Abstract
Background
Many infants worldwide are not breastfeeding according to WHO recommendations and this impacts on the health of women and children. Increasing breastfeeding is identified as a priority area supported by current policy targets. However, interventions are complex and multi-component and it is unclear which elements of interventions are most effective to increase breastfeeding in which settings. Breastfeeding counselling is often part of complex interventions but evidence is lacking on the specific effect of counselling interventions on breastfeeding practices. The aim of this systematic review is to examine evidence on effectiveness of breastfeeding counselling to inform global guidelines.
Methods
A systematic search was conducted of six electronic databases in January 2018. Randomised controlled trials comparing breastfeeding counselling with no breastfeeding counselling or different formulations of counselling were included if they measured breastfeeding practices between birth and 24 months after birth.
Results
From the 5180 records identified in searches and a further 11 records found by hand searching, 63 studies were included. Of these, 48 were individually-randomised trials and 15 were cluster-randomised trials. A total of 69 relevant comparisons were reported involving 33,073 women. There was a significant effect of counselling interventions on any breastfeeding at 4 to 6 weeks (Relative risk [RR] 0.85, 95% CI 0.77, 0.94) and 6 months (RR 0.92, 95% CI 0.87, 0.94). Greater effects were found on exclusive breastfeeding at 4 to 6 weeks (RR 0.79, 95% CI 0.72, 0.87) and 6 months (RR 0.84, 95% CI 0.78, 0.91). Counselling delivered at least four times postnatally is more effective than counselling delivered antenatally only and/or fewer than four times. Evidence was mostly of low quality due to high or unclear risk of bias of the included trials and high heterogeneity.
Conclusions
Breastfeeding counselling is an effective public health intervention to increase rates of any and exclusive breastfeeding. Breastfeeding counselling should be provided face-to-face, and in addition, may be provided by telephone, both antenatally and postnatally, to all pregnant women and mothers with young children. To inform scale-up globally there is a need to further understand the elements of breastfeeding interventions such as counselling and their effectiveness in different contexts and circumstances.
Study registration
This systematic review was registered in Prospero (CRD42018086494).
Keywords: Breastfeeding, Counselling, Intervention, Randomised control trial, Systematic review, Meta-analysis
Background
From a global perspective, the prevalence of breastfeeding varies widely, with high-income countries continually faring worse than middle- and low-income countries on nearly every standard breastfeeding indicator (i.e., from ‘ever breastfed’ to ‘breastfeeding at 12 months’ [1]). It has been estimated that infant mortality rates are nearly 12% higher when infants are not breastfed due to infections and illnesses such as pneumonia and diarrhoea [2], therefore breastfeeding has the largest known impact of any preventive intervention [3]. Additionally, the impact of breastfeeding, particularly exclusive breastfeeding, on an infant’s healthy growth and development have been well documented and not breastfeeding increases several conditions, including gastroenteritis, respiratory tract infections, obesity, and neurodevelopmental behavioural problems [4–6]. Mothers who do not breastfeed also have increased risks of breast and ovarian cancer, obesity, type II diabetes and postpartum depression [6–8]. It is therefore not surprising that exclusive breastfeeding has been identified as a priority area, with global targets recently increased from 50% of children being exclusively breastfed at 6 months by 2025 to at least 70% by 2030 [9]. A call for scaling up programming efforts to achieve these goals has been put forward, yet the question remains as to which elements of past and current preventative intervention programming are most effective in increasing standard breastfeeding indicators.
Both design and implementation of public health preventive interventions targeting breastfeeding indicators are vastly heterogeneous and often multi-component, making the ability to concisely evaluate which specific elements are most effective challenging. For example, preventative interventions vary in type (e.g., counselling, education, Baby-Friendly Hospital Initiative (BFHI), support, media and mass-marketing), setting (e.g., hospital, health facility, community/home), mode (e.g., group, individual, telephone, face-to-face), provider (e.g., healthcare professional, layperson/peer) stage of delivery (e.g., antenatal, postpartum), and frequency. Moreover, consensus and standard definitions, particularly related to types of preventative interventions, are lacking and often ill-defined. Recent systematic reviews have aimed to evaluate the efficacy that differing programming efforts have had in increasing standard breastfeeding indicators [10–15]. While these reviews all report effectiveness of interventions to increase breastfeeding rates, the effect size varies dependant on the review inclusion criteria and outcomes assessed.
While these reviews have advanced our knowledge regarding evaluation of best practices, gaps in the knowledge base remain. This is in part due to considerable heterogeneity in interventions and outcomes, and is compounded by poor reporting on/definitions of the differing ‘types’ of interventions. A systematic review by Sinha et al. [14], found that interventions that are complex and delivered in a combination of settings (e.g. interventions involving health systems, such as the BFHI were most effective). However, it is difficult to identify which elements of such complex, multi-component interventions are effective in which settings. Breastfeeding counselling is often part of complex interventions but evidence is lacking on the specific effect of counselling interventions on breastfeeding practices.
Barriers in operationalising what counselling specifically entails is a consistent shortcoming in published studies and protocols. When the term ‘counselling’ is used there is often much overlap with other types of preventative interventions such as education, resulting in difficultly in differentiating between the two. The World Health Organization (WHO) defines breastfeeding counselling as the support of mothers and infants, as provided by healthcare workers, in decision-making, overcoming difficulties, and implementation of optimal feeding practices [16, 17]. A key element is the interaction that takes places between a healthcare worker and mother, which should support women and their decision making. Counselling is therefore a type of preventative intervention which places emphasis on the dyadic interaction between a healthcare worker and a mother, rather than the top-down approach often more characteristic of education-based types of interventions. Counselling is therefore a type of support delivered directly to mothers and infants. All counselling can be considered support but not all support interventions involve counselling. For example, this review does not include studies of only higher-level interventions such as additional training for staff providing support [18–20] or policy interventions [21].
The aim of this systematic review and meta-analysis was to examine the evidence on the effectiveness of breastfeeding counselling to inform global guidelines [22].
Methods
This systematic review followed the Cochrane Collaboration guidance [23], and was registered in Prospero (CRD42018086494).
Search strategy
We searched six electronic databases: WHO International Clinical Trials Registry; clinicaltrials.gov; Cochrane Trials Register, Medline, CINAHL and Embase in January 2018, using the key search terms “breastfeeding” AND “counselling” AND “trials” (see Additional file 1 for detailed search strategy in Medline). We did not apply any language or date restrictions. We also scanned reference lists of three relevant systematic reviews [11, 14, 15]. Title, abstracts and potentially relevant full texts were screened independently by two authors and any disagreement resolved through discussion and consultation with a third author.
Inclusion criteria
Studies were included if they were randomised (including cluster-randomised, or quasi-randomised controlled), involving pregnant women considering or intending to breastfeed, or women who may initiate or are breastfeeding. Eligible interventions were those described as (or containing elements of) breastfeeding counselling. For the purposes of this review breastfeeding counselling was defined as a process by which a health worker supports mothers and infants to implement optimal feeding practices and helps them to overcome difficulties, involving interaction with a woman to support her in solving actual or anticipated problems, reviewing options, and making decisions. Interventions described as ‘counselling’ but where insufficient detail was reported to judge whether it met the above definition were included, as were interventions described as education or home visits that included features of counselling such as discussion of breastfeeding goals, challenges and techniques. Eligible comparisons were no breastfeeding counselling or different formulations of counselling. To be included, studies had to report at least one of the following outcomes:
Number of women who do not initiate breastfeeding within 1 h of birth;
- Number of women who stop any breastfeeding before 6 months as assessed at two time-points:
- ◦ Four to six weeks postpartum;
- ◦ Six months postpartum;
- Number of women who stop exclusive breastfeeding before 6 months as assessed at two time-points:
- ◦ Four to six weeks postpartum;
- ◦ Six months postpartum;
Number of women who stop any breastfeeding before 12 months postpartum;
Number of women who stop any breastfeeding before 24 months postpartum;
Number of newborns given prelacteal or additional food, fluids or infant formula within the first 3 days postpartum;
Number of infants fed with bottles during the first 6 months postpartum. For this outcome we included studies that reported the number of infants fed with bottles at the last study assessment.
Exclusion criteria
Non-randomised designs were excluded as were interventions targeted only at families, communities or healthcare providers. We excluded interventions that did not include any elements of the above definition of breastfeeding counselling, and multi-component interventions where the effects could not be attributed only to counselling.
Data extraction, risk of bias and quality of evidence assessment
Two authors independently extracted information using a specifically designed data extraction form. Any discrepancies were resolved through discussion. When information regarding study methods and results was unclear, we attempted to contact authors to provide further details. Two authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions [23]. Any disagreement was resolved by discussion with a third assessor. We used the GRADE approach [24] to assess the quality of the evidence.
Data analysis and synthesis
Cluster randomised trial sample sizes were adjusted, incorporating an estimate of the intra-cluster correlation coefficient (ICC) derived from the trial (if possible) to calculate an effective sample size. To avoid ‘double counting’ in multi-arm studies, we split the control group number of events and participants in half to enable two independent comparisons. For all outcomes, analyses were carried out, where possible, on an intention-to-treat basis. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
We carried out statistical analysis using Review Manager 5 software [25]. We used random-effects meta-analysis for combining data where significant statistical heterogeneity was present. The average treatment effects with 95% confidence intervals are presented.
Subgroup analysis
Where data were available, we carried out the following seven main subgroup analyses for all review outcomes: timing, frequency, mode, provider of counselling, involvement of anticipatory approaches, setting, and counselling targeted for specific population sub-groups.
Sensitivity analysis
We carried out sensitivity analysis for all outcomes by study quality by dividing the studies according to whether they were at low risk of bias as opposed to unclear or high risk of bias for allocation concealment.
Results
Results of the search
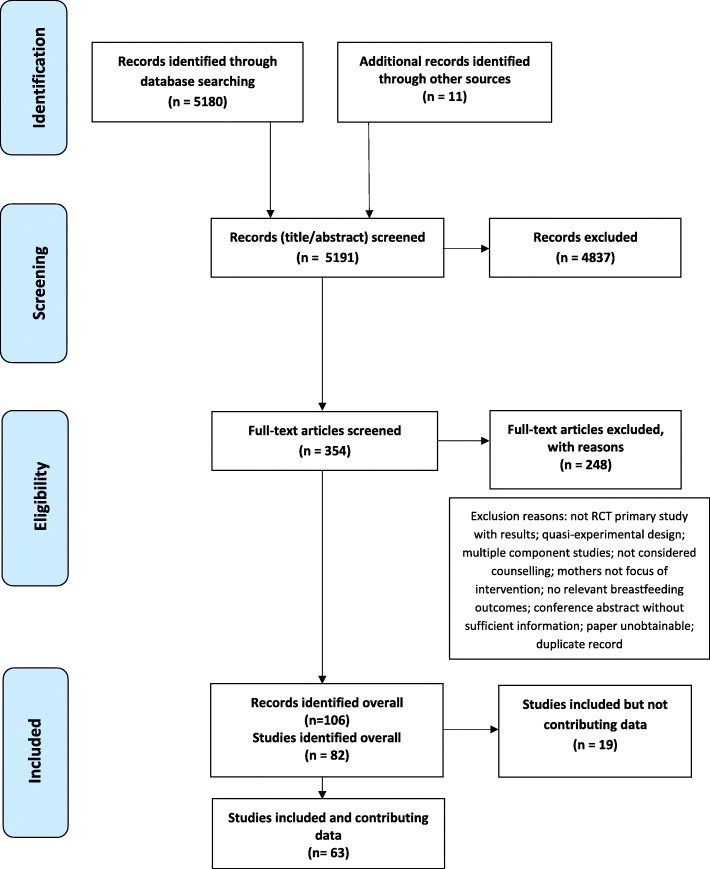
The searches resulted in 5180 original records and a further 11 records were identified through checking reference lists of included studies and published systematic reviews. We excluded 4837 titles and abstracts. We assessed 354 full text articles and excluded 248, leaving 106 articles reporting 82 studies (see Fig. 1). Nineteen studies were subsequently excluded from the analyses because they did not report data in a useable form or did not report relevant outcomes [26–44]. Therefore 63 studies contributed data to the analyses (see Fig. 1). Of note, two trials were published in a single paper [45]. To differentiate we refer to the BINGO trial as Bonuck (BINGO) [45] and the PAIRINGS trial as Bonuck (PAIRINGS) [45]. Additionally, the PROMISE-EBF trial [46] was conducted in three countries which we have classed as three separate trials due to substantial differences between countries in the trial methods and comparators. The 63 studies comprised 48 individually-randomised and 15 cluster-randomised trials. The 63 trials incorporated 69 comparisons as six studies [47–52] had two relevant interventions in different trial arms. These are referred to separately by the author name and the relevant feature of the trial arm (e.g. home based or facility based). More specifically, Aidam AN & PN [47] refers to counselling provided in the antenatal and postnatal period and Aidam PN [47] refers to counselling provided in the postnatal period only. Fu Hospital [48] refers to in-hospital visits only and Fu Telephone refers to telephone calls only. McLachlan [49] Home refers to a home visiting intervention and McLachlan Drop-in refers to home visiting plus access to a community-based breastfeeding drop-in centre. Morrow [50] three visits and Morrow six visits refer to the number of visits in different intervention arms. Ochola [51] Facility refers to counselling delivered in a healthcentre and Ochola Home refers to counselling delivered in the home. Su [52] AN refers to counselling delivered in the antenatal period only and Su PN refers to counselling delivered in the postnatal period only. See Additional file 2 for further details of all included studies (n = 63).
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart
Participants and settings
The participants in the 63 trials comprised 33,073 women and their infants (range 41–9675) from 26 countries. Almost two thirds of the studies, representing 76% of the participants, were from 10 high-income countries (40 studies; 25,223 participants). Fourteen studies, involving 3236 participants (10% of participants) were from nine upper middle-income countries. Seven studies involving 3055 participants (9% of participants) were from five lower middle-income countries. Two studies, both from the PROMISE-EBF trial [46], involving 1559 participants (5% of the total number of participants) were from two low-income countries, Burkina Faso and Uganda.
The 63 studies encompassed a broad range of participant characteristics. For example, mean age was most commonly in the 20 to 30 year range (32 studies) with eight studies having a mean of over 30 years and just one study of women under 20 years [53]. In the remaining studies age was unclear or not reported.
Two thirds (n = 42) of the studies included both primiparous and multiparous women, while seven included only primiparous women and seven studies did not report parity. Four studies excluded women who had caesarean births [54–57], while the remaining studies either included both vaginal and caesarean births or did not report mode of birth. Most studies included only healthy term newborns with no congenital anomalies or admission to neonatal unit. One study recruited only low birthweight infants [56], another recruited only preterm infants [58], one study was of twin births only [59] and another included only those who were jaundiced [60].
Interventions
A broad range of interventions was apparent across the 63 studies. The amount and nature of counselling along with detail of interventions reported varied considerably. Interventions commonly included an element of education, for example, about the importance and benefits to health of exclusive breastfeeding, but women were usually also encouraged to ask questions and raise concerns [47, 48, 56, 61, 62]. Many interventions included the provision of technical information and support for practical aspects of breastfeeding, for example giving advice or ensuring the baby was breastfeeding effectively e.g. [50, 63–68] or counselling to manage problems [57, 69, 70].
The timing, frequency and intensity of contacts varied considerably across the 69 interventions. Most interventions were provided only after birth (n = 35) or had antenatal and postnatal components (n = 26). The majority of postnatal interventions (whether there was an antenatal component or not) included at least one contact during the first 6 days following birth (n = 43). Eight interventions were provided only in the antenatal period and one study did not clearly report when the intervention was provided [71]. The number of sessions ranged from one to 24 scheduled contacts with over half of the interventions including more than four contacts (n = 39).
More than two thirds of interventions were provided to women one-to-one (n = 51) whereas some interventions included one-to-one and group contacts (n = 7). Sessions were less often provided only to groups of women (n = 3) [59, 72, 73] and one study involved two supporters for each mother [57]. The majority of interventions were provided face-to-face (n = 37) but many also incorporated counselling by telephone (n = 28) and three interventions were delivered by telephone only [55, 74, 75]. Interventions were provided by a range of personnel and volunteers and were categorized into lay (peer, community health workers, doulas) or non-lay (health professionals, lactation consultants/counsellors, breastfeeding consultants/counsellors and researchers). In several trials members of the research team delivered the intervention, and it was not always clear whether these personnel were health professionals. In many studies specific training was provided to counsellors but this was often poorly reported. When reported, the content and length of the training were variable (e.g. some had no training; brief orientation; between 6 and 40 h or 2 weeks).
Comparisons
Most comparisons were described in the studies as usual or standard care and in ten studies this included either care in a UNICEF/WHO accredited hospital [50, 63, 66, 76, 77], working towards accreditation [78] or a session using UNICEF/WHO guidelines [57, 59, 61, 75]. In 11 studies extra contacts were provided either to support women with different aspects such as breast examination or infant safety, or to provide counselling that was not breastfeeding related such as general nutrition counselling.
Risk of bias
Included studies were judged to be of mixed risk of bias across all domains. For example, just under half (49%) were judged to be at low risk of bias for allocation concealment; 40% were judged to be at low risk of bias for blinding of outcome assessment and 46% were judged to be of low risk of bias for incomplete outcome data. It was difficult to assess selective outcome reporting because so few studies referred to a registered/published protocol. All studies were judged to be at high or unclear risk of performance bias as it is not possible to blind participants and personnel to counselling interventions.
Effects of interventions
Counselling interventions compared to no counselling/standard care
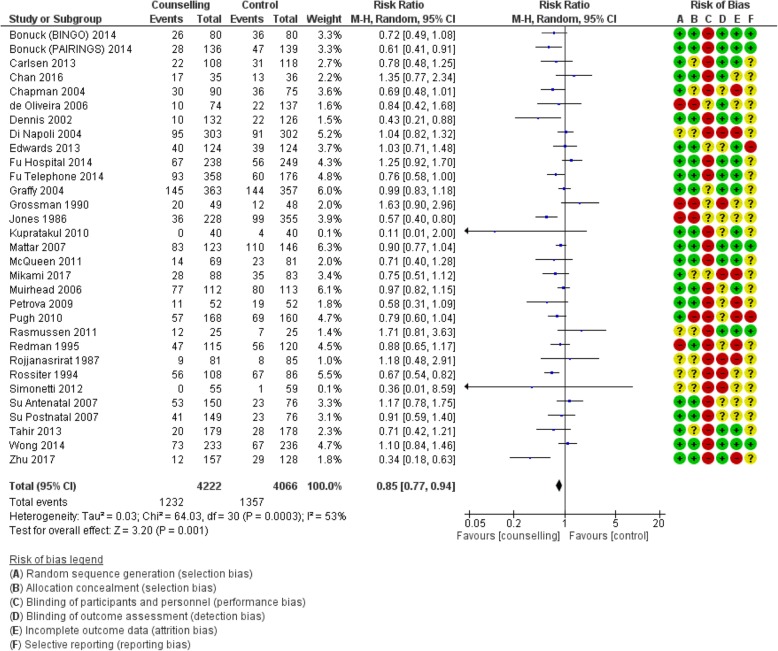
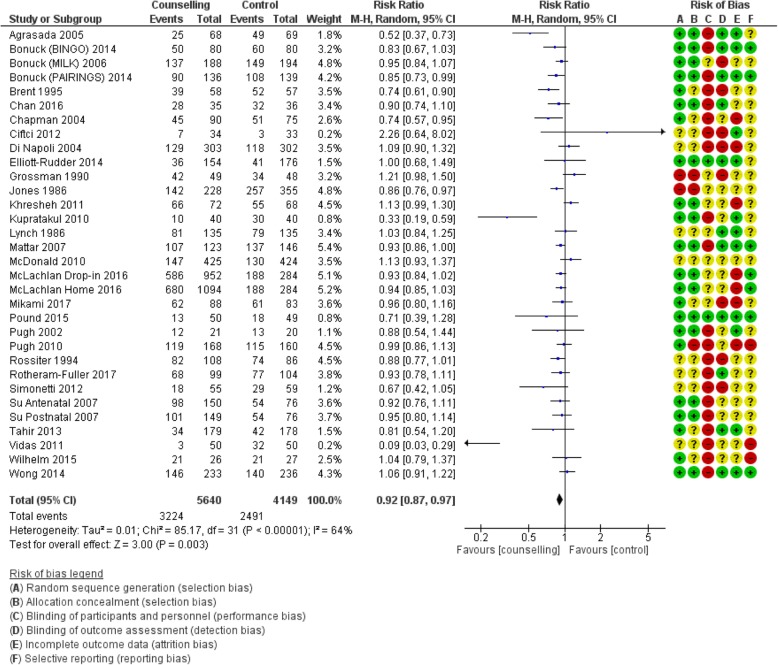
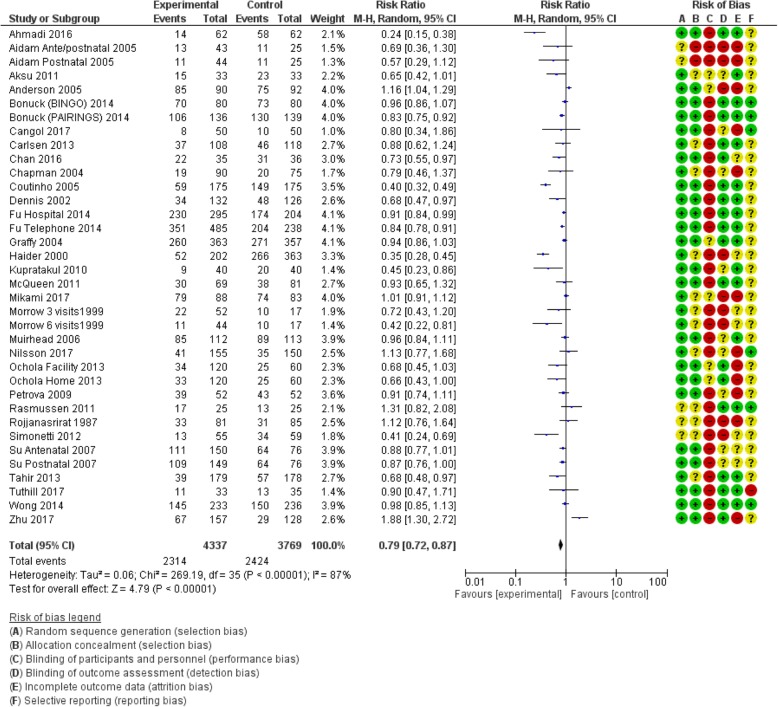
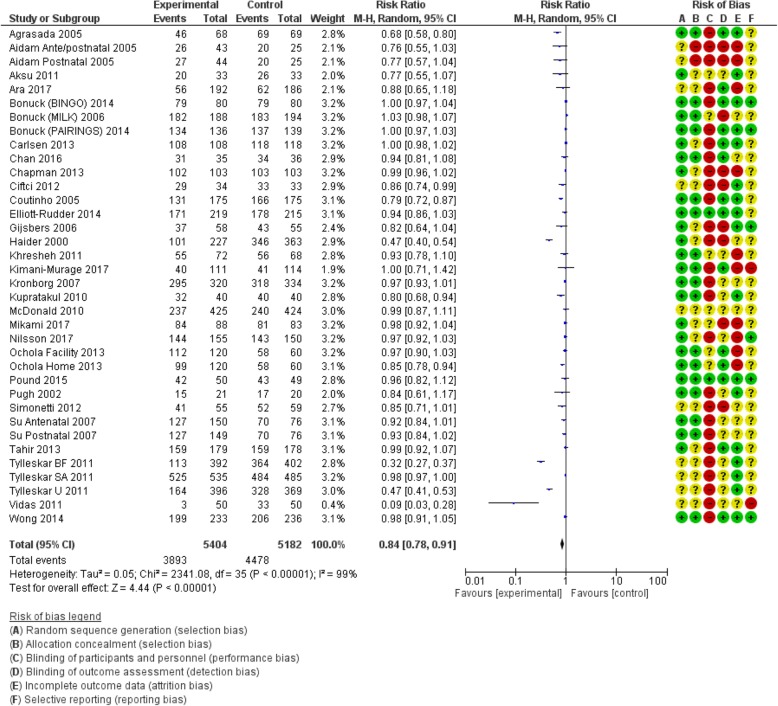
Table 1 shows the pooled effects of counselling interventions on eight of the nine outcomes of this review; no trials assessed breastfeeding rates at 24 months. Counselling interventions reduced the risk of women stopping any breastfeeding at 4 to 6 weeks by 15% (risk ratio [RR] 0.85, 95% confidence interval [CI] 0.77,0.94), and at 6 months by 8% (RR 0.92, CI 0.87,0.97). For exclusive breastfeeding the effect was greater with a 21% (RR 0.79, CI 0.72, 0.87) reduction at 4 to 6 weeks and a 16% (RR 0.84, CI 0.78, 0.91) reduction at 6 months. Sensitivity analyses demonstrated a similar positive effect. Statistical heterogeneity was significant for all outcomes: any breastfeeding at 4 to 6 weeks Tau2 = 0.03, I2 = 53%, Chi2 = 64.03, p < 0.0003); any breastfeeding at 6 months Tau2 = 0.01, I2 = 64%, Chi2 = 85.17, p < 0.00001; exclusive breastfeeding at 4 to 6 weeks (Tau2 = 0.06, I2 = 87%, Chi2 = 269.19, p < 0.00001); exclusive breastfeeding at 6 months (Tau2 = 0.05, I2 = 99%, Chi2 = 2341.08, p < 0.00001). The quality of the evidence was low due to high or unclear risk of bias and high unexplained heterogeneity (Figs. 2, 3, 4 and 5).
Table 1.
Effects of counselling versus no counselling
| Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | ||
| Number of women who do not initiate breastfeeding within 1 h of birth | |||||
| 7 trials | 1038/1913 (54.3%) | 1188/1818 (65.3%) | RR 0.74 (0.53 to 1.02) | 170 fewer per 1000 (from 13 more to 307 fewer) | Moderate |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | |||||
| 29 trials (31 comparisons) | 1232/4222 (29.2%) | 1357/4066 (33.4%) | RR 0.85 (0.77 to 0.94) | 50 fewer per 1000 (from 20 fewer to 77 fewer) | Low |
| Number of women who stop any breastfeeding before 6 months postpartum | |||||
| 30 trials (32 comparisons) | 3224/5640 (57.2%) | 2491/4149 (60.0%) | RR 0.92 (0.87 to 0.97) | 48 fewer per 1000 (from 18 fewer to 78 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | |||||
| 31 trials (36 comparisons) | 2314/4337 (53.4%) | 2424/3769 (64.3%) | RR 0.79 (0.72 to 0.87) | 135 fewer per 1000 (from 84 fewer to 180 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | |||||
| 33 trials (36 comparisons) | 3893/5404 (72.0%) | 4478/5182 (86.4%) | RR 0.84 (0.78 to 0.91) | 138 fewer per 1000 (from 78 fewer to 190 fewer) | Low |
| Number of women who stop any breastfeeding before 12 months postpartum | |||||
| 2 trials | 349/416 (83.9%) | 516/549 (94.0%) | RR 0.88 (0.69 to 1.12) | 113 fewer per 1000 (from 113 more to 291 fewer) | Low |
| Number of newborns given prelacteal or additional food, fluids or infant formula within the first 2 days postpartum | |||||
| 1 trial | 26/50 (52.0%) | 40/50 (80.0%) | RR 0.65 (0.48 to 0.88) | 280 fewer per 1000 (from 96 fewer to 416 fewer) | Low |
| Number of infants fed with bottles during the first 6 months postpartum | |||||
| 5 trials | 349/416 (83.9%) | 516/549 (94.0%) | RR 0.88 (0.69 to 1.12) | 113 fewer per 1000 (from 113 more to 291 fewer) | Moderate |
Fig. 2.
Number of women who stop any breastfeeding before 4–6 weeks postpartum
Fig. 3.
Number of women who stop any breastfeeding before 6 months postpartum
Fig. 4.
Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum
Fig. 5.
Number of women who stop exclusive breastfeeding before 6 months postpartum
The pooled effects of counselling interventions on the number of women who did not initiate breastfeeding within 1 h of birth, the number of women who stopped breastfeeding at 12 months and the number of infants fed with bottles during the first 6 months were not statistically significant. One trial of 100 women [79] provided moderate quality evidence that counselling interventions reduced the number of infants given prelacteal or other additional food, fluids or infant formula in the first 3 days of life by 35% (RR 0.65, CI 0.48,0.88).
Sub-group analyses: intervention characteristics
Because of the low number of relevant trials, we did not conduct sub-group analyses for two outcomes: number of women who stop breastfeeding at 12 months (two trials), and number of newborns given prelacteal or other foods or fluids within the first 2 days following birth (one trial).
Timing
Table 2 shows the effects of counselling interventions according to whether the intervention was provided antenatally, postnatally, or both. For ‘any breastfeeding’, six trials provided low quality evidence that counselling interventions delivered both antenatally and postnatally were more effective in reducing the risk of women stopping any breastfeeding before 6 months (21% reduction, RR 0.79, CI 0.67,0.93) compared to those provided only in the antenatal or postnatal periods. For exclusive breastfeeding at both time points, counselling interventions with a postnatal component were more effective than counselling delivered antenatally only. For example, based on 15 trials involving 5411 women, counselling interventions with antenatal and postnatal components reduced the risk of women stopping exclusive breastfeeding before 6 months by 29% (RR 0.71, CI 0.55, 0.93). The quality of evidence was low due to high or unclear risk of bias and high unexplained heterogeneity. One trial [72] provided evidence that counselling in the antenatal period only reduced the risk of women not initiating breastfeeding within 1 h of birth although this trial was at high risk of bias. Moderate evidence from three trials (659 women) suggested that counselling interventions provided postnatally only reduce the risk of infants being fed with bottles during the first 6 months, by 23% (RR 0.77, CI 0.68,0.87).
Table 2.
Effects of different timings of interventions
| Time intervention delivered | Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | |||
| Number of women who do not initiate breastfeeding within 1 h of birth | ||||||
| Antenatal only | 1 trial | 35/108 (32.4%) | 58/86 (67.4%) | RR 0.48 (0.35 to 0.65) | 351 fewer per 1000 (from 236 fewer to 438 fewer) | Low |
| Antenatal and postnatal | 6 trials | 1003/1805 (55.6%) | 1130/1732 (65.2%) | RR 0.79 (0.57 to 1.08) | 137 fewer per 1000 (from 52 more to 281 fewer) | Low |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | ||||||
| Antenatal only | 6 trials | 319/782 (40.8%) | 338/707 (47.8%) | RR 0.86 (0.72 to 1.03) | 67 fewer per 1000 (from 14 more to 134 fewer) | Low |
| Postnatal only | 12 trials (13 comparisons) | 461/2039 (22.6%) | 467/1838 (25.4%) | RR 0.83 (0.69 to 1.00) | 43 fewer per 1000 (from 0 fewer to 79 fewer) | Low |
| Antenatal and postnatal | 11 trials | 416/1173 (35.5%) | 453/1166 (38.9%) | RR 0.91 (0.78 to 1.05) | 35 fewer per 1000 (from 19 more to 85 fewer) | Moderate |
| Number of women who stop any breastfeeding before 6 months postpartum | ||||||
| Antenatal only | 6 trials | 545/782 (69.7%) | 526/707 (74.4%) | RR 0.93 (0.88 to 0.98) | 52 fewer per 1000 (from 15 fewer to 89 fewer) | Moderate |
| Postnatal only | 18 trials (19 comparisons) | 2188/4083 (53.6%) | 1286/2546 (50.5%) | RR 0.96 (0.88 to 1.04) | 20 fewer per 1000 (from 20 more to 61 fewer) | Low |
| Antenatal and postnatal | 6 trials | 334/547 (61.1%) | 407/541 (75.2%) | RR 0.79 (0.67 to 0.93) | 158 fewer per 1000 (from 53 fewer to 248 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | ||||||
| Antenatal only | 6 trials | 450/704 (63.9%) | 399/570 (70.0%) | RR 0.95 (0.89 to 1.02) | 35 fewer per 1000 (from 14 more to 77 fewer) | Moderate |
| Postnatal only | 12 trials (13 comparisons) | 1009/1943 (51.9%) | 935/1503 (62.2%) | RR 0.71 (0.59 to 0.85) | 180 fewer per 1000 (from 93 fewer to 255 fewer) | Low |
| Antenatal and postnatal | 16 trials (17 comparisons) | 855/1690 (50.6%) | 1090/1696 (64.3%) | RR 0.81 (0.69 to 0.94) | 122 fewer per 1000 (from 39 fewer to 199 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | ||||||
| Antenatal only | 5 trials | 601/671 (89.6%) | 494/535 (92.3%) | RR 0.98 (0.96 to 1.01) | 18 fewer per 1000 (from 9 more to 37 fewer) | Moderate |
| Postnatal only | 16 trials | 1483/2002 (74.1%) | 1575/1926 (81.8%) | RR 0.88 (0.81 to 0.96) | 98 fewer per 1000 (from 33 fewer to 155 fewer) | Low |
| Antenatal and postnatal | 15 trials | 1663/2718 (61.2%) | 2334/2693 (86.7%) | RR 0.71 (0.55 to 0.93) | 251 fewer per 1000 (from 61 fewer to 390 fewer) | Low |
| Number of infants fed with bottles during the first 6 months postpartum | ||||||
| Postnatal only | 3 trials | 143/331 (43.2%) | 188/328 (57.3%) | RR 0.77 (0.68 to 0.87) | 132 fewer per 1000 (from 75 fewer to 183 fewer) | Moderate |
| Antenatal and postnatal | 2 trials | 260/398 (65.3%) | 280/393 (71.2%) | RR 0.92 (0.85 to 1.00) | 57 fewer per 1000 (from 0 fewer to 107 fewer) | Moderate |
Frequency
Table 3 shows the pooled effect of counselling interventions categorised by whether counselling was delivered fewer than four times or four or more times. Interventions delivered four or more times showed a statistically significant effect on both any and exclusive breastfeeding, but the effect size was greater for exclusive breastfeeding. The greatest effect was for exclusive breastfeeding at 4 to 6 weeks, which showed a 31% (RR 0.69, CI 0.58, 0.82) reduction in the risk of women stopping breastfeeding. The comparative reduction for the same outcome for counselling delivered on fewer than four occasions was 8% (RR 0.92, CI 0.88, 0.97). The evidence was low quality due to high or unclear risk of bias and high unexplained heterogeneity. There was high quality evidence from one trial involving 350 women [61] that counselling interventions with four or more contacts reduced the risk of infants being fed with bottles in the first 6 months by 23% (RR 0.77, CI 0.68, 0.88).
Table 3.
Effects of different frequencies of interventions
| Frequency of intervention | Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | |||
| Number of women who do not initiate breastfeeding within 1 h of birth | ||||||
| < 4 times | 1 trial | 35/108 (32.4%) | 58/86 (67.4%) | RR 0.48 (0.35 to 0.65) | 351 fewer per 1000 (from 236 fewer to 438 fewer) | Very low |
| ≥ 4 times | 6 trials | 1003/1805 (55.6%) | 1130/1732 (65.2%) | RR 0.79 (0.57 to 1.08) | 137 fewer per 1000 (from 52 more to 281 fewer) | Low |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | ||||||
| < 4 times | 14 trials (15 comparisons) | 733/2129 (34.4%) | 725/2050 (35.4%) | RR 0.95 (0.84 to 1.07) | 18 fewer per 1000 (from 25 more to 57 fewer) | Low |
| ≥ 4 times | 15 trials | 463/1865 (24.8%) | 533/1661 (32.1%) | RR 0.77 (0.66 to 0.90) | 74 fewer per 1000 (from 32 fewer to 109 fewer) | Low |
| Number of women who stop any breastfeeding before 6 months postpartum | ||||||
| < 4 times | 13 trials (14 comparisons) | 1599/2675 (59.8%) | 1029/1720 (59.8%) | RR 0.96 (0.92 to 1.01) | 24 fewer per 1000 (from 6 more to 48 fewer) | Moderate |
| ≥ 4 times | 16 trials | 882/1785 (49.4%) | 1002/1790 (56.0%) | RR 0.85 (0.75 to 0.96) | 84 fewer per 1000 (from 22 fewer to 140 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | ||||||
| < 4 times | 15 trials (16 comparisons) | 1178/1971 (59.8%) | 1036/1629 (63.6%) | RR 0.92 (0.88 to 0.97) | 51 fewer per 1000 (from 19 fewer to 76 fewer) | Moderate |
| ≥ 4 times | 19 trials (20 comparisons) | 1136/2366 (48.0%) | 1388/2140 (64.9%) | RR 0.69 (0.58 to 0.82) | 201 fewer per 1000 (from 117 fewer to 272 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | ||||||
| < 4 times | 12 trials (13 comparisons) | 1444/1682 (85.9%) | 1326/1471 (90.1%) | RR 0.96 (0.94 to 0.98) | 36 fewer per 1000 (from 18 fewer to 54 fewer) | Moderate |
| ≥ 4 times | 22 trials (23 comparisons) | 2369/3709 (63.9%) | 3077/3683 (83.5%) | RR 0.76 (0.66 to 0.88) | 201 fewer per 1000 (from 100 fewer to 284 fewer) | Low |
| Number of infants fed with bottles during the first 6 months postpartum | ||||||
| < 4 times | 4 trials | 292/554 (52.7%) | 324/546 (59.3%) | RR 0.91 (0.82 to 1.01) | 53 fewer per 1000 (from 6 more to 107 fewer) | Moderate |
| ≥ 4 times | 1 trial | 111/175 (63.4%) | 144/175 (82.3%) | RR 0.77 (0.68 to 0.88) | 189 fewer per 1000 (from 99 fewer to 263 fewer) | High |
Mode of provision
We conducted sub-group analyses according to whether the counselling was delivered face-to-face, by telephone, or included a combination of both (see Table 4). The greatest effect was again for exclusive breastfeeding at 4 to 6 weeks where there was low quality evidence from 17 comparisons (3550 women) that face-to-face counselling reduced the risk of women stopping breastfeeding by a third (RR 0.67, CI 0.56, 0.81). For this outcome there was also a statistically significant effect of counselling by telephone, which reduced the risk of women stopping exclusive breastfeeding at 4 to 6 weeks by 28% (RR 0.72, CI 0.55, 0.95). For the outcome exclusive breastfeeding at 6 months, pooled analysis of interventions delivered face-to-face showed a statistically significant effect, reducing the risk of women stopping breastfeeding by 26% (RR 0.74, CI 0.63, 0.87). The pooled effects of counselling interventions on the number of women who did not initiate breastfeeding within 1 h of birth, and the number of infants fed with bottles during the first 6 months were not statistically significant.
Table 4.
Effects of different modes of interventions
| Mode of intervention | Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | |||
| Number of women who do not initiate breastfeeding within 1 h of birth | ||||||
| Face-to-face | 6 trials | 1022/1863 (54.9%) | 1167/1768 (66.0%) | RR 0.73 (0.52 to 1.03) | 178 fewer per 1000 (from 20 more to 317 fewer) | Very low |
| Face-to-face and telephone | 1 trial | 16/50 (32.0%) | 21/50 (42.0%) | RR 0.76 (0.45 to 1.28) | 101 fewer per 1000 (from 118 more to 231 fewer) | Very low |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | ||||||
| Face-to-face | 10 trials (11 comparisons) | 520/1586 (32.8%) | 594/1644 (36.1%) | RR 0.86 (0.75 to 1.00) | 51 fewer per 1000 (from 0 fewer to 90 fewer) | Low |
| Telephone | 4 trials | 135/700 (19.3%) | 120/531 (22.6%) | RR 0.75 (0.61 to 0.93) | 56 fewer per 1000 (from 16 fewer to 88 fewer) | Moderate |
| Face-to-face and telephone | 16 trials | 577/1936 (29.8%) | 643/1891 (34.0%) | RR 0.86 (0.73 to 1.01) | 48 fewer per 1000 (from 3 more to 92 fewer) | Low |
| Number of women who stop any breastfeeding before 6 months postpartum | ||||||
| Face-to-face | 13 trials (14 comparisons) | 893/1541 (57.9%) | 1001/1542 (64.9%) | RR 0.89 (0.81 to 0.98) | 71 fewer per 1000 (from 13 fewer to 123 fewer) | Low |
| Telephone | 2 trials | 52/234 (22.2%) | 71/237 (30.0%) | RR 0.74 (0.55 to 1.00) | 78 fewer per 1000 (from 0 fewer to 135 fewer) | Moderate |
| Face-to-face and telephone | 15 trials (16 comparisons) | 2264/3865 (58.6%) | 1404/2370 (59.2%) | RR 0.95 (0.88 to 1.02) | 30 fewer per 1000 (from 12 more to 71 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | ||||||
| Face-to-face | 13 trials (17 comparisons) | 1019/1923 (53.0%) | 1200/1627 (73.8%) | RR 0.67 (0.56 to 0.81) | 243 fewer per 1000 (from 140 fewer to 325 fewer) | Low |
| Telephone | 4 trials | 440/827 (53.2%) | 341/593 (57.5%) | RR 0.72 (0.55 to 0.95) | 161 fewer per 1000 (from 29 fewer to 259 fewer) | Moderate |
| Face-to-face and telephone | 15 trials | 855/1587 (53.9%) | 883/1549 (57.0%) | RR 0.96 (0.86 to 1.07) | 23 fewer per 1000 (from 40 more to 80 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | ||||||
| Face-to-face | 21 trials (24 comparisons) | 2587/3887 (66.6%) | 3196/3653 (87.5%) | RR 0.74 (0.63 to 0.87) | 227 fewer per 1000 (from 114 fewer to 324 fewer) | Low |
| Telephone | 3 trials | 285/342 (83.3%) | 306/355 (86.2%) | RR 0.96 (0.83 to 1.12) | 34 fewer per 1000 (from 103 more to 147 fewer) | Low |
| Face-to-face and telephone | 9 trials | 875/1162 (75.3%) | 901/1146 (78.6%) | RR 0.96 (0.91 to 1.01) | 31 fewer per 1000 (from 8 more to 71 fewer) | Low |
| Number of infants fed with bottles during the first 6 months postpartum | ||||||
| Face-to-face | 2 trials | 115/259 (44.4%) | 155/260 (59.6%) | RR 0.65 (0.34 to 1.23) | 209 fewer per 1000 (from 137 more to 393 fewer) | Low |
| Face-to-face and telephone | 3 trials | 288/490 (58.8%) | 313/461 (67.9%) | RR 0.77 (0.57 to 1.03) | 156 fewer per 1000 (from 20 more to 292 fewer) | Low |
Provider
Sub-group analysis was conducted according to whether the intervention was delivered by lay, non-lay personnel, or by both (Table 5). The largest effect was on reducing the risk of women not initiating breastfeeding within the first hour when counselling was delivered by non-lay personnel, the reduction being 42% based on low quality evidence from two trials (RR 0.58, CI 0.37, 0.90). As can be seen in Table 5, there were smaller effects of non-lay counselling on any breastfeeding at both assessed time-points. Counselling by lay, or combined lay and non-lay personnel reduced the risk of women stopping exclusive breastfeeding at 4 to 6 weeks by about a third, although the quality of evidence was low (lay: RR 0.64, CI 0.42,0.97; lay and non-lay: RR 0.67, CI 0.50,0.90), the effects were not statistically significant for exclusive breastfeeding at 6 months.
Table 5.
Effects of different providers of interventions
| Provider of intervention | Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | |||
| Number of women who do not initiate breastfeeding within 1 h of birth | ||||||
| Lay | 5 trials | 987/1755 (56.2%) | 1109/1682 (65.9%) | RR 0.79 (0.56 to 1.11) | 138 fewer per 1000 (from 73 more to 290 fewer) | Low |
| Non-lay | 2 trials | 51/158 (32.3%) | 79/136 (58.1%) | RR 0.58 (0.37 to 0.90) | 244 fewer per 1000 (from 58 fewer to 366 fewer) | Moderate |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | ||||||
| Lay | 4 trials | 157/458 (34.3%) | 177/438 (40.4%) | RR 0.82 (0.62 to 1.10) | 73 fewer per 1000 (from 40 more to 154 fewer) | Low |
| Non-lay | 24 trials (26 comparisons) | 1018/3596 (28.3%) | 1111/3468 (32.0%) | RR 0.86 (0.77 to 0.96) | 45 fewer per 1000 (from 13 fewer to 74 fewer) | Low |
| Both lay and non-lay | 1 trial | 57/168 (33.9%) | 69/160 (43.1%) | RR 0.79 (0.60 to 1.04) | 91 fewer per 1000 (from 17 more to 173 fewer) | Very low |
| Number of women who stop any breastfeeding before 6 months postpartum | ||||||
| Lay | 3 trials | 123/257 (47.9%) | 162/248 (65.3%) | RR 0.71 (0.48 to 1.04) | 189 fewer per 1000 (from 26 more to 340 fewer) | Moderate |
| Non-lay | 23 trials (24 comparisons) | 2359/4158 (56.7%) | 1963/3354 (58.5%) | RR 0.94 (0.89 to 0.99) | 35 fewer per 1000 (from 6 fewer to 64 fewer) | Low |
| Both lay and non-lay | 3 trials | 717/1141 (62.8%) | 316/464 (68.1%) | RR 0.95 (0.88 to 1.02) | 34 fewer per 1000 (from 14 more to 82 fewer) | Moderate |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | ||||||
| Lay | 8 trials (9 comparisons) | 382/930 (41.1%) | 690/1011 (68.2%) | RR 0.64 (0.42 to 0.97) | 246 fewer per 1000 (from 20 fewer to 396 fewer) | Low |
| Non-lay | 21 trials (24 comparisons) | 1851/3105 (59.6%) | 1626/2576 (63.1%) | RR 0.91 (0.85 to 0.96) | 57 fewer per 1000 (from 25 fewer to 95 fewer) | Low |
| Both lay and non-lay | 1 trial (2 comparisons) | 67/240 (27.9%) | 50/120 (41.7%) | RR 0.67 (0.50 to 0.90) | 137 fewer per 1000 (from 42 fewer to 208 fewer) | Moderate |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | ||||||
| Lay | 10 trials | 1241/2219 (55.9%) | 1937/2271 (85.3%) | RR 0.67 (0.30 to 1.51) | 281 fewer per 1000 (from 435 more to 597 fewer) | Very low |
| Non-lay | 19 trials 21 comparisons) | 2314/2827 (81.9%) | 2267/2660 (85.2%) | RR 0.97 (0.94 to 0.99) | 26 fewer per 1000 (from 9 fewer to 51 fewer) | Low |
| Both lay and non-lay | 2 trials (3 comparisons) | 160/261 (61.3%) | 133/140 (95.0%) | RR 0.61 (0.18 to 2.05) | 371 fewer per 1000 (from 779 fewer to 997 more) | Very low |
| Number of infants fed with bottles during the first 6 months postpartum | ||||||
| Lay | 2 trials | 115/259 (44.4%) | 155/260 (59.6%) | RR 0.65 (0.34 to 1.23) | 209 fewer per 1000 (from 137 more to 393 fewer) | Low |
| Non-lay | 3 trials | 288/490 (58.8%) | 313/461 (67.9%) | RR 0.77 (0.57 to 1.03) | 156 fewer per 1000 (from 20 more to 292 fewer) | Moderate |
Setting
For each outcome in sub-group analyses according to whether the intervention was delivered in an urban, rural or both urban and rural setting, there was low quality evidence of effect for urban settings and a lack of statistically significant findings for rural or combined settings (see Table 6).
Table 6.
Effects of interventions in different settings
| Setting of intervention | Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | |||
| Number of women who do not initiate breastfeeding within 1 h of birth | ||||||
| Urban | 2 trials | 80/300 (26.7%) | 117/272 (43.0%) | RR 0.59 (0.39 to 0.91) | 176 fewer per 1000 (from 39 fewer to 262 fewer) | Low |
| Rural | 1 trial | 378/392 (96.4%) | 388/402 (96.5%) | RR 1.00 (0.97 to 1.03) | 0 fewer per 1000 (from 29 fewer to 29 more) | Moderate |
| Urban and rural | 2 trials | 460/931 (49.4%) | 455/854 (53.3%) | RR 0.91 (0.64 to 1.29) | 48 fewer per 1000 (from 155 more to 192 fewer) | Very low |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | ||||||
| Urban | 21 trials (23 comparisons) | 978/3428 (28.5%) | 984/3032 (32.5%) | RR 0.85 (0.76 to 0.96) | 49 fewer per 1000 (from 13 fewer to 78 fewer) | Low |
| Rural | 1 trial | 12/25 (48.0%) | 7/25 (28.0%) | RR 1.71 (0.81 to 3.63) | 199 more per 1000 (from 53 fewer to 736 more) | Low |
| Number of women who stop any breastfeeding before 6 months postpartum | ||||||
| Urban | 19 trials (20 comparisons) | 1444/2680 (53.9%) | 1418/2496 (56.8%) | RR 0.91 (0.84 to 0.98) | 51 fewer per 1000 (from 11 fewer to 91 fewer) | Low |
| Rural | 2 trials | 57/180 (31.7%) | 62/203 (30.5%) | RR 1.03 (0.82 to 1.29) | 9 more per 1000 (from 55 fewer to 89 more) | Moderate |
| Urban and rural | 1 trial | 81/135 (60.0%) | 79/135 (58.5%) | RR 1.03 (0.84 to 1.25) | 18 more per 1000 (from 94 fewer to 146 more) | Low |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | ||||||
| Urban | 23 trials (28 comparisons) | 2031/3561 (57.0%) | 1893/2810 (67.4%) | RR 0.81 (0.74 to 0.89) | 128 fewer per 1000 (from 74 fewer to 175 fewer) | Low |
| Rural | 1 trial | 17/25 (68.0%) | 13/25 (52.0%) | RR 1.31 (0.82 to 2.08) | 161 more per 1000 (from 94 fewer to 562 more) | Low |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | ||||||
| Urban | 18 trials (21 comparisons) | 1757/2500 (70.3%) | 1697/2181 (77.8%) | RR 0.87 (0.81 to 0.93) | 101 fewer per 1000 (from 54 fewer to 148 fewer) | Low |
| Rural | 2 trials | 284/611 (46.5%) | 542/617 (87.8%) | RR 0.55 (0.15 to 1.95) | 395 fewer per 1000 (from 747 fewer to 835 more) | Very low |
| Urban and rural | 3 trials | 984/1251 (78.7%) | 1130/1188 (95.1%) | RR 0.77 (0.47 to 1.24) | 219 fewer per 1000 (from 228 more to 504 fewer) | Very low |
| Number of infants fed with bottles during the first 6 months postpartum | ||||||
| Urban | 3 trials | 371/573 (64.7%) | 424/568 (74.6%) | RR 0.87 (0.80 to 0.94) | 97 fewer per 1000 (from 45 fewer to 149 fewer) | Moderate |
Sub-group analyses: participant characteristics
Parity
We compared pooled effects of interventions provided for primiparous women only with those provided for both multiparous and primiparous women (see Table 7). Mostly, interventions provided for primiparous women specifically did not show statistically significant effects whereas those for primiparous and multiparous women did. For example, there was low quality evidence that the risk of women stopping exclusive breastfeeding at 4 to 6 weeks was reduced by 25% (RR 0.75, CI 0.65, 0.86) in primiparous and multiparous women. However, this effect was not significant in primiparous women. Conversely, interventions provided for primiparous women showed a 33% reduction in the number of infants fed with bottles compared to a non-statistically significant finding for interventions provided for primiparous and multiparous women.
Table 7.
Effects of interventions on women of different parity
| Setting of intervention | Number of trials | No of events | Effect | Certainty | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Relative (95% CI) | Absolute (95% CI) | |||
| Number of women who do not initiate breastfeeding within 1 h of birth | ||||||
| Primiparous | 1 trial | 16/50 (32.0%) | 21/50 (42.0%) | RR 0.76 (0.45 to 1.28) | 101 fewer per 1000 (from 118 more to 231 fewer) | Very low |
| Primiparous and multiparous | 5 trials | 987/1755 (56.2%) | 1109/1682 (65.9%) | RR 0.79 (0.56 to 1.11) | 138 fewer per 1000 (from 73 more to 290 fewer) | Low |
| Number of women who stop any breastfeeding before 4–6 weeks postpartum | ||||||
| Primiparous | 9 trials (10 comparisons) | 342/1473 (23.2%) | 335/1296 (25.8%) | RR 0.85 (0.67 to 1.08) | 39 fewer per 1000 (from 21 more to 85 fewer) | Low |
| Primiparous and multiparous | 19 trials (20 comparisons) | 834/2641 (31.6%) | 955/2684 (35.6%) | RR 0.87 (0.78 to 0.96) | 46 fewer per 1000 (from 14 fewer to 78 fewer) | Low |
| Number of women who stop any breastfeeding before 6 months postpartum | ||||||
| Primiparous | 6 trials | 322/521 (61.8%) | 357/525 (68.0%) | RR 0.84 (0.68 to 1.04) | 109 fewer per 1000 (from 27 more to 218 fewer) | Low |
| Primiparous and multiparous | 18 trials (20 comparisons) | 2694/4781 (56.3%) | 1899/3304 (57.5%) | RR 0.94 (0.89 to 0.99) | 34 fewer per 1000 (from 6 fewer to 63 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 4–6 weeks postpartum | ||||||
| Primiparous | 10 trials (11 comparisons) | 948/1625 (58.3%) | 772/1276 (60.5%) | RR 0.88 (0.77 to 1.00) | 73 fewer per 1000 (from 0 fewer to 139 fewer) | Low |
| Primiparous and multiparous | 20 trials (24 comparisons) | 1355/2679 (50.6%) | 1639/2458 (66.7%) | RR 0.75 (0.65 to 0.86) | 167 fewer per 1000 (from 93 fewer to 233 fewer) | Low |
| Number of women who stop exclusive breastfeeding before 6 months postpartum | ||||||
| Primiparous | 7 trials | 425/688 (61.8%) | 482/687 (70.2%) | RR 0.85 (0.75 to 0.97) | 105 fewer per 1000 (from 21 fewer to 175 fewer) | Moderate |
| Primiparous and multiparous | 23 trials (26 comparisons) | 3275/4598 (71.2%) | 3838/4364 (87.9%) | RR 0.81 (0.73 to 0.90) | 167 fewer per 1000 (from 88 fewer to 237 fewer) | Low |
| Number of infants fed with bottles during the first 6 months postpartum | ||||||
| Primiparous | 2 trials | 59/127 (46.5%) | 67/104 (64.4%) | RR 0.67 (0.49 to 0.91) | 213 fewer per 1000 (from 58 fewer to 329 fewer) | Moderate |
| Primiparous and multiparous | 2 trials | 340/538 (63.2%) | 390/532 (73.3%) | RR 0.84 (0.71 to 1.00) | 117 fewer per 1000 (from 0 fewer to 213 fewer) | Moderate |
We were unable to conduct several prespecified sub-group analyses due either to unclear reporting or lack of data. There was unclear reporting for counselling delivered by a provider with specialist training versus those without such training. Most of the interventions appeared to include some elements of anticipatory approaches, however these were not clearly described and therefore it was not possible to undertake analyses for this sub-category of interventions. There were insufficient data to conduct analyses for the following sub-groups: adolescent women (one study, [53], birth by caesarean section (no studies), multiple pregnancies (one study [59]), mothers planning to return to work (two studies [80, 81]), or mothers with high BMI [74].
Discussion
This review found that breastfeeding counselling is an effective public health intervention to increase rates of any and exclusive breastfeeding up to 6 months postpartum. Counselling interventions had a significant effect on any and exclusive breastfeeding at the two time points assessed, 4 to 6 weeks and 6 months. Furthermore, counselling appeared to be most effective at maintaining exclusive breastfeeding. In terms of optimal timing and frequency, this review indicates that counselling delivered at least four times in the postnatal period (with or without an antenatal component) is more effective than counselling delivered in the antenatal period only and/or fewer than four times. Face-to face counselling appears to be more effective than telephone counselling. There were mixed findings in terms of who provides the counselling but the largest effects were for lay or combined lay and non-lay providers on exclusive breastfeeding at 4 to 6 weeks postpartum. We also found that counselling interventions appear to be effective in urban settings and when both primiparous and multiparous women are included.
The overall finding of this review that counselling reduced the risk of women stopping any and exclusive breastfeeding is in agreement with other systematic reviews of similar interventions that aim to increase breastfeeding rates [11, 12]. This review differs from others in that it has focused specifically on counselling interventions that are delivered directly to women, and are interactive and support women with their decision-making, rather than including studies of interventions that only provided education [11] and/or systems level interventions, such as implementation of WHO/UNICEF Baby friendly initiative [14, 15, 82]. As others have suggested [12, 83], it is crucial to identify the elements of these important but heterogeneous interventions that are effective and this review contributes specifically to this.
The effect size found in this review is smaller than that found in others [11, 14] which may be partly due to the focus on one type of intervention, as previous reviews have found multicomponent interventions to be most effective [14, 15, 82]. It is also likely that counselling interventions to encourage and support breastfeeding are affected by the context within which breastfeeding occurs. In particular, the interactive and responsive nature of counselling may mean it is more effective in areas where breastfeeding is seen as the norm and when women are already motivated to breastfeed. One implication of this is that breastfeeding initiation needs to be considered alongside initiatives to improve breastfeeding duration and exclusivity.
Furthermore, this review included relatively few studies from low- and middle-income countries where breastfeeding rates are generally higher (approximately a third of studies and a quarter of participants). In countries where breastfeeding rates are high interventions to promote and support breastfeeding appear to have greater effect, particularly in maintaining exclusive breastfeeding [11, 12, 82]. This may partially explain both the smaller effect size and the greater effect of counselling interventions on exclusive rather than on any breastfeeding found in this review. The existing provision of healthcare in each country or area may also be relevant. In a review including only interventions delivered in low- and middle-income countries, Olufunlayo et al. [82] estimate a much greater effect, a two to three-fold increase in exclusive breastfeeding at 6 months, and as they suggest, there may be more potential for interventions to be effective where standard healthcare provision is lacking.
Counselling emphasises interactions with individual mothers to support their decision-making, which means that the content and style of the intervention inevitably varies for different women at different times. Whilst at the micro level this is variable, at the macro level it is possible to identify criteria that make it effective. The subgroup analyses in this review found that counselling was most effective when delivered face-to-face and was not effective when only delivered antenatally. These findings are perhaps not surprising given the relational nature of counselling. It is highly likely that relations between health workers and mothers can be established more easily face-to-face, and when provided across the childbearing continuum, may develop in a way that enhances women’s confidence and self-efficacy. This needs careful consideration as in many countries the reduced healthcare provision for breastfeeding mothers may mean many only receive breastfeeding counselling before birth, and telephone support may be considered a cheaper and easier option.
More frequent counselling may also enable women and healthcare workers to build rapport and may be important in enabling counsellors to respond in a timely way when women encounter challenges, particularly in the early days after birth. This review found that when counselling was provided four or more times it was more effective for maintaining exclusive breastfeeding (≥ 4 times 31% compared to < 4 times 8%). However, there was huge variation in the frequency of counselling (from 1 to 24 contacts) and a counselling intervention that is only delivered once in the hospital setting is very different to one provided regularly within an established relationship. This is similar to the recent review of support interventions, which found greatest effect on exclusive breastfeeding when the intervention was provided between four and eight times [12]. While an optimal number of counselling sessions could not be definitely pinpointed from the evidence, the World Health Organization guideline recommends counselling is provided at least six times and more if needed [22] based on the available evidence and other considerations. It is also likely that there is interplay between frequency of counselling and its timing to coincide with the period when women encounter most challenges, such as in the early period after birth when they are developing breastfeeding skills and/or at times when they may be considering introducing other foods or returning to work [84] .
Strengths and limitations
This systematic review was conducted robustly, included a large number of studies and was limited to randomised controlled trials to ensure it is based on the strongest evidence available. However, findings should be treated with caution as the evidence was mostly of low quality due to high or unclear risk of bias of the included trials. This is partly attributable to a lack of blinding which would not be feasible with such an intervention. Breastfeeding counselling is often part of complex multicomponent interventions and, as in most systematic reviews of breastfeeding interventions [12–14], there was considerable heterogeneity of the counselling interventions within the review. This included frequency and timing of counselling, who delivered the intervention (e.g., a qualified health professional or a lay person), and if they were specifically trained in breastfeeding counselling. Additionally, reporting of interventions within studies was not always comprehensive, clear or sufficiently detailed, making it difficult to identify the components of the counselling intervention and/or care received by control groups. In particular training of non-lay providers in breastfeeding counselling knowledge and skills was poorly described which meant we could not include this aspect in a meta-analysis. We could not conduct planned sub-group analysis by mode of birth because there were no studies of the effectiveness of breastfeeding counselling following caesarean birth. We also found no studies of breastfeeding counselling that measured breastfeeding outcomes at 24 months.
Conclusions
The findings of this systematic review demonstrate that counselling interventions are effective for improving breastfeeding practices with the greatest effect on exclusive breastfeeding. The review has informed a recent global guideline [22]. Recommendations include that breastfeeding counselling should be provided face-to-face, and, in addition, may be provided by telephone, both antenatally and postnatally to all pregnant women and breastfeeding mothers. However, in order to inform scale-up and sustainability globally, there is a need to further understand the elements of interventions such as counselling and their effectiveness in different contexts and circumstances.
Supplementary information
Additional file 2. Characteristics of included studies and description of intervention and comparison.
Acknowledgements
We would like to thank Nigel Rollins, Pura Rayco-Solon, and Nandi Siegfried for their advice on the conduct of this review.
Abbreviations
- CI
Confidence interval
- ICC
Intra-cluster correlation coefficient
- RR
Relative risk
- WHO
World Health Organization
Authors’ contributions
AMcF led the design of the review, screening, data extraction, critical appraisal, data synthesis, was involved in data analysis and drafted the manuscript. LS was involved in designing the review, screening, data extraction, critical appraisal, data analysis and synthesis. JLM was involved in screening, data extraction, critical appraisal, data synthesis, and drafting the manuscript. AG was involved in designing the review, screening, data extraction, critical appraisal, and data analysis. L-CG was involved in screening, data extraction, critical appraisal and drafting the manuscript. AGS was involved in screening, data extraction, critical appraisal, data analysis and synthesis. SMacG was involved in designing the review, screening, data extraction, critical appraisal and led the data analysis. All authors were involved in revising the manuscript for intellectual content and approved the final version.
Funding
This work was commissioned by the World Health Organization as part of the evidence considered in developing recommendations on counselling to improve breastfeeding practices.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Additional information files.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Alison McFadden, Email: a.m.mcfadden@dundee.ac.uk.
Lindsay Siebelt, Email: l.siebelt@hotmail.com.
Joyce L. Marshall, Email: j.marshall@hud.ac.uk
Anna Gavine, Email: a.gavine@dundee.ac.uk.
Lisa-Christine Girard, Email: Lisa-Christine.Girard@ed.ac.uk.
Andrew Symon, Email: a.g.symon@dundee.ac.uk.
Stephen MacGillivray, Email: s.a.macgillivray@dundee.ac.uk.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13006-019-0235-8.
References
- 1.Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 3.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. Bellagio child survival study group: how many child deaths can we prevent this year? Lancet. 2003;362(9377):65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 4.Horta BL, Loret De Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:30–37. doi: 10.1111/apa.13133. [DOI] [PubMed] [Google Scholar]
- 5.Girard L-C, Farkas C. Breastfeeding and behavioural problems: propensity score matching with a national cohort of infants in Chile. BMJ Open. 2019;9(2):e025058. doi: 10.1136/bmjopen-2018-025058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med. 2009;4(S1):S17–S30. doi: 10.1089/bfm.2009.0050. [DOI] [PubMed] [Google Scholar]
- 7.Hahn-Holbrook J, Haselton MG, Schetter CD, Glynn LM. Does breastfeeding offer protection against maternal depressive symptomatology? Arch Womens Ment Health. 2013;16(5):411–422. doi: 10.1007/s00737-013-0348-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Narod S. Modifiers of risk of hereditary breast cancer. Oncogene. 2006;25(43):5832. doi: 10.1038/sj.onc.1209870. [DOI] [PubMed] [Google Scholar]
- 9.WHO, UNICEF . The extension of the 2025 maternal, infant and young child nutrition targets to 2030. Geneva: World Health Organization; 2018. [Google Scholar]
- 10.Balogun OO, O'Sullivan EJ, McFadden A, Ota E, Gavine A, Garner CD, Renfrew MJ, MacGillivray S. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev. 2016;11:CD001688. doi: 10.1002/14651858.CD001688.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haroon S, Das JK, Salam RA, Imdad A, Bhutta ZA. Breastfeeding promotion interventions and breastfeeding practices: a systematic review. BMC Public Health. 2013;13(Suppl 3):S20. doi: 10.1186/1471-2458-13-S3-S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McFadden A, Gavine A, Renfrew MJ, Wade A, Buchanan P, Taylor JL, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2017;2:CD001141. doi: 10.1002/14651858.CD001141.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shakya P, Kunieda MK, Koyama M, Rai SS, Miyaguchi M, Dhakal S, Sandy S, Sunguya BF, Jimba M. Effectiveness of community-based peer support for mothers to improve their breastfeeding practices: a systematic review and meta-analysis. PLoS One. 2017;12(5):e0177434. doi: 10.1371/journal.pone.0177434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sinha B, Chowdhury R, Sankar MJ, Martines J, Taneja S, Mazumder S, Rollins N, Bahl R, Bhandari N. Interventions to improve breastfeeding outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104(Supplement 467):114–135. doi: 10.1111/apa.13127. [DOI] [PubMed] [Google Scholar]
- 15.Kim SK, Park S, Oh J, Kim J, Ahn S. Interventions promoting exclusive breastfeeding up to six months after birth: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2018;80:94–105. doi: 10.1016/j.ijnurstu.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 16.WHO, UNICEF . Breastfeeding counselling: a training course. Geneva: World Health Organization; 1993. [Google Scholar]
- 17.WHO . Infant and young child feeding: model chapter for textbooks for medical stduents and allied health professionals. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 18.Labarere J, Gelbert-Baudino N, Ayral A-S, Duc C, Berchotteau M, Bouchon N, et al. Efficacy of breastfeeding support provided by trained clinicians during an early, routine, preventive visit: a prospective, randomized, open trial of 226 mother-infant pairs. Pediatrics. 2005;115(2):e139–e146. doi: 10.1542/peds.2004-1362. [DOI] [PubMed] [Google Scholar]
- 19.Santiago LB, Bettiol H, Barbieri MA, Guttierrez MRP, Del Ciampo LA. Promotion of breastfeeding: the importance of pediatricians with specific training. J Pediatr. 2003;79(6):504–512. doi: 10.2223/JPED.1110. [DOI] [PubMed] [Google Scholar]
- 20.Ekstrom A, Widstrom A-M, Nissen E. Does continuity of care by well-trained breastfeeding counselors improve a mother's perception of support? Pediatrics. 2006;118(2):123–130. doi: 10.1542/peds.2005-2064. [DOI] [PubMed] [Google Scholar]
- 21.Hoddinott P, Britten J, Prescott GJ, Tappin D, Ludbrook A, Godden DJ. Effectiveness of policy to provide breastfeeding groups (BIG) for pregnant and breastfeeding mothers in primary care: cluster randomised controlled trial. BMJ. 2009;338:a3026. doi: 10.1136/bmj.a3026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO . Guideline: counselling of women to improve breastfeeding practices. Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 23.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011] Oxford: The Cochrane Collaboration; 2011. [Google Scholar]
- 24.Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013: The GRADE Working Group; 2013. https://gdt.gradepro.org/app/handbook/handbook.html.
- 25.RevMan . Review Manager (RevMan) 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. [Google Scholar]
- 26.Ahmed AH. Breastfeeding preterm infants: an educational program to support mothers of preterm infants in Cairo, Egypt. Pediatr Nurs. 2008;34(2):125–130. [PubMed] [Google Scholar]
- 27.Albernaz E, Victora CG, Haisma H, Wright A, Coward WA. Lactation counseling increases breast-feeding duration but not breast milk intake as measured by isotopic methods. J Nutr. 2003;133:205–210. doi: 10.1093/jn/133.1.205. [DOI] [PubMed] [Google Scholar]
- 28.Caulfield LE, Gross SM, Bentley ME, Bronner Y, Kessler L, Jensen J, Weathers B, Paige DM. WIC-based interventions to promote breastfeeding among African-American women in Baltimore: effects on breastfeeding initiation and continuation. J Hum Lact. 1998;14:15–22. doi: 10.1177/089033449801400110. [DOI] [PubMed] [Google Scholar]
- 29.Frank DA, Wirtz SJ, Sorensen JR, Heeren T. Commercial discharge packs and breast-feeding counseling: effects on infant-feeding practices in a randomized trial. Pediatrics. 1987;80(6):845–854. [PubMed] [Google Scholar]
- 30.Gagnon AJ, Dougherty G, Jimenez V, Leduc N. Randomized trial of postpartum care after hospital discharge. Pediatrics. 2002;109(6):1074–1080. doi: 10.1542/peds.109.6.1074. [DOI] [PubMed] [Google Scholar]
- 31.Gross SM, Caulfield LE, Bentley ME, Bronner Y, Kessler L, Jensen J, Paige DM. Counselling and motivational videotapes increase duration of breast- feeding in Africa-American WIC participants who initiate breast-feeding. J Am Diet Assoc. 1998;98(2):143–148. doi: 10.1016/S0002-8223(98)00037-6. [DOI] [PubMed] [Google Scholar]
- 32.Jolly K, Ingram L, Freemantle N, Khan K, Chambers J, Hamburger R, Brown J, Dennis C-L, Macarthur C. Effect of a peer support service on breast-feeding continuation in the UK: a randomised controlled trial. Midwifery. 2012;28:740–745. doi: 10.1016/j.midw.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 33.Kools EJ, Thijs C, Kester AD, Brandt PA, Vries H. A breast-feeding promotion and support program a randomized trial in the Netherlands. Prev Med. 2005;40(1):60–70. doi: 10.1016/j.ypmed.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 34.Leite AJM, Puccini RF, Atalah AN, Alves Da Cunha AL, Machado MT. Effectiveness of home-based peer counselling to promote breastfeeding in the northeast of Brazil: a randomized clinical trial. Acta Paediatr. 2005;94:741–746. doi: 10.1111/j.1651-2227.2005.tb01974.x. [DOI] [PubMed] [Google Scholar]
- 35.McKeever P, Stevens B, Miller KL, MacDonell JW, Gibbins S, Guerriere D, Dunn MS, Coyte PC. Home versus hospital breastfeeding support newborns: a randomized controlled trial. Birth. 2002;29(4):258–265. doi: 10.1046/j.1523-536X.2002.00200.x. [DOI] [PubMed] [Google Scholar]
- 36.Merewood A, Chamberlain LB, Cook JT, Philipp BL, Malone K, Bauchner H. The effect of peer counselors on breastfeeding rates in the neonatal intensive care unit: results of a randomized controlled trial. Arch Pediatr Adolesc Med. 2006;160:681–685. doi: 10.1001/archpedi.160.7.681. [DOI] [PubMed] [Google Scholar]
- 37.Reeder JA, Joyce T, Sibley K, Arnold D, Altindag O. Telephone peer counseling of breastfeeding among WIC participants: a randomized controlled trial. Pediatrics. 2014;134:e700–e709. doi: 10.1542/peds.2013-4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ryser FG. Breastfeeding attitudes, intention, and initiation in low-income women: the effect of the best start program. J Hum Lact. 2004;20(3):300–305. doi: 10.1177/0890334404266985. [DOI] [PubMed] [Google Scholar]
- 39.Schy DS, Maglaya CF, Mendelson SG, Race KE, Ludwig-Beymer P. The effects of in-hospital lactation education on breastfeeding practice. J Hum Lact. 1996;12:117–122. doi: 10.1177/089033449601200215. [DOI] [PubMed] [Google Scholar]
- 40.Sellen D, Mbugua S, Webb Girard A, Kalungu S, Sarange C, Lou W, et al. A randomized controlled trial indicates benefits of cell phone based peer counseling to support exclusive breastfeeding in Kenya. Ann Nutr Metab. 2013;63:751. [Google Scholar]
- 41.Srinivas GL, Benson M, Worley S, Schulte E. A clinic-based breastfeeding peer counselor intervention in an urban, low-income population: interaction with breastfeeding attitude. J Hum Lact. 2015;31:120–128. doi: 10.1177/0890334414548860. [DOI] [PubMed] [Google Scholar]
- 42.Stockdale J, Sinclair M, Kernohan WG, Keller JM, Dunwoody L, Cunningham JB, Lawther L, Weir P. Feasibility study to test DESIGNER BREASTFEEDING: a randomised controlled trial. Evid Based Midwifery. 2008;6(3):76–82. [Google Scholar]
- 43.Thakur SK, Roy SK, Paul K, Khanam M, Khatun W, Sarker D. Effect of nutrition education on exclusive breastfeeding for nutritional outcome of low birth weight babies. Eur J Clin Nutr. 2012;66:376–381. doi: 10.1038/ejcn.2011.182. [DOI] [PubMed] [Google Scholar]
- 44.Wambach KA, Aaronson L, Breedlove G, Domian EW, Rojjanasrirat W, Yeh H-W. A randomized controlled trial of breastfeeding support and education for adolescent mothers. West J Nurs Res. 2011;33:486–505. doi: 10.1177/0193945910380408. [DOI] [PubMed] [Google Scholar]
- 45.Bonuck K, Stuebe A, Barnett J, Fletcher J, Bernstein P. Routine, primary-care based interventions to increase breastfeeding: results of two randomized clinical trials. Breastfeed Med. 2013;8:S19. [Google Scholar]
- 46.Tylleskar T, Jackson D, Meda N, Engebretsen IMS, Chopra M, Diallo AH, et al. Exclusive breastfeeding promotion by peer counsellors in sub-Saharan Africa (PROMISE-EBF): a cluster-randomised trial. Lancet. 2011;378:420–427. doi: 10.1016/S0140-6736(11)60738-1. [DOI] [PubMed] [Google Scholar]
- 47.Aidam BA, Perez-Escamilla R, Lartey A. Lactation counseling increases exclusive breast-feeding rates in Ghana. J Nutr. 2005;135:1691–1695. doi: 10.1093/jn/135.7.1691. [DOI] [PubMed] [Google Scholar]
- 48.Fu ICY, Fong DYT, Heys M, Lee ILY, Sham A, Tarrant M. Professional breastfeeding support for first-time mothers: a multicentre cluster randomised controlled trial. Br J Obstet Gynaecol. 2014;121:1673–1683. doi: 10.1111/1471-0528.12884. [DOI] [PubMed] [Google Scholar]
- 49.McLachlan HL, Forster DA, Amir LH, Cullinane M, Shafiei T, Watson LF, Ridgway L, Cramer RL, Small R. Supporting breastfeeding in local communities (SILC) in Victoria, Australia: a cluster randomised controlled trial. BMJ Open. 2016;6:e008292. doi: 10.1136/bmjopen-2015-008292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morrow AL, Guerrero ML, Shults J, Calva JJ, Lutter C, Bravo J, Ruiz-Palacios G, Morrow RC, Butterfoss FD. Efficacy of home-based peer counselling to promote exclusive breastfeeding: a randomised controlled trial. Lancet. 1999;353:1226–1223. doi: 10.1016/S0140-6736(98)08037-4. [DOI] [PubMed] [Google Scholar]
- 51.Ochola SA, Labadarios D, Nduati RW. Impact of counselling on exclusive breast-feeding practices in a poor urban setting in Kenya: a randomized controlled trial. Public Health Nutr. 2013;16:1732–1740. doi: 10.1017/S1368980012004405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Su LL, Chong YS, Chan YH, Chan YS, Fok D, Tun KT, Ng FSP, Rauff M. Antenatal education and postnatal support strategies for improving rates of exclusive breast feeding: randomised controlled trial. BMJ. 2007;335(7620):596–599. doi: 10.1136/bmj.39279.656343.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Edwards RC, Thullen MJ, Korfmacher J, Lantos JD, Henson LG, Hans SL. Breastfeeding and complementary food: randomized trial of community doula home visiting. Pediatrics. 2013;132(Suppl 2):S160–S166. doi: 10.1542/peds.2013-1021P. [DOI] [PubMed] [Google Scholar]
- 54.Khresheh R, Suhaimat A, Jalamdeh F, Barclay L. The effect of a postnatal education and support program on breastfeeding among primiparous women: a randomized controlled trial. Int J Nurs Stud. 2011;48(9):1058–1065. doi: 10.1016/j.ijnurstu.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 55.Tahir NM, Al-Sadat N. Does telephone lactation counselling improve breastfeeding practices? A randomised controlled trial. Int J Nurs Stud. 2013;50:16–25. doi: 10.1016/j.ijnurstu.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 56.Agrasada GV, Gustafsson J, Kylberg E, Ewald U. Postnatal peer counselling on exclusive breastfeeding of low-birthweight infants: a randomized, controlled trial. Acta Paediatr. 2005;94:1109–1115. doi: 10.1111/j.1651-2227.2005.tb02053.x. [DOI] [PubMed] [Google Scholar]
- 57.Aksu H, Kucuk M, Duzgun G. The effect of postnatal breastfeeding education/support offered at home 3 days after delivery on breastfeeding duration and knowledge: a randomized trial. J Matern Fetal Neonatal Med. 2011;24:354–361. doi: 10.3109/14767058.2010.497569. [DOI] [PubMed] [Google Scholar]
- 58.Ahmadi S, Kazemi F, Masoumi SZ, Parsa P, Roshanaei G. Intervention based on BASNEF model increases exclusive breastfeeding in preterm infants in Iran: a randomized controlled trial. Int Breastfeed J. 2016;11:30. doi: 10.1186/s13006-016-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mikami FCF, de Lourdes BM, Tase TH, Saccuman E, Vieira Francisco RP, Zugaib M. Effect of prenatal counseling on breastfeeding rates in mothers of twins. J Obstet Gynecol Neonatal Nurs. 2017;46:229–237. doi: 10.1016/j.jogn.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 60.Pound CM, Moreau K, Rohde K, Barrowman N, Aglipay M, Farion KJ, Plint AC. Lactation support and breastfeeding duration in jaundiced infants: a randomized controlled trial. PLoS One. 2015;10(3):e0119624. doi: 10.1371/journal.pone.0119624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coutinho SB, Lira PI, Carvalho Lima M, Ashworth A. Comparison of the effect of two systems for the promotion of exclusive breastfeeding. Lancet. 2005;366(9491):1094–1100. doi: 10.1016/S0140-6736(05)67421-1. [DOI] [PubMed] [Google Scholar]
- 62.Grossman LK, Harter C, Sachs L, Kay A. The effect of postpartum lactation counseling on the duration of breast-feeding in low-income women. Am J Dis Child. 1990;144:471–474. doi: 10.1001/archpedi.1990.02150280093019. [DOI] [PubMed] [Google Scholar]
- 63.Anderson AK, Damio G, Young S, Chapman DJ, Perez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. JAMA Pediatr. 2005;159:836–841. doi: 10.1001/archpedi.159.9.836. [DOI] [PubMed] [Google Scholar]
- 64.Bonuck K, Freeman K, Trombley M. Randomized controlled trial of a prenatal and postnatal lactation consultant intervention on infant health care use. Arch Pediatr Adolesc Med. 2006;160:953–960. doi: 10.1001/archpedi.160.9.953. [DOI] [PubMed] [Google Scholar]
- 65.Davies-Adetugbo AA, Adetugbo K, Orewole Y, Fabiyi AK. Breast-feeding promotion in a diarrhoea programme in rural communities. J Diarrhoeal Dis Res. 1997;15:161–166. [PubMed] [Google Scholar]
- 66.de Oliveira LD, Giugliani ERJ, do Espirito Santo LC, Franca MCT, Weigert EML, Kohler CVF, de Lourenzi Bonilha AL. Effect of intervention to improve breastfeeding technique on the frequency of exclusive breastfeeding and lactation-related problems. J Hum Lact. 2006;22:315–321. doi: 10.1177/0890334406290221. [DOI] [PubMed] [Google Scholar]
- 67.Di Napoli A, Di Lallo D, Fortes C, Franceschelli C, Armeni E, Guasticchi G. Home breastfeeding support by health professionals: findings of a randomized controlled trial in a population of Italian women. Acta Paediatr. 2004;93:1108–1114. doi: 10.1111/j.1651-2227.2004.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 68.Lynch SA, Koch AM, Hislop TG, Coldman AJ. Evaluating the effect of a breastfeeding consultant on the duration of breastfeeding. Can J Public Health. 1986;77:190–195. [PubMed] [Google Scholar]
- 69.Haider R, Ashworth A, Kabir I, Huttly SR. Effect of community-based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: a randomised controlled trial. Lancet. 2000;356:1643–1647. doi: 10.1016/S0140-6736(00)03159-7. [DOI] [PubMed] [Google Scholar]
- 70.Zhu Y, Zhang Z, Ling Y, Wan H. Impact of intervention on breastfeeding outcomes and determinants based on theory of planned behavior. Women Birth. 2017;30:146–152. doi: 10.1016/j.wombi.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 71.Nilsson IMS, Strandberg-Larsen K, Knight CH, Hansen AV, Kronborg H. Focused breastfeeding counselling improves short- and long-term success in an early-discharge setting: a cluster-randomized study. Matern Child Nutr. 2017;13:e12432. doi: 10.1111/mcn.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rossiter JC. The effect of a culture-specific education program to promote breastfeeding among Vietnamese women in Sydney. Int J Nurs Stud. 1994;31:369–379. doi: 10.1016/0020-7489(94)90077-9. [DOI] [PubMed] [Google Scholar]
- 73.Vidas M, Folnegovic-Smalc V, Catipovic M, Kisic M. The application of autogenic training in counseling center for mother and child in order to promote breastfeeding. Coll Antropol. 2011;35:723–731. [PubMed] [Google Scholar]
- 74.Carlsen EM, Kyhnaeb A, Renault KM, Cortes D, Michaelsen KF, Pryds O. Telephone-based support prolongs breastfeeding duration in obese women: a randomized trial. Am J Clin Nutr. 2013;98:1226–1232. doi: 10.3945/ajcn.113.059600. [DOI] [PubMed] [Google Scholar]
- 75.Simonetti V, Palma E, Giglio A, Mohn A, Cicolini G. A structured telephonic counselling to promote the exclusive breastfeeding of healthy babies aged zero to six months: a pilot study. Int J Nurs Pract. 2012;18:289–294. doi: 10.1111/j.1440-172X.2012.02040.x. [DOI] [PubMed] [Google Scholar]
- 76.Chapman D, Damio G, Young S, Perez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med. 2004;158:897–902. doi: 10.1001/archpedi.158.9.897. [DOI] [PubMed] [Google Scholar]
- 77.Chapman DJ, Morel K, Bermúdez-Millán A, Young S, Damio G, Pérez-Escamilla R. Breastfeeding education and support trial for overweight and obese women: a randomized trial. Pediatrics. 2013;131(1):e162–e170. doi: 10.1542/peds.2012-0688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McDonald SJ, Henderson JJ, Faulkner S, Evans SF, Hagan R. Effect of an extended midwifery postnatal support programme on the duration of breast feeding: a randomised controlled trial. Midwifery. 2010;26:88–100. doi: 10.1016/j.midw.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 79.Cangol E, Sahin NH. The effect of a breastfeeding motivation program maintained during pregnancy on supporting breastfeeding: a randomized controlled trial. Breastfeed Med. 2017;12(4):218–226. doi: 10.1089/bfm.2016.0190. [DOI] [PubMed] [Google Scholar]
- 80.Ciftci EK, Arikan D. The effect of training administered to working mothers on maternal anxiety levels and breastfeeding habits. J Clin Nurs. 2012;21:2170–2178. doi: 10.1111/j.1365-2702.2011.03957.x. [DOI] [PubMed] [Google Scholar]
- 81.Rojjanasrirat W. The effects of a nursing intervention on breastfeeding duration among primiparous mothers planning to return to work. Doctoral Dissertation. Kansas: University of Kansas; 2000. [Google Scholar]
- 82.Olufunlayo TF, Roberts AA, MacArthur C, Thomas N, Odeyemi KA, Price M, Jolly K. Improving exclusive breastfeeding in low and middle-income countries: A systematic review. Matern Child Nutr. 2019;15(3):e12788. doi: 10.1111/mcn.12788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hoddinott P, Seyara R, Marais D. Global evidence synthesis and UK idiosyncrasy: why have recent UK trials had no significant effects on breastfeeding rates? Matern Child Nutr. 2011;7(3):221–227. doi: 10.1111/j.1740-8709.2011.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fein SB, Mandal B, Roe BE. Success of strategies for combining employment and breastfeeding. Pediatrics. 2008;122(Supplement 2):S56–S62. doi: 10.1542/peds.2008-1315g. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Characteristics of included studies and description of intervention and comparison.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its Additional information files.