the region of interest (ROI) were sculpted manually and removed with step by step segmentation and careful recapitulation from all the aspects of the volume rendered view. Thereafter, the mandibular incisors were isolated in the volume rendered view. Finally, the crown and root of the mandibular incisors were segmented separately, and volume of the root was calculated with the help of volume determination tool of the ROI.[14] Threshold range was determined by the Artificial Intelligence (AI) software itself for standardization. Then the volumetric root resorption was calculated by subtracting pretreatment volumetric measurement from post alignment volumetric measurement [Figure 3].
Figure 3.

Evaluation of root volume for calculating root resorption using CBCT scan
Marginal bone height[15] was measured as a perpendicular distance between cementoenamel junction and the interdental bone margin, in the coronal section at the center of buccolingual dimensions of the concerned tooth i.e., mesial to teeth (43, 41, 31, 33) and distal to teeth (42, 32). Then the marginal bone height loss was calculated by subtracting post alignment alveolar bone height value from the pretreatment alveolar bone height value [Figure 4].
Figure 4.
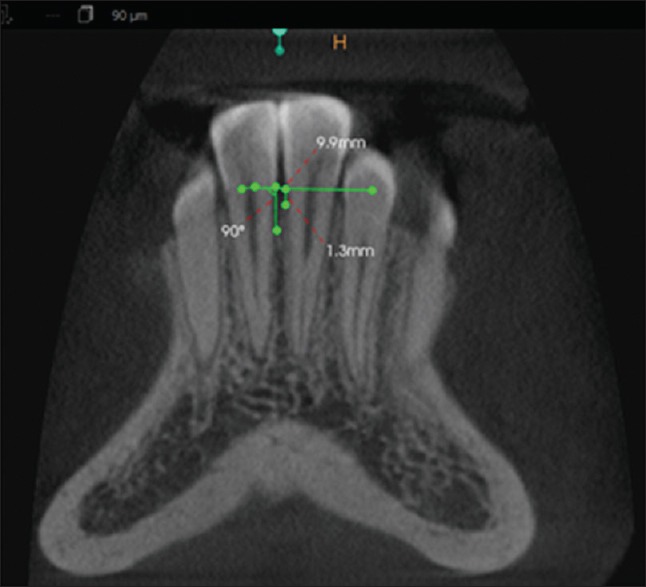
Evaluation of alveolar bone height using CBCT scan
Blinding
Patient codes were assigned to the models prior to measurement to ensure blinding of the evaluators. The subjects and the operator administering treatment were aware of the group assignment and therefore were not blinded. However, the investigators performing the measurements and data analysis were blinded from the group assignments.
Error of method
Both intraobserver and interobserver errors were evaluated. For the evaluation of the intraobserver error, 10 dental casts were randomly chosen, and Little's irregularity index was remeasured 2 weeks apart after the first measurement. For the interobserver error, a second investigator measured the same set of models twice, and the mean values of the two measurements by each investigator were compared. Similarly, the volumes of root resorption and marginal bone height of 6 randomly selected teeth were remeasured to determine the overall standard error of measurement and the coefficient of variation. Intraclass correlation (ICC) gave a strong intraexaminer reliability (ICC = 0.992), and the Dahlberg formula showed minimal error. Cronbach's alpha was 0.81 reflected the minimal error that does not affect the reliability of questionnaire.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) program version 21.0 (SPSS Inc, Chicago, USA). The data was found to be normally distributed (Shapiro-Wilk test) therefore, parametric tests were used. Independent sample t test was used to compare the overall time needed to complete alignment of mandibular anterior teeth, alignment improvement percentage, root resorption, and marginal bone height loss. Frequencies and responses to questionnaire were compared using Chi square test. For all the statistical tests, P < 0.05 was considered to be statistically significant.
Results
Patient flow through the study is illustrated in the CONSORT flow diagram [Figure 5].[10] Thirty patients were recruited and allocated randomly to either the experimental group or the control group. No dropout occurred, and complete follow-up and analysis were achieved for all patients.
Figure 5.
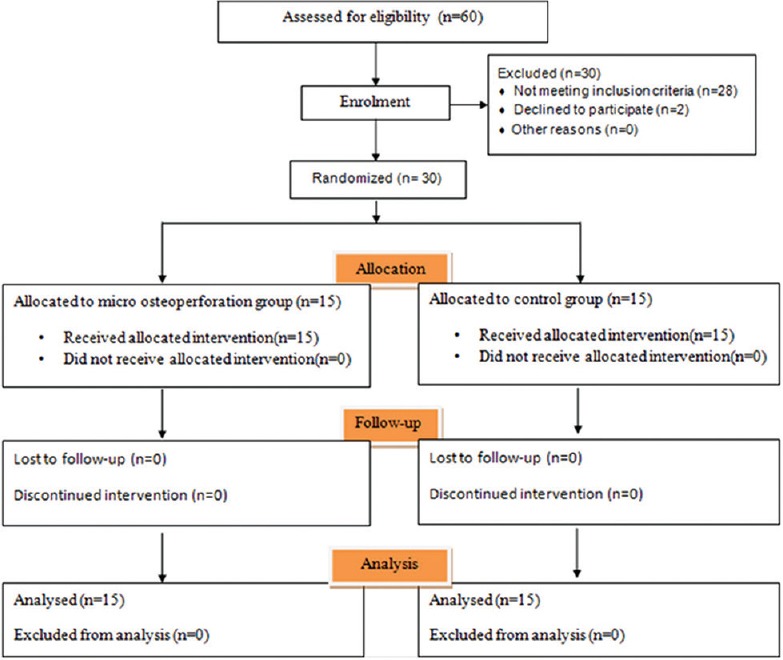
CONSORT FLOW DIAGRAM
Baseline data
The statistical comparison of the baseline data between the two groups did not reveal any significant difference [Table 2].
Table 2.
Demographics and clinical characteristics of sample
| Variable | Total | Control | Experimental | P | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age (years) | 15.6 | 1.476 | 15.33 | 1.175 | 15.87 | 1.727 | 0.331* |
| Gender | |||||||
| Male | 14 | 7 | 7 | ||||
| Female | 16 | 8 | 8 | ||||
| Crowding (irregularity index) mm | 5.33 | 0.329 | 5.31 | 0.361 | 5.35 | 0.304 | 0.729* |
*P≥0.05 is non-significant
Primary outcome
The overall treatment time needed to complete alignment in experimental group and control group was 7.40 ± 1.549 week and 13.20 ± 1.521 week, respectively. There was statistically highly significant difference seen for the intergroup comparison of the case completion time in weeks with the completion of cases in experimental group 43.93% times faster than the control group [Table 3].
Table 3.
Intergroup comparison of mean treatment time needed for complete alignment of mandibular anterior teeth
| Groups | n | Mean | Std. Deviation | P |
|---|---|---|---|---|
| Experimental | 15 | 7.40 | 1.549 | 0.000* |
| Control | 15 | 13.20 | 1.521 |
n – Number of subjects. *P≤0.001 is highly significant
Mean crowding of mandibular incisors in the experimental group was 5.31 mm at T0, 2.76 mm at T1, 1.08 mm at T2, 0.50 mm at T3 while in the control group, it was 5.35 mm at T0, 4.14 mm at T1, 3.08 mm at T2, 1.91 mm at T3, 0.93 mm at T4 and 0.38 mm at T5 respectively [Figure 6 and Table 4]. The difference in the value of LII during the time intervals (i.e., T1, T2, T3) between the two groups was statistically significant. Alignment improvement percentage was calculated by dividing the amount of change in the LII value at a specific time point (calculated by subtracting the LII value at T1, T2, or T3 from the LII value at T0) by LII value at T0 and was 113.10% (2.13 times), 88.95% (1.88 times) and 42.09% (1.42 times) faster at the end of 3rd, 6th, and 9th week respectively, as compared to the control group [Table 5].[16]
Figure 6.
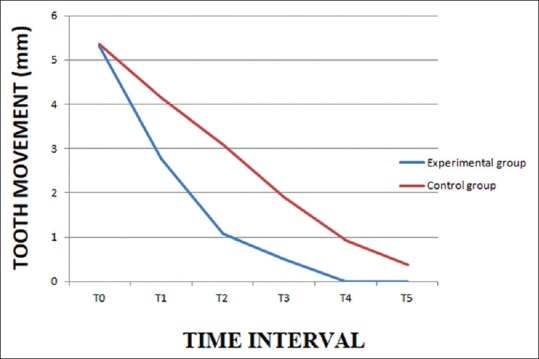
Intergroup comparison of amount of mandibular anterior crowding at different time intervals
Table 4.
Intergroup comparison of amount of crowding in mandibular incisors at various time intervals
| Time Interval | Experimental group | Control group | P | Mean difference (mm) (95% CI) | ||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |||
| T0 | 5.31 | 0.3615 | 5.35 | 0.3046 | 0.729* | −0.04 (−0.29, 0.21) |
| T1 | 2.76 | 0.5681 | 4.14 | 0.3469 | 0.000** | −1.38 (−1.732, −1.028) |
| T2 | 1.08 | 0.5053 | 3.08 | 0.4579 | 0.000** | −2 (−2.361, −1.639) |
| T3 | 0.50 | 0.200 | 1.91 | 0.4319 | 0.000** | −1.41 (−1.662, −1.158) |
| T4 | - | - | 0.93 | 0.2611 | - | - |
| T5 | - | - | 0.38 | 0.0449 | - | - |
T0, Baseline; T1, after 3 weeks; T2, after 6 weeks; T3, after 9 weeks; T4, after 12 weeks; T5, after 15 weeks. *P≥0.05 is non-significant, **P≤0.001 is highly significant
Table 5.
Intergroup comparison of alignment improvement percentage change
| Assessment point | Experimental | Control | P | % change | Times faster |
|---|---|---|---|---|---|
| (T0-T1)/T0 | 48.14±9.10 | 22.59±3.64 | 0.000* | 113.10 | 2.13 |
| (T0-T2)/T0 | 79.93±8.51 | 42.30±8.35 | 0.000* | 88.95 | 1.88 |
| (T0-T3)/T0 | 91.07±3.49 | 64.09±8.1 | 0.000* | 42.09 | 1.42 |
*P≤0.001 is highly significant
Secondary outcome
Intergroup comparison of mean volumetric root resorption showed no statistically significant (P > 0.05) difference between experimental and control group for all the mandibular incisors [Table 6]. Similarly, intergroup comparison showed no statistically significant (P > 0.05) difference in marginal alveolar bone height loss between experimental and control group for all the interested sites [Table 7].
Table 6.
Intergroup comparison of volumetric root resorption
| Tooth number | Experimental group | Control group | P | Mean difference (mm3) (95% CI) | ||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |||
| 42 | 16.87 | 6.368 | 14.67 | 5.851 | 0.333* | 2.2 (−2.278, 6.678) |
| 41 | 16.53 | 6.685 | 14.53 | 7.019 | 0.431* | 2 (−3.127, 7.127) |
| 31 | 16.27 | 6.076 | 15.80 | 6.461 | 0.840* | 0.47 (−4.221, 5.161) |
| 32 | 15.40 | 5.475 | 13.80 | 5.321 | 0.424* | 1.6 (−2.438, 5.638) |
*P≥0.05 is non-significant
Table 7.
Intergroup comparison of marginal bone loss
| Tooth number | Experimental group | Control group | P | Mean difference (mm) (95% CI) | ||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |||
| 43(M) | 0.206 | 0.2763 | 0.093 | 0.0961 | 0.145* | 0.113 (−0.041,0.267) |
| 42(D) | 0.133 | 0.1496 | 0.093 | 0.1438 | 0.461* | 0.04 (−0.069,0.149) |
| 41(M) | 0.040 | 0.1056 | 0.093 | 0.0961 | 0.159* | −0.053 (−0.128,0.022) |
| 31(M) | 0.053 | 0.1060 | 0.020 | 0.1474 | 0.483* | −0.033 (−0.063,0.129) |
| 32(D) | 0.060 | 0.1502 | 0.153 | 0.1506 | 0.100* | −0.093 (−0.205,0.019) |
| 33(M) | 0.147 | 0.2416 | 0.100 | 0.1604 | 0.538* | 0.047 (−0.106,0.200) |
*P≥0.05 is non-significant
Pain was measured using a VAS scale from 0 to 100 mm. There was statistically significant difference seen for the intergroup comparison of the VAS (P < 0.05 P < 0.01) at 12 hours and 24 hours with higher values in experimental group while no significant difference was seen at 4 hours and 3rd day [Figure 7] with no significant difference between males and females. There was statistically no significant difference seen in patient's satisfaction and discomfort level (P > 0.05).
Figure 7.
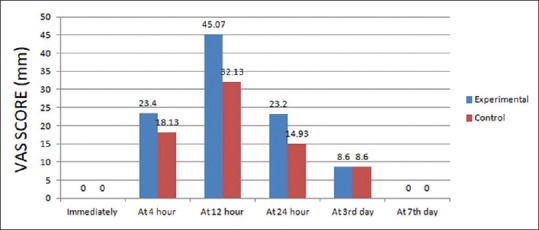
Assessment of VAS scores
Discussion
The present two arm, parallel group designed RCT evaluated the effect of MI-facilitated MOPs on the total time needed for alignment of mandibular anterior teeth of 30 nonextraction mandibular dental arch crowding patients. Half of these 30 patients were aligned performing six transmucosal MOPs interproximally between the six anterior teeth on the labial aspect (experimental group), rest 15 were aligned using conventional orthodontics (control group). The MI-facilitated MOP procedure used in our study is a minimally invasive method that can be done without raising the flap and by using routinely/readily available devices in an orthodontic office i.e., miniscrews and screwdrivers.
In the present study, mandibular crowding has been used as a model for investigating the effectiveness of micro-osteoperforations as dental crowding is the most common type of malocclusion with leveling and alignment of such cases taking upto eight months.[16]
The nonsignificant difference in the baseline demographic and clinical characteristics of the experimental and control group ruled out difference in results because of age, sex, and level of crowding. Equally distributing male and female subjects in the experimental and control group eliminated the effect of gender variability on the rate of tooth movement.[17] Same sequence of the alignment arch wires were used in both the groups to rule out any variability.
Our study found highly significant difference in the total time needed for alignment and the rate of alignment between both the groups. The alignment was 2.13, 1.88, and 1.42 times faster in the experimental group at the 3rd, 6th, and 9th week recall visit. This is in accordance with Teixeira et al.,[4] Alikhani et al.,[5] Tsai et al.,[8] Cheung et al.[6] showing 2.13, 2.3, 1.49, and 1.86 times faster orthodontic tooth movement in MOP assisted experimental group than in the control group, respectively. The treatment time needed for complete alignment of mandibular incisors was reduced by 44% in the MOP group thus clearly indicating that MOPs accelerated the rate of alignment. Similar results have been reported by Teixeira et al.,[4] Alikhani et al.,[5] Tsai et al.[8] showing 53%, 62% and 33% reduction in treatment time in the MOP side as compared to the control side, respectively.
A study by Alkebsi however showed lack of significant increase in the rate of tooth movement which can be explained by the minimal surgical insult of MOP that may not be enough to trigger the inflammatory response to activate the RAP or even cytokine expression.[7] It has been reported that the greater the surgical insults, the greater the rate of the tooth movement triggered by the RAP.[18] A recent study by Cramer et al. concluded that MOPs placed 3 mm away from teeth may produce a slight and temporary increase in tooth movements during the first 2 weeks, but the effects are small, of limited duration, and clinically insignificant and also have limited and transitory effect on bone.[19]
We also found a decrease in the difference in the rate of alignment between both the groups at subsequent visits i.e., the rate decreased from being 2.13 times faster at TI to 1.88 at T2 and 1.42 times at T3. This decrease has been reported and explained in various studies as due to waning effects of the RAP phenomenon with the effects lasting between 5 weeks to six months in various studies.[20] The effect of RAP in our study was however observed even at 9 weeks.
The higher pain values seen in the experimental group as compared to the control group in our study were statistically significant only at 12 and 24 hours and returned to baseline at the end of seventh day with no patient in MOP group reporting the use of any anti-inflammatory medication. The level of satisfaction and ease with the procedure as assessed by the questionnaire was high with the patients willing to repeat the MOP procedure and recommend it to friends.
A major concern associated with accelerated orthodontics is of increased root resorption as the same cytokines that promote RAP also activate cementoclasts, which cause root resorption.[21] However there are few studies evaluating this aspect and the lacunae has been pointed out in the systematic reviews and meta analysis on accelerated orthodontics.[3,22] Root resorption has been assessed in our study by volumetric CBCT evaluation. Results of our study showed no significant difference in root resorption between both the groups. Similar findings have been reported by Cheung et al.[6] and Alkebsi[7] who evaluated the root resorption using micro computed tomography and periapical X-rays, respectively.
The marginal bone levels assessed in our study by CBCT have not been reported in any other previous study on MOPs though concerns have also been raised on the effect of rapid tooth movement on marginal bone levels. In our study the change in the marginal bone height levels did not show any significant difference between the two groups.
No harm was observed in the current research.
Limitations
The difficulty in obtaining the same values for LII and controlling all the variables in the alignment stage, as well as the absence of any standardization regarding the number and site of perforations were some of the limitations of our study.
Conclusions
Following conclusions can be drawn from the present study:-
MI-facilitated MOPs significantly reduced the treatment time needed for complete alignment by 44% as compared to the control group
No increased root resorption or marginal bone height loss occurs with this procedure
Patient acceptability and satisfaction with the procedure is good.
Within the limits of the study, we can conclude that combining MI-facilitated MOP procedure with routine orthodontics can reduce the duration of orthodontic treatment that can be safely incorporated in routine practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wilcko MT, Wilcko WM, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: A synthesis of scientific perspectives. Semin Orthod. 2008;14:305–16. [Google Scholar]
- 2.Roscoe MG, Meira JB, Cattaneo PM. Association of orthodontic force system and root resorption: A systematic review. Am J Orthod Dentofacial Orthop. 2015;147:610–26. doi: 10.1016/j.ajodo.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 3.Hoogveen EJ, Jansama J, Ren Y. Surgically facilitated orthodontic treatment: A systematic review. Am J Orthod Dentofacial Orthop. 2014;145:S51–64. doi: 10.1016/j.ajodo.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira CC, Khoo E, Tran J, Chartres I, Liu Y, Thant LM, et al. Cytokine expression and accelerated tooth movement. J Dent Res. 2010;89:1135–41. doi: 10.1177/0022034510373764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alikhani M, Raptis M, Zoldan B, Sangsuwon C, Lee YB, Alyami B, et al. Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013;144:639–48. doi: 10.1016/j.ajodo.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Cheung T, Park J, Lee D, Kim C, Olson J, Javadi S, et al. Ability of mini-implant-facilitated miro-osteoperforations to accelerate tooth movement in rats. Am J Orthod Dentofacial Orthop. 2016;150:958–67. doi: 10.1016/j.ajodo.2016.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alkebsi A, Al-Maaitah E, Al-Shorman H, Alhaija EA. Three-dimensional assessment of the effect of micro-osteoperforations on the rate of tooth movement during canine retraction in adults with Class II malocclusion: A randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 2018;153:771–85. doi: 10.1016/j.ajodo.2017.11.026. [DOI] [PubMed] [Google Scholar]
- 8.Tsai CY, Yang TK, Hsieh HY, Yang LY. Comparison of the effects of micro-osteoperforation and corticision on the rate of orthodontic tooth movements in rats. Angle Orthod. 2016;86:558–64. doi: 10.2319/052015-343.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee J, Cha J, Park K, Kang Y, Kim S. Effect of flapless osteoperforation-assisted tooth movement on atrophic alveolar ridge: Histomorphometric and gene-enrichment analysis. Angle Orthod. 2018;88:82–90. doi: 10.2319/061217-388.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schultz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibreal O, Hajeer MY, Brad B. Efficacy of piezocision-based flapless corticotomy in the orthodontic correction of severely crowded lower anterior teeth: A randomized controlled trial. Eur J Orthod. 2018 doi: 10.1093/ejo/cjy042. doi: 10.1093/ejo/cjy042. [DOI] [PubMed] [Google Scholar]
- 12.Little RM. The irregularity index: A quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 13.Mehr R. Efficiency of piezotome-corticision assisted orthodontics in alleviating mandibular anterior crowding—A Randomized Controlled Clinical Trial [master's thesis] Storrs, Conn: University of Connecticut; 2013. [DOI] [PubMed] [Google Scholar]
- 14.Li W, Chen F, Zhang F, Ding W, Ye Q, Shi J, et al. Volumetric measurement of root resorption following molar mini-screw implant intrusion using cone beam computed tomography. PLoS One. 2013;8:e60962. doi: 10.1371/journal.pone.0060962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menezes CC, Janson G, Massaro CS, Cambiaghi L, Garib DG. Precision, reproducibility, and accuracy of bone crest level measurements of CBCT cross sections using different resolutions. Angle Orthod. 2016;86:535–42. doi: 10.2319/040115-214.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.AlSayed Hasan MMA, Sultan K, Hamadah O. Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: A randomized controlled clinical trial. Angle Orthod. 2017;87:499–504. doi: 10.2319/062716-503.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haruyama N, Igarashi K, Saeki S, Otsuka-Isoya M, Shinoda H, Mitani H. Estrous cycle-dependent variation in orthodontic tooth movement. J Dent Res. 2002;81:406–10. doi: 10.1177/154405910208100610. [DOI] [PubMed] [Google Scholar]
- 18.Frost HM. The regional acceleratory phenomenon: A review. Henry Ford Hosp Med J. 1983;31:3–9. [PubMed] [Google Scholar]
- 19.Cramer CL, Campbell PM, Opperman LA, Tadlock LP, Buschang PH. Effects of micro-osteoperforations on tooth movement and bone in the beagle maxilla. Am J Orthod Dentofacial Orthop. 2019;155:681–92. doi: 10.1016/j.ajodo.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 20.AlGhamdi A. Corticotomy facilitated orthodontics: Review of a technique. The Saudi Dent J. 2010;22:1–5. doi: 10.1016/j.sdentj.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bartok RI, Vaideanu T, Dimitriu B, Varlan CM, Suciu I, Podoleanu D. External radicular resorption: Selected cases and review of the literature. J Med Life. 2012;5:145–8. [PMC free article] [PubMed] [Google Scholar]
- 22.Gkantidis N, Mistakidis I, Kouskoura T, Pandis N. Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: A systematic review and meta-analysis. J Dentistry. 2014;42:1300–19. doi: 10.1016/j.jdent.2014.07.013. [DOI] [PubMed] [Google Scholar]


