Abstract
Background and study aims This study aimed to investigate the diagnostic accuracy and utility of endoscopic ultrasound-guided fine-needle biopsy (EUS-FNB) performed using a Franseen needle on solid pancreatic lesions.
Patients and methods This study included 132 consecutive lesions sampled by endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) using a 22-G conventional needle and 95 consecutive lesions evaluated by EUS-FNB using a 22-G Franseen needle to evaluate solid pancreatic lesions at our medical center between July 2013 and November 2018. We used propensity-matched analysis with adjustment for confounders. Patient data were analyzed retrospectively.
Results Diagnostic accuracy was higher in the Franseen needle group (Group F; 91.6 %, 87 /95) than in the conventional needle group (Group C; 86.3 %, 82 /95), showing no significant difference ( P = 0.36). In Group F, diagnostic accuracies for pancreatic head lesions and lesions sampled by transduodenal puncture were 98.0 % (48/49) and 97.9 % (46/47), respectively. These values were significantly higher than values in Group C ( P = 0.013, 0.01). Group F displayed a significantly lower number of punctures. In terms of differentiating benign from malignant lesions, Group C showed 85.1 % sensitivity (74/87), 100 % specificity (8/8), 100 % positive predictive value (74/74), and 38.1 % negative predictive value (8/21), compared to values of 90.1 % (73/81), 100 % (14/14), 100 % (73/73), and 63.6 % (14/22), respectively, in Group F. Sensitivity and negative predictive value were better in Group F.
Conclusions Franseen needles for EUS-FNB of solid pancreatic lesions offer similar puncture performance at different lesion sites while requiring fewer punctures than conventional needles.
Introduction
Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) was first reported in 1992 1 and is now used for a wide range of lesions. This widely used non-surgical biopsy procedure provides safe, consistent results under ultrasound guidance 2 3 4 .
A recent meta-analysis of pancreatic lesions showed that EUS-FNA was a modality producing excellent diagnostic accuracy, and EUS-FNA has now been established as an important modality for histopathologic diagnosis of pancreatic lesions 5 . This modality is not, however, without unresolved issues, including the need for by-lesion needle selection, availability of rapid onsite evaluation (ROSE), and skilled endoscopists 6 7 .
New clinical applications for biopsies are on the horizon, such as genetic diagnostics and anticancer drug-sensitivity assays in addition to conventional diagnostics. Such applications will inevitably require collection of an adequate tissue volume to achieve better diagnostic accuracy 8 . In EUS-FNA, 19-G needles are useful for histologic diagnostics, providing sufficient sample for immunostaining, but the greater puncture resistance encountered at this size increases the difficulty of the procedure 9 10 . This has left users wanting smaller-gauge needles that could collect comparable volumes of tissue. Needle options for fine-needle biopsy (FNB) have increased with recent development of needles including a core-trap construction 11 12 and fork-tip needles 13 .
Marketing of an FNB needle with a reversed bevel design in 2011 (ProCore; Cook Medical, Tokyo, Japan) was well received. A meta-analysis, however, showed no significant difference in diagnostic accuracy between the ProCore (85 %) and conventional FNA needles (86 %) 14 . No consensus has yet been reached regarding which needles are best. In 2016, the Franseen needle emerged as an FNB device 15 with the potential to provide better histologic diagnostic accuracy than conventional FNA needles 8 . This device, however, remains under-researched. The Franseen needle, with three tips, is designed to collect biopsy samples by cutting and holding tissue from three cut surfaces 15 . The tip structure of the needle may allow acquisition of a large volume of tissue, but may show poor puncture performance.
We recently evaluated diagnostic accuracy and utility of EUS-FNB performed with a 22-G Franseen needle for solid pancreatic lesions, comparing the results to those obtained through EUS-FNA with conventional needles.
Patients and methods
This study was approved by the ethics review board at Saitama Medical University International Medical Center and complied with the Declaration of Helsinki, as revised in Brazil 2013. All patients provided written informed consent for EUS-FNA and FNB.
We carried out a retrospective review of all patients who underwent EUS-FNA or EUS-FNB to evaluate solid pancreatic lesions at our center between July 2013 and November 2018. During the study period, we enrolled 132 patients who had undergone EUS-FNA using a 22-G conventional needle from July 2013 to January 2017. A total of 95 patients who had undergone EUS-FNB using a 22-G Franseen needle from February 2017 to November 2018 were enrolled in another group. We checked electronic medical records of patients, and recorded age, sex, tumor size, tumor site, puncture site, experience of the clinician who performed examination, and final diagnosis. After propensity score-matching, data on 190 patients were analyzed ( Fig. 1 ).
Fig. 1.
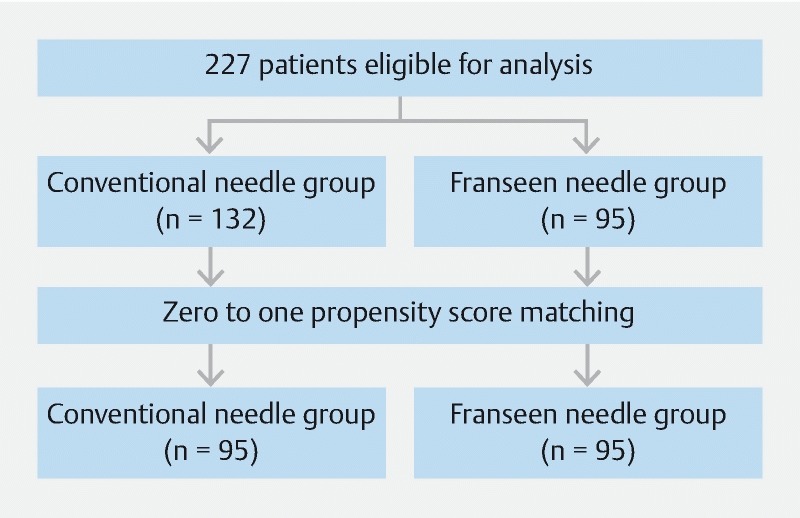
Diagram of the study design.
The primary endpoint of this study was to compare diagnostic accuracy between a 22-G conventional needle group and a 22-G Franseen needle group. The secondary endpoint was to compare the number of punctures required.
Procedures
EUS-FNA and FNB procedures were performed using a convex linear-array echoendoscope (GF-UCT260; Olympus Optical, Tokyo, Japan) paired with an ultrasound system (EU-ME2 Premier Plus; Olympus Optical). EUS was performed with the patient under conscious sedation using intravenous midazolam and pethidine hydrochloride. After excluding regional and collateral vasculature, the target lesion was punctured. The stylet was removed, and continuous suction was applied with a 20-ml syringe.
Next, 20 to 30 rapid strokes were made within the lesion, suction was released, and the needle was removed. Aspirated samples were smeared onto glass slides by inserting the stylet and applying air pressure. Samples were examined visually for white color and then fixed in formalin for histologic examination.
Because on-site cytologic examination was not performed, the procedure was repeated whenever possible under our supervision with a cytology technician until visual confirmation was obtained of an adequate sample for histopathology and immunostaining.
The puncture needles used were a 22-G conventional needle (Group C) and a 22-G Franseen needle (Group F). The Expect conventional needle (Boston Scientific Japan, Tokyo, Japan) used in Group C was primarily used in patients between July 2013 and January 2017, while the Acquire Franseen needle (Boston Scientific Japan) used in Group F was primarily used in patients thereafter ( Fig. 2 ). Procedures were performed by six endoscopists (three trainee endoscopists and three experienced in performing EUS-FNA). The three trainee endoscopists had sufficient experience, having conducted more than 1,000 regular esophagogastroduodenoscopies (EGDs), 500 colonoscopies, and 20 EUS procedures. They had also attended 20 EUS-FNA procedures performed by EUS-FNA experts as assistants. The three expert endoscopists had performed regular EGD, colonoscopy, and EUS procedures, and had performed more than 50 EUS-FNA procedures before the beginning of this study. Technical success was defined as a successful puncture to the target.
Fig. 2.

A 22-gauge Franseen needle with three tips for puncture.
Histologic evaluation
EUS-FNA and EUS-FNB specimens were smeared onto glass slides, and we checked if an adequate sample had been obtained. The sample was then preserved in 10 % formalin and embedded in paraffin. Sections were stained with hematoxylin and eosin (ΗΕ) for histologic examination, and immunostaining was performed if needed. These sections were examined by two pathology technicians and two pathologists. Only histologic diagnoses were analyzed in this study.
Study definitions
Final diagnosis was classified as the histologic diagnosis from surgery for those patients who underwent surgery, and as the clinical outcome after ≥ 6 months for those patients who did not undergo surgery. Pancreatic adenocarcinoma, pancreatic neuroendocrine tumor (NET), metastatic tumor from an extra-pancreatic malignancy, pancreatic carcinoma other than adenocarcinoma, and solid pseudopapillary neoplasms (SPN) were considered as malignant lesions. Lesions such as focal pancreatitis and other non-neoplastic lesions were considered benign, absent malignant findings on histologic examinations and a lack of progression for ≥ 6 months of follow-up. NET, metastases from extra-pancreatic malignancies, pancreatic carcinomas other than adenocarcinoma, and SPN requiring immunostaining were classified as “special pancreatic tumors.”
Statistical analysis
Categorical variables are expressed as absolute (n) and relative (%) frequencies, and were compared using Fisher’s exact test. For comparisons of continuous data, the two-sample t-test was used if a normal distribution was likely, and the Mann-Whitney test was used if normality could not be demonstrated. A propensity score-matched cohort was created by attempting to match each patient who had undergone EUS-FNA with a patient who had undergone EUS-FNB. In this regard, we used an optimal matching technique to reduce selection bias and potential confounding. A total of seven variables that could possibly influence outcome were used to generate, by logistic regression, a propensity score ranging from zero to one. P < 0.05 was considered significant. Statistical calculations were performed using SAS JMP version 14.1.0 and SAS version 9.4 software (SAS Institute, Cary, North Carolina, United States).
Results
We used the propensity-matched analysis and performed confounder adjustment. Clinical features of each propensity-matched patient group are shown in Table 1 . As a result, Groups C and F showed no significant differences in sex, age, lesion diameter, or tumor type. In Group F, the ratio of pancreatic head lesions and trans-duodenal punctures were higher compared to Group C ( P < 0.001 each). The most common final diagnosis from surgery or clinical outcome was adenocarcinoma (141 patients) ( Table 2 ). No procedural complications were encountered in this study.
Table 1. Clinical features of patients.
| All patients | Propensity-matched patients | |||||
| Group C | Group F | P | Group C | Group F | P | |
| Sex, male/female | 72/60 | 52/43 | > 0.99 | 50/45 | 52/43 | 0.89 |
| Age (years), median (IQR) | 66.5 (60.0 – 73.0) | 68.0 (58.0 – 74.0) | 0.54 | 67.0 (60.0 – 74.0) | 68.0 (58.0 – 74.0) | 0.89 |
| Tumor size (mm), median (IQR) | 27.4 (19.8 – 34.2) | 28.3 (21.4 – 37.1) | 0.35 | 27.5 (20.0 – 34.4) | 28.3 (21.4 – 37.1) | 0.59 |
| Pancreatic head/body or tail | 34/98 | 49/46 | < 0.001 | 24/71 | 49/46 | < 0.001 |
| Transgastric/transduodenal | 107/25 | 48/47 | < 0.001 | 72/23 | 48/47 | < 0.001 |
| Trainee/expert | 92/40 | 88/7 | < 0.001 | 88/7 | 88/7 | > 0.99 |
| Lesions requiring/not requiring immunostaining | 15/117 | 17/78 | 0.18 | 10/85 | 17/78 | 0.21 |
IQR, interquartile range; n, number of lesions
Table 2. Final diagnosis of propensity-matched patients.
| Final diagnosis | n (%) |
| Adenocarcinoma | 141 (74.2 %) |
| NET | 10 (5.3 %) |
| SPN | 10 (5.3 %) |
| Metastatic pancreatic tumor | 4 (2.1 %) |
| Acinar cell carcinoma | 3 (1.6 %) |
| Benign lesions | 22 (11.6 %) |
| Overall | 190 (100 %) |
n, number of lesions; NET, neuroendocrine tumor; SPN, solid pseudopapillary neoplasm
Groups C and F showed no significant differences in in technical success rate. Group F displayed a significantly lower number of punctures and slightly longer procedure time than Group C ( Table 3 ).
Table 3. Comparison of procedure outcomes between Franseen needle and conventional needle groups.
| Propensity-matched patients | |||
| Group C | Group F | P | |
| Number of punctures, median (IQR) | 3 (2 – 3) | 2 (2 – 3) | 0.028 |
| Procedure time (min), median (IQR) | 28.0 (21.0 – 39.0) | 33.0 (28.0 – 42.0) | 0.003 |
| Technical success, n (%) | 95/95 (100 %) | 94/95 (98.9 %) | > 0.99 |
IQR, interquartile range; n, number of lesions; n, number of lesions
Diagnostic accuracy was higher in Group F (91.6 %, 87/95) than in Group C (86.3 %, 82/95; P = 0.36), but no significant difference was evident. In Group F, diagnostic accuracy for pancreatic head lesions and lesions sampled by transduodenal puncture was 98.0 % (48/49) and 97.9 % (46/47) respectively. These values were significantly higher than in Group C ( P = 0.013, 0.01) ( Table 4 ).
Table 4. Comparison of diagnostic accuracy between Franseen needle and conventional needle groups.
| Propensity-matched patients | |||
| Diagnostic accuracy, n (%) | Group C | Group F | P |
| Location | |||
|
19/24 (79.2 %) | 48/49 (98.0 %) | 0.013 |
|
63/71 (88.7 %) | 39/46 (84.8 %) | 0.58 |
| Puncture route | |||
|
64/72 (88.9 %) | 41/48 (85.4 %) | 0.59 |
|
18/23 (78.3 %) | 46/47 (97.9 %) | 0.01 |
| Tumor type | |||
|
64/77 (83.1 %) | 57/64 (89.1 %) | 0.34 |
|
10/10 (100 %) | 16/17 (94.1 %) | > 0.99 |
|
8/8 (100 %) | 14/14 (100 %) | > 0.99 |
| Tumor size | |||
|
62/72 (86.1 %) | 71/76 (93.4 %) | 0.18 |
|
20/23 (87.0 %) | 16/19 (84.2 %) | > 0.99 |
|
82/95 (86.3 %) | 87/95 (91.6 %) | 0.36 |
n, number of lesions
In differentiation of benign from malignant lesions, Group C showed 85.1 % sensitivity (74/87), 100 % specificity (8/8), 100 % positive predictive value (74/74), and 38.1 % negative predictive value (8/21), compared to values of 90.1 % (73/81), 100 % (14/14), 100 % (73/73), and 63.6 % (14/22), respectively, in Group F. Sensitivity and negative predictive value were better in Group F ( Table 5 ).
Table 5. Diagnostic performance in differentiating malignant and benign lesions.
| Propensity-matched patients | |||
| Diagnostic accuracy, n (%) | Group C | Group F | P |
| Sensitivity | 85.1 % (74/87) | 90.1 % (73/81) | 0.36 |
| Specificity | 100 % (8/8) | 100 % (14/14) | > 0.99 |
| Positive predictive value | 100 % (74/74) | 100 % (73/73) | |
| Negative predictive value | 38.1 % (8/21) | 63.6 % (14/22) | |
n, number of lesions
Discussion
The Franseen needle, with three tips, is designed to collect biopsy samples by cutting and holding tissue from three cut surfaces. Tissue acquisition with Franseen needles is therefore adequate 11 . We have previously reported on the usefulness of Franseen needles 16 . Although the unique tip design of the Franseen needle may not allow puncture as easily as conventional FNA needles, we found no significant difference in technical success rates in evaluations at our hospital and encountered only one unsuccessful puncture, which was in a patient scheduled to undergo puncture from within the stomach. In that case, we performed puncture from the body of the stomach, but failed to penetrate the stomach wall and the procedure was unsuccessful. Although transduodenal puncture may involve greater needle-related variability than transgastric puncture because of poorer scope operability, Group F actually showed significantly higher diagnostic accuracy in terms of transduodenal puncture biopsies in the current study. We attribute this finding to the larger number of patients with pancreatic head lesions than lesions of the body and tail in Group F and the effectiveness of the specific procedure applied due to the up angle of the puncture that allows the lesion to be fixed firmly and the puncture to be completed quickly 16 . The current study showed that trainee operators are capable of properly performing the procedure with a Franseen needle, provided they have been correctly trained under the guidance of an expert. Although procedure time was slightly longer in Group F, which had a larger proportion of procedures performed very carefully by trainees, no complications were encountered and all times were within an acceptable range. From the above findings, puncture performance with a Franseen needle can be concluded to be relatively good.
Franseen needles have been shown to collect larger volumes of tissue than conventional FNA needles 8 11 . Following puncture, tissue is collected from the target by stroking while moving the needle within the target. At our institution, we stroke the tissue using the “door-knocking method,” which involves rapidly moving the needle back and forth within the target. A multicenter study showed no differences in diagnostic accuracy between door-knocking and conventional methods, but revealed that more tissue was acquired under the door-knocking method 17 . This finding of greater tissue acquisition suggests that using the door-knocking method with a Franseen needle should prove useful. Use of the Franseen needle increases the sample volume. As a result, visual confirmation becomes easier and the number of punctures is significantly reduced.
ROSE has been shown to improve diagnostic accuracy 6 , and pairing ROSE with use of a Franseen needle offers diagnostic accuracy in excess of 95 % 11 14 . Implementing ROSE, however, is not feasible in certain medical institutions, even in high-volume sites such as ours. Iwashita et al. reported achieving diagnostic results comparable to ROSE when evaluating macroscopically identifiable white samples 18 . Larger amounts of tissue can be acquired with a Franseen needle, which could simplify macroscopic identification of white tissue samples. Acquiring larger amounts of sample could improve diagnostic precision by pathologists and fewer punctures. In the present study, Group F showed a diagnostic accuracy exceeding 90 % and required fewer punctures than Group C. Larger sample volumes would facilitate not only sample-based histologic diagnosis, but also genetic diagnosis and anticancer drug-sensitivity assays performed with samples collected by FNB, as well as other clinical applications 19 20 21 22 .
In recent years, occasional reports about the Franseen needle have been published 23 24 . To the best of our knowledge, this is the largest study to compare Franseen FNB and conventional FNA in the diagnosis of solid pancreatic lesions. Although ROSE is unavailable at our hospital, we achieved high diagnostic accuracy, with particularly excellent results for transduodenal puncture and pancreatic head lesions.
Conclusion
We conclude that Franseen needles have similar puncture performance at different lesion sites, provide high diagnostic accuracy even at facilities where ROSE is unavailable, and require fewer punctures than conventional needles. However, because this study was retrospective, some limitations must be considered when interpreting the results. The potential influence of use of different needles during different periods cannot be excluded. In addition, all data were retrospectively collected from a single center. The procedures were performed by six endosonographers, and thus carried a risk of heterogeneity between operators. A prospective study with a larger number of cases will be necessary.
Footnotes
Competing interests None
References
- 1.Vilmann P, Jacobsen G K, Henriksen F W et al. Endoscopic ultrasonography with guided fine needle aspiration biopsy in pancreatic disease. Gastrointest Endosc. 1992;38:172–173. doi: 10.1016/s0016-5107(92)70385-x. [DOI] [PubMed] [Google Scholar]
- 2.Haba S, Yamao K, Bhatia V et al. Diagnostic ability and factors affecting accuracy of endoscopic ultrasound-guided fine needle aspiration for pancreatic solid lesions: Japanese large single center experience. J Gastroenterol. 2013;48:973–981. doi: 10.1007/s00535-012-0695-8. [DOI] [PubMed] [Google Scholar]
- 3.Mekky M A, Yamao K, Sawaki A et al. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010;71:913–919. doi: 10.1016/j.gie.2009.11.044. [DOI] [PubMed] [Google Scholar]
- 4.Yasuda I, Tsurumi H, Omar S et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy for lymphadenopathy of unknown origin. Endoscopy. 2006;38:919–924. doi: 10.1055/s-2006-944665. [DOI] [PubMed] [Google Scholar]
- 5.Hewitt M J, McPhail M J, Possamai L et al. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointestinal endoscopy. 2012;75:319–331. doi: 10.1016/j.gie.2011.08.049. [DOI] [PubMed] [Google Scholar]
- 6.Iglesias-Garcia J, Dominguez-Munoz J E, Abdulkader I et al. Influence of on-site cytopathology evaluation on the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of solid pancreatic masses. The American journal of gastroenterology. 2011;106:1705–1710. doi: 10.1038/ajg.2011.119. [DOI] [PubMed] [Google Scholar]
- 7.Madhoun M F, Wani S B, Rastogi A et al. The diagnostic accuracy of 22-gauge and 25-gauge needles in endoscopic ultrasound-guided fine needle aspiration of solid pancreatic lesions: a meta-analysis. Endoscopy. 2013;45:86–92. doi: 10.1055/s-0032-1325992. [DOI] [PubMed] [Google Scholar]
- 8.Mukai S, Itoi T, Yamaguchi H et al. A retrospective histological comparison of EUS-guided fine-needle biopsy using a novel franseen needle and a conventional end-cut type needle. Endoscopic Ultrasound. 2019;8:50–57. doi: 10.4103/eus.eus_11_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwashita T, Yasuda I, Doi S et al. Use of samples from endoscopic ultrasound-guided 19-gauge fine-needle aspiration in diagnosis of autoimmune pancreatitis. Clin Gastroenterol Hepatol. 2012;10:316–322. doi: 10.1016/j.cgh.2011.09.032. [DOI] [PubMed] [Google Scholar]
- 10.Yasuda I, Goto N, Tsurumi H et al. Endoscopic ultrasound-guided fine needle aspiration biopsy for diagnosis of lymphoproliferative disorders: feasibility of immunohistological, flow cytometric, and cytogenetic assessments. Am J Gastroenterol. 2012;107:397–404. doi: 10.1038/ajg.2011.350. [DOI] [PubMed] [Google Scholar]
- 11.Lee Y N, Moon J H, Kim H K et al. Core biopsy needle versus standard aspiration needle for endoscopic ultrasound-guided sampling of solid pancreatic masses: a randomized parallel-group study. Endoscopy. 2014;46:1056–1062. doi: 10.1055/s-0034-1377558. [DOI] [PubMed] [Google Scholar]
- 12.Lin M, Hair C D, Green L K et al. Endoscopic ultrasound-guided fine-needle aspiration with on-site cytopathology versus core biopsy: a comparison of both techniques performed at the same endoscopic session. Endosc Int Open. 2014;2:E220–223. doi: 10.1055/s-0034-1377611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bang J Y, Hebert-Magee S, Navaneethan U et al. Randomized trial comparing the Franseen and Fork-tip needles for EUS-guided fine-needle biopsy sampling of solid pancreatic mass lesions. Gastrointest Endosc. 2018;87:1432–1438. doi: 10.1016/j.gie.2017.11.036. [DOI] [PubMed] [Google Scholar]
- 14.Bang J Y, Hawes R, Varadarajulu S. A meta-analysis comparing ProCore and standard fine-needle aspiration needles for endoscopic ultrasound-guided tissue acquisition. Endoscopy. 2016;48:339–349. doi: 10.1055/s-0034-1393354. [DOI] [PubMed] [Google Scholar]
- 15.Bang J Y, Hebert-Magee S, Hasan M K et al. Endoscopic ultrasonography-guided biopsy using a Franseen needle design: initial assessment. Dig Endosc. 2017;29:338–346. doi: 10.1111/den.12769. [DOI] [PubMed] [Google Scholar]
- 16.Fujita A, Ryozawa S, Kobayashi M et al. Diagnostic ability of a 22G Franseen needle in endoscopic ultrasound-guided fine needle aspiration of subepithelial lesions. Mol Clin Oncol. 2018;9:527–531. doi: 10.3892/mco.2018.1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mukai S, Itoi T, Ashida R et al. Multicenter, prospective, crossover trial comparing the door-knocking method with the conventional method for EUS-FNA of solid pancreatic masses (with videos) Gastrointest Endosc. 2016;83:1210–1217. doi: 10.1016/j.gie.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 18.Iwashita T, Yasuda I, Mukai T et al. Macroscopic on-site quality evaluation of biopsy specimens to improve the diagnostic accuracy during EUS-guided FNA using a 19-gauge needle for solid lesions: a single-center prospective pilot study (MOSE study) Gastrointest Endosc. 2015;81:177–185. doi: 10.1016/j.gie.2014.08.040. [DOI] [PubMed] [Google Scholar]
- 19.Ashida R, Nakata B, Shigekawa M et al. Gemcitabine sensitivity-related mRNA expression in endoscopic ultrasound-guided fine-needle aspiration biopsy of unresectable pancreatic cancer. J Exp Clin Cancer Res. 2009;28:83. doi: 10.1186/1756-9966-28-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogura T, Yamao K, Hara K et al. Prognostic value of K-ras mutation status and subtypes in endoscopic ultrasound-guided fine-needle aspiration specimens from patients with unresectable pancreatic cancer. J Gastroenterol. 2013;48:640–646. doi: 10.1007/s00535-012-0664-2. [DOI] [PubMed] [Google Scholar]
- 21.Ryozawa S, Iwano H, Taba K et al. Genetic diagnosis of pancreatic cancer using specimens obtained by EUS-FNA. Dig Endosc. 2011;23 01:43–45. doi: 10.1111/j.1443-1661.2011.01117.x. [DOI] [PubMed] [Google Scholar]
- 22.Zagouri F, Sergentanis T N, Chrysikos D et al. Molecularly targeted therapies in metastatic pancreatic cancer: a systematic review. Pancreas. 2013;42:760–773. doi: 10.1097/MPA.0b013e31827aedef. [DOI] [PubMed] [Google Scholar]
- 23.Leung Ki E L, Lemaistre A I, Fumex F et al. Macroscopic onsite evaluation using endoscopic ultrasound fine needle biopsy as an alternative to rapid onsite evaluation. Endosc Int Open. 2019;7:E189–E194. doi: 10.1055/a-0770-2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishikawa T, Kawashima H, Ohno E et al. Clinical Impact of EUS-guided fine needle biopsy using a novel Franseen needle for histological assessment of pancreatic diseases. Can J Gastroenterol Hepatol. 2019;2019:8.581743E6. doi: 10.1155/2019/8581743. [DOI] [PMC free article] [PubMed] [Google Scholar]


