Abstract
Aim
The aim of this study was to describe inhaler use in primary health care patients with chronic obstructive pulmonary disease (COPD) and to categorize these patients into those making errors related to devices, those making errors related to inhalation technique and those making errors related to both.
Design
Observational study.
Methods
COPD nurses used a checklist to assess the use of inhalers by patients with spirometry‐verified COPD (N = 183) from primary healthcare centres. The STROBE checklist has been used.
Results
The mean age of the patients was 71 (SD 9) years. Almost half of them (45%) made at least one error; of these, 50% made errors related to devices, 31% made errors related to inhalation technique and 19% made errors related both to devices and to inhalation technique.
Keywords: administration, inhalation, pulmonary disease, chronic obstructive, dry powder inhalers, inhaler technique, metered‐dose inhalers, patient education
1. INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is one of the leading global causes of morbidity and mortality, causing a considerable and increasing social and economic burden (GOLD, 2019). Inhaled medication can reduce symptoms, reduce the severity and frequency of exacerbations and improve exercise tolerance and health status in patients with COPD (GOLD, 2019). However, incorrect inhaler use may lead to only a certain amount of the drug reaching the lungs (Laube et al., 2011). Devices used to inhale medication can be divided into three groups: Soft Mist Inhaler (SMI), pressurized Metered‐Dose Inhaler (pMDI) and Dry Powder Inhaler (DPI) (Newman, 2005). DPIs can be further subdivided into capsule DPI (cDPI), which are single‐dose inhaler, and multi‐DPI (mDPI), which are multi‐dose inhaler (Sanchis, Corrigan, Levy, & Viejo, 2013). A pMDI can also be used together with a spacer (Newman, 2005).
1.1. Background
A systematic review of assessment of inhaler use over the past 40 years concluded that only 31% of patients with COPD or asthma used their inhalers correctly and that the frequency of errors had not improved over time (Sanchis, Gich, & Pedersen, 2016). Correct inhaler use is crucial for the effectiveness of therapy (Usmani et al., 2018). The type of device and mastery of it is important for improving adherence, clinical outcome, quality of life and use of healthcare resources (Usmani et al., 2018).
One‐fifth of patients with COPD have reported being unsure of how or when to use their inhaler and 25% said that they regularly questioned whether their inhaler was working properly (Mulhall, Zafar, Record, Channell, & Panos, 2017). Additionally, it has been found that 49%–55% of patients using a DPI and 76% of patients using a pMDI do not inhale their medication correctly (Molimard et al., 2003). A systematic review to define critical error found that there were 299 descriptions of critical errors across the different devices, although the most common definition of critical error was “an action affecting the lung deposition of inhaled drug, resulting in little or no medicine being inhaled or reaching the lungs” (p. 4) (Usmani et al., 2018). Making at least one critical error due to device switch leads to increased healthcare expenditure because of healthcare visits and pharmacological treatment (Roggeri, Micheletto, & Roggeri, 2016).
In a recent review, Usmani et al. (2018) suggested that future studies should “classify individual errors into categories such as inhalation manoeuvre, dose preparation, inhaler handling, device‐specific or generic” (p. 15). Two studies (Molimard et al., 2017; Takaku et al., 2017) have classified errors into device‐specific or generic. Only one of them reported the actual number of patients making the errors (Takaku et al., 2017) while the other reported the number of errors committed by the patients (Molimard et al., 2017).
Inhaled medication is often prescribed for patients with COPD in primary health care. Assessing and reporting the number of patients making errors is more useful in clinical praxis than reporting the number of errors committed by the patients, since patients who are not using the inhaler correctly can be identified and educational efforts can be targeted where they are needed the most. The classification of patients into those making errors related to inhalation technique and those making errors related to the device might give guidance for the consultation. Can a more structured assessment of what kind of errors patients make be helpful when instructing and assessing patients' inhaler use or choosing a new device?
The aim of the present study was to describe inhaler use in primary health care patients with COPD and to categorize these patients into those making errors related to devices, those making errors related to inhalation technique and those making errors related to both.
1.2. Design
This observational study presents baseline data from the Communication and Inhalation technique study (ComIn), a randomized controlled trial which is yet to be published.
2. METHOD
2.1. Patients
Patients were recruited to ComIn from primary health care in four counties in central Sweden. Three primary healthcare centres (PHCCs) from each county were invited and a total of 11 PHCCs with 14 COPD nurses agreed to participate. Inclusion criteria were patients of all ages with spirometry‐verified COPD (ICD‐10 codes J44.0, J44.1, J44.8 and J44.9) diagnosed between September 2013–September 2015, selected at each PHCC. All eligible patients were randomized by the research group and the PHCCs received randomized lists of their patients. The COPD nurses started from the top of the list and assessed each patient according to the exclusion criteria: drug abuse, acute psychiatric disease, cognitive impairment (defined as a diagnostic code of dementia), insufficient knowledge of the Swedish language, not being registered at the PHCC, or being incapable of visiting the PHCC. An information letter about the study was sent to twenty consecutive patients that met the inclusion criteria and the COPD nurses then phoned the patients and asked if they wanted to participate. If a patient declined to participate, the COPD nurse contacted the next patient on the list. The recruitment procedure was completed after at least twenty patients agreed to participate. The present study used baseline data from those patients who used inhalers, regardless of whether the patient was in the ComIn intervention or control group (Figure 1).
Figure 1.
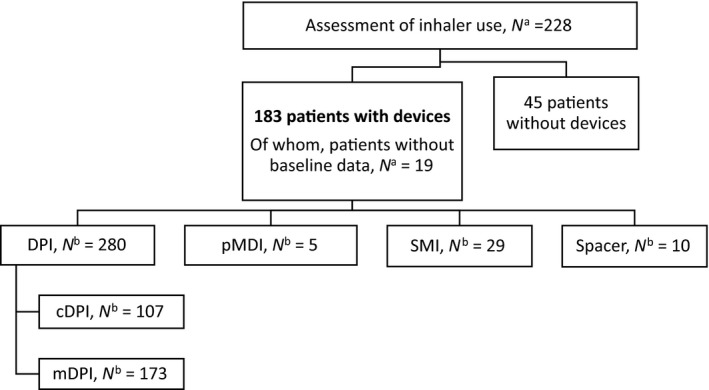
Data collection flow chart, numbers of patients (n = 228) and devices (n = 324)
2.2. Assessments
Sociodemographic data (sex, age, civil status, education and occupation), COPD Assessment Test (CAT) scores and data regarding self‐reported exacerbations, comorbidities and smoking status were collected at baseline through questionnaires filled in at the PHCC or at home straight after the visit and posted directly to the research group. The COPD nurses did not see the completed questionnaires.
COPD Assessment Test is a validated test used to assess health status in COPD patients (Jones et al., 2009). The questionnaire includes eight items with a maximum score of 40, and a higher score represents more impaired health. Each item is answered on a scale from 0–5 (0 = no problem and 5 = severe problem) (Jones et al., 2009).
Inhaler use was assessed by the COPD nurses using a checklist originally developed by Price et al. (2013), which included pMDI, pMDI with spacer and two DPI devices. The research group translated and adapted the checklist for this study by including more devices, using the manufacturers' descriptions and clinical experience. The revised checklist had two parts; one covering errors related to each device and one covering generic errors related to inhalation technique.
In this study, inhaler use was defined as the complete action from preparation of the device through the inhalation manoeuvre to completion, while inhalation technique was defined as the manoeuvres that start with expiration before inhalation and end with holding the breath after inhalation. Errors related to the device were defined as errors in those actions involving handling of the device before and after inhalation. The “generic for all DPI” section in the checklist (Appendix S1) was modified into “errors related to inhalation technique” by excluding errors that did not fit into our definition (see above) and by including errors related to inhalation technique with pMDI and with spacer. This was done to distinguish errors related to devices from those related to inhalation technique. Some devices in the checklist contained errors related to inhalation technique and in these cases, the error was moved to “errors related to inhalation technique” instead. SMI was included in the pMDI group in the analysis, due to similar inhalation technique. The COPD nurses marked the errors (yes or no) committed by the patient in the checklist and also had the opportunity to write comments next to each error.
Errors were separated into four steps for the analysis. Errors related to devices included steps 1, 2 and 4 and errors related to inhalation technique included step 3. The steps were numbered consecutively according to the order in which they occur when patients use their inhalers:
“Preparing the device” was defined as the initial steps when the patient prepares the device before dose preparation. Example of error: “does not remove the cap”.
“Dose preparation” was defined as the actions performed by the patient to make the drug available to inhale. Example of error: “does not shake the device when necessary”.
“Inhalation technique” was defined as the actual process where the patient inhales and makes the drug leave the inhaler, from expiration before inhalation to breath hold after inhalation. Example of error: Does not exhale slowly before inhalation.
“Completion of handling” was defined as the final steps of inhaler use. Example of error: “does not put on the cap after inhalation”.
2.3. Analysis
Categorical data (sociodemographic, number of inhalers per patient, exacerbation history and errors) were analysed using non‐parametric analysis and reported as absolute values and percentages. Continuous data (age and CAT score (Jones et al., 2009)) were analysed using parametric analysis and reported as means with standard deviations. Differences between groups were assessed with the chi‐square test for categorical data and independent‐sample t test for continuous data. Logistic regression was used to assess confounding factors. A p‐value < 0.05 was considered statistically significant. The statistical analysis was performed using version 21.0 of IBM SPSS Statistics for Windows (IBM Corp.).
2.4. Ethics
The study was approved by the Regional Ethical Board in Uppsala (ref: 2014/406). All patients provided their informed consent to participate at the baseline visit and had the right to withdraw their participation at any time without further explanation.
The STROBE checklist (Appendix S2) was used to guide construction of this article.
3. RESULTS
3.1. Patient characteristics
Of the 228 patients who were included in the study and visited the COPD nurse, 45 did not use any inhaled medication. Consequently, 183 patients who used a total of 324 devices were assessed. The devices included eight DPIs: Turbuhaler® (AstraZeneca), Diskus® (GlaxoSmithKline), Novolizer® (Meda), Eklira® (AstraZeneca), Easyhaler® (Orion Pharma), Spiriva HandiHaler® (Boehringer Ingelheim), Spiromax® (Teva) and Onbrez® (Novartis); one SMI: Spiriva Respimat® (Boehringer Ingelheim); and one pMDI: Flutiform® (Mundipharma). Ten patients used an inhaler with spacer: Evohaler® (GlaxoSmithKline), Alvesco® (AstraZeneca), Innovair® (Chiesi Farmaceutici SpA), Atrovent® (Boehringer Ingelheim) and four inhalers of unknown type. Two‐thirds (66%) of the patients used more than one inhaler, with a maximum of four inhalers (Table 1).
Table 1.
Number of devices among patients (n = 183)
| Number of devices per patient | Patients, n (%) |
|---|---|
| 4 | 2 (1) |
| 3 | 18 (10) |
| 2 | 100 (55) |
| 1 | 63 (34) |
| Number of patients using a DPI | 174 |
| Number of patients using a pMDI or SMI | 31 |
| Number of patients using a spacer | 10 |
Abbreviations: DPI, dry powder inhaler; pMDI, pressurized metered‐dose inhaler; SMI, soft mist inhaler.
Of the 183 patients who used devices, 19 did not answer the baseline data questionnaire but were included in the analysis of the inhaler technique. Therefore, sociodemographic data were based on the 164 patients that were both assessed for the inhaler technique and answered the baseline questionnaire (Figure 1). More than half of participants were women, the mean age was 71 (SD 9) years, and a quarter of the patients were smokers. The mean CAT score was 15 (SD 7) (Table 2). There were no differences in characteristics between those patients making at least one error and those making no error.
Table 2.
Characteristics of patients with COPD answering the baseline questionnaire (n = 164) and differences between patients making at least one error and patients making no error
| All patients | Patients making at least one error, n = 69 | Patients making no errors, n = 95 | p‐value | |
|---|---|---|---|---|
| Total n = 164 | n (%) | |||
| Age, mean ± SD (missing n = 5) | 71 ± 9 | 71 ± 9 | 71 ± 8 | .724 |
| Female sex | 85 (52) | 36 (52) | 49 (52) | .940 |
| Civil status (missing n = 3) | (missing n = 2) | (missing n = 1) | .355 | |
| Cohabiting | 91 (57) | 35 (52) | 56 (60) | |
| Living alone | 70 (43) | 32 (48) | 38 (40) | |
| Education (missing n = 4) | (missing n = 3) | (missing n = 1) | .520 | |
| Elementary school | 58 (36) | 27 (41) | 31 (33) | |
| Upper secondary school | 71 (44) | 26 (39) | 45 (48) | |
| University | 31 (19) | 13 (20) | 18 (19) | |
| Occupation (missing n = 5) | (missing n = 2) | (missing n = 3) | .667 | |
| Working | 31 (19) | 12 (18) | 19 (21) | |
| Other | 128 (81) | 55 (82) | 73 (79) | |
| Smoking status (missing n = 1) | (missing n = 1) | (missing n = 0) | .605 | |
| Never smoked on a regular basis | 9 (6) | 4 (6) | 5 (5) | |
| Ex‐smoker | 117 (72) | 47 (69) | 70 (74) | |
| Smoker | 37 (23) | 17 (25) | 20 (21) | |
| Comorbidities (missing n = 1) | (missing n = 1) | (missing n = 0) | ||
| Diabetes | 27 (17) | 8 (12) | 19 (20) | .163 |
| Heart disease | 44 (27) | 19 (28) | 25 (26) | .818 |
| Stroke | 10 (6) | 4 (6) | 6 (6) | .909 |
| High blood pressure | 94 (58) | 39 (57) | 55 (58) | .945 |
| Anxiety/depression | 24 (15) | 7 (10) | 17 (18) | .177 |
| Sleep apnoea | 15 (9) | 5 (7) | 10 (11) | .489 |
| Rheumatic disease | 15 (9) | 7 (10) | 8 (8) | .683 |
| Cancer | 23 (14) | 11 (16) | 12 (13) | .521 |
| Exacerbations (missing n = 0) | (missing n = 0) | (missing n = 0) | .064 | |
| At least one exacerbation in the past 12 months | 73 (45) | 27 (39) | 46 (48) | |
| CAT score, mean ± SD (missing = 3) | 15 ± 7 | 14 ± 6 | 16 ± 7 | .302 |
Abbreviations: CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease; SD, standard deviation.
Forty‐five per cent of the patients had had at least one exacerbation in the past 12 months. Exacerbation was defined as treatment with antibiotics and/or oral corticosteroids and/or emergency visit to healthcare facility and/or hospitalization because of deterioration of their lung disease.
3.2. Frequency of errors
A total of 83 patients (45%) made at least one error when using their inhaler. The number of errors per patient ranged from 1–6. The proportion of patients who made at least one error related to the devices was significantly larger than the proportion of the patients who made at least one error related to inhalation technique (50% vs. 31%, p = .007). Sixteen patients (19%) made errors in both categories. A multiple logistic regression analysis showed that age (>70 years), sex, exacerbations in the past year (>1), education (only elementary school) and CAT score (≥10) were not associated with whether the patients made at least one error; they were also not associated with whether the patients made errors related to inhalation technique, to device, or to both adjusted for all these confounders.
Patients with two or more devices made more errors than those with only one device, but the difference was not statistically significant (Table 3).
Table 3.
Errors made by patients with ≥2 devices and patients with 1 device
| Type of error | Total number of patients | Number of patients with ≥2 devices making error, n (%) | Number of patients with 1 device making error, n (%) | p‐value |
|---|---|---|---|---|
| Patients making any error | 83 | 58 (70) | 25 (30) | .264 |
| Patients making error related to inhalation technique | 26 | 18 (69) | 8 (31) | .672 |
| Patients making error related to device | 41 | 27 (66) | 14 (34) | .966 |
| Patients making error related to inhalation technique and device | 16 | 13 (81) | 3 (19) | .167 |
Most of the 184 errors committed by the patients when using their inhalers occurred in dose preparation (step 2) and inhalation technique (step 3); 39% and 52%, respectively. A minority of the errors occurred in preparing the device (step 1) and completion of handling (step 4); 7% and 2%, respectively.
The most frequent errors in step 3 were “Does not exhale slowly before inhalation” (22%) and “Does not tilt their head so that their chin is pointing slightly up” (22%) (Table 4).
Table 4.
Description of errors (n = 96) related to inhalation technique made by patients in the study
| Errors related to inhalation technique | Frequency of errors, n (%) |
|---|---|
| Does not exhale slowly before inhalation | 21 (22) |
| Exhales in the inhaler before inhalation | 12 (13) |
| Does not place mouthpiece between the teeth | 12 (13) |
| Does not close their lips around the mouthpiece | 4 (4) |
| Does not tilt their head so that their chin is pointing slightly up | 21 (22) |
| Does not inhale as fast as possible (defined as a strong audible inhalation) | 5 (5) |
| Does not inhale forcefully at the beginning | 7 (7) |
| Does not inhale for as long as possible | 4 (4) |
| Inhales through their nose | 0 (0) |
| Does not hold their breath | 9 (9) |
| Does not take 3–5 breaths in the spacer (read specific instructions for each spacer) | 1 (1) |
| Mouthpiece valve does not move when inhaling (spacer) | 0 (0) |
Errors are presented in the order in which they occur when inhaling medication.
The COPD nurses wrote 64 comments about errors that were not assessed in the checklist.
4. DISCUSSION
Almost half of the patients in this study made at least one error when using their inhalers. Most of those who used their inhalers incorrectly had problems with either the device or the inhalation technique itself, while a fifth made both errors related to the device and errors related to inhalation technique. Half of the patients made errors related to devices and about a third made errors related to inhalation technique. To our knowledge, only one study has reported the classification of errors related to devices and to inhalation technique by counting the number of patients making each type of error; the authors found that patients with COPD made more errors related to inhalation than errors related to device handling (Takaku et al., 2017). These results are not quite comparable to ours, since in that study the assessment was performed after one instruction from a pharmacist while in the present study no instruction was given prior the assessment. The patients in the present study used an average of 1.77 devices each, which is more than the 1.13 in the study of Takaku et al. (2017). The use of more than one device is a predictor of a higher frequency of error (Chrystyn et al., 2017) and many patients with COPD use more than one device. Another difference between the studies is the number of different devices that were assessed; ten plus spacer in the present study, compared with five by Takaku et al. (2017). Finally, Takaku et al. (2017) excluded patients with impaired finger dexterity, which may have impaired patients' ability to handle the device. With respect to the arguments above, our study might give more of a real‐life assessment of how many errors and what kind of errors patients with COPD are making.
As most (8/10) of the devices were DPI, the results of this study are similar to the findings of Molimard et al. (2003), who reported that 49%–55% of patients with DPI made at least one error. The device and the ability to handle it is important for adherence, clinical outcomes and quality of life (Usmani et al., 2018). Incorrect inhaler use can result in impaired disease control, which in turn leads to increased costs due to use of unscheduled healthcare resources (Melani et al., 2011). Although research into inhaler technique confirms that this is a substantial issue, the problem of a high frequency of errors remains constant (Sanchis et al., 2016). Another way to approach the problem of incorrect inhaler technique is to assess what kind of error the patient makes, not just whether the patient makes an error. Our suggested classification of errors might enable healthcare professionals to be more specific when assessing and instructing patients in inhaler use.
Of the 184 errors noted in the checklist, 88 were related to devices and 96 were related to inhalation technique. The results of this study are in line with previous studies, where two of the errors related to inhalation technique, “not exhaling before inhalation” and “not holding the breath after inhalation”, were reported as most common (Lavorini et al., 2008; Molimard et al., 2003; Sangita, Gharti, & Laxman, 2015; Westerik et al., 2016). This means that it is important to pay attention to these steps when teaching individualized inhalation technique (Sangita et al., 2015).
Choosing an appropriate device according to patient characteristics is one of the primary steps in optimal control of the disease (Rogliani et al., 2017; Scichilone et al., 2015) and in fact may be just as important as using disease severity as a guide to choosing the right medication (Rogliani et al., 2017). A study using the Delphi method to examine factors influencing pulmonologists' choice of device revealed an awareness and consensus that the selection of device was relevant, though 85% of the respondents stated that they prioritized the selection of drug over the selection of device (Miravitlles, Soler‐Cataluna, Alcazar, Viejo, & Garcia‐Rio, 2018). The wide range of devices on the market today increases the possibility to choose a device based on the patient's needs (Arora et al., 2014; Rogliani et al., 2017). More focus is needed on considering the patient's characteristics when choosing a device; this requires healthcare professionals to have knowledge of different devices as well as enough time to assess the patient's abilities.
The fact that almost half of the patients in this study did not use their inhaler correctly shows the need for further assessment and training by healthcare professionals. However, according to a review, only 15%–69% of healthcare professionals are able to demonstrate correct inhaler use (Price et al., 2013). Another review reported that the number of healthcare professionals who know the correct usage of inhalers had decreased over the last 20 years from 20.5%–10.8% (Plaza, Giner, Rodrigo, Dolovich, & Sanchis, 2018). The increase in the number of different inhalers on the market might be one reason for this decreased knowledge. To address the widespread problem of patients' incorrect inhaler use, it is necessary to start by educating the healthcare professionals.
5. STRENGTHS
One strength of this study is the classification of patients into those making errors related to devices and those making errors related to inhalation technique, which to our knowledge has rarely been reported before. This is in line with a recent review that emphasized the need for further studies to classify errors into device‐specific and generic errors to simplify comparison and analysis (Usmani et al., 2018). This classification could increase the knowledge of where focus is needed to provide patients with person‐centred care.
Observational studies can give a more accurate picture of how devices really work (Price, 2014), as well as a more accurate rate of errors. Participants in clinical trials are trained in inhaler use, and the results might not be transferable to real‐life patients with poor training (Molimard et al., 2017). Thus, the design of this study is suitable to estimate the rate of errors among primary care patients with COPD.
Patients in this study were selected from primary healthcare. Patients with a more severe disease and thus a higher risk of making errors (Lavorini et al., 2008; Wieshammer & Dreyhaupt, 2008) are often treated in secondary care. On the other hand, in Sweden, primary care is the first compulsory contact and most patients with COPD are treated there. It is rare that patients are treated in secondary care (Stallberg et al., 2014). Thus, the results of this study are relevant to primary healthcare. Patients were recruited from eleven PHCCs in four different counties in central Sweden, which increases the generalizability to the Swedish population.
6. LIMITATIONS
One exclusion criterion in this study was cognitive impairment, which is more common in older people. COPD is also more common in older people, as reflected in the mean age of 71 years among participants in the present study. Cognitive ability seems to be important in learning and remembering how to use inhalers (Crompton et al., 2006). If patients with cognitive impairment had been included in this study, the number of errors might have been even higher, and the pattern of errors might have differed.
No comparison was made between devices in the present study, since some devices had only a limited number of users. No conclusions can therefore be drawn regarding whether patients have a lower risk of making errors with any of the devices.
The COPD nurses assessed inhaler use among their own patients, which may have biased the results. Often, initial instructions and further assessment are delivered by the same healthcare provider (Rootmensen, Keimpema, Jansen, & Haan, 2010), which may contribute to a risk of biased assessment. If a patient makes many errors, the COPD nurse might see themselves as a poor educator. However, as the nurses in this study wrote a substantial number of comments about the errors they observed, it seems likely that they aimed to be objective.
Comments written by the COPD nurses revealed that the checklist was missing some errors, which affects its validity. The number of errors might have been higher if those errors had been included in the checklist. Checklists vary substantially between studies and are often created by the authors themselves, taken from previous studies, or taken from the instruction leaflet with no external validation (Chrystyn et al., 2017; Usmani et al., 2018). This affects the possibility to draw conclusions and to make comparisons between different devices and studies (Usmani et al., 2018) and highlights the need for a standardized checklist that is easy to analyse and enables comparison between studies and devices.
Assessment using checklists is subjective; however, assessment with electronic monitoring devices might give a more objective view. There are different electronic monitoring devices that can be helpful (Blum, Thavarajah, & Martirosov, 2019; Taylor et al., 2018). Yet, not all errors can be detected with help from electronic monitoring devices (Carpenter, Roberts, Sage, George, & Horne, 2017). Therefore, assessment from a provider together with electronic monitoring devices can give a better assessment of patient's inhaler use (Carpenter et al., 2017).
All COPD nurses in this study were assumed to be educated in inhaler use, since according to Swedish recommendations COPD nurses should have further education on an advanced level (Kull & Ställberg, 2018). We therefore chose not to control for the knowledge of the participating nurses in this aspect. However, their skills in inhaler use may have varied, thus biasing the results. The reliability of the assessment could have been increased by either training the COPD nurses in inhaler technique and assessment before the study began, or having an independent COPD nurse perform the assessments.
7. FURTHER RESEARCH
Since inhaler use has not improved over the past 40 years (Sanchis et al., 2016), educational interventions are needed. An educational intervention which includes the classification of errors into those related to inhalation technique and those related to devices might give information that facilitates the design of inhaler use instructions provided to patients.
There is also a need to improve and optimize the checklist used in this study to make it more inclusive and easier to analyse. It would also be desirable to have a validated checklist that enables comparison between studies and devices.
8. CONCLUSION
The patients in this study made both errors related to device and errors related to inhalation technique, but more patients made errors of the first type.
9. RELEVANCE TO CLINICAL PRACTICE
It is important to assess what kind of error the patient makes and more focus is needed on assessment of the patient's individual ability to handle their device. This knowledge can help healthcare professionals when instructing and choosing an appropriate device for each individual patient and thus increase the chances for optimal inhaled medication.
CONFLICT OF INTEREST
AL has received honoraria for educational activities and lectures from Teva and has served on advisory board arranged by GSK. KL has received payments for educational activities and lectures from Novartis, AstraZeneca, TEVA, Chiesi and Boehringer Ingelheim and participated on advisory boards with Boehringer Ingelheim and GlaxoSmith Kline. BS has received honoraria for educational activities and lectures from AstraZeneca, Boehringer Ingelheim, Meda, Novartis, and Teva, and has served on advisory boards arranged by AstraZeneca, Novartis, Meda, GSK, Teva, and Boehringer Ingelheim. HS has received honoraria for educational activities from Boehringer Ingelheim, Novartis, AstraZeneca, and Teva, and an unrestricted research grant from AstraZeneca. ABZ has received honoraria for educational activities and lectures from AstraZeneca. EW, KT, MA, LL and ETA have no conflicts of interest to declare.
Supporting information
ACKNOWLEDGEMENTS
We thank all the participants, including the healthcare professionals, who made this study possible.
Lindh A, Theander K, Arne M, et al. Errors in inhaler use related to devices and to inhalation technique among patients with chronic obstructive pulmonary disease in primary health care. Nursing Open. 2019;6:1519–1527. 10.1002/nop2.357
Funding information
This work was supported by the Uppsala‐Örebro Regional Research Council.
REFERENCES
- Arora, P. , Kumar, L. , Vohra, V. , Sarin, R. , Jaiswal, A. , Puri, M. M. , … Chakraborty, P. (2014). Evaluating the technique of using inhalation device in COPD and bronchial asthma patients. Respiratory Medicine, 108, 992–998. 10.1016/j.rmed.2014.04.021 [DOI] [PubMed] [Google Scholar]
- Blum, E. , Thavarajah, K. , & Martirosov, A. L. (2019). Optimization of patient‐specific inhaler regimens with the use of the aerosol inhalation monitor. Journal of the American Pharmacists Association, 59, 252–257. 10.1016/j.japh.2018.10.012 [DOI] [PubMed] [Google Scholar]
- Carpenter, D. M. , Roberts, C. A. , Sage, A. J. , George, J. , & Horne, R. (2017). A review of electronic devices to assess inhaler technique. Current Allergy and Asthma Reports, 17, 17 10.1007/s11882-017-0684-3 [DOI] [PubMed] [Google Scholar]
- Chrystyn, H. , van der Palen, J. , Sharma, R. , Barnes, N. , Delafont, B. , Mahajan, A. , & Thomas, M. (2017). Device errors in asthma and COPD: Systematic literature review and meta‐analysis. NPJ Primary Care Respiratory Medicine, 27, 22 10.1038/s41533-017-0016-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crompton, G. K. , Barnes, P. J. , Broeders, M. , Corrigan, C. , Corbetta, L. , Dekhuijzen, R. , … Voshaar, T. (2006). The need to improve inhalation technique in Europe: A report from the Aerosol Drug Management Improvement Team. Respiratory Medicine, 100, 1479–1494. 10.1016/j.rmed.2006.01.008 [DOI] [PubMed] [Google Scholar]
- GOLD (2019). Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2019 report). Global Initiative for Chronic Obstructive Lung Disease; https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf [Google Scholar]
- Jones, P. W. , Harding, G. , Berry, P. , Wiklund, I. , Chen, W. H. , & Kline Leidy, N. (2009). Development and first validation of the COPD Assessment Test. European Respiratory Journal, 34, 648–654. 10.1183/09031936.00102509 [DOI] [PubMed] [Google Scholar]
- Kull, I. S. , & Ställberg, B. (2018). Nya kriterier för astma/KOLmottagningar i primärvården. Updated criteria's for an asthma/COPD clinic in primary care based on Swedish guidelines. Lakartidningen, 115, 1–3. https://www.lakartidningen.se/EditorialFiles/LT/%5BEWLT%5D/EWLT.pdf [Google Scholar]
- Laube, B. L. , Janssens, H. M. , de Jongh, F. H. , Devadason, S. G. , Dhand, R. , Diot, P. , … Chrystyn, H. (2011). What the pulmonary specialist should know about the new inhalation therapies. European Respiratory Journal, 37, 1308–1331. 10.1183/09031936.00166410 [DOI] [PubMed] [Google Scholar]
- Lavorini, F. , Magnan, A. , Dubus, J. C. , Voshaar, T. , Corbetta, L. , Broeders, M. , … Crompton, G. K. (2008). Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respiratory Medicine, 102, 593–604. 10.1016/j.rmed.2007.11.003 [DOI] [PubMed] [Google Scholar]
- Melani, A. S. , Bonavia, M. , Cilenti, V. , Cinti, C. , Lodi, M. , Martucci, P. , … Neri, M. (2011). Inhaler mishandling remains common in real life and is associated with reduced disease control. Respiratory Medicine, 105, 930–938. 10.1016/j.rmed.2011.01.005 [DOI] [PubMed] [Google Scholar]
- Miravitlles, M. , Soler‐Cataluna, J. J. , Alcazar, B. , Viejo, J. L. , & Garcia‐Rio, F. (2018). Factors affecting the selection of an inhaler device for COPD and the ideal device for different patient profiles. Results of EPOCA Delphi consensus. Pulmonary Pharmacology and Therapeutics, 48, 97–103. 10.1016/j.pupt.2017.10.006 [DOI] [PubMed] [Google Scholar]
- Molimard, M. , Raherison, C. , Lignot, S. , Balestra, A. , Lamarque, S. , Chartier, A. , … Girodet, P. O. (2017). Chronic obstructive pulmonary disease exacerbation and inhaler device handling: Real‐life assessment of 2935 patients. European Respiratory Journal, 49(2), 1601794 10.1183/13993003.01794-2016 [DOI] [PubMed] [Google Scholar]
- Molimard, M. , Raherison, C. , Lignot, S. , Depont, F. , Abouelfath, A. , & Moore, N. (2003). Assessment of handling of inhaler devices in real life: An observational study in 3811 patients in primary care. Journal of Aerosol Medicine, 16, 249–254. 10.1089/089426803769017613 [DOI] [PubMed] [Google Scholar]
- Mulhall, A. M. , Zafar, M. A. , Record, S. , Channell, H. , & Panos, R. J. (2017). A tablet‐based multimedia education tool improves provider and subject knowledge of inhaler use techniques. Respiratory Care, 62, 163–171. 10.4187/respcare.05008 [DOI] [PubMed] [Google Scholar]
- Newman, S. P. (2005). Inhaler treatment options in COPD. European Respiratory Review, 14, 102–108. 10.1183/09059180.05.00009605 [DOI] [Google Scholar]
- Plaza, V. , Giner, J. , Rodrigo, G. J. , Dolovich, M. B. , & Sanchis, J. (2018). Errors in the use of inhalers by health care professionals: A systematic review. The Journal of Allergy and Clinical Immunology: in Practice, 6, 987–995. 10.1016/j.jaip.2017.12.032 [DOI] [PubMed] [Google Scholar]
- Price, D. (2014). Expert review. The significance of inhaler technique & how to improve it. Retrieved from www.ondrugdelivery.com [Google Scholar]
- Price, D. , Bosnic‐Anticevich, S. , Briggs, A. , Chrystyn, H. , Rand, C. , Scheuch, G. , & Bousquet, J. (2013). Inhaler competence in asthma: Common errors, barriers to use and recommended solutions. Respiratory Medicine, 107, 37–46. 10.1016/j.rmed.2012.09.017 [DOI] [PubMed] [Google Scholar]
- Roggeri, A. , Micheletto, C. , & Roggeri, D. P. (2016). Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: Critical health and economic issues. International Journal of Chronic Obstructive Pulmonary Disease, 11, 597–602. 10.2147/COPD.S103335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogliani, P. , Calzetta, L. , Coppola, A. , Cavalli, F. , Ora, J. , Puxeddu, E. , … Cazzola, M. (2017). Optimizing drug delivery in COPD: The role of inhaler devices. Respiratory Medicine, 124, 6–14. 10.1016/j.rmed.2017.01.006 [DOI] [PubMed] [Google Scholar]
- Rootmensen, G. N. , van Keimpema, A. R. , Jansen, H. M. , & de Haan, R. J. (2010). Predictors of incorrect inhalation technique in patients with asthma or COPD: A study using a validated videotaped scoring method. Journal of Aerosol Medicine and Pulmonary Drug Delivery, 23, 323–328. 10.1089/jamp.2009.0785 [DOI] [PubMed] [Google Scholar]
- Sanchis, J. , Corrigan, C. , Levy, M. L. , & Viejo, J. L. (2013). Inhaler devices – From theory to practice. Respiratory Medicine, 107, 495–502. 10.1016/j.rmed.2012.12.007 [DOI] [PubMed] [Google Scholar]
- Sanchis, J. , Gich, I. , & Pedersen, S. (2016). Systematic review of errors in inhaler use: Has patient technique improved over time? Chest, 150, 394–406. 10.1016/j.chest.2016.03.041 [DOI] [PubMed] [Google Scholar]
- Sangita, P. , Gharti, K. P. , & Laxman, B. (2015). Assessment of inhalation techniques in COPD patients using metered‐dose inhaler and rotahaler at a tertiary care hospital in Nepal. International Research Journal of Pharmacy, 6(5), 288–293. [Google Scholar]
- Scichilone, N. , Benfante, A. , Bocchino, M. , Braido, F. , Paggiaro, P. , Papi, A. , … Sanduzzi, A. (2015). Which factors affect the choice of the inhaler in chronic obstructive respiratory diseases? Pulmonary Pharmacology and Therapeutics, 31, 63–67. 10.1016/j.pupt.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Stallberg, B. , Janson, C. , Johansson, G. , Larsson, K. , Stratelis, G. , Telg, G. , & Lisspers, K. H. (2014). Management, morbidity and mortality of COPD during an 11‐year period: An observational retrospective epidemiological register study in Sweden (PATHOS). Primary Care Respiratory Journal, 23, 38–45. 10.4104/pcrj.2013.00106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takaku, Y. , Kurashima, K. , Ohta, C. , Ishiguro, T. , Kagiyama, N. , Yanagisawa, T. , & Takayanagi, N. (2017). How many instructions are required to correct inhalation errors in patients with asthma and chronic obstructive pulmonary disease? Respiratory Medicine, 123, 110–115. 10.1016/j.rmed.2016.12.012 [DOI] [PubMed] [Google Scholar]
- Taylor, T. E. , Zigel, Y. , De Looze, C. , Sulaiman, I. , Costello, R. W. , & Reilly, R. B. (2018). Advances in audio‐based systems to monitor patient adherence and inhaler drug delivery. Chest, 153, 710–722. 10.1016/j.chest.2017.08.1162 [DOI] [PubMed] [Google Scholar]
- Usmani, O. S. , Lavorini, F. , Marshall, J. , Dunlop, W. C. N. , Heron, L. , Farrington, E. , & Dekhuijzen, R. (2018). Critical inhaler errors in asthma and COPD: A systematic review of impact on health outcomes. Respiratory Research, 19, 10 10.1186/s12931-017-0710-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerik, J. A. , Carter, V. , Chrystyn, H. , Burden, A. , Thompson, S. L. , Ryan, D. , … Price, D. B. (2016). Characteristics of patients making serious inhaler errors with a dry powder inhaler and association with asthma‐related events in a primary care setting. Journal of Asthma, 53, 321–329. 10.3109/02770903.2015.1099160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieshammer, S. , & Dreyhaupt, J. (2008). Dry powder inhalers: Which factors determine the frequency of handling errors? Respiration, 75, 18–25. 10.1159/000109374 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


