Noise and air pollution as cardiovascular risk factors needing more attention!
“One day man will have to fight the noise as fiercely as cholera and plague” predicted Nobel prize winner Robert Koch in 1910. In fact, the spectrum of diseases has changed significantly in recent decades, so that currently non-communicable, often chronic, diseases such as cardiovascular diseases account for a significant proportion of the global burden of disease. In particular, the successful control of infectious diseases, demographic changes and changing lifestyles in Western societies are responsible for the shift in the burden of disease. Although research efforts in recent years have focused primarily on traditional risk factors such as arterial hypertension, smoking, hypercholesterolaemia, and diabetes mellitus—more and more studies point to a high impact of environmental factors such as noise and air pollution on the development of cardiovascular disease.
Epidemiological studies have shown that exposure to traffic noise is associated with increased cardiovascular morbidity and mortality (for review, see refs1,2). The World Health Organization (WHO) estimates that in Western Europe annually 61 000 healthy years of life are lost due to noise-induced cardiovascular disease, 45 000 healthy years due to noise-induced cognitive impairment in children, 903 000 healthy years due to noise-induced sleep disorders, 22 000 healthy years due to tinnitus, and 654 000 healthy years due to noise-induced annoyance.3 In total, there is annually a loss of more than one million healthy life years in Western Europe, measured on the basis of disability-adjusted life years, due to traffic noise-induced diseases.
Using new hazard ratio functions combined with ambient air pollution exposure data to estimate the impacts in Europe and the 28 countries of the European Union (EU-28), we recently demonstrated that the annual excess mortality rate from ambient air pollution (due to PM2.5 µm) in Europe is 790 000 and 659 000 in the EU-28.4 Importantly, between 40% and 80% are due to cardiovascular events, which clearly dominate health outcomes.4 These estimates substantially exceed recent analyses, such as the Global Burden of Disease for 2017,5 by more than a factor of two. Thus, the conclusion is that air pollution reduces the mean life expectancy in Europe by about 2.2 years with an annual, attributable per capita mortality rate in Europe of 133/100 000 per year.
What are the mechanisms by which noise and air pollution can cause cardiovascular disease?
In recent years, noise and air pollution research has made substantial progress, particularly with regard to relevant clinical studies as well as pathophysiological mechanisms that may play an important role in noise and air pollution-induced cardiovascular effects. There are only few studies that provide mechanistic insight into the relationship between noise exposure and increased cardiovascular risk. In 2011, we started to tackle this problem by combining it with sophisticated methodologies to measure vascular function such as flow-mediated dilation in subjects exposed to noise.
In a field study (exposure to noise at home and not in sleep laboratories) we established that simulated night-time aircraft noise (MP3 player; 30 and 60 flights/night, peak sound level of 60 dB (A), mean sound level of 43 and 46 dB (A), respectively) is associated with worsening of vascular (endothelial) function (measured by flow-mediated dilation), increased stress hormone levels (epinephrine), and decreased sleep quality.6,7 Importantly, in a small subgroup of subjects endothelial dysfunction was reversed by prior administration of the antioxidant vitamin C (2 g po) suggesting that increased oxidative stress was at least in part responsible for aircraft noise-induced impairment of endothelial function.6 Two recent animal studies could further reveal relevant molecular mechanisms by which aircraft noise induces vascular dysfunction.8,9 Hereby, we demonstrated that simulated aircraft noise exposure for 4 days led to a significant increase in stress hormone levels, increased blood pressure, changes in vascular wall gene expression, and impaired vascular function, mainly due to increased free radical formation and oxidative stress. With these studies, two important enzymes were identified as being involved in the initiation of aircraft noise-induced vascular dysfunction: the nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase; phagocytic form or NOX-2) and the nitric oxide synthase (NOS).8,9 The noise-induced dysregulation of these enzymes enhanced the formation of reactive oxygen species, which directly led to decreased vascular bioavailability of nitric oxide (NO), an important radical with powerful vasodilator and anti-atherosclerotic properties and thus resulted in the impairment of endothelial function. Mainly aircraft noise applied during the sleeping phase of the animals reduced the expression of genes responsible in the regulation of the circadian clock, reduced the expression of neuronal NOS, an enzyme responsible for memory and learning, and also uncoupled the enzyme along with an increase in cerebral NOX-2 expression.8 In Nox2 knockout mice aircraft noise was not able to increase blood pressure and to cause damage to the vasculature and the brain.8
The activation of oxidative stress pathways also plays a crucial role in causing vascular (endothelial) dysfunction caused by air pollution constituents. Thus, increased production of vascular reactive oxygen species and evidence for increased vascular inflammation have been demonstrated in response to diesel exhaust, wood smoke, fine (PM2.5), or ultrafine particulate matter exposure (0.1 µm) (for review, see refs10,11). Experimental research has also established an activation of central nerve system reflex arcs further enhancing systemic inflammation. Enzymatic sources being responsible for increased oxidative stress within the vasculature include an uncoupled endothelial NOS and an activation of the phagocytic NADPH oxidase (NOX-2; for review, see ref.11). Interestingly, for subsequent development of insulin resistance, adiposity, and inflammation in response to PM 2.5 µm reactive oxygen species generation by NADPH oxidase appears to mediate this risk.10
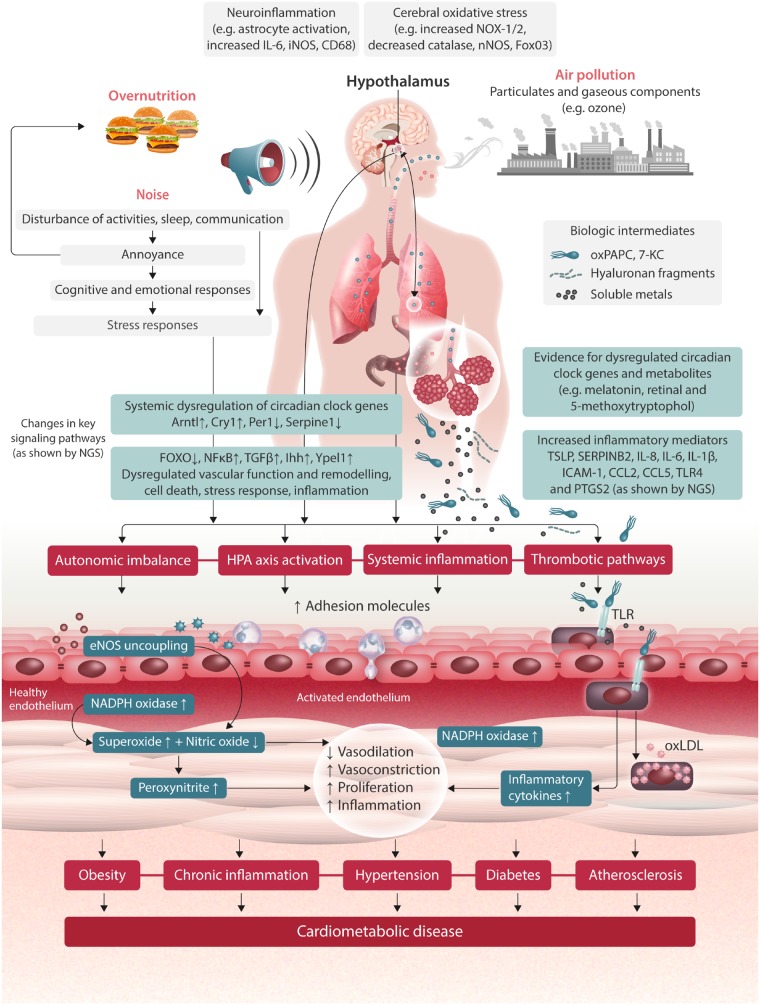
The important aspect of all these studies is that environmental stressors such as noise and air pollution are damaging the cardiovascular system probably by similar mechanisms. Noise and air pollution constituents induce endothelial dysfunction due to increased oxidative stress. Both stressors have also been shown to cause and/or to be associated with or even to potentiate the cardiovascular side effects of traditional risk factors such as hypertension, smoking, hyperlipidaemia, and diabetes, thereby further stimulating and/or accelerating the atherosclerotic process (Figure 1).
Figure 1.
Proposed pathophysiological mechanisms of cardiovascular disease induced by environmental air pollution and/or noise. Modified from Munzel et al.12
Tasks for future research addressing environmental stressors
Taken together, there is an urgent need to study the cardiovascular consequences of simultaneous noise and air pollution exposure in experimental animal models and in men. To my knowledge, no studies have addressed so far this topic yet and there are numerous questions to be answered—in particular whether there are additive or even potentiating harmful adverse effects of these environmental stressors on the cardiovascular system. Specifically, we need to address the effects of co-exposure on haemodynamics such as blood pressure and heart rate, vascular (endothelial) function, oxidative stress pathways, and the impact of both stressors on the circadian rhythm (Figure 1). We have to invest more research into the topics of mitigation, prevention and the impact of lifestyle changes such as exercise and diet on cardiometabolic diseases caused by such stressors. We have to convince policy makers that both air pollution and noise represent important cardiovascular risk factors that can be significantly influenced not by doctors or the patient, but rather by politicians lowering noise and air pollution limits to levels where almost no cardiovascular side effects are to be expected.
Acknowledgement
The author would like to thank Margot Neuser for graphical assistance. Thomas Münzel is PI of the DZHK (German Center for Cardiovascular Research), Partner Site Rhine-Main, Mainz, Germany.
Conflict of interest: none declared.
Author

Biography: Thomas Münzel MD, is Chief of the Department of Cardiology at the University Medical Center, Johannes Gutenberg University Mainz, Germany. He is an interventionist and also a vascular biologist and got his post doc training as a vascular biologist at the Institute of Applied Physiology, Professor Eberhard Bassenge, Albert Ludwigs University Freiburg and in the Laboratories of David G Harrison, Emory University, Atlanta, GA, USA with focus on endothelial function and oxidative stress. He is co-initiator of the Gutenberg Health Study, one of the largest prospective cohort trials worldwide and was the founding director of the Center for Thrombosis and Hemostasis, CTH in Mainz. Since 2011, his research group is focusing on environmental risk factors for cardiovascular disease with a focus on aircraft noise and air pollution.
References
- 1. Munzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sorensen M.. Environmental noise and the cardiovascular system. J Am Coll Cardiol 2018;71:688–697. [DOI] [PubMed] [Google Scholar]
- 2. Munzel T, Sorensen M, Schmidt F, Schmidt E, Steven S, Kroller-Schon S, Daiber A.. The adverse effects of environmental noise exposure on oxidative stress and cardiovascular risk. Antioxid Redox Signal 2018;28:873–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burden of Disease from Environmental Noise—Quantification of Healthy Life Years Lost in Europe. Copenhagen: World Health Organization. Regional office for Europe; 2011. [Google Scholar]
- 4. Lelieveld J, Klingmuller K, Pozzer A, Poschl U, Fnais M, Daiber A, Munzel T.. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J 2019;40:1590–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA 3rd, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH.. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017;389:1907–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schmidt FP, Basner M, Kroger G, Weck S, Schnorbus B, Muttray A, Sariyar M, Binder H, Gori T, Warnholtz A, Munzel T.. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J 2013;34:3508–3514a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, Binder H, Gori T, Munzel T.. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol 2015;104:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kroller-Schon S, Daiber A, Steven S, Oelze M, Frenis K, Kalinovic S, Heimann A, Schmidt FP, Pinto A, Kvandova M, Vujacic-Mirski K, Filippou K, Dudek M, Bosmann M, Klein M, Bopp T, Hahad O, Wild PS, Frauenknecht K, Methner A, Schmidt ER, Rapp S, Mollnau H, Munzel T.. Crucial role for Nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur Heart J 2018;39:3528–3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Munzel T, Daiber A, Steven S, Tran LP, Ullmann E, Kossmann S, Schmidt FP, Oelze M, Xia N, Li H, Pinto A, Wild P, Pies K, Schmidt ER, Rapp S, Kroller SS.. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J 2017;38:2838–2849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rajagopalan S, Al-Kindi SG, Brook RD.. Air pollution and cardiovascular disease: JACC State-of-the-Art review. J Am Coll Cardiol 2018;72:2054–2070. [DOI] [PubMed] [Google Scholar]
- 11. Munzel T, Gori T, Al-Kindi S, Deanfield J, Lelieveld J, Daiber A, Rajagopalan S.. Effects of gaseous and solid constituents of air pollution on endothelial function. Eur Heart J 2018;39:3543–3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook FR, Chen LC, Brook RD, Rajagopalan S.. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J 2017;38:557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]