Abstract
Background
Characterizing and assessing the prevalence, awareness, and treatment patterns of patients with isolated diastolic hypertension (IDH) can generate new knowledge and highlight opportunities to improve their care.
Methods and Results
We used data from the China PEACE (Patient‐centered Evaluative Assessment of Cardiac Events) Million Persons Project, which screened 2 351 035 participants aged 35 to 75 years between 2014 and 2018. IDH was defined as systolic and diastolic blood pressure of <140 and ≥90 mm Hg; awareness as self‐reported diagnosis of hypertension; and treatment as current use of antihypertensive medications. Of the 2 310 184 participants included (mean age 55.7 years; 59.5% women); 73 279 (3.2%) had IDH, of whom 63 112 (86.1%) were untreated, and only 6512 (10.3%) of the untreated were aware of having hypertension. When compared with normotensives, participants who were <60 years, men, at least college educated, had body mass index of >28 kg/m2, consumed alcohol, had diabetes mellitus, and prior cardiovascular events were more likely to have IDH (all P<0.01). Among those with IDH, higher likelihood of awareness was associated with increased age, women, college education, body mass index of >28 kg/m2, higher income, diabetes mellitus, prior cardiovascular events, and Central or Eastern region (all P<0.05). Most treated participants with IDH reported taking only 1 class of antihypertensive medication.
Conclusions
IDH affects a substantial number of people in China, however, few are aware of having hypertension and most treated participants are poorly managed, which suggests the need to improve the diagnosis and treatment of people with IDH.
Keywords: awareness, hypertension subtypes, isolated diastolic hypertension, prevalence, treatment
Subject Categories: Hypertension, Epidemiology, Cardiovascular Disease
Clinical Perspective
What Is New?
This is one of the largest population‐based studies to evaluate the characteristics, prevalence, awareness, and treatment patterns of individuals with isolated diastolic hypertension (IDH) in China, allowing us to draw robust conclusions across diverse subgroups.
We found that IDH affected a large number of adults in China, and these patients had some unique characteristics as compared with people without hypertension as well as those with other types of hypertension.
Awareness of hypertension was significantly lower among people with IDH as compared with other types of hypertension, and most participants with IDH despite treatment had scope for further intensification of therapy.
What Are the Clinical Implications?
Given that diastolic hypertension can independently influence the risk of adverse cardiovascular events, identifying characteristics that may be associated with IDH and understanding the current awareness and treatment patterns among those with IDH can help identify the patients at increased cardiovascular risk and highlight opportunities to improve their care.
Focusing on people with IDH and improving their diagnosis and treatment, may be critical to mitigate the burden of hypertension, especially in the young‐ and middle‐aged population.
Introduction
Isolated diastolic hypertension (IDH), whether in treated or untreated patients, is an uncommon type of hypertension accounting for <20% of hypertension cases.1, 2, 3, 4 Nevertheless, IDH is independently associated with an increased risk of stroke, heart disease, and the other sequelae of hypertension.5, 6, 7, 8, 9, 10, 11, 12, 13, 14 However, the most recent US, Chinese, and European high blood pressure guidelines do not specifically address IDH as a distinct phenotype or provide any specific guidance for its management.15, 16, 17
Although many studies have focused on patient characteristics, knowledge, and treatment, patients with IDH constitute a small subset of all patients with hypertension, and have traditionally been included within the total population of hypertensive patients,1, 18, 19, 20 even though they may have unique features.20, 21 Given its low prevalence, a large sample size would be required to fully capture the range of attributes of individuals with IDH across diverse population subgroups, and draw robust conclusions with high precision. Characterizing these patients specifically and assessing their awareness and treatment patterns can generate new knowledge about this distinct subtype of hypertension. This information will not only expand our knowledge about the IDH phenotype, but could also equip us to identify targets for improvement of care.
Accordingly, we sought to identify and study patients with IDH, whether treated or untreated, using data from the China PEACE (Patient‐centered Evaluative Assessment of Cardiac Events) Million Persons Project, a large‐scale population‐based screening project which was initiated with the aim of providing detailed information on smaller subgroups of patients who have traditionally been hard to identify in the population. We sought to describe the characteristics and prevalence of individuals with IDH across diverse population subgroups among both untreated and treated hypertensives; assess awareness of having hypertension among untreated IDH participants; assess the number and classes of medications used by treated participants with IDH; and identify the associations between individual characteristics with prevalence of, and awareness among those with IDH. Although some of the treated patients may be individuals who initially had systolic and diastolic hypertension, but with medications have only diastolic hypertension, this does represent the spectrum of patients who would be seen in practice with IDH, either as a de novo condition or as inadequately treated diastolic hypertension. Moreover, the treatment rates in China are sufficiently low that the population with IDH largely represents those with the de novo condition.
Methods
The China PEACE Million Persons Project is a major national program, and as the government policy stipulates, it is not permissible for the researchers to make the raw data publicly available at this time.
Study Design and Population
Details of the China PEACE Million Persons Project have been described previously.22, 23 Briefly, we used a convenience sampling strategy to select 184 sites (111 rural counties and 73 urban districts) from all 31 provinces in mainland China. People were encouraged to participate in the project through publicity campaigns in the newspaper and on the television. Of the 2 351 035 participants aged 35 to 75 years enrolled at these sites between September 15, 2014 and May 29, 2018, we excluded 14 904 participants because of missing or extreme blood pressure values (systolic blood pressure [SBP] <70 or >270 mm Hg; diastolic blood pressure [DBP] <30 or >150 mm Hg), 142 participants due to missing or extreme body mass index values (<10 or >50 kg/m2), and 25 805 participants due to missing data on covariates, including geographical region, education, occupation, marital status, household income, and alcohol use (Figure S1).
Blood Pressure Collection and Classification
For every participant, blood pressure was measured twice at enrollment, at an interval of 1 minute, on their right upper arm using an electronic blood pressure monitor (Omron HEM‐7430; Omron Corporation, Kyoto, Japan) after 5 minutes of rest in the seated position. The values of both the readings as well as their mean were recorded. If the difference between the 2 SBP measurements was >10 mm Hg, a third blood pressure reading was taken and the mean SBP and DBP was calculated using the last 2 readings in such cases. The mean SBP and DBP were used for all calculations. Additionally, information was collected on any prescription drugs taken by the participants in the past 2 weeks for antiplatelet, blood pressure, lipid, or glucose control during an in‐person interview.
Since this study was done in a Chinese cohort, we used the Chinese Guidelines for the Management of Hypertension to define hypertension and classify patients with hypertension into different hypertension subtypes.15 Participants were considered to have hypertension if they had an average SBP of at least 140 mm Hg or an average DBP of at least 90 mm Hg or self‐reported use of an antihypertensive medication in the past 2 weeks. IDH was defined as an average SBP of <140 mm Hg but a DBP of at least 90 mm Hg. We defined IDH based on the participant's SBP and DBP at the time of screening, and the IDH group included both untreated IDH participants and those with IDH despite antihypertensive medication. The “other hypertensive subtypes” group included all hypertensives, except those with IDH, including participants with isolated systolic hypertension (ISH; SBP ≥140 mm Hg and DBP <90 mm Hg), combined systolic‐diastolic hypertension (SDH; SBP ≥140 mm Hg and DBP ≥90 mm Hg), and controlled hypertensives (participants who reported having a history of hypertension or taking antihypertensive medications but had an SBP <140 mm Hg and a DBP <90 mm Hg). Participants who did not have a history of hypertension or antihypertensive medication use and who had an SBP <140 mm Hg and a DBP <90 mm Hg were defined as normotensives.
Participants were considered to be aware of their hypertension if they responded “yes” to the question “Have you ever been diagnosed with hypertension?”. Participants were considered to be receiving treatment for hypertension if they reported using antihypertensive medication (Western or traditional Chinese medication) currently or within the last 2 weeks.
Independent Variables
Information on the participants’ sociodemographic characteristics, health behaviors, medical history, and cardiovascular risk factors was recorded during in‐person interviews as described previously.22 Height and weight were collected using standard protocols, and body mass index (BMI) was calculated by dividing the weight in kilograms by the square of height in meters. Obesity was defined as a BMI of at least 28 kg/m2, which was in accordance with the recommendations of the Working Group on Obesity in China.24
We also formed diverse, mutually exclusive subgroups, to assess if some population subgroups had higher or lower rates of prevalence and awareness compared with the average rates of the total population. These subgroups were defined a priori by all possible combinations of 10 characteristics: age group (35–44, 45–54, 55–64, and 65–75 years), sex (men, women), geographic region (Western, Central, Eastern), urbanity (urban, rural), occupation (farmer, non‐farmer), annual household income (<10 000, 10 000–50 000, and >50 000 Yuan/year), education (primary school and below, middle school, high school, college and above), prior cardiovascular events (myocardial infarction or stroke; yes versus no), current smoker (yes versus no), and diabetes mellitus (yes versus no).
Statistical Analysis
We assessed the prevalence of IDH among the overall study population and among hypertensive participants (both overall and among untreated and treated hypertensives) and compared the prevalence of IDH with other hypertension subtypes across different age groups. We also calculated age‐ and sex‐standardized prevalence of IDH at the national level, standardizing against data from all 31 provinces in the 2010 Chinese Census. We then described the characteristics of participants with IDH and compared these with normotensive as well as with other hypertensive subgroups, and described the characteristics of untreated and treated participants with IDH separately. Next, we assessed the awareness of hypertension among untreated IDH participants across different population characteristics; and compared the awareness rates of untreated IDH participants with those of untreated ISH and SDH participants across different age groups. We assessed awareness only among untreated IDH participants as some treated participants with IDH may have adequately lowered their DBP and moved to the controlled hypertensive group, thus underestimating awareness rates among those having IDH despite treatment. The statistical significance of the differences between groups was assessed using Pearson Chi‐squared test.
We retained 1198 mutually exclusive subgroups of at least 200 participants each, which included 84.1% of the participants with IDH, and calculated the prevalence of IDH among all study participants and the awareness rates among untreated IDH participants. We also used histograms to show the rate distributions, and repeated the analysis by restricting to 731 subgroups containing at least 500 participants each (which included 77.6% of the participants with IDH).
Among participants who had IDH despite treatment, we assessed the number and class of medications reported by them. Medication usage was divided into 6 medication classes defined by the 2010 Chinese guidelines for the management of hypertension15 and included angiotensin‐converting enzyme inhibitors or angiotensin receptor blockers, beta‐blockers, calcium channel blockers, diuretics, and fixed‐dose combination drugs. We also collected information on the traditional Chinese medications (TCMs) used for hypertension. To assess whether the management of IDH patients varied by severity, we stratified them into 3 groups based on the degree DBP elevation (90–95, 96–100, and >100 mm Hg) and compared the most frequently used antihypertensive medication class and the number of antihypertensive medications used by patients in each of these groups.
Finally, we developed 2 multivariable generalized linear mixed models with a logit link function and township‐specific random intercepts (to account for geographic autocorrelation) to identify individual characteristics associated with prevalence of IDH, and the awareness of hypertension among untreated IDH participants (details in Data S1). For identifying the characteristics associated with IDH, we compared IDH participants with both normotensives as well as other hypertensives using 2 separate models. Explanatory variables included participants’ age, sex, marital status, annual household income, education level, occupation, geographical region, health insurance status, smoking, alcohol use, obesity, physician‐diagnosed diabetes mellitus (DM), and prior cardiovascular events (myocardial infarction or stroke).
All analyses were conducted using R 3.33 (The R Foundation for Statistical Computing, Vienna, Austria) and SAS 9.4 (SAS Institute Inc, Cary, NC). The central ethics committee at the China National Center for Cardiovascular Disease and the Internal Review Board at Yale University approved this project, and written informed consent was obtained from all enrolled participants.
Results
Population Characteristics
Our sample included 2 310 184 participants with a mean age of 55.7 (SD 9.8) years; 1 374 684 (59.5%) were women; and 1 023 780 (44.3%) had hypertension. Compared with the population aged 35 to 75 years in the 2010 Chinese Census, our sample contained more people from older age groups (70.4% of people with age 50 and older in the Million Persons Project versus 46.1% in Census).
Prevalence and Characteristics of Participants With IDH
Overall, 73 279 (3.2% of the study population and 7.2% of hypertensives) participants had IDH and 950 501 (41.1% of the study population) participants had other types of hypertension (including, 469 349 [20.3%] with ISH, 403 912 [17.5%] with SDH, and 77 240 [3.3%] with controlled hypertension). When we standardized our results to national census‐based estimates, we found a higher prevalence of IDH (3.8%) but a lower prevalence of other hypertension subgroups (34.0%). Overall, participants with IDH were more likely to be younger, men, employed, married, more educated, have higher income, consume alcohol, be current smoker, and obese than those who were normotensive or who had other types of hypertension (all P<0.001; Table 1). Additionally, participants with IDH were more likely to have a history of myocardial infarction, stroke, and DM (0.7%, 2.2%, and 4.8% respectively) when compared with normotensive participants (0.5%, 1.2%, and 4.0% respectively), and less likely to have a history of myocardial infarction, stroke, and DM compared with participants with other types of hypertension (1.1%, 4.1%, and 9.8% respectively). Both untreated and treated IDH participants had similar characteristics (Table S1).
Table 1.
Baseline Characteristics of Participants With Isolated Diastolic Hypertension Compared With Normotensives and Other Hypertensives
| Characteristics, n (%) | Normotensives | Isolated Diastolic Hypertension | Other Hypertensives |
|---|---|---|---|
| n (%) | 1 286 404 (55.7%) | 73 279 (3.2%) | 950 501 (41.1%) |
| Age, y | |||
| 35 to 39 | 91 686 (7.1%) | 4603 (6.3%) | 14 056 (1.5%) |
| 40 to 44 | 181 177 (14.1%) | 10 538 (14.4%) | 45 006 (4.7%) |
| 45 to 49 | 229 912 (17.9%) | 15 328 (20.9%) | 91 801 (9.7%) |
| 50 to 54 | 235 412 (18.3%) | 16 479 (22.5%) | 149 641 (15.7%) |
| 55 to 59 | 170 190 (13.2%) | 10 082 (13.8%) | 147 992 (15.6%) |
| 60 to 64 | 182 963 (14.2%) | 8910 (12.2%) | 205 833 (21.7%) |
| 65 to 69 | 123 906 (9.6%) | 4985 (6.8%) | 176 376 (18.6%) |
| 70 to 75 | 71 158 (5.5%) | 2354 (3.2%) | 119 796 (12.6%) |
| Sex | |||
| Men | 501 100 (39.0%) | 42 360 (57.8%) | 392 040 (41.2%) |
| Women | 785 304 (61.0%) | 30 919 (42.2%) | 558 461 (58.8%) |
| Urbanity | |||
| Urban | 517 420 (40.2%) | 26 309 (35.9%) | 345 720 (36.4%) |
| Rural | 768 984 (59.8%) | 46 970 (64.1%) | 604 781 (63.6%) |
| Region | |||
| Eastern | 416 104 (32.3%) | 23 902 (32.6%) | 352 929 (37.1%) |
| Western | 494 433 (38.4%) | 28 156 (38.4%) | 308 351 (32.4%) |
| Central | 375 867 (29.2%) | 21 221 (29.0%) | 289 221 (30.4%) |
| Education | |||
| Primary school or lower | 512 301 (39.8%) | 26 212 (35.8%) | 473 213 (49.8%) |
| Middle school | 432 275 (33.6%) | 25 959 (35.4%) | 288 724 (30.4%) |
| High school | 211 349 (16.4%) | 12 368 (16.9%) | 126 468 (13.3%) |
| College or above | 111 560 (8.7%) | 7602 (10.4%) | 49 895 (5.2%) |
| Unknown* | 18 919 (1.5%) | 1138 (1.6%) | 12 201 (1.3%) |
| Employment | |||
| Employed | 963 858 (74.9%) | 57 582 (78.6%) | 649 247 (68.3%) |
| Unemployed | 17 294 (1.3%) | 1345 (1.8%) | 11 630 (1.2%) |
| Retired | 185 763 (14.4%) | 8342 (11.4%) | 191 626 (20.2%) |
| Housework | 95 722 (7.4%) | 4470 (6.1%) | 83 403 (8.8%) |
| Unknown* | 23 767 (1.8%) | 1540 (2.1%) | 14 595 (1.5%) |
| Occupation | |||
| Farmer | 602 369 (46.8%) | 34 562 (47.2%) | 492 275 (51.8%) |
| Non‐farmer | 660 268 (51.3%) | 37 177 (50.7%) | 443 631 (46.7%) |
| Unknown* | 23 767 (1.8%) | 1540 (2.1%) | 14 595 (1.5%) |
| Household income, Yuan/y | |||
| <10 000 | 256 630 (19.9%) | 14 307 (19.5%) | 216 481 (22.8%) |
| 10 000 to 50 000 | 711 228 (55.3%) | 40 359 (55.1%) | 521 951 (54.9%) |
| >50 000 | 199 441 (15.5%) | 11 908 (16.3%) | 128 457 (13.5%) |
| Unknown* | 119 105 (9.3%) | 6705 (9.1%) | 83 612 (8.8%) |
| Marital status | |||
| Married | 1 208 737 (94.0%) | 69 159 (94.4%) | 869 211 (91.4%) |
| Widowed, separated, divorced, single | 61 396 (4.8%) | 3192 (4.4%) | 70 389 (7.4%) |
| Unknown* | 16 271 (1.3%) | 928 (1.3%) | 10 901 (1.1%) |
| Health insurance status | |||
| Insured | 1 258 190 (97.8%) | 71 580 (97.7%) | 932 199 (98.1%) |
| Uninsured | 8388 (0.7%) | 502 (0.7%) | 4890 (0.5%) |
| Unknown* | 19 826 (1.5%) | 1197 (1.6%) | 13 412 (1.4%) |
| Medical history | |||
| Myocardial infarction | 6281 (0.5%) | 496 (0.7%) | 10 447 (1.1%) |
| Stroke | 15 628 (1.2%) | 1614 (2.2%) | 38 626 (4.1%) |
| Diabetes mellitus | 51 410 (4.0%) | 3499 (4.8%) | 93 329 (9.8%) |
| Cardiovascular disease risk factor | |||
| Current smoker | 249 422 (19.4%) | 20 667 (28.2%) | 185 778 (19.5%) |
| Current drinker | 292 489 (22.7%) | 26 529 (36.2%) | 240 183 (25.3%) |
| Obesity | 134 244 (10.4%) | 17 241 (23.5%) | 214 058 (22.5%) |
P‐value <0.001 for all comparisons among the 3 groups.
Participants either refused to answer the question or did not know the answer.
The prevalence of IDH decreased with age, whereas the prevalence of other hypertension subtypes (including ISH, SDH and controlled hypertensives) increased with age (Figure 1). The prevalence of IDH was significantly higher for men (4.5% of overall population and 9.8% of hypertensives) as compared with women (2.2% of overall population and 5.2% of hypertensives; Table 2). The prevalence was also significantly higher among those living in rural areas and Western regions, who were at least college educated, and had a higher income (Table 2). Prevalence of IDH showed a similar distribution across different population subgroups in both treated and untreated hypertensive participants (Table 3 and Table S2).
Figure 1.
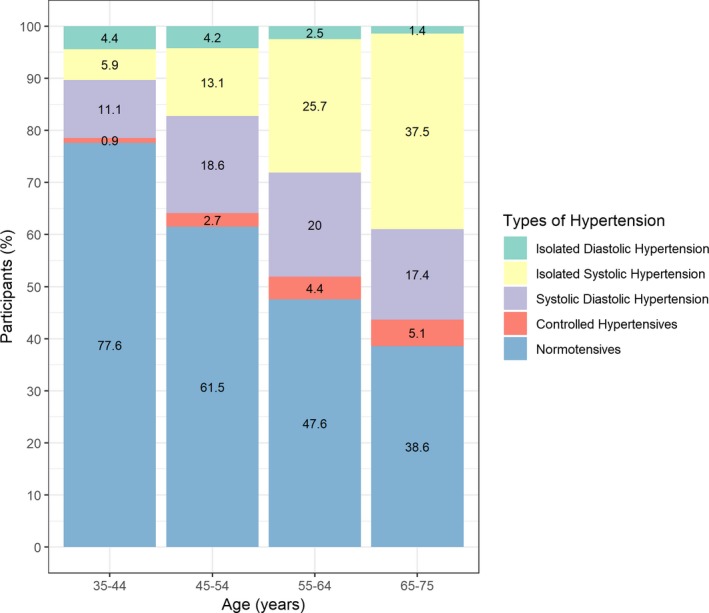
Prevalence of isolated diastolic hypertension and other types of hypertension (isolated systolic hypertension, systolic‐diastolic hypertension, and controlled hypertension), by age group.
Table 2.
Prevalence of Isolated Diastolic Hypertension Among All Participants and Hypertensive Participants, by Population Characteristics
| Characteristics | All Participants | Hypertensive Participants | ||
|---|---|---|---|---|
| n | Prevalence of IDH n (%, 95% CI) | n | Prevalence of IDH n (%, 95% CI) | |
| n (%, 95% CI) | 2 310 184 | 73 279 (3.2%, 3.1–3.2) | 1 023 780 | 73 279 (7.2%, 7.1–7.2) |
| Age, y | ||||
| 35 to 39 | 110 345 | 4603 (4.2%, 4.1–4.3) | 18 659 | 4603 (24.7%, 24.1–25.3) |
| 40 to 44 | 236 721 | 10 538 (4.5%, 4.4–4.5) | 55 544 | 10 538 (19.0%, 18.6–19.3) |
| 45 to 49 | 337 041 | 15 328 (4.5%, 4.5–4.6) | 107 129 | 15 328 (14.3%, 14.1–14.5) |
| 50 to 54 | 401 532 | 16 479 (4.1%, 4.0–4.2) | 166 120 | 16 479 (9.9%, 9.8–10.1) |
| 55 to 59 | 328 264 | 10 082 (3.1%, 3.0–3.1) | 158 074 | 10 082 (6.4%, 6.3–6.5) |
| 60 to 64 | 397 706 | 8910 (2.2%, 2.2–2.3) | 214 743 | 8910 (4.1%, 4.1–4.2) |
| 65 to 69 | 305 267 | 4985 (1.6%, 1.6–1.7) | 181 361 | 4985 (2.7%, 2.7–2.8) |
| 70 to 75 | 193 308 | 2354 (1.2%, 1.2–1.3) | 122 150 | 2354 (1.9%, 1.9–2.0) |
| Sex | ||||
| Men | 935 500 | 42 360 (4.5%, 4.5–4.6) | 434 400 | 42 360 (9.8%, 9.7–9.8) |
| Women | 1 374 684 | 30 919 (2.2%, 2.2–2.3) | 589 380 | 30 919 (5.2%, 5.2–5.3) |
| Urbanity | ||||
| Urban | 889 449 | 26 309 (3.0%, 2.9–3.0) | 372 029 | 26 309 (7.1%, 7.0–7.2) |
| Rural | 1 420 735 | 46 970 (3.3%, 3.3–3.3) | 651 751 | 46 970 (7.2%, 7.1–7.3) |
| Region | ||||
| Eastern | 792 935 | 23 902 (3.0%, 3.0–3.1) | 376 831 | 23 902 (6.3%, 6.3–6.4) |
| Western | 830 940 | 28 156 (3.4%, 3.3–3.4) | 336 507 | 28 156 (8.4%, 8.3–8.5) |
| Central | 686 309 | 21 221 (3.1%, 3.1–3.1) | 310 442 | 21 221 (6.8%, 6.7–6.9) |
| Education | ||||
| Primary school or lower | 1 011 726 | 26 212 (2.6%, 2.6–2.6) | 499 425 | 26 212 (5.2%, 5.2–5.3) |
| Middle school | 746 958 | 25 959 (3.5%, 3.4–3.5) | 314 683 | 25 959 (8.2%, 8.2–8.3) |
| High school | 350 185 | 12 368 (3.5%, 3.5–3.6) | 138 836 | 12 368 (8.9%, 8.8–9.1) |
| College or above | 169 057 | 7602 (4.5%, 4.4–4.6) | 57 497 | 7602 (13.2%, 12.9–13.5) |
| Unknown* | 32 258 | 1138 (3.5%, 3.3–3.7) | 13 339 | 1138 (8.5%, 8.1–9.0) |
| Employment | ||||
| Employed | 1 670 687 | 57 582 (3.4%, 3.4–3.5) | 706 829 | 57 582 (8.1%, 8.1–8.2) |
| Unemployed | 30 269 | 1345 (4.4%, 4.2–4.7) | 12 975 | 1345 (10.4%, 9.8–10.9) |
| Retired | 385 731 | 8342 (2.2%, 2.1–2.2) | 199 968 | 8342 (4.2%, 4.1–4.3) |
| Housework | 183 595 | 4470 (2.4%, 2.4–2.5) | 87 873 | 4470 (5.1%, 4.9–5.2) |
| Unknown* | 39 902 | 1540 (3.9%, 3.7–4.0) | 16 135 | 1540 (9.5%, 9.1–10.0) |
| Occupation | ||||
| Farmer | 1 129 206 | 34 562 (3.1%, 3.0–3.1) | 526 837 | 34 562 (6.6%, 6.5–6.6) |
| Non‐farmer | 1 141 076 | 37 177 (3.3%, 3.2–3.3) | 480 808 | 37 177 (7.7%, 7.7–7.8) |
| Unknown* | 39 902 | 1540 (3.9%, 3.7–4.0) | 16 135 | 1540 (9.5%, 9.1–10.0) |
| Household income, Yuan/y | ||||
| <10 000 | 487 418 | 14 307 (2.9%, 2.9–3.0) | 230 788 | 14 307 (6.2%, 6.1–6.3) |
| 10 000 to 50 000 | 1 273 538 | 40 359 (3.2%, 3.1–3.2) | 562 310 | 40 359 (7.2%, 7.1–7.2) |
| >50 000 | 339 806 | 11 908 (3.5%, 3.4–3.6) | 140 365 | 11 908 (8.5%, 8.3–8.6) |
| Unknown* | 209 422 | 6705 (3.2%, 3.1–3.3) | 90 317 | 6705 (7.4%, 7.3–7.6) |
| Marital status | ||||
| Married | 2 147 107 | 69 159 (3.2%, 3.2–3.2) | 938 370 | 69 159 (7.4%, 7.3–7.4) |
| Widowed, separated, divorced, single | 134 977 | 3192 (2.4%, 2.3–2.4) | 73 581 | 3192 (4.3%, 4.2–4.5) |
| Unknown* | 28 100 | 928 (3.3%, 3.1–3.5) | 11 829 | 928 (7.8%, 7.4–8.3) |
| Health insurance status | ||||
| Insured | 2 261 969 | 71 580 (3.2%, 3.1–3.2) | 1 003 779 | 71 580 (7.1%, 7.1–7.2) |
| Uninsured | 13 780 | 502 (3.6%, 3.3–4.0) | 5392 | 502 (9.3%, 8.5–10.1) |
| Unknown* | 34 435 | 1197 (3.5%, 3.3–3.7) | 14 609 | 1197 (8.2%, 7.7–8.6) |
| Medical history | ||||
| Myocardial infarction | 17 224 | 496 (2.9%, 2.6–3.1) | 10 943 | 496 (4.5%, 4.1–4.9) |
| Stroke | 55 868 | 1614 (2.9%, 2.8–3.0) | 40 240 | 1614 (4.0%, 3.8–4.2) |
| Diabetes mellitus | 148 238 | 3499 (2.4%, 2.3–2.4) | 96 828 | 3499 (3.6%, 3.5–3.7) |
| CVD risk factor | ||||
| Current smoker | 455 867 | 20 667 (4.5%, 4.5–4.6) | 206 445 | 20 667 (10.0%, 9.9–10.1) |
| Current drinker | 559 201 | 26 529 (4.7%, 4.7–4.8) | 266 712 | 26 529 (9.9%, 9.8–10.1) |
| Obesity | 365 543 | 17 241 (4.7%, 4.6–4.8) | 231 299 | 17 241 (7.5%, 7.3–7.6) |
CVD indicates cardiovascular disease; IDH, isolated diastolic hypertension.
Participants either refused to answer the question or did not know the answer.
Table 3.
Prevalence and Awareness of Isolated Diastolic Hypertension Among Untreated Hypertensives, by Population Characteristics
| Characteristics | Untreated Hypertensive Participants (n) | Prevalence of IDH n (%, 95% CI) | Awareness Among IDH Participants n (%, 95% CI) |
|---|---|---|---|
| n (%, 95% CI) | 718 666 | 63 112 (8.8%, 8.7–8.8) | 6512 (10.3%, 10.1–10.6) |
| Age, y | |||
| 35 to 39 | 16 425 | 4361 (26.6%, 25.9–27.2) | 274 (6.3%, 5.6–7.0) |
| 40 to 44 | 46 923 | 9658 (20.6%, 20.2–20.9) | 633 (6.6%, 6.1–7.0) |
| 45 to 49 | 84 788 | 13 560 (16.0%, 15.7–16.2) | 1179 (8.7%, 8.2–9.2) |
| 50 to 54 | 121 131 | 13 939 (11.5%, 11.3–11.7) | 1551 (11.1%, 10.6–11.6) |
| 55 to 59 | 109 324 | 8354 (7.6%, 7.5–7.8) | 1022 (12.2%, 11.5–12.9) |
| 60 to 64 | 144 370 | 7258 (5.0%, 4.9–5.1) | 969 (13.4%, 12.6–14.1) |
| 65 to 69 | 117 786 | 4062 (3.4%, 3.3–3.6) | 619 (15.2%, 14.1–16.3) |
| 70 to 75 | 77 919 | 1920 (2.5%, 2.4–2.6) | 265 (13.8%, 12.3–15.3) |
| Sex | |||
| Men | 311 796 | 36 421 (11.7%, 11.6–11.8) | 3777 (10.4%, 10.1–10.7) |
| Women | 406 870 | 26 691 (6.6%, 6.5–6.6) | 2735 (10.2%, 9.9–10.6) |
| Urbanity | |||
| Urban | 250 233 | 22 345 (8.9%, 8.8–9.0) | 2187 (9.8%, 9.4–10.2) |
| Rural | 468 433 | 40 767 (8.7%, 8.6–8.8) | 4325 (10.6%, 10.3–10.9) |
| Region | |||
| Eastern | 259 305 | 20 374 (7.9%, 7.8–8.0) | 2432 (11.9%, 11.5–12.4) |
| Western | 240 487 | 24 697 (10.3%, 10.1–10.4) | 1998 (8.1%, 7.7–8.4) |
| Central | 218 874 | 18 041 (8.2%, 8.1–8.4) | 2082 (11.5%, 11.1–12.0) |
| Education | |||
| Primary school or lower | 357 641 | 23 063 (6.4%, 6.4–6.5) | 2450 (10.6%, 10.2–11.0) |
| Middle school | 220 050 | 22 377 (10.2%, 10.0–10.3) | 2292 (10.2%, 9.8–10.6) |
| High school | 92 551 | 10 333 (11.2%, 11.0–11.4) | 1035 (10.0%, 9.4–10.6) |
| College or above | 38 218 | 6314 (16.5%, 16.1–16.9) | 673 (10.7%, 9.9–11.4) |
| Unknown* | 10 206 | 1025 (10.0%, 9.5–10.6) | 62 (6.0%, 4.6–7.5) |
| Employment | |||
| Employed | 522 751 | 50 534 (9.7%, 9.6–9.7) | 4909 (9.7%, 9.5–10.0) |
| Unemployed | 8739 | 1109 (12.7%, 12.0–13.4) | 147 (13.3%, 11.3–15.3) |
| Retired | 116 143 | 6351 (5.5%, 5.3–5.6) | 897 (14.1%, 13.3–15.0) |
| Housework | 58 954 | 3761 (6.4%, 6.2–6.6) | 441 (11.7%, 10.7–12.8) |
| Unknown* | 12 079 | 1357 (11.2%, 10.7–11.8) | 118 (8.7%, 7.2–10.2) |
| Occupation | |||
| Famer | 387 791 | 30 616 (7.9%, 7.8–8.0) | 3040 (9.9%, 9.6–10.3) |
| Non‐farmer | 318 796 | 31 139 (9.8%, 9.7–9.9) | 3354 (10.8%, 10.4–11.1) |
| Unknown* | 12 079 | 1357 (11.2%, 10.7–11.8) | 118 (8.7%, 7.2–10.2) |
| Household income, Yuan/y | |||
| <10 000 | 168 343 | 12 725 (7.6%, 7.4–7.7) | 1222 (9.6%, 9.1–10.1) |
| 10 000 to 50 000 | 390 550 | 34 601 (8.9%, 8.8–8.9) | 3462 (10.0%, 9.7–10.3) |
| >50 000 | 92 258 | 9903 (10.7%, 10.5–10.9) | 1186 (12.0%, 11.3–12.6) |
| Unknown* | 67 515 | 5883 (8.7%, 8.5–8.9) | 642 (10.9%, 10.1–11.7) |
| Marital status | |||
| Married | 662 083 | 59 671 (9.0%, 8.9–9.1) | 6141 (10.3%, 10.0–10.5) |
| Widowed, separated, divorced, single | 47 873 | 2629 (5.5%, 5.3–5.7) | 321 (12.2%, 11.0–13.5) |
| Unknown* | 8710 | 812 (9.3%, 8.7–9.9) | 50 (6.2%, 4.5–7.8) |
| Health insurance status | |||
| Insured | 704 139 | 61 637 (8.8%, 8.7–8.8) | 6371 (10.3%, 10.1–10.6) |
| Uninsured | 4130 | 448 (10.8%, 9.9–11.8) | 48 (10.7%, 7.9–13.6) |
| Unknown* | 10 397 | 1027 (9.9%, 9.3–10.5) | 93 (9.1%, 7.3–10.8) |
| Medical history | |||
| Myocardial infarction | 5167 | 334 (6.5%, 5.8–7.1) | 99 (29.6%, 24.7–34.5) |
| Stroke | 18 897 | 986 (5.2%, 4.9–5.5) | 309 (31.3%, 28.4–34.2) |
| Diabetes mellitus | 51 296 | 2521 (4.9%, 4.7–5.1) | 650 (25.8%, 24.1–27.5) |
| CVD risk factor | |||
| Current smoker | 149 972 | 17 842 (11.9%, 11.7–12.1) | 1847 (10.4%, 9.9–10.8) |
| Current drinker | 193 777 | 22 740 (11.7%, 11.6–11.9) | 2389 (10.5%, 10.1–10.9) |
| Obesity | 146 456 | 13 970 (9.5%, 9.4–9.7) | 1908 (13.7%, 13.1–14.2) |
CVD indicates cardiovascular disease; IDH, isolated diastolic hypertension.
Participants either refused to answer the question or did not know the answer.
The 1198 subgroups varied with respect to the prevalence of participants with IDH (median: 2.9%, [IQR: 1.7–4.7]; Figure S2). The prevalence of IDH was substantially higher in subgroups with participants who were younger, men, without prior cardiovascular event, and without DM as compared with participants who were older, women, with prior cardiovascular event, and with DM (Figure 2). Subgroups with at least 500 participants had similar results (Figures S3 and S4).
Figure 2.
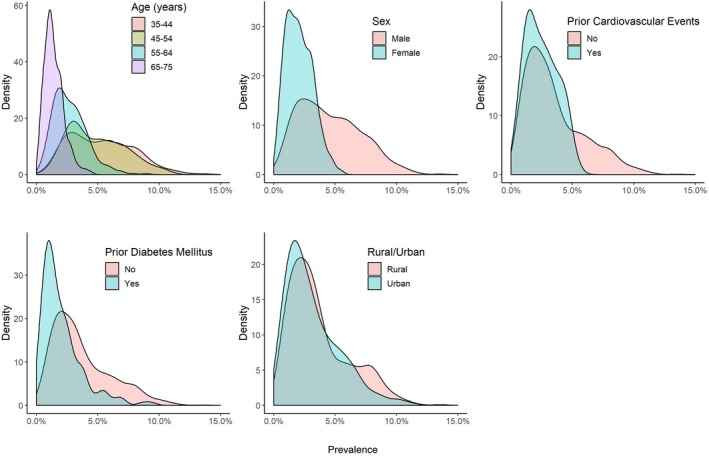
Density plots of prevalence of isolated diastolic hypertension among all study participants in 1198 mutually exclusive population subgroups (of at least 200 participants), by age, sex, prior cardiovascular events, history of diabetes mellitus, and urbanity.
In mixed effects multivariable logistic regression analysis assessing independent predictors of IDH, we identified several individual characteristics associated with the prevalence of IDH (Table 4). When compared with normotensives, participants who were young‐ and middle‐aged, men, were at least college educated, consumed alcohol, had DM, were obese, and had prior cardiovascular events were more likely to have IDH than those who were older, women, less educated, did not consume alcohol, were not obese, and did not have DM or prior cardiovascular events (all P<0.01). Participants who were married, farmers, and current smokers were less likely to have IDH (all P<0.001). Income and health insurance did not have a significant association with prevalence of IDH. Similarly, when compared with participants with other hypertension subtypes, participants who were younger, men, were at least college educated, and consumed alcohol were more likely to have IDH (all P<0.001); whereas, participants who were older, farmer, current smokers, had DM, were obese, had prior cardiovascular events, and belonged to the Central or Eastern regions were more likely to have other types of hypertension (all P<0.001).
Table 4.
Mixed Effects Multivariable Regression Models for Association Between Individual Characteristics and the Prevalence of Isolated Diastolic Hypertension and the Awareness Among Untreated Participants With Isolated Diastolic Hypertension
| Prevalence of IDH | Awareness Among IDH Participants | |||||
|---|---|---|---|---|---|---|
| Model 1 Odds Ratio (95% CI) | P Value | Model 2 Odds Ratio (95% CI) | P Value | Odds Ratio (95% CI) | P Value | |
| Age, y | ||||||
| 35 to 39 | 1 | 1 | 1 | |||
| 40 to 44 | 1.27 (1.22–1.32) | <0.001 | 0.81 (0.78–0.84) | <0.001 | 1.24 (1.08–1.43) | 0.003 |
| 45 to 49 | 1.46 (1.41–1.52) | <0.001 | 0.59 (0.57–0.62) | <0.001 | 1.65 (1.45–1.88) | <0.001 |
| 50 to 54 | 1.54 (1.48–1.60) | <0.001 | 0.40 (0.38–0.42) | <0.001 | 2.13 (1.87–2.43) | <0.001 |
| 55 to 59 | 1.29 (1.25–1.35) | <0.001 | 0.25 (0.24–0.26) | <0.001 | 2.37 (2.07–2.72) | <0.001 |
| 60 to 64 | 0.99 (0.95–1.03) | 0.534 | 0.15 (0.14–0.15) | <0.001 | 2.75 (2.40–3.17) | <0.001 |
| 65 to 69 | 0.79 (0.75–0.83) | <0.001 | 0.09 (0.09–0.10) | <0.001 | 3.26 (2.80–3.79) | <0.001 |
| 70 to 75 | 0.64 (0.61–0.68) | <0.001 | 0.06 (0.06–0.07) | <0.001 | 3.05 (2.53–3.68) | <0.001 |
| Sex | ||||||
| Men | 1 | 1 | 1 | |||
| Women | 0.45 (0.44–0.45) | <0.001 | 0.50 (0.49–0.51) | <0.001 | 1.07 (1.00–1.14) | 0.052 |
| Marital status | ||||||
| Not married | 1 | 1 | 1 | |||
| Married | 0.91 (0.88–0.95) | <0.001 | 1.02 (0.98–1.07) | 0.279 | 0.88 (0.78–1.00) | 0.057 |
| Household income, Yuan/y | ||||||
| <10 000 | 1 | 1 | 1 | |||
| 10 000 to 50 000 | 0.97 (0.95–1.00) | 0.031 | 1.01 (0.99–1.04) | 0.277 | 1.04 (0.97–1.13) | 0.264 |
| >50 000 | 0.99 (0.95–1.02) | 0.417 | 1.05 (1.01–1.08) | 0.014 | 1.17 (1.06–1.30) | 0.003 |
| Education level | ||||||
| Lower than college | 1 | 1 | 1 | |||
| College or above | 1.08 (1.04–1.11) | <0.001 | 1.10 (1.07–1.14) | <0.001 | 1.16 (1.05–1.28) | 0.003 |
| Occupation | ||||||
| Not farmer | 1 | 1 | 1 | |||
| Farmer | 0.95 (0.92–0.97) | <0.001 | 0.92 (0.89–0.94) | <0.001 | 0.94 (0.87–1.00) | 0.066 |
| Health insurance status | ||||||
| Uninsured | 1 | 1 | 1 | |||
| Insured | 1.07 (0.98–1.15) | 0.115 | 1.02 (0.94–1.10) | 0.699 | 0.87 (0.69–1.10) | 0.259 |
| CVD risk factor | ||||||
| Current smoker | 0.88 (0.86–0.90) | <0.001 | 0.96 (0.94–0.99) | 0.001 | 1.02 (0.95–1.09) | 0.656 |
| Current drinker | 1.38 (1.35–1.41) | <0.001 | 1.07 (1.04–1.09) | <0.001 | 1.02 (0.96–1.09) | 0.529 |
| Diabetes mellitus | 1.05 (1.01–1.09) | 0.012 | 0.63 (0.60–0.65) | <0.001 | 2.31 (2.09–2.55) | <0.001 |
| Obesity | 2.49 (2.44–2.54) | <0.001 | 0.92 (0.90–0.94) | <0.001 | 1.50 (1.41–1.59) | <0.001 |
| Prior CVE | 1.65 (1.57–1.74) | <0.001 | 0.80 (0.76–0.84) | <0.001 | 3.14 (2.75–3.59) | <0.001 |
| Geographic region | ||||||
| Western | 1 | 1 | 1 | |||
| Eastern | 0.91 (0.88–0.95) | <0.001 | 0.78 (0.75–0.81) | <0.001 | 1.52 (1.38–1.67) | <0.001 |
| Central | 0.97 (0.93–1.01) | 0.167 | 0.82 (0.79–0.86) | <0.001 | 1.43 (1.30–1.58) | <0.001 |
Model 1 includes normotensive participants and participants with isolated diastolic hypertension. Model 2 includes participants with isolated diastolic hypertension and participants with other types of hypertension (isolated systolic hypertension, systolic diastolic hypertension, controlled hypertension). CVD indicates cardiovascular disease; CVE, cardiovascular event; IDH, isolated diastolic hypertension; ISH, isolated systolic hypertension; SDH, systolic diastolic hypertension.
Awareness of Having Hypertension Among Untreated Participants
Among untreated IDH participants (n=63 112 or 86.1% of the overall IDH group), only 6512 (or 10.3%) were aware of having hypertension, whereas 72 220 (or 24.8%) of the 290 645 untreated ISH and 89 516 (or 44.1%) of the 203 173 untreated SDH participants were aware of having hypertension. Awareness among untreated participants across all subtypes of hypertension increased with age; however, awareness among participants with IDH was significantly lower than other hypertensives (ISH and SDH), across all age groups (Figure 3; P<0.005 for all age ‐groups). The awareness rates were higher among those who lived in rural areas or Eastern or Central regions, were retired, had a higher income, and were widowed/separated/or divorced (Table 3). Fewer than 15% of the IDH participants with at least 1 or more cardiovascular risk factors (including smoking, alcohol use, and obesity) and <33% of IDH participants with a prior cardiovascular event or DM were aware of having hypertension. The 1198 subgroups varied with respect to awareness of having hypertension among untreated IDH participants (median: 9.7% [IQR: 4.0–17.6]; Figure S2). Awareness was higher in subgroups of participants who were older, had prior cardiovascular event, and had prior DM (Figure 4). Awareness rates were similar among men and women and in rural and urban areas. Subgroups with at least 500 participants had similar results (Figures S3 and S4).
Figure 3.
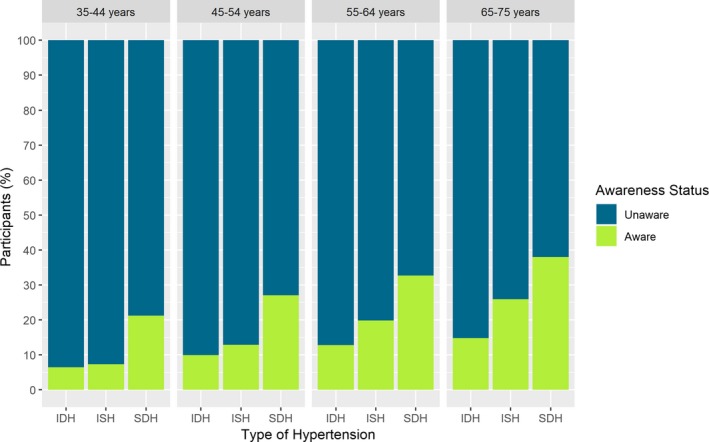
Awareness of having hypertension among untreated participants with isolated diastolic hypertension (IDH), isolated systolic hypertension (ISH), and systolic‐diastolic hypertension (SDH), by age group.
Figure 4.
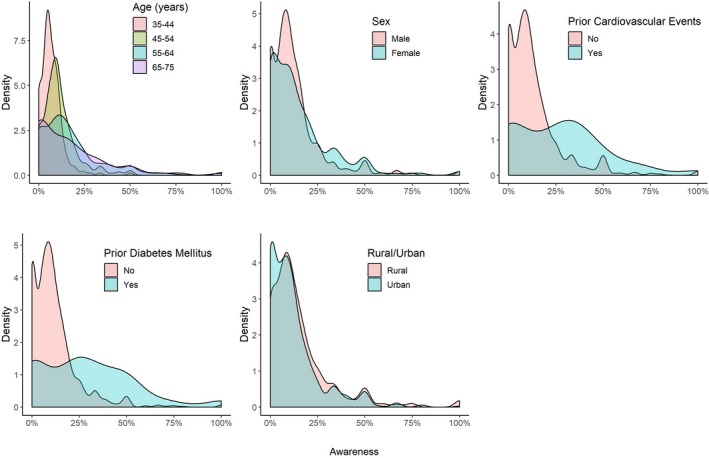
Density plots of awareness of having hypertension among untreated participants with isolated diastolic hypertension in 1198 mutually exclusive population subgroups (of at least 200 participants), by age, sex, prior cardiovascular events, history of diabetes mellitus, and urbanity.
We identified several independent factors associated with awareness of having hypertension among untreated IDH participants (Table 4). Awareness was significantly higher among IDH participants who were older, women, had higher income (>50 000 Yuan/year), were at least college educated, obese, had DM, prior cardiovascular event, and belonged to Central or Eastern region (all P<0.05). Participant's marital status, occupation, health insurance status, and health behaviors like smoking and alcohol use, were not independently associated with their awareness of having hypertension.
Treatment Patterns Among Treated Participants With IDH
Most treated participants with IDH reported taking 1 antihypertensive medication in both urban and rural areas (Figure 5). Even though use of combination therapy increased slightly with age, <5% of the participants received ≥3 drugs across all age groups. Most treated participants with IDH reported taking Western antihypertensive medications (9969 or 98%). Among IDH participants using 2 or fewer classes of medications, calcium channel blockers (42%) were the most frequent class of medication used, followed by angiotensin‐converting enzyme inhibitors or angiotensin receptor blockers (20%), and diuretics (7%), respectively (Table 5). On stratification of IDH patients based on their degree of DBP elevation, we found that the majority (74.7%) had DBP of 90 to 95 mm Hg, followed by 96 to 100 mm Hg (19.6%), and >100 mm Hg (5.7%), respectively. The most frequently used antihypertensive medication class and the number of antihypertensive medications used did not vary significantly between 3 groups (both P>0.05; Figure S5).
Figure 5.
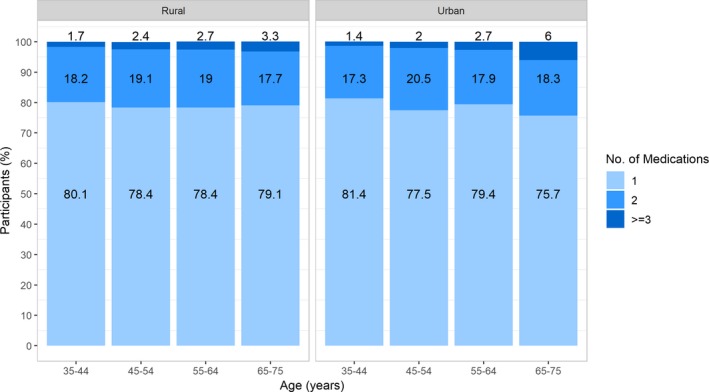
Number of antihypertensive medications used by treated participants with isolated diastolic hypertension, by age and urbanity.
Table 5.
Classes of Antihypertensive Medications Used by Treated Participants With Isolated Diastolic Hypertension
| A | B | C | D | F | T | |
|---|---|---|---|---|---|---|
| A | 1808 (20.08%) | 136 (1.51%) | 602 (6.69%) | 276 (3.07%) | 10 (0.11%) | 4 (0.04%) |
| B | 331 (3.68%) | 224 (2.49%) | 27 (0.30%) | 13 (0.14%) | 3 (0.03%) | |
| C | 3780 (41.99%) | 71 (0.79%) | 43 (0.48%) | 14 (0.16%) | ||
| D | 638 (7.09%) | 11 (0.12%) | 0 (0%) | |||
| F | 563 (6.25%) | 1 (0.01%) | ||||
| T | 198 (2.20%) |
A indicates angiotensin converting enzyme inhibitors or angiotensin receptor blockers; B, beta‐blockers; C, calcium channel blockers; D, diuretics; F, fixed‐dose combination drugs; T, traditional Chinese medication.
Discussion
In this large study, we report the characteristics, prevalence, awareness, and treatment patterns of people with IDH in China, and how these differ from other hypertensives and vary across diverse population subgroups. We found that IDH affected almost 4% of adults between 35 and 75 years in China (and represents nearly 25% of the hypertensive population aged <45 years). Awareness of hypertension was significantly lower among people with IDH as compared with other types of hypertension and was lowest among young‐ and middle‐aged adults in whom IDH was most prevalent. Additionally, among those with IDH despite treatment, the vast majority were treated with only 1 class of antihypertensive medication.
This study extends the scientific literature in several ways. First, this is one of the largest population‐based studies, to our knowledge, to evaluate the characteristics and prevalence of IDH, allowing us to draw robust conclusions across a wide variety of diverse subgroups. Our findings that young age, male sex, obesity, DM, alcohol consumption, and prior cardiovascular events are positively associated with IDH prevalence supports and expands on the associations previously described in the literature but with smaller numbers of patients with IDH.1, 3, 20, 25, 26, 27 For example, Franklin et al20 and Liu et al25 showed that younger age, male sex, and BMI were predictors of IDH in a small population of IDH patients. In this study, we identified additional factors associated with IDH including DM, alcohol consumption, history of prior cardiovascular event, and showed that these associations were consistent across tens of thousands of individuals with IDH and across diverse population subgroups. The prevalence rates of IDH found in our study were also comparable with those reported previously in studies not only from Chinese cohorts (for example, Huang et al3 found a prevalence of 4.4% among adults aged 35 to 74 and Sun et al11 found a prevalence of 5.8% among adults >35 years), but also from other low‐ and middle‐income countries.26, 27
Second, to the best of our knowledge, our study is the first to assess the awareness of having hypertension among a large Chinese population with IDH compared with other hypertension subtypes, and to identify characteristics that are associated with awareness. Our findings suggest that even though awareness among participants with IDH increases with age, it is significantly lower as compared with awareness among participants with other hypertension subtypes, across all age groups. These findings are consistent with previous reports from other countries which have shown 26% lower diagnosis (hazard ratio 0.74; CI 0.60–0.92) and 31% lower medication initiation (hazard ratio 0.69; CI 0.55–0.86) among younger patients with IDH as compared with systolic/diastolic hypertension.18
Third, our assessment of the antihypertensive medications among treated participants with IDH provides information on what medications may not be effectively treating IDH or that people are not taking. We found that the majority of these patients were treated with only 1 class of antihypertensive medication. Calcium channel blockers was the most frequently used class of antihypertensive medication among these patients, even though they may not be most effective for this phenotype, which could be due to the prescription habits of the physicians, availability, and cost‐related factors of other classes of antihypertensive medications.28
Clinical Implications
These findings have important clinical implications as IDH is independently associated with a higher risk of incident heart failure and cardiovascular mortality as compared with normal BP, and BP lowering in patients with IDH has been shown to protect against major vascular events.29, 30, 31 As such, identifying characteristics that may be associated with IDH and understanding the current awareness and treatment patterns among those with IDH can help identify the patients at increased cardiovascular risk and highlight the opportunities for improving their care. Current hypertension management guidelines15, 16, 17 lack guidance on management of patients with IDH and the recent randomized clinical trials32, 33 focused only on SBP targets for improving outcomes, resulting in lack of contemporary guidance on optimal DBP targets for management of patients with IDH. As clinicians and public health professionals develop and implement strategies to help prevent and control hypertension, our findings suggest the need to target people with IDH among other hypertension subtypes for reducing the burden of hypertension.
Considering that patients with IDH are much younger and often without additional cardiovascular risk factors as compared with other hypertension subtypes, they are less likely to come in contact with the health system and hence, more likely to not to be diagnosed. These patients could benefit from more targeted hypertension screening initiatives focusing on the young‐ and middle‐aged adults. For example, promoting free BP screenings at work places and in schools and colleges could result in early diagnosis of those with IDH, and prevent the catastrophic sequelae of hypertension in these patients. Additionally, given the growing burden of obesity in China and its strong association with IDH, it is critical to slow the increase in BMI through public health interventions, to prevent the development of IDH in unaffected individuals. Moreover, increasing awareness of the clinical significance of an elevated DBP in the young and providing clear guidance on management of patients with IDH could also ensure better management of these patients. The point is that the emphasis on SBP should not lead to the neglect of people with IDH.
This study was derived from a large Chinese population. China is of special interest because it represents 25% of the world's population and hypertension is a major public health challenge in China. However, given that China is more recent in the epidemiological transition, and treatment rates are much lower than many Western countries, similar large‐scale studies in other countries are warranted to understand impact of nation‐specific characteristics on the epidemiology of IDH. Nevertheless, these findings are relevant for several low‐ and middle‐income countries where hypertension is growing in importance, treatment rates tend to be lower, and fewer evidence exists to guide public health programs.
Limitations
Our study has several potential limitations. First, for estimation of characteristics and prevalence of participants with IDH, we classified patients into different hypertension subgroups based on the value of the SBP and DBP at enrollment, irrespective of their medication use. As such, some treated hypertensive participants may have had their SBP controlled with medication, and may have been included in the IDH group. However, the vast majority (86%) of the participants in the IDH group were untreated. Moreover, since the treated participants with IDH had persistent elevation of their DBP even after treatment, they were not much different from the untreated IDH group, as shown in Table S1. Second, treated IDH patients who had their DBP <90 mm Hg were classified as having “controlled hypertension” instead of IDH, which could have underestimated the prevalence of IDH of China. However, considering that less than one third of the people with hypertension receive treatment in China and an even fewer proportion actually have controlled hypertension, and that these rates are even lower for younger age groups where IDH is most prevalent,23 few individuals in the IDH group would have been classified as having “controlled hypertension”. Third, our study used convenience rather than a nationally representative sample for large‐scale recruitment. This could have resulted in a sampling bias resulting in overestimation of the awareness and treatment rates since these participants would be more likely to be in contact with the health system. Fourth, awareness and treatment rates could also have been affected by a participant's access to and use of healthcare services, however, we did not collect this information in this study. Fifth, since we also used “self‐reported use of an antihypertensive medication in the past 2 weeks” as a criterion for defining hypertension, some patients taking hypertensive medication might not have reported that use, possibly underestimating the burden of hypertension in China. Lastly, for individuals who were aware of having hypertension, our study did not collect information on the duration of hypertension, which could have influenced the treatment patterns seen among these participants.
Conclusions
IDH affects a large number of adults in China, and these patients may have some unique characteristics as compared with people without hypertension as well as those with other types of hypertension. However, patients with IDH have the lowest rate of awareness compared with other hypertension subtypes, and most participants with IDH despite treatment had scope for further increase in the intensity of therapy. Our findings suggest the need to specifically focus public health and clinical strategies on people with IDH and improve their diagnosis and treatment, to mitigate the burden of hypertension, especially in the young‐ and middle‐aged population.
Appendix
Members of the Provincial Coordinating Office in China PEACE Million Persons Project
Beijing Center for Diseases Prevention and Control: Chun Huang, Zhong Dong, Bo Jiang; Tianjin Chest Hospital: Zhigang Guo, YingYi Zhang; Hebei Center for Diseases Prevention and Control: Jixin Sun, Yuhuan Liu; Shanxi Center for Diseases Prevention and Control: Zeping Ren, Yaqing Meng; Inner Mongolia Center for Diseases Prevention and Control: Zhifen Wang, Yunfeng Xi; Liaoning Center for Diseases Prevention and Control: Liying Xing, Yuanmeng Tian; Jilin Center for Diseases Prevention and Control: Jianwei Liu, Yao Fu, Ting Liu; Heilongjiang Center for Diseases Prevention and Control: Wei Sun, Shichun Yan, Lin Jin; Shanghai Center for Diseases Prevention and Control: Yang Zheng, Jing Wang; Jiangsu Center for Diseases Prevention and Control; Zhejiang Provincial People's Hospital: Jing Yan, Xiaoling Xu; Anhui Center for Diseases Prevention and Control: Yeji Chen, Xiuya Xing, Luan Zhang; Fujian Center for Diseases Prevention and Control: Wenling Zhong, Xin Fang; Jiangxi Center for Diseases Prevention and Control: Liping Zhu, Yan Xu; Shandong Center for Diseases Prevention and Control: Xiaolei Guo, Chunxiao Xu; Henan Center for Diseases Prevention and Control: Gang Zhou, Lei Fan, Minjie Qi; Hubei Center for Diseases Prevention and Control: Shuzhen Zhu, Junfeng Qi, Junlin Li; Hunan Center for Diseases Prevention and Control: Li Yin, Qiong Liu; Guangdong Provincial People's Hospital: Qingshan Geng, Yingqing Feng, Jiabin Wang; The First Affiliated Hospital of Guangxi Medical University: Hong Wen; Health Commission of Hainan: Xuemei Han; Hainan Center for Diseases Prevention and Control: Puyu Liu; Chongqing Center for Diseases Prevention and Control: Xianbin Ding, Jie Xu; Sichuan Center for Diseases Prevention and Control: Ying Deng, Jun He; Guizhou Provincial People's Hospital: Gui'e Liu, Chenxi Jiang; Yunnan Center for Diseases Prevention and Control: Shun Zha, Cangjiang Yang; Tibet Center for Diseases Prevention and Control: Guoxia Bai, Yue Yu, Zongji Tashi; Shaanxi Center for Diseases Prevention and Control: Lin Qiu, Zhiping Hu; Gansu Center for Diseases Prevention and Control: Hupeng He, Jing Zhang; Qinghai Center for Diseases Prevention and Control: Minru Zhou, Xiaoping Li; Ningxia Center for Diseases Prevention and Control: Jianhua Zhao, Shaoning Ma; The First Affiliated Hospital of Xinjiang Medical University: Yitong Ma, Ying Huang, Yuchen Zhang; and Xinjiang Corps Center for Diseases Prevention and Control: Fanka Li, Jiacong Shen.
Sources of Funding
The National Key Research and Development Program from the Ministry of Science and Technology of China (2018YFC1312400); the Chinese Academy of Medical Sciences Innovation Fund for Medical Science (2016‐I2M‐1‐006); the Major Public Health Service Project from the Ministry of Finance and National Health Commission of China; and the 111 Project from the Ministry of Education of China (B16005).
Disclosures
Dr Krumholz works under contract with the Centers for Medicare & Medicaid Services to support quality measurement programs; was a recipient of a research grant, through Yale, from Medtronic and the U.S. Food and Drug Administration to develop methods for post‐market surveillance of medical devices; was a recipient of a research grant with Medtronic and is the recipient of a research grant from Johnson & Johnson, through Yale University, to support clinical trial data sharing; was a recipient of a research agreement, through Yale University, from the Shenzhen Center for Health Information for work to advance intelligent disease prevention and health promotion; collaborates with the National Center for Cardiovascular Diseases in Beijing; receives payment from the Arnold & Porter Law Firm for work related to the Sanofi clopidogrel litigation, from the Ben C. Martin Law Firm for work related to the Cook IVC filter litigation, and from the Siegfried and Jensen Law Firm for work related to Vioxx litigation; chairs a Cardiac Scientific Advisory Board for UnitedHealth; was a participant/participant representative of the IBM Watson Health Life Sciences Board; is a member of the Advisory Board for Element Science, the Advisory Board for Facebook, and the Physician Advisory Board for Aetna; and is the founder of HugoHealth, a personal health information platform and co‐founder of Refactor Health. Dr Lu is supported by the National Heart, Lung, and Blood Institute (K12HL138037). Dr Gupta is supported by grant T32 HL007854 from the National Heart, Lung and Blood Institute of the National Institutes of Health; is a member of Heartbeat Health, Inc, a preventive cardiology platform; received payment from the Ben C. Martin Law Firm for work related to the Cook IVC filter litigation. The remaining authors have no disclosures to report.
Supporting information
Data S1. Supplemental methods.
Table S1. Baseline Characteristics of Participants With Isolated Diastolic Hypertension, by Treatment Status
Table S2. Prevalence of Isolated Diastolic Hypertension Among Treated Hypertensive Participants, by Population Characteristics
Figure S1. Flowchart of study participant selection in China Patient‐Centered Evaluative Assessment of Cardiac Events Million Persons Project.
Figure S2. Histograms of prevalence of isolated diastolic hypertension (IDH) and awareness among untreated IDH participants in 1198 mutually exclusive population subgroups (at least 200 participants each) defined priori by 10 selected characteristics.
Figure S3. Histograms prevalence of isolated diastolic hypertension (IDH) and awareness among untreated IDH participants in 731 mutually exclusive population subgroups (at least 500 participants each) defined priori by 10 selected characteristics.
Figure S4. Density plots of prevalence of isolated diastolic hypertension (IDH) among all study participants (A) and awareness among untreated IDH participants (B) in 731 mutually exclusive population subgroups (of at least 500 participants), by age, sex, prior cardiovascular events, history of diabetes mellitus, and urbanity.
Figure S5. Number of antihypertensive medications used by treated participants with isolated diastolic hypertension, by degree of diastolic blood pressure elevation.
Acknowledgments
The authors thank all study participants and appreciate the contributions made by project teams at the National Center for Cardiovascular Diseases and the Yale‐New Haven Hospital Center for Outcomes Research and Evaluation in the realm of project design and operations. They also thank all provincial and regional officers and research staff for data collection.
(J Am Heart Assoc. 2019;8:e012954 DOI: 10.1161/JAHA.119.012954.)
Contributor Information
Xin Zheng, Email: xin.zheng@fwoxford.org.
Jing Li, Email: jing.li@fwoxford.org.
the China PEACE Collaborative Group:
Zhong Dong, Bo Jiang, YingYi Zhang, Yuhuan Liu, Yaqing Meng, Yunfeng Xi, Yuanmeng Tian, Yao Fu, Ting Liu, Shichun Yan, Lin Jin, Jing Wang, Xiaoling Xu, Xiuya Xing, Luan Zhang, Xin Fang, Yan Xu, Chunxiao Xu, Lei Fan, Minjie Qi, Junfeng Qi, Junlin Li, Qiong Liu, Yingqing Feng, Jiabin Wang, Hong Wen, Jie Xu, Jun He, Chenxi Jiang, Cangjiang Yang, Yue Yu, Zongji Tashi, Zhiping Hu, Jing Zhang, Xiaoping Li, Shaoning Ma, Yitong Ma, Ying Huang, Yuchen Zhang, and Jiacong Shen
References
- 1. Kelly TN, Gu D, Chen J, Huang JF, Chen JC, Duan X, Wu X, Yau CL, Whelton PK, He J. Hypertension subtype and risk of cardiovascular disease in Chinese adults. Circulation. 2008;118:1558–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Franklin SS, Jacobs MJ, Wong ND, L'Italien GJ, Lapuerta P. Predominance of isolated systolic hypertension among middle‐aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension. 2001;37:869–874. [DOI] [PubMed] [Google Scholar]
- 3. Huang J, Wildman RP, Gu D, Muntner P, Su S, He J. Prevalence of isolated systolic and isolated diastolic hypertension subtypes in China. Am J Hypertens. 2004;17:955–962. [DOI] [PubMed] [Google Scholar]
- 4. Qi SF, Zhang B, Wang HJ, Yan J, Mi YJ, Liu DW, Tian QB. Prevalence of hypertension subtypes in 2011 and the trends from 1991 to 2011 among Chinese adults. J Epidemiol Community Health. 2016;70:444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guichard JL, Desai RV, Ahmed MI, Mujib M, Fonarow GC, Feller MA, Ekundayo OJ, Bittner V, Aban IB, White M, Aronow WS, Love TE, Bakris GL, Zieman SJ, Ahmed A. Isolated diastolic hypotension and incident heart failure in older adults. Hypertension. 2011;58:895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kanegae H, Oikawa T, Okawara Y, Hoshide S, Kario K. Which blood pressure measurement, systolic or diastolic, better predicts future hypertension in normotensive young adults? J Clin Hypertens (Greenwich). 2017;19:603–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li H, Kong F, Xu J, Zhang M, Wang A, Zhang Y. Hypertension subtypes and risk of cardiovascular diseases in a Mongolian population, inner Mongolia, China. Clin Exp Hypertens. 2016;38:39–44. [DOI] [PubMed] [Google Scholar]
- 8. Li Y, Wei FF, Thijs L, Boggia J, Asayama K, Hansen TW, Kikuya M, Bjorklund‐Bodegard K, Ohkubo T, Jeppesen J, Gu YM, Torp‐Pedersen C, Dolan E, Liu YP, Kuznetsova T, Stolarz‐Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka‐Jaszcz K, Mena L, Maestre GE, Filipovsky J, Imai Y, O'Brien E, Wang JG, Staessen JA. Ambulatory hypertension subtypes and 24‐hour systolic and diastolic blood pressure as distinct outcome predictors in 8341 untreated people recruited from 12 populations. Circulation. 2014;130:466–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lotfaliany M, Akbarpour S, Mozafary A, Boloukat RR, Azizi F, Hadaegh F. Hypertension phenotypes and incident cardiovascular disease and mortality events in a decade follow‐up of a Middle East cohort. J Hypertens. 2015;33:1153–1161. [DOI] [PubMed] [Google Scholar]
- 10. Manios E, Michas F, Stamatelopoulos K, Koroboki E, Stellos K, Tsouma I, Vemmos K, Zakopoulos N. Association of isolated systolic, isolated diastolic, and systolic‐diastolic masked hypertension with carotid artery intima‐media thickness. J Clin Hypertens (Greenwich). 2015;17:22–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sun Z, Han X, Zheng L, Zhang X, Li J, Hu D, Sun Y. Subtypes of hypertension and risk of stroke in rural Chinese adults. Am J Hypertens. 2014;27:193–198. [DOI] [PubMed] [Google Scholar]
- 12. Wei FF, Li Y, Zhang L, Xu TY, Ding FH, Staessen JA, Wang JG. Association of target organ damage with 24‐hour systolic and diastolic blood pressure levels and hypertension subtypes in untreated Chinese. Hypertension. 2014;63:222–228. [DOI] [PubMed] [Google Scholar]
- 13. Wu Y, Liu F, Adi D, Yang YN, Xie X, Li XM, Ma X, Fu ZY, Huang Y, Chen BD, Shan CF, Ma YT. Association between carotid atherosclerosis and different subtypes of hypertension in adult populations: a multiethnic study in Xinjiang, China. PLoS One. 2017;12:e0171791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yano Y, Stamler J, Garside DB, Daviglus ML, Franklin SS, Carnethon MR, Liu K, Greenland P, Lloyd‐Jones DM. Isolated systolic hypertension in young and middle‐aged adults and 31‐year risk for cardiovascular mortality: the Chicago Heart Association Detection Project in Industry study. J Am Coll Cardiol. 2015;65:327–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu L; Writing Group of Chinese Guidelines for the Management of Hypertension . 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615. [PubMed] [Google Scholar]
- 16. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 17. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; Group ESCSD . 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 18. Johnson HM, Bartels CM, Thorpe CT, Schumacher JR, Pandhi N, Smith MA. Differential diagnosis and treatment rates between systolic and diastolic hypertension in young adults: a multidisciplinary observational study. J Clin Hypertens (Greenwich). 2015;17:885–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saladini F, Dorigatti F, Santonastaso M, Mos L, Ragazzo F, Bortolazzi A, Mattarei M, Garavelli G, Mormino P, Palatini P. Natural history of hypertension subtypes in young and middle‐age adults. Am J Hypertens. 2009;22:531–537. [DOI] [PubMed] [Google Scholar]
- 20. Franklin SS, Pio JR, Wong ND, Larson MG, Leip EP, Vasan RS, Levy D. Predictors of new‐onset diastolic and systolic hypertension: the Framingham Heart Study. Circulation. 2005;111:1121–1127. [DOI] [PubMed] [Google Scholar]
- 21. Asgari S, Khalili D, Mehrabi Y, Kazempour‐Ardebili S, Azizi F, Hadaegh F. Incidence and risk factors of isolated systolic and diastolic hypertension: a 10 year follow‐up of the Tehran Lipids and Glucose Study. Blood Press. 2016;25:177–183. [DOI] [PubMed] [Google Scholar]
- 22. Lu J, Xuan S, Downing NS, Wu C, Li L, Krumholz HM, Jiang L. Protocol for the China PEACE (Patient‐centered Evaluative Assessment of Cardiac Events) Million Persons Project pilot. BMJ Open. 2016;6:e010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, Su M, Zhao H, Spatz ES, Spertus JA, Masoudi FA, Krumholz HM, Jiang L. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population‐based screening study (China PEACE Million Persons Project). Lancet. 2017;390:2549–2558. [DOI] [PubMed] [Google Scholar]
- 24. Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut‐off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 25. Liu F, Adi D, Xie X, Li XM, Fu ZY, Shan CF, Huang Y, Chen BD, Gai MT, Gao XM, Ma YT, Yang YN. Prevalence of isolated diastolic hypertension and associated risk factors among different ethnicity groups in Xinjiang, China. PLoS One. 2015;10:e0145325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Midha T, Lalchandani A, Nath B, Kumari R, Pandey U. Prevalence of isolated diastolic hypertension and associated risk factors among adults in Kanpur, India. Indian Heart J. 2012;64:374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Saeed AA, Al‐Hamdan NA. Isolated diastolic hypertension among adults in Saudi Arabia: prevalence, risk factors, predictors and treatment. Results of a national survey. Balkan Med J. 2016;33:52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Su M, Zhang Q, Bai X, Wu C, Li Y, Mossialos E, Mensah GA, Masoudi FA, Lu J, Li X, Salas‐Vega S, Zhang A, Lu Y, Nasir K, Krumholz HM, Jiang L. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross‐sectional survey. Lancet. 2017;390:2559–2568. [DOI] [PubMed] [Google Scholar]
- 29. Sheriff HM, Tsimploulis A, Valentova M, Anker MS, Deedwania P, Banach M, Morgan CJ, Blackman MR, Fonarow GC, White M, Alagiakrishnan K, Allman RM, Aronow WS, Anker SD, Ahmed A. Isolated diastolic hypertension and incident heart failure in community‐dwelling older adults: insights from the Cardiovascular Health Study. Int J Cardiol. 2017;238:140–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Arima H, Anderson C, Omae T, Woodward M, Hata J, Murakami Y, Macmahon S, Neal B, Chalmers J. Effects of blood pressure lowering on major vascular events among patients with isolated diastolic hypertension: the perindopril protection against recurrent stroke study (PROGRESS) trial. Stroke. 2011;42:2339–2341. [DOI] [PubMed] [Google Scholar]
- 31. Fang XH, Zhang XH, Yang QD, Dai XY, Su FZ, Rao ML, Wu SP, Du XL, Wang WZ, Li SC. Subtype hypertension and risk of stroke in middle‐aged and older Chinese: a 10‐year follow‐up study. Stroke. 2006;37:38–43. [DOI] [PubMed] [Google Scholar]
- 32. Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons‐Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail‐Beigi F. Effects of intensive blood‐pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplemental methods.
Table S1. Baseline Characteristics of Participants With Isolated Diastolic Hypertension, by Treatment Status
Table S2. Prevalence of Isolated Diastolic Hypertension Among Treated Hypertensive Participants, by Population Characteristics
Figure S1. Flowchart of study participant selection in China Patient‐Centered Evaluative Assessment of Cardiac Events Million Persons Project.
Figure S2. Histograms of prevalence of isolated diastolic hypertension (IDH) and awareness among untreated IDH participants in 1198 mutually exclusive population subgroups (at least 200 participants each) defined priori by 10 selected characteristics.
Figure S3. Histograms prevalence of isolated diastolic hypertension (IDH) and awareness among untreated IDH participants in 731 mutually exclusive population subgroups (at least 500 participants each) defined priori by 10 selected characteristics.
Figure S4. Density plots of prevalence of isolated diastolic hypertension (IDH) among all study participants (A) and awareness among untreated IDH participants (B) in 731 mutually exclusive population subgroups (of at least 500 participants), by age, sex, prior cardiovascular events, history of diabetes mellitus, and urbanity.
Figure S5. Number of antihypertensive medications used by treated participants with isolated diastolic hypertension, by degree of diastolic blood pressure elevation.


