Oseltamivir phosphate is used as a first line of defense in the event of an influenza pandemic prior to vaccine administration. Treatment failure through selection and replication of drug-resistant viruses is a known complication in the field and was also demonstrated in our study with spread of resistant 1918 influenza virus in multiple respiratory tissues. This emphasizes the importance of early treatment and the possibility that noncompliance may exacerbate treatment effectiveness. It also demonstrates the importance of implementing combination therapy and vaccination strategies as soon as possible in a pandemic situation.
KEYWORDS: 1918 influenza virus, treatment, oseltamivir, drug resistance
ABSTRACT
The 1918 influenza virus, subtype H1N1, was the causative agent of the most devastating pandemic in the history of infectious diseases. In vitro studies have confirmed that extreme virulence is an inherent property of this virus. Here, we utilized the macaque model for evaluating the efficacy of oseltamivir phosphate against the fully reconstructed 1918 influenza virus in a highly susceptible and relevant disease model. Our findings demonstrate that oseltamivir phosphate is effective in preventing severe disease in macaques but vulnerable to virus escape through emergence of resistant mutants, especially if given in a treatment regimen. Nevertheless, we conclude that oseltamivir would be highly beneficial to reduce the morbidity and mortality rates caused by a highly pathogenic influenza virus although it would be predicted that resistance would likely emerge with sustained use of the drug.
INTRODUCTION
The influenza pandemic in 1918, caused by an influenza A virus of subtype H1N1, remains the deadliest infectious disease outbreak recorded in human history, with an estimated 50 million deaths worldwide (1–4). The reconstructed 1918 influenza virus (5, 6) is highly pathogenic in mice, ferrets, and cynomolgus macaques (Macaca fascicularis), and the virulent phenotype is multigenic in origin (5–9). Infection with the 1918 virus in mice and nonhuman primates is characterized by a dysregulated antiviral response that is insufficient for protection, indicating that atypical host innate immune responses may contribute to lethality (6, 10). The observed virulence of the 1918 virus, the rapid global spread of the 2009 H1N1 influenza virus (11, 12), and the continued pandemic potential posed by circulation of the highly virulent H5N1 virus substantiated the need for evaluating antiviral options against infections with virulent influenza viruses.
Here, we demonstrate that oseltamivir phosphate, which has never been evaluated in macaques against infection with the fully reconstructed 1918 influenza virus (5, 6), is effective in preventing severe disease in cynomolgus macaques if given prophylactically. Efficacy was reduced in a treatment regimen through emergence of oseltamivir-resistant mutants that led to the death of one of four animals. Our demonstration of the presence of oseltamivir-resistant virus in upper respiratory tract secretions suggests that spread of drug-resistant virus, even from successfully treated individuals, is likely to be a problem where sustained transmission of virus occurs. This emphasizes the importance of implementing combination therapy and vaccination strategies early in an epidemic or pandemic.
RESULTS
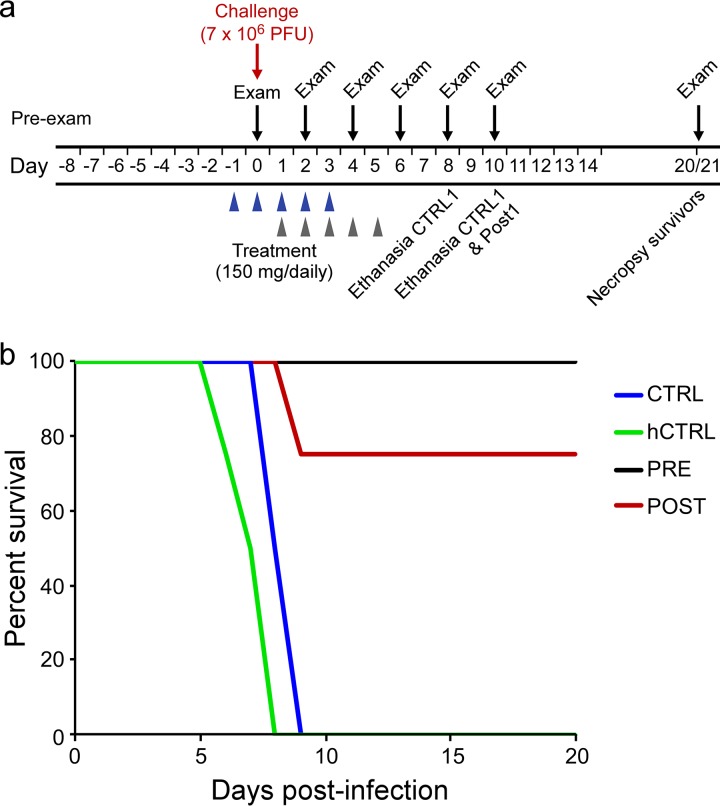
Cynomolgus macaques (Macaca fascicularis) (n = 10), confirmed to be seronegative against current H1N1 and H3N2 influenza reference viruses by hemagglutination (HA) inhibition assay, were randomly divided into prophylaxis (n = 4), treatment (n = 4), and control (n = 2) groups. All animals were infected with 7 × 106 PFU of the 1918 influenza virus through a combination of routes optimized for infection of the upper and lower respiratory tract tissues (6). The prophylaxis group (animals PRE1 to PRE4) was given oseltamivir phosphate starting 24 h prior to infection, while animals in the treatment group (animals POST1 to POST4) were treated starting 24 h postinfection (hpi) (Fig. 1). All animals were given a single dose of 150 mg oseltamivir phosphate daily, to provide the daily dose given for human treatment (2 × 75 mg), and administration was continued in both groups for a total of 5 days, the course recommended for uncomplicated seasonal influenza (13). The drug was given as a supplement in food for the first 3 days in the PRE group and first 2 days in the POST group, and animals were observed to ensure that the drug was consumed. Following refusal of animal POST1 to voluntarily consume all of the drug/food 2 days postinfection (dpi), all animals were subsequently treated using an intragastric tube. The control group (animals CTRL1 and CTRL2) was treated with phosphate-buffered saline (PBS) using the same protocol.
FIG 1.
Oseltamivir treatment. (a) Experimental design. Four animals (PRE1 to PRE4) were treated with a single dose of oseltamivir phosphate (150 mg) starting 24 h before infection, 4 animals (POST1 to POST4) were treated with oseltamivir starting 24 h postinfection, and 2 animals (CTRL1 and CTRL2) served as controls and were treated with PBS. Treatment was continued for a total of 5 consecutive days. All animals were challenged with the 1918 influenza virus (total, 7 × 106 PFU) by four different routes. (b) Survival curve. Both controls (CTRL1 and CTRL2) and one posttreated animal (POST1) had to be euthanized on 8 and 9 dpi. All other treated animals developed mild to moderate/severe clinical symptoms but survived. Four untreated controls were added from a separate experiment (historical controls [hCTRL]) (6).
Animals were monitored twice daily for clinical signs using an approved scoring sheet. At indicated time points prior and after infection (Fig. 1a) as well as at euthanasia, blood and swabs (oral, nasal, throat, and rectal) were collected from anaesthetized animals and vital signs (pulse rate, blood pressure, temperature, respiration rate, and oxygen saturation) were recorded. All infected animals became symptomatic within 48 h postinfection, showing reduced or no food intake, elevated respiration rates, and decreased oxygen saturation, with the POST treatment animals being more highly affected (see Table S1 in the supplemental material). The two PBS-treated control animals (CTRL1 and CTRL2) and the POST1 animal became progressively moribund and developed an acute respiratory distress syndrome, reaching the predetermined euthanasia score on days 8 and 9 (Fig. 1; see also Table S1). All other treated animals recovered after mild/moderate (PRE1 to PRE4) or moderate/severe (POST2 to POST4) clinical signs (Fig. 1b; see also Table S1). The recovered animals were euthanized on day(s) post infection (dpi) 20 or 21 for pathological and virological examination of tissues in the upper and lower respiratory tract tissues, the primary sites of viral replication as previously identified (6).
Clinical presentation of animals. Download Table S1, DOCX file, 0.01 MB (9.6KB, docx) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
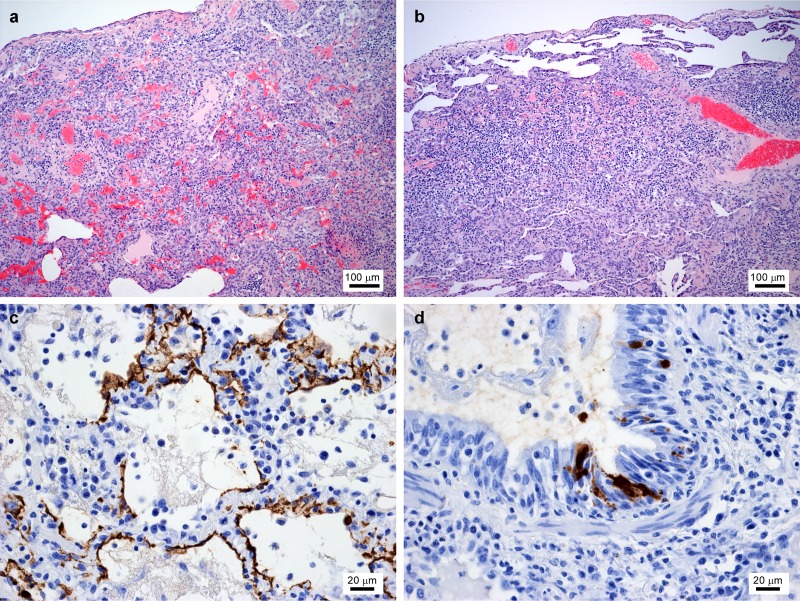
The lungs of animals CTRL1, CTRL2, and POST1 exhibited macroscopic pathological changes, with 60% to 90% of tissue found to be affected at necropsy. As previously described (6), microscopic changes, including bronchiolitis and bronchitis, were prominent, with widespread alveolar damage, extensive edema, and hemorrhagic exudates. Flattened alveolar cells and desquamation of plumb alveolar cells into the alveolar space were observed (see Kobasa et al. [6]). Viral antigen was found predominantly in peribronchiolar alveoli and the bronchiolar epithelium (Fig. 2c and d). At 20/21 dpi, lungs of surviving animals from the PRE and POST groups showed a chronic healing stage following pneumonia, with remaining areas of consolidation and thickening of alveolar walls due to infiltration of mononuclear cells and deposition of fibrous tissue (Fig. 2a and b). Viral antigen was not found in respiratory tissues of these animals at these later time points.
FIG 2.
Histopathology of oseltamivir-treated animals. (a and b) Hematoxylin and eosin (HE) staining of the lungs of oseltamivir-pretreated (a) and -posttreated (b) surviving animals at day 20 postinfection, showing a chronic healing stage of pneumonia with areas of consolidation and thickening of alveolar walls due to infiltration of mononuclear cells and deposition of fibrous tissue. (c and d) The presence of viral antigen was demonstrated using an antibody directed to the viral nucleoprotein and was detectable only at the time of euthanasia in the controls (not shown) and animal POST1, which was euthanized on 9 dpi. Viral nucleoprotein was found in alveolar cells (c) and bronchiolar epithelium (d).
Infectious virus was found by 50% tissue culture infective dose (TCID50) assay in respiratory tissues and the heart of POST1 and the control animals. All other treated animals were found at euthanasia to have cleared infectious virus (Table S2). Quantitative real-time reverse transcription-PCR (qRT-PCR), performed using primers targeting the hemagglutinin (HA) and matrix protein (M) genes, confirmed the results of the infectivity assay, but lung and tonsil tissues of animal POST2 and lung and bronchial tissue of animal PRE1 remained weakly positive by RT-PCR. Virus titers in both the upper and lower respiratory tract tissues of POST1 were substantially lower than those measured for the controls (Table S2). As previously reported (6), virus was also isolated from the heart, the only tissue outside the respiratory tract that seemed infected. Virus replication and shedding from mucosal surfaces were quantified by TCID50 assay and qRT-PCR in oral, throat, nasal and rectal swab samples. Virus isolation was successful only from throat and nasal swabs (Table 1). Viral replication and shedding occurred mainly in the controls and in animal POST1, although virus was sporadically detected in some successfully treated animals (PRE2 to PRE4 and POST2) (Table 1). qRT-PCR confirmed the infectivity data, but the results remained weakly positive in qRT-PCR for a longer period than infectious virus could be detected (data not shown).
TABLE 1.
Virus titers in nasal and throat swabsa
| Animal ID | Nasal swab/throat swab titers (TCID50) |
|||||
|---|---|---|---|---|---|---|
| Day 2 | Day 4 | Day 6 | Day 8 | Day 10 | Day 14 | |
| CTRL1 | 1.5 × 103/neg | 1.5 × 101/neg | 7.0 × 103/8.8 × 103 | 1 × 104/neg | NA | NA |
| CTRL2 | 1.5 × 103/neg | 1.5 × 102/neg | 1.5 × 101/neg | 1.5 × 101/neg | NA | NA |
| PRE1 | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg |
| PRE2 | neg/neg | 1.5 × 102/neg | neg/1.5 × 101 | neg/neg | neg/neg | neg/neg |
| PRE3 | neg/neg | 1.5 × 101/neg | 1.5 × 101/neg | neg/neg | neg/neg | neg/neg |
| PRE4 | 8 × 101/neg | 1.5 × 102/5 × 100 | neg/3 × 102 | neg/neg | neg/neg | neg/neg |
| POST1 | neg/neg | 7.0 × 102/neg | 1.5 × 102/6.6 × 101 | 1.5 × 101/6.6 × 101 | NA | NA |
| POST2 | 1.5 × 101/neg | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg |
| POST3 | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg |
| POST4 | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg | neg/neg |
Virus titers were determined using a TCID50 assay as described in Materials and Methods; CTRL, control animal; ID, identifier; neg, negative; PRE, pretreated animal; POST, posttreated animal; NA, not applicable (animal already euthanized).
Virus titers in tissues at time of euthanasia. Download Table S2, DOCX file, 0.01 MB (9.6KB, docx) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Respiratory tissues of POST1 contained virus at lower levels than those of the untreated controls (Table S2). To characterize whether the virus, which had continued to replicate after antiviral treatment was withdrawn, was wild type or was drug-resistant virus that had become established during treatment, we used a two-step approach. First, we isolated individual virus plaques from the nasal mucosa and the right caudal lung tissues. The HA and neuraminidase (NA) genes of 20 individual plaques isolated from the lung were PCR amplified and completely sequenced. All plaques (20/20) showed a His275Tyr mutation in NA (N2 numbering position 274) (Table 2). Most plaques (17/20) showed an additional mutation, Asp187Val (H3 numbering position 190), in the HA, which has not previously been reported in association with oseltamivir resistance (Table 2), while the remaining three plaques had mutation Asp187Asn. Similar analysis of plaques from the nasal mucosa showed that all (20/20) contained the His275Tyr mutation in NA but that none contained mutations in HA. Neither the NA nor HA mutations occurred in virus isolated from the lung or nasal mucosa of the untreated controls.
TABLE 2.
Mutations occurring in animal POST1 under oseltamivir treatmenta
| Tissue | Analysis | % of sequence showing mutations (no. of plaques showing mutations/total no. of plaques analyzed) |
||||
|---|---|---|---|---|---|---|
| NA His275Tyr |
HA Asp187Val |
HA Asp187Asn |
HA Asp222Asn |
HA Asp222Gly |
||
| Nasal mucosa | Plaque | 100 (20/20) | 0 (0/20) | NT | NT | NT |
| Trachea | PCR | 100 (5/5) | 0 (wt) | 0 (wt) | 75 (3/4) | 25 (1/4) |
| Right bronchus | PCR | 100 (2/2) | 75 (3/4) | 0 (wt) | 25 (1/4) | 0 (wt) |
| Left bronchus | PCR | 100 (3/3) | 75 (wt) (3/4) | 25 (1/4) | 25 (1/4) | 75 (wt) (3/4) |
| Right lung upper | PCR | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) |
| Right lung middle | PCR | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) |
| Right lung caudal | Plaque | 100 (20/20) | 85 (17/20) | 15 (3/20) | 0 (wt) | 0 (wt) |
| Left lung upper | PCR | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) |
| Left lung middle | PCR | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) |
| Left lung caudal | PCR | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) | 0 (wt) |
Plaque, virus isolation by plaque assay and subsequent direct sequence determination; PCR, RT-PCR of total RNA isolated from the specimen followed by molecular cloning and sequence determination (2 to 6 individual clones each); NT, not tested; wt, wild-type sequence.
Further analysis for the presence of drug-resistant virus in other tissues that contained virus (Table S2) was done by RT-PCR amplification and sequencing. No tissues from the controls contained mutant virus. In animal POST1, analysis of virus populations in the nasal mucosa by this method showed a mixed population of NA genes with both wild-type sequences and mutant sequences (His275Tyr). However, the NA sequences in viruses from other tissues consisted exclusively of either wild-type sequence (other lobes of the right and the entire left lung) or mutant sequence (trachea and bronchi) (Table 2). The only other tissue containing the Asp187Val mutation in HA was the right bronchus (75% of clones). However, several other HA mutations were identified: Asp222Asn (H3 numbering position 225) (25%, right bronchus; 75%, trachea); Asp222Gly (25%, trachea); Asp222Asn or Asp187Asn (50%, left bronchus); and Asp187Asn (15%, right caudal lung). Mutations at position 222 have been reported in viruses isolated from individuals treated with oseltamivir (14). Asp222 is associated with preferential binding to NeuAc-α2,6-Gal, the dominant species of sialic acid found in the human upper respiratory tract, while Gly or Asn at this position shifts the preferential binding specificity to NeuAc-α2,3-Gal, the primary species of sialic acid found at sites of viral replication in avian species (15, 16). It was suggested that the appearance of Asn or Gly at position 225 occurred in response to the requirement to reduce dependence on NA activity. Similarly, Asp190Asn and Asp190Val in a H1 HA have been shown to result in lower binding affinity for NeuAc-α2,6-Gal and higher affinity for NeuAc-α2,3-Gal (17, 18). Mutations in NA that confer resistance to oseltamivir generally reduce NA enzymatic activity; therefore, concomitant mutations in HA that reduce its affinity for its cellular receptor may be needed to maintain the critical balance between the activities of HA and NA to permit virus to spread efficiently (16, 19).
Following identification of oseltamivir-resistant virus in upper and lower respiratory tract tissues of animal POST1, we examined virus in throat and nasal swabs to determine whether the animal was shedding the oseltamivir-resistant virus (Table 1) and, if so, when resistance had first appeared. Drug-resistant viruses were first detected in the throat swab at 6 dpi and in both throat and nasal swabs at 8 dpi. There were equal proportions of wild-type and His275Tyr mutant viruses in the two swab types. No viruses contained mutations in HA, indicating that HA mutations are not required for shedding of drug-resistant virus. It was also of interest to determine whether any of the successfully treated animals were shedding or contained drug-resistant viruses (Table 1). POST2 had viruses (25% of clones) containing NA His275Tyr in lung tissue samples but not in tonsil samples, representing the only two tissues containing virus detectable by RT-PCR at the time of euthanasia. Interestingly, HA from the same animal showed the Asp187Val mutation (33% of the clones) in the lung. PRE1 had virus with only wild-type sequences in the tissues that still contained virus detectable by RT-PCR (bronchi, lung). Examination of virus shed from the successfully treated animals showed that animal PRE2 had detectable levels of drug-resistant virus, containing NA mutation His275Tyr at 8 dpi in both nasal and oral swabs. All described RT-PCR-positive samples likely represented very low titers of virus, since virus was not isolated on Madin-Darby canine kidney (MDCK) cells in any of these cases (Table S2). Although shed virus was detected by RT-PCR for most of the other animals at 6 to 8 dpi, none of the other successfully treated animals shed drug-resistant virus. These findings show that development of resistance to oseltamivir occurred even in successfully treated animals.
To confirm that the NA mutation His275Tyr conferred resistance to oseltamivir, we engineered recombinant influenza viruses containing either 1918 influenza virus wild-type NA or the 1918 His275Tyr mutant, with the rest of the genes coming from A/WSN/33 (H1N1). The concentration of oseltamivir carboxylate, the active form of the drug, that inhibited the NA activity by 50% (IC50) was 448 times higher for the mutant (IC50 = 1,750 nM) than for the wild-type NA (IC50 = 3.9 nM), demonstrating the effect of the mutation on resistance to oseltamivir. However, the mutation did not confer resistance to zanamivir, with IC50 values for wild-type and mutant NA of 0.72 nM and 0.52 nM, respectively. The observation that His275Tyr differentially confers resistance to oseltamivir and zanamivir is consistent with previously reported findings (16, 19). Considering the well-characterized role of NA mutations in development of resistance to oseltamivir (19) and the presence of high tissue titers of drug-resistant virus without HA mutations, the role of the HA mutations was not further assessed. However, it should be recognized that the Asp187Val HA mutation was never previously found in association with oseltamivir treatment and that HA mutations may play a supporting role in the development of resistance of NA mutated virus or in its adaptation to enhanced in vivo replication.
DISCUSSION
Oseltamivir phosphate is a neuraminidase inhibitor and may be used as a first line of defense in the event of an influenza pandemic caused by a newly emerged influenza virus, such as the pandemic H1N1 influenza virus (20), highly pathogenic avian H5 viruses (21), and other emerging influenza viruses, including H7N9 viruses (22, 23). Oseltamivir phosphate had previously shown efficacy in mice against infection with recombinant viruses bearing the 1918 influenza HA, NA, and M gene segments (7), but evaluation against the fully reconstructed 1918 influenza virus has never been reported previously in macaques. Here, we show that oseltamivir treatment of macaques infected with the 1918 virus was successful in reducing disease and increasing survival when initiated prior to infection and partially successful when administered 24 h postinfection. However, the latter scenario represents an expected treatment regimen following known exposure to a virus, such as accidental infection with the 1918 virus, and selection and replication of drug-resistant virus complicated treatment and reduced the effectiveness of treatment. Treatment failure in one of four treated animals, associated with development and spread of resistant virus in multiple respiratory tissues, emphasizes the importance of early treatment and the possibility that noncompliance may exacerbate treatment ineffectiveness. Our demonstration of oseltamivir-resistant virus in upper respiratory tract secretions suggests that spread of drug-resistant virus, even from successfully treated individuals, is likely to be a problem where sustained transmission of virus occurs, such as in a pandemic.
Two classes of drugs against influenza virus infections have been approved over the decades, namely, the M2 ion channel inhibitors and neuraminidase inhibitors such as amantadine and oseltamivir, respectively (24, 25). Recently, a member of a new class of drugs has been promoted for influenza treatment, the polymerase inhibitor baloxavir (26), which is now approved in the United States. Oseltamivir alone is active against the 1918 virus and would be highly beneficial to reduce morbidity and mortality during a pandemic, even with a highly pathogenic virus such as the 1918 influenza virus as the causal agent. However, combination treatment with oseltamivir and baloxavir might be more beneficial given the fact that for each drug, viruses with reduced sensitivity have been reported.
MATERIALS AND METHODS
Animal ethics and biosafety statement.
All infectious procedures using the 1918 influenza virus were performed in the biosafety level 4 (BSL4) facility of the National Microbiology Laboratory of the Public Health Agency of Canada, applying standard operating protocols approved by the Institutional Biosafety Committee. All nonhuman primate work was performed under a protocol approved by the Institutional Animal Care Committee, according to the guidelines of the Canadian Council on Animal Care. Animal procedures were carried out under anesthesia administered by trained personnel under the supervision of veterinary staff, and all efforts were made to promote the welfare of and to minimize the suffering of the animals in accordance with the recommendations provided by the “Weatherall report for the use of nonhuman primates in reasearch.” Cynomolgus macaques were housed in adjoining individual primate cages allowing social interactions, under controlled conditions of humidity, temperature, and light (12-h light/12-h dark cycles). Food and water were available ad libitum. Animals were monitored at least twice daily and fed commercial monkey chow, treats, and fruit twice daily by trained personnel. Environmental enrichment consisted of commercial toys, videos, and music. Humane endpoint criteria, specified and approved by the Institutional Animal Care and Use Committee, were applied to determine when animals should be humanely euthanized.
Virus and drug.
The 1918 influenza virus was reconstructed using reverse genetics and propagated in MDCK cells as described previously (6). The neuraminidase inhibitor oseltamivir phosphate was obtained in the commercially available capsule form provided for human use.
Treatment experiment.
Ten female cynomolgus macaques (Macaca fascicularis), 13 to 19 years old, weighing 4.3 to 8.0 kg, were confirmed to be seronegative against current H1N1 and H3N2 influenza reference viruses by hemagglutination inhibition assay. Animals were infected with the 1918 influenza virus through a combination of intratracheal (4 ml), intranasal (0.5 ml per nostril), intraocular (0.5 ml per eye), and oral (1 ml) routes with 1 × 106 PFU ml−1 (total dose, 7 × 106 PFU). For treatment, animals were randomly divided into three groups. Two groups (n = 4) were treated daily for 5 consecutive days with 150 mg oseltamivir phosphate starting either 24 h prior or 24 h postinfection. The third group (n = 2) served as a control and was treated with PBS. Animals were monitored twice or more daily for clinical signs using an approved scoring sheet. Before infection (day −8 and day 0) and on dpi 2, 4, 6, 8, 10, and 14 as well as prior to euthanasia, blood and swabs (oral, nasal, throat, and rectal) were collected from anaesthetized animals and vital signs (e.g., pulse rate, blood pressure, temperature, respiration rate, and blood oxygen saturation as measured by pulse oximetry) were recorded. Necropsies were performed on all euthanized animals, focusing on the respiratory tract (lungs, bronchi, trachea, oropharynx, mediastinal lymph nodes, and nasal mucosa) and selected other organs (liver, spleen, kidney, and heart).
Virus titration.
Virus titration was done by plaque forming unit (PFU) assay or tissue culture infectious dose (TCID) assay to identify the dilution required to infect 50% of replicate cultures (TCID50). Virus stock titers were determined in 10-fold serial dilutions by standard PFU assay on Madin-Darby canine kidney (MDCK) cells in the presence of 1 μg/ml tosyl phenylalanyl chloromethyl ketone (TPCK)-treated trypsin, in duplicate for each dilution. A TCID50 assay was used for titration of virus in clinical specimens (tissues, blood, and swabs). Tissues were harvested during necropsies and homogenized in tissue culture medium (minimal essential medium [MEM]–0.1% bovine serum albumin [BSA]) (10% [wt/vol]) using a bead mill tissue homogenizer (Tissuelyzer; Qiagen), and debris was subsequently removed by centrifugation (2,000 × g, 5 min). Whole blood was used directly for titration. Swabs (oral, throat, nasal, and rectal) were collected with cotton swabs and placed into DMEM, and debris was pelleted by centrifugation (2,000 × g, 5 min) prior to titration. Virus titers were determined in 10-fold serial dilutions of supernatant by TCID50 assay performed on MDCK cells at 48 h postinfection in quadruple for each dilution.
Determination of virus in tissue and swabs by RT-PCR.
Tissue samples from necropsies were placed in RNAlater (Ambion) for subsequent extraction of total RNA (Qiagen RNeasy kit). Similarly, RNA was extracted from swab suspensions (Qiagen viral RNA minikit). Viral RNA was detected by reverse transcription-PCR (RT-PCR) (Quantitec Probe RT-PCR kit) using primers and probes (sequences available upon request) targeting the M and HA genes.
Histopathology.
Tissues taken during necropsies were fixed in 10% phosphate-buffered formalin (>1:10 [wt/vol]) for a minimum of 30 days prior to removal from BSL4 containment. Fixed tissues were dehydrated, embedded in paraffin, cut into 5-μm-thick sections and stained with standard hematoxylin and eosin. For viral antigen, sections were processed for immunostaining by the two-step dextran polymer method (Dako) with an antibody to the viral nucleoprotein (NP).
Detection of drug-resistant viral mutants.
To analyze tissue for the presence of drug-resistant viruses, the tissue lysates from the nasal mucosa and the right lung (lower lobe) was plated on MDCK cells in a standard PFU assay as described above. Twenty individual plaques from each tissue were grown on MDCK cells as previously described (6). Viral RNA was isolated from the supernatants of each virus culture (Qiagen Viral RNA minikit) and cDNA generated by reverse transcription using primer uni12 (5′-AGCGAAAGCAGG-3′). The full sequences of the HA and NA genes of all viruses were determined following PCR amplification using gene-specific universal primers as previously described (27). Analysis for mutations in the HA and NA of other tissues and swabs was done for tissues previously shown to contain virus by RT-PCR or virus isolation. The full open reading frame for the HA and NA genes was amplified by RT-PCR (Qiagen OneStep RT-PCR kit) using HA-specific primers (Sp-HA-1F [5′-ACAACCAAAATGGAGGCAAGAC-3′] and Sp-HA-1742R [5′-ATCCTAATCTCAAATGCATATTCT-3′]) and NA-specific primers (Sp-NA-1F [5′-AAGCAGGAGTTTAAATGAATCCA-3′] and Sp-NA-1433R [5′-CAAACTACTTGTCAATG-3′]). Each PCR product was subsequently ligated into PCR cloning vector pCR2.1 (Invitrogen TOPO TA cloning kit), and 2 to 6 individual clones for each gene from each tissue were sequenced to identify mutations associated with drug resistance.
Analysis of contribution of NA mutation His275Tyr to resistance to NA inhibitors.
Plasmids for the expression of the 1918 influenza wild-type NA gene were constructed as described previously (6); subsequently, the His275Tyr mutation was introduced into the plasmid. Recombinant influenza viruses based on the background of A/WSN/33 (H1N1) carrying only the 1918 influenza virus wild-type NA or the His275Tyr mutant were then generated by reverse genetics as described previously (28), propagated in MDCK cells twice, and stored at –80°C as stock viruses. All constructed plasmids were sequenced to ensure the absence of unwanted mutations. The sensitivity of NA to the NA inhibitors was evaluated by use of an NA activity inhibition assay based on the method of Gubareva et al. (29). Methylumbelliferyl-N-acetylneuraminic acid (MUNANA; Sigma) was used as a fluorescent substrate at a final concentration of 0.1 mM. Virus dilutions containing 800 to 1,200 fluorescence units were mixed with test compound (0.01 nM to 1 mM) and 33 mM 2-[N-morpholino]ethanesulfonic acid (pH 6.0) containing 4 mM CaCl2 and were incubated for 30 min at 37°C. After addition of the substrate and incubation at 37°C for 1 h, the reaction was stopped by the addition of 0.1 M NaOH–80% ethanol (pH 10.0). Fluorescence was measured at an excitation wavelength of 360 nm and an emission wavelength of 465 nm. The relationship between the concentration of inhibitor and the percentage of fluorescence inhibition was determined, and 50% inhibitory concentration (IC50) values were obtained by extrapolating those findings.
Data availability.
The data supporting the findings of this study are available within the paper and the supplemental material or from the corresponding authors upon request.
ACKNOWLEDGMENTS
We thank John Copps and John Pasick (both National Centre for Foreign Animal Diseases, Canadian Food Inspection Agency, Winnipeg, Canada) and Jocelyn Fournier (Non-Human Primate Colony, Animal Resources, Health Canada) for veterinary support and Nicole Beausoleil (National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, Canada) for animal care support.
The study was financially supported by the Public Health Agency of Canada and by Leading Advanced Projects for Medical Innovation (LEAP) of the Japan Agency for Medical Research and Development (AMED) (JP18am001007), by a Grant-in-Aid for Scientific Research on Innovative Areas from the Ministry of Education, Culture, Science, Sports, and Technology (MEXT) of Japan (16H06429, 16K21723, and 16H06434), by the Japan Initiative for Global Research Network on Infectious Diseases (J-GRID) of AMED (JP18fm0108006), and by the Research Program on Emerging and Re-emerging Infectious Diseases of AMED (JP18fk0108104). F.F. and H.F. are currently supported by the Intramural Research Program of NIAID, NIH.
No U.S. Government funds were used in the performance of the work described in this publication. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication. All work was performed in appropriate biocontainment settings under approved biosafety conditions. The institutional Dual Use Research of Concern (DURC) Committees of the NIAID, NIH, and of the University of Wisconsin—Madison, the current locations of the corresponding authors, have reviewed this material. This research can be considered dual use in nature and should be performed only under appropriate risk management conditions with appropriate institutional approvals.
Y.K. has received grant support from Daiichi Sankyo Pharmaceutical, Toyama Chemical, Tauns Laboratories, Inc., Denka Seiken Co. Ltd., and Ttsumura and Co.; has received royalties from MedImmune; and is a founder of FluGen.
Footnotes
Citation Feldmann F, Kobasa D, Embury-Hyatt C, Grolla A, Taylor T, Kiso M, Kakugawa S, Gren J, Jones SM, Kawaoka Y, Feldmann H. 2019. Oseltamivir is effective against 1918 influenza virus infection of macaques but vulnerable to escape. mBio 10:e02059-19. https://doi.org/10.1128/mBio.02059-19.
REFERENCES
- 1.Taubenberger JK, Reid AH, Lourens RM, Wang R, Jin G, Fanning TG. 2005. Characterization of the 1918 influenza virus polymerase genes. Nature 437:889–893. doi: 10.1038/nature04230. [DOI] [PubMed] [Google Scholar]
- 2.Taubenberger JK, Hultin JV, Morens DM. 2007. Discovery and characterization of the 1918 pandemic influenza virus in historical context. Antivir Ther 12:581–591. [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed R, Oldstone M, Palese P. 2007. Protective immunity and susceptibility to infectious diseases: lessons from the 1918 influenza pandemic. Nat Immunol 8:1188–1193. doi: 10.1038/ni1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taubenberger JK, Morens DM. 2006. The 1918 influenza: the mother of all pandemics. Emerg Infect Dis 12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tumpey TM, Basler CF, Aguilar PV, Zeng H, Solórzano A, Swayne DE, Cox NJ, Katz JM, Taubenberger JK, Palese P, García-Sastre A. 2005. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 6.Kobasa D, Jones SM, Shinya K, Kash JC, Copps J, Ebihara H, Hatta Y, Kim JH, Halfmann P, Hatta M, Feldmann F, Alimonti JB, Fernando L, Li Y, Katze MG, Feldmann H, Kawaoka Y. 2007. Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature 445:319–323. doi: 10.1038/nature05495. [DOI] [PubMed] [Google Scholar]
- 7.Tumpey TM, García-Sastre A, Mikulasova A, Taubenberger JK, Swayne DE, Palese P, Basler CF. 2002. Existing antivirals are effective against influenza viruses with genes from the 1918 pandemic virus. Proc Natl Acad Sci U S A 99:13849–13854. doi: 10.1073/pnas.212519699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solórzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, García-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 9.Kobasa D, Takada A, Shinya K, Hatta M, Halfmann P, Theriault S, Suzuki H, Nishimura H, Mitamura K, Sugaya N, Usui T, Murata T, Maeda Y, Watanabe S, Suresh M, Suzuki T, Suzuki Y, Feldmann H, Kawaoka Y. 2004. Enhanced virulence of influenza A viruses with the haemagglutinin of the 1918 pandemic virus. Nature 431:703–707. doi: 10.1038/nature02951. [DOI] [PubMed] [Google Scholar]
- 10.Kash JC, Tumpey TM, Proll SC, Carter V, Perwitasari O, Thomas MJ, Basler CF, Palese P, Taubenberger JK, García-Sastre A, Swayne DE, Katze MG. 2006. Genomic analysis of increased host immune and cell death responses induced by 1918 influenza virus. Nature 443:578–581. doi: 10.1038/nature05181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fraser C, Donnelly CA, Cauchemez S, Hanage WP, Van Kerkhove MD, Hollingsworth TD, Griffin J, Baggaley RF, Jenkins HE, Lyons EJ, Jombart T, Hinsley WR, Grassly NC, Balloux F, Ghani AC, Ferguson NM, Rambaut A, Pybus OG, Lopez-Gatell H, Alpuche-Aranda CM, Chapela IB, Zavala EP, Guevara DM, Checchi F, Garcia E, Hugonnet S, Roth C, WHO Rapid Pandemic Assessment Collaboration. 2009. Pandemic potential of a strain of influenza A (H1N1): early findings. Science 324:1557–1561. doi: 10.1126/science.1176062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, Sessions WM, Xu X, Skepner E, Deyde V, Okomo-Adhiambo M, Gubareva L, Barnes J, Smith CB, Emery SL, Hillman MJ, Rivailler P, Smagala J, de Graaf M, Burke DF, Fouchier RA, Pappas C, Alpuche-Aranda CM, López-Gatell H, Olivera H, López I, Myers CA, Faix D, Blair PJ, Yu C, Keene KM, Dotson PD Jr, Boxrud D, Sambol AR, Abid SH, St George K, Bannerman T, Moore AL, Stringer DJ, Blevins P, Demmler-Harrison GJ, Ginsberg M, Kriner P, Waterman S, Smole S, Guevara HF, Belongia EA, Clark PA, Beatrice ST, et al. 2009. Antigenic and genetic characteristics of swine-origin 2009 A (H1N1) influenza viruses circulating in humans. Science 325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schünemann HJ, Hill SR, Kakad M, Bellamy R, Uyeki TM, Hayden FG, Yazdanpanah Y, Beigel J, Chotpitayasunondh T, Del Mar C, Farrar J, Tran TH, Ozbay B, Sugaya N, Fukuda K, Shindo N, Stockman L, Vist GE, Croisier A, Nagjdaliyev A, Roth C, Thomson G, Zucker H, Oxman AD, WHO Rapid Advice Guideline Panel on Avian Influenza. 2007. WHO rapid advice guidelines for pharmacological management of sporadic human infection with avian influenza A (H5N1) virus. Lancet Infect Dis 7:21–31. doi: 10.1016/S1473-3099(06)70684-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gubareva LV, Kaiser L, Matrosovich MN, Soo-Hoo Y, Hayden FG. 2001. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J Infect Dis 183:523–531. doi: 10.1086/318537. [DOI] [PubMed] [Google Scholar]
- 15.Rogers GN, Paulson JC. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127:361–373. doi: 10.1016/0042-6822(83)90150-2. [DOI] [PubMed] [Google Scholar]
- 16.Wagner R, Matrosovich M, Klenk HD. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol 12:159–166. doi: 10.1002/rmv.352. [DOI] [PubMed] [Google Scholar]
- 17.Xu X, Rocha EP, Regenery HL, Kendal AP, Cox NJ. 1993. Genetic and antigenic analyses of influenza A (H1N1) viruses, 1986–1991. Virus Res 28:37–55. doi: 10.1016/0168-1702(93)90088-5. [DOI] [PubMed] [Google Scholar]
- 18.Takemae N, Ruttanapumma R, Parchariyanon S, Yoneyama S, Hayashi T, Hiramatsu H, Sriwilaijaroen N, Uchida Y, Kondo S, Yagi H, Kato K, Suzuki Y, Saito T. 2010. Alterations in receptor-binding properties of swine influenza viruses of the H1 subtype after isolation in embryonated chicken eggs. J Gen Virol 91:938–948. doi: 10.1099/vir.0.016691-0. [DOI] [PubMed] [Google Scholar]
- 19.Gubareva LV. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res 103:199–203. doi: 10.1016/j.virusres.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 20.Anonymous. 2009. Pandemic alert level 6: sustained community transmission of influenza A (H1N1) virus in two different WHO regions. Eurosurveillance 14:19237 https://www.eurosurveillance.org/content/10.2807/ese.14.23.19237-en.19531339 [Google Scholar]
- 21.Sutton TC. 2018. The pandemic threat of emerging H5 and H7 avian influenza viruses. Viruses 10:E461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Shen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao X, Zhou L, Li X, Zou S, Zhang Y, Li X, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Zhang Y, Han J, Yu H, Li D, Gao GF, Wu G, Wang Y, Yuan Z, Shu Y. 2013. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 368:1888–1897. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 23.Zhou L, Ren R, Yang L, Bao C, Wu J, Wang D, Li C, Xiang N, Wang Y, Li D, Sui H, Shu Y, Feng Z, Li Q, Ni D. 2017. Sudden increase in human infection with avian influenza A(H7N9) virus in China, September-December 2016. Western Pac Surveill Response J 8:6–9. doi: 10.5365/WPSAR.2017.8.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Homeyer N, Ioannidis H, Kolarov F, Gauglitz G, Zikos C, Kolocouris A, Gohlke H. 2016. Interpreting thermodynamic profiles of aminoadamantane compounds inhibiting the M2 proton channel of influenza A by free energy calculations. J Chem Inf Model 56:110–126. doi: 10.1021/acs.jcim.5b00467. [DOI] [PubMed] [Google Scholar]
- 25.Jackson RJ, Cooper KL, Tappenden P, Rees A, Simpson EL, Read RC, Nicholson KG. 2011. Oseltamivir, zanamivir and amantadine in the prevention of influenza: a systematic review. J Infect 62:14–25. doi: 10.1016/j.jinf.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Hayden FG, Sugaya N, Hirotsu N, Lee N, de Jong MD, Hurt AC, Ishida T, Sekino H, Yamada K, Portsmouth S, Kawaguchi K, Shishido T, Arai M, Tsuchiya K, Uehara T, Watanabe A, Baloxavir Marboxil Investigators Group. 2018. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med 379:913–923. doi: 10.1056/NEJMoa1716197. [DOI] [PubMed] [Google Scholar]
- 27.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol 146:2275–2289. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- 28.Neumann G, Watanabe T, Ito H, Watanabe S, Goto H, Gao P, Hughes M, Perez DR, Donis R, Hoffmann E, Hobom G, Kawaoka Y. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci U S A 96:9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gubareva LV, Webster RG, Hayden FG. 2001. Comparison of the activities of zanamivir, oseltamivir, and RWJ-270201 against clinical isolates of influenza virus and neuraminidase inhibitor-resistant variants. Antimicrob Agents Chemother 45:3403–3408. doi: 10.1128/AAC.45.12.3403-3408.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Clinical presentation of animals. Download Table S1, DOCX file, 0.01 MB (9.6KB, docx) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Virus titers in tissues at time of euthanasia. Download Table S2, DOCX file, 0.01 MB (9.6KB, docx) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Data Availability Statement
The data supporting the findings of this study are available within the paper and the supplemental material or from the corresponding authors upon request.