Abstract
Background
Traumatic dental injuries (TDIs) are highly prevalent during childhood and adolescence and have a significant effect on their oral health related quality of life (OHRQoL). Uncomplicated TDIs, dental trauma involving enamel, enamel and dentin and tooth discolorations, account for approximately two-thirds of all diagnosed TDIs in children and adolescents. Hence, it may be important to understand the impact of uncomplicated TDIs on OHRQoL, by synthesizing the available literature.
Methods
Medline, Embase, Web of Science and Scopus databases were systematically searched from January 1966 to April 2018. Studies that evaluated the effect of TDIs on the OHRQoL of children and adolescents using validated methods were selected for analysis. A narrative synthesis and a meta-analysis were performed. The studies were pooled according to age groups and OHRQoL questionnaire used. A random-effect model was applied to calculate the pooled odds ratios (OR) and their respective 95% confidence intervals.
Results
There were 712 identified studies. Of these, 26 articles were selected for the review and included in the narrative synthesis, 20 of these articles concluded that uncomplicated TDIs were not associated with a negative impact in OHRQoL. Seventeen were included in the meta-analysis. The estimates were pooled by age groups: children (OR: 1.01; 95%CI; 0.85–1.19; I2 = 51.9%) and adolescents (OR: 1.07; 95%CI; 0.91, 1.26; I2 = 50.2%).When pooling all estimates the OR was 0.96 (95% CI: 0.85–1.10; I2 = 61.4%).
Conclusions
Uncomplicated TDIs do not have a negative impact on the OHRQoL of children and adolescents. Further prospective studies are needed to confirm the results of this review. The majority of the studies included were of cross-sectional design, which may have limited the ability to reach conclusions on the nature of this association. The PROSPERO systematic review registry is CRD42018110471.
Keywords: Uncomplicated, Traumatic dental injuries, Quality of life, OHRQoL, Children, Adolescents
Background
Traumatic dental injuries (TDIs) are one of the most prevalent oral pathologies in children and adolescents [1]. Approximately 22.7% of children aged 0 to 6 years have a TDI involving the primary dentition in their early childhood [1] and nearly 25% of all schoolchildren and adolescents aged 7 to 19 years have a TDI involving their permanent dentition [2, 3]. Uncomplicated TDIs (enamel fractures, enamel and dentin fractures and tooth discolorations) are the least severe, but most frequent type of TDI in children and adolescents, as they account for approximately two thirds of all diagnosed TDIs [2].
Previous studies showed that subsequent to the dental tissue trauma (e.g., enamel or dentinal fracture), bacterial invasion in the fracture could determine further infection and exposed dentinal tubules can cause pulp inflammation that leads to either repair or necrosis of the pulp [3]. Discoloration of the tooth after trauma can negatively affect the Oral Health related Quality of Life (OHRQoL) of children and adolescents [4, 5]. Also, the monetary costs of immediate and follow-up care to dental trauma patients, their families and oral health services are substantial [6]. In this way, uncomplicated TDIs, can have medium and long-term consequences, which should be identified, monitored and their treatment needs assessed [7]. Thus, clarification of the effects and consequences of uncomplicated TDIs on the quality of life of adolescents and children would be beneficial for the public health care system.
In recent times, researchers are increasingly using OHRQoL measures to evaluate the effect that oral conditions such as TDIs have on quality of life. OHRQoL is a measure of the impact of oral conditions on daily functioning; for example the impact oral conditions have on a patient’s wellbeing when talking, smiling, laughing, sleeping, and eating; their satisfaction and; their self-esteem [8]. A series of validated questionnaires which are self-reported or answered by proxy are used to measure OHRQoL [9]. Some examples of these questionnaires for children include the Early Childhood Oral Health Impact Scale (ECOHIS) [10] which uses parents or guardians as proxy and the Scale of Oral Health Outcomes for 5-year-olds (SOHO-5) [11] which is self-reported. And for adolescents, the child perceptions questionnaire (CPQ) for ages 11–14, [12], with a version for younger children aged 8–10 which are self-reported [13].
Two previous systematic reviews quantified the effect of TDIs, without considering the type of TDIs, on the OHRQoL of preschool children and schoolchildren [14, 15]. Both systematic reviews concluded that TDIs have a negative impact on the OHRQoL of preschool children and schoolchildren. However, neither of these reviews explored the implications of only uncomplicated TDIs on the OHRQoL of children and adolescent. Given the frequency of this type of traumatic dental injury, it is worthwhile to determine its consequences on quality of life. Therefore, the research question is as it follows: Do uncomplicated TDIs affect the OHRQoL of children and adolescents? And the aim is to evaluate the impact of uncomplicated TDIs on the OHRQoL of children and adolescents, by synthesizing the available literature.
Methods
This review was prospectively registered in PROSPERO (CRD42018110471) and follows the Guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [16].
Search strategy and eligibility criteria
A systematic search of literature was done on Medline, Embase, Web of Science and Scopus, from January 1966 to April 2018. Using MeSH terms and keywords related to dental traumatic injuries and quality of life the databases were systematically searched. The search terms used in Medline and EMBASE ovid were: (Dental or tooth or teeth) AND adj5 (Trauma* or injur*) AND Child* or infant* or adolescen* or toddler* or young* or minor* AND quality of life. Additional articles were identified from the reference section of the selected studies from the original search. Further details of the search terms are provided in Additional file 1.
The inclusion criteria were as follows: Studies with epidemiological design (case-control, cross-sectional, and cohort) in English, Spanish and Portuguese; traumatic dental injuries as the exposure variable and was measured with an established criteria for diagnosis; quality of life as the outcome and measured using a validated questionnaire [12, 13, 17].; presented the type of traumatic dental injuries group stratification; study samples that includes children and/or adolescents up to 19 years of age [18]. The exclusion criteria were as follows: case reports, studies and articles without the predefined outcome and exposure; studies that focus on particular groups (athletes, patients with cerebral palsy, and victims of violence).
Study selection and data extraction
Endnote™ X8.2 reference management software for Windows (9 January 2018 release) was used to manage relevant citations. A database was created to facilitate management and checked for duplicate articles. Two researchers (DL and CZ) independently reviewed the titles and abstracts. Discrepancies were resolved by consulting a third reviewer (RM). Citations were sorted based on the relevance of the articles to the research question and selection criteria into: “not relevant”, “relevant”, “highly relevant” and “final selection”. Full text of the “highly relevant” group were reviewed. Studies which met the requirements for the qualitative and/or quantitative synthesis were placed into the “final selection” group. Neither authors nor journals were blinded to reviewers.
Data extraction of the studies were conducted by agreement of two reviewers (DL and CZ) using a predefined, standardized data collection form. Using four potentially eligible articles a pilot test was performed to homogenize criteria among reviewers. The Kappa statistic was used (K = 0.79), which demonstrated substantial agreement between the reviewers. The data extracted from the selected studies were: Author and year, Title, country, type of population and sample size, exposure, age when was measured and its definition, outcome, age when was measured and its definition, Stratification, confounders/selection bias, reverse causation, results and findings by the authors. The effect estimate is the dichotomous association between uncomplicated TDI and OHRQoL of children and adolescents, and this was extracted from each paper. Uncomplicated TDIs were classified as those in which dislocation of the tooth and/or pulp tissue was not involved; that is, enamel fractures, enamel and dentin fractures, and tooth discolorations. Complicated TDIs were classified as those in which dislocation of the tooth and/or pulp was involved. We contacted study authors by e-mail to obtain additional information when data were missing or unclear.
Quality assessment
Two authors were independently involved in the quality assessment of the studies methodological quality (DL and CZ). Using the Newcastle-Ottawa scale (NOS) adapted for observational studies, [19] a star system was developed to assess study quality. Each study is judged on three broad perspectives: the ascertainment of either the exposure or outcome: the comparability of the groups; and the selection of the study groups [19]. There are no universally accepted standardized grading methods for NOS, the quality of the studies were graded as follows: very good (8–9), good (6–7), satisfactory (5–4) and unsatisfactory (0–3). The scale is provided in Additional file 2.
Data analysis
Following Green et al. recommendations [20], the narrative overview model which is broad narrative syntheses of formerly published studies, was used. The full text of the selected studies was examined and information on these was extracted into tables. The studies were divided by study design groups and study characteristics within each group were reported to articulate broader similarities and differences among and between the groups.
The main outcome was the impact on OHRQoL measured through validated OHRQoL instruments. Studies that provided the effect estimates Odds ratio (OR) or the data necessary for calculating the effect estimate were included in the meta-analysis. The later was used to generate single 2 by 2 tables and the odds ratios and their respective 95% confidence intervals were calculated for each study. Subsequently, random effects meta-analysis was performed and studies were grouped according to age groups and OHRQoL questionnaire used. The I2 was used to evaluate the heterogeneity of the pooled Odds ratio (25, 50, and 75% were considered to be low, moderate and high heterogeneity respectively) [21]. The decision of pooling the studies by age groups and OHRQoL questionnaire used was done a priori because it is expected to be a source of heterogeneity. Data were not pooled if I2 was over 75%.
In addition, Funnel plots and correspondent Egger’s test were done to explore possible publication bias. All analysis were performed using Stata Statistical Software: Release 13 (Stata Corp, College Station, TX, USA).
Results
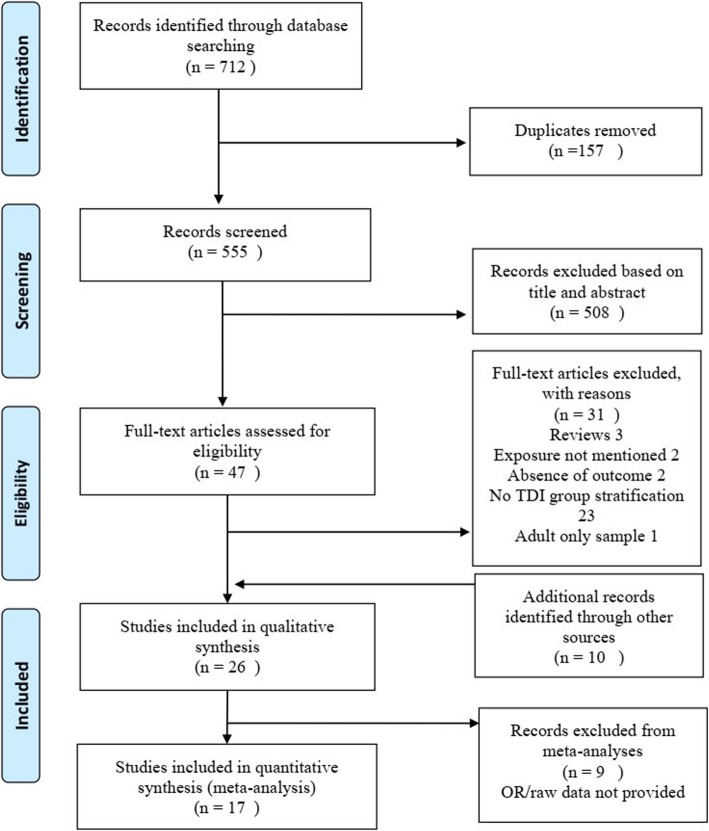
The PRISMA diagram (Fig. 1) shows the selection of studies in this review. Thorough electronic searches identified 712 studies. After excluding 157 duplicates and after reviewing titles and abstracts, 47 publications were evaluated in full text. Of those, 31 studies were excluded and ten additional studies were identified from the reference section of the studies selected for full text review, giving a total of 26 studies, 25 studies in English and one study in Portuguese. The characteristics of these studies are presented in Table 1. The list of excluded studies after the full-text review is provided in Additional file 3.
Fig. 1.
PRISMA flowchart of the selection of eligible literature
Table 1.
Characteristics of included studies
| Study | Study design | Country | Analysed sample/total sample | Setting | Diagnostic criteria | OHRQoL questionnaire (age) | Effect estimates measure |
|---|---|---|---|---|---|---|---|
| Soares, Barasuol et al. 2018 [22] | Cross-sectional | Brazil | 1589/1671 | Population-based | Andreasen classification | CPQ8–10 (8–10 years) | Prevalence ratio |
| Silva-Oliveira, Goursand et al. 2018 [23] | Cross-sectional | Brazil | 588/633 | Population-based | Andreasen classification | CPQ11–14 (12 years) | Odds ratio |
| Martins, Sardenberg et al. 2018 [24] | Cross-sectional | Brazil | 1204/1439 | Population-based | Andreasen classification | CPQ8–10 (8–10 years) | Odds ratio |
| Ramos-Jorge, Sa-Pinto et al. 2017 [4] | Cross-sectional | Brazil | 391/459 | preschool-based | Andreasen classification | ECOHIS (3–5 years) | Prevalence ratio |
| Neves, Perazzo et al. 2017 [25] | Cross-sectional | Brazil | 769/769 | school-based | Andreasen classification | SOHO-5 (5 years) | Prevalence ratio |
| Gonçalves, Dias et al. 2017 [26] | Cross-sectional | Brazil | 192/192 | school-based | Andreasen classification | ECOHIS (3–5 years) | Risk ratio |
| Gomes, Perazzo et al. 2017 [27] | Cross-sectional | Brazil | 769/769 | school-based | Andreasen classification | SOHO-5 (5 years) | Prevalence ratio |
| Bomfim, Herrera et al. 2017 [28] | Cross-sectional | Brazil | 7328/7328 | Population-based | Andreasen classification | OIDP (12 years) | Odds ratio |
| Pulache, Abanto et al. 2016 [29] | Cross-sectional | Peru | 473/513 | school-based | Andreasen classification | CPQ11–14 (11–14 years) | Risk ratio |
| Firmino, Gomes et al. 2016 [30] | Case-control | Brazil | 830/845 | Population-based | Andreasen classification | ECOHIS (3–5 years) | Odds ratio |
| Feldens, Day et al. 2016 [31] | Cross-sectional | Brazil | 1683 /1683 | Population-based | Andreasen classification | ECOHIS (3–5 years) | Prevalence ratio |
| Vieira-Andrade, Siqueira et al. 2015 [32] | Case-control | Brazil | 335/335 | Population-based | Andreasen classification | ECOHIS (3–5 years) | Odds ratio |
| Freire-Maia, Auad et al. 2015 [33] | Cross-sectional | Brazil | 1201/1201 | school-based | Andreasen classification | CPQ8–10 (8–10 years) | Odds ratio |
| Abanto, Tello et al. 2015 [34] | Cross-sectional | Brazil | 1215/1215 | Population-based | Glendor classification | ECOHIS (1–4 years) | Prevalence ratio |
| Viegas, Paiva et al. 2014 [5] | Cross-sectional | Brazil | 1632/1632 | School-based | Andreasen classification | ECOHIS (5–6 years) | Odds ratio |
| Gomes, Pinto-Sarmento et al. 2014 [35] | Cross-sectional | Brazil | 834/864 | preschool-based | Andreasen classification | ECOHIS (3–5 years) | Odds ratio |
| Bendo, Paiva et al. 2014 [36] | Case-control | Brazil | 1215/1215 | Population-based | Andreasen classification | CPQ11–14 (11–14 years) | Odds ratio |
| Abanto, Tsakos et al. 2014 [37] | Cross-sectional | Brazil | 335/394 | Dental school-based | Glendor classification | SOHO-5 (5–6 years) | Risk ratio |
| Siqueira, Firmino et al. 2013 [38] | Cross-sectional | Brazil | 814/864 | Population-based | Andreasen classification | ECOHIS (3–5 years) | Odds ratio |
| Dame-Teixeira, Alves et al. 2013 [39] | Cross-sectional | Brazil | 1528/1837 | School-based | O’Brien classification | CPQ11–14 (14 years) | Risk ratio |
| Viegas, Scarpelli et al. 2012 [40] | Cross-sectional | Brazil | 388 /413 | preschool-based | Andreasen classification | ECOHIS (5 years) | Risk ratio |
| Traebert, de Lacerda et al. 2012 [41] | Cross-sectional | Brazil | 403/409 | Population-based | WHO criteria | CPQ11–14 (11–14 years) | Prevalence ratio |
| Piovesan, Abella et al. 2011 [42] | Cross-sectional | Brazil | 713/ 792 | School-based | O’Brien classification | CPQ11–14 (12 years) | Risk ratio |
| Aldrigui, Abanto et al. 2011 [43] | Cross-sectional | Brazil | 260/305 | preschool-based | Andreasen classification | ECOHIS (2–5 years) | Risk ratio |
| Bendo, Paiva et al. 2010 [44] | Cross-sectional | Brazil | 1612 /1870 | School-based | Andreasen classification | CPQ11–14 (11–14 years) | Prevalence ratio |
| Piovesan, Antunes et al. 2010 [45] | Cross-sectional | Brazil | 713/ 792 | School-based | O’Brien classification | CPQ11–14 (11–14 years) | Risk Ratio |
OHRQoL Oral health related quality of life, CPQ8–10 Child Perceptions Questionnaire version for 8 to 10 years old, CPQ11–14 Child Perceptions Questionnaire version for 11 to 14 years old, ECOHIS Early Childhood Oral Health Impact Scale, SOHO-5 Scale of Oral Health Outcomes for Five-Year-Old Children
Narrative synthesis
The 26 papers included in the review were grouped by study design: 3 were case control studies [30, 32, 36] and there were 23 cross-sectional studies [4, 5, 22–29, 31, 33–35, 37–45]. The study findings were reported in condensed tables that summarized the information extracted from each paper. This table is provided in Additional file 4.
The Andreasen Classification [3] was used in 19 studies. Others used either Glendor’s [46] or O’Brien’s classifications [47]. The age of participants also differed between studies; children (1 to 6 years), adolescents (8 to 14 years). All studies used trained and calibrated dentists to diagnose the TDIs. TDIs were presented by type of injury and some studies presented TDIs as either complicated or uncomplicated.
The use of OHRQOL instruments was according to age of participants. For adolescent samples, 3 studies used the Child Perceptions Questionnaire (CPQ) version for 8 to 10 years (CPQ 8–10) [22, 24, 33], 8 studies used the CPQ version 11 to 14 years (CPQ 11–14) [23, 29, 36, 39, 41, 42, 44, 45] and 1 study used the Oral Impact on Daily Performance (OIDP) [28]. From the studies that used samples of children, 11 studies used the Early Childhood Oral Health Impact Scale (ECOHIS) [4, 5, 26, 30–32, 34, 35, 38, 40, 43] and 3 studies used the Scale of Oral Health Outcomes for Five-Year-Old Children (SOHO-5) [25, 27, 37].
The majority of the cross-sectional studies (n = 15) determined that uncomplicated TDIs were not associated with a negative impact on OHRQoL [5, 24–27, 29, 34, 35, 37, 38, 40, 42–45]. However, 4 studies found an association between uncomplicated TDIs and negative impact on quality of life [23, 33, 39, 41]. Nevertheless, these studies presented estimates with wide confidence intervals and high p-values, which reduced their statistical significance. The remaining 4 cross-sectional studies explored the effect of either only enamel fractures and/or enamel and dentin fractures in OHRQoL [4, 22, 28, 31]. Remarkably, these papers concluded that only enamel fractures did not have a negative effect on the OHRQoL. Yet, enamel and dentin fractures were associated with a negative impact on the oral health related quality of life of children and adolescents.
Study quality
All of the studies included in the review were observational studies. Table 2 shows that all three case-control studies were considered ‘Very good’ quality (i.e. score of 8 or more). Similarly, most of the cross-sectional studies achieved 8 or more out of 9. However, 4 achieved 6 or 7 and two studies scored 5, which is considered ‘Good’ and ‘Satisfactory’, respectively. Common areas of strength were the ascertainment of the exposure and the assessment of the outcome because the sample was randomly selected from schools in most studies. Also, all of the studies used established diagnosis for TDIs and validated instruments to assess OHRQoL. These were measured by trained and calibrated examiners. Hence, the studies included presented low risk of bias.
Table 2.
Study quality assessment
| Study | Selection criteria | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Case definition | Representativeness of the cases | Selection of controls | Definition of controls | Ascertainment of exposure | Same method of ascertainment for cases and controls | Non-respondent rate | Total score | ||
| Case-control Studies | |||||||||
| Firmino et al. 2016 [30] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8/9 |
| Vieira-Andrade et al. 2015 [32] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Bendo et al. 2014 [36] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Cross-sectional studies | |||||||||
| Soares et al. 2018 [22] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Silva-Oliveira et al. 2018 [23] | ★ | ★ | ★★ | ★ | ★ | ★ | 7/9 | ||
| Martins et al. 2018 [24] | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 | |
| Ramos-Jorge et al. 2017 [4] | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8/9 | |
| Neves et al. 2017 [25] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Gonçalves et al. 2017 [26] | ★ | ★ | ★ | ★ | ★ | 5/9 | |||
| Gomes et al. 2017 [27] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7/9 | |
| Bomfim et al. 2017 [28] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8/9 |
| Pulache et al. 2016 [29] | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8/9 | |
| Feldens et al. 2016 [31] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Freire-Maia et al. 2015 [33] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Abanto et al. 2015 [34] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Viegas et al. 2014 [5] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Gomes et al. 2014 [35] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Abanto et al. 2014 [37] | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8/9 | |
| Siqueira et al. 2013 [38] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Dame-Teixeira et al. 2013 [39] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7/9 | |
| Viegas et al. 2012 [40] | ★ | ★ | ★★ | ★ | ★ | ★ | 7/9 | ||
| Traebert et al. 2012 [41] | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8/9 | |
| Piovesan et al. 2011 [42] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
| Aldrigui et al. 2011 [43] | ★ | ★★ | ★ | ★ | 5/9 | ||||
| Bendo et al. 2010 [44] | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8/9 | |
| Piovesan et al. 2010 [45] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9/9 |
Based on the Newcastle-Ottawa scale (NOS) adapted for observational studies
Of the studies included, 21 adjusted for oral conditions (dental caries and/or malocclusion) and other confounding factors such as sex, age, socio-economic status. The remainder presented unadjusted estimates, only. The overwhelming majority (n = 20), concluded that uncomplicated TDIs were not associated with a negative impact on the quality of life of children and adolescents. Two of the three case control studies did not find evidence that uncomplicated TDI affected OHRQoL in pre-schoolers (OR: 1.05; 95% CI: 0.54–1.99) [32] and adolescents (OR: 0.64; 95% CI: 0.38–1.06 [36]. The third case control study [30] found that pre-schoolers with uncomplicated TDIs had greater odds of having their OHRQoL impacted compared to children without TDIs (OR: 1.57; CI: 0.92–2.64).
Quantitative analysis
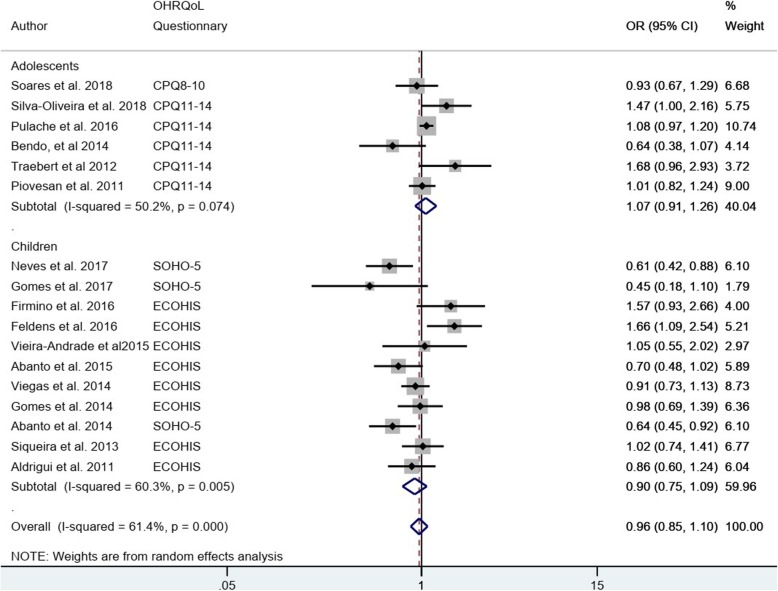
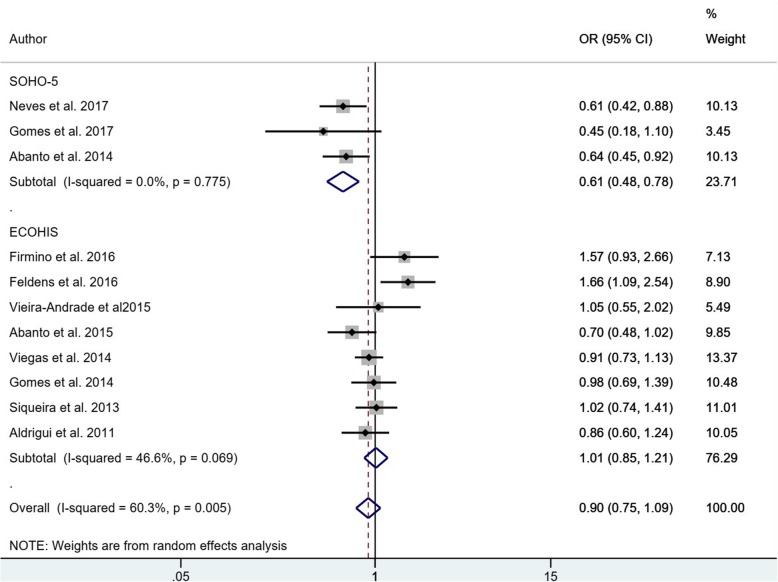
Nine studies were excluded from the meta-analysis because they did not provide the Odds ratio or the necessary data for its estimation [4, 24, 26, 28, 33, 39, 40, 44, 45]. The 17 studies included in quantitative analysis had 14,457 participants, which were evaluated for the dichotomous association between uncomplicated TDIs (presence/absence) and any impact on OHRQoL (presence/absence) (Fig. 2). The sub-total estimates for age groups (in two groups: early children (4 to 6 years old) and adolescents (8 to 19 years old)) are different: the pooled OR for studies of children was 0.90 (95% CI: 0.75–1.09), while heterogeneity was considerable (I2 = 60.3%) compared to adolescent studies with pooled OR 1.07 (95% CI: 0.91–1.26) and moderate heterogeneity (I2 = 50.2%). Both estimated confidence intervals included the null value (i.e.: 1), the overall pooled OR was 0.96 (95% CI: 0.85–1.10) and heterogeneity was moderate (I2 = 61.4%). The adolescent studies used the same OHRQoL questionnaire. However, the children studies used 2 types of OHRQoL questionnaire, for that reason a separate meta-analysis is presented. (Fig. 3) The sub-total estimates are different: SOHO-5 with a pooled OR of 0.61 (95% CI: 0.48, 0.78) and ECOHIS with a pooled OR of 1.01 (95% CI: 0.75, 1.09). The dataset is available in Additional file 5.
Fig. 2.
Meta-analysis: The association of uncomplicated TDI and OHRQoL by age groups
Fig. 3.
Meta-analysis: The association of uncomplicated TDI and OHRQoL by OHRQoL questionnaire used in children studies
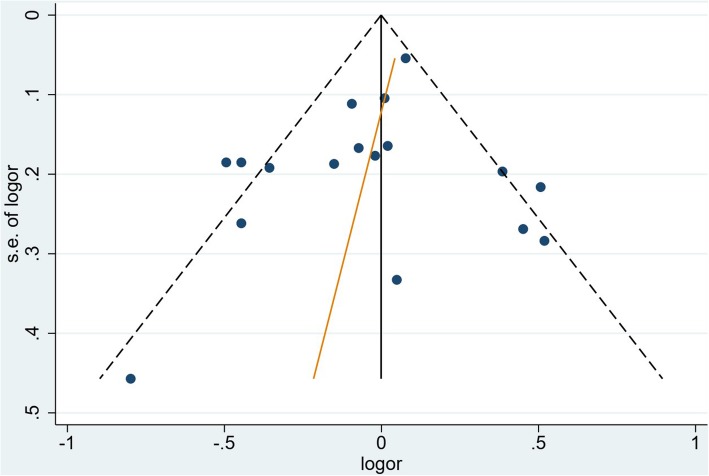
The risk of publication bias for the 17 studies included in the meta-analysis was assessed using a funnel plot and the Egger’s test (p: 0.415) in Fig. 4. The funnel is approximately symmetrical and the Egger’s test failed to detect publication bias. This implies that publication bias does not seems to be significant to the validity of the research.
Fig. 4.
Funnel plot with correspondent Egger’s test for all included studies. (p: 0.415)
Discussion
The narrative synthesis and the meta-analysis provided evidence that children and adolescents with uncomplicated TDIs have similar chances of any impact on OHRQoL to children and adolescents without TDIs. Most of the studies included in the review concluded that uncomplicated TDIs were not associated with a negative impact on the OHRQoL of life of children or adolescents. This is reflected in the findings of the meta-analysis, even after adjusting by age groups. Concordantly, some authors have suggested that enamel fractures, which are the most common uncomplicated TDI, have a minimal impact on OHRQoL from the standpoint of children and their families [4, 22, 24, 31, 42].
This review focused on the consequences of uncomplicated traumatic dental injuries alone as opposed to the implications of all types of TDIs combined, as in the two previously published systematic reviews [14, 15]. Present findings differ from these two systematic reviews. This may be due to differences in the research question, and because the estimates represent the effect of the less severe type of TDI on the OHRQoL of children and adolescents. One of these reviews [15] concluded that complicated TDIs were associated with a higher OHRQoL impact relative to uncomplicated TDIs.
As shown by the exposure assessment in the narrative synthesis, there is no universally accepted set of diagnostic, classification, and registration criteria for TDIs, which makes true comparisons difficult [48]. As argued by Petti et al., the majority of TDIs are relatively easy to diagnose; however, their classification is difficult because there are more than 50 distinct diagnostic criteria, and on top of that, of course, more than one injury can happen at the same time [1]. Since the diagnosis of TDI was based on prevalent cases, some TDI fractures, such as crown fractures, could be misclassified with other dental condition such as tooth wear or developmental dental defects [49].
From the narrative synthesis, the outcome assessment revealed that for studies with preschooler samples, the most used validated questionnaire was the ECOHIS, which relies on a proxy (parents or guardians) to answer the questionnaire. A systematic review concluded that parents have limited knowledge and a different perspective about some aspects compared with their children, especially perspectives related to quality of life and its dimensions [50]. This could lead to parents or guardians underestimating the true impact of children’s oral conditions on their oral health related quality of life. Furthermore, oral trauma in primary teeth is often disregarded by parents and guardians, unless the TDI is severe [50].
Studies with adolescent samples used either the CPQ for 11 to 14 years or its 8 to 10 years version (CPQ 8–10). These instruments rely on self-reported answers, which may provide more precise data on how quality of life is affected by TDIs. The use of the same questionnaire can explain the moderate heterogeneity compared to studies with samples of children in the meta-analysis. This review noticed an age gap in the current literature evaluating the impact of TDIs on the OHRQoL of children age 6 to 8 years. In general, studies with samples of children presented lower effect estimates compared to studies with adolescent samples, for the association between uncomplicated TDIs and OHRQoL. This could be explained, firstly, because the ECOHIS relies on proxy answers from a parent or guardian and a large percentage of guardians or parents may not recognise the occurrence of minor TDIs in their children [50, 51]; and secondly, adolescents may be more capable of understanding TDI’s effects on their quality of life. Further research should clarify the clinical importance of this difference.
The heterogeneity for the 17 studies included in the meta-analysis was substantial (I2: 61.4%). The primary source of heterogeneity was the different age of the samples; for that reason, sub-group analysis by age group was performed to reduce the heterogeneity. Other sources of heterogeneity were the fact that some studies were school-based, clinic-based or population-based, and the use of different diagnostic criteria for TDIs. Conversely, an influence that decreased heterogeneity was the fact that almost all of the studies were from Brazil.
Some limitations to this study must be noted. The most obvious one is that the majority of the studies included were of cross-sectional design, which may have limited the ability to reach conclusions on the nature of this association. Therefore, effects over a period of time may not have been properly evaluated. Additionally, the prevalence of the impact on OHRQoL could be overestimated due the lowest cut-off point (at least one item) used. Also, the external validity of the study might be reduced given that almost all of the studies were from Brazil.
On the other hand, the use of the broad search strategy is one of the strengths of the study, as it ensures that all studies on this topic were included. Another strength is that it used both narrative synthesis and meta-analysis to assess the association between uncomplicated TDIs and OHRQoL. Additionally, the decision to include studies with an established diagnostic criteria and a validated questionnaire further reinforced the reliability of the data. Finally, the high quality of the studies included and the absence of publication bias increased the validity of present results.
Conclusion
The narrative synthesis and the meta-analysis provided evidence that children and adolescents with any uncomplicated TDIs have similar chances of having an impact on OHRQoL to children and adolescents without TDIs. Suitable cut-off points to define when OHRQoL is impacted in children and adolescents are required. Public health programs can achieve the maximum impact in reducing the negative impact on OHRQoL from dental injury if more severe TDIs are the focus of such programs. However, the implications of uncomplicated TDIs over time is not well understood, and prospective cohort studies are required to confirm the results of this review.
Supplementary information
Additional file 1. Specific search strategy: Includes the specific terms used in the literature search in the mentioned databases.
Additional file 2. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of case control studies and Cross-sectional: Study quality assessment tool used in the review.
Additional file 3. List of excluded studies and reasons after the full-text review: Studies excluded from the review with the reasons.
Additional file 4. Study characteristics and the association between uncomplicated TDI and OHRQoL in children and adolescents: Condensed tables that summarized the information extracted from each paper.
Additional file 5. Study dataset: The dataset used in the meta-analysis.
Abbreviations
- CPQ 11–14
Child Perceptions Questionnaire version for 11 to 14 years old
- CPQ 8–10
Child Perceptions Questionnaire version for 8 to 10 years old
- ECOHIS
Early Childhood Oral Health Impact Scale
- OHRQoL
Oral health related quality of life
- SOHO-5
Scale of Oral Health Outcomes for Five-Year-Old Children
- TDIs
Traumatic Dental Injuries
Authors’ contributions
DL contributed the conception of the study, the data analysis and the design and draft of the manuscript, and read and approved the final manuscript. NW contributed the data analysis, the design and draft of the manuscript, and read and approved the final manuscript. CZ contributed with the selection of the studies, quality assessment, the design and draft of the manuscript, and read and approved the final manuscript. RM contributed the conception of the study and the design and draft of the manuscript, and read and approved the final manuscript.
Authors’ information
DL is a DDS and Master of Public health graduate of the University of Melbourne, Melbourne, Australia.
NW works Co-coordinator Epidemiology 3 in the School of Population and Global Health and at the Allergy and Lung health department, University of Melbourne, Melbourne, Australia.
CZ is an Associate Professor at the Department of Pediatric Dentistry and Orthodontics, Universidad de La Frontera, Temuco, Chile.
RM is a Professor at the Melbourne Dental School, University of Melbourne, Melbourne, Australia.
Funding
The authors received no specific funding for this work.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Ethics approval and consent to participate
Data reported in this manuscript are available from public sources, with no element of intervention. As such, it does not need IRB approval. Hence, it did not formally go through the review of an ethics committee.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests. RM is a Section Editor for BMC Oral Health.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Diego Lopez, Email: diegol@student.unimelb.edu.au.
Nilakshi Waidyatillake, Email: nilakshi.waidyatillake@unimelb.edu.au.
Carlos Zaror, Email: carlos.zaror@ufrontera.cl.
Rodrigo Mariño, Email: r.marino@unimelb.edu.au.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12903-019-0916-0.
References
- 1.Petti S, Glendor U, Andersson L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent Traumatol. 2018;34(2):71–86. doi: 10.1111/edt.12389. [DOI] [PubMed] [Google Scholar]
- 2.Glendor U. Epidemiology of traumatic dental injuries - a 12 year review of the literature. Dent Traumatol. 2008;24(6):603–611. doi: 10.1111/j.1600-9657.2008.00696.x. [DOI] [PubMed] [Google Scholar]
- 3.Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. 4. Oxford; Ames: Blackwell; 2007. [Google Scholar]
- 4.Ramos-Jorge J, Sa-Pinto AC, Almeida Pordeus I, Martins Paiva S, Castro Martins C, Ramos-Jorge ML. Effect of dark discolouration and enamel/dentine fracture on the oral health-related quality of life of pre-schoolers. Eur Arch Paediatr Dent. 2017;18(2):83–89. doi: 10.1007/s40368-017-0271-2. [DOI] [PubMed] [Google Scholar]
- 5.Viegas CM, Paiva SM, Carvalho AC, Scarpelli AC, Ferreira FM, Pordeus IA. Influence of traumatic dental injury on quality of life of Brazilian preschool children and their families. Dent Traumatol. 2014;30(5):338–347. doi: 10.1111/edt.12091. [DOI] [PubMed] [Google Scholar]
- 6.Kenny KP, Day PF, Sharif MO, Parashos P, Lauridsen E, Feldens CA, Cohenca N, Skapetis T, Levin L, Kenny DJ, et al. What are the important outcomes in traumatic dental injuries? An international approach to the development of a core outcome set. Dent Traumatol. 2018;34(1):4–11. doi: 10.1111/edt.12367. [DOI] [PubMed] [Google Scholar]
- 7.Aldrigui JM, Cadioli IC, Mendes FM, Antunes JL, Wanderley MT. Predictive factors for pulp necrosis in traumatized primary incisors: a longitudinal study. Int J Paediatr Dent. 2013;23(6):460–469. doi: 10.1111/ipd.12019. [DOI] [PubMed] [Google Scholar]
- 8.Baiju RM, Peter E, Varghese NO, Sivaram R. Oral health and quality of life: current concepts. J Clin Diagn Res. 2017;11(6):Ze21–ze26. doi: 10.7860/JCDR/2017/25866.10110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaror C, Pardo Y, Espinoza-Espinoza G, Pont A, Munoz-Millan P, Martinez-Zapata MJ, Vilagut G, Forero CG, Garin O, Alonso J, et al. Assessing oral health-related quality of life in children and adolescents: a systematic review and standardized comparison of available instruments. Clin Oral Investig. 2019;23(1):65–79. doi: 10.1007/s00784-018-2406-1. [DOI] [PubMed] [Google Scholar]
- 10.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children’s oral health: the Early Childhood Oral Health Impact Scale (ECOHIS) Health Qual Life Outcomes. 2007;5:6–6. doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsakos G, Blair YI, Yusuf H, Wright W, Watt RG, Macpherson LM. Developing a new self-reported scale of oral health outcomes for 5-year-old children (SOHO-5) Health Qual Life Outcomes. 2012;10:62. doi: 10.1186/1477-7525-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81(7):459–463. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 13.Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. 2003. [PubMed] [Google Scholar]
- 14.Borges TS, Vargas-Ferreira F, Kramer PF, Feldens CA. Impact of traumatic dental injuries on oral health-related quality of life of preschool children: a systematic review and meta-analysis. PLoS One. 2017;12(2):e0172235. doi: 10.1371/journal.pone.0172235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaror C, Martiinez-Zapata MJ, Abarca J, Diaz J, Pardo Y, Pont A, Ferrer M. Impact of traumatic dental injuries on quality of life in preschoolers and schoolchildren: a systematic review and meta-analysis. Community Dent Oral Epidemiol. 2018;46(1):88–101. doi: 10.1111/cdoe.12333. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilchrist F, Rodd H, Deery C, Marshman Z. Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health. 2014;14:40. 10.1186/1472-6831-14-40. [DOI] [PMC free article] [PubMed]
- 18.Sacks D, Canadian Paediatric S, Adolescent Health C. Age limits and adolescents. Paediatr Child Health. 2003;8(9):577. doi: 10.1093/pch/8.9.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wells GA, Shea B, O'Connell D. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. 2006. [Google Scholar]
- 20.Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101–117. doi: 10.1016/S0899-3467(07)60142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed) 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soares JP, Barasuol JC, Torres FM, Giacomin A, Goncalves BM, Klein D, Borgatto AF, Ramos-Jorge ML, Cardoso M, Bolan M. The impact of crown fracture in the permanent dentition on children’s quality of life. Dent Traumatol. 2018;30:30. doi: 10.1111/edt.12400. [DOI] [PubMed] [Google Scholar]
- 23.Silva-Oliveira F, Goursand D, Ferreira RC, Paiva PCP, Paiva HN, Ferreira EF, Zarzar PM. Traumatic dental injuries in Brazilian children and oral health-related quality of life. Dent Traumatol. 2018;34(1):28–35. doi: 10.1111/edt.12358. [DOI] [PubMed] [Google Scholar]
- 24.Martins MT, Sardenberg F, Bendo CB, Vale MP, Paiva SM, Pordeus IA. Dental caries are more likely to impact on children's quality of life than malocclusion or traumatic dental injuries. Eur J Paediatr Dent. 2018;19(3):194–198. doi: 10.23804/ejpd.2018.19.03.5. [DOI] [PubMed] [Google Scholar]
- 25.Neves ETB, Perazzo MF, Gomes MC, Martins CC, Paiva SM, Granville-Garcia AF. Perception of parents and self-reports of children regarding the impact of traumatic dental injury on quality of life. Dent Traumatol. 2017;33(6):444–450. doi: 10.1111/edt.12366. [DOI] [PubMed] [Google Scholar]
- 26.Gonçalves BM, Dias LF, Pereira CS, Ponte Filho MX, Konrath AC, Bolan MS, Cardoso M. O impacto do traumatismo dental e do comprometimento estético na qualidade de vida de pré-escolares. Rev Paul Pediatr. 2017;35(4):448–455. doi: 10.1590/1984-0462/;2017;35;4;00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gomes MC, Perazzo MF, Neves ÉT, Martins CC, Paiva SM, Granville-Garcia AF. Oral problems and self-confidence in preschool children. Braz Dent J. 2017;28(4):523–530. doi: 10.1590/0103-6440201601295. [DOI] [PubMed] [Google Scholar]
- 28.Bomfim RA, Herrera DR, De-Carli AD. Oral health-related quality of life and risk factors associated with traumatic dental injuries in Brazilian children: a multilevel approach. Dent Traumatol. 2017;33(5):358–368. doi: 10.1111/edt.12348. [DOI] [PubMed] [Google Scholar]
- 29.Pulache J, Abanto J, Oliveira LB, Bonecker M, Porras JC. Exploring the association between oral health problems and oral health-related quality of life in Peruvian 11- to 14-year-old children. Int J Paediatr Dent. 2016;26(2):81–90. doi: 10.1111/ipd.12160. [DOI] [PubMed] [Google Scholar]
- 30.Firmino RT, Gomes MC, Clementino MA, Martins CC, Paiva SM, Granville-Garcia AF. Impact of oral health problems on the quality of life of preschool children: a case-control study. Int J Paediatr Dent. 2016;26(4):242–249. doi: 10.1111/ipd.12182. [DOI] [PubMed] [Google Scholar]
- 31.Feldens CA, Day P, Borges TS, Feldens EG, Kramer PF. Enamel fracture in the primary dentition has no impact on children's quality of life: implications for clinicians and researchers. Dent Traumatol. 2016;32(2):103–109. doi: 10.1111/edt.12222. [DOI] [PubMed] [Google Scholar]
- 32.Vieira-Andrade RG, Siqueira MB, Gomes GB, D’Avila S, Pordeus IA, Paiva SM, Granville-Garcia AF. Impact of traumatic dental injury on the quality of life of young children: a case-control study. Int Dent J. 2015;65(5):261–268. doi: 10.1111/idj.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freire-Maia FB, Auad SM, Abreu MH, Sardenberg F, Martins MT, Paiva SM, Pordeus IA, Vale MP. Oral health-related quality of life and traumatic dental injuries in young permanent incisors in Brazilian schoolchildren: a multilevel approach. PLoS One. 2015;10(8):e0135369. doi: 10.1371/journal.pone.0135369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abanto J, Tello G, Bonini GC, Oliveira LB, Murakami C, Bonecker M. Impact of traumatic dental injuries and malocclusions on quality of life of preschool children: a population-based study. Int J Paediatr Dent. 2015;25(1):18–28. doi: 10.1111/ipd.12092. [DOI] [PubMed] [Google Scholar]
- 35.Gomes MC, Pinto-Sarmento TC, Costa EM, Martins CC, Granville-Garcia AF, Paiva SM. Impact of oral health conditions on the quality of life of preschool children and their families: a cross-sectional study. Health Qual Life Outcomes. 2014;12:55. doi: 10.1186/1477-7525-12-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bendo CB, Paiva SM, Varni JW, Vale MP. Oral health-related quality of life and traumatic dental injuries in Brazilian adolescents. Community Dentistry Oral Epidemiol. 2014;42(3):216–223. doi: 10.1111/cdoe.12078. [DOI] [PubMed] [Google Scholar]
- 37.Abanto J, Tsakos G, Paiva SM, Carvalho TS, Raggio DP, Bonecker M. Impact of dental caries and trauma on quality of life among 5- to 6-year-old children: perceptions of parents and children. Community Dentistry Oral Epidemiol. 2014;42(5):385–394. doi: 10.1111/cdoe.12099. [DOI] [PubMed] [Google Scholar]
- 38.Siqueira MB, Firmino RT, Clementino MA, Martins CC, Granville-Garcia AF, Paiva SM. Impact of traumatic dental injury on the quality of life of Brazilian preschool children. Int J Environ Res Public Health. 2013;10(12):6422–6441. doi: 10.3390/ijerph10126422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dame-Teixeira N, Alves LS, Ardenghi TM, Susin C, Maltz M. Traumatic dental injury with treatment needs negatively affects the quality of life of Brazilian schoolchildren. Int J Paediatr Dent. 2013;23(4):266–273. doi: 10.1111/ipd.12002. [DOI] [PubMed] [Google Scholar]
- 40.Viegas CM, Scarpelli AC, Carvalho AC, Ferreira Fde M, Pordeus IA, Paiva SM. Impact of traumatic dental injury on quality of life among Brazilian preschool children and their families. Pediatr Dent. 2012;34(4):300–306. [PubMed] [Google Scholar]
- 41.Traebert J, de Lacerda JT, Foster Page LA, Thomson WM, Bortoluzzi MC. Impact of traumatic dental injuries on the quality of life of schoolchildren. Dent Traumatol. 2012;28(6):423–428. doi: 10.1111/j.1600-9657.2012.01114.x. [DOI] [PubMed] [Google Scholar]
- 42.Piovesan C, Abella C, Ardenghi TM. Child oral health-related quality of life and socioeconomic factors associated with traumatic dental injuries in schoolchildren. Oral Health Prev Dent. 2011;9(4):405–411. [PubMed] [Google Scholar]
- 43.Aldrigui JM, Abanto J, Carvalho TS, Mendes FM, Wanderley MT, Bonecker M, Raggio DP. Impact of traumatic dental injuries and malocclusions on quality of life of young children. Health Qual Life Outcomes. 2011;9:78. doi: 10.1186/1477-7525-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bendo CB, Paiva SM, Torres CS, Oliveira AC, Goursand D, Pordeus IA, Vale MP. Association between treated/untreated traumatic dental injuries and impact on quality of life of Brazilian schoolchildren. Health Qual Life Outcomes. 2010;8:114. doi: 10.1186/1477-7525-8-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Piovesan C, Antunes JL, Guedes RS, Ardenghi TM. Impact of socioeconomic and clinical factors on child oral health-related quality of life (COHRQoL) Qual Life Res. 2010;19(9):1359–1366. doi: 10.1007/s11136-010-9692-7. [DOI] [PubMed] [Google Scholar]
- 46.Glendor U, Halling A, Andersson L, Eilert-Petersson E. Incidence of traumatic tooth injuries in children and adolescents in the county of Vastmanland, Sweden. Swed Dent J. 1996;20(1–2):15–28. [PubMed] [Google Scholar]
- 47.O’Brien M. Children’s dental health in the United Kingdom, 1993: a survey carried out by the Social Survey Division of OPCS, on behalf of the United Kingdom health departments, in collaboration with the Dental Schools of the Universities of Birmingham and Newcastle. London: HMSO; 1994. [Google Scholar]
- 48.Sharif MO, Tejani-Sharif A, Kenny K, Day PF. A systematic review of outcome measures used in clinical trials of treatment interventions following traumatic dental injuries. Dent Traumatol. 2015;31(6):422–428. doi: 10.1111/edt.12227. [DOI] [PubMed] [Google Scholar]
- 49.Chadwick BL, White DA, Morris AJ, Evans D, Pitts NB. Non-carious tooth conditions in children in the UK, 2003. Br Dent J. 2006;200(7):379–384. doi: 10.1038/sj.bdj.4813424. [DOI] [PubMed] [Google Scholar]
- 50.Barbosa TS, Gaviao MB. Oral health-related quality of life in children: part III. Is there agreement between parents in rating their children's oral health-related quality of life? A systematic review. Int J Dent Hyg. 2008;6(2):108–113. doi: 10.1111/j.1601-5037.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 51.Ramos-Jorge ML, Ramos-Jorge J, Mota-Veloso I, Oliva KJ, Zarzar PM, Marques LS. Parents’ recognition of dental trauma in their children. Dent Traumatol. 2013;29(4):266–271. doi: 10.1111/edt.12005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Specific search strategy: Includes the specific terms used in the literature search in the mentioned databases.
Additional file 2. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of case control studies and Cross-sectional: Study quality assessment tool used in the review.
Additional file 3. List of excluded studies and reasons after the full-text review: Studies excluded from the review with the reasons.
Additional file 4. Study characteristics and the association between uncomplicated TDI and OHRQoL in children and adolescents: Condensed tables that summarized the information extracted from each paper.
Additional file 5. Study dataset: The dataset used in the meta-analysis.
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].