Abstract
Actinomyces is an anaerobic, gram-positive bacillus that is known to cause chronic granulomatous infections. Common risk factors predisposing patients to this life-threatening infection are recent dental procedures, immunosuppression from malignancy, or history of smoking and alcohol use. Actinomyces, commonly found in the normal flora of the oral cavity, is one of the pathogens that can cause Ludwig’s angina. Ludwig's angina is diffuse cellulitis and edema of the soft tissues of the neck and floor of the mouth. Cervicofacial actinomyces is an invasive infection that can form life-threatening abscesses through its rapid spread. Actinomyces turicensis is an isolate that has emerged recently to cause infections in humans. There are few reported cases of this species causing abdominal and genital infections; however, there is no report of it invading the cervicofacial space. A feared complication of Ludwig’s angina and cervicofacial actinomyces is airway compromise. Therefore, prompt initiation of intravenous antibiotics is required for the treatment and prevention of deadly complications. We present a patient with left-sided neck swelling after a recent oral surgical procedure and was found to grow Actinomyces turicensis on wound culture. The patient was treated with intravenous ampicillin-sulbactam, which not only decreased the swelling but improved the necrotic appearance of his abscess wound.
Keywords: Actinomyces, Actinomyces turicensis, Cervicofacial actinomycosis, Ludwig’s angina
Introduction
Actinomycosis is a chronic granulomatous infection. This unique microorganism is an anaerobic, filamentous, non-spore-forming, gram-positive bacillus that can be seen in the normal flora of oral, gastrointestinal and genital tracts [1]. Actinomyces spp. can cause severe infections if the organism infiltrates exposed tissues. The most common form is the cervicofacial actinomycosis. Patients who are at high risk for this life-threatening infection have typically undergone recent dental procedures or have had some sort of dental trauma. Other risk factors include immunosuppression from malignancy and a history of smoking or alcohol use (1).
Ludwig's angina is diffuse cellulitis and edema of the soft tissues of the neck and floor of the mouth. It originates in the submandibular gland and progresses to other spaces. The most common causative bacterial agents are Streptococci viridans, Staphylococcus aureus, and Staphylococcus epidermidis [2]. Typically, it is a polymicrobial infection involving those listed above along with anaerobes such as Actinomyces spp. and Peptostreptococcus spp. [2]. Mortality used to be greater than 50% mostly due to airway compromise; however, this has decreased significantly since the introduction of appropriate antibiotics and increased education on good dental hygiene [3]. Appropriate therapy includes maintenance of the airway, intravenous antibiotics, and surgical intervention if indicated [4]. Actinomyces turicensis is an emerging new isolate that can cause human infections [5]. It has been linked to meningitis and gynecological infections, however, it has not been associated with Ludwig’s angina in the past. Here we present the first case of Actinomyces turicensis presenting as cervicofacial actinomycosis causing Ludwig’s angina.
Case presentation
A 61-year-old male with a medical history of oral cancer status post chemotherapy and radiation therapy in remission presented with oral bleeding.
The patient was previously seen one month ago for extensive oral cavity bleeding, which required cauterization of the left retromolar area. He required 4 units of packed red blood cell transfusions. He was discharged once there were no further episodes of bleeding and his condition stabilized. One week since this procedure, he reported increased swelling in the submandibular region bilaterally, more so on the left side of his neck. Two weeks prior to this admission, he reported increasing pain that was dull and 7/10 in intensity, localized to his left neck. On the morning of this admission, he was noted to have a small amount of oral bleeding and decided to come to the hospital for further evaluation.
Upon initial presentation, he was afebrile with a heart rate of 71 beats per minute, respiratory rate of 14 breaths per minute, blood pressure of 135/65 and oxygen saturation of 89% on room air. On physical examination, he was awake, alert, and in mild respiratory distress. On neck examination, there was an 8 by 5 cm left-sided fluctuant mass with central darkening and serous drainage and a right-sided 4 by 4 cm fluctuant mass. There was no evidence of stridor or visible oral bleeding at this time. He was started on intravenous (IV) Vancomycin and Piperacillin-tazobactam on admission. Due to the concern of recurrence of oral cancer, ENT and oncology were consulted.
Computerized tomography (CT) neck soft tissue with and without contrast showed a mass-like infiltration involving the larynx and deep spaces of the neck, more significant on the left side with a mild narrowing of the supraglottic airway. Magnetic resonance imaging (MRI) neck soft tissue showed diffuse soft tissue swelling involving the deep spaces of the neck, base of the tongue, and left submandibular region with fluid measuring 1 cm surrounding the left sternocleidomastoid muscle. A CT guided biopsy of the neck was performed and showed benign, suppurative material consistent with abscess contents.
As his hospitalization progressed, the left side of his neck seemed to have a draining opening with a necrotic appearance associated with a foul smell. Wound culture was positive for Actinomyces turicensis. Infectious disease (ID) was consulted for further antibiotic management. His antibiotics were switched to IV Penicillin G, levofloxacin, and metronidazole. He also underwent aggressive bedside wound debridement of the necrotic tissue. The patient had significant improvement of the swelling after seven days of antibiotic treatment, thus precluding the need for surgical intervention. His clinical status was improving and upon discharge, ID switched the antibiotics to IV ampicillin-sulbactam. He required long term IV antibiotic treatment for four to six weeks before he could be transitioned to oral antibiotics. He was discharged home with home health and IV ampicillin-sulbactam for a total of six weeks.
Discussion
Cervicofacial actinomycosis is a rare, invasive bacterial disease that can lead to the development of life-threatening abscesses through its rapid spread. Actinomyces spp. are filamentous, anaerobic, gram-positive bacilli that typically reside in the normal flora of the human oral, gastrointestinal and genital tracts [6]. This specific microorganism has the potential to cause serious infections when it invades exposed tissue or lesions. It can develop into a chronic granulomatous infection with characteristic sulfur granules and fragments. The components of the yellowish sulfur granules are clusters of bacteria confined within a biofilm [6]. While there are many predisposing conditions involving the pathophysiology pathway of cervical actinomycosis, the most common mode of transmission is through oral mucosal trauma such as dental extraction or gingival trauma [6]. Actinomyces is often misdiagnosed and can present under the guise of malignancy [7].
Actinomyces spp. are a known cause of Ludwig’s angina, which is defined as diffuse cellulitis involving the submandibular, sublingual or submental spaces, characterized by its ability to rapidly spread to the surrounding tissues [8]. It usually starts as a submandibular space infection, later spreading to the sublingual space on the ipsilateral side [9]. The major cause of Ludwig’s angina is odontogenic infection with penetrating injury to the floor of the mouth [9]. Initially, the swelling can be confined to a particular area but can lead to major respiratory complications via rapid lymphatic spread. Airway management remains a top priority in these patients as this is primarily the leading cause of death [8]. Early detection and immediate initiation of treatment with antibiotics are essential in preventing life-threatening complications, such as necrotizing fasciitis and airway obstruction. Ludwig’s angina is a medical emergency, especially in its later stages. Emergency cricothyroidotomy or tracheostomy is indicated in patients who are unable to maintain their airway [8]. For those patients who develop abscesses, such as those from cervicofacial actinomycosis, and are unresponsive to medical management, surgery is indicated for decompression of the oral space and external incision and drainage (Fig. 1, Fig. 2).
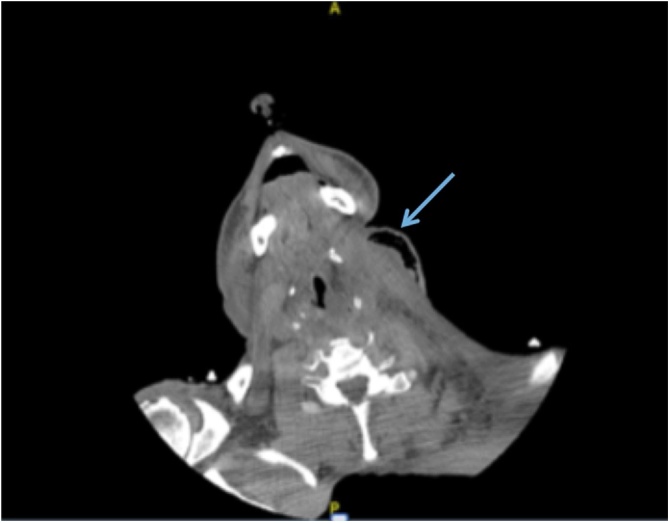
Fig. 1.
CT Soft Tissue Neck w/o contrast showing left-sided soft tissue emphysema.
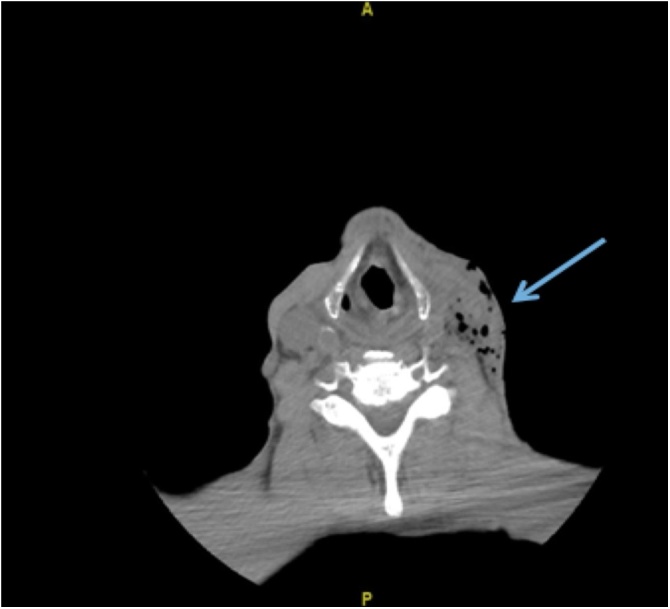
Fig. 2.
CT Soft Tissue Neck w/o contrast showing improvement of left-sided swelling and emphysema after seven days of IV antibiotic treatment.
A thorough history and physical is required to clinically make the diagnosis of Ludwig's angina. Patients should always be questioned about recent oral cavity or dental procedures. In our case, the patient had a cauterization of the trigone cavity area weeks prior to developing the infection. This was determined to be the known cause of cellulitis. Ludwig's angina is commonly polymicrobial as this is the normal flora of the oral cavity. The most common organisms are Streptococcus spp along with anaerobes such as Peptostreptococcus spp. and Actinomyces spp. [8].
Actinomyces turicensis is a rare isolate from the Actinomyces genus. There are a limited number of cases reported regarding this particular organism causing human infections, but no reports of association with Ludwig’s angina. Actinomyces turicensis has been described as a microorganism involving genital, urinary tract and skin infections most of the time [10]. The table below provides a thorough description of the different types of infections, mainly abdominal or gynecological, caused by this species (Table 1).
Table 1.
Types of Infections caused by Actinomyces Turicensis.
| Reference | Age | Diagnosis | Country | Therapy | Sequel |
|---|---|---|---|---|---|
| [11] | 43 | Mastoiditis/Meningitis | Hungary | Medicine/Surgery (Mastoidectomy) | Death |
| [12] | 42 | Pelvic-abdominal peritonitis | Netherlands | Medicine/Surgery (Explorative laparotomy) | Treated successfully |
| [13] | 80 | Pyometra | Japan | Medicine | Treated successfully |
| [14] | 30 | Liver abscess/Eustachian Valve endocarditis | Michigan, United States of America (USA) | Medicine/Surgery (Surgical drainage) | Treated successfully |
| [15] | 22 | Breast | United Kingdom (UK) | Medicine | Treated successfully |
| [16] | 73 | Left iliac fossa mass and liver lesions | Australia | Medicine | Treated successfully |
| [17] | 33 | Right breast abscess | United Kingdom | Needle aspiration/Medicine | Complete resolution |
| [18] | 59 | Hepatic abscess | Minnesota, USA | Medical | Complete recovery |
| [19] | 23 | Right knee joint | Germany | Medicine/surgery | Successfully Treated |
| [20] | 64 | Anterior abdominal wall | Italy | Surgery/Medicine | Successfully Treated |
| [21] | 44 | Right breast | Spain | Medicine | Successfully Treated |
In conclusion, with the increased availability of broad-spectrum antibiotics and the education provided on proper oral hygiene, the incidence of Ludwig’s angina has decreased and is now a rare emergency in the United States [8]. Cervicofacial actinomycosis is uncommon, however, when presented it can be treated effectively with IV antibiotics, specifically Penicillin, for four to six weeks. Prompt evaluation and initiation of treatment are required to prevent the mortality of this severe infection.
Declaration of Competing Interest
I hereby enclose a letter that there are no conflicts of interests for the submission of “Actinomyces turicensis: An Unusual Cause of Cervicofacial Actinomycosis presenting as Ludwig Angina in an Immunocompromised Host - Case Report and Literature Review”. Thank you for your time and interest.
References
- 1.Moghimi M., Salentijn E., Debets-Ossenkop Y., Karagozoglu K.H., Forouzanfar T. Treatment of cervicofacial actinomycosis: a report of 19 cases and review of literature. Med Oral Patol Oral Cir Bucal [Internet] 2013;18(July (4)):e627–32. doi: 10.4317/medoral.19124. https://www.ncbi.nlm.nih.gov/pubmed/23722146 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kassam K., Messiha A., Heliotis M. Ludwig’s angina: the original angina. Case Rep Surg [Internet] 2013;22(May 2013):974269. doi: 10.1155/2013/974269. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saifeldeen K. Ludwig’s angina [Internet] Emerg Med J. 2004;Vol. 21:242–243. doi: 10.1136/emj.2003.012336. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moreland L.W., Corey J., McKenzie R. Ludwig’s angina: report of a case and review of the literature. Arch Intern Med [Internet] 1988;148(2):461–466. doi: 10.1001/archinte.148.2.461. https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/609468 Available from: [DOI] [PubMed] [Google Scholar]
- 5.Könönen E., Wade W.G. Actinomyces and related organisms in human infections. Clin Microbiol Rev [Internet] 2015;28(April (2)):419–442. doi: 10.1128/CMR.00100-14. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valour F., Sénéchal A., Dupieux C., Karsenty J., Lustig S., Breton P. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist [Internet] 2014;5(July 7):183–197. doi: 10.2147/IDR.S39601. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong V.K., Turmezei T.D., Weston V.C. Actinomycosis. BMJ. 2011;343:d6099. doi: 10.1136/bmj.d6099. [DOI] [PubMed] [Google Scholar]
- 8.Pak S., Cha D., Meyer C., Dee C., Fershko A. Ludwig’s angina. Cureus [Internet] 2017;9(August (8)):e1588. doi: 10.7759/cureus.1588. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balasubramanian S., Elavenil P., Shanmugasundaram S., Himarani J., Raja V.B.K. Ludwig’s angina: a case report and review of management. SRM J Res Dental Sci [Internet] 2014;5(July (3)):211. http://www.srmjrds.in/article.asp?issn=0976-433X;year=2014;volume=5;issue=3;spage=211;epage=214;aulast=Balasubramanian 1 [cited 2019 Apr 12] Available from: [Google Scholar]
- 10.Chudácková E., Geigerová L., Hrabák J., Bergerová T., Liska V., Scharfen J., Jr Seven isolates of Actinomyces turicensis from patients with surgical infections of the anogenital area in a Czech hospital. J Clin Microbiol [Internet] 2010;48(July (7)):2660–2661. doi: 10.1128/JCM.00548-10. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kocsis B., Tiszlavicz Z., Jakab G., Brassay R., Orbán M., Sárkány Á. Case report of Actinomyces turicensis meningitis as a complication of purulent mastoiditis. BMC Infect Dis [Internet] 2018;18(December (1)):686. doi: 10.1186/s12879-018-3610-y. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eenhuis L.L., de Lange M.E., Samson A.D., Busch O.R.C. Spontaneous bacterial peritonitis due to Actinomyces Mimicking a perforation of the proximal jejunum. Am J Case Rep [Internet] 2016;26(August 17):616–620. doi: 10.12659/AJCR.897956. https://www.ncbi.nlm.nih.gov/pubmed/27561364 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hagiya H., Ogawa H., Takahashi Y., Kimura K., Hasegawa K., Otsuka F. Vol. 54. Internal Medicine; 2015. pp. 2775–2777. (Actinomyces turicensis bacteremia secondary to pyometra [internet]). Available from: [DOI] [PubMed] [Google Scholar]
- 14.Kottam A., Kaur R., Bhandare D., Zmily H., Bheemreddy S., Brar H. Actinomycotic endocarditis of the eustachian valve: a rare case and a review of the literature. Tex Heart Inst J [Internet] 2015;42(1):44–49. doi: 10.14503/THIJ-13-3517. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdulrahman G.O., Gateley C.A. Vol. 35. Breast Disease; 2015. pp. 45–47. (Primary actinomycosis of the breast caused by actinomyces turicensis with associated peptoniphilus harei [internet]). Available from: [DOI] [PubMed] [Google Scholar]
- 16.Ong C., Barnes S., Senanayake S. Actinomyces turicensis infection mimicking ovarian tumour. Singapore Med J [Internet] 2012;53(January (1)):e9–e11. https://www.ncbi.nlm.nih.gov/pubmed/22252197 Available from: [PubMed] [Google Scholar]
- 17.Attar K.H., Waghorn D., Lyons M., Cunnick G. Rare species of actinomyces as causative pathogens in breast abscess. Breast J [Internet] 2007;13(September (5):501–505. doi: 10.1111/j.1524-4741.2007.00472.x. Available from: [DOI] [PubMed] [Google Scholar]
- 18.Riegert‐Johnson D.L., Sandhu N., Vincent Rajkumar S., Patel R. Vol. 35. Clinical Infectious Diseases; 2002. pp. 636–637. (Thrombotic thrombocytopenic purpura associated with a hepatic abscess due toActinomyces turicensis [internet]). Available from: [DOI] [PubMed] [Google Scholar]
- 19.Zautner A.E., Schmitz S., Aepinus C., Schmialek A., Podbielski A. Subcutaneous fistulae in a patient with femoral hypoplasia due to Actinomyces europaeus and Actinomyces turicensis. Infection [Internet] 2009;37(June (3)):289–291. doi: 10.1007/s15010-008-7392-9. Available from: [DOI] [PubMed] [Google Scholar]
- 20.Gatti M., Gasparini L.E., Grimaldi C.M., Abbati D., Clemente S., Brioschi P.R. Septic shock due to NSTI caused by Actinomyces turicensis: the role of clinical pharmacology. Case report and review of the literature. J Chemother [Internet] 2017;29(December (6)):372–375. doi: 10.1080/1120009X.2017.1306154. Available from: [DOI] [PubMed] [Google Scholar]
- 21.Cobo F. Breast abscess due to Actinomyces turicensis in a non-puerperal woman. Enferm Infecc Microbiol Clin [Internet] 2018;36(June (6)):388–389. doi: 10.1016/j.eimc.2017.09.014. Available from: [DOI] [PubMed] [Google Scholar]