Abstract
Objective
To compare consumer rated quality of care among individuals living long-term in homelike clustered domestic and standard models of residential care in Australia.
Design
Cross-sectional study.
Setting
Seventeen residential aged care facilities in four Australian states providing alternative models of care.
Study participants
A sample of individuals with high prevalence of cognitive impairment living in residential care for 12 months or longer, not immediately in palliative care and having a proxy available to provide consent and assist with data collection. Of 901 eligible participants, 541 consented and participated in the study.
Main outcome measure
Consumer rated quality of care was measured using the Consumer Choice Index–6 Dimension instrument (CCI-6D) providing a preference weighted summary score ranging from 0 to 1. The six dimensions of care time, shared-spaces, own-room, outside and gardens, meaningful activities and care flexibility were individually evaluated.
Results
Overall consumer rated quality of care (Mean ∆: 0.138, 95% CI 0.073–0.203 P < 0.001) was higher in clustered domestic models after adjusting for potential confounders. Individually, the dimensions of access to outside and gardens (P < 0.001) and flexibility of care (P < 0.001) were rated significantly better compared to those living in standard model of care.
Conclusions
Homelike, clustered domestic models of care are associated with better consumer rated quality of care, specifically the domains of access to outdoors and care flexibility, in a sample of individuals with cognitive impairment. Including consumer views on quality of care is feasible and should be standard in future evaluations of residential care.
Keywords: dementia, nursing homes, quality of healthcare, Australia, self-report
‘Long term care is intimate care, and how it is given, when it is given, and by whom it is given shapes the biography of the long term care consumer…’[1]—Rosaline Kane
Including consumer perspectives in the evaluation of quality of care is common in health but less common in residential aged care settings. Previous studies evaluating the quality of care of residents of aged care facilities have used measures such as pressure ulcers, restraints and falls, [2–5] that do not take into consideration the consumer perspective. Such an approach limits the definition of quality of care to medical and clinical components while ignoring the psychological and social aspects of care that are integral to overall health and wellbeing. Those indicators are also focused towards safety and quality compliance rather than promoting resident wellbeing and quality of life [6].
Evaluating the quality of care in residential care from a consumer perspective is critical, with the introduction of consumer directed care (and similar care philosophies) in long-term care worldwide [4]. Similarly, with care philosophies consistently moving from a medical model to a person-centred model, quality of care needs to be evaluated from the perspective of the care recipients.
Providing residential care for people with dementia has evolved in the recent few decades to include an increasing emphasis on domestic, small-scale environments and person-centred care [7]. In addition, the concept of personhood in dementia care has received increasing attention. Several innovative models of long-term residential care have been developed and use different terminologies and methods of practice. These models of care share several common themes or components including the design of the physical building, providing housing and services in smaller living units, continuity of care staff in the unit, additional training for staff, involvement of residents in administration of the organization, flexibility and personalization in care routines.
Efforts have been made to evaluate these models of care and improvements in outcomes for residents including quality of life, emotional and physical wellbeing, participation and interaction, food intake and behavioural and psychological symptoms of dementia have been demonstrated [3, 8]. A study of the Greenhouse model of care in the US found reduction in hospitalizations for residents, as well as reduction in measures of clinical care quality such as restraint use, pressure ulcers and catheter use [2].
Other studies evaluating this model of care have found mixed results with some finding benefits for physical function, fewer hospitalizations and clinical indicators of quality of care in comparison to standard care and other studies finding no evidence for benefits in measures such as ADL, pain, ulcers, mobility and other Minimum Data Set quality indicators [5, 8, 9]. However there is limited evidence examining the quality of this model from a consumer perspective [3, 10].
The Consumer Choice Index–6 Dimension (CCI-6D) is a recently developed instrument to measure quality of care in long-term facilities from a consumer perspective [11]. The instrument comprises a 6-item questionnaire that can be completed by participants and/or their family members, and better quality of care as measured by the instrument has been shown to be associated with better quality of life among residents. Its six dimensions include care time, shared-spaces, own-room, outside and gardens, meaningful activities and care flexibility. The CCI-6D has strong content and construct validity, and includes a scoring system weighted according to the preferences of people living in residential aged care, and their family member carers [11, 12]. The homelike models of care have never been evaluated with a standardized instrument of quality of care such as the CCI-6D.
The aim of this analysis is to evaluate quality of care from the consumer perspective in a population of older adults living long-term in residential care in Australia; specifically, to compare standard residential care facilities with a clustered, domestic model of care.
Methods
Study sample
The sample for this analysis emanates from the Investigating Services Provided in the Residential Care Environment for Dementia (INSPIRED) study which has been described elsewhere [3, 13]. Briefly, this cross-sectional study included individuals who had lived for at least 12 months in one of 17 care facilities across four states in Australia. Facilities providing different models of care were purposefully sampled to include those located in urban and rural locations and include residents living with cognitive impairment and, or dementia. Within facilities all individuals were assessed for eligibility, those in palliative care and for whom it was not possible to obtain consent and collect data either directly or through a proxy were excluded. A total of 1323 individuals were assessed for eligibility, 901 were eligible and 541 consented (majority (84%) with dementia or cognitive impairment) to participate in the study. Data were collected at a single time point in the period between January 2015 and February 2016. Individual level data on demographic and social characteristics, health and function, care provision, quality of life and quality of care were collected through questionnaires from participants or their proxies and from facility records. Facility level data were collected through a facility level questionnaire (adapted from a similar study [14]) from the administrators of each facility. Ethics approval for the study was obtained from the Flinders University Social and Behavioural Research Ethics Committee.
Variables
The main outcome for this analysis, i.e. consumer rated quality of care, was measured using the Consumer Choice Index–6 Dimension (CCI-6D) as introduced earlier. In this study responses to CCI-6D were collected from the participants or their proxies (where participants were assessed to have moderate to severe cognitive impairment (a PAS-Cog cognitive assessment score of ≥11)). A proxy needed to be in a close relationship with the resident, visiting them regularly and assisting them with decision making (i.e. usually this role was fulfilled by a close family member or friend). Several studies have indicated the difficulty using proxies to rate abstract concepts such as quality in people living with dementia, with poor agreement between the ratings given by proxies and the people with dementia [15]. However, in this population including proxy responses is the only opportunity to include individuals with severe cognitive impairment in research that involves them [16]. Family members are also preferred over clinicians as proxies [16]. A preference weighted scoring algorithm derived from resident ratings was applied to the CCI-6D responses to derive a summary quality of care score on a scale of 0–1 with higher scores indicating better quality of care [12]. Complete CCI-6D responses were not available for one participant and excluded from further analyses.
The main explanatory variable was the model of care [8, 17] provided at the facilities where these participants resided. The model of care was defined based on the following six criteria: small size living units, consistent allocation of staff to living units, accessibility to outdoor areas, meals cooked within the living unit, opportunity for self-service of meals or opportunity for residents to participate in meal preparations. These criteria were based on the literature [18–21] and consultations with industry (clinicians, researchers and care providers) and consumer representatives. Consultation involved initial discussions regarding concepts and evidence around the key features of these models of care, collation of the information considering the context of the evidence, drafting an initial list of criteria which was reviewed and then finalized by all parties. A binary variable to define the model of care was used since all facilities met either two or less and five or more of the six criteria. A facility was defined as providing a clustered domestic model of residential care if it met five of the six criteria. All other facilities were defined as those providing standard residential care as they met only one or two of the criteria.
Descriptive analysis compared means and proportions of participant characteristics between the two models of care using standard t-tests or chi-square tests as appropriate. Facility level characteristics were not compared statistically due to prohibitively low sample of 17 facilities. Analyses used multi-level random effect linear regression models adjusting for individual (age, gender, cognition (PAS-Cog) [22], ADL (Modified Barthel Index) [23], social interactions (frequency of visits from family and/or friends) and comorbidities (Cohen–Mansfield comorbidity index) [24]) and facility level (geographic location, size, staff training and direct care hours) characteristics. Geographical location was categorized as urban or rural based on standard Australian classifications, size of facilities was based on the total number of beds in each facility, staff training was defined based on the facility level expenditure on staff training in the preceding 2 years and direct care hours was defined as all care provided by nurses, care workers and allied health staff. Age of facility was the years since either initial construction, extension or major refurbishment. It was not possible to ascertain if the exact location the study participants' lived in the facility was original build, new extension or that which was significantly refurbished. Hence age of facility was not included in the final adjusted model but only included in a sensitivity analysis to test its effect on the adjusted difference.
Unadjusted proportions of participants’ (or proxies’) responses and adjusted odds ratios of reporting best ratings in the 6 individual dimension of the CCI-6D among those living in the clustered domestic facilities were estimated using multi-level generalized linear regression models, with binary link functions. Confidence intervals were reported for all summary measures and statistical significance was determined at P < 0.05. All statistical analysis was performed using SAS software version 9.4. Copyright © 2018 SAS Institute Inc.
Results
Four facilities (120 participants) of the 17 provided the clustered domestic model of care (Table 1). Overall the mean age of participants was 86 years, and 75% of the sample were female. Participants on average had 3.7 comorbid disease groups. Eighty-four percent had a medical diagnosis of dementia or were cognitively impaired (PAS-Cog score ≥5). Study participants living in facilities providing a clustered domestic model of care were significantly younger, had more neuropsychiatric symptoms, had fewer comorbid conditions, were more cognitively impaired, had fewer weekly social interactions, a higher proportion had dementia and the clear majority of the quality of care (CCI-6D) responses were by proxies. The clustered domestic model facilities had higher investment in staff training, higher hours of direct care staff allocated and were younger aged facilities.
Table 1.
Baseline participant and facility characteristics
| Participant characteristics | Clustered domestic model of care (n = 120) | Standard model of care (n = 421) |
|---|---|---|
| Age, mean (SD) | 83.3 (9.0) | 86.1 (8.3)* |
| Female, n (%) | 90 (75.0) | 313 (74.4) |
| Married, n (%) | 36 (30.0) | 101 (24.1)* |
| Modified Barthel Index, mean (SD) | 37.1 (31.1) | 41.3 (33.3) |
| Number of comorbid conditions, (Cohen–Mansfield Index), mean (SD) | 3.2 (1.4) | 3.8 (1.4)* |
| PAS-Cog, mean (SD) | 17.4 (16.5) | 12.2 (11.4)* |
| Diagnosis of dementia in medical records, n (%) | 117 (97.5) | 231 (55.1%)* |
| PAS-Cog 0–<4 (no cognitive impairment), n (%) | 3 (2.5) | 90 (21.4) |
| Pas-Cog 4–<10 (mild cognitive impairment), n (%) | 12 (10.0) | 88 (20.9) |
| Pas-Cog 10–<16 (moderate cognitive impairment), n (%) | 18 (15.0) | 64 (15.2) |
| Pas-Cog 16–21 (severe cognitive impairment), n (%) | 87 (72.5) | 179 (42.5) |
| Dementia diagnosis or PAS-Cog ≥5, n (%) | 120 (100) | 333 (79)* |
| Weekly interaction with close social ties, n (%) | 66 (56.4) | 312 (75.2)* |
| CCI-6D proxy responses, n (%) | 114 (95.0) | 277 (65.8)* |
| Facility characteristics | Clustered domestic model of care (n = 4) | Standard model of care (n = 13) |
| Metropolitan location, n (%) | 3 (75) | 10 (77) |
| Total facility size (No. beds), mean (SD) | 83 (6.6) | 83 (6.9) |
| High staff training costs (>$1000 per resident annually), n (%) | 4 (100) | 4 (33) |
| High direct care hours (>2.5 per resident per day), n (%) | 3 (75.0) | 6 (46) |
| Years since construction, extension or major refurbishment, mean (SD) | 10 (4.3) | 17 (25.1) |
SD, Standard Deviation; NPI-Q, Neuropsychiatric Inventory–Questionnaire; PAS-Cog, Psychogeriatric Assessment Scales–Cognitive Impairment Scale, CCI-6D, Consumer Choice Index–6 Dimensions, *P < 0.05.
Living in a facility providing clustered domestic model of care was significantly associated with better overall quality of care as measured by the CCI-6D (Mean ∆: 0.138, 95% CI 0.073–0.203 P < 0.001) after adjusting for potential confounding factors (Table 2). Subgroup analyses of only those individuals who responded through a proxy (Supplementary Table 1) and those with severe cognitive impairment (Supplementary Table 2), despite reduced sample size showed similar significant differences. Inclusion of the age of facility in the adjusted model gave similar findings (Mean ∆: 0.128, 95% CI 0.033–0.223 P < 0.008 (not tabulated)).
Table 2.
Quality of care (CCI-6D total weighted score) by models of residential care
| Quality of care (CCI-6D) | Adjusteda model predicted CCI-6D mean values (95% CI) | Mean difference (Clustered domestic-standard) (95% CI) | P-value (Adjusteda) | ||
|---|---|---|---|---|---|
| Clustered domestic (n = 120) | Standard (n = 420) | Unadjusted | Adjusteda | ||
| Consumer rated quality of care | 0.856 (0.792, 0.919) | 0.718 (0.674, 0.761) | 0.082* (0.009, 0.016) | 0.138 (0.073, 0.203) | <0.001 |
PAS-Cog, Psychogeriatric Assessment Scales–Cognitive Impairment Scale; CCI-6D, Consumer Choice Index–6 Dimensions.
aAdjusted for age, gender, PAS-Cog, Barthel Index, Social ties, number of comorbidities, regional location, facility size, staff training and direct care hours. *P < 0.05.
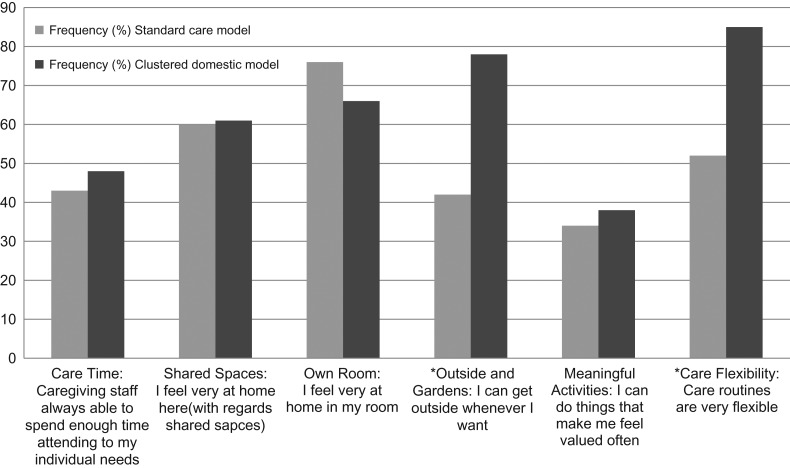
Individually, a significantly higher proportion of those living in clustered domestic facilities reported better ratings for the dimensions of access to outside and gardens and flexibility of care. After adjusting for potential confounders, the probabilities of reporting better ratings for these two dimensions were significantly better among those living in the clustered domestic facilities compared to those living in standard model of care (Table 3 and Fig. 1).
Table 3.
Unadjusted proportions and adjusted odds of individual dimensions of CCI-6D by models of care
| Dimension | Frequency N(%*) | Adjusted | ||
|---|---|---|---|---|
| Standard care model | Clustered domestic model | Odds ratio (95% CI) | P-value | |
| Care Time: How much time are Caregiving staff able to spend with me (your family member)? | 1.48 (0.75, 2.96) | 0.261 | ||
| Always able to spend enough time attending to my individual needs | 180 (43%) | 57 (48%) | ||
| Sometimes able to spend enough time attending to my individual needs | 197 (47%) | 58 (48%) | ||
| Rarely able to spend enough time attending to my individual needs | 43 (10%) | 5 (4%) | ||
| Shared Spaces: Do the shared spaces of the Aged care home as a whole make you (or your family member) feel ‘at home’? | 1.05 (0.52, 2.13) | 0.881 | ||
| I feel very at home here | 251 (60%) | 73 (61%) | ||
| I feel at home here sometimes | 110 (26%) | 30 (25%) | ||
| I feel at home here rarely | 59 (14%) | 17 (14%) | ||
| Own Room: Does your own room here make you (or your family member) feel ‘at home’? | 1.02 (0.49, 2.15) | 0.950 | ||
| I feel very at home in my room | 318 (76%) | 79 (66%) | ||
| I feel at home in my room sometimes | 87 (21%) | 33 (28%) | ||
| I feel at home in my room rarely | 15 (4%) | 8 (7%) | ||
| Outside and Gardens: Is there access to outside and gardens in this Aged care home? | 7.46 (3.35, 16.63) | <0.001 | ||
| I can get outside whenever I want | 175 (42%) | 93 (78%) | ||
| I can get outside sometimes | 94 (23%) | 12 (10%) | ||
| I cannot get outside easily | 151 (36%) | 15 (13%) | ||
| Meaningful Activities: How often does the facility offer me (or my family member) things to do that make me feel valued? | 1.47 (0.71, 3.04) | 0.297 | ||
| I can do things that make me feel valued often | 143 (34%) | 45 (38%) | ||
| I can sometimes do things that make me feel valued | 149 (36%) | 39 (33%) | ||
| I can only rarely or occasionally do things that make me feel valued | 128 (31%) | 36 (30%) | ||
| Care Flexibility: How flexible is the Aged care home with the care routines? | 7.81 (3.47, 17.60) | <0.001 | ||
| Care routines are very flexible | 220 (52%) | 102 (85%) | ||
| There is a little flexibility in the care routines | 141 (34%) | 14 (12%) | ||
| There is not much flexibility in the care routines | 59 (14%) | 4 (3%) | ||
*Some percentages summing up to more than 100 due to rounding up.
Figure 1.
Unadjusted proportions of individual dimensions of CCI-6D by models of care. *P < 0.05.
Discussion
Living in a facility providing a clustered domestic model of care was associated with better consumer rated quality of care even though individuals living in this model had poorer health and function as indicated by several measures. This study used the Consumer Choice Index–6 Dimension (CCI-6D) instrument which not only provides a consumer perspective but was also developed with recipients of care [11]. Specifically, the individual dimensions of access to outdoors and flexibility in care were rated better among residents in the clustered domestic model of care.
Being a recently developed instrument, a minimally important difference (MID) for this quality of care measure has not been established. For the current analysis, the best opportunity to understand the importance of this association is by comparing it to a within sample distribution based MID [25] of 0.107 (0.5*SD of difference). Another option is to compare the observed difference to the MID of other preference-based measures in this population. The EQ-5D, a measure of health-related quality of life which is among the most widely used preference-based measures and is recommended for use in aged care populations has a published range of minimal important differences from 0.03 to 0.074 [26]. Our observed difference of 0.138 is higher than the within sample MID of 0.107 as well as those reported to be clinically meaningful for the EQ-5D. However, future studies need to independently determine the MID for the CCI-6D.
Two individual dimensions of the CCI-6D were strongly associated with the clustered domestic model of care, namely access to outdoors and care routine flexibility. The facilities that provide a clustered domestic model of care are purpose built to provide outdoor and garden access for the residents. However, it is important to differentiate between environmental design and the actual resident experience of using the outdoors. Whilst independent access to outdoors is required for residents to experience it, other factors such as supportive safety and risk policies and assistance from staff are also required for the use of outdoor spaces by residents.
Care routine flexibility is often restricted in standard care facilities due to the physical, institutional group living and staffing environment. However, flexibility in care routines is an important aspect of person-centred care which contributes to promoting individual rights and dignity [27, 28]. It also provides a sense of control to individuals living in residential care where much of their life and environment is restricted to adhere to safety regulations. Greater flexibility in care routines in homelike models of care as rated by the individuals and family members has not been shown previously.
The Australian government’s productivity commission report [29] also recommends the need for increased choice and flexibility in residential care. This was echoed in the rapid review commissioned by the Australian Aged Care Quality Agency, which identified independence and autonomy as one of the main considerations of high quality residential care [30]. This study’s finding that the clustered homelike model of care is a better environment for flexibility and care from the consumer’s perspective, provides an opportunity to fulfil those identified recommendations.
In this analysis, the remaining four dimensions of the CCI-6D, namely, care time, shared spaces, own room and meaningful activities were found not to be significantly different between the residents of the two models of care. All participating facilities in the study were not-for-profit organizations which are generally recognized to provide high quality of care [31]. It is also possible that of facilities that were approached for inclusion in this study, only those that provided a higher level of care were willing to participate. This may explain why there were minimal differences between the two models of care with respect to these domains.
Conversely, it is plausible that the distinguishing characteristics of the clustered domestic model of care have a larger impact on the two domains of access to outside and gardens and care flexibility. These two domains (along with ‘own room’) were also weighted higher for the most flexible choice in the resident-rating based algorithm used to calculate the overall quality of care score [12].
However, given the possibility that all the facilities in this study generally provide high quality of care, the observed differences between the two models of care are statistically (and potentially clinically) significant. This points to the strength of the evidence that the clustered domestic model of care is associated with better overall consumer rated quality of care.
The homelike models of care have also been shown to be associated with better quality of life outcomes in other studies, including within this study sample [3, 8, 21]. Hence, it is possible that providing a homelike model of care is associated with both an independent and complementary benefit in terms of quality of life and quality of care. The findings of this study further strengthen the argument that investing in homelike models of care should be a priority for all stakeholders involved in the care of people with dementia. As the proportion of populations needing and living long-term in residential care increases worldwide, planning for increased supply of care services needs to prioritize incorporating these and other factors that characterize homelike models of care into development, management and delivery of care services. While the costs and consequences of this model of care have been evaluated [8], a full economic evaluation of these models of care is a future research priority.
This analysis has some strengths and limitations. This is the first study that examines quality of care from a consumer perspective in these homelike models of care. The sample of this study is largely representative of Australian residential aged care populations [13]. All facilities offering the homelike model of care in this study were operated by a single provider, hence it is not possible to delineate the effect the provider and its policies and resources have on the quality of care. However, one of the other facilities administered by this provider provided standard residential care. On the contrary one of the limitations of the larger evaluations of the Greenhouse model is the heterogeneity in the implementation of the model of care across organizations and facilities [21]. Our study reduces the effects of the heterogeneity in the implementation of the model of care.
The CCI-6D as described earlier has strong content and construct validity, and includes a scoring system weighted according to the preferences of people living in residential aged care, and their family member carers [11, 12]. However, it is still a relatively new instrument and is yet to undergo wider testing. In this analysis, the responses were predominantly reported by proxies in the clustered domestic model. Proxies are generally known to provide lower ratings than residents for subjective measures such as quality of life [15]. Hence, the higher proportion of proxy ratings in the clustered domestic model is unlikely to affect the significantly better rating, instead it has the potential to under estimate the ratings in that group. Irrespective of the resident or proxy reported quality of care this study shows that it is feasible to evaluate quality of care from a consumer perspective.
Another factor to consider in the interpretation of these findings is the potential bias due to self-selection of individuals into facilities. The Australian residential aged care system in theory provides some choice to entrants into the system. However, in practice for many people the decision to move into residential care is necessitated by a period of acute illness and, or loss of physical function that is sudden. Due to the shortage of available residential care places at a given point in time, the ability to self-select is limited [32]. Hence, the potential bias due to self-selection into one model of care or other is unknown but potentially limited.
This study is cross-sectional in design and hence no temporal or causative inferences can be drawn based on these associations. Confirmation of these findings in longitudinal studies is needed. Similarly, there were noted differences between facilities providing the two models of care and the individual characteristics of people living in the two groups. We have statistically controlled for observed differences, but it is possible that the quality of care may be affected by other factors which were not adjusted for or not measured as part of this study. One of those factors is the age of facility. The clustered domestic model facilities were newer than the standard care ones which has the potential to affect the perception of quality. However, the age of facility when adjusted for in the analysis remained statistically significant and only marginally reduced the difference in care quality between the two models of care.
Conclusion
This analysis suggests that clustered domestic models of care provide a higher quality of care from the consumer perspective, in a study which included a high proportion of residents with dementia. Specifically, the homelike, clustered domestic model of care is associated with better ratings for two of the six domains of consumer rated quality of care, namely access to outdoors and care flexibility. Changes to the way aged care is provided to better align with a homelike model of care has the potential to better meet consumer preferences. This analysis of the quality of this model of care provides preliminary evidence to warrant further study and investigation of its implementation. Including consumer views on the quality of care is feasible and should be considered essential in future evaluations of residential care.
Supplementary Material
Acknowledgements
The authors sincerely thank the INSPIRED study participants and their family members for their participation and interest in the study. The assistance of facility staff, care worker researchers, facility pharmacists and data collectors in data collection in each state and facility is gratefully acknowledged. Non-Author members of the study team are thanked for their input into study management, data collection and data coordination of the INSPIRED study.
Supplementary material
Supplementary material is available at International Journal for Quality in Health Care online.
Funding
This work was supported by funding provided by the National Health and Medical Research Council (NHMRC) Partnership Centre on Dealing with Cognitive and Related Functional Decline in Older People (CDPC) (grant number GNT9100000). The contents of the published materials are solely the responsibility of the Administering Institution, Flinders University, and the individual authors identified, and do not reflect the views of the NHMRC or any other Funding Bodies or the Funding Partners.
References
- 1. Kane RA. Long-term care and a good quality of life: bringing them closer together. Gerontologist 2001;41:293–304. [DOI] [PubMed] [Google Scholar]
- 2. Afendulis CC, Caudry DJ, O’Malley AJ et al. Green house adoption and nursing home quality. Health Serv Res 2016;51:454–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ausserhofer D, Deschodt M, De Geest S et al. ‘There’s No Place Like Home’: a scoping review on the impact of homelike residential care models on resident-, family-, and staff-related outcomes. J Am Med Dir Assoc 2016;17:685–93. [DOI] [PubMed] [Google Scholar]
- 4. Castle NG, Ferguson JC. What is nursing home quality and how is it measured? Gerontologist 2010;50:426–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grabowski DC, O’Malley AJ, Afendulis CC et al. Culture change and nursing home quality of care. Gerontologist 2014;54:S35–45. [DOI] [PubMed] [Google Scholar]
- 6. Rahman AN, Applebaum RA. The nursing home minimum data set assessment instrument: Manifest functions and unintended consequences—past, present, and future. Gerontologist 2009;49:727–35. [DOI] [PubMed] [Google Scholar]
- 7. Verbeek H, van Rossum E, Zwakhalen SMG. Kempen GIJM, Hamers JPH. Small, homelike care environments for older people with dementia: a literature review. Int Psychogeriatr 2009;21:252–64. [DOI] [PubMed] [Google Scholar]
- 8. Dyer SM, Liu E, Gnanamanickam ES et al. Clustered domestic residential aged care in Australia: fewer hospitalisations and better quality of life. Med J Aust 2018;208:1–8. [DOI] [PubMed] [Google Scholar]
- 9. Shier V, Khodyakov D, Cohen LW et al. What does the evidence really say about culture change in nursing homes? Gerontologist 2014;54:S6–16. [DOI] [PubMed] [Google Scholar]
- 10. Milte R, Shulver W, Killington M et al. Quality in residential care from the perspective of people living with dementia: the importance of personhood. Arch Gerontol Geriatr 2016;63:9–17. [DOI] [PubMed] [Google Scholar]
- 11. Milte R, Ratcliffe J, Bradley C et al. Evaluating the quality of care received in long-term care facilities from a consumer perspective: development and construct validity of the Consumer Choice Index–Six Dimension instrument. Ageing Soc 2017: 1–23. doi: 10.1017/S0144686X17000861. [Google Scholar]
- 12. Milte R, Ratcliffe J, Chen G et al. What characteristics of nursing homes are most valued by consumers? A discrete choice experiment with residents and family members. Value Health 2018;21:843–9. [DOI] [PubMed] [Google Scholar]
- 13. Gnanamanickam ES, Dyer SM, Milte R et al. Direct health and residential care costs of people living with dementia in Australian residential aged care. Int J Geriatr Psychiatry 2018;33:859–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Palm R, Kohler K, Schwab CG et al. Longitudinal evaluation of dementia care in German nursing homes: the ‘DemenzMonitor’ study protocol. BMC Geriatr 2013;13:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hounsome N, Orrell M, Edwards RT. EQ-5D as a quality of life measure in people with dementia and their carers: evidence and key issues. Value Health 2011;14:390–9. [DOI] [PubMed] [Google Scholar]
- 16. Bryan S, Hardyman W, Bentham P et al. Proxy completion of EQ-5D in patients with dementia. Qual Life Res 2005;14:107–18. [DOI] [PubMed] [Google Scholar]
- 17. Harrison SL, Kouladjian O’Donnell L, Milte R et al. Costs of potentially inappropriate medication use in residential aged care facilities. BMC Geriatr 2018;18:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fleming R, Purandare N. Long-term care for people with dementia: environmental design guidelines. Int Psychogeriatr 2010;22:1084–96. [DOI] [PubMed] [Google Scholar]
- 19. Lawton MP. The physical environment of the person with Alzheimer’s disease. Aging Ment Health 2001;5:56–64. [DOI] [PubMed] [Google Scholar]
- 20. Verbeek H, Zwakhalen SM, van Rossum E et al. Dementia care redesigned: effects of small-scale living facilities on residents, their family caregivers, and staff. J Am Med Dir Assoc 2010;11:662–70. [DOI] [PubMed] [Google Scholar]
- 21. Zimmerman S, Bowers BJ, Cohen LW et al. New evidence on the green house model of nursing home care: synthesis of findings and implications for policy, practice, and research. Health Serv Res 2016;51:475–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jorm AF, Mackinnon AJ, Henderson AS et al. The psychogeriatric assessment scales: a multidimensional alternative to categorical diagnoses of dementia and depression in the elderly. Psychol Med 1995;25:447–60. [DOI] [PubMed] [Google Scholar]
- 23. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 1989;42:703–9. [DOI] [PubMed] [Google Scholar]
- 24. Cohen-Mansfield J, Marx MS, Regier NG et al. The impact of personal characteristics on engagement in nursing home residents with dementia. Int J Geriatr Psychiatry 2009;24:755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Revicki D, Hays RD, Cella D et al. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 2008;61:102–9. [DOI] [PubMed] [Google Scholar]
- 26. Bulamu NB, Kaambwa B, Ratcliffe J. A systematic review of instruments for measuring outcomes in economic evaluation within aged care. Health Qual Life Outcomes 2015;13:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Edvardsson D, Winblad B, Sandman PO. Person-centred care of people with severe Alzheimer’s disease: current status and ways forward. Lancet Neurol 2008;7:362–7. [DOI] [PubMed] [Google Scholar]
- 28. Laver K, Cumming RG, Dyer SM et al. Clinical practice guidelines for dementia in Australia. Med J Aust 2016;204:191–3. [DOI] [PubMed] [Google Scholar]
- 29. Australian Government Productivity Commission Caring for older Australians. Inquiry report Canberra: Australian Government Productivity Commission. 2011.
- 30. Jeon Y-H, Forsyth R Final Report: A Rapid Review for the development of Consumer Experience Report (CER). Sydney: Sydney Nursing School, The University of Sydney; 2016.
- 31. Comondore VR, Devereaux PJ, Zhou Q et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. BMJ 2009;339:381–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Access Economics Caring places: planning for aged care and dementia 2010–2050: Access Economics; 2010.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.