Abstract
Introduction
Aneurysms of the extracranial carotid artery are rare. They are often asymptomatic but can lead to disabling stroke. This report describes a case of bilateral internal carotid artery aneurysms in a patient with Marfan syndrome.
Report
A 65 year old woman with Marfan syndrome presented with an asymptomatic swelling in the right anterior triangle of the neck. Imaging revealed bilateral extracranial fusiform internal carotid artery aneurysms. Staged open repair was performed. The right side was repaired by aneurysm excision and primary end to end anastomosis. The left side was repaired with a great saphenous vein interposition graft. The patient is free from aneurysm related complications at six years, although recurrent dilatation is present on surveillance.
Discussion
Internal carotid aneurysms can be managed successfully by open repair. In patients with connective tissue disorders surveillance is required to monitor for post-operative aneurysmal dilatation.
Keywords: Carotid artery aneurysm, Marfan syndrome
Highlights
-
•
Internal carotid artery aneurysms are rare.
-
•
Higher incidence is noted in patients with connective tissue disorders.
-
•
Open repair with primary end to end closure or vein interposition graft are feasible options.
-
•
Surveillance is required in connective tissue disorders patients to monitor for recurrence.
Introduction
Aneurysms of the extracranial carotid artery are rare and represent a small minority of the carotid interventional workload in most vascular units.1 Many aneurysms arise as a consequence of atherosclerosis, trauma, or carotid artery intervention.2 They are often asymptomatic or may present with transient ischaemic attacks or stroke from distal embolisation or luminal stenosis. Spontaneous aneurysm rupture is rare. Secondary symptoms due to local nerve compression can present with dysphagia, and changes in voice or from facial swelling due to venous congestion. Management strategies include an open surgical approach, aneurysm excision, and either primary closure or use of autologous or prosthetic conduits. Endovascular approaches with carotid stenting are also described. The optimal management strategy is unclear as the natural history and risks of intervention are poorly understood.
The case of a 65 year old woman with Marfan syndrome presenting with asymptomatic bilateral extracranial internal carotid artery (ICA) aneurysms is reported. The operative procedure, outcome, follow up, and review of the published literature are described.
Case report
A 65 year old woman with Marfan syndrome presented to the otolaryngology service with asymptomatic swelling in the right anterior triangle of the neck (Fig. 1). The medical history included hypertension, dyslipidaemia, a small abdominal aortic aneurysm, and a type B aortic dissection managed by best medical therapy, with excellent aortic remodelling and no aneurysmal dilatation on computed tomography (CT) surveillance imaging.
Figure 1.
Right anterior neck swelling.
She underwent ultrasound imaging of the neck, which revealed bilateral carotid artery aneurysms and was referred to a tertiary vascular surgery unit. CT angiography revealed bilateral extracranial fusiform ICA aneurysms (Fig. 2), with significant tortuosity and thrombus. The maximum diameters were 3.5 cm on the right and 3.1 cm on the left. There was considerable thrombus within the left ICA. CT imaging of the brain did not reveal any intracranial aneurysms or evidence of stroke.
Figure 2.
Pre-operative computed tomography angiography.
Following extensive multidisciplinary team discussion and consultation with the patient, a shared decision was made to proceed with open repair of the ICA aneurysms, with the aim of reducing the risk of stroke and rupture. The patient had a good understanding of the complications associated with Marfan syndrome and was keen on intervention. Given the significant vessel tortuosity an endovascular approach was not considered optimal, so staged open surgical repairs were performed.
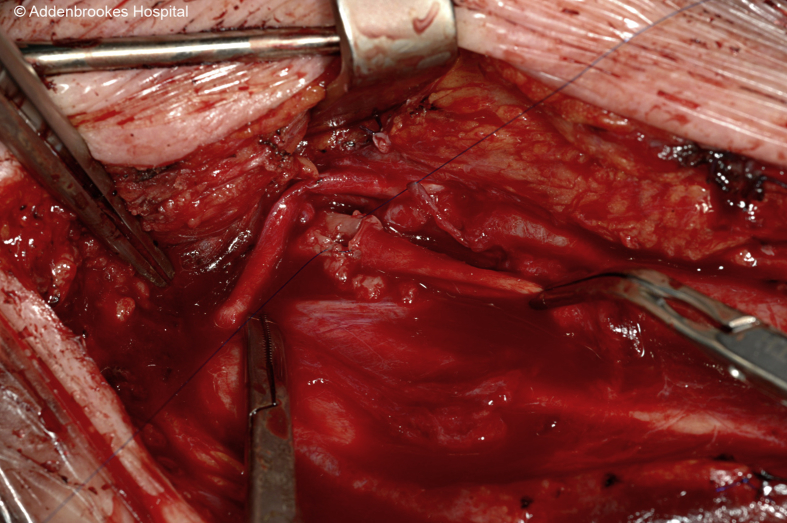
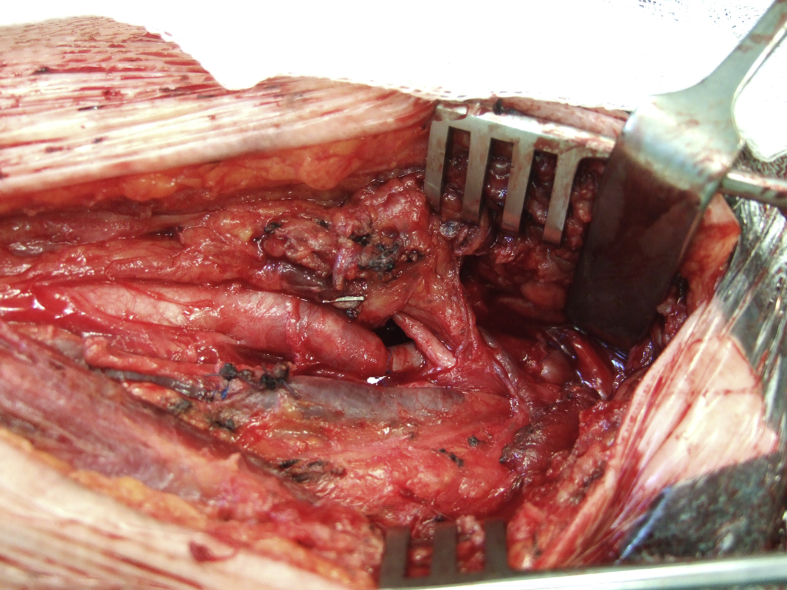
In view of the larger aneurysm size and greater prominence, the right ICA aneurysm was repaired first. Under general anaesthesia, with nasotracheal intubation and transcranial Doppler (TCD) monitoring, a standard oblique neck incision was made to expose the common, external, and internal carotid arteries proximal and distal to the aneurysm. The hypoglossal nerve was clearly visualised draped over the aneurysm sac (Fig. 3) and was mobilised to permit access for clamp placement (Fig. 4). Middle cerebral blood flow was maintained on TCD after clamp application and an excellent pulse was palpable; hence, no shunt was used. The aneurysm sac was excised and the ICA tortuosity permitted an end to end reconstruction (Fig. 5). The patient made an uneventful recovery and was discharged on post-operative day two. After four months and assessment of the vocal cords by fibreoptic naso-endoscopy, the patient underwent treatment of the left ICA aneurysm. An identical surgical approach was performed, although the ICA dilatation extended more distally on the left side. Therefore, the digastric muscle was divided to permit greater distal access. The aneurysm sac was excised and an autologous great saphenous vein interposition graft was used to reconstruct the artery (Fig. 6). The patient had transient dysphagia, but this settled, and she was discharged on post-operative day five.
Figure 3.
Hypoglossal nerve overlying the right internal carotid artery aneurysm.
Figure 4.
Tortuous right internal carotid artery aneurysm.
Figure 5.
Right internal carotid artery after aneurysm excision and end to end anastomosis.
Figure 6.
Left internal carotid artery aneurysm managed by great saphenous vein interposition graft.
She was seen at nine months and colour duplex imaging revealed excellent flow in both reconstructions, with no dilatation. Subsequent carotid duplex at three years showed some aneurysmal changes in the left ICA at 1.9 cm × 2cm.
The patient had an unrelated acute left posterior frontal intraparenchymal haemorrhage four years post-operatively, which was managed conservatively with rehabilitation. There were no aneurysm related complications at the six year follow up.
Discussion
The most common cardiovascular manifestation seen in patients with Marfan syndrome is progressive aortic root enlargement progressing to aneurysmal change.3 However, given the connective tissue defect, it is conceivable that aneurysmal change may occur in various arterial territories. Aneurysmal change of the ICA in patients with connective tissue disorders has been reported but is commonly due to false aneurysm formation.4 This is the first reported case of bilateral ICA true aneurysms in a patient with Marfan syndrome, as only unilateral pathology has been described previously.5
Extracranial internal carotid aneurysms present with symptoms and signs of cerebrovascular insufficiency secondary to thrombo-embolism, or with signs related to local compression, such as involvement of the recurrent laryngeal nerve, vagus nerve, or facial nerve.6 However, aneurysms may remain asymptomatic or present as a neck swelling, as in this case. Furthermore, there is a small risk of aneurysm rupture. There is no agreed consensus as to when to consider treatment of an extracranial internal carotid aneurysm as the relationship between complications and size has yet to be defined.7
Treatment is dependent on local aneurysm anatomy. Typically, open surgical treatment involving resection and reconstruction has been used in the treatment of carotid aneurysms;8 open placement of clips has also been undertaken.9 Although the role of endovascular treatment has been explored, it has been suggested that this route is safe when it is technically possible to undertake the procedure.10 In the present patient, the multidisciplinary consensus selected an open repair in staged manner given the size and, in particular the angulation of the left ICA.
Recurrence of aneurysmal dilatation was noted at three years on the left side. Therefore, in patients with connective tissue disorders, follow up by duplex sonography is important as, owing to the underlying nature of the disease, recurrence should be expected. Prior to intervention, patients should be counselled regarding the risk of recurrence and the requirement for long term surveillance.
Bilateral ICA aneurysms are rare; however, treatment is required to prevent disabling sequelae such as stroke, stenosis, or rupture.
Conflict of interest
None.
Funding sources
None.
References
- 1.Pulli R., Dorigo W., Alessi Innocenti A., Pratesi G., Fargion A., Pratesi C. A 20-year experience with surgical management of true and false internal carotid artery aneurysms. Eur J Vasc Endovasc Surg. 2013;45:1–6. doi: 10.1016/j.ejvs.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Longo G.M., Kibbe M.R. Aneurysms of the carotid artery. Semin Vasc Surg. 2005;18:178–183. doi: 10.1053/j.semvascsurg.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Milewicz D.M., Dietz H.C., Miller D.C. Treatment of aortic disease in patients with Marfan syndrome. Circulation. 2005;111:e150–e157. doi: 10.1161/01.CIR.0000155243.70456.F4. [DOI] [PubMed] [Google Scholar]
- 4.Kim S.T., Brinjikji W., Lanzino G., Kallmes D.F. Neurovascular manifestations of connective-tissue diseases: a review. Interv Neuroradiol. 2016;22:624–637. doi: 10.1177/1591019916659262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Latter D.A., Ricci M.A., Forbes R.D., Graham A.M. Internal carotid artery aneurysm and Marfan's syndrome. Can J Surg. 1989;32:463–466. [PubMed] [Google Scholar]
- 6.Kaczynski J., Wilczynska M., Blaszczynski M., Fligelstone L. Extracranial saccular atherosclerotic aneurysm of the internal carotid artery (ICA) treated by an oblique end-to-end primary anastomosis. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-007705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huyzer M., Reijnen M.M., Sybrandy J.E., Buth J., Zeebregts C.J. Interposition grafting of large extracranial carotid aneurysm. Tex Heart Inst J. 2011;38:52–55. [PMC free article] [PubMed] [Google Scholar]
- 8.Attigah N., Külkens S., Zausig N., Hansmann J., Ringleb P., Hakimi M. Surgical therapy of extracranial carotid artery aneurysms: long-term results over a 24-year period. Eur J Vasc Endovasc Surg. 2009;37:127–133. doi: 10.1016/j.ejvs.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Rana N.R., Hodgson K.J., Ramsey D., Johnson C.M. Management approach to an extracranial internal carotid artery aneurysm. J Vasc Surg. 2013;57:526. doi: 10.1016/j.jvs.2011.11.101. [DOI] [PubMed] [Google Scholar]
- 10.Li Z., Chang G., Yao C., Guo L., Liu Y., Wang M. Endovascular stenting of extracranial carotid artery aneurysm: a systematic review. Eur J Vasc Endovasc Surg. 2011;42:419–426. doi: 10.1016/j.ejvs.2011.05.008. [DOI] [PubMed] [Google Scholar]