Abstract
Objective:
To investigate the clinical differences between intermittent explosive disorder (IED) (disorder of aggression primarily directed towards others) and nonsuicidal self-injury (NSSI) (disorder of aggression predominantly directed towards the self) in order to better understand the different clinical subtypes of aggression.
Methods:
We used treatment-seeking samples to compare demographic and clinical correlates between 82 participants with IED and 55 participants with NSSI.
Results:
The IED group was older, more likely to be male, in a relationship, and employed than the NSSI group. With respect to clinical variables, the NSSI group had more severe depressive symptoms and more social adjustment difficulties. Regarding psychiatric co-morbidities, the IED group had higher rates of generalized anxiety disorder. On the other hand, the NSSI group had higher rates of major depressive disorder, agoraphobia, substance use disorder, and bulimia nervosa.
Conclusions:
Individuals with NSSI may benefit from better management of psychiatric comorbidities, specifically depressive symptoms and social adjustment difficulties. Conversely, the treatment of individuals with IED may be improved by targeting comorbid generalized anxiety disorder. Our results provide important insight for the development of tailored interventions for specific subtypes of aggression.
Keywords: Aggression, intermittent explosive disorder, nonsuicidal self-injury
Introduction
Pathological aggression is associated with substantial physical, psychological, and economical burden.1-4 Despite its negative impacts on society and its potential to cause intrapersonal and interpersonal harm, aggression has only recently been empirically investigated in the field of psychiatry and clinical psychology. Nevertheless, mental health intervention may benefit a number of mental disorders linked to aggression.4 Unfortunately, due to gaps in the empirical literature, individuals with aggressive behavior are not being effectively treated. Specifically, there is a lack of understanding on the different subtypes of aggression, and resolving this lack of understanding may help develop tailored interventions.
The present study classified aggression based on the target of the aggressive behavior: aggression directed towards others vs. aggression directed towards the self.2 Intermittent explosive disorder (IED) is considered a hallmark diagnosis of aggression directed towards others3,5 with 89% of individuals showing aggression against other people and the remaining 11% against property.6 The lifetime prevalence of IED has been estimated to be 6.9% in the United States and 3% in studies outside of the United States.3 To the best of our knowledge, no national studies have been conducted in Brazil. However, studies have estimated the lifetime prevalence in the city of São Paulo, Brazil, at 4.9%.7 The high rate of IED in the general population suggests that aggression directed towards others may be an important public health issue and warrants greater empirical investigation.3,6,8 Another way that people manifest aggression is self-injurious behavior.2 One of the most common means of aggression directed towards the self is nonsuicidal self-injury (NSSI).9 In NSSI individuals do not intend to commit suicide, but to cause physical harm to themselves.9,10 Self-injurious behavior is often an attempt to obtain relief from negative feelings or thoughts.9,10 NSSI is a common and significant problem.9-11 A systematic review of data from Asia, North America, Oceania, and Europe estimated the lifetime prevalence of NSSI between 5.5 and 17.2%.12 Although suicide is not the goal of NSSI, previous evidence has suggested that NSSI is a predictor of future suicide attempts and completed suicide.11 Frequent forms of self-injury include cutting, scratching, burning, hitting, and scraping.9,10 Thus, NSSI may be a good representation of the subtype of aggression directed towards the self.
In the present study, we propose that comparing clinical correlates between IED (aggression disorder primarily directed towards others) and NSSI (disorder of aggression predominantly directed towards the self) may provide a better understanding of the different subtypes of aggression. In support of this supposition, the available evidence suggests that IED and NSSI have different demographic and clinical profiles. IED appears to predominantly affect males6 while NSSI tends to be more prevalent in women.10 Individuals with IED tend to have higher rates of other externalizing and impulse-control disorders,6 whereas individuals with NSSI appear to have elevated rates of mood disorders.12 While the limited empirical literature provides preliminary evidence of the potential differences between IED and NSSI, no direct investigation of the similarities and differences between IED and NSSI has been conducted. This is a gap in the literature since previous clinical trials have suggested that tailored treatments for specific subtypes of aggressive behaviors may increase treatment efficacy.13,14 For example, IED-focused cognitive-behavioral psychotherapy that specifically targets cognitive distortions and automatic thoughts related to IED, such as interpreting neutral stimuli as threats, as well as assertiveness training, appears to improve outcomes. Unfortunately, tailored treatments for IED are scarce.13,14 Furthermore, tailored interventions targeting self-aggression (i.e., NSSI) are rare15,16 and are usually based on treatments for other disorders, including dialectic behavioral therapy, which was developed to treat borderline personality disorder.15
In light of these issues, the objective of the present study was to directly investigate the clinical differences between individuals whose aggression is predominantly directed towards others (IED) and individuals whose aggression is primarily directed towards the self (NSSI). To this end, we compared demographics and clinical variables between the two groups. The results of the present study may provide further insight into the differences between IED and NSSI and may aid in the development of tailored interventions based on subtypes of aggression.
Methods
Participants
The sample consisted of 137 consecutive treatment-seeking patients from the Programa Ambulatorial Integrado dos Transtornos do Impulso (PRO-AMITI), Instituto de Psiquiatria, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, Brazil, between 2007 and 2013. Recruitment took place during the initial intake interview at PRO-AMITI. During the intake process, patients were informed about the potential study and were invited to participate. They were clearly informed that treatment was not based on participation in the study. Patients who agreed to participate then completed the measures of interest and underwent a semi-structured clinical interview.
The inclusion criteria were as follows: i) a primary diagnosis of IED or NSSI; ii) formal education of at least 5 years; and (iii) age 18 years or older. IED or NSSI were diagnosed through semi-structured clinical interviews by registered and research-trained psychologists and psychiatrists. We used the DSM-IV Structured Clinical Interview (SCID)17 adapted for impulse-control disorders. Since NSSI is not an official diagnosis in the DSM-IV, the criteria were adapted from the Functional Assessment of Self-Mutilation (FASM).18 A similar approach has been used in previous studies on other impulse-control disorders without official DSM-IV criteria.19,20 We excluded individuals: i) who had both IED and NSSI; ii) presented with psychotic symptoms; iii) required emergency care; or iv) refused to participate in the study. Three individuals met the diagnostic criteria for both IED and NSSI. Due to the small sample size, we were unable to conduct robust statistical analyses in individuals with both disorders, and thus they were excluded from the final analyses.
Measures
Demographics
We assessed the sample for age (in years), gender, ethnicity, marital status, educational level (in years of formal education), and professional status.
Clinical variables
The 75-item Buss-Durkee Hostility Inventory was used to evaluate aggressive/hostile behavior. The self-report questionnaire is divided in eight sub-factors: assault (10 items), irritability (11 items), indirect hostility (nine items), resentment (eight items), negativism (five items), guilt (nine items), suspicion (10 items), and verbal hostility (13 items). In addition to subscale scores, the factors can be summed to provide a total score.21 The Buss-Durkee Hostility Inventory has demonstrated good internal consistency (Cronbach’s alpha between 0.72 and 0.79), test-retest reliability (stability coefficients between .64 and .82), and convergent validity (correlation coefficients between 0.40 and 0.70 for measurements of aggression/hostility/anger).21
Impulsivity was investigated with the widely-used Barratt Impulsiveness Scale (BIS-11).22 This self-report questionnaire assesses three components of impulsivity: 1) motor; 2) attentional; and 3) lack of planning.22 The BIS-11 has high internal consistency (Cronbach’s alpha between 0.79 and 0.82).22 The scale was translated to Brazilian Portuguese by Malloy-Diniz et al.23 and the translated version showed satisfactory psychometric properties, including high correlations with the English version.
Impairments in social adjustment was assessed using the Social Adjustment Scale (self-report), a 42-item inventory that evaluates participants’ adjustment in seven areas: work, social and leisure activities, relationship with extended family, marital role, parental role, membership in the family unit, and economic situation.24 Each item is scored on a 5-point scale in which higher scores indicate greater impairment (1 = normal functioning; 5 = severe maladjustment).24 The Social Adjustment Scale was validated for Brazilian Portuguese by Gorenstein et al.25 The translated version could discriminate between psychiatric patients and individuals without mental disorders, and has been shown to be useful in outcome studies.
Depressive symptoms were assessed using the Beck Depression Inventory (BDI). This self-report instrument consists of 21 items evaluating depressive symptoms in the last 7 days and is one of the most widely used self-report measures of depression.26 The total score ranges from 0 to 63, with higher scores indicating more severe depressive symptoms.26 It was adapted to Brazilian Portuguese and validated by Gorenstein & Andrade.27
Current prevalence of psychiatric comorbidities was assessed with the Mini International Neuropsychiatric Interview (MINI), a widely-used brief semi-structured interview that assess psychiatric disorders using DSM-IV criteria.28 The MINI has demonstrated reliable diagnoses compared to the Composite International Diagnostic Interview,28 and the Brazilian Portuguese of the MINI has also demonstrated satisfactory reliability.29,30
Statistical analysis
The two groups (IED and NSSI) were compared on demographic characteristics, clinical variables, and psychiatric comorbidities. Categorical variables were evaluated using chi-square tests. Fisher’s exact test was used when cell counts were less than five. Student’s t-tests were used for normally distributed continuous variables, and Mann-Whitney’s U-tests were used for non-normally distributed continuous variables.
Ethics
This study was approved by the ethics committee of Hospital das Clínicas, Universidade de São Paulo. Written informed consent was obtained from all participants. The study protocol followed Declaration of Helsinki guidelines for human experiments.
Results
In terms of demographic characteristics, the IED group was older, more likely to be male, in a relationship, and employed (Table 1).
Table 1. Demographic characteristics of participants with IED and NSSI (N=137).
| Participants with IED (n=82) | Participants with NSSI (n=55) | |||||||
|---|---|---|---|---|---|---|---|---|
| Clinical variables | n (%) | Mean (SD) | Median | n (%) | Mean (SD) | Median | Test | p |
| Age | 42.2 (12.1) | 41.0 | 28.2 (9.5) | 27.0 | U = 736.5 | < 0.001 | ||
| Gender | ||||||||
| Male | 67 (81.7) | 8 (14.5) | U = 918.5 | < 0.001 | ||||
| Female | 15 (18.3) | 9.4 (1.6) | 10.0 | 47 (85.5) | 8.1 (2.2) | 8.0 | U = 1.063.5 | |
| Ethnicity | χ2 = 1.308 | 0.253 | ||||||
| Caucasian | 56 (68.3) | 41 (77.4) | ||||||
| Non-Caucasian | 26 (31.7) | 12 (22.6) | ||||||
| Marital status | χ2 = 16.669 | < 0.001 | ||||||
| With partner | 49 (60.5) | 13 (24.5) | ||||||
| Without partner | 32 (39.5) | 40 (75.5) | ||||||
| Years of education | 14.4 (3.7) | 15.0 | 13.2 (3.5) | 13.0 | U = 1.615.0 | 0.059 | ||
| Professional status | χ2 = 13.245 | < 0.001 | ||||||
| Working and/or studying | 62 (76.5) | 21 (44.7) | ||||||
| Unemployed | 19 (23.5) | 26 (55.3) | ||||||
χ2 = chi-square; IED = intermittent explosive disorder; NSSI = nonsuicidal self-injury; SD = standard deviation; U = Mann-Whitney U.
The entire sample (N=137) was assessed for age and gender. The number of participants investigated for the other demographics were ethnicity (n=135), marital status (n=134), years of education (n=131) and professional status (n=128).
Bold font indicates statistical significance (p < 0.05).
Regarding the clinical variables, the IED group scored higher on the Buss-Durkee Hostility Inventory than the NSSI group. Not surprisingly, individuals with IED reported higher levels of aggression directed towards others, such as verbal hostility and assault. Conversely, the NSSI group had more severe depressive symptoms, higher BIS total scores, as well as greater social adjustment difficulties. Regarding co-occurring psychiatric disorders, the IED group had higher rates of generalized anxiety disorder (GAD). On the other hand, the NSSI group had higher rates of major depressive disorder (MDD), agoraphobia, substance use disorder, and bulimia nervosa (Table 2).
Table 2. Clinical comparison between participants with IED and NSSI (N=137).
| Participants with IED (n=82) | Participants with NSSI (n=55) | |||||||
|---|---|---|---|---|---|---|---|---|
| Clinical variables | n (%) | Mean (SD) | Median | n (%) | Mean (SD) | Median | Test* | p |
| BDHI | ||||||||
| Verbal hostility | 10.1 (2.1) | 10.0 | 7.7 (3.4) | 8.0 | U = 944.0 | < 0.001 | ||
| Assault | 6.3 (1.6) | 7.0 | 4.5 (2.3) | 4.0 | U = 918.5 | < 0.001 | ||
| Irritability | 9.4 (1.6) | 10.0 | 8.1 (2.2) | 8.0 | U = 1,063.5 | 0.001 | ||
| Negativism | 3.4 (1.3) | 4.0 | 2.6 (1.5) | 3.0 | U = 1,178.0 | 0.007 | ||
| Resentment | 5.5 (1.8) | 6.0 | 5.8 (1.8) | 6.0 | U = 1,491.5 | 0.362 | ||
| Guilt | 6.8 (1.8) | 7.0 | 6.8 (2.2) | 7.0 | U = 1,605.0 | 0.779 | ||
| Suspicion | 6.7 (2.1) | 7.0 | 6.3 (2.2) | 6.0 | U = 1,493.0 | 0.369 | ||
| Indirect hostility | 6.4 (1.3) | 7.0 | 5.6 (1.9) | 6.0 | U = 1,250.5 | 0.023 | ||
| Total score | 54.6 (8.1) | 56.0 | 47.5 (11.0) | 50.0 | U = 1,027.5 | 0.001 | ||
| BIS total score | 72.7 (11.2) | 71.0 | 79.4 (11.8) | 80.0 | t = -3.218 | 0.002 | ||
| SAS total score | 2.3 (0.5) | 2.3 | 2.8 (0.6) | 2.7 | t = -4.306 | < 0.001 | ||
| BDI total score | 19.1 (9.8) | 19.0 | 29.1 (12.8) | 33.0 | t = -5.052 | < 0.001 | ||
| MINI | ||||||||
| Any psychiatric co-morbidity | 58 (80.6) | 31 (88.6) | Fisher’s | 0.412 | ||||
| Number of psychiatric co-morbidities | 2.1 (2.1) | 1.0 | 2.4 (1.7) | 2.0 | U = 1,017.5 | 0.100 | ||
| Major depressive disorder | 28 (37.3) | 28 (71.8) | χ2 = 16.906 | < 0.001 | ||||
| Bipolar disorder | 20 (26.3) | 4 (10.3) | Fisher’s | 0.054 | ||||
| Dysthymia | 9 (12.0) | 4 (10.5) | Fisher’s | 1.000 | ||||
| Generalized anxiety disorder | 38 (50.7) | 7 (17.9) | χ2 = 11.406 | 0.001 | ||||
| Agoraphobia | 14 (18.4) | 14 (35.9) | χ2 = 4.274 | 0.039 | ||||
| Social phobia | 11 (14.5) | 10 (25.6) | χ2 = 2.153 | 0.142 | ||||
| Panic disorder | 9 (11.8) | 8 (20.5) | χ2 = 1.538 | 0.215 | ||||
| Obsessive-compulsive disorder | 7 (9.2) | 4 (10.3) | Fisher’s | 1.000 | ||||
| Post-traumatic stress disorder | 2 (2.6) | 4 (10.8) | Fisher’s | 0.089 | ||||
| Alcohol use disorder | 14 (18.4) | 4 (10.5) | Fisher’s | 0.414 | ||||
| Substance use disorder | 5 (6.7) | 8 (21.1) | Fisher’s | 0.031 | ||||
| Bulimia nervosa | 1 (1.3) | 4 (10.5) | Fisher’s | 0.043 | ||||
| Anorexia nervosa | 0 (0.0) | 1 (2.7) | Fisher’s | 0.330 | ||||
χ2 = chi-square; BDHI = Buss-Durkee Hostility Inventory; BDI = Beck Depression Inventory; BIS = Barratt Impulsiveness Scale; IED = intermittent explosive disorder; IED = intermittent explosive disorder; MINI = Mini-International Neuropsychiatric Interview; NSSI = nonsuicidal self-injury; NSSI = nonsuicidal self-injury; SAS = Social Adjustment Scale; SD = standard deviation; U = Mann-Whitney U.
Total individuals assessed for the clinical variables: BDHI, n=120; BIS, n=130; SAS Self-Report, n=125; BDI, n=130; and MINI, n=114.
Bold font indicates statistical significance (p < 0.05).
Fisher’s exact test was used when expected cell counts were less than 5.
Discussion
The present study is, to our knowledge, the first to directly investigate the clinical differences between individuals with aggressive behavior primarily directed towards others (IED) and individuals with aggressive behavior primarily directed towards the self (NSSI). Several differences were found between the two subtypes of aggression, and some of our findings could have potential treatment implications. First, there were significant demographic differences between the groups. Second, the NSSI group had higher rates of psychiatric co-morbidities, including severe depressive symptoms and higher rates of MDD than the IED group. Third, the NSSI group reported poorer social adjustment than the IED group. Finally, the IED group had a higher prevalence of GAD than the NSSI group. These findings may provide insight for the development of tailored interventions for different subtypes of aggressive behavior (i.e., aggression directed towards others vs. aggression directed towards the self).
Differences in demographic characteristics
We found that individuals in the IED group were older and more likely to be male than those in the NSSI group. This age difference might be a result of discrepancies in the duration of the two disorders. The age of onset for NSSI is around 16 years. However, at age 20, half of the individuals tend to remit from self-injurious behaviors.31 The onset of IED is also during adolescence, with a mean age of onset between 14.0 and 16.2.6,32 In contrast to NSSI, however, IED persists longer.6,33 Kessler et al.6 observed a mean duration of approximately 12 years for IED. In addition, IED may be considered a more ego-syntonic disorder,32 and thus individuals with IED may seek treatment later, which may account for the age difference between the groups in our study.
In terms of gender differences, our findings are consistent with previous studies in that males tend to present more aggression directed towards others than females.34 Male aggression towards others may be rooted in evolutionary traits related to fighting, survival and reproduction.34 In addition, testosterone has been found to decrease the amygdala-prefrontal coupling, which may affect emotional processing in males and tend to increase aggression directed towards others.35
Our findings also suggest that there is a need to reduce the time between IED onset and treatment seeking. Corroborating this, our results indicate that although IED onset is in adolescence,6,32 individuals seek treatment only in their early forties. Increased awareness that there is treatment for aggressive behavior may increase treatment-seeking behavior and reduce the negative consequences of aggression directed towards others.
Depressive symptoms and rates of major depressive disorder (MDD)
We found more severe depressive symptoms (measured by the BDI) and a higher prevalence of MDD in individuals with NSSI than IED. Although, individuals with IED have higher rates of MDD than the general population,6,9,36 MDD prevalence in the IED group was less than half that of the NSSI group. In addition, MDD was not only more frequent, but also more severe in individuals with NSSI. Depressed participants with NSSI had a mean BDI score of 29.9 (standard deviation [SD] = 11.8), while depressed participants with IED had an average score of 21.1 (SD = 10.2), p < 0.001. These results suggest that depression may be a particularly important co-morbidity in individuals with NSSI. This finding converges with the literature, which reports an association between NSSI and negative emotions, specifically that self-injurious behavior may briefly attenuate negative affect.9,10 Thus, it is plausible that individuals engage in NSSI to cope with their depression. As such, it may be important to manage depression symptoms to reduce self-injurious behavior. To this end, pharmacological and psychotherapeutic interventions focused on depressive manifestations might facilitate NSSI treatment. Moreover, the development of coping skills to deal with depressive symptoms in a more adaptable manner may be particularly useful.
Social adjustment
In the present study, the NSSI group reported poorer social adjustment than the IED group. There are several potential explanations for this finding. One possibility is that individuals with poorer social adjustment are more vulnerable to developing self-injurious behavior. Another possibility is that NSSI causes more negative consequences in global functioning and adjustment than IED. It is also possible that self-aggression further deteriorates the social adjustment of individuals with NSSI (i.e., a combination of the two factors). Corroborating these findings, previous studies have found that interpersonal difficulties may be a core component of social adjustment and functionality problems in NSSI.9,37 Therefore, therapeutic interventions focused on improving problem-solving strategies and interpersonal skills may be particularly helpful. Furthermore, peer-support and group psychotherapy may create a supportive environment in which individuals can share common concerns such as stigma and interpersonal difficulties.38
Prevalence of generalized anxiety disorder (GAD)
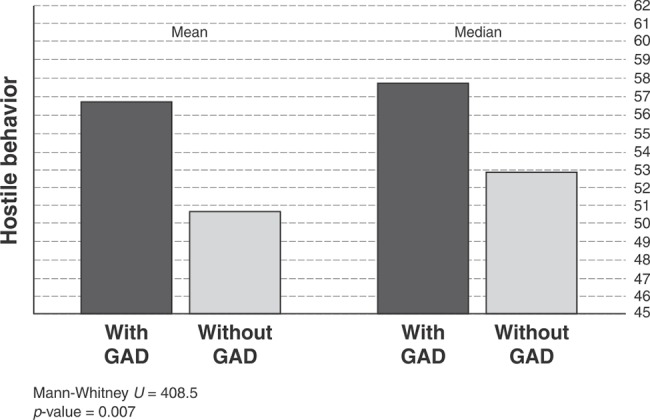
The IED group had a higher prevalence of GAD than the NSSI group. Previous studies have suggested that GAD is the most strongly associated psychiatric comorbidity with IED.6 One potential reason for the association between IED and GAD could be that the two disorders share similar clinical and neurobiological aspects, including: a hyper-active amygdala,38,39 overstimulation of the adrenergic system, irritability, racing thoughts,2,3,9 and an association with the fight-or-flight response.39 In the present study, individuals with comorbid IED and GAD had higher mean and median hostility scores than individuals who had IED without comorbid GAD (Figure 1). Conversely, anxiety symptoms in NSSI appear to have a different clinical and neurobiological basis in that they appear to be more self-directed, internalizing and associated with self-criticism.36 According to Thompson & Zuroff,40 self-criticism is associated with low self-esteem, neuroticism and an avoidant conflict management style. Neuroimaging studies have also suggested that self-criticizing anxiety may be associated with increased activity in the dorsal anterior cingulate and the lateral prefrontal cortex.41
Figure 1. Level of hostile behavior (measured by Buss-Durkee Hostility Inventory) in participants with intermittent explosive disorder with and without co-occurring generalized anxiety disorder (GAD) (n=72 [sample sizes with GAD = 36; without GAD = 36]). There were no demographic differences between subjects with and without GAD.
Our study suggests that comorbid GAD appears to increase the severity of aggression directed toward others. Some treatments that may address IED and GAD simultaneously include selective serotonin reuptake inhibitors, exercise, communication skills to improve interpersonal relationships, and managing alcohol/substance use disorders.4,42,43
Limitations
Our study should be interpreted in light of its limitations. First, it did not include healthy controls and, thus, we could not compare individuals with IED and NSSI to individuals without these clinical disorders. Nevertheless, our main goal was to investigate the clinical differences between aggression directed towards others and aggression directed towards the self. Despite the absence of healthy controls, our findings provide important insight into the different subtypes of aggression. Second, since our sample consisted of treatment-seeking participants, it may not be representative of the general population, and caution is needed when generalizing our results. That said, participants were recruited in a typical treatment setting and, thus, our findings could have high clinical utility. Third, we excluded individuals with both IED + NSSI due to the small sample size (n=3). Examining differences between individuals with IED, or NSSI and both IED + NSSI would be informative and a potential avenue for future research. Finally, it was beyond the scope of the paper to examine variables that mediate/moderate the effects between our variables of interest. However, such research would be highly informative and provide more insight into the relationship between pathological aggression (others, self) and its clinical characteristics.
Conclusions
The present study found several clinical differences between individuals with aggression predominantly directed towards others (IED) and individuals with aggression primarily directed towards the self (NSSI). Our results may provide important insight for the development of tailored interventions for specific subtypes of aggression. For example, individuals with NSSI may particularly benefit from a better management of depressive symptoms and difficulties in social adjustment. On the other hand, treatments for individuals with IED may wish to target comorbid GAD in conjunction with the aggressive behavior. Indeed, such tailored interventions may help increase treatment efficacy for different subtypes of aggression.
Disclosure
EFC is a member of the Scientific Advisory Board of Azevan Pharmaceuticals, Inc. HT receives compensation from the Caixa Econômica Federal to develop responsible gambling interventions. The other authors report no conflicts of interest.
Footnotes
How to cite this article: Medeiros GC, Seger-Jacob L, Garreto AK, Kim HS, Coccaro EF, Tavares H. Aggression directed towards others vs. aggression directed towards the self: clinical differences between intermittent explosive disorder and nonsuicidal self-injury. Braz J Psychiatry. 2019;41:303-309. http://dx.doi.org/10.1590/1516-4446-2018-0149
References
- 1.World Health Organization (WHO) 2002. The world health report 2002: reducing risks, promoting healthy life [Internet]http://www.who.int/whr/2002/en/ [cited 2018 Aug 29]. [Google Scholar]
- 2.Siever LJ. Neurobiology of aggression and violence. Am J Psychiatry. 2008;165:429–42. doi: 10.1176/appi.ajp.2008.07111774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coccaro EF. Intermittent explosive disorder as a disorder of impulsive aggression for DSM-5. Am J Psychiatry. 2012;169:577–88. doi: 10.1176/appi.ajp.2012.11081259. [DOI] [PubMed] [Google Scholar]
- 4.Medeiros GC, Leppink E, Seger L, Costa AM, Bernardo C, Tavares H. Impulsive aggression in Brazil: losing opportunities to intervene. Rev Bras Psiquiatr. 2015;37:177–8. doi: 10.1590/1516-4446-2014-1609. [DOI] [PubMed] [Google Scholar]
- 5.Grant JE, Atmaca M, Fineberg NA, Fontenelle LF, Matsunaga H, Janardhan Reddy YC, et al. Impulse control disorders and “behavioural addictions” in the ICD‐11. World Psychiatry. 2014;13:125–7. doi: 10.1002/wps.20115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Coccaro EF, Fava M, Jaeger S, Jin R, Walters E. The prevalence and correlates of DSM-IV intermittent explosive disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2006;63:669–78. doi: 10.1001/archpsyc.63.6.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viana MC, Andrade LH. Lifetime prevalence, age and gender distribution and age-of-onset of psychiatric disorders in the São Paulo metropolitan area, Brazil: results from the São Paulo megacity mental health survey. Rev Bras Psiquiatr. 2012;34:249–60. doi: 10.1016/j.rbp.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Seger L, Costa AM, Bernardo CF, Morillo J, Santos ND, Medeiros GC. Transtorno explosivo intermitente In: In: Tavares H, Abreu CN, Seger L, Mariani MMC, Filomensky TZF, editores, editors. Psiquiatria, saúde mental e a clínica da impulsividade. São Paulo: Manole; 2015. pp. p87–102. [Google Scholar]
- 9.American Psychiatric Association. Arlington: American Psychiatric Publishing; 2013. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [Google Scholar]
- 10.In-Albon T, Ruf C, Schmid M. Proposed diagnostic criteria for the DSM-5 of nonsuicidal self-injury in female adolescents: diagnostic and clinical correlates. Psychiatry J. 2013;2013:159208. doi: 10.1155/2013/159208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilkinson P. Non-suicidal self-injury. Eur Child Adolesc Psychiatry. 2013;22:S75–9. doi: 10.1007/s00787-012-0365-7. [DOI] [PubMed] [Google Scholar]
- 12.Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self‐injury in nonclinical samples: systematic review, meta‐analysis and meta‐regression. Suicide Life Threat Behav. 2014;44:273–303. doi: 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- 13.McCloskey MS, Look AE, Chen EY, Pajoumand G, Berman ME. Nonsuicidal self‐injury: relationship to behavioral and self‐rating measures of impulsivity and self‐aggression. Suicide Life Threat Behav. 2012;42:197–209. doi: 10.1111/j.1943-278X.2012.00082.x. [DOI] [PubMed] [Google Scholar]
- 14.Costa AM, Medeiros GC, Redden S, Grant JE, Tavares H, Seger L. Cognitive-behavioral group therapy for intermittent explosive disorder: description and preliminary analysis. Rev Bras Psiquiatr. 2018;40:316–9. doi: 10.1590/1516-4446-2017-2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guerdjikova AI, Gwizdowski IS, McElroy SL, McCullumsmith C, Suppes P. Treating nonsuicidal self-injury. Curr Treat Options Psychiatry. 2014;1:325–34. [Google Scholar]
- 16.Cordás TA, Tavares H, Calderoni DM, Stump GV, Ribeiro RB. Oxcarbazepine for self-mutilating bulimic patients. Int J Neuropsychopharmacol. 2006;9:769–71. doi: 10.1017/S1461145706006687. [DOI] [PubMed] [Google Scholar]
- 17.First MB, Spitzer RL, Gibbon MW, Williams JB. New York: New York State Psychiatric Institute; 1995. Structured clinical interview for DSM-IV axis I disorders. [Google Scholar]
- 18.Lloyd EE, Kelley ML, Hope T. Annual Meeting of the Society for Behavioral Medicine. New Orleans: EUA; 1997. Self-mutilation in a community sample of adolescents: descriptive characteristics and provisional prevalence rates In. [Google Scholar]
- 19.Nicoli de Mattos C, Kim HS, Requião MG, Marasaldi RF, Filomensky TZ, Hodgins DC, et al. Gender differences in compulsive buying disorder: assessment of demographic and psychiatric co-morbidities. PloS One. 2016;11:e0167365. doi: 10.1371/journal.pone.0167365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim HS, Christianini AR, Bertoni D, de Oliveira MD, Hodgins DC, Tavares H. Kleptomania and co-morbid addictive disorders. Psychiatry Res. 2017;250:35–7. doi: 10.1016/j.psychres.2017.01.048. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez E, Day A, Boyle GJ. Measures of anger and hostility in adults In. In: Boyle G, Saklofske D, Matthews G, editors, editors. Measures of personality and social psychological constructs. Cambridge: Academic Press; 2015. pp. p 74–100. [Google Scholar]
- 22.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 23.Malloy-Diniz LF, Mattos P, Leite WB, Abreu N, Coutinho G, Paula JJ, et al. Tradução e adaptação cultural da Barratt impulsiveness scale (BIS-11) para aplicação em adultos brasileiros. J Bras Psiquiatr. 2010;59:99–105. [Google Scholar]
- 24.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–5. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 25.Gorenstein C, Moreno RA, Bernik MA, Carvalho SC, Nicastri S, Cordás T, et al. Validation of the Portuguese version of the social adjustment scale on Brazilian samples. J Affect Disord. 2002;69:167–75. doi: 10.1016/s0165-0327(01)00300-7. [DOI] [PubMed] [Google Scholar]
- 26.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 27.Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck depression inventory and state-trait anxiety inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29:453–7. [PubMed] [Google Scholar]
- 28.Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, et al. The Mini International Neuropsychiatric Interview (MINI): a short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997;12:224–31. [Google Scholar]
- 29.Amorim P. Mini International Neuropsychiatric Interview (MINI): validação de entrevista breve para diagnóstico de transtornos mentais. Rev Bras Psiquiatr. 2000;22:106–15. [Google Scholar]
- 30.de Azevedo Marques JM, Zuardi AW. Validity and applicability of the Mini International Neuropsychiatric Interview administered by family medicine residents in primary health care in Brazil. Gen Hosp Psychiatry. 2008;30:303–10. doi: 10.1016/j.genhosppsych.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychol Med. 2011;41:1981–6. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- 32.Archer J. Does sexual selection explain human sex differences in aggression? Behav Brain Sci. 2009;32:249–66. doi: 10.1017/S0140525X09990951. [DOI] [PubMed] [Google Scholar]
- 33.Coccaro EF, Posternak MA, Zimmerman M. Prevalence and features of intermittent explosive disorder in a clinical setting. J Clin Psychiatry. 2005;66:1221–7. doi: 10.4088/jcp.v66n1003. [DOI] [PubMed] [Google Scholar]
- 34.Book AS, Starzyk KB, Quinsey VL. The relationship between testosterone and aggression: a meta-analysis Aggress Violent Behav. 2001;6:579–99. [Google Scholar]
- 35.Medeiros GC, Seger L, Grant JE, Tavares H. Major depressive disorder and depressive symptoms in intermittent explosive disorder. Psychiatry Res. 2018;262:209–12. doi: 10.1016/j.psychres.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Klonsky ED, Victor SE, Saffer BY. Nonsuicidal self-injury: what we know, and what we need to know. Can J Psychiatry. 2014;59:565–8. doi: 10.1177/070674371405901101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coccaro EF, McCloskey MS, Fitzgerald DA, Phan KL. Amygdala and orbitofrontal reactivity to social threat in individuals with impulsive aggression. Biol Psychiatry. 2007;62:168–78. doi: 10.1016/j.biopsych.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 38.Nitschke JB, Sarinopoulos I, Oathes DJ, Johnstone T, Whalen PJ, Davidson RJ, et al. Anticipatory activation in the amygdala and anterior cingulate in generalized anxiety disorder and prediction of treatment response. Am J Psychiatry. 2009;166:302–10. doi: 10.1176/appi.ajp.2008.07101682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McTeague LM, Lang PJ. The anxiety spectrum and the reflex physiology of defense: from circumscribed fear to broad distress. Depress Anxiety. 2012;29:264–81. doi: 10.1002/da.21891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson R, Zuroff DC. The levels of self-criticism scale: comparative self-criticism and internalized self-criticism. Pers Individ Dif. 2004;36:419–30. [Google Scholar]
- 41.Longe O, Maratos FA, Gilbert P, Evans G, Volker F, Rockliff H, et al. Having a word with yourself: neural correlates of self-criticism and self-reassurance. NeuroImage. 2010;49:1849–56. doi: 10.1016/j.neuroimage.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 42.Mahe V, Balogh A. Long-term pharmacological treatment of generalized anxiety disorder. Int Clin Psychopharmacol. 2000;15:99–105. doi: 10.1097/00004850-200015020-00006. [DOI] [PubMed] [Google Scholar]
- 43.Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. 2007;1:CD001848. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]


