Abstract
Context
Recent studies suggested that a large population of high school-aged athletes participate on club sport teams. Despite attempts to document emergency preparedness in high school athletics, the adherence to emergency and medical coverage standards among club sport teams is unknown.
Objective
To determine if differences in emergency preparedness and training existed between coaches of high school teams and coaches of high school-aged club teams.
Design
Cross-sectional survey.
Setting
Online questionnaire.
Patients or Other Participants
A total of 769 coaches (females = 266, 34.6%) completed an anonymous online questionnaire regarding their emergency preparedness and training.
Main Outcome Measure(s)
The questionnaire consisted of (1) demographics and team information, (2) emergency preparedness factors (automated external defibrillator [AED] availability, emergency action plan [EAP] awareness, medical coverage), and (3) emergency training requirements (cardiopulmonary resuscitation/AED, first aid).
Results
High school coaches were more likely than club sport coaches to be aware of the EAP for their practice venue (83.9% versus 54.4%, P < .001), but most coaches in both categories had not practiced their EAP in the past 12 months (70.0% versus 68.9%, P = .54). High school coaches were more likely to be made aware of the EAP during competitions (47.5% versus 37.1%, P = .02), but the majority of coaches in both categories indicated that they were never made aware of EAPs. High school coaches were more likely than club coaches to (1) have an AED available at practice (87.9% versus 58.8%, P < .001), (2) report that athletic trainers were responsible for medical care at practices (31.2% versus 8.8%, P < .001) and competitions (57.9% versus 31.2%, P < .001), and (3) be required to have cardiopulmonary resuscitation, AED, or first-aid training (P < .001).
Conclusions
High school coaches displayed much greater levels of emergency preparedness and training than coaches of high school-aged club teams. Significant attention and effort may be needed to address the lack of emergency preparedness and training observed in club coaches.
Keywords: secondary school, emergency action plans, medical coverage, sudden cardiac death
Key Points
High school coaches reported greater levels of emergency preparedness and training than club sport coaches.
High school coaches were more likely than club sport coaches to indicate that an athletic trainer was present at practices and competitions and that the athletic trainer was the primary individual responsible for providing medical care at these events.
Nearly 8 million adolescents participated in high school interscholastic sports during the 2017–2018 school year.1 A wide variety of benefits are associated with high school sport participation, such as encouragement of a healthy lifestyle, development of social and leadership skills, and improved academic performance.2,3 However, youth athletes show a trend toward specializing in a single sport, which has been linked with an increased risk of overuse injuries and potentially dropout from sport participation.2,4 As part of this trend, athletes may be encouraged to join club sport teams outside of school to train year round in their chosen sport.2 In a recent study of more than 1500 high school athletes, nearly 50% participated on club teams in a league outside their high school.4 Therefore, applying this rate to the overall population of high school athletes, 4 million adolescents may be participating in club sports outside the interscholastic setting.
Over the past few decades, as a result of legislation, regulation, and self-assessment, high schools and high school associations have improved their training and preparedness for responding to emergencies and injuries. In the United States, 34% to 70% of high schools used the services of an athletic trainer (AT),5–8 48% to 94% had at least 1 automated external defibrillator (AED) on campus,7–13 and 38% to 84% had established an emergency action plan (EAP).7–9,11–14 These improvements in emergency preparedness are very important, as the implementation of an EAP by trained medical professionals that led to prompt use of an AED dramatically increased survival rates after sudden cardiac arrest in adolescents.7,12,13,15 Additionally, the presence of an AT has been cited as integral to prompt evaluation and management of more common but still serious injuries, such as concussion.16
Despite improvements in emergency preparedness and medical coverage for high school athletics, implementation remains variable. In contrast, these topics have yet to be studied among club sport teams, which are not subject to many rules and regulations applied to high school and often rely on volunteer coaches.
Therefore, the primary purpose of our study was to determine if differences in emergency preparedness existed between coaches of high school teams and coaches of high school-aged club sport teams. We hypothesized that coaches of high school teams would be more likely than coaches of club teams to have AEDs available and easily accessible at practice, be aware of an EAP for their practice venue, and have an AT present at practices and competitions. A secondary purpose was to compare emergency training characteristics between high school and club coaches. We hypothesized that high school coaches would be more likely than club team coaches to have training in cardiopulmonary resuscitation (CPR), use of an AED, and first aid.
METHODS
Participants
The Institutional Review Board at the University of Wisconsin–Madison approved this study. Coaches of high school teams and club teams with high school-aged athletes in 3 sports (basketball, soccer, and volleyball) were invited via e-mail to complete an anonymous electronic questionnaire regarding their emergency preparedness and awareness of medical coverage pertaining to their team. We chose these sports due to their popularity in both the high school and club settings.1 Coaches were eligible to participate if they had served as the head or assistant coach of a high school sport team or high school-aged club sport team in the past 12 months. They were asked to respond based on their primary sport coaching responsibility, which was defined as the organized sport that was most important to the coach and that the coach would choose if allowed to coach only 1 sport. Potential respondents were supplied with an information sheet in the distribution e-mail that provided detail regarding the study, but they were not required to sign a consent form before participating due to the anonymous nature of the survey.
E-mails were distributed to high school coaches through the Michigan High School Athletic Association and to club coaches via e-mail addresses gathered from club sport organizations in Illinois, Michigan, Minnesota, and Wisconsin. Club sport organizations were defined as teams that were organized completely outside of a scholastic setting (ie, neither interscholastic nor intramural). Coaches in these organizations were recruited via the study team's previous relationships and familiarity with the organizations and based on geographic constraints. We chose to recruit club coaches from multiple nearby states to ensure a sufficient number of responses for comparison because of difficulty recruiting club coaches in Michigan. All of our high school coaches were from Michigan, so we limited club coach recruitment to 3 additional nearby Midwestern states with similar emergency preparedness requirements to Michigan's (high school coaches were required to undergo annual CPR/AED training17) to maximize comparability between the groups.
A total of 11 248 e-mails were sent, and we received 1156 responses (10.3% response rate). Of the total responses, 769 coaches fully completed the questionnaire and their data were analyzed (66.5% completion rate, 6.8% effective response rate). The effective response rate for high school coaches was 17.4% (497 fully completed questionnaires, 2852 e-mails sent), and the effective response rate for club coaches was 3.2% (272 fully completed questionnaires, 8396 e-mails sent).
Questionnaire
The questionnaire consisted of 3 major sections: (1) demographics and information regarding the teams that the respondent coached, (2) emergency preparedness factors (ie, AED availability at practices, EAP awareness during practices and competitions, medical coverage during practices and competitions) related to their teams, and (3) emergency care training requirements (CPR/AED, first aid). The questionnaire was designed using feedback from the University of Wisconsin–Madison Survey Center. The specific questions of interest for each section of the questionnaire are presented in the tables and figures.
A panel of 6 content-area experts determined the content validity index (CVI) of the questions in each section of the survey. The panel consisted of 2 youth sport coaches with 10 and 12 years of coaching experience, 1 strength and conditioning coach (Certified Strength and Conditioning Specialist and Registered Strength and Conditioning Coach) with 8 years of experience, and 3 ATs with graduate-level education (2 with master's degrees, 1 with a doctoral degree) and between 2.5 and 15 years of experience. The relevance of each item to its corresponding research aim was rated on a 4-point ordinal scale, based on the method of Polit and Beck.18 The CVI for each item was calculated by dividing the number of raters who ranked an item as quite or highly relevant by the total number of raters. Based on the recommendations of Lynn19 for a panel with 6 members, only items with a CVI ≥0.83 were included in the final questionnaire.
Statistical Analysis
Data were summarized using frequencies and proportions (%) and means and standard deviations (SDs). The primary analyses consisted of (1) overall χ2 analyses, which were used to compare the frequency of emergency preparedness responses between high school and club sport coaches, and then (2) each χ2 test was reanalyzed by stratifying for either coach's sex or sport to identify whether these factors were potential confounders in the association between emergency preparedness and team type. Because the results did not change when we stratified by coach's sex or sport, only the results of the overall χ2 analyses are presented. Statistical significance was set a priori at 2-sided P < .05, and all analyses were performed in R statistical software (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Participant demographics are presented in Table 1. A total of 769 coaches (females = 266, 34.6%; males = 503, 65.4%; age = 41.0 ± 11.5 years) completed the questionnaire and their data were analyzed. Overall, 64.6% (n = 497) were coaches of high school teams, and 35.4% (n = 272) were coaches of club sport teams involving high school-aged athletes. The coaches' sport responsibilities were split nearly evenly among basketball, volleyball, and soccer (basketball = 290, 37.7%; volleyball = 256, 33.3%; soccer = 223, 29.0%). High school and club coaches did not differ according to the coach's sex, coach's age, or team sex (P values > .05). High school players were older than club sport players (P < .001). More high school coaches reported having a graduate or professional degree than did club coaches (48.3% versus 31.3%, P < .001). More high school coaches indicated that teaching was their primary source of employment compared with club coaches (51.7% versus 25.7%, P < .001). Finally, more high school coaches than club coaches were involved in basketball (40.8% versus 32.0%, P = .03).
Table 1.
Participant Demographics
| Variable |
Coaches, No. (%) |
P Value |
||
| Overall (N = 769) |
High School (n = 497) |
Club Sport (n = 272) |
||
| Sport | .03 | |||
| Basketball | 290 (37.7) | 203 (40.8) | 87 (32.0) | |
| Volleyball | 256 (33.3) | 152 (30.6) | 104 (38.2) | |
| Soccer | 223 (29.0) | 142 (28.6) | 81 (29.8) | |
| Coach's sex | .76 | |||
| Female | 266 (34.6) | 170 (34.2) | 96 (35.3) | |
| Male | 503 (65.4) | 327 (65.8) | 176 (64.7) | |
| Coach's agea | .46 | |||
| Coach's education level | <.001 | |||
| High school diploma or general educational development | 48 (6.2) | 34 (6.8) | 14 (5.1) | |
| Associate or 2-year college degree | 90 (11.7) | 42 (8.5) | 48 (17.6) | |
| Bachelor or 4-year college degree | 306 (39.8) | 181 (36.4) | 125 (46.0) | |
| Graduate or professional degree | 325 (42.3) | 240 (48.3) | 85 (31.3) | |
| Coach's primary source of employment | <.001 | |||
| Teaching | 327 (42.5) | 257 (51.7) | 70 (25.7) | |
| Coaching | 366 (47.6) | 216 (43.5) | 150 (55.1) | |
| Other | 76 (9.9) | 24 (4.8) | 52 (19.1) | |
| Team sex | .38 | |||
| Female | 451 (58.6) | 283 (56.9) | 168 (61.8) | |
| Male | 238 (31.0) | 162 (32.6) | 76 (27.9) | |
| Both | 80 (10.4) | 52 (10.5) | 28 (10.3) | |
| Typical player age, y | <.001 | |||
| 14 | 72 (9.4) | 1 (0.2) | 71 (26.1) | |
| 15 | 83 (10.8) | 21 (4.2) | 62 (22.8) | |
| 16 | 287 (37.3) | 210 (42.3) | 77 (28.3) | |
| 17 | 308 (40.0) | 258 (51.9) | 50 (18.4) | |
| 18 | 19 (2.5) | 7 (1.4) | 12 (4.4) | |
Coach age in years, mean ± SD: overall = 41.0 ± 11.5; high school = 41.3 ± 10.6; club sport = 40.6 ± 12.9.
Participants' responses to questions regarding awareness of EAPs and AED availability during practices and competitions are presented in Table 2. More high school coaches reported being aware of the EAP for their practice venue compared with club coaches (83.9% versus 54.4%, P < .001). However, high school coaches did not differ from club coaches with respect to practicing their EAP in the past 12 months; most coaches in both categories indicated they had not practiced their EAP during that time (70.0% versus 68.9%, P = .54). Compared with high school coaches, more club coaches commented that they were never made aware of the EAP during competitions (62.9% versus 52.5%, P = .02). High school coaches were more likely than club coaches to report having an AED available at their practice venue (87.9% versus 58.8%, P < .001). Among coaches who responded yes to an AED being available at their practice venue, high school coaches were more likely than club coaches to be aware of the location of the AED, but most coaches in both categories were aware of the AED's location (97.5% versus 90.0%, P < .001).
Table 2.
Coaches' Awareness of Emergency Action Plans (EAPs) and Automated External Defibrillator (AED) Availability During Practices and Competitions
| Variable |
Coaches, No. (%) |
χ2 Value |
P Value |
|
| High School |
Club Sport |
|||
| Aware of EAP for practice venue? | 76.9 | <.001 | ||
| Yes | 417 (83.9) | 148 (54.4) | ||
| No | 80 (16.1) | 124 (45.6) | ||
| Practiced EAP for practice venue in past 12 months?a | 1.2 | .54 | ||
| Yes | 103 (24.7) | 41 (27.7) | ||
| No | 292 (70.0) | 102 (68.9) | ||
| Not sure/cannot remember | 22 (5.3) | 5 (3.4) | ||
| Is AED available at practice venue? | 95.8 | <.001 | ||
| Yes | 437 (87.9) | 160 (58.8) | ||
| No | 45 (9.1) | 56 (20.6) | ||
| Do not know/not sure | 15 (3.0) | 56 (20.6) | ||
| Aware of AED location at practice venue?b | 13.5 | <.001 | ||
| Yes | 426 (97.5) | 144 (90.0) | ||
| No | 11 (2.5) | 16 (10.0) | ||
| Distance of practice-venue AED from location where team practices, minb | 39.7 | <.001 | ||
| 0–1 | 325 (74.4) | 93 (58.1) | ||
| 1–3 | 86 (19.7) | 49 (30.6) | ||
| 3–5 | 20 (4.6) | 4 (2.5) | ||
| >5 | 3 (0.7) | 0 (0.0) | ||
| Do not know/not sure | 3 (0.7) | 14 (8.8) | ||
| How often are you made aware of the EAP at competition venues? | 9.9 | .02 | ||
| None of the time | 261 (52.5) | 171 (62.9) | ||
| Some of the time | 162 (32.6) | 77 (28.3) | ||
| Most of the time | 52 (10.5) | 15 (5.5) | ||
| Almost all of the time | 22 (4.4) | 9 (3.3) | ||
Respondents were asked this question only if they answered yes to being aware of the EAP at their practice venue.
Respondents were asked this question only if they answered yes to an AED being available at their practice venue.
Participants' responses regarding medical coverage for practices and competitions are presented in Table 3. High school coaches were more likely than club coaches to report that ATs were responsible for immediate medical care during practices (31.2% versus 8.8%, P < .001) and competitions (57.9% versus 31.2%, P < .001), whereas the majority of club coaches stated that coaches were typically the first care provider during both practices and competitions. High school coaches were also more likely to indicate that an AT was present most of the time or almost all of the time at practices (29.6%) or competitions (60.2%) versus club coaches (practices = 8.4%, P < .001; competitions = 38.6%, P < .001).
Table 3.
Medical Coverage During Practices and Competitions
| Variable |
Coaches, No. (%) |
χ2 Value |
P Value |
|
| High School |
Club Sport |
|||
| Who is typically responsible for immediate medical care during practices? | 63.7 | <.001 | ||
| AT | 155 (31.2) | 24 (8.8) | ||
| Coaches | 332 (66.8) | 230 (84.6) | ||
| Parents | 3 (0.6) | 14 (5.1) | ||
| Other | 7 (1.4) | 4 (1.5) | ||
| How often is an AT present at practices? | 71.5 | <.001 | ||
| None of the time | 227 (45.7) | 207 (76.1) | ||
| Some of the time | 123 (24.7) | 42 (15.4) | ||
| Most of the time | 75 (15.1) | 11 (4.0) | ||
| Almost all of the time | 72 (14.5) | 12 (4.4) | ||
| Who is typically responsible for immediate medical care during competitions? | 70.7 | <.001 | ||
| AT | 288 (57.9) | 85 (31.2) | ||
| Coaches | 197 (39.6) | 161 (59.2) | ||
| Parents | 3 (0.6) | 22 (8.1) | ||
| Other | 9 (1.8) | 4 (1.5) | ||
| How often is an AT present at competitions? | 49.1 | <.001 | ||
| None of the time | 103 (20.7) | 58 (21.3) | ||
| Some of the time | 95 (19.1) | 109 (40.1) | ||
| Most of the time | 76 (15.3) | 39 (14.3) | ||
| Almost all of the time | 223 (44.9) | 66 (24.3) | ||
Abbreviation: AT, athletic trainer.
Finally, high school coaches were more likely than club coaches to be required to have CPR training (98.8% versus 33.8%, P < .001; Figure 1), AED training (81.3% versus 26.8%, P < .001; Figure 2), or first-aid training (67.4% versus 35.3%, P < .001; Figure 3). Overall, 58.6% of high school coaches were required to have training in all 3 of these categories compared with 23.9% of club coaches (χ2 = 84.9, P < .001).
Figure 1.
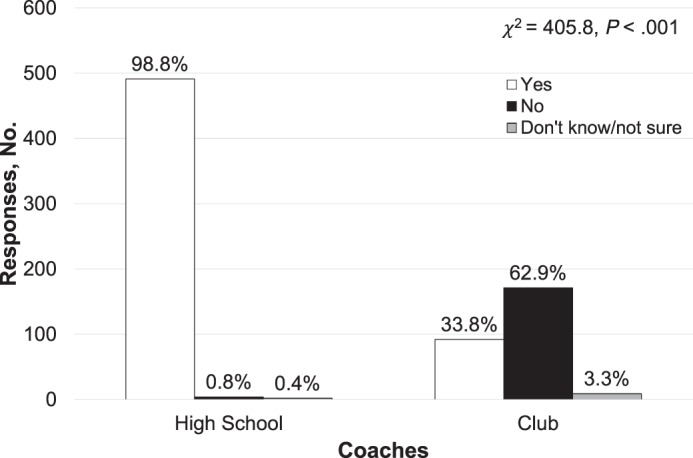
Differences between high school and club sport coaches in cardiopulmonary resuscitation training.
Figure 2.
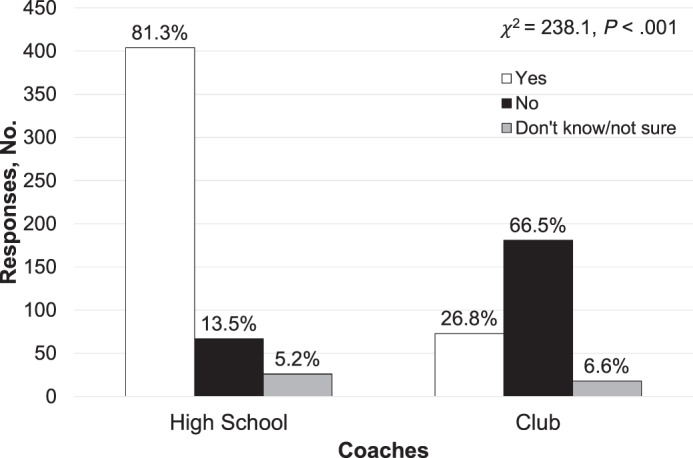
Differences between high school and club sport coaches in automated external defibrillator training.
Figure 3.
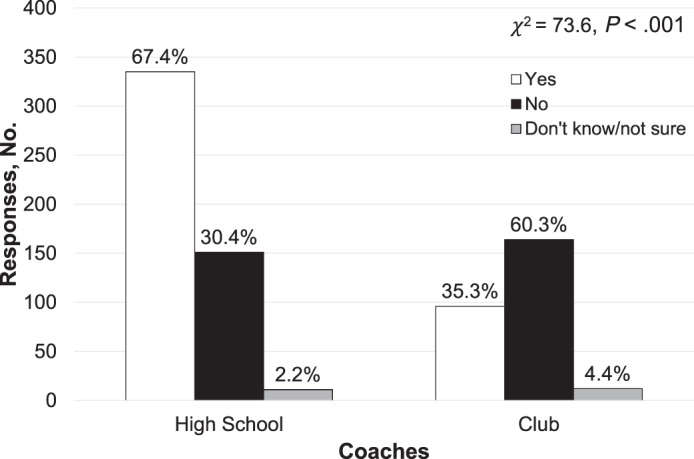
Differences between high school and club sport coaches in first-aid training.
DISCUSSION
Our most important finding was that large differences existed between high school and club sport coaches across a variety of measures of emergency preparedness and training. Specifically, high school coaches were (1) more aware of EAPs for their practice and competition venues, (2) more likely to have an AED available at practices, (3) more likely to have ATs providing immediate medical care at practices and competitions, and (4) more likely to be required to have CPR, AED, and first-aid training. Emergency preparedness and training of high school coaches have been investigated extensively.6–9,11–14,20 However, to our knowledge, this is the first study to compare emergency preparedness and training among high school coaches and coaches of high school-aged club teams.
Position statements on emergency planning from the National Athletic Trainers' Association and other national medical organizations exist for emergency safety and planning at both the secondary school and youth sports levels.20–22 These position statements recommended that schools and organizations develop venue-specific EAPs to be practiced annually and that AEDs should be located onsite and available within 3 minutes.20–22 We observed that high school coaches were more likely than club sport coaches to be aware of the EAPs for their practice venues, but the majority of both groups had not practiced their EAPs in the past 12 months. Previous researchers7,8,11–14,23 found that between 38% and 84% of high schools had venue-specific EAPs. Our high school coaches' awareness of emergency preparedness was at the higher end of this range, which may indicate improved implementation of these recommendations. However, similar to rates seen in previous studies,8,11,13,23 most high school coaches did not practice their EAP annually, which represents a potential area for improvement at the secondary school level. Despite these deficiencies, high school coaches were much more likely to be aware of their practice-venue EAPs than were club coaches. Roughly half of all club coaches were not aware of an EAP for their practice venues, and of those who were aware, the vast majority had not practiced their EAPs in the past 12 months.
Another crucial component of emergency planning is the rapid availability of an AED in case of sudden cardiac arrest.20–22 Survival rates from cardiac arrest after AED use at the secondary school level are between 60% and 64% and drop 10% for every minute that defibrillation is delayed.14,23,24 Among the high school coaches in this study, nearly 9 in 10 reported having an AED available at practice, and nearly all were aware of the specific location of the AED. Further, nearly 95% of high school coaches indicated that the AED was located within 3 minutes of their practice location, suggesting high compliance with best practices for emergency care. These rates are high compared with previous findings in this population, which showed that between 47% and 90% of schools reported at least 1 AED available at the school8–13 and between 56% and 66% of schools had an AED available for use in an athletic setting within 3 to 5 minutes.7,11 This high level of compliance was not matched by the club coaches: only 58.8% of club coaches reported that an AED was available at their practice venue. Among those club coaches who had an AED available at their practice venue, approximately 90% were both aware of the location of the AED and cited the location as being within 3 minutes of their team's practice venue. However, although these rates were high among club coaches who had an AED available at practices, they were still lower than those observed among high school coaches. Thus, our findings demonstrate a significant gap between the high school and club sport settings in both emergency planning and AED availability.
In addition to EAP and AED presence and availability, a third component of emergency care best practices consists of proper training and certification in CPR, AED, and first aid among all personnel associated with sport practices and competitions.21,22 High school coaches were much more likely than club sport coaches to be required to have training in all 3 categories. Nearly all (98.8%) high school coaches were required to have CPR training, and roughly 4 in 5 (81.3%) were required to have AED training. Earlier investigators7,9,10,12–14,25,26 found similarly high rates of AED training among high school coaches, but the rates of CPR training in our study were higher than previously established values for high school coaches (28%–50%). Because all of our high school coaches were from Michigan, this reflects a significant achievement as a result of regulation by the state athletic association. The lower rates of training among high school coaches in AED and first aid compared with CPR likely reflect the fact that these certifications were not required by the state athletic association and, thus, the rates may be driven instead by requirements at the school or district level. Conversely, only about 1 in 3 club coaches (26.8%–35.3%) were required to have training in each of the 3 categories. This represents a significant concern considering the high number of club coaches who reported being responsible for immediate medical care during practices and competitions.
High school and club coaches both reported that coaches were typically responsible for immediate medical care during practices. However, the majority of high school coaches reported that ATs provided immediate medical care during competitions, whereas the majority of club coaches reported that they were still responsible for immediate medical care during competitions. The large number of club coaches who reported providing medical care during competitions and practices in club sports is concerning, as previous researchers27–29 showed that coaches lacked the necessary preparation and training to properly diagnose or treat athletes with musculoskeletal injuries. Compared with club coaches, more high school coaches described ATs as being present at practices and competitions. Just over half of high school coaches reported that an AT was present at their practices at least some of the time versus nearly 80% who stated that an AT was present at their competitions at least some of the time. These coverage levels are similar to those observed earlier5–8,30,31: between 34% and 70% of high schools used the services of an AT, but the level of coverage provided (full time, part time, etc) varied widely based on school and community characteristics. Significant resources have been expended with the goal of increasing medical coverage at the secondary school level, and although improvements can still be made, these efforts have increased access to AT services in high schools during the past 20 years. However, it is clear from our results that a significant gap exists in the level of medical care being provided to the large number of athletes who participate on club sport teams.32
National medical organizations have devoted substantial efforts toward increasing the level of medical care provided to athletes in the high school setting, leading to increased training and preparedness of coaches and enhanced levels of medical coverage by ATs at practices and competitions. Up to half of high school athletes may be participating on club teams in addition to their school teams, and club teams and organizations have a responsibility to provide a high level of medical care to this increasing population of athletes.4 Therefore, an effort similar to that exerted for the secondary school setting may be needed to advocate for adolescent athletes in all sport settings, as our data indicate a significant gap in the preparedness of club teams to respond to medical emergencies. An examination of the barriers to improving medical care and emergency preparedness at the secondary school level can provide insights into possible barriers at the club sport level. Financial restrictions have been repeatedly identified as the primary barrier to hiring an AT, purchasing AEDs, and providing training to school personnel.6,9,10,25 At the high school level, these funds are typically appropriated through the school or school district budget, which in turn is funded via federal, state, and local taxes. Conversely, the funds available to club teams and organizations stem primarily from fees paid by participants. Thus, one potential negative side effect to increasing medical coverage and emergency preparedness at the club level may be the raising of activity fees, which could “price out” many participants from youth sports.
This study had several limitations that are important to note. First, the overall response rate for this study was low. Although the survey was distributed using specific e-mail lists provided by the Michigan High School Athletic Association and various club organizations, the overall response rate was around 7%. This low response rate may have created a selection bias in terms of the coaches who ultimately responded. Also, we only surveyed coaches from a small sample of states (Illinois, Michigan, Minnesota, and Wisconsin), which may limit the generalizability of these findings to coaches in different states or regions. Additionally, the recruitment of club coaches from multiple states and high school coaches from a single state may have resulted in geographic differences between the groups that could count for the differences in emergency preparedness we observed. However, a post hoc subanalysis examining differences between the high school coaches and club coaches from Michigan revealed similarly significant differences for nearly all of the analyses in this study (Appendices 1 and 2), indicating that the differences between club and high school coaches and not the differences in geography were responsible for our findings. Furthermore, because all of our high school coaches were from Michigan, the level of medical care and emergency preparedness they endorsed may be specific to that state. Yet the additional states from which we chose to recruit club coaches all required annual CPR and AED training for their high school coaches.17 Therefore, we expect that the Michigan high school coaches in this study are representative of high school coaches from the other 3 states, and similar differences in emergency preparedness would exist between club coaches and high school coaches in any of the states included in this study. Given the budgetary limitations of our study, we were only able to recruit high school coaches in 1 state. Future researchers need to assess emergency preparedness in high school and club coaches nationwide, as geographic, demographic, or socioeconomic factors that were not addressed in the current study may be important.
In addition, we did not ask the coaches where their sport practices and competitions were taking place. Some club practices and events may take place at school venues, and thus, the club coaches at these venues may be less familiar with emergency planning than the high school coaches. Regardless of the reason why club coaches were deficient regarding emergency preparedness, we believe that athletes participating on club teams deserve the same level of emergency care provided to high school athletes. Finally, we limited our survey to coaches of basketball, soccer, and volleyball teams. We chose these teams due to their popularity in both the high school and club settings. Therefore, comparisons of emergency preparedness and medical coverage between high school and club teams in other sports may differ from our results.
CONCLUSIONS
High school sport coaches displayed much greater levels of emergency preparedness and training than coaches of high school-aged club sport teams. High school coaches were more likely than club coaches to report that ATs were available to provide immediate medical care and were present during both practices and competitions. Significant attention and effort may be needed to address the differences in preparedness and training between high school and club coaches.
Appendix 1.
Training and Awareness of Michigan High School and Club Sport Coaches
| Variable |
Coaches, No. (%) |
χ2 Value |
P Value |
|
| High School (N = 497) |
Club (N = 31) |
|||
| CPR training required? | 174.4 | <.001 | ||
| Yes | 491 (98.8) | 17 (54.8) | ||
| No | 4 (0.8) | 14 (45.2) | ||
| Do not know/not sure | 2 (0.4) | 0 (0.0) | ||
| AED training required? | 49.2 | <.001 | ||
| Yes | 404 (81.3) | 9 (29.0) | ||
| No | 67 (13.5) | 18 (58.1) | ||
| Do not know/not sure | 26 (5.2) | 4 (12.9) | ||
| First aid training required? | 8.5 | .014 | ||
| Yes | 335 (67.4) | 13 (41.9) | ||
| No | 151 (30.4) | 17 (54.8) | ||
| Do not know/not sure | 11 (2.2) | 1 (3.2) | ||
| Aware of EAP for practice venue? | 10.4 | .005 | ||
| Yes | 417 (83.9) | 19 (61.3) | ||
| No | 80 (16.1) | 12 (38.7) | ||
| Practiced EAP for practice venue in past 12 months?a | 1.3 | .52 | ||
| Yes | 103 (24.7) | 4 (21.1) | ||
| No | 292 (70.0) | 15 (78.9) | ||
| Not sure/cannot remember | 22 (5.3) | 0 (0.0) | ||
| Is AED available at practice venue? | 55.6 | <.001 | ||
| Yes | 437 (87.9) | 12 (38.7) | ||
| No | 45 (9.1) | 14 (45.2) | ||
| Don't know/not sure | 15 (3.0) | 5 (16.1) | ||
| Aware of AED location at practice venue?b | 1.5 | .22 | ||
| Yes | 426 (97.5) | 11 (91.7) | ||
| No | 11 (2.5) | 1 (8.3) | ||
| Distance of practice-venue AED from location where team practices, minb | 28.2 | <.001 | ||
| 0–1 | 325 (74.4) | 9 (75.0) | ||
| 1–3 | 86 (19.7) | 1 (8.3) | ||
| 3–5 | 20 (4.6) | 0 (0.0) | ||
| >5 | 3 (0.7) | 0 (0.0) | ||
| Do not know/not sure | 3 (0.7) | 2 (16.7) | ||
| How often are you made aware of the EAP at competition venues? | 5.0 | .17 | ||
| None of the time | 261 (52.5) | 17 (54.8) | ||
| Some of the time | 162 (32.6) | 11 (35.5) | ||
| Most of the time | 52 (10.5) | 0 (0.0) | ||
| Almost all of the time | 22 (4.4) | 3 (9.7) | ||
Abbreviations: AED, automated external defibrillator; CPR, cardiopulmonary resuscitation; EAP, emergency action plan.
Respondents were asked this question only if they answered yes to being aware of the EAP at their practice venue.
Respondents were asked this question only if they answered yes to an AED being available at their practice venue.
Appendix 2.
Medical Coverage During Practices and Competitions According to Michigan High School and Club Sport Coaches
| Variable |
Coaches, No. (%) |
χ2 Value |
P Value |
|
| High School (N = 497) |
Club (N = 31) |
|||
| Who is typically responsible for immediate medical care during practices? | 25.0 | <.001 | ||
| AT | 155 (31.2) | 2 (6.5) | ||
| Coaches | 332 (66.8) | 28 (90.3) | ||
| Parents | 3 (0.6) | 0 (0.0) | ||
| Other | 7 (1.4) | 1 (3.2) | ||
| How often is an AT present at practices? | 10.9 | .012 | ||
| None of the time | 227 (45.7) | 23 (74.2) | ||
| Some of the time | 123 (24.7) | 6 (19.4) | ||
| Most of the time | 75 (15.1) | 1 (3.2) | ||
| Almost all of the time | 72 (14.5) | 1 (3.2) | ||
| Who is typically responsible for immediate medical care during competitions? | 27.6 | <.001 | ||
| AT | 288 (57.9) | 10 (32.3) | ||
| Coaches | 197 (39.6) | 18 (58.1) | ||
| Parents | 3 (0.6) | 3 (9.7) | ||
| Other | 9 (1.8) | 0 (0.0 | ||
| How often is an AT present at competitions? | 10.7 | .014 | ||
| None of the time | 103 (20.7) | 13 (41.9) | ||
| Some of the time | 95 (19.1) | 6 (19.4) | ||
| Most of the time | 76 (15.3) | 6 (19.4) | ||
| Almost all of the time | 223 (44.9) | 6 (19.4) | ||
Abbreviation: AT, athletic trainer.
REFERENCES
- 1.High school sports participation increases for 29th consecutive year. National Federation of State High School Associations Web site. 2018 https://www.nfhs.org/articles/high-school-sports-participation-increases-for-29th-consecutive-year/ Published. Accessed September 4, 2018.
- 2.DiFiori JP, Benjamin HJ, Brenner JS, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48(4):287–288. doi: 10.1136/bjsports-2013-093299. [DOI] [PubMed] [Google Scholar]
- 3.Fox CK, Barr-Anderson D, Neumark-Sztainer D, Wall M. Physical activity and sports team participation: associations with academic outcomes in middle school and high school students. J Sch Health. 2010;80(1):31–37. doi: 10.1111/j.1746-1561.2009.00454.x. [DOI] [PubMed] [Google Scholar]
- 4.McGuine TA, Post EG, Hetzel SJ, Brooks MA, Trigsted S, Bell DR. A prospective study on the effect of sport specialization on lower extremity injury rates in high school athletes. Am J Sports Med. 2017;45(12):2706–2712. doi: 10.1177/0363546517710213. [DOI] [PubMed] [Google Scholar]
- 5.Pryor RR, Casa DJ, Vandermark LW, et al. Athletic training services in public secondary schools: a benchmark study. J Athl Train. 2015;50(2):156–162. doi: 10.4085/1062-6050-50.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pike AM, Pryor RR, Vandermark LW, Mazerolle SM, Casa DJ. Athletic trainer services in public and private secondary schools. J Athl Train. 2017;52(1):5–11. doi: 10.4085/1062-6050-51.11.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson ST, Norcross MF, Bovbjerg VE, Hoffman MA, Chang E, Koester MC. Sports-related emergency preparedness in Oregon high schools. Sports Health. 2017;9(2):181–184. doi: 10.1177/1941738116686782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olympia RP, Dixon T, Brady J, Avner JR. Emergency planning in school-based athletics: a national survey of athletic trainers. Pediatr Emerg Care. 2007;23(10):703–708. doi: 10.1097/PEC.0b013e318155adfc. [DOI] [PubMed] [Google Scholar]
- 9.Toresdahl BG, Harmon KG, Drezner JA. High school automated external defibrillator programs as markers of emergency preparedness for sudden cardiac arrest. J Athl Train. 2013;48(2):242–247. doi: 10.4085/1062-6050-48.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rothmier JD, Drezner JA, Harmon KG. Automated external defibrillators in Washington State high schools. Br J Sports Med. 2007;41(5):301–305. doi: 10.1136/bjsm.2006.032979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monroe A, Rosenbaum DA, Davis S. Emergency planning for sudden cardiac events in North Carolina high schools. N C Med J. 2009;70(3):198–204. [PubMed] [Google Scholar]
- 12.Watson AM, Kannankeril PJ, Meredith M. Emergency response planning and sudden cardiac arrests in high schools after automated external defibrillator legislation. J Pediatr. 2013;163(6):1624–1627.e1. doi: 10.1016/j.jpeds.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 13.Meredith ML, Watson AM, Gregory A, Givens TG, Abramo TJ, Kannankeril PJ. Sudden cardiac arrests, automated external defibrillators, and medical emergency response plans in Tennessee high schools. Pediatr Emerg Care. 2013;29(3):352–356. doi: 10.1097/PEC.0b013e31828530c1. [DOI] [PubMed] [Google Scholar]
- 14.Lear A, Hoang M, Zyzanski SJ. Preventing sudden cardiac death: automated external defibrillators in Ohio high schools. J Athl Train. 2015;50(10):1054–1058. doi: 10.4085/1062-6050-50.8.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aschieri D, Penela D, Pelizzoni V, et al. Outcomes after sudden cardiac arrest in sports centres with and without on-site external defibrillators. Heart. 2018;104(16):1344–1349. doi: 10.1136/heartjnl-2017-312441. [DOI] [PubMed] [Google Scholar]
- 16.Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014;49(2):245–265. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.State High School Sports Safety Policy Rankings. Korey Stringer Institute Web site. 2018 https://ksi.uconn.edu/high-school-state-policies-2018/#. Published. Accessed September 4, 2018.
- 18.Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006;29(5):489–497. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 19.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–385. [PubMed] [Google Scholar]
- 20.Pryor RR, Huggins RA, Casa DJ. Best practice recommendations for prevention of sudden death in secondary school athletes: an update. Pediatr Exerc Sci. 2014;26(2):124–126. doi: 10.1123/pes.2014-0014. [DOI] [PubMed] [Google Scholar]
- 21.Huggins RA, Scarneo SE, Casa DJ, et al. The Inter-Association Task Force Document on Emergency Health and Safety: best-practice recommendations for youth sports leagues. J Athl Train. 2017;52(4):384–400. doi: 10.4085/1062-6050-52.2.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen J, Courson RW, Kleiner DM, McLoda T. National Athletic Trainers' Association position statement: emergency planning in athletics. J Athl Train. 2002;37(1):99–104. [PMC free article] [PubMed] [Google Scholar]
- 23.Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009;120(6):518–525. doi: 10.1161/CIRCULATIONAHA.109.855890. [DOI] [PubMed] [Google Scholar]
- 24.Marenco JP, Wang PJ, Link MS, Homoud MK, Estes NAM., III Improving survival from sudden cardiac arrest: the role of the automated external defibrillator. JAMA. 2001;285(9):1193–1201. doi: 10.1001/jama.285.9.1193. [DOI] [PubMed] [Google Scholar]
- 25.Schneider K, Meeteer W, Nolan JA, Campbell HD. Health care in high school athletics in West Virginia. Rural Remote Health. 2017;17(1):3879. doi: 10.22605/rrh3879. [DOI] [PubMed] [Google Scholar]
- 26.Harer MW, Yaeger JP. A survey of certification for cardiopulmonary resuscitation in high school athletic coaches. WMJ. 2014;113(4):144–148. [PubMed] [Google Scholar]
- 27.Ransone J, Dunn-Bennett LR. Assessment of first-aid knowledge and decision making of high school athletic coaches. J Athl Train. 1999;34(3):267–271. [PMC free article] [PubMed] [Google Scholar]
- 28.Barron MJ, Powell JW, Ewing ME, Nogle SE, Branta CF. First aid and injury prevention knowledge of youth basketball, football, and soccer coaches. Int J Coach Sci. 2009;3(1):55–67. [Google Scholar]
- 29.Yard EE, Collins CL, Comstock RD. A comparison of high school sports injury surveillance data reporting by certified athletic trainers and coaches. J Athl Train. 2009;44(6):645–652. doi: 10.4085/1062-6050-44.6.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buxton BP, Okasaki EM, McCarthy MR, Ho KW. Legislative funding of athletic training positions in public secondary schools. J Athl Train. 1995;30(2):115–120. [PMC free article] [PubMed] [Google Scholar]
- 31.Kroshus E, Rivara FP, Whitlock KB, Herring SA, Chrisman SPD. Disparities in athletic trainer staffing in secondary school sport: implications for concussion identification. Clin J Sport Med. 2017;27(6):542–547. doi: 10.1097/JSM.0000000000000409. [DOI] [PubMed] [Google Scholar]
- 32.Post EG, Bell DR, Trigsted SM, et al. Association of competition volume, club sports, and sport specialization with sex and lower extremity injury history in high school athletes. Sports Health. 2017;9(6):518–523. doi: 10.1177/1941738117714160. [DOI] [PMC free article] [PubMed] [Google Scholar]


