Abstract
PURPOSE:
We know little about how increased technological sophistication of clinical practices affects safety of chemotherapy delivery in the outpatient setting. This study investigated to what degree electronic health records (EHRs), satisfaction with technology, and quality of clinician-to-clinician communication enable a safety culture.
METHODS:
We measured actions consistent with a safety culture, satisfaction with practice technology, and quality of clinician communication using validated instruments among 297 oncology nurses and prescribers in a statewide collaborative. We constructed an index to reflect practice reliance on EHRs (1 = “all paper” to 5 = “all electronic”). Linear regression models (with robust SEs to account for clustering) examined relationships between independent variables of interest and safety. Models were adjusted for clinician age.
RESULTS:
The survey response rate was 68% (76% for nurses and 59% for prescribers). The mean (standard deviation) safety score was 5.3 (1.1), with a practice-level range of 4.9 to 5.4. Prescribers reported fewer safety actions than nurses. Higher satisfaction with technology and higher-quality clinician communication were significantly associated with increased safety actions, whereas increased reliance on EHRs was significantly associated with lower safety actions.
CONCLUSION:
Practices vary in their performance of patient safety actions. Supporting clinicians to integrate technology and strengthen communication are promising intervention targets. The inverse relationship between reliance on EHRs and safety suggests that technology may not facilitate clinicians’ ability to attend to patient safety. Efforts to improve cancer care quality should focus on more seamless integration of EHRs into routine care delivery and emphasize increasing the capacity of all care clinicians to communicate effectively and coordinate efforts when administering high-risk treatments in ambulatory settings.
INTRODUCTION
Given the narrow therapeutic index of chemotherapy agents and the volume of agents administered, patient safety in ambulatory oncology settings is a high-priority consideration.1 Safe chemotherapy delivery requires effective communication among clinicians to identify and manage adverse events. Increasingly, oncology practices have turned to technology solutions to improve communication and patient safety, with little empirical evidence for their efficacy.
The recent, rapid diffusion of health information technologies in clinical settings, specifically electronic health records (EHRs), has raised mounting concerns that immature technology designs as well as poor integration of these technologies can threaten patient safety, clinician well-being, and job satisfaction.2,3 Furthermore, health information technology enhances but may also disrupt standard modes of communication.4 Established communication practices can change when organizations move from a paper-based to an electronic patient record-keeping system,5,6 because the content and patterns of communication are altered.7
The mechanisms described above have an effect on the safety culture of a practice. By safety culture we mean performance of behaviors by clinicians theorized to support safety in health care settings. We know little about the impact of communication processes and communication technologies (eg, EHRs, synchronous messaging) on safety culture in ambulatory oncology practices. It is essential to understand the ways in which communication processes and technology are integrated in these settings to reduce errors and manage physiologic adverse responses to chemotherapy. The purpose of this study was to investigate the degree to which EHRs, satisfaction with technology, and clinician communication enable a safety culture in ambulatory oncology treatment settings. We hypothesized that practices with low reliance on EHRs that have clinicians who are more satisfied with the technology in their practice and report higher-quality clinician-to-clinician communication would be more likely to report increased behaviors that promote patient safety.
METHODS
Data Source
This study is a secondary data analysis of a larger study, the OCTET (Oncology Communication, Technology, and Patient Events) study (R01HS024914) a mixed-methods investigation aimed at characterizing clinician communication processes, communication technologies, and adverse patient events in a sample of ambulatory chemotherapy practices and examining how these practices and technologies influence safe chemotherapy administration. The study’s conceptual model is rooted in the sociotechnical framework, which posits that patient and practice outcomes are associated with two social system constructs (structure and people) and two technical system constructs (technology and communication).8 Data for the current study came from clinician surveys and daily practice event logs from the quantitative data collection phase. All study procedures were reviewed and approved by the University of Michigan Health Sciences and Behavioral Sciences institutional review board.
Sample
Practices.
We recruited 29 ambulatory oncology practices that are members of the Michigan Oncology Quality Collaborative (MOQC). MOQC practices share data to develop best practices in areas of care with high variation and costs. Currently, 48 practices across the state participate in MOQC, representing nearly 90% of all Michigan’s medical oncologists. To recruit practices, study investigators commenced the project at a regularly scheduled MOQC biannual meeting with physician, nursing, and administrative leaders in attendance. The MOQC Program Director then distributed e-mail invitations to physician leaders in each practice with a cover letter, a brief study synopsis, and a page of frequently asked questions. Once practices were recruited, study staff identified at least one staff member at each practice who completed (60-minute) Web-based training in study procedures. In partnership with trained staff, we disseminated a tip sheet for data collection procedures.
An on-site study coordinator at each participating practice completed a one-page daily log for 6 weeks that summarized key actions and processes that occurred and then faxed the daily logs to the MOQC Coordinating Center. All data were collected between May and October 2017.
Clinicians.
Clinicians were eligible to participate if they were registered nurses, physicians, nurse practitioners, or physician assistants who managed adult patients before, during, and after receipt of infusion treatments for cancer. We prepared two survey formats, one for nurses and one for prescribers (physicians, nurse practitioners, and/or physician assistants). Clinicians received survey packets containing a cover letter, either the nurse or prescriber survey, a $10 cash incentive, and a self-addressed stamped envelope for returning completed surveys to the study team. On-site study coordinators sent scripted e-mail reminders to clinicians to complete the survey. A total of 438 clinicians were sent recruitment materials and confirmed to be eligible. Of those, 297 (68%) consented to participate and completed surveys.
Measures and Outcome Assessments
Trained research assistants entered surveys into the Research Entry and Data Capture web application. Research Entry and Data Capture is a password-protected, user-authenticated, encrypted, and firewalled application used to collect and enter sensitive data in compliance with the Health Insurance Portability and Accountability Act. Research assistants double-entered all data, and discrepancies were resolved by the project manager.
Actions consistent with a safety culture.
Our primary outcome of interest was safety, specifically actions consistent with a safety culture. This was measured using the Safety Organizing Scale (SOS). The SOS is a reliable (α = 0.88) nine-item scale for clinicians to self-report the actual performance of behaviors theorized to support a safety culture in health care settings.9 For each item, clinicians are asked the degree to which they and their colleagues engage in the behavior or practice (eg, “We talk about mistakes and ways to learn from them”). Items are scored on a 7-point Likert scale (1 = “not at all” to 7 = “to a very great extent”) and summed, with higher scores indicating greater actions consistent with a safety culture.
Quality of clinician communication.
Quality of overall clinician communication was measured through a version of the Nurse-Physician Communication Questionnaire (α = 0.92), which was adapted for our study setting with the developer’s permission.10,11 Four aspects of communication are expressed in four subscales: timeliness, understanding, accuracy, and openness of communication. Clinicians rated 21 items on a 5-point Likert scale (1 = “strongly disagree” to 5 = “strongly agree”). A final item rated their overall satisfaction with clinician-to-clinician communication on a 5-point Likert scale (1 = “very dissatisfied” to 5 = “very satisfied”). Each of the four subscales was averaged, and then all four were summed together to form one overall nurse/prescriber communication score, with higher scores indicating higher-quality clinician communication.
Communication satisfaction with practice technology.
Clinicians’ communication satisfaction with practice technology was measured through a single item adapted from Venkatesh et al,12 measured on a 5-point Likert scale (1 = “very dissatisfied” to 5 = “very satisfied”): “How satisfied are you with the technology available for communication with other clinicians?” Higher scores indicated greater communication satisfaction with practice technology.12
Reliance on EHRs.
Reliance on EHRs was measured at the practice level and was defined as the extent to which a practice’s documentation practices are electronic. Two different measures were used in the study. First, we had a dichotomous measure of whether the practice had an entirely electronic health record or had either all-paper or a hybrid health record. For the second measure, each practice also provided information to the study team on whether the following five elements of a practice’s documentation system were electronic or paper-based: any portion of their record captured electronically, electronic chemotherapy orders, electronic documentation of chemotherapy administration, electronic system to document communication with patients/families, and electronic system to document communication among clinicians in the practice. This second measure was a scale reflecting whether five elements of their record were nonelectronic (0 points), or partially or fully electronic (1 point). The score was summed and practices were distributed from 0 = “no elements electronic” to 5 = “all elements electronic”.
All clinicians reported their sex, race, ethnicity, age, years in practice, and years employed in their current setting. Through daily practice event logs and a practice characteristics questionnaire collected by on-site study coordinators, we also ascertained patient volume during the 1-month survey data collection period, practice ownership, and rural versus urban location.
Data Analyses
All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC). Descriptive statistics were computed to examine demographic and clinical characteristics of clinicians and their practice settings, stratified by registered nurses and prescribers. Bivariate analyses (t test, χ2) examined differences in communication, safety behaviors, and communication satisfaction with technology between nurses and prescribers and the dichotomous measure of reliance on EHRs in the practice setting.
A linear regression model with robust SEs to account for clustering within practices examined the relationships between potential predictors of actions consistent with a safety culture, including communication satisfaction with practice technology, the quality of communication with other clinicians, reliance on EHRs in the practice (scaled measure), and type of clinician (nurse or prescriber). Given that other work suggests that there is variation in EHR adoption by age and years in practice,13,14 we adjusted the model for clinician age. Results did not differ for the model adjusted for clinicians’ years of experience. Alpha values less than 0.05 were considered significant.
RESULTS
Practice and Clinician Characteristics
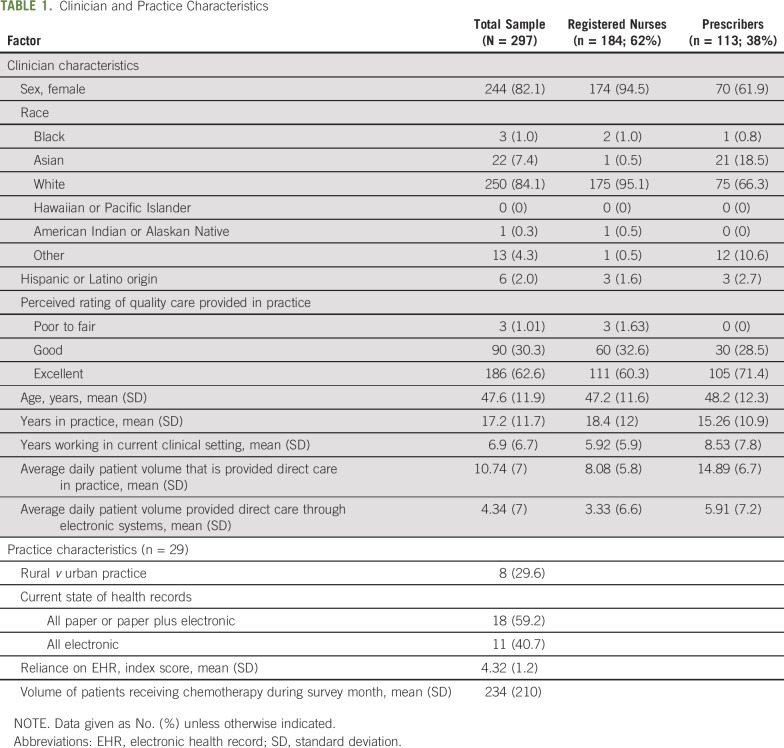
The survey response rate was 68% (76% for nurses and 59% for prescribers). Table 1 shows practice and clinician characteristics. Sixty-two percent of clinicians were registered nurses, and 38% were prescribers.
TABLE 1.
Clinician and Practice Characteristics
Communication, Safety Behaviors, and Satisfaction
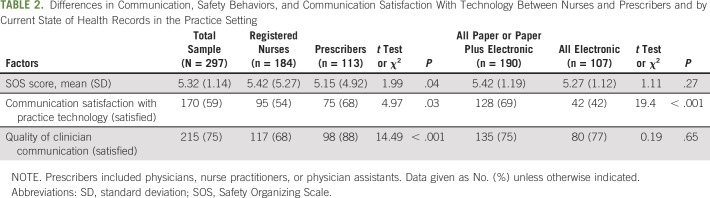
Table 2 shows unadjusted differences in communication, safety behaviors, and communication satisfaction with technology between nurses and prescribers and by reliance on EHRs in the practice setting. Fifty-nine percent of clinicians reported that they were satisfied with the available technology in their practice, and 75% reported high-quality clinician-to-clinician communication.
TABLE 2.
Differences in Communication, Safety Behaviors, and Communication Satisfaction With Technology Between Nurses and Prescribers and by Current State of Health Records in the Practice Setting
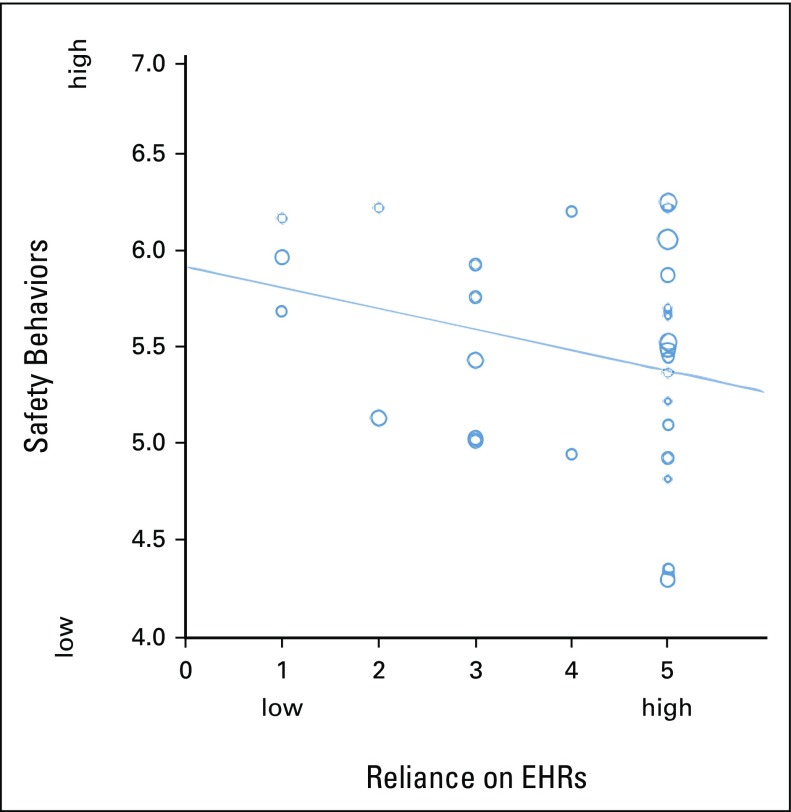
Significant differences were observed between registered nurses and prescribers in terms of safety scores, with registered nurses reporting higher use of behaviors consistent with a safety culture compared with prescribers (5.4 v 5.1; P < .04). Significant differences were also evident between prescribers’ and nurses’ reports of communication satisfaction with practice technology (68% v 54%; P < .03) and quality of communication with other clinicians (88% v 68%; P < .001), with prescribers reporting more favorably on both measures compared with nurses. Figure 1 shows the unadjusted relationship between actions consistent with a safety culture (SOS scores) and reliance on EHR in the practice. In this unadjusted analysis, differences were evident between practices that used all electronic systems versus both electronic systems and paper in terms of communication satisfaction with technology (42% v 69%; P < .001).
Fig 1.
Unadjusted relationship between practice reliance on EHR and actions consistent with a safety culture (Safety Organizing Scale [SOS] scores). Each circle represents one practice’s mean score on the SOS. Larger circles reflect larger variances in the SOS score. These values are plotted by the practice-level reliance on EHR index. EHR, electronic health record.
Factors Associated With Behaviors Congruent With Patient Safety
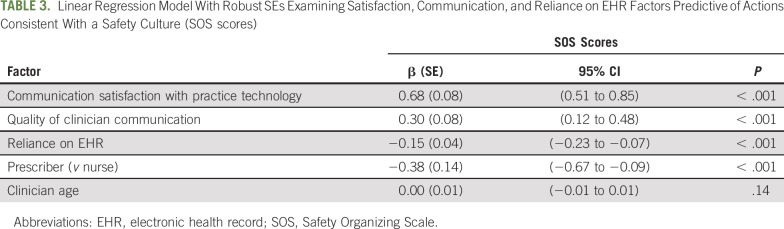
In a linear regression model examining factors associated with actions consistent with a safety culture and adjusted for clinician age, higher communication satisfaction with technology (P < .001) and more favorable clinician communication (P < .001) were significantly associated with increased safety scores. Conversely, increased reliance on EHRs in the practice was associated with lower safety scores (P < .001). Prescribers reported lower safety scores compared with nurses (P < .001; Table 3).
TABLE 3.
Linear Regression Model With Robust SEs Examining Satisfaction, Communication, and Reliance on EHR Factors Predictive of Actions Consistent With a Safety Culture (SOS scores)
DISCUSSION
From clinicians’ perspectives, we found that practices vary in their performance of what we refer to as patient safety actions. This is especially evident as it relates to communication with other clinicians, extent of reliance on EHRs, and their satisfaction with communication through technology used in the practice, invariant of clinician age or years in practice. Factors contributing to increased safety scores included clinicians’ report of higher satisfaction with technology used in the practice and more favorable communication with other clinicians. Our findings are consistent with other clinical studies showing that health information technology integration in care delivery settings can have unintended consequences on patient safety and communication.6,15-19 To our knowledge, this is among the first multisite studies to examine the impact of communication processes and communication technologies on patient safety actions in ambulatory oncology practices—care settings that deliver high-risk and high-cost cancer treatments.
Notably, we found that increased EHR capability in the practice was associated with lower safety scores and that this relationship was even stronger in an adjusted model. It is important to note that clinicians’ length of experience with an EHR system might influence patient safety; information on length of EHR experience was not available to the study team. Even though the EHR is meant to help with patient safety and lead to less variation, we saw the most variation in patient safety in practices that fully relied on EHRs (Fig 1). The inverse relationship between reliance on EHRs in the practice and safety suggests that technology may detract from patient safety. Scholars critical of current health information technology argue that EHRs were not designed with clinician usability in mind, nor were they designed to capture and highlight data in an intuitive manner.3,20 The tasks and interactions required with EHRs differ fundamentally from paper records, including e-prescribing, numerous alerts, reminders, and data entry forms and documentation requirements resulting from health care regulations, such as Meaningful Use requirements. Furthermore, clinicians have reported that EHR transitions placed additional burdens on their workload and, in some instances, did not replace paper-based documentation practices.21 Coupled with rapid rollout of health information technology in clinical settings since the 2009 federal requirement, it seems that patient safety has the potential to be compromised as clinicians struggle with adapting to new technology features and fundamentally different documentation processes. For some, these adaptations disrupt clinicians’ ability to deliver safe cancer care. These findings are consistent with other work demonstrating numerous unintended consequences of an electronic prescribing system, including communication and clinical disruption.18,22
We found that perceptions of prescribers and nurses varied when it came to performing behaviors consistent with a safety culture and their perception of quality communication with other clinicians. Specifically, prescribers reported lower safety scores compared with nurses; however, prescribers reported higher communication satisfaction with practice technology and higher-quality communication with other nurses. Nurses are responsible for a large portion of the documentation that addresses quality measures, safety measures, and the overall clinical picture of the patient and are thus one of the most frequent users of EHRs.23 Our findings are consistent with other studies that have shown that nurses notice significant challenges with the EHR when it comes to facilitating communication and supporting efficient care delivery.6,22 Prescribers and nurses have different perspectives and experiences that should be considered as leaders consider EHR modifications, quality-improvement efforts, and/or additional training. Our data suggest that improvement strategies may benefit from tailoring by clinician type to account for the notable differences observed in this study.
There are limitations to this study that should be noted. Data were cross-sectional; therefore, the true direction of association between some variables may not be easily discerned. The study sample comprised practices in Michigan only, where oncology practices have high rates of integration with health systems. Thus, the findings may not be generalizable to all areas. Survey measures of clinician communication and satisfaction with technology were not specific to EHRs. Although comprehensive in domains captured, the Nurse-Physician Communication Questionnaire is limited by measuring communication between physicians and nurses. Ambulatory oncology practices have more diverse teams for clinical decision making. Hence, communication measures that reflect diverse perspectives (pharmacy, advanced practice nurses, physician assistants, medical assistants) would be worthy of additional exploration. Objective safety measures were not available across all practices. These limitations are presented alongside a large, multisite survey of diverse members of the cancer care team that collected previously validated measures of technology use, communication, and patient safety behaviors.
Notwithstanding these limitations, this study provides important implications for clinical practice. There is substantial variation in patient safety perceptions in practices with full reliance on technology. Practices interested in improving patient safety should consider monitoring clinicians’ safety perceptions as technology is introduced or updated. In addition, effort to strengthen clinician communication, regardless of form, is an evidence-based strategy to improve patient safety. Careful attention to technology adoption and updates coupled with high-quality communication skills across clinicians are promising strategies to administer high-risk treatments safely in ambulatory oncology settings and improve cancer care quality.
ACKNOWLEDGMENT
Supported through the Agency for Healthcare Research and Quality Grant No. R01HS024914 and the National Cancer Institute Grant No. P30CA046592. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Health and Human Services. We thank the patients and staff of the participating practices.
Footnotes
Presented at the 2018 ASCO Annual Meeting, Chicago, IL, June 1-5, 2018.
AUTHOR CONTRIBUTIONS
Conception and design: Minal R. Patel, Minal R. Patel, Christopher R. Friese, Kari Mendelsohn-Victor, Bidisha Ghosh, Jennifer J. Griggs, Milisa Manojlovich
Collection and assembly of data: Minal R. Patel, Minal R. Patel, Christopher R. Friese, Kari Mendelsohn-Victor, Bidisha Ghosh, Jennifer J. Griggs, Milisa Manojlovich
Data analysis and interpretation: Minal R. Patel, Minal R. Patel, Christopher R. Friese, Kari Mendelsohn-Victor, Bidisha Ghosh, Jennifer J. Griggs, Milisa Manojlovich
Manuscript writing: All authors
Final approval: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Clinician Perspectives on Electronic Health Records, Communication, and Patient Safety Across Diverse Medical Oncology Practices
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
No potential conflicts of interest were reported.
REFERENCES
- 1.Centers for Disease Control and Prevention, National Center for Health Statistics Ambulatory Health Care Data. 2015 http://www.cdc.gov/nchs/ahcd.htm
- 2.Institute of Medicine . Health IT and Patient Safety: Building Safer Systems for Better Care. The National Academies Press; Washington, DC: 2012. [PubMed] [Google Scholar]
- 3.Verghese A.How tech can turn doctors into clerical workers.The New York Times, May 16, 2018https://www.nytimes.com/interactive/2018/05/16/magazine/health-issue-what-we-lose-with-data-driven-medicine.html?smid=pl-share
- 4.Weir CR, Hammond KW, Embi PJ, et al. An exploration of the impact of computerized patient documentation on clinical collaboration. Int J Med Inform. 2011;80:e62–e71. doi: 10.1016/j.ijmedinf.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care--an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14:542–549. doi: 10.1197/jamia.M2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmgren AJ, Pfeifer E, Manojlovich M, et al. A novel survey to examine the relationship between health IT adoption and nurse-physician communication. Appl Clin Inform. 2016;7:1182–1201. doi: 10.4338/ACI-2016-08-RA-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chiasson M, Reddy M, Kaplan B, et al. Expanding multi-disciplinary approaches to healthcare information technologies: What does information systems offer medical informatics? Int J Med Inform. 2007;76(suppl 1):S89–S97. doi: 10.1016/j.ijmedinf.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Bostrom RP, Heinen JS. MIS problems and failures: A socio-technical perspective, part II: The application of socio-technical theory. MIS Quarterly. 1977;1:11–28. [Google Scholar]
- 9.Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: Development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;45:46–54. doi: 10.1097/01.mlr.0000244635.61178.7a. [DOI] [PubMed] [Google Scholar]
- 10.Shortell SM, Rousseau DM, Gillies RR, et al. Organizational assessment in intensive care units (ICUs): Construct development, reliability, and validity of the ICU nurse-physician questionnaire. Med Care. 1991;29:709–726. doi: 10.1097/00005650-199108000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Manojlovich M. Linking the practice environment to nurses’ job satisfaction through nurse-physician communication. J Nurs Scholarsh. 2005;37:367–373. doi: 10.1111/j.1547-5069.2005.00063.x. [DOI] [PubMed] [Google Scholar]
- 12. Venkatesh V, Morris MG, Davis GB, et al: User acceptance of information technology: Toward a unified view. MIS Quarterly 27:425-478, 2003.
- 13. Menachemi N, Powers TL, Brooks RG: Physician and practice characteristics associated with longitudinal increases in electronic health records adoption. J Healthc Manag 56:183-197, 2011; discussion 197-198. [PubMed]
- 14.Bae J, Encinosa WE. National estimates of the impact of electronic health records on the workload of primary care physicians. BMC Health Serv Res. 2016;16:172. doi: 10.1186/s12913-016-1422-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rizzato Lede DA, Benítez SE, Mayan JC, III, et al. Patient safety at transitions of care: Use of a compulsory electronic reconciliation tool in an academic hospital. Stud Health Technol Inform. 2015;216:232–236. [PubMed] [Google Scholar]
- 16.Pell JM, Cheung D, Jones MA, et al. Don’t fuel the fire: Decreasing intravenous haloperidol use in high risk patients via a customized electronic alert. J Am Med Inform Assoc. 2014;21:1109–1112. doi: 10.1136/amiajnl-2014-002777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Overhage JM, Gandhi TK, Hope C, et al: Ambulatory computerized prescribing and preventable adverse drug events. J Patient Saf 12:69-74, 2016. [DOI] [PubMed]
- 18.Nanji KC, Rothschild JM, Boehne JJ, et al. Unrealized potential and residual consequences of electronic prescribing on pharmacy workflow in the outpatient pharmacy. J Am Med Inform Assoc. 2014;21:481–486. doi: 10.1136/amiajnl-2013-001839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford EW, Silvera GA, Kazley AS, et al. Assessing the relationship between patient safety culture and EHR strategy. Int J Health Care Qual Assur. 2016;29:614–627. doi: 10.1108/IJHCQA-10-2015-0125. [DOI] [PubMed] [Google Scholar]
- 20.Tubaishat A. The effect of electronic health records on patient safety: A qualitative exploratory study. Inform Health Soc Care. 2019;44:79–91. doi: 10.1080/17538157.2017.1398753. [DOI] [PubMed] [Google Scholar]
- 21.McAlearney AS, Sieck C, Hefner J, et al. Facilitating ambulatory electronic health record system implementation: Evidence from a qualitative study. BioMed Res Int. 2013;2013:629574. doi: 10.1155/2013/629574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi K, Gitelman Y, Asch DA. Subscribing to your patients - reimagining the future of electronic health records. N Engl J Med. 2018;378:1960–1962. doi: 10.1056/NEJMp1800874. [DOI] [PubMed] [Google Scholar]
- 23.Boyd AD, Dunn Lopez K, Lugaresi C, et al. Physician nurse care: A new use of UMLS to measure professional contribution: Are we talking about the same patient a new graph matching algorithm? Int J Med Inform. 2018;113:63–71. doi: 10.1016/j.ijmedinf.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]