Abstract
While peripheral neuropathy is the most common complication of long-term diabetes, cognitive deficits associated with encephalopathy and myelopathy also occur. Diabetes is a risk factor for Alzheimer disease (AD) and increases the risk of progression from mild cognitive impairment to AD. The only current recommendation for preventing or slowing the progression of peripheral neuropathy is to maintain close glycemic control, while there is no recommendation for central nervous system disorders. NSI-189 is a new chemical entity that when orally administered promotes neurogenesis in the adult hippocampus, increases hippocampal volume, enhances synaptic plasticity, and reduces cognitive dysfunction. To establish the potential for impact on peripheral neuropathy, we first showed that NSI-189 enhances neurite outgrowth and mitochondrial functions in cultured adult rat primary sensory neurons. Oral delivery of NSI-189 to murine models of type 1 (female) and type 2 (male) diabetes prevented multiple functional and structural indices of small and large fiber peripheral neuropathy, increased hippocampal neurogenesis, synaptic markers and volume, and protected long-term memory. NSI-189 also halted progression of established peripheral and central neuropathy. NSI-189, which is currently in clinical trials for treatment of major depressive disorder, offers the opportunity for the development of a single therapeutic agent against multiple indices of central and peripheral neuropathy.
Introduction
Small fiber neuropathy, as detected by quantitative sensory testing, skin biopsy specimen, or corneal confocal microscopy, is an early feature of diabetic peripheral neuropathy, while large myelinated fiber dysfunction is detected as slowing of conduction velocity (1,2). It is increasingly recognized that diabetes also affects the central nervous system (CNS) (3,4), with cognitive dysfunction reported in patients with type 1 (5) and type 2 (6,7) diabetes supporting a growing consensus that diabetes is a risk factor for cognitive impairment and Alzheimer disease (3,8,9).
Preclinical studies have identified multiple mechanisms that may contribute to diabetic peripheral neuropathy (10). However, clinical recommendations remain restricted to maintaining glycemic control (2). Moreover, although reduced cognitive function, synaptic plasticity, and brain volume also occur in rodent models of diabetes (11,12), there have been few preclinical or clinical attempts to prevent or reverse CNS dysfunction. Insulin and C-peptide, acting in their neuroprotective capacities, both ameliorate multiple indices of peripheral neuropathy and encephalopathy (12–14), and ideal therapeutics would similarly target both peripheral nervous system (PNS) and CNS damage. The potential for neuroprotection to extend throughout the nervous system led us to hypothesize that drugs that are neuroprotective in CNS neurodegenerative diseases might be effective against diabetes-induced damage to both the CNS and PNS.
NSI-189 is an orally active benzylpiperizine-aminopyridine that stimulates neurogenesis, synaptogenesis, and increased hippocampal volume in mice (15), demonstrates long-term neurogenic capacity in a rat model of ischemic stroke (16), ameliorates cognitive impairment in rats with irradiation-induced brain injury (17), and enhances synaptic plasticity and cognitive function in a mouse model of Angelman syndrome (18). A double-blind phase Ib safety study in patients with major depressive disorder demonstrated that oral NSI-189 was safe and had significant long-acting antidepressant and procognitive effects (19), with efficacy recently confirmed in a phase II double-blind placebo-controlled study (20). The known safety profile and emerging efficacy profile of NSI-189 prompted us to evaluate its ability to stimulate peripheral neurons and impact central and peripheral neuropathy in rodent models of diabetes.
Research Design and Methods
Sensory Neuron Cultures
Dorsal root ganglia (DRG) from normal and 3- to 4-month streptozotocin (STZ)-induced diabetic adult male Sprague-Dawley rats were dissociated as previously described (21), and sensory neurons were cultured in insulin-free defined Hams F12 media containing 10 mmol/L or 25 mmol/L (cells from control or diabetic rats, respectively) d-glucose. Total neurite outgrowth has been directly related to an arborizing form of axonal plasticity homologous to in vivo collateral sprouting (22).
Mitochondrial Respiration
An XF24 Analyzer (Seahorse Biosciences, Billerica, MA) was used to measure basal mitochondrial oxygen consumption, maximal respiration, spare respiratory capacity, and nonmitochondrial oxygen consumption of sensory neurons in culture (21).
Estimation of Pharmacokinetic Properties and Bioavailability in Mouse
Male C57Bl/6J mice were administered NSI-189 by oral gavage or intravenous injection. Plasma and snap-frozen brains were collected at eight time points for analysis of NSI-189 levels by liquid chromatography–tandem mass spectrometry assay (19).
Animals
Experiments were performed in adult female Swiss Webster mice (Harlan, Indianapolis, IN), adult male C57/BLKS/J and C57BLKS|BKS.Cg-Dock7m+/+ Leprdb/J (also called db/db) mice (stock nos. 000662 and 000642; The Jackson Laboratory, Bar Harbor, ME), and adult male Sprague-Dawley rats (University of Manitoba). Rats were housed in pairs and mice four to five per cage with free access to water and food (RMH300 for rats [LabDiet, St. Louis, MO] and 5001 PMI diet for mice [Harlan]). Studies followed protocols approved by the Institutional Animal Care and Use Committee of the University of California, San Diego, and by the University of Manitoba Animal Care Committee following Canadian Council of Animal Care rules.
Type 1 diabetes was induced by injection of STZ (90 mg/kg) (Sigma-Aldrich, St. Louis, MO) that was freshly dissolved in 0.9% sterile saline and administered after an overnight fast as a single injection to rats or on two consecutive days to mice. Hyperglycemia was measured using a test strip and meter for rats (AlphaTrak 2; Zoetis, Parsippany, NJ) and OneTouch Ultra for mice (Lifescan, Milpitas, CA) in a blood sample obtained 4 days after STZ injection. Rodents with blood glucose >270 mg/dL were accepted as diabetic. This regimen does not produce direct STZ-induced neurotoxicity in mice (23) or rats (24). One group of STZ-diabetic mice received subcutaneous implants of slow-release insulin pellets (three pellets/mouse, release rate 0.1 units/24 h) (LinBits; LinShin Canada, Toronto, Ontario, Canada) at the onset of diabetes, with additional pellets implanted as needed.
Type 2 diabetes was modeled using db/db mice, which develop impaired leptin receptor function leading to polyphagia, obesity, insulin resistance, hyperinsulinemia, and mild-moderate hyperglycemia by 6–8 weeks of age.
Drugs
NSI-189 phosphate, (4-benzylpiperazin-1-yl)-[2-(3-methylbutylamino)pyridin-3-yl] methanone, was provided by Neuralstem, Inc., and first dissolved in 0.2 N HCl and then diluted 1:10 with distilled water (pH 4–5). NSI-189 or vehicle (0.02 N HCl, pH 4–5) was administered daily by oral gavage. Unless noted, assays were performed 24 h after the most recent treatment to preclude detection of transient effects. For cell culture, NSI-189 phosphate was dissolved in 100% DMSO.
Behavioral Assays
Memory Tests
The object recognition test was performed to assess short-term (1-h) memory without the requirement of an acquisition phase. After exposure to two similar objects, the amount of time taken to explore the new object provides an index of recognition memory. Long-term memory was assessed using the Barnes maze (11). Mice were placed on the Barnes maze and allowed to locate the escape box on five consecutive days to facilitate learning (acquisition phase). The test was repeated 4 weeks later to assess long-term memory of the learned behavior (retention phase).
Tactile Responses
Paw responsiveness to light touch was measured using von Frey filaments (25). Both hind paws were tested, and the mean was used to represent the 50% paw withdrawal threshold (PWT).
Thermal Responses
Paw withdrawal from heat was measured using a thermal testing apparatus (UARD, San Diego, CA). Both hind paws were tested three times at 5-min intervals. The median response time for each paw was calculated and the mean of the two medians used to represent each mouse (25).
Electrophysiology
Motor nerve conduction velocity (MNCV) was measured in the sciatic nerve–interosseus muscle system of isoflurane-anesthetized animals (25). Three measurements were made per mouse, and MNCV was calculated using the median value and distance between the stimulation points.
Epidermal Nerve Visualization and Quantification
Animals were killed, and the hind paw plantar skin was removed into 4% paraformaldehyde for 24 h. Samples were embedded in paraffin and cut as 6-μm sections before incubation with antibodies against the panneuronal marker PGP 9.5 (1:1,000; Biogenesis Ltd., Poole, U.K.). Slides were coded and epidermal PGP9.5 immunoreactive profiles quantified by light microscopy (25).
Corneal Nerve Visualization and Quantification
Mice were anesthetized with isoflurane and placed in a custom-designed imaging platform connected to a Heidelberg Retina Tomograph 3 with the Rostock Corneal Module (Heidelberg Engineering, Heidelberg, Germany). The image collecting procedure has previously been described (25). Nerve occupancy or the total nerve length, traced using ImageJ software, was calculated for five sequential images (2-µm spacing) of the subbasal plexus.
Neurogenesis and Hippocampal Volume
Mice received an intraperitoneal injection of BrdU (Sigma-Aldrich) in PBS (pH 7.2) every 8 h over 72 h prior to study termination. Animals were sacrificed 3 h after the last BrdU injection and perfused with 4% paraformaldehyde. BrdU-positive cells represent neurogenesis as BrdU incorporates into the newly synthesized DNA of replicating cells (26). Hippocampal sections (40 µm) were viewed using a Nikon AZ100 light microscope, BrdU-positive cells were counted, and hippocampal volume was measured by tracing (17).
Western Blotting
Hippocampi were homogenized in buffer (50 mmol/L Tris-HCl [pH 7.4], 150 mmol/L NaCl, 0.5% Triton X, 1 mmol/L EDTA, protease inhibitor cocktail), processed, and separated on 4–12% SDS-PAGE Bis-Tris gels (Novex; Invitrogen, Carlsbad, CA) as described previously (11). Blots were incubated with antibodies against NeuN (1:1,000; Millipore), synaptophysin (1:10,000; Millipore), PSD95 (1:500; Chemicon), BDNF (1:1,000; Abcam), or actin (1:5,000; Sigma-Aldrich), followed by the corresponding secondary antibodies tagged with infrared dyes (IRDye, 1:15,000; LI-COR Biosciences, Lincoln, NE).
Data Analysis
All animals and tissues were coded during assay to prevent observer bias. Data are presented as group mean ± SD. Statistical comparisons were made by one-way or repeat ANOVA with between-group differences identified using the Dunnett post hoc test.
Data and Resource Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request. The compound NSI-189 that supports the findings of this study is available from Neuralstem, Inc./Dr. Karl Johe. NSI-189 may be available from the authors and/or Neuralstem, Inc., upon reasonable request and with permission of Neuralstem, Inc.
Results
Adult Sensory Neurons In Vitro
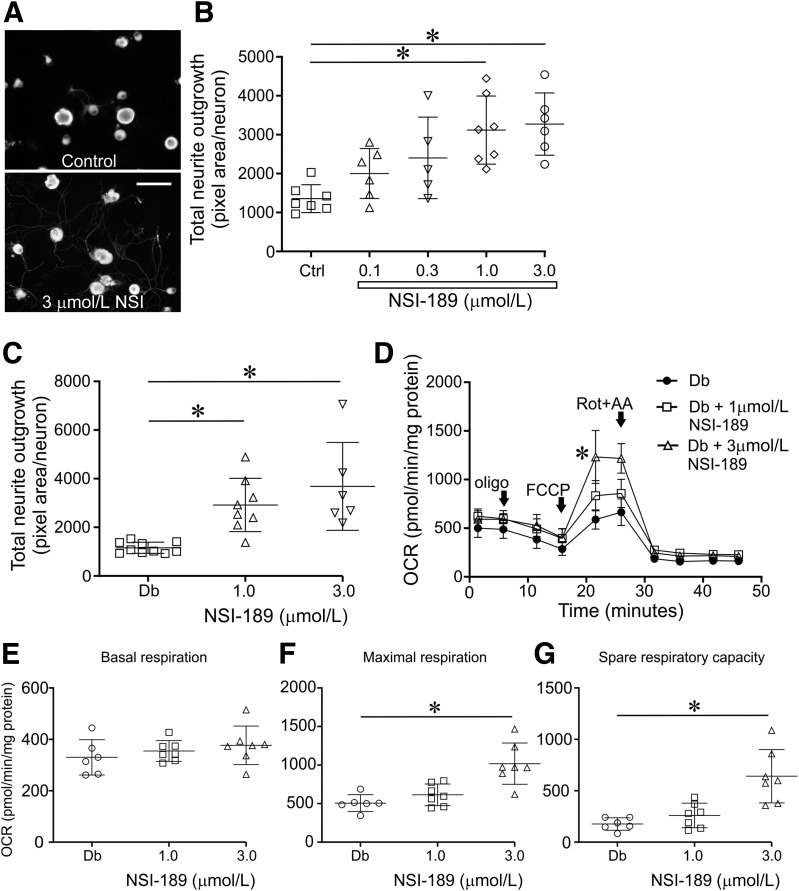
NSI-189 (1.0–3.0 µmol/L) significantly increased 24 h total neurite outgrowth in neurons from normal or diabetic rats (Fig. 1A–C). Mitochondrial function was assessed in sensory neurons from control (Supplementary Fig. 1) and STZ-diabetic rats using the Seahorse XF24 analyzer and sequential addition of uncouplers and inhibitors (Fig. 1D). Basal respiration in neurons from control or diabetic rats was unchanged by NSI-189 (Fig. 1E and Supplementary Fig. 1). Maximal respiration and spare respiratory capacity were significantly (P < 0.05) increased after 24-h exposure to NSI-189 in neurons from diabetic rats (Fig. 1F and G) and trended upward in neurons from control rats (Supplementary Fig. 1).
Figure 1.
NSI-189 augments neurite outgrowth and mitochondrial function in adult rat DRG sensory neurons. A and B: Effect of NSI-189 on neurite outgrowth from normal neurons (n = 5–7 replicate cultures). C: Effect of NSI-189 on DRG neurons derived from a 3- to 4-month STZ-induced diabetic rat (n = 6–10 replicate cultures). D: Seahorse XF24 trace showing oxygen consumption rate (OCR) of neurons from diabetic rats treated for 24 h with 1.0 or 3.0 μmol/L NSI-189. The following drugs were added: oligomycin (oligo), carbonyl cyanide-4-(trifluoromethoxy)phenylhydrazone (FCCP), and rotenone + antimycin A (Rot+AA) . Basal respiration (E), maximal respiration (F), and spare respiratory capacity (G) derived from D (n = 6–7 replicate cultures). Data are mean ± SD. *P < 0.05, **P < 0.01 by one-way ANOVA, followed by the Dunnett post hoc test.
Drug Distribution in Normal Mice
The brain-to-plasma ratio of the NSI-189 distribution area under the curve (AUC0-t) was well above the minimal penetration limit of 0.04 at all doses and routes, indicating good brain penetration. NSI-189 penetrated the brain rapidly, with maximal concentrations (Tmax) observed at initial sampling, 8 min after intravenous (i.v.) administration (Table 1). Tmax occurred 18–30 min after oral (per os [po]) dosing, and the absolute oral bioavailability (Fabs) of NSI-189 phosphate in the brain at 10 mg/kg was 20% (Fabs = 100 × [AUCpo/AUCi.v.]).
Table 1.
Pharmacokinetics parameters after intravenous or oral delivery of NSI-189 to normal mouse
| Dose (mg/kg) | Tmax (h) | Cmax (ng/mL) | AUC0–t (ng∗h/mL) | |
|---|---|---|---|---|
| Intravenous delivery | ||||
| Plasma | 1 | 0.083 | 215 | 172 |
| 3 | 0.083 | 858 | 625 | |
| 10 | 0.083 | 3,014 | 2,135 | |
| Brain | 1 | 0.13 | 298 | 165 |
| 3 | 0.13 | 654 | 522 | |
| 10 | 0.13 | 2,280 | 1,278 | |
| Oral delivery | ||||
| Plasma | 10 | 0.5 | 116 | 105 |
| 30 | 0.25 | 270 | 420 | |
| Brain | 10 | 0.5 | 78 | 258 |
| 30 | 0.3 | 170 | 425 |
Type 1 Diabetes: Prevention Study
Promising in vitro data (Fig. 1) prompted us to investigate efficacy of NSI-189 against indices of neuropathy in both the CNS and PNS of the STZ-induced diabetic mouse model of type 1 diabetes, as this model develops encephalopathy, impaired cognitive functions, and multiple indices of peripheral neuropathy (11,25). Female STZ-diabetic mice were treated with vehicle or NSI-189 (10 mg/kg/day) from onset of diabetes for 16 weeks, with a group of mice treated with insulin (0.1 units/24 h) included as a positive control. Vehicle-treated diabetic mice had elevated blood glucose and HbA1c levels at study end that were lowered by insulin therapy but not NSI-189 (Table 2).
Table 2.
Impact of diabetes and NSI-189 on terminal systemic parameters in mice
| N | Body weight | Blood glucose | Blood HbA1c | Blood HbA1c | Deaths during study | |
|---|---|---|---|---|---|---|
| (g) | (mg/dL) | (%) | (mmol/mol) | |||
| Type 1: Prevention | ||||||
| Control + vehicle | 10 | 32.4 ± 4.7* | 153 ± 26*** | 3.1 ± 0.2*** | 10.1 ± 2.7*** | 0 |
| STZ + vehicle | 9 | 28.4 ± 3.0 | 562 ± 17 | 6.1 ± 0.2 | 43.6 ± 2.3 | 1 |
| STZ + insulin | 8 | 29.2 ± 2.2 | 215 ± 132*** | 4.0 ± 0.8*** | 19.9 ± 8.4*** | 2 |
| STZ + NSI-189 | 9 | 29.9 ± 2.2 | 567 ± 43 | 6.3 ± 0.7 | 45.9 ± 7.1 | 1 |
| Type 1: Intervention | ||||||
| Control + vehicle | 10 | 31.6 ± 2.2*** | 118 ± 12*** | ND | ND | 0 |
| STZ + vehicle | 10 | 25.9 ± 2.1 | 559 ± 47 | ND | ND | 0 |
| STZ + NSI-189 | 9 | 27.5 ± 1.7 | 589 ± 16 | ND | ND | 1 |
| Type 2: Prevention | ||||||
| WT + vehicle | 10 | 29.6 ± 1.7*** | 143 ± 24** | 4.1 ± 0.2*** | 21.3 ± 1.9*** | 0 |
| WT + NSI-189 | 10 | 29.6 ± 1.5*** | 161 ± 20** | 4.2 ± 0.2*** | 21.6 ± 1.8*** | 0 |
| db/db + vehicle | 10 | 62.6 ± 7.2 | 307 ± 180 | 5.7 ± 1.4 | 38.9 ± 15.7 | 0 |
| db/db + NSI-189 | 8 | 66.2 ± 2.9 | 189 ± 19* | 5.1 ± 0.9 | 31.8 ± 10.0 | 2 |
| Type 2: Intervention | ||||||
| WT + vehicle | 10 | 30.2 ± 1.2*** | 167 ± 9*** | ND | ND | 0 |
| db/db + vehicle | 10 | 54.8 ± 8.0 | 439 ± 61 | ND | ND | 0 |
| db/db + NSI-189 | 10 | 55.6 ± 5.3 | 483 ± 71 | ND | ND | 0 |
Data are mean ± SD. Statistical comparison by one-way ANOVA with the Dunnett post hoc test. ND, not determined.
*P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle-treated diabetic mice.
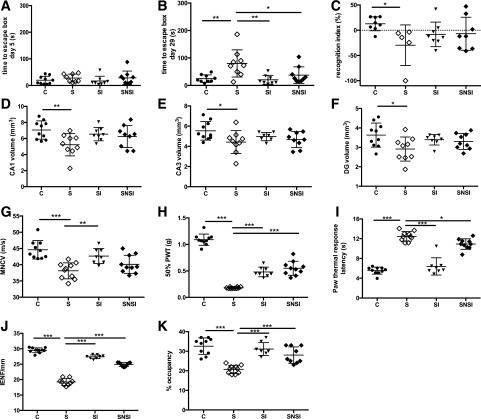
The acquisition phase of the Barnes maze test was performed during week 11, and retention was tested 4 weeks later to assess long-term memory. All groups of mice exhibited similar performance on the last day of the acquisition phase (Fig. 2A). Vehicle-treated diabetic mice had impaired short-term (Fig. 2C) and long-term (Fig. 2B) memory retention, accompanied by significant (P < 0.05) reductions in hippocampal cornu ammonis (CA)1, CA3, and dentate gyrus (DG) volume compared with control mice (Fig. 2D–F). Treatment with insulin or NSI-189 significantly protected long-term memory (P < 0.01 and P < 0.05 vs. vehicle-treated diabetic mice, respectively) and attenuated reductions in the volume of the CA1 and DG regions so that values were not different from control or untreated diabetic mice. In contrast, neither treatment significantly improved short-term memory or the reduced volume of the CA3 region (Fig. 2C and E).
Figure 2.
NSI-189 prevents PNS and CNS neuropathy in type 1 diabetic mice. A: Acquisition phase in the Barnes maze (day 5 of training, week 11 of diabetes and treatment). B: Memory retention (week 15 of diabetes and treatment). C: Short-term memory using the object recognition test after 16 weeks of diabetes. CA1 volume (D), CA3 volume (E), DG volume (F), MNCV (G), paw tactile 50% PWT (H), paw thermal response latency (I), paw IENF density (J), and nerve density in the corneal subbasal plexus (K) after 16 weeks of diabetes and treatment. C, control mice treated daily with vehicle; S, STZ mice treated daily with vehicle; SI, STZ mice with insulin pellet; SNSI, STZ mice treated daily with oral NSI-189. Data are mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA, followed by the Dunnett post hoc test (n = 8–10/group).
At study end, STZ-diabetic mice showed multiple functional and structural indices of peripheral neuropathy, including MNCV slowing, paw tactile allodynia, paw heat hypoalgesia, reduced paw intraepidermal nerve fiber (IENF) density, and reduced corneal nerve density in the subbasal nerve plexus (all P < 0.001 vs. control mice) (Fig. 2G–K). Insulin or NSI-189 significantly prevented or attenuated all deficits, although in the case of MNCV slowing, the effect of NSI-189 did not reach statistical significance.
Type 1 Diabetes: Intervention Study
Female mice were treated with vehicle or NSI-189 (10 mg/kg/day) for the last 8 weeks of a 16-week period of diabetes, with indices of peripheral nerve function measured throughout to assess reversal of established neuropathy. NSI-189 treatment did not alter the lower body weight or hyperglycemia of STZ-diabetic mice (Table 2).
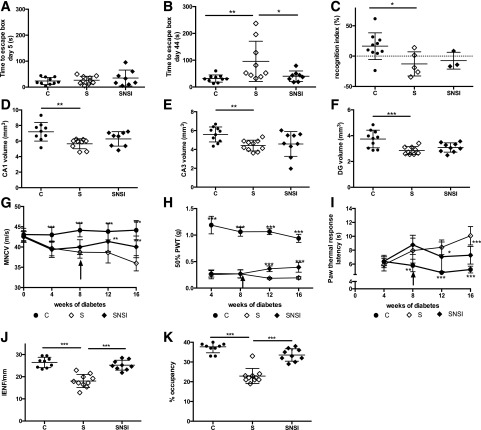
The acquisition phase of the Barnes maze test was performed during week 11 and retention tested 5 weeks later. All groups of mice showed similar performance on the last day of the acquisition phase (Fig. 3A). Five weeks later, vehicle-treated diabetic mice showed significantly (P < 0.01) impaired long-term memory retention (Fig. 3B) compared with control mice. This was accompanied by significant (P < 0.01) reductions in hippocampal CA1 and DG volume compared with control mice (Fig. 3D–F). Treatment with NSI-189 protected long-term memory but had minimal effect on the reductions in CA1 and DG volume and no effect on short-term memory or CA3 volume (Fig. 3C and E).
Figure 3.
NSI-189 ameliorates CNS and PNS neuropathy in type 1 diabetic mice. A: Acquisition phase in the Barnes maze (day 5 of training, week 10 of diabetes, week 2 of treatment). B: Memory retention in the Barnes maze (week 16 of diabetes, week 8 of treatment). C: Short-term memory using the object recognition test after 16 weeks of diabetes. CA1 (D), CA3 (E), and DG (F) volume after 16 weeks of diabetes, 8 weeks of treatment. MNCV (G), paw tactile 50% PWT (H), paw thermal response latency (I), paw IENF density (J), and nerve density of the corneal subbasal plexus (K) after 16 weeks of diabetes, 8 weeks of treatment. C, control mice treated daily with vehicle; S, STZ mice treated daily with vehicle; SNSI, STZ mice treated daily with oral NSI-189. Data are mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA, followed by the Dunnett post hoc test, for panels A–F, J, and K. *P < 0.05, **P < 0.01, ***P < 0.001 vs. STZ + vehicle mice by repeated-measures ANOVA, followed by the Dunnett post hoc test, for panels G–I (n = 9–10/group).
STZ-diabetic mice developed progressive MNCV slowing, early and consistent tactile allodynia, and progressive thermal hypoalgesia, all of which were established after 8 weeks of diabetes (Fig. 3G–K). Intervention with NSI-189 for a further 8 weeks halted progression of these indices of peripheral neuropathy, such that by study end, values were significantly different from vehicle-treated diabetic mice, while also being significantly different from controls. Vehicle-treated STZ-diabetic mice also showed significantly reduced paw skin IENF density (Fig. 3J) and occupancy (Fig. 3K) in the corneal subbasal nerve plexus that was attenuated by NSI-189 treatment.
Type 2 Diabetes: Prevention Study
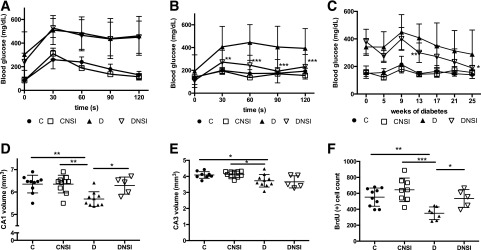
We extended studies to the db/db mouse model of type 2 diabetes to model the most common form of diabetes. Homozygotes develop multiple indices of peripheral neuropathy and encephalopathy but are not viable in memory assays due to obesity (Table 2) that limits ambulation. Male control and db/db mice were treated with NSI-189 (30 mg/kg/day) or vehicle from onset of diabetes (7–8 weeks of age) for 26 weeks. NSI-189 had no impact on body weight, nonfasting blood glucose levels, or glucose clearance following oral glucose delivery of control mice. NSI-189 was also without effect on elevated body weight (Table 2) and impaired blood glucose clearance of db/db mice in early stages (8 weeks) of diabetes (Fig. 4A). However, a decline in nonfasted blood glucose of db/db mice in the terminal stages of the study was accelerated by NSI-189 (Fig. 4C), while impaired glucose clearance was significantly improved by NSI-189 after 25 weeks of diabetes (Fig. 4B).
Figure 4.
Oral glucose tolerance test in db/db mice after 8 weeks of diabetes (A) and after 25 weeks of diabetes and treatment (B). C: Blood glucose levels for db/db mice with NSI-189 treatment starting at onset of diabetes. CA1 (D) and CA3 (E) volume and BrdU-positive cells (F) counted in the hippocampus after 26 weeks of diabetes and treatment. C, control mice treated daily with vehicle; CNSI, control mice treated daily with NSI-189; D, db/db mice treated daily with vehicle; DNSI, db/db mice treated daily with oral NSI-189. Data are mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 against db/db + vehicle by repeated-measures ANOVA, followed by the Dunnett post hoc test, for panels A–C (n = 8–10/group). *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA, followed by the Dunnett post hoc test, for panels D–F (n = 5–10/group).
Histological examination of the hippocampus showed that vehicle-treated db/db mice had significantly (P < 0.01) reduced CA1 volume (Fig. 4D) and a trend to reduced CA3 volume (Fig. 4E) accompanied by a significantly (P < 0.01) reduced number of BrdU-positive cells (Fig. 4F). NSI-189 treatment of db/db mice prevented loss of CA1 volume and increased BrdU-positive cell number, while having no effect on CA3 volume or any measured parameter of control mice.
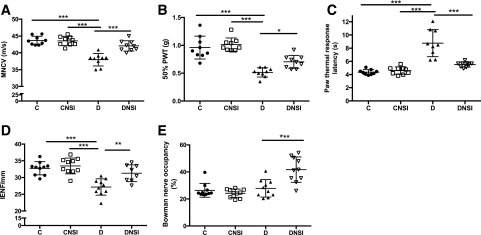
At study end, vehicle-treated db/db mice showed multiple indices of peripheral neuropathy (Fig. 5A–D), all of which were prevented by NSI-189. While db/db mice showed no loss of corneal nerve density in the subbasal nerve plexus compared with control mice, NSI-189 promoted a significant increase in corneal nerve density in the diabetic mice (P < 0.001 vs. vehicle-treated db/db mice) (Fig. 5E).
Figure 5.
NSI-189 prevents peripheral neuropathy in db/db mice. MNCV (A), paw tactile 50% PWT (B), paw thermal response latency (C), paw IENF density (D), and corneal subbasal nerve plexus density (E) after 26 weeks of diabetes and treatment. C, control mice treated daily with vehicle; CNSI, control mice treated daily with NSI-189; D, db/db mice treated daily with vehicle; DNSI: db/db mice treated daily with oral NSI-189. Data are mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA, followed by the Dunnett post hoc test (n = 8–10/group).
Type 2 Diabetes: Intervention Study
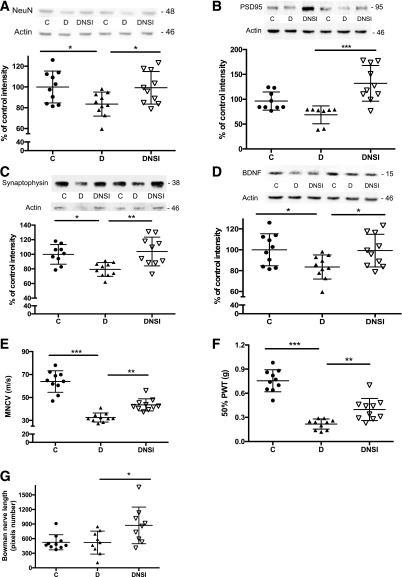
At 16 weeks of age (8 weeks of untreated diabetes), male db/db mice had developed peripheral neuropathy, as indicated by MNCV slowing (controls 45.1 ± 0.9 vs. db/db 34.3 ± 1.2 m/s; P < 0.001 by unpaired t test). Control and db/db mice were then treated with vehicle or NSI-189 (30 mg/kg/day) for a further 16 weeks. At study end there was no effect of NSI-189 on elevated body weight and blood glucose levels of db/db mice (Table 2). NeuN, PSD95, and synaptophysin protein levels were significantly decreased in the hippocampus of vehicle-treated but not NSI-189–treated db/db mice (Fig. 6A–C). In contrast, significantly reduced hippocampal BDNF levels were not altered by NSI-189 (Fig. 6D). Peripheral neuropathy in db/db mice, as indicated by MNCV slowing and tactile allodynia, was attenuated by NSI-189 treatment (Fig. 6E–G). Diabetic mice again showed no reduction in corneal nerve density, while NSI-189 treatment significantly increased this parameter (Fig. 6G).
Figure 6.
NSI-189 ameliorates CNS and PNS neuropathy in db/db mice. Hippocampal NeuN (A), PSD95 (B), synaptophysin (C), and BDNF (D) protein levels, and MNCV (E), paw tactile 50% PWT (F), and corneal subbasal plexus nerve length (G) after 24 weeks of diabetes, with NSI treatment for the last 16 weeks. C, control mice treated daily with vehicle; D, db/db mice treated daily with vehicle; DNSI, db/db mice treated daily with oral NSI-189. Data are mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA, followed by the Dunnett post hoc test (n = 8–10/group).
Discussion
Cognitive impairment is associated with reduced hippocampal volume in patients and rodents with diabetes (27–32). In the current study, female type 1 and male type 2 diabetic mice both showed decreased hippocampal volume, while measures of neurodegeneration (NeuN protein), synaptic integrity (PSD95 and synaptophysin protein), and neurogenesis (BrdU incorporation) were also reduced in the hippocampus of type 2 diabetic mice. Diabetic encephalopathy has been attributed to acceleration of age-related neuronal death, reduced replacement from the pool of neural progenitor cells (neurogenesis), or a combination of these processes (33). The reduced number of BrdU-positive cells in the brain of type 2 diabetic mice is consistent with prior reports of impaired neurogenesis in type 1 and type 2 diabetic mice (34). Protecting or accelerating neurogenesis and the appropriate insertion of new cells into neural networks offers a novel approach to halting or reversing diabetic encephalopathy.
NSI-189 prevents impaired neurogenesis in rodent models of ischemic stroke and irradiation (16,17). The present studies demonstrate that reduced neurogenesis was prevented when NSI-189 was given to type 2 diabetic mice from the onset of diabetes at a dose of 30 mg/kg/day. NSI-189 also selectively protected hippocampal structure when given either throughout the period of diabetes (both models) or following a period of untreated diabetes (30 mg/kg/day in the type 2 model). The minimal efficacy of the intervention paradigm using 10 mg/kg/day in type 1 diabetic mice may suggest that higher doses and/or longer durations of treatment are necessary. Although type 2 diabetic mice could not be used in behavioral assays of cognitive function due to obesity that severely limits ambulation, impaired long-term memory in type 1 diabetic mice was prevented by concurrent treatment with NSI-189. Ambulation is not impaired in type 1 diabetic mice, and they performed similar to controls during memory acquisition. Protection of long-term memory by NSI-189 occurred in both prevention and intervention paradigms, although whether intervention reversed established loss of long-term memory or halted progression remains to be established. Efficacy against long-term memory was accompanied by protection of CA1 and DG volume. It is notable that NSI-189 was ineffective against loss of short-term memory or reduced hippocampal CA3 volume. This is consistent with distinct roles of the CA1 and CA3 regions in different aspects of memory. Both CA1 and CA3 regions contribute to acquisition of memory, but only the CA1 is required for memory retrieval (35) and for memory over long intervals (36). The impact of NSI-189 on memory in diabetic mice may also result from protection of synaptic organization, as indicated by protection of pre- and postsynaptic protein levels (synaptophysin and PSD-95, respectively) in the hippocampus of db/db mice. This is consistent with reports that long-term potentiation is impaired in diabetic rodents and that NSI-189 enhances long-term potentiation in mouse hippocampal slice preparations (18). Bioactivity of NSI-189 requires protein synthesis (18), and it increases expression of the neurotrophic factor BDNF by hippocampal cells in culture (16). Interestingly, BDNF is reduced in the hippocampus of db/db mice. However, reduced hippocampal BDNF protein levels in db/db mice were not corrected by NSI-189, excluding this potential mechanism of action. Nevertheless, our data show that NSI-189 promotes neurogenesis and ameliorates structural and behavioral indices of diabetic encephalopathy.
The neurogenic properties of NSI-189 were discovered using a stable line of human fetal hippocampal neural stem cells, and exploration of the properties of NSI-189 has been restricted to CNS-derived cells and brain disorders (16–20). Our finding that NSI-189 enhanced neurite outgrowth in adult sensory neuron cultures extends the known cellular actions of this molecule to promoting regenerative growth of PNS axons. Stimulation of neurite growth is consistent with a prior report that NSI-189 increased hippocampal MAP2 expression (16), as MAP2 stabilizes microtubules and assists neurite elongation. Moreover, enhanced neurite extension by adult sensory diabetic neuron cultures was accompanied by stimulation of mitochondrial maximal respiratory capacity. A recent report that NSI-189 promotes Akt pathway signaling (18) is consistent with enhancement of mitochondrial respiration of adult sensory neurons, as signaling through Akt is involved in increased mitochondrial function and neurite outgrowth when these cells are exposed to NT-3, insulin, or IGF-1 (37,38). Stimulation of mitochondrial respiration by NSI-189 therefore has the potential to serve as the mechanism driving neurite growth in peripheral sensory neurons.
We previously used adult sensory neuron cultures to identify biological actions of molecules in peripheral neurons (21,39–41). Enhancement of mitochondrial energetics and neurite outgrowth in this system predicted the neuroprotective efficacy of guaifenesin, resveratrol, and muscarinic antagonists in multiple animal models of peripheral neuropathy (21,39,41). The similar in vitro profile of NSI-189 prompted us to assess efficacy of NSI-189 against indices of peripheral neuropathy in mouse models of type 1 and type 2 diabetes. Use of 10 mg/kg/day NSI-189 from the onset of diabetes gave partial protection against indices of large fiber motor (MNCV) and sensory (tactile allodynia) neuropathy and also attenuated functional (thermal hypoalgesia) and structural (reduced IENF and corneal nerve density) measures of small sensory fiber neuropathy. Efficacy was similar to that of insulin, which, in addition to glucose regulation, is a direct neurotrophic factor for sensory neurons (40). The ability of NSI-189 to protect sensory fiber density in the skin and cornea is particularly striking and consistent with its capacity to enhance neurite outgrowth in vitro. Efficacy across multiple manifestations of peripheral neuropathy suggests a fundamental neuroprotective mechanism distinct from the actions of individual neurotrophic factors, which tend to be fiber-type specific (42). Enhancement of mitochondrial function, as detected in diabetic sensory neurons in vitro, may offer this fundamental mechanism, although we do not yet have confirmation that NSI-189 impacted mitochondria in vivo. Importantly, efficacy was also noted when NSI-189 was delivered only after functional indices of neuropathy were established. This may have clinical implications, as a therapy that halts and/or reverses neuropathy is more desirable than one that requires prophylactic use.
Following guidance from pharmacokinetics data, we increased the dose of NSI-189 to 30 mg/kg/day when extending studies into a model of type 2 diabetes. Efficacy was again detected against multiple indices of peripheral neuropathy in both prevention and intervention treatment paradigms and was generally more effective than 10 mg/kg/day in the type 1 diabetes model. Dose-efficacy studies are warranted to establish whether this is a dose- or model-related phenomenon. Corneal nerve density was lower in control C57BLKS mice than in control Swiss Webster mice, reflecting known between-strain differences (43,44). It is notable that db/db mice did not show loss of sensory nerves in the corneal subbasal nerve plexus. This finding was apparent in two separate studies using two different methods of corneal nerve quantification. There are multiple reports of corneal nerve depletion in rodent models of type 1 diabetes (13,45,46) and also in a model of type 2 diabetes produced by a high-fat diet to promote insulin resistance combined with low-dose STZ to reduce insulin levels (47). As corneal nerve loss is prevented by topical insulin in type 1 diabetic mice (45), it is plausible that the extreme hyperinsulinemia of db/db mice is sufficient to protect corneal nerves or promote sprouting from surviving fibers. The low inherent corneal nerve density of C57BLKS mice could also contribute to failure to detect loss, although there is diabetes-induced loss in C57Bl/6J mice (46). Interestingly, NSI-189 treatment increased corneal nerve density in diabetic but not control mice, suggesting efficacy in the presence of other growth-promoting agents such as glucose and/or insulin.
The unanticipated acceleration of the late-stage disease phenotype of db/db mice, with progressive attenuation of hyperglycemia, could complicate interpretation of the therapeutic effects of NSI-189, as it may be argued that they are secondary to glucose regulation. However, attenuation of hyperglycemia was not observed in the intervention study using similarly aged db/db mice, while positive effects of NSI-189 were also detected in type 1 diabetic mice without impacting hyperglycemia. While we cannot yet explain why NSI-189 may have accelerated the late-stage disease phenotype in one study of db/db mice, the effects of NSI-189 on PNS and CNS disorders across all studies are not consistently associated with restoration of normoglycemia.
The pathogenesis of diabetic neuropathy and encephalopathy likely involves multiple pathways downstream of both hyperglycemia and loss of insulin/neurotrophic support (10,48,49). This complexity presents a challenge for developing therapies to augment the current standard of care (50), and polypharmaceutical approaches have been suggested as being necessary to intervene against this plethora of pathogenic pathways. NSI-189 offers the opportunity for development of a single therapeutic agent against multiple indices of central and peripheral neuropathy that is effective in both sexes and both forms of diabetes. These are desired properties in a molecule that, because of its advanced stage of development against other diseases (19,20), has the potential for rapid translation to clinical testing in patients with diabetes.
Supplementary Material
Article Information
Funding. This work was partly funded by National Institute on Aging, National Institutes of Health (NIH), grant AG-039736 to C.G.J.; by National Institute of Neurological Disorders and Stroke, NIH, grant 1R44-NS-103703 to C.G.J. and K.J.; and by National Institute of Neurological Disorders and Stroke, NIH, grant NS-081082 to N.A.C.
Duality of Interest. This study was also funded by Neuralstem, Inc. M.H. is a former employee and K.J. and D.Q. are employees of Neuralstem, Inc. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. C.G.J., M.H., P.F., K.J., and N.A.C. designed experiments, analyzed and interpreted the data, and contributed to writing the manuscript. A.M., D.Q., M.C.N.D., C.A., B.K., N.M., G.S., L.G., and D.R.S. collected and analyzed data. C.G.J. and N.A.C. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db19-0271/-/DC1.
References
- 1.Bril V. The perfect clinical trial. Int Rev Neurobiol 2016;127:27–41 [DOI] [PubMed] [Google Scholar]
- 2.Pop-Busui R, Martin C. Neuropathy in the DCCT/EDIC-what was done then and what we would do better now. Int Rev Neurobiol 2016;127:9–25 [DOI] [PubMed] [Google Scholar]
- 3.Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol 2006;5:64–74 [DOI] [PubMed] [Google Scholar]
- 4.Riederer P, Korczyn AD, Ali SS, et al. . The diabetic brain and cognition. J Neural Transm (Vienna) 2017;124:1431–1454 [DOI] [PubMed] [Google Scholar]
- 5.Brands AM, Biessels GJ, de Haan EH, Kappelle LJ, Kessels RP. The effects of type 1 diabetes on cognitive performance: a meta-analysis. Diabetes Care 2005;28:726–735 [DOI] [PubMed] [Google Scholar]
- 6.Biessels GJ, Reagan LP. Hippocampal insulin resistance and cognitive dysfunction. Nat Rev Neurosci 2015;16:660–671 [DOI] [PubMed] [Google Scholar]
- 7.de Bresser J, Tiehuis AM, van den Berg E, et al.; Utrecht Diabetic Encephalopathy Study Group . Progression of cerebral atrophy and white matter hyperintensities in patients with type 2 diabetes. Diabetes Care 2010;33:1309–1314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM. Diabetes mellitus and the risk of dementia: the Rotterdam Study. Neurology 1999;53:1937–1942 [DOI] [PubMed] [Google Scholar]
- 9.Velayudhan L, Poppe M, Archer N, Proitsi P, Brown RG, Lovestone S. Risk of developing dementia in people with diabetes and mild cognitive impairment. Br J Psychiatry 2010;196:36–40 [DOI] [PubMed] [Google Scholar]
- 10.Zochodne DW. Sensory neurodegeneration in diabetes: beyond glucotoxicity. Int Rev Neurobiol 2016;127:151–180 [DOI] [PubMed] [Google Scholar]
- 11.Jolivalt CG, Lee CA, Beiswenger KK, et al. . Defective insulin signaling pathway and increased glycogen synthase kinase-3 activity in the brain of diabetic mice: parallels with Alzheimer’s disease and correction by insulin. J Neurosci Res 2008;86:3265–3274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sima AA. Encephalopathies: the emerging diabetic complications. Acta Diabetol 2010;47:279–293 [DOI] [PubMed] [Google Scholar]
- 13.Jolivalt CG, Rodriguez M, Wahren J, Calcutt NA. Efficacy of a long-acting C-peptide analogue against peripheral neuropathy in streptozotocin-diabetic mice. Diabetes Obes Metab 2015;17:781–788 [DOI] [PubMed] [Google Scholar]
- 14.Sima AA, Kamiya H, Li ZG. Insulin, C-peptide, hyperglycemia, and central nervous system complications in diabetes [published correction appears in Eur J Pharmacol 2004;494:77] Eur J Pharmacol 2004;490:187–197 [DOI] [PubMed] [Google Scholar]
- 15.McIntyre RS, Johe K, Rong C, Lee Y. The neurogenic compound, NSI-189 phosphate: a novel multi-domain treatment capable of pro-cognitive and antidepressant effects. Expert Opin Investig Drugs 2017;26:767–770 [DOI] [PubMed] [Google Scholar]
- 16.Tajiri N, Quach DM, Kaneko Y, et al. . NSI-189, a small molecule with neurogenic properties, exerts behavioral, and neurostructural benefits in stroke rats. J Cell Physiol 2017;232:2731–2740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allen BD, Acharya MM, Lu C, et al. . Remediation of radiation-induced cognitive dysfunction through oral administration of the neuroprotective compound NSI-189. Radiat Res 2018;189:345–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y, Johe K, Sun J, et al. . Enhancement of synaptic plasticity and reversal of impairments in motor and cognitive functions in a mouse model of Angelman Syndrome by a small neurogenic molecule, NSI-189. Neuropharmacology 2019;144:337–344 [DOI] [PubMed] [Google Scholar]
- 19.Fava M, Johe K, Ereshefsky L, et al. . A Phase 1B, randomized, double blind, placebo controlled, multiple-dose escalation study of NSI-189 phosphate, a neurogenic compound, in depressed patients. Mol Psychiatry 2016;21:1483–1484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papakostas GI, Johe K, Hand H, et al. . A phase 2, double-blind, placebo-controlled study of NSI-189 phosphate, a neurogenic compound, among outpatients with major depressive disorder. Mol Psychiatry. 9 January 2019 [Epub ahead of print]. DOI: 10.1038/s41380-018-0334-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calcutt NA, Smith DR, Frizzi K, et al. . Selective antagonism of muscarinic receptors is neuroprotective in peripheral neuropathy. J Clin Invest 2017;127:608–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith DS, Skene JH. A transcription-dependent switch controls competence of adult neurons for distinct modes of axon growth. J Neurosci 1997;17:646–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davidson E, Coppey L, Lu B, et al. . The roles of streptozotocin neurotoxicity and neutral endopeptidase in murine experimental diabetic neuropathy. Exp Diabetes Res 2009;2009:431980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marshall AG, Lee-Kubli C, Azmi S, et al. . Spinal disinhibition in experimental and clinical painful diabetic neuropathy. Diabetes 2017;66:1380–1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jolivalt CG, Frizzi KE, Guernsey L, et al. . Peripheral neuropathy in mouse models of diabetes. Curr Protoc Mouse Biol 2016;6:223–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kee N, Sivalingam S, Boonstra R, Wojtowicz JM. The utility of Ki-67 and BrdU as proliferative markers of adult neurogenesis. J Neurosci Methods 2002;115:97–105 [DOI] [PubMed] [Google Scholar]
- 27.den Heijer T, Vermeer SE, van Dijk EJ, et al. . Type 2 diabetes and atrophy of medial temporal lobe structures on brain MRI. Diabetologia 2003;46:1604–1610 [DOI] [PubMed] [Google Scholar]
- 28.Ferguson SC, Blane A, Wardlaw J, et al. . Influence of an early-onset age of type 1 diabetes on cerebral structure and cognitive function. Diabetes Care 2005;28:1431–1437 [DOI] [PubMed] [Google Scholar]
- 29.Lobnig BM, Krömeke O, Optenhostert-Porst C, Wolf OT. Hippocampal volume and cognitive performance in long-standing Type 1 diabetic patients without macrovascular complications. Diabet Med 2006;23:32–39 [DOI] [PubMed] [Google Scholar]
- 30.Manschot SM, Brands AM, van der Grond J, et al.; Utrecht Diabetic Encephalopathy Study Group . Brain magnetic resonance imaging correlates of impaired cognition in patients with type 2 diabetes. Diabetes 2006;55:1106–1113 [DOI] [PubMed] [Google Scholar]
- 31.Piotrowski P. Morphology of experimental diabetes and cerebral ischemia in the rat brain. Folia Neuropathol 1999;37:252–255 [PubMed] [Google Scholar]
- 32.Reagan LP, Magariños AM, McEwen BS. Neurological changes induced by stress in streptozotocin diabetic rats. Ann N Y Acad Sci 1999;893:126–137 [DOI] [PubMed] [Google Scholar]
- 33.Dorsemans AC, Couret D, Hoarau A, Meilhac O, Lefebvre d’Hellencourt C, Diotel N. Diabetes, adult neurogenesis and brain remodeling: new insights from rodent and zebrafish models. Neurogenesis (Austin) 2017;4:e1281862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stranahan AM, Arumugam TV, Cutler RG, Lee K, Egan JM, Mattson MP. Diabetes impairs hippocampal function through glucocorticoid-mediated effects on new and mature neurons. Nat Neurosci 2008;11:309–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ji J, Maren S. Differential roles for hippocampal areas CA1 and CA3 in the contextual encoding and retrieval of extinguished fear. Learn Mem 2008;15:244–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farovik A, Dupont LM, Eichenbaum H. Distinct roles for dorsal CA3 and CA1 in memory for sequential nonspatial events. Learn Mem 2009;17:12–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aghanoori MR, Smith DR, Roy Chowdhury S, Sabbir MG, Calcutt NA, Fernyhough P. Insulin prevents aberrant mitochondrial phenotype in sensory neurons of type 1 diabetic rats. Exp Neurol 2017;297:148–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang TJ, Verkhratsky A, Fernyhough P. Insulin enhances mitochondrial inner membrane potential and increases ATP levels through phosphoinositide 3-kinase in adult sensory neurons. Mol Cell Neurosci 2005;28:42–54 [DOI] [PubMed] [Google Scholar]
- 39.Chowdhury SR, Saleh A, Akude E, et al. . Ciliary neurotrophic factor reverses aberrant mitochondrial bioenergetics through the JAK/STAT pathway in cultured sensory neurons derived from streptozotocin-induced diabetic rodents. Cell Mol Neurobiol 2014;34:643–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fernyhough P, Willars GB, Lindsay RM, Tomlinson DR. Insulin and insulin-like growth factor I enhance regeneration in cultured adult rat sensory neurones. Brain Res 1993;607:117–124 [DOI] [PubMed] [Google Scholar]
- 41.Hadimani MB, Purohit MK, Vanampally C, et al. . Guaifenesin derivatives promote neurite outgrowth and protect diabetic mice from neuropathy. J Med Chem 2013;56:5071–5078 [DOI] [PubMed] [Google Scholar]
- 42.Calcutt NA, Jolivalt CG, Fernyhough P. Growth factors as therapeutics for diabetic neuropathy. Curr Drug Targets 2008;9:47–59 [DOI] [PubMed] [Google Scholar]
- 43.Pham TL, Kakazu A, He J, Bazan HEP. Mouse strains and sexual divergence in corneal innervation and nerve regeneration. FASEB J 2019;33:4598–4609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reichard M, Weiss H, Poletti E, et al. . Age-related changes in murine corneal nerves. Curr Eye Res 2016;41:1021–1028 [DOI] [PubMed] [Google Scholar]
- 45.Chen DK, Frizzi KE, Guernsey LS, Ladt K, Mizisin AP, Calcutt NA. Repeated monitoring of corneal nerves by confocal microscopy as an index of peripheral neuropathy in type-1 diabetic rodents and the effects of topical insulin. J Peripher Nerv Syst 2013;18:306–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yorek MS, Obrosov A, Shevalye H, et al. . Effect of glycemic control on corneal nerves and peripheral neuropathy in streptozotocin-induced diabetic C57Bl/6J mice. J Peripher Nerv Syst 2014;19:205–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coppey LJ, Shevalye H, Obrosov A, Davidson EP, Yorek MA. Determination of peripheral neuropathy in high-fat diet fed low-dose streptozotocin-treated female C57Bl/6J mice and Sprague-Dawley rats. J Diabetes Investig 2018;9:1033–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Biessels GJ, Reijmer YD. Brain changes underlying cognitive dysfunction in diabetes: what can we learn from MRI? Diabetes 2014;63:2244–2252 [DOI] [PubMed] [Google Scholar]
- 49.Fernyhough P, Calcutt NA. An introduction to the history and controversies of the pathogenesis of diabetic neuropathy. Int Rev Neurobiol 2016;127:115–120 [DOI] [PubMed] [Google Scholar]
- 50.Pop-Busui R, Boulton AJ, Feldman EL, et al. . Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care 2017;40:136–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.