Key Points
Question
What is the prevalence of survival without major comorbidities in adulthood among persons born prematurely?
Findings
In this population-based cohort study of more than 2.5 million persons born in Sweden from 1973 to 1997, 54.6% of those born preterm (gestational age <37 weeks) and 22.3% of those born extremely preterm (22-27 weeks) were alive with no major comorbidities at ages 18 to 43 years, compared with 63.0% of those born full-term. The prevalences were statistically significantly lower in those born at earlier gestational ages vs full-term.
Meaning
Among Swedish persons born prematurely, a large percentage survived into adulthood and had no major comorbidities.
Abstract
Importance
Preterm birth has been associated with cardiometabolic, respiratory, and neuropsychiatric disorders in adulthood. However, the prevalence of survival without any major comorbidities is unknown.
Objective
To determine the prevalence of survival without major comorbidities in adulthood among persons born preterm vs full-term.
Design, Setting, and Participants
National cohort study of all 2 566 699 persons born in Sweden from January 1, 1973, through December 31, 1997, who had gestational age data and who were followed up for survival and comorbidities through December 31, 2015 (ages 18-43 years).
Exposures
Gestational age at birth.
Main Outcomes and Measures
Survival without major comorbidities among persons born extremely preterm (22-27 weeks), very preterm (28-33 weeks), late preterm (34-36 weeks), or early term (37-38 weeks), compared with full-term (39-41 weeks). Comorbidities were defined using the Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) Comorbidity Index, which includes conditions that commonly manifest in adolescence or young adulthood, including neuropsychiatric disorders; and the Charlson Comorbidity Index (CCI), which includes major chronic disorders predictive of mortality in adulthood. Poisson regression was used to determine prevalence ratios and differences, adjusted for potential confounders.
Results
In this study population, 48.6% were female, 5.8% were born preterm, and the median age at end of follow-up was 29.8 years (interquartile range, 12.6 years). Of all persons born preterm, 54.6% were alive with no AYA HOPE comorbidities at the end of follow-up. Further stratified, this prevalence was 22.3% for those born extremely preterm, 48.5% for very preterm, 58.0% for late preterm, 61.2% for early term, and 63.0% for full-term. These prevalences were significantly lower for earlier gestational ages vs full-term (eg, adjusted prevalence ratios: extremely preterm, 0.35 [95% CI, 0.33 to 0.36; P < .001]; all preterm, 0.86 [95% CI, 0.85 to 0.86; P < .001]; adjusted prevalence differences: extremely preterm, −0.41 [95% CI, −0.42 to −0.40; P < .001]; all preterm, −0.09 [95% CI, −0.09 to −0.09; P < .001]). Using the CCI, the corresponding prevalences were 73.1% (all preterm), 32.5% (extremely preterm), 66.4% (very preterm), 77.1% (late preterm), 80.4% (early term), and 81.8% (full-term) (adjusted prevalence ratios: extremely preterm, 0.39 [95% CI, 0.38 to 0.41; P < .001]; all preterm, 0.89 [95% CI, 0.89 to 0.89; P < .001]; adjusted prevalence differences: extremely preterm, −0.50 [95% CI, −0.51 to −0.49; P < .001]; all preterm, −0.09 [95% CI, −0.09 to −0.09; P < .001]).
Conclusions and Relevance
Among persons born preterm in Sweden between 1973 and 1997, the majority survived to early to mid-adulthood without major comorbidities. However, outcomes were worse for those born extremely preterm.
This cohort study uses data from the Swedish Birth Registry to determine the prevalence of survival without major comorbidities in adulthood among persons born preterm vs full-term in Sweden between 1973 and 1997.
Introduction
In 2014, preterm birth (gestational age <37 completed weeks) had a prevalence of 10.6% worldwide, 9.6% in the United States, and 5% to 9% in most European countries.1 Because of advances in neonatal and pediatric care, more than 95% of preterm infants in developed countries now survive into adulthood.2,3,4 Preterm birth has been associated with increased relative risks of cardiometabolic, respiratory, and neuropsychiatric disorders in adulthood.2,3,4,5,6 Despite these increased risks, most of the absolute risks are low, and it has been asserted that “most” people born prematurely remain in good health in adulthood.5,6 However, to our knowledge, the prevalence of good health in this population has never been systematically examined and remains unknown.
The few prior studies that have assessed positive outcomes in persons born preterm have focused on quality of life. Several of these have suggested that most adolescents or young adults born prematurely have a good self-reported quality of life that is commensurate with that of their full-term counterparts.7,8,9,10 However, no studies have examined survival without major comorbidities in persons born prematurely who were followed up into adulthood. A better understanding of their long-term health trajectory is needed for these patients, their families, clinicians, and policy makers.
To address this knowledge gap, a national cohort study was conducted of more than 2.5 million persons in Sweden. The specific goals were to (1) examine associations between gestational age at birth and survival without major comorbidities at ages 18 to 43 years, the maximum follow-up currently possible in this large cohort; (2) assess whether these associations differ according to birth year or sex; (3) explore for potential confounding by shared familial (genetic and/or environmental) factors using co-sibling analyses; and (4) assess education, employment, and income as additional measures of overall function and well-being in adulthood.
Methods
Study Population
The Swedish Birth Registry contains prenatal and birth information for nearly all births nationwide since 1973. The present study included all live births identified in this registry during 1973-1997. These birth years were chosen to allow sufficient follow-up into adulthood (ages ≥18 years). Individuals with missing information for gestational age (0.3%) were excluded. This study was approved by the ethics committee of Lund University in Sweden. Participant consent was not required by the ethics committee as this study used only deidentified registry-based secondary data.
Gestational Age at Birth Ascertainment
Gestational age at birth was identified from the Swedish Birth Registry based on maternal report of last menstrual period in the 1970s and ultrasound estimation starting in the 1980s and onward. This was analyzed both as a continuous variable and categorical variable with 6 groups: extremely preterm (22-27 weeks), very preterm (28-33 weeks), late preterm (34-36 weeks), early term (37-38 weeks), full-term (39-41 weeks, used as the reference group), and postterm (≥42 weeks). These categories were chosen to facilitate comparisons with prior studies of other outcomes. “Early term” was examined as a separate group because it has previously been associated with increased mortality in adulthood relative to later term births.2,11 In addition, the first 3 groups were combined to provide summary estimates for preterm birth (<37 weeks).
Outcome Ascertainment
The primary outcome was defined as survival without any comorbidities in the Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) Comorbidity Index through December 31, 2015 (maximum ages, 18 to 43 years). This index was developed specifically to assess comorbidities that commonly manifest during adolescence or young adulthood.12,13 It includes a number of conditions that have previously been associated with preterm birth, such as asthma, hypertension, diabetes, kidney disease, mental disorders, cerebral palsy, and epilepsy14,15,16,17,18,19,20,21,22,23,24,25 (see eTable 1 in the Supplement for complete list).
As a secondary outcome, survival without any comorbidities in the Charlson Comorbidity Index (CCI) was also examined. The CCI is the most extensively studied comorbidity index and has been widely used to predict mortality and disability outcomes.26 It includes 19 major comorbidities such as chronic pulmonary disease (including asthma), diabetes, and kidney or liver disease, but does not include mental disorders (see eTable 2 in the Supplement for complete list). The CCI was previously adapted for use with International Classification of Diseases (ICD) codes from administrative inpatient or outpatient data,27,28,29 which have been reported to have good agreement with CCI scores based on medical chart review.29
Survival was determined by identifying all deaths in the Swedish Death Registry, which includes deaths among all persons registered in Sweden since 1960, with compulsory reporting nationwide. AYA HOPE and CCI comorbidities were identified primarily using ICD codes (eTables 1 and 2 in the Supplement) from all diagnoses in the Swedish Hospital and Outpatient Registries. The Swedish Hospital Registry contains all primary and secondary hospital discharge diagnoses from 6 populous counties in southern Sweden starting in 1964 and with nationwide coverage starting in 1987; the Swedish Outpatient Registry contains all primary and secondary outpatient diagnoses from all specialty clinics nationwide starting in 2001. Diagnoses in the hospital registry are currently more than 99% complete and their positive predictive value has been reported to be 85% to 95% for most chronic disorders.30 Because resolution of comorbidities could not be reliably determined, any diagnosis of a comorbidity contributed to the outcome; however, most AYA HOPE and CCI conditions are likely to be chronic.
Because diagnoses from primary care settings were unavailable, nationwide pharmacy data were used to improve ascertainment of comorbidities commonly treated in primary care. The Swedish Pharmacy Register contains a record of each medication prescribed by a clinician and dispensed by any pharmacy in Sweden since July 1, 2005. All medications are classified according to the Anatomic Therapeutic Chemical (ATC) Classification System. These data were used to further ascertain the following conditions: diabetes (prescription of any medication with ATC code A10), hypertension (C02, C03, C07, C08, C09), lipid disorders (C10), thyroid disorders (H03), and asthma (both R03AC and R03BA, or R03AK04 through R03AK13 [ie, prescription of both a β2 agonist and glucocorticoid inhalant]).
As secondary outcomes, the highest education level attained during the study period (>12 vs ≤12 years) and employment (yes vs no) or high income (above vs below the cohort median) during the last 2 years of follow-up were examined. Each of these was ascertained using census data that are more than 99% complete for the national population. These outcomes may serve as additional proxies for overall function and well-being in adulthood.
Other Study Variables
Other perinatal and maternal characteristics that may be associated with gestational age at birth and comorbidities were identified using the Swedish Birth Registry and national census data, which were linked using an anonymous personal identification number. The following were included as adjustment variables: birth year (modeled simultaneously as continuous and categorical [1973-1979, 1980-1989, 1990-1997] variables), sex, fetal growth (small for gestational age [<10th percentile], appropriate for gestational age [10th-90th percentile], large for gestational age [>90th percentile]), multiple birth (singleton, twin or higher order), birth order (1, 2, ≥3), maternal age at delivery (continuous and categorical [<20, 20-29, 30-39, ≥40 years]), maternal education level (<10, 10-12, >12 years), maternal smoking (0, 1-9, ≥10 cigarettes/d), preeclampsia (ICD-8: 637; ICD-9: 624.4-624.7; ICD-10: O14-O15), other hypertensive disorders during pregnancy (ICD-8: 400-404; ICD-9: 401-405, 642.0-642.3, 642.9; ICD-10: I10-I15, O10-O11, O13, O15-O16), and diabetes during pregnancy (ICD-8: 250; ICD-9: 250, 648.0; ICD-10: E10-E14, O24). Maternal smoking was assessed at the beginning of prenatal care starting in 1982 and was available for 60.1% of women. Data were more than 99% complete for all other variables.
Statistical Analysis
Poisson regression with robust standard errors was used to compute prevalence ratios (PRs) and 95% confidence intervals (CIs) for survival without major comorbidities (ie, AYA HOPE score = 0 or CCI score = 0) and other secondary outcomes (high education, employment, high income) associated with gestational age at birth relative to full-term births. Analyses were conducted both unadjusted and adjusted for covariates (as above). Missing data for maternal smoking were multiply imputed using ordinal logistic regression to produce 20 imputations with all other covariates and the outcome as predictors.31 To account for treatment changes over time, analyses were performed after stratifying by birth decade (1973-1979, 1980-1989, 1990-1997). In secondary analyses, outcomes were also assessed after stratifying by birth decade with follow-up to age 18 years (rather than maximum possible follow-up). Potential interactions between gestational age and sex were examined on the additive and multiplicative scale. Poisson model goodness-of-fit was assessed using deviance and Pearson tests, which showed a good fit in all models.
Co-sibling analyses were performed to assess for potential confounding effects of unmeasured shared familial (genetic and/or environmental) factors. Shared environmental exposures that potentially may be associated with preterm birth and comorbidities include lifestyle factors such as diet, or ambient exposures such as passive smoking or air pollution. These analyses used Poisson fixed-effects models with a separate stratum for each family as identified by the mother’s anonymous identification number. In these models, each set of siblings had its own baseline incidence rate that reflects the family’s shared genetic and environmental factors; thus, comparisons of different gestational ages were made within the family, controlling for their shared factors. In addition, these analyses were further adjusted for the same covariates as in the main analyses.
All statistical tests were 2-sided and used an α level of .05. All analyses were conducted using Stata version 15.1 (StataCorp).
Results
A total of 2 574 537 live births were identified in Sweden during 1973-1997. Of this total, 7838 (0.3%) had missing information for gestational age and were excluded, leaving 2 566 699 persons (99.7%) for inclusion in the study. Table 1 shows perinatal and maternal characteristics by gestational age at birth. Preterm infants were more likely than full-term infants to be male, multiple births, or first-born; their mothers were more likely to be at the extremes of age, have low education level, smoke, or have preeclampsia, other hypertensive disorders, or diabetes during their pregnancy.
Table 1. Characteristics of Study Cohort by Gestational Age at Birth, Sweden, 1973-1997.
| Characteristic | No. (%) | |||||
|---|---|---|---|---|---|---|
| Preterm | Early Term (37-38 wk) | Full-term (39-41 wk) | Postterm (≥42 wk) | |||
| Extremely (22-27 wk) | Very (28-33 wk) | Late (34-36 wk) | ||||
| No. (% of total) | 5391 (0.2) | 33 025 (1.3) | 110 649 (4.3) | 447 249 (17.4) | 1 742 809 (67.9) | 227 576 (8.9) |
| Child characteristics | ||||||
| Sex | ||||||
| Male | 2938 (54.5) | 18 219 (55.2) | 60 010 (54.2) | 233 117 (52.1) | 884 793 (50.8) | 119 480 (52.5) |
| Female | 2453 (45.5) | 14 806 (44.8) | 50 639 (45.8) | 214 132 (47.9) | 858 016 (49.2) | 108 096 (47.5) |
| Fetal growth percentile | ||||||
| <10th | 26 (0.5) | 3785 (11.5) | 12 127 (11.0) | 34 862 (7.8) | 159 876 (9.2) | 46 079 (20.2) |
| 10th-90th | 5115 (94.9) | 27 779 (84.1) | 89 517 (80.9) | 361 856 (80.9) | 1 402 814 (80.5) | 166 260 (73.1) |
| >90th | 250 (4.6) | 1461 (4.4) | 9005 (8.1) | 50 531 (11.3) | 180 119 (10.3) | 15 237 (6.7) |
| Multiple birth | ||||||
| Singleton | 4259 (79.0) | 26 313 (79.7) | 95 373 (86.2) | 426 617 (95.4) | 1 731 866 (99.4) | 227 034 (99.8) |
| Twin or higher order | 1132 (21.0) | 6712 (20.3) | 15 276 (13.8) | 20 632 (4.6) | 10 943 (0.6) | 542 (0.2) |
| Birth order | ||||||
| 1 | 2348 (43.5) | 14 864 (45.0) | 49 495 (44.7) | 174 039 (38.9) | 713 237 (40.9) | 109 526 (48.1) |
| 2 | 1682 (31.2) | 10 159 (30.8) | 34 364 (31.1) | 162 534 (36.3) | 656 995 (37.7) | 75 619 (33.2) |
| ≥3 | 1361 (25.3) | 8002 (24.2) | 26 790 (24.2) | 110 676 (24.8) | 372 577 (21.4) | 42 431 (18.6) |
| Maternal characteristics | ||||||
| Age, y | ||||||
| <20 | 290 (5.4) | 1867 (5.6) | 5523 (5.0) | 16 994 (3.8) | 65 154 (3.7) | 11 250 (4.9) |
| 20-29 | 2951 (54.7) | 18 690 (56.6) | 64 691 (58.5) | 261 265 (58.4) | 1 090 254 (62.6) | 147 502 (64.8) |
| 30-39 | 2015 (37.4) | 11 649 (35.3) | 37 999 (34.3) | 158 963 (35.5) | 563 886 (32.4) | 66 380 (29.2) |
| ≥40 | 135 (2.5) | 819 (2.5) | 2436 (2.2) | 10 027 (2.2) | 23 515 (1.3) | 2444 (1.1) |
| Education, y | ||||||
| <10 | 1081 (18.9) | 6179 (18.7) | 19 760 (17.9) | 73 563 (16.5) | 260 963 (15.0) | 37 651 (16.5) |
| 10-12 | 2706 (50.2) | 16 969 (51.4) | 55 632 (50.3) | 220 961 (49.4) | 855 235 (49.1) | 111 107 (48.8) |
| >12 | 1667 (30.9) | 9877 (29.9) | 35 257 (31.9) | 152 725 (34.1) | 626 611 (35.9) | 78 818 (34.6) |
| Smoking, cigarettes/d | ||||||
| 0 | 3168 (58.8) | 19 757 (59.8) | 69 298 (62.6) | 293 373 (65.6) | 1 145 634 (65.7) | 137 123 (60.3) |
| 1-9 | 1795 (33.3) | 10 628 (32.2) | 33 272 (30.1) | 123 686 (27.6) | 505 789 (29.0) | 81 573 (35.8) |
| ≥10 | 428 (7.9) | 2640 (8.0) | 8079 (7.3) | 30 190 (6.8) | 91 386 (5.2) | 8880 (3.9) |
| Preeclampsia | 420 (7.8) | 4520 (13.7) | 11 321 (10.2) | 28 430 (6.4) | 73 625 (4.2) | 10 196 (4.5) |
| Other hypertensive disorders | 45 (0.8) | 439 (1.3) | 1209 (1.1) | 4041 (0.9) | 10 517 (0.6) | 1001 (0.4) |
| Diabetes mellitus | 21 (0.4) | 267 (0.8) | 1175 (1.1) | 3059 (0.7) | 3525 (0.2) | 167 (0.1) |
Attained ages at the end of follow-up ranged from 18 to 43 years (mean, 30.3 [SD, 7.2]; median, 29.8 [interquartile range, 12.6]; 48.6% female). A total of 149 065 persons (5.8%) were born preterm, of whom 94.2% survived to adulthood (age ≥18 years). The percentage of preterm infants who survived to adulthood increased over time, from 91.1% of those born in 1973-1979, to 94.7% of those born in 1980-1989, to 95.7% of those born in 1990-1997 (Table 2).
Table 2. Prevalence of Survival Without Major Comorbidities in Adulthood by Gestational Age at Birth and Birth Year, Sweden.
| Gestational Age at Birth | Total Births, No. | Survival | Survival and AYA HOPE Score = 0 | Survival and CCI Score = 0 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Age 18 y, % | End of Follow-up, % | Age 18 y, % | End of Follow-upa | Age 18 y, % | End of Follow-upb | ||||
| % | PR (95% CI)c | % | PR (95% CI)c | ||||||
| 1973-1997 | |||||||||
| All births, 1973-1997 (attained ages 18-43 y; median, 29.8 y) | 2 566 699 | 99.1 | 98.5 | 85.5 | 62.1 | 84.6 | 81.1 | ||
| Preterm (<37 wk) | 149 065 | 94.2 | 93.5 | 76.6 | 54.6 | 0.86 (0.85-0.86) | 76.9 | 73.1 | 0.89 (0.89-0.89) |
| Extremely (22-27 wk) | 5391 | 51.3 | 50.8 | 31.4 | 22.3 | 0.35 (0.33-0.36) | 36.3 | 32.5 | 0.39 (0.38-0.41) |
| Very (28-33 wk) | 33 025 | 89.5 | 88.8 | 68.4 | 48.5 | 0.76 (0.75-0.77) | 70.9 | 66.4 | 0.81 (0.80-0.81) |
| Late (34-36 wk) | 110 649 | 97.7 | 97.0 | 81.3 | 58.0 | 0.91 (0.91-0.92) | 80.7 | 77.1 | 0.94 (0.94-0.94) |
| Early term (37-38 wk) | 447 249 | 99.1 | 98.5 | 84.0 | 61.2 | 0.97 (0.96-0.97) | 83.8 | 80.4 | 0.98 (0.98-0.98) |
| Full-term (39-41 wk) | 1 742 809 | 99.4 | 98.9 | 86.2 | 63.0 | 1 [Reference] | 85.3 | 81.8 | 1 [Reference] |
| Postterm (≥42 wk) | 227 576 | 99.3 | 98.6 | 88.1 | 62.2 | 1.00 (0.99-1.00) | 85.5 | 81.5 | 1.00 (1.00-1.00) |
| Per additional wkd | 1.02 (1.02-1.02) | 1.02 (1.02-1.02) | |||||||
| 1973-1979 | |||||||||
| Born 1973-1979 (attained ages 36-43 y; median, 39.7 y) | 699 473 | 98.8 | 97.7 | 94.9 | 59.9 | 85.9 | 80.0 | ||
| Preterm (<37 wk) | 35 636 | 91.1 | 89.7 | 85.8 | 51.7 | 0.84 (0.83-0.85) | 77.2 | 70.9 | 0.87 (0.87-0.88) |
| Extremely (22-27 wk) | 1155 | 30.0 | 29.3 | 26.6 | 15.3 | 0.25 (0.21-0.28) | 24.9 | 21.4 | 0.26 (0.23-0.29) |
| Very (28-33 wk) | 7869 | 81.3 | 79.9 | 74.5 | 43.1 | 0.69 (0.68-0.71) | 67.7 | 61.2 | 0.75 (0.74-0.77) |
| Late (34-36 wk) | 26 612 | 96.6 | 95.2 | 91.7 | 55.8 | 0.91 (0.90-0.92) | 82.3 | 75.9 | 0.94 (0.93-0.94) |
| Early term (37-38 wk) | 98 895 | 98.8 | 97.6 | 94.6 | 59.3 | 0.96 (0.96-0.97) | 85.4 | 79.6 | 0.98 (0.98-0.98) |
| Full-term (39-41 wk) | 475 210 | 99.3 | 98.3 | 95.6 | 60.7 | 1 [Reference] | 86.6 | 80.8 | 1 [Reference] |
| Postterm (≥42 wk) | 89 732 | 99.2 | 98.1 | 95.4 | 59.9 | 1.00 (1.00-1.01) | 86.3 | 80.4 | 1.00 (1.00-1.00) |
| Per additional wkd | 1.02 (1.02-1.02) | 1.02 (1.02-1.02) | |||||||
| 1980-1989 | |||||||||
| Born 1980-1989 (attained ages 26-35 y; median, 30.7 y) | 989 229 | 99.1 | 98.5 | 89.6 | 62.4 | 86.0 | 82.2 | ||
| Preterm (<37 wk) | 60 203 | 94.7 | 93.9 | 82.1 | 55.6 | 0.87 (0.87-0.88) | 79.4 | 75.2 | 0.91 (0.90-0.91) |
| Extremely (22-27 wk) | 1957 | 50.9 | 50.2 | 35.6 | 22.8 | 0.36 (0.33-0.39) | 38.3 | 33.9 | 0.41 (0.38-0.43) |
| Very (28-33 wk) | 12 760 | 90.2 | 89.4 | 73.9 | 49.6 | 0.78 (0.76-0.79) | 73.7 | 68.6 | 0.83 (0.82-0.83) |
| Late (34-36 wk) | 45 486 | 97.9 | 97.1 | 86.4 | 58.8 | 0.92 (0.91-0.93) | 82.7 | 78.8 | 0.95 (0.94-0.95) |
| Early term (37-38 wk) | 186 892 | 99.2 | 98.5 | 88.8 | 61.5 | 0.97 (0.96-0.97) | 85.4 | 81.6 | 0.98 (0.98-0.99) |
| Full-term (39-41 wk) | 665 583 | 99.5 | 98.8 | 90.4 | 63.2 | 1 [Reference] | 86.7 | 82.9 | 1 [Reference] |
| Postterm (≥42 wk) | 76 551 | 99.3 | 98.6 | 90.7 | 62.9 | 0.99 (0.99-1.00) | 86.7 | 82.8 | 1.00 (1.00-1.00) |
| Per additional wkd | 1.02 (1.02-1.02) | 1.02 (1.01-1.02) | |||||||
| 1990-1997 | |||||||||
| Born 1990-1997 (attained ages 18-25 y; median, 22.5 y) | 877 997 | 99.3 | 99.1 | 73.1 | 63.6 | 81.8 | 80.6 | ||
| Preterm (<37 wk) | 53 226 | 95.7 | 95.6 | 64.2 | 55.4 | 0.85 (0.85-0.86) | 74.0 | 72.3 | 0.89 (0.88-0.89) |
| Extremely (22-27 wk) | 2279 | 62.5 | 62.3 | 30.2 | 25.4 | 0.39 (0.36-0.41) | 40.4 | 37.0 | 0.45 (0.43-0.47) |
| Very (28-33 wk) | 12 396 | 94.0 | 93.9 | 58.8 | 50.8 | 0.78 (0.76-0.79) | 69.9 | 67.4 | 0.82 (0.81-0.83) |
| Late (34-36 wk) | 38 551 | 98.3 | 98.1 | 68.0 | 58.7 | 0.90 (0.89-0.91) | 77.3 | 76.0 | 0.93 (0.92-0.94) |
| Early term (37-38 wk) | 161 462 | 99.3 | 99.2 | 71.9 | 62.1 | 0.96 (0.96-0.96) | 80.8 | 79.6 | 0.98 (0.97-0.98) |
| Full-term (39-41 wk) | 602 016 | 99.6 | 99.4 | 74.2 | 64.6 | 1 [Reference] | 82.7 | 81.5 | 1 [Reference] |
| Postterm (≥42 wk) | 61 293 | 99.5 | 99.3 | 74.1 | 64.6 | 1.00 (0.99-1.00) | 82.9 | 81.6 | 1.00 (1.00-1.01) |
| Per additional wkd | 1.02 (1.02-1.02) | 1.02 (1.02-1.02) | |||||||
Abbreviations: AYA HOPE, Adolescent and Young Adult Health Outcomes and Patient Experience; CCI, Charlson Comorbidity Index; PR, prevalence ratio.
Survival without any comorbidities in the AYA HOPE Comorbidity Index through 2015.
Survival without any comorbidities in the CCI through 2015.
Adjusted for child characteristics (birth year, sex, fetal growth, multiple birth, birth order) and maternal characteristics (age, education, smoking, preeclampsia, other hypertensive disorders, diabetes).
Per additional 1 week of gestation.
Survival Without Major Comorbidities in Adulthood
Using the AYA HOPE Comorbidity Index, 62.1% of persons in the entire cohort were alive without major comorbidities at the end of follow-up (Table 2). The corresponding prevalences by gestational age at birth were 54.6% for all preterm, 22.3% for extremely preterm, 48.5% for very preterm, 58.0% for late preterm, 61.2% for early term, 63.0% for full-term, and 62.2% for postterm. Using the CCI, the overall prevalence of survival without major comorbidities was higher (81.1%), because this index excludes several common conditions that are in the AYA HOPE index (eg, hypertension and mental disorders). The corresponding CCI-based prevalences by gestational age at birth were 73.1% for all preterm, 32.5% for extremely preterm, 66.4% for very preterm, 77.1% for late preterm, 80.4% for early term, 81.8% for full-term, and 81.5% for postterm.
Except for postterm births, the prevalences of survival without major comorbidities were significantly lower among all gestational age groups compared with full-term births. For example, based on the AYA HOPE index and CCI, respectively, the adjusted PRs were 0.86 (95% CI, 0.85 to 0.86) and 0.89 (95% CI, 0.89 to 0.89) for all preterm, 0.76 (95% CI, 0.75 to 0.77) and 0.81 (95% CI, 0.80 to 0.81) for very preterm, and 0.35 (95% CI, 0.33 to 0.36) and 0.39 (95% CI, 0.38 to 0.41) for extremely preterm, compared with full-term (P < .001 for each) (Table 2). The adjusted prevalence differences using the AYA HOPE index and CCI, respectively, were −0.09 (95% CI, −0.09 to −0.09) and −0.09 (95% CI, −0.09 to −0.09) for all preterm, −0.15 (95% CI, −0.16 to −0.15) and −0.16 (95% CI, −0.16 to −0.15) for very preterm, and −0.41 (95% CI, −0.42 to −0.40) and −0.50 (95% CI, −0.51 to −0.49) for extremely preterm, compared with full-term (P < .001 for each). When gestational age was modeled as a continuous variable, the adjusted PR for survival without major comorbidities per each additional week of gestation was 1.02 (95% CI, 1.02 to 1.02; P < .001), based on either the AYA HOPE index or CCI (Table 2). All adjusted results were nearly the same as unadjusted results (eTable 3 in the Supplement); ie, neither birth year nor any other variables in Table 1 were important confounders.
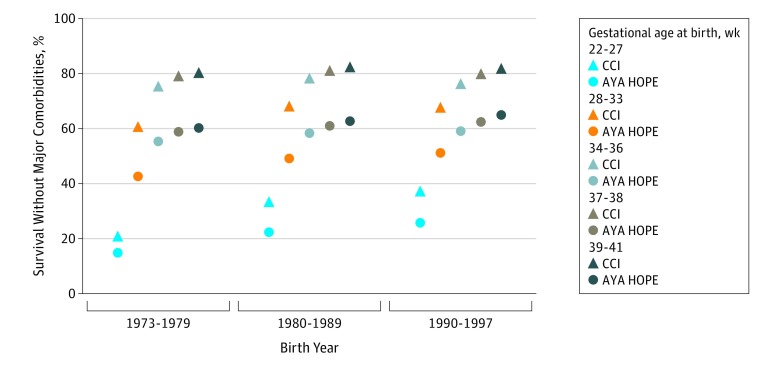
When stratifying by birth decade, most findings were very similar to the overall results. For example, using the AYA HOPE index, the prevalence of survival without major comorbidities among persons born preterm was 51.7% for those born in 1973-1979, 55.6% for those born in 1980-1989, and 55.4% for those born in 1990-1997; using the CCI, the corresponding prevalences were 70.9%, 75.2%, and 72.3%. Among persons born extremely preterm, 15.3% of those born in 1973-1979 were alive without AYA HOPE comorbidities at the end of follow-up, compared with 22.8% of those born in 1980-1989 and 25.4% of those born in 1990-1997. Using the CCI, the corresponding prevalences for successive birth decades were 21.4%, 33.9%, and 37.0%, respectively (Table 2). The Figure shows the prevalence of survival without major comorbidities in adulthood by gestational age at birth and birth year.
Figure. Prevalence of Survival Without Major Comorbidities.
Based on the Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) Comorbidity Index and Charlson Comorbidity Index (CCI) at ages 18 to 43 years. Total Ns are reported in Table 2.
In secondary analyses, the outcomes were assessed after stratifying by birth decade with follow-up of each birth cohort to age 18 years, rather than maximum follow-up to the end of 2015 (eTable 4 in the Supplement). Using the AYA HOPE index, the prevalence of survival without major comorbidities among all persons born preterm was 76.6% at age 18 years, compared with 54.6% at the end of follow-up (median age, 29.8 years) (Table 2). However, this difference appeared to be driven by the unavailability of outpatient data until after age 18 years for the earliest birth cohorts (eg, 1973-1979). Several comorbidities included in the AYA HOPE index are commonly treated in outpatient settings (eg, hypertension, mood and anxiety disorders), from which data were unavailable until 2001 and later. The results based on the CCI were little changed compared with the main analyses (Table 2; complete results in eTable 4 in the Supplement).
Prevalences of specific comorbidities by gestational age at birth are reported in eTables 5 and 6 in the Supplement. The most common AYA HOPE and CCI comorbidity in the entire cohort and among those born preterm was asthma. Asthma prevalences by gestational age at birth were 15.0% for all preterm, 12.5% for extremely preterm, 16.2% for very preterm, 14.8% for late preterm, 13.5% for early term, 12.5% for full-term, and 12.1% for postterm.
Interactions
Interactions between gestational age at birth and sex are reported in eTables 7A and 7B in the Supplement. Using the AYA HOPE index, a positive interaction was found on the additive but not multiplicative scale. The prevalence of survival without major comorbidities was lower among women, but this difference was slightly greater among persons born full-term than those born preterm (eTable 7A in the Supplement). The stronger association of preterm birth with adverse outcomes in men resulted in a modestly positive additive interaction (ie, the combined association of preterm birth and sex with the outcome exceeded the sum of their separate associations; P < .001). Using the CCI, positive additive and multiplicative interactions were observed (P < .001 for each) (eTable 7B in the Supplement). The positive additive interactions suggest that preterm birth was associated with adverse outcomes in significantly more men than women.
Co-sibling Analyses
A total of 2 163 208 persons (84.3%) had at least 1 sibling and were included in co-sibling analyses to control for unmeasured shared familial factors. The results were little changed compared with the main analyses (eTable 8 in the Supplement). For example, across all birth years examined, the adjusted PR based on the AYA HOPE index and comparing preterm vs full-term was 0.88 (95% CI, 0.87 to 0.88) in the co-sibling analysis and 0.86 (95% CI, 0.85 to 0.86) in the main analysis. The corresponding PRs based on the CCI were 0.90 (95% CI, 0.89 to 0.90) in the co-sibling analysis and 0.89 (95% CI, 0.89 to 0.89) in the main analysis. The results after stratifying by birth decade also were very similar in the co-sibling (eTable 8 in the Supplement) vs main (Table 2) analyses.
Socioeconomic Outcomes
Adults born preterm were slightly less likely to have a high education level, be employed, or have high income compared with those born full-term (Table 3). In the entire cohort, the prevalence of high education level (>12 years) was 33.5% in persons born preterm and 23.0% in those born extremely preterm, compared with 37.2% in those born full-term. The corresponding prevalences for employment were 84.8% and 40.7%, compared with 91.6%, and for high income (above the cohort median) were 47.8% and 37.0%, compared with 50.2%. These findings were similar across all birth decades except for lower prevalences of high education or income, as expected, in the youngest birth cohort. Further adjustment for comorbidities had little effect on these findings (eg, adjusted PRs comparing preterm with full-term: high education, 0.96 [95% CI, 0.95 to 0.97]; employment, 0.93 [95% CI, 0.93 to 0.93]; high income, 0.97 [95% CI, 0.96 to 0.97]), compared with the main results in Table 3.
Table 3. Education Level, Employment, and Income by Gestational Age at Birth and Birth Year After Follow-up Through 2015, Sweden.
| Gestational Age at Birth | Total Births, No. | Education >12 y | Employed | Income >Cohort Median | |||
|---|---|---|---|---|---|---|---|
| % | PR (95% CI)a | % | PR (95% CI)a | % | PR (95% CI)a | ||
| 1973-1997 | |||||||
| All births, 1973-1997 (attained ages 18-43 y; median, 29.8 y) | 2 566 699 | 36.9 | 91.0 | 50.0 | |||
| Preterm (<37 wk) | 149 065 | 33.5 | 0.95 (0.95-0.96) | 84.8 | 0.93 (0.93-0.93) | 47.8 | 0.96 (0.95-0.96) |
| Extremely (22-27 wk) | 5391 | 23.0 | 0.74 (0.70-0.79) | 40.7 | 0.45 (0.43-0.46) | 37.0 | 0.79 (0.76-0.83) |
| Very (28-33 wk) | 33 025 | 31.0 | 0.91 (0.90-0.93) | 79.2 | 0.87 (0.86-0.87) | 45.9 | 0.93 (0.92-0.94) |
| Late (34-36 wk) | 110 649 | 34.4 | 0.97 (0.96-0.97) | 88.6 | 0.97 (0.97-0.97) | 48.6 | 0.97 (0.96-0.98) |
| Early term (37-38 wk) | 447 249 | 35.6 | 0.99 (0.99-0.99) | 90.6 | 0.99 (0.99-0.99) | 49.1 | 0.99 (0.98-0.99) |
| Full-term (39-41 wk) | 1 742 809 | 37.2 | 1 [Reference] | 91.6 | 1 [Reference] | 50.2 | 1 [Reference] |
| Postterm (≥42 wk) | 227 576 | 38.8 | 0.98 (0.97-0.99) | 91.4 | 1.00 (1.00-1.00) | 51.3 | 0.99 (0.98-0.99) |
| 1973-1979 | |||||||
| Born 1973-1979 (attained ages 36-43 y; median, 39.7 y) | 699 473 | 48.0 | 91.3 | 57.4 | |||
| Preterm (<37 wk) | 35 636 | 43.0 | 0.92 (0.90-0.93) | 82.9 | 0.91 (0.90-0.91) | 56.5 | 0.96 (0.95-0.97) |
| Extremely (22-27 wk) | 1155 | 32.8 | 0.70 (0.60-0.81) | 26.1 | 0.29 (0.26-0.31) | 50.5 | 0.88 (0.79-0.98) |
| Very (28-33 wk) | 7869 | 40.9 | 0.88 (0.85-0.90) | 73.5 | 0.80 (0.79-0.81) | 56.0 | 0.95 (0.93-0.97) |
| Late (34-36 wk) | 26 612 | 43.7 | 0.93 (0.92-0.94) | 88.1 | 0.96 (0.96-0.97) | 56.7 | 0.97 (0.96-0.98) |
| Early term (37-38 wk) | 98 895 | 47.3 | 0.98 (0.97-0.99) | 90.9 | 0.99 (0.99-0.99) | 57.8 | 0.99 (0.98-0.99) |
| Full-term (39-41 wk) | 475 210 | 48.8 | 1 [Reference] | 91.9 | 1 [Reference] | 57.6 | 1 [Reference] |
| Postterm (≥42 wk) | 89 732 | 46.8 | 0.99 (0.98-1.00) | 92.0 | 1.00 (1.00-1.01) | 56.6 | 0.99 (0.98-1.00) |
| 1980-1989 | |||||||
| Born 1980-1989 (attained ages 26-35 y; median, 30.7 y) | 989 229 | 45.9 | 93.0 | 56.0 | |||
| Preterm (<37 wk) | 60 203 | 42.5 | 0.95 (0.94-0.96) | 87.4 | 0.94 (0.93-0.94) | 55.0 | 0.97 (0.96-0.98) |
| Extremely (22-27 wk) | 1957 | 32.6 | 0.73 (0.67-0.80) | 42.3 | 0.45 (0.43-0.48) | 44.3 | 0.79 (0.74-0.85) |
| Very (28-33 wk) | 12 760 | 40.0 | 0.91 (0.89-0.93) | 82.1 | 0.88 (0.87-0.89) | 53.3 | 0.94 (0.92-0.95) |
| Late (34-36 wk) | 45 486 | 43.4 | 0.97 (0.96-0.98) | 90.8 | 0.97 (0.97-0.98) | 55.6 | 0.98 (0.97-0.99) |
| Early term (37-38 wk) | 186 892 | 45.0 | 0.98 (0.98-0.99) | 92.8 | 0.99 (0.99-0.99) | 55.9 | 0.99 (0.99-1.00) |
| Full-term (39-41 wk) | 665 583 | 46.5 | 1 [Reference] | 93.5 | 1 [Reference] | 56.1 | 1 [Reference] |
| Postterm (≥42 wk) | 76 551 | 46.1 | 0.98 (0.98-0.99) | 93.0 | 1.00 (1.00-1.00) | 55.9 | 0.99 (0.99-1.00) |
| 1990-1997 | |||||||
| Born 1990-1997 (attained ages 18-25 y; median, 22.5 y) | 877 997 | 17.6 | 88.5 | 37.6 | |||
| Preterm (<37 wk) | 53 226 | 17.1 | 0.99 (0.97-1.01) | 83.1 | 0.93 (0.93-0.94) | 34.7 | 0.93 (0.92-0.94) |
| Extremely (22-27 wk) | 2279 | 13.9 | 0.80 (0.71-0.90) | 46.8 | 0.52 (0.50-0.55) | 28.8 | 0.77 (0.71-0.84) |
| Very (28-33 wk) | 12 396 | 16.4 | 0.97 (0.93-1.01) | 79.9 | 0.90 (0.89-0.90) | 33.4 | 0.90 (0.88-0.93) |
| Late (34-36 wk) | 38 551 | 17.4 | 1.00 (0.98-1.03) | 86.2 | 0.97 (0.96-0.97) | 35.3 | 0.94 (0.93-0.96) |
| Early term (37-38 wk) | 161 462 | 17.3 | 0.99 (0.98-1.01) | 87.9 | 0.99 (0.98-0.99) | 36.3 | 0.96 (0.95-0.97) |
| Full-term (39-41 wk) | 602 016 | 17.7 | 1 [Reference] | 89.2 | 1 [Reference] | 38.1 | 1 [Reference] |
| Postterm (≥42 wk) | 61 293 | 17.7 | 0.97 (0.96-0.99) | 88.6 | 1.00 (1.00-1.00) | 38.3 | 1.00 (0.99-1.01) |
Abbreviation: PR, prevalence ratio.
Adjusted for child characteristics (birth year, sex, fetal growth, multiple birth, birth order) and maternal characteristics (age, education, smoking, preeclampsia, other hypertensive disorders, diabetes).
Discussion
In this large national cohort study, 54.6% of persons born preterm and 22.3% of those born extremely preterm were alive without major comorbidities at ages 18 to 43 years, compared with 63.0% of those born full-term. The prevalences of this outcome were statistically significantly lower in those born at earlier gestational ages vs full-term. These findings were similar among men and women and were independent of birth year and other perinatal or maternal factors. In addition, co-sibling analyses suggested that the findings were not attributable to shared genetic or environmental factors in families.
Prior studies of long-term sequelae of preterm birth have focused almost entirely on specific adverse outcomes, either physical, mental, or social. Such studies have reported that persons born prematurely have increased risks of cardiometabolic,16,17,18,19,20 respiratory,14,15 and neuropsychiatric22,23,24,25 disorders; social adversity32; and premature mortality2,3,11,32 in young adulthood. Potential positive outcomes or indicators of resilience have rarely been assessed. A few clinical follow-up studies have examined self-reported quality of life in adolescents or young adults born prematurely with very or extremely low birth weight (<1500 or <1000 g).7,8,9,10 Such studies have suggested that despite having more functional limitations, most of these individuals reported a high subjective quality of life that was similar to that of their full-term or normal birth weight counterparts.7,8,9,10 Positive educational outcomes have also been explored. A New Zealand cohort study of 613 521 children reported that most of those born extremely preterm had positive educational outcomes in primary or secondary school that were commensurate with those of full-term children33; however, this was in contrast to other reports of lower educational performance or attainment.32,34,35
To our knowledge, the present study provides the first population-based estimates of the prevalence of survival without major comorbidities in adults born prematurely. The relatively high prevalence of this outcome reflects not only the treatment advances that have occurred over the past 50 years but also the apparent resilience of preterm survivors in maintaining good health.5 However, those born at the earliest gestational ages face significantly greater long-term challenges. Persons born very or extremely preterm were not only significantly more likely to have major comorbidities but less likely to have high education, employment, or high income in adulthood. Additional studies are needed to identify protective factors across the life course that enhance resilience and the long-term health trajectory of persons born prematurely, particularly at the earliest gestational ages. A life-course approach to health has been declared a major priority by the World Health Organization36 and will be essential for monitoring and promoting the health of preterm birth survivors across the lifespan.
A key strength of the present study was the ability to assess an extensive range of comorbidities in a large cohort with follow-up into early to mid-adulthood, using birth, medical, and pharmacy registry data that were prospectively collected and highly complete. This study design minimizes potential selection or ascertainment biases and enables more robust estimates based on a national population. The results were controlled for other perinatal and maternal factors, as well as unmeasured shared familial factors using co-sibling analyses.
Limitations
This study has several limitations. First, detailed clinical data were unavailable to validate comorbidities. Administrative ICD codes are known to underascertain many chronic disorders, especially milder cases.29 However, diagnoses in the Swedish Hospital Registry have been reported to have high validity for most conditions,30 and Sweden’s universal health system also reduces disparities in health care access, which may improve ascertainment of many chronic disorders in the general population. Second, outpatient data were available only since 2001 from specialty clinics. This limitation was partially reduced by using pharmacy data to further ascertain comorbidities commonly treated in primary care. Third, diagnostic changes and different ICD versions may limit comparability of results across the study period. Fourth, despite having up to 43 years of follow-up, this was still a relatively young cohort. Additional follow-up will be needed to assess these outcomes among preterm survivors in older adulthood, as well as in later birth cohorts when such data become available.
Conclusions
Among persons born preterm in Sweden between 1973 and 1997, the majority survived to early to mid-adulthood without major comorbidities. However, outcomes were worse for those born extremely preterm.
eTable 1. International Classification of Diseases (ICD) Codes for Diagnoses in the AYA HOPE Comorbidity Index
eTable 2. International Classification of Diseases (ICD) Codes for Diagnoses in the Charlson Comorbidity Index (CCI)
eTable 3. Unadjusted Prevalence Ratios for Survival Without Major Comorbidities in Adulthood by Gestational Age at Birth and Birth Year, Sweden
eTable 4. Prevalence of Survival Without Major Comorbidities at Age 18 Years by Gestational Age at Birth and Birth Year, Sweden
eTable 5. Prevalence of AYA HOPE Comorbidity Index Diagnoses at Ages 18-43 Years by Gestational Age at Birth
eTable 6. Prevalence of Charlson Comorbidity Index Diagnoses at Ages 18-43 Years by Gestational Age at Birth
eTable 7A. Interactions Between Gestational Age at Birth and Sex in Relation to Survival Without Any AYA HOPE Comorbidities at Ages 18-43 Years
eTable 7B. Interactions Between Gestational Age at Birth and Sex in Relation to Survival Without Any CCI Comorbidities at Ages 18-43 Years
eTable 8. Co-sibling Analyses for Associations Between Gestational Age at Birth (1973-1997) and Survival Without Major Comorbidities Through 2015, Sweden
References
- 1.Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7(1):e37-e46. doi: 10.1016/S2214-109X(18)30451-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crump C, Sundquist J, Winkleby MA, Sundquist K. Gestational age at birth and mortality from infancy into mid-adulthood: a national cohort study. Lancet Child Adolesc Health. 2019;3(6):408-417. doi: 10.1016/S2352-4642(19)30108-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crump C, Sundquist K, Sundquist J, Winkleby MA. Gestational age at birth and mortality in young adulthood. JAMA. 2011;306(11):1233-1240. doi: 10.1001/jama.2011.1331 [DOI] [PubMed] [Google Scholar]
- 4.Raju TNK, Pemberton VL, Saigal S, Blaisdell CJ, Moxey-Mims M, Buist S; Adults Born Preterm Conference Speakers and Discussants . Long-term healthcare outcomes of preterm birth: an executive summary of a conference sponsored by the National Institutes of Health. J Pediatr. 2017;181:309-318. doi: 10.1016/j.jpeds.2016.10.015 [DOI] [PubMed] [Google Scholar]
- 5.Raju TNK, Buist AS, Blaisdell CJ, Moxey-Mims M, Saigal S. Adults born preterm: a review of general health and system-specific outcomes. Acta Paediatr. 2017;106(9):1409-1437. doi: 10.1111/apa.13880 [DOI] [PubMed] [Google Scholar]
- 6.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261-269. doi: 10.1016/S0140-6736(08)60136-1 [DOI] [PubMed] [Google Scholar]
- 7.Saigal S, Feeny D, Rosenbaum P, Furlong W, Burrows E, Stoskopf B. Self-perceived health status and health-related quality of life of extremely low-birth-weight infants at adolescence. JAMA. 1996;276(6):453-459. doi: 10.1001/jama.1996.03540060029031 [DOI] [PubMed] [Google Scholar]
- 8.Saigal S, Stoskopf B, Pinelli J, et al. Self-perceived health-related quality of life of former extremely low birth weight infants at young adulthood. Pediatrics. 2006;118(3):1140-1148. doi: 10.1542/peds.2006-0119 [DOI] [PubMed] [Google Scholar]
- 9.Dinesen SJ, Greisen G. Quality of life in young adults with very low birth weight. Arch Dis Child Fetal Neonatal Ed. 2001;85(3):F165-F169. doi: 10.1136/fn.85.3.F165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bjerager M, Steensberg J, Greisen G. Quality of life among young adults born with very low birthweights. Acta Paediatr. 1995;84(12):1339-1343. doi: 10.1111/j.1651-2227.1995.tb13565.x [DOI] [PubMed] [Google Scholar]
- 11.Crump C, Sundquist K, Winkleby MA, Sundquist J. Early-term birth (37-38 weeks) and mortality in young adulthood. Epidemiology. 2013;24(2):270-276. doi: 10.1097/EDE.0b013e318280da0f [DOI] [PubMed] [Google Scholar]
- 12.Parsons HM, Harlan LC, Seibel NL, Stevens JL, Keegan TH. Clinical trial participation and time to treatment among adolescents and young adults with cancer: does age at diagnosis or insurance make a difference? J Clin Oncol. 2011;29(30):4045-4053. doi: 10.1200/JCO.2011.36.2954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu XC, Prasad PK, Landry I, et al. ; AYA HOPE Study Collaborative Group . Impact of the AYA HOPE Comorbidity Index on assessing health care service needs and health status among adolescents and young adults with cancer. Cancer Epidemiol Biomarkers Prev. 2015;24(12):1844-1849. doi: 10.1158/1055-9965.EPI-15-0401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crump C, Winkleby MA, Sundquist J, Sundquist K. Risk of asthma in young adults who were born preterm: a Swedish national cohort study. Pediatrics. 2011;127(4):e913-e920. doi: 10.1542/peds.2010-2603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vollsæter M, Røksund OD, Eide GE, Markestad T, Halvorsen T. Lung function after preterm birth: development from mid-childhood to adulthood. Thorax. 2013;68(8):767-776. doi: 10.1136/thoraxjnl-2012-202980 [DOI] [PubMed] [Google Scholar]
- 16.de Jong F, Monuteaux MC, van Elburg RM, Gillman MW, Belfort MB. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension. 2012;59(2):226-234. doi: 10.1161/HYPERTENSIONAHA.111.181784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crump C, Winkleby MA, Sundquist K, Sundquist J. Risk of hypertension among young adults who were born preterm: a Swedish national study of 636,000 births. Am J Epidemiol. 2011;173(7):797-803. doi: 10.1093/aje/kwq440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hofman PL, Regan F, Jackson WE, et al. Premature birth and later insulin resistance. N Engl J Med. 2004;351(21):2179-2186. doi: 10.1056/NEJMoa042275 [DOI] [PubMed] [Google Scholar]
- 19.Crump C, Winkleby MA, Sundquist K, Sundquist J. Risk of diabetes among young adults born preterm in Sweden. Diabetes Care. 2011;34(5):1109-1113. doi: 10.2337/dc10-2108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Markopoulou P, Papanikolaou E, Analytis A, Zoumakis E, Siahanidou T. Preterm birth as a risk factor for metabolic syndrome and cardiovascular disease in adult life: a systematic review and meta-analysis. J Pediatr. 2019;210:69-80. doi: 10.1016/j.jpeds.2019.02.041 [DOI] [PubMed] [Google Scholar]
- 21.Crump C, Sundquist J, Winkleby MA, Sundquist K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ. 2019;365:1346. doi: 10.1136/bmj.l1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nosarti C, Reichenberg A, Murray RM, et al. Preterm birth and psychiatric disorders in young adult life. Arch Gen Psychiatry. 2012;69(6):E1-E8. doi: 10.1001/archgenpsychiatry.2011.1374 [DOI] [PubMed] [Google Scholar]
- 23.Crump C, Winkleby MA, Sundquist K, Sundquist J. Preterm birth and psychiatric medication prescription in young adulthood: a Swedish national cohort study. Int J Epidemiol. 2010;39(6):1522-1530. doi: 10.1093/ije/dyq103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Jong M, Verhoeven M, van Baar AL. School outcome, cognitive functioning, and behaviour problems in moderate and late preterm children and adults: a review. Semin Fetal Neonatal Med. 2012;17(3):163-169. doi: 10.1016/j.siny.2012.02.003 [DOI] [PubMed] [Google Scholar]
- 25.Crump C, Sundquist K, Winkleby MA, Sundquist J. Preterm birth and risk of epilepsy in Swedish adults. Neurology. 2011;77(14):1376-1382. doi: 10.1212/WNL.0b013e318231528f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 27.Perkins AJ, Kroenke K, Unützer J, et al. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57(10):1040-1048. doi: 10.1016/j.jclinepi.2004.03.002 [DOI] [PubMed] [Google Scholar]
- 28.Yurkovich M, Avina-Zubieta JA, Thomas J, Gorenchtein M, Lacaille D. A systematic review identifies valid comorbidity indices derived from administrative health data. J Clin Epidemiol. 2015;68(1):3-14. doi: 10.1016/j.jclinepi.2014.09.010 [DOI] [PubMed] [Google Scholar]
- 29.Stavem K, Hoel H, Skjaker SA, Haagensen R. Charlson Comorbidity Index derived from chart review or administrative data: agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017;9:311-320. doi: 10.2147/CLEP.S133624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987. doi: 10.1002/9780470316696 [DOI] [Google Scholar]
- 32.D’Onofrio BM, Class QA, Rickert ME, Larsson H, Långström N, Lichtenstein P. Preterm birth and mortality and morbidity: a population-based quasi-experimental study. JAMA Psychiatry. 2013;70(11):1231-1240. doi: 10.1001/jamapsychiatry.2013.2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry MJ, Foster T, Rowe K, Robertson O, Robson B, Pierse N. Gestational age, health, and educational outcomes in adolescents. Pediatrics. 2018;142(5):1-12. doi: 10.1542/peds.2018-1016 [DOI] [PubMed] [Google Scholar]
- 34.Chan E, Quigley MA. School performance at age 7 years in late preterm and early term birth: a cohort study. Arch Dis Child Fetal Neonatal Ed. 2014;99(6):F451-F457. doi: 10.1136/archdischild-2014-306124 [DOI] [PubMed] [Google Scholar]
- 35.van Baar AL, Vermaas J, Knots E, de Kleine MJ, Soons P. Functioning at school age of moderately preterm children born at 32 to 36 weeks’ gestational age. Pediatrics. 2009;124(1):251-257. doi: 10.1542/peds.2008-2315 [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization The Minsk Declaration: The Life-course Approach in the Context of Health 2020. Copenhagen, Denmark: WHO Regional Office for Europe; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. International Classification of Diseases (ICD) Codes for Diagnoses in the AYA HOPE Comorbidity Index
eTable 2. International Classification of Diseases (ICD) Codes for Diagnoses in the Charlson Comorbidity Index (CCI)
eTable 3. Unadjusted Prevalence Ratios for Survival Without Major Comorbidities in Adulthood by Gestational Age at Birth and Birth Year, Sweden
eTable 4. Prevalence of Survival Without Major Comorbidities at Age 18 Years by Gestational Age at Birth and Birth Year, Sweden
eTable 5. Prevalence of AYA HOPE Comorbidity Index Diagnoses at Ages 18-43 Years by Gestational Age at Birth
eTable 6. Prevalence of Charlson Comorbidity Index Diagnoses at Ages 18-43 Years by Gestational Age at Birth
eTable 7A. Interactions Between Gestational Age at Birth and Sex in Relation to Survival Without Any AYA HOPE Comorbidities at Ages 18-43 Years
eTable 7B. Interactions Between Gestational Age at Birth and Sex in Relation to Survival Without Any CCI Comorbidities at Ages 18-43 Years
eTable 8. Co-sibling Analyses for Associations Between Gestational Age at Birth (1973-1997) and Survival Without Major Comorbidities Through 2015, Sweden