Introduction
Perniosis, or chilblains, is a cold-induced inflammatory skin disorder characterized by a bilateral and symmetrical distribution. This typical clinical presentation is usually suggestive for diagnosis. Diagnostic criteria are localized erythema and swelling involving acral sites persistent for more than 24 hours, onset and/or worsening in cooler months, and histopathologic findings consistent with perniosis and without findings of lupus erythematosus.1 Histopathology may also be of value in less-typical cases, mainly for exclusion of other diseases.1, 2, 3 Here we describe a patient with an atypical unilateral presentation of perniosis on her right hand, which manifested after a traumatic injury.
Case report
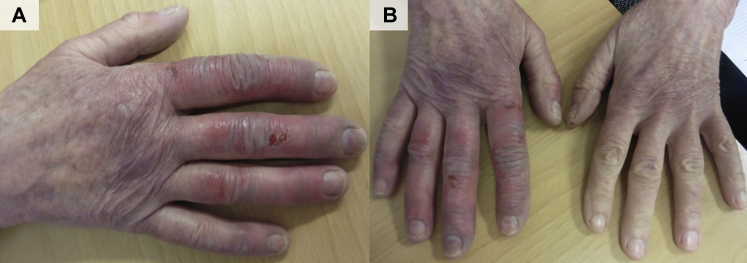
A 66-year-old nonsmoking woman was referred to our hospital for a second opinion regarding slightly tender swelling, erythrocyanotic discoloration, and occasionally spontaneous ulceration of her right hand (Fig 1). The symptoms were present for 6 years, periodically during autumn and winter, and were slowly progressive. One year before the onset of her symptoms, the patient was bitten by a dog in her right hand, resulting in extensive soft tissue injury for which she underwent surgical reconstruction. The patient did not have symptoms or signs of cutaneous or systemic lupus erythematosus. She had a medical history of metacarpal fractures in the right hand about 20 years ago, and Lyme disease 10 years ago. Her family history was negative for autoimmune diseases, in particular, lupus erythematosus and antiphospholipid syndrome. Before referral, acrodermatitis chronica atrophicans was suspected for which she was treated unsuccessfully with antibiotics, highly potent topical steroids, and prednisolone. Later, IgG and IgM Borrelia antibodies were found to be negative. Arterial Doppler examination by a vascular surgeon found no abnormalities. A diagnosis of unilateral perniosis was considered, and the patient was referred to our hospital for confirmation.
Fig 1.
Clinical presentation. A, Unilateral erythrocyanotic swelling with ulcerations of the right hand. B, For comparison, the left hand is unaffected.
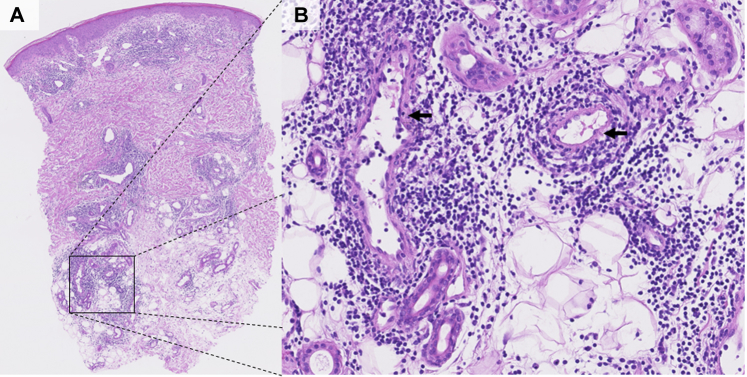
To exclude underlying diseases, we performed a punch biopsy from the dorsal side of the fourth of her right hand and additional laboratory tests. Histopathology found a superficial and deep lymphocytic perivascular and infiltrate around the sweat glands, and a slightly swollen endothelium. There was no significant dermal edema and no vacuolization of the basal cell layer. Alcian blue stain found a mild increase of mucin deposition, and staining for spirochetes was negative (Fig 2). Additional laboratory investigations were carried out to exclude lupus erythematosus. Complete blood count, differential white blood count, and urinalysis were unremarkable. Cryoglobulins and anticardiolipin antibodies, anti-dsDNA antibodies, and antinuclear antibodies were undetectable. Given the typical symptoms and signs, in the absence of underlying disease, and supported by histopathologic findings, we confirmed the diagnosis of unilateral perniosis.1, 2 Treatment options were discussed with the patient. Conservative treatment, in particular keeping her right hand warm, was advised. As second-line therapy, a trial of nifedipine was proposed but refused by the patient. When spring season started, symptoms gradually waned in a few weeks.
Fig 2.
A, Histopathology shows a superficial and deep lymphocytic perivascular infiltrate. B, Larger magnification shows a slightly swollen endothelium with a few lymphocytes (arrows), and without other signs of vasculitis.
Discussion
Perniosis is an inflammatory skin disorder that typically has a symmetrical and bilateral distribution. It most commonly affects middle-aged women and has a female/male ratio of 2 to 3:1.1, 3, 4 The pathogenesis of perniosis is largely unknown but seems to be related to abnormal vasospasms, vasoconstriction, hyperviscosity, or autoimmunity.3, 5 Several systemic diseases like lupus erythematosus, antiphospholipid syndrome, rheumatoid arthritis, and cryoglobulinemia have been associated with perniosis, usually with bilateral involvement.1, 2, 3, 4, 5, 6 Our case is atypical given the unilateral presentation, which raises questions about disease pathogenesis.
Three other cases of unilateral perniosis have been described in literature.7, 8 These cases may gain insight in the pathogenesis, as they have similar specific conditions. A recent report described 2 cases of periodically occurring unilateral perniosis in patients with monoparesis resulting from lumbar compression and from radiation and surgery, respectively.7 Another report described a case of unilateral perniosis occurring every winter in the right foot of a Chinese woman who had undergone surgery of the right ankle to correct a childhood polio defect.8 As suggested in these reports, the unilateral presentation of perniosis may be caused by disturbed localized circulation as a result of a dysfunctioning autonomous nervous system in the context of nerve damage, in our case potentially present as a result of a dog bite.7
According to the literature, unilateral and bilateral pernioses are treated similarly.7, 8 Treatment should focus on conservative measures such as keeping the affected areas warm and dry and smoking avoidance.1 As first-line therapy, topical steroids could be considered as well.1, 3 Nifedipine, 20 to 60 mg daily, has been suggested as second-line therapy by Cappel and Wetter1 although others question its efficacy.9 Third-line treatment may include pentoxifylline, nicotinamide, aspirin, minoxidil 5% solution, nitroglycerin 2% ointment, or tacrolimus 0.1% ointment.1
This case illustrates that perniosis can present unilaterally in certain conditions. Dermatologists should be aware of the possibility of perniosis in patients presenting with cold-induced unilateral swelling and erythrocyanotic discoloration of an acral site. Conducting a focused history on trauma to the affected limb may explain the unilateral presentation.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Cappel J.A., Wetter D.A. Clinical characteristics, etiologic associations, laboratory findings, treatment, and proposal of diagnostic criteria of pernio (chilblains) in a series of 104 patients at Mayo Clinic, 2000 to 2011. Mayo Clin Proc. 2014;89:207–215. doi: 10.1016/j.mayocp.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Viguier M., Pinquier L., Cavelier-Balloy B. Clinical and histopathologic features and immunologic variables in patients with severe chilblains: a study of the relationship to lupus erythematosus. Medicine. 2001;80:180–188. doi: 10.1097/00005792-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Bolognia J.L., Schaffer J.V., Jorizzo J.L. 2012. Dermatology - third edition. Disorders due to physical agents: Pernio; pp. 1493–1494. New Haven. [Google Scholar]
- 4.Takci Z., Vahaboglu G., Eksioglu H. Epidemiological patterns of perniosis, and its association with systemic disorder. Clin Exp Dermatol. 2012;37:844–849. doi: 10.1111/j.1365-2230.2012.04435.x. [DOI] [PubMed] [Google Scholar]
- 5.Ibarra B.S., Meeker J., Jalali O., Lynch M.C. Cold-induced dermatoses: case report and review of literature. Am J Dermatopathol. 2018;40:291–294. doi: 10.1097/DAD.0000000000001018. [DOI] [PubMed] [Google Scholar]
- 6.Yang X., Perez O.A., English J.C. Adult perniosis and cryoglobulinemia: a retrospective study and review of the literature. J Am Acad Dermatol. 2010;62:21–22. doi: 10.1016/j.jaad.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 7.Couture P., Moguelet P., Chasset F., Barbaud A., Senet P., Monfort J.B. Two cases of unilateral chilblains associated with monoparesis. Ann Dermatol Venereol. 2019 doi: 10.1016/j.annder.2019.01.022. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Klapman M.H., Johnston W.H. Localized recurrent postoperative pernio associated with leukocytoclastic vasculitis. J Am Acad Dermatol. 1991;24:811–813. doi: 10.1016/0190-9622(91)70119-m. [DOI] [PubMed] [Google Scholar]
- 9.Souwer I.H., Bor J.H.J., Smits P., Lagro-Janssen A.L. Nifedipine vs placebo for treatment of chronic chilblains: a randomized controlled trial. Ann Fam Med. 2016;14:453–459. doi: 10.1370/afm.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]