Abstract
Purpose
To report a case of necrotic uveal melanoma presenting as orbital cellulitis with an intraocular hemorrhage.
Observations
A 61 year-old non-verbal male presented with a two-week history of right eyelid swelling and erythema unresponsive to antibiotics. In addition to these signs of orbital cellulitis, he presented with an opaque media precluding fundus visualization. He was later found to have a collar-button shaped mass consistent with uveal melanoma on B scan ultrasonography during an exam under anesthesia. The patient underwent enucleation with histopathology confirming a necrotic uveal melanoma.
Conclusion and Importance
This case demonstrates how necrotic uveal melanoma can present as orbital cellulitis and the importance of keeping the diagnosis on the differential.
Keywords: Orbital cellulitis, Necrotic uveal melanoma
1. Introduction
Orbital cellulitis is a rare presenting feature of necrotic uveal melanoma, as most patients present incidentally with a painless intraocular mass. However, ocular inflammation can be the primary clinical sign of necrotic uveal melanoma, highlighting the importance of keeping malignancy in the differential diagnosis of orbital cellulitis.1 Here, we report a case of necrotic uveal melanoma presenting as orbital cellulitis with an intraocular hemorrhage in a non-verbal patient.
2. Case report
A 61 year-old non-verbal male with a history of developmental delay presented as a transfer from an outside hospital for further work-up of a two-week history of right eyelid swelling and eye redness unresponsive to antibiotics. The patient was a resident of a group home and was noted by caregivers to have progressively worsening eyelid swelling and agitation with attempts to touch the eye. The patient was initially started on antibiotic eye drops with no improvement in symptoms, and then later transitioned to intravenous antibiotics for concern for orbital cellulitis at the outside hospital.
On presentation to our facility, the patient was afebrile with a white blood cell count of 11.0 × 103 cells/microliter. Examination was extremely limited due to the patient's non-verbal status, inability to follow commands, and agitation with attempts to assess the eye due to presumed eye pain. Assessment of visual acuity and extraocular motility were unable to be obtained. Evaluation of the pupils was also limited, though the right pupil was noted to be round, mid-dilated and fixed. The left pupil was round and reactive to light. Evaluation for a relative afferent pupillary defect using a reverse technique was attempted but unsuccessful due to patient cooperation. Intraocular pressure was 37 mmHg in the right eye, and was soft by palpation in the left eye. External examination revealed mild proptosis, marked upper and lower lid edema, and mild erythema overlying the eyelids of the right eye (Fig. 1). Anterior segment exam disclosed significant conjunctival injection with chemosis, an opaque cornea, and a hyphema in the anterior chamber. There was no view to the fundus in the right eye. Examination of the left eye was unremarkable.
Fig. 1.
An external photograph of the right eye revealed significant upper eyelid edema, erythema, and chemosis.
Orbital computed tomography (CT) scan with contrast showed preseptal and postseptal inflammation along with a hyperdensity in the vitreous cavity (Fig. 2). Due to poor cooperation with a complete examination, the patient later underwent an examination under anesthesia. Ocular media opacity precluded any view to the fundus, the cornea was edematous, and iris details were not visible. B-scan ultrasonography was then conducted on the right eye and revealed the presence of a choroidal mass with a collar button-shaped configuration in the vitreous cavity consistent with a uveal melanoma (Fig. 3).
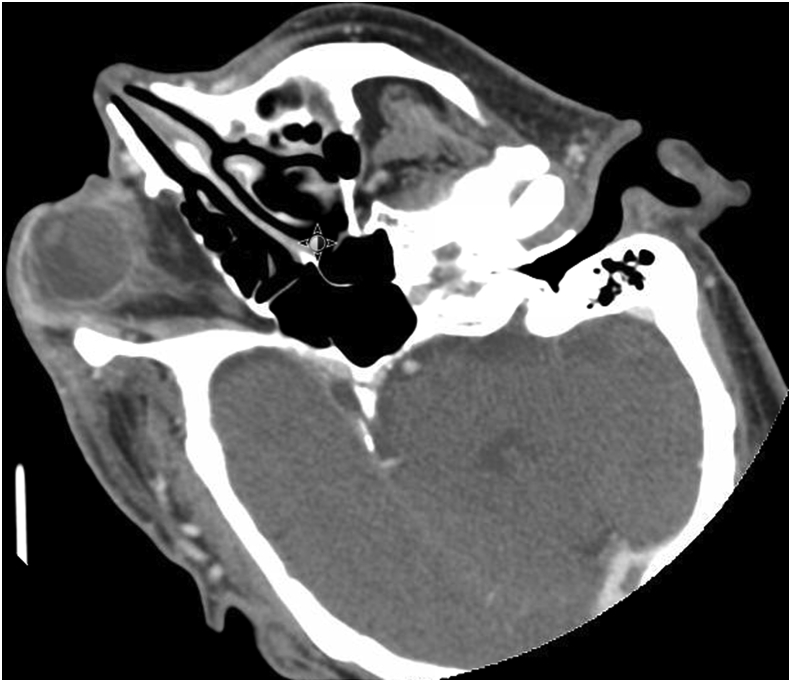
Fig. 2.
CT of the orbits with contrast showed post-septal fat stranding and a hyperdensity in the vitreous cavity in the right eye.
Fig. 3.
B scan ultrasonography of the right eye revealed a choroidal mass with a collar button-shaped configuration.
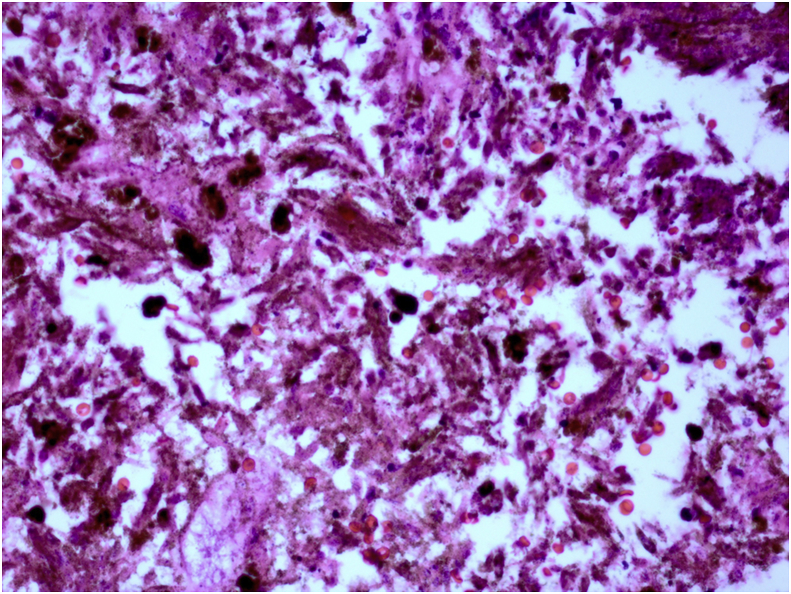
Based on this new diagnosis of a uveal melanoma, enucleation was subsequently performed with a posterior tenonectomy due to intraoperative discovery of extrascleral extension of the tumor involving the posterior Tenon's capsule. Gross inspection of the specimen exhibited old hemorrhage in the vitreous and a 12 mm × 12 mm x 5 mm heavily pigmented mass in the choroid (Fig. 4). Histopathology revealed ischemic necrosis of the iris, a necrotic and partially liquefied retina, and a choroidal tumor composed of necrotic, spindle-shaped cells with fusiform nuclei and spindle-shaped cytoplasm (Fig. 5). A specimen of orbital tissue contained macrophages and a cluster of cells that stained for HMB-45, likely representing a focal infiltrate of melanoma. Gene expression profile testing and chromosomal analysis were not performed. The patient underwent a negative metastatic work-up and an exenteration per family request. Histopathology of the orbital tissue submitted from the exenteration stained negatively for HMB-45.
Fig. 4.
Cross-section of the globe reveals a 12 mm × 12 mm x 5 mm pigmented mass in the choroid.
Fig. 5.
Higher magnification of the necrotic tumor showed that it was composed of heavily pigmented, spindle shaped cells. (hematoxylin and eosin, 100X).
3. Discussion
Ocular inflammation is an atypical presenting feature of necrotic uveal melanoma. In a retrospective study of 450 consecutive enucleations for malignant melanoma of the choroid and ciliary body, Fraser and Font reported that 22 patients (4.9%) initially appeared with ocular inflammation involving some component of episcleritis, anterior uveitis, posterior uveitis, endophthalmitis, or panophthalmitis.1 Orbital cellulitis specifically is an even more uncommon presentation of necrotic uveal melanoma. Only one patient in Fraser and Fonts’ series of 450 patients presented with panophthalmitis with orbital cellulitis.1 There are few reports in the literature describing orbital cellulitis as a presenting feature of a uveal melanoma, and they have been recounted in both cases with and without extraocular tumor extension.2,3
In our patient, in addition to orbital cellulitis, intraocular hemorrhage was also a presenting clinical sign. Fraser and Font investigated the presence of ocular hemorrhage as the initial manifestation of uveal malignant melanomas.1 They found that 13 of the 450 cases presented with intraocular hemorrhage as the initial clinical feature, with only one case displaying both an anterior chamber and vitreous hemorrhage.1 Biswas et al. also reported a case describing a patient with proptosis, lid edema, and chemosis who was later found to have a hyphema with no view to the fundus.4 B-scan ultrasonography revealed a well-defined choroidal mass extending into the vitreous cavity, and the patient was diagnosed with a necrotic uveal mixed cell type melanoma.
Regarding the pathophysiology underlying orbital inflammation in necrotic uveal melanoma, it has been hypothesized that as the tumor outgrows its vascular source, it can undergo necrosis as a result of hypoxia in the watershed area in the center of the tumor.4,5 The process of necrosis in turn releases cytokines and other inflammatory mediators inciting inflammation and features mimicking orbital cellulitis.4 In fact, an association between high levels of macrophages in uveal melanoma and a larger tumor size has been reported.6,7 An inflammatory phenotype of uveal melanoma has also been described which features an increased presence of different types of lymphocytes and macrophages, increased HLA class I and II expression, and association with a loss of one chromosome 3.8 Finally, inflammation associated with uveal melanoma may also be secondary to neovascularization or acute angle closure glaucoma due to anterior displacement of the lens and iris from enlargement of the tumor.9
Imaging techniques such as magnetic resonance imaging (MRI) scans and ultrasound can assist in making the diagnosis of a necrotic uveal melanoma, especially when there is a poor view to the fundus. Eviscerations have been performed in blind, painful eyes later found to have unsuspected uveal melanomas on histopathology, highlighting the importance of obtaining imaging in the evaluation of a blind, painful eye to rule out an intraocular malignancy.10,11 A hyperintense signal on T1-weighted images and a hypointense signal on T2-weighted images are distinctive MRI findings in uveal melanomas.12 B scan ultrasonography is also valuable in visualizing the mass, and the A scan will typically display the characteristic low to medium internal reflectivity of uveal melanomas.12 Orbital computed tomography (CT) scans have also been used to estimate the size of uveal melanomas. However, in certain cases of a necrotic uveal melanoma, there is a failure to detect intraocular tumors with a CT scan due to loss of tumor density secondary to total necrosis of the tumor.13 In our case, the intraocular mass was not detectable upon first glance in the orbital CT likely due to complete necrosis of the tumor.
Regarding the treatment options for orbital invasion of necrotic uveal melanomas, there is currently a lack of a clear set of established guidelines. It is important to evaluate each case individually, assessing the patient's overall health and the degree of extrascleral extension. However, in general, most clinicians lean towards a more conservative approach with a modified enucleation, tenonectomy, or subtotal exenteration in cases with a resectable extension.14 These surgical techniques can also be accompanied by adjuvant radiotherapy, chemotherapy, or immunotherapy. Complete exenteration is considered in cases with massive orbital extension.14 Our patient initially had an enucleation with a tenonectomy performed given the extrascleral extension observed intra-operatively, and then later underwent a lid-sparing exenteration after further discussion with the family.
4. Conclusions
In summary, this case illustrates the importance of keeping necrotic uveal melanoma in the differential diagnosis of a patient presenting with orbital cellulitis and an intraocular hemorrhage. The dramatic presentation of orbital cellulitis can often times draw consideration away from the presence of an underlying intraocular tumor.15 In unfortunate cases, a delay in the diagnosis of uveal melanomas can lead to massive orbital extension at the time of diagnosis.16 While orbital cellulitis is a very rare presenting feature of necrotic uveal melanoma, this report highlights the importance of considering necrotic uveal melanoma in the setting of orbital inflammation and an intraocular hemorrhage.
Patient consent
The patient's legal guardian consented to publication of the case in writing.
Funding
No funding or grant support
Conflicts of interest
The following authors have no financial disclosures: AL, JK, DB, KP, AH.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Fraser D.J., Font R.L. Ocular inflammation and hemorrhage as initial manifestations of uveal malignant melanoma incidence and prognosis. Arch Ophthalmol. 1979;97(7):1311–1314. doi: 10.1001/archopht.1979.01020020053012. [DOI] [PubMed] [Google Scholar]
- 2.Nalcaci S., Melis P., Banu Y. Choroidal malignant melanoma with no extraocular extension presenting as orbital cellulitis. Orbit. 2016;35(5):285–287. doi: 10.1080/01676830.2016.1176216. [DOI] [PubMed] [Google Scholar]
- 3.Nair A.G., Kaliki S., Ali M.J. Intraocular malignant melanoma of the choroid presenting as orbital cellulitis. Int Ophthalmol. 2014;34:647–650. doi: 10.1007/s10792-013-9836-1. [DOI] [PubMed] [Google Scholar]
- 4.Biswas J., Ahuja V.K., Shanmugam M.P. Malignant melanoma of the choroid presenting as orbital cellulitis: report of two cases with a review of the literature. Orbit. 1999;18(2):123–130. doi: 10.1076/orbi.18.2.123.2718. [DOI] [PubMed] [Google Scholar]
- 5.Thareja S., Rashid A., Grossniklaus H.E. Spontaneous necrosis of choroidal melanoma. Ocul Oncol and Pathol. 2015;1:63–69. doi: 10.1159/000366559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makitie T., Summanen P., Tarkkanen A., Kivela T. Tumor-infiltrating macrophages (CD68(+) cells) and prognosis in malignant uveal melanoma. Investig Ophthalmol Vis Sci. 2001;42:1414–1421. [PubMed] [Google Scholar]
- 7.Jager M.J., Ly L.V., El Filali M., Madigan M.C. Macrophages in uveal melanoma and in experimental ocular tumor models: Friends or foes. Prog Retin Eye Res. 2011;30:129–146. doi: 10.1016/j.preteyeres.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Maat W., Ly L.V., Jordanova E.S. Monosomy of chromosome 3 and an inflammatory phenotype occur together in uveal melanoma. Investig Ophthalmol Vis Sci. 2008;49(2):505–510. doi: 10.1167/iovs.07-0786. [DOI] [PubMed] [Google Scholar]
- 9.Rose G.E., Hoh H.B., Harrad R.A., Hungerford J.L. Intraocular malignant melanomas presenting with orbital inflammation. Eye. 1993;7:539–541. doi: 10.1038/eye.1993.117. [DOI] [PubMed] [Google Scholar]
- 10.Eagle R.C., Grossniklaus H.E., Syed N. Inadvertent evisceration of eyes containing uveal melanoma. Arch Ophthalmol. 2009;127(2):141–145. doi: 10.1001/archophthalmol.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pereira P.R., Odashiro A.N., Souza Filho J.P. Malignancy in the blind painful eye–report of two cases and literature review. Diagn Pathol. 2006;1(1):45. doi: 10.1186/1746-1596-1-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fezza J., Chaudhry I.A., Kwon Y.H., Grannum E.E. Orbital melanoma presenting as orbital cellulitis: a clinicopathologic report. Ophthalmic Plast Reconstr Surg. 1998;14(4):286–289. doi: 10.1097/00002341-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Goh A.S., Francis I.C., Kappagoda M.B., Marijian F. Orbital inflammation in a patient with extrascleral spread of choroidal malignant melanoma. Clin Exp Ophthalmol. 2001;29:97–99. doi: 10.1046/j.1442-9071.2001.d01-14.x. [DOI] [PubMed] [Google Scholar]
- 14.Blanco G. Diagnosis and treatment of orbital invasion in uveal melanoma. Can J Ophthalmol. 2004;39(4):388–396. doi: 10.1016/s0008-4182(04)80010-3. [DOI] [PubMed] [Google Scholar]
- 15.Thatcher D.B. Necrotic choroidal melanoma presenting with severe inflammation. Surv Ophthalmol. 1967;12(3):247–253. [PubMed] [Google Scholar]
- 16.Shields J.A., Shields C.L. Massive orbital extension of posterior uveal melanomas. Ophthalmic Plast Reconstr Surg. 1991;7(4):238–251. doi: 10.1097/00002341-199112000-00002. [DOI] [PubMed] [Google Scholar]